Abstract
Background
Malignant mesothelioma of the tunica vaginalis testis (MMTVT) is a rare disease with a poor prognosis. The diagnosis and management of these lesions are often difficult for pathologists, surgeons, oncologists and occupational physicians. A preoperative diagnosis of malignancy is rarely made, and there is no established effective therapy except orchidectomy.
Methods
A systematic literature review was conducted among the articles published in the English literature on primary MMTVT. Moreover four cases from the Apulia mesothelioma register are reported here.
Results
Two hundred eighty-nine cases of MMTVT have been reported from 1943 to 2018. Overall asbestos exposure has been investigated only for 58% of all cases reported in this review, while in 41.8% this data are not available. Noteworthy is the fact that in many reports there is not an anamnestic reconstruction of any asbestos exposure. A history of direct occupational, environmental or familial asbestos exposure is found in 27.6% of the cases. The four cases from the Apulia mesothelioma register are all with ascertained occupational exposure to asbestos.
Conclusions
The true incidence of asbestos exposure in MMTVT is underestimated because of insufficient information reported in older literature. To establish a broad consensus on the causal relationship between asbestos and MMTVT in the scientific community its necessary to analyze the same variables in the epidemiological studies. In general it should be recommended that a positive history of exposure to asbestos or to asbestos–containing materials are at risk for the development of a MMTVT and should be monitored.
Keywords: Asbestos, Mesothelioma, Tunica vaginalis, Review, Apulia southern Italy, Mesothelioma register
Background
Malignant mesothelioma (MM) is a rare tumour that can occur in the body cavities covered by mesothelium, i.e., the pleura, peritoneum, pericardium and testicular vaginal tunica [1], with benign and malignant variants. Among MM cases, a very small percentage (< 3%) [2] arise in the tunica vaginalis testis. Malignant mesothelioma of the testicular vaginal tunica (MMTVT) is very rare with potentially aggressive behaviour, and it can invade the testicular parenchyma, spermatic cord, epididymis and subcutaneous tissue of the penis; therefore, it has also been classified with the term paratesticular mesothelioma [3], rather than adenomatoid tumours, malignant adenomatoid tumours, mixed mesoblastic tumours or other various diagnoses, which is how it has been misinterpreted in the past [4–9]. The confusion over nomenclature was due to the difficulty of histological classification [10].
Over the years, three groups of mesothelial tumours have been identified, defined and classified: well differentiated papillary mesothelioma (WDPM); an emerging diagnostic category of papillary mesothelioma with borderline features or localized mesothelioma of low grade malignancy, also called mesothelioma of uncertain malignant potential (MUMP); and mesothelioma of low malignancy potential (MLMP) [11, 12], representing a morphological continuum between WDPM and malignant mesothelioma (MM) [11, 13].
As reported by Rankin (1956) [10] and by Kossow (1981) [14], the first two cases of mesothelioma of the genital tract were reported in 1912 by Naegeli [15] and in 1916 by Sakaguchi [16], followed by Thompson (1936), Evans (1943), Golden and Ash (1945), Lee (1950), Bailey (1955) and Barbera (1957) [4, 17–21], although the last was actually classified as benign papillary mesothelioma (WDPM). These cases were described by various names until 1970, when Marcus and Lynn [22] demonstrated by electron microscopy that there were no differences between so-called adenomatoid tumours and malignant mesothelioma [23].
To date, the WHO(world health organization) classification of tumours of the urinary system and male genital organs [24], in the classification of tumours of the testis and paratesticular tissue, has reported MM and the WDPM, noting that the latter “may have a progression to malignant mesothelioma if the lesions are not completely excised”.
This review points out only case series and case reports of primary MM of the tunica vaginalis testis. We conducted a comprehensive review from Medline (National Library of Medicine database) and a PubMed database search of the English medical literature and on the references lists of published articles. Nevertheless, the data are often incomplete or not comparable due to the long period covered by the scientific literature examined (1943-2018) and the relative evolution of diagnostic techniques and classifications of mesotheliomas, as well as knowledge about the risk factors related to the onset of the disease [5, 21, 25, 26]. Similarly, despite the rarity of this disease, all of the various reviews reported might not indicate the true incidence because of the relatively recent agreement about the definition of the clinicopathologic entity. In addition, we report four cases from the Apulia (Southern Italy) mesothelioma register.
Methods
A PubMed computerized search was performed using the following keywords: mesothelioma tunica vaginalis testis (127 articles), testicular (276 articles), paratesticular (50 articles), testis (179 articles), and scrotum (46 articles); and it was filtered for human patients and English language. The English literature search without time limits, from 1943 to 2018, the cut-off date was December 15, 2018, and were identified a total of more than 276 previously published scientific articles on MMTVT (MEDLINE-PUBMED National Library of Medicine, National Center for Biotechnology Information; available from URL: http://www.ncbi.nlm.nih.gov/pubmed).
We undertook a review using the following criteria: we excluded articles with the diagnosis of benign mesothelioma as stated by the authors on the basis of histopathological findings and cases of adenomatoid tumours and other benign tumours and WDPM [27], although some authors, such as Grove (1989) [28], suggested that these tumours should always be considered “borderline malignancy”. Similarly, cases with doubtful primary tumour origin or with concomitant pleural or peritoneal disease were excluded.
Using the above criteria, the review of the literature to date revealed 289 previously described cases in 165 published articles from PubMed and from the reference lists of the available publications in the English literature, which we considered bona fide malignant MTVT(Table 1) [4, 5, 9, 11–14, 23, 28–184].
Table 1.
Summary features MMTVT cases (1943-2018)
| N° | Year | Author (Reference) | N° Cases | Age Years | Asbestos Exposure (latency in years) | Follow Up Months | Side-Laterality | Histologic Subtype | Recurrence Months | Clinical Presentation Onset |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 1943 | Evans [4] | 2 | 66 | NA | 2 | LEFT | NA | NA | MASS |
| 53 | NA | NA | LEFT | NA | NA | SMALL NODULE PAINLESS | ||||
| 2 | 1945 | Robinson [28] | 2 | 30 | NA | NA | NA | NA | NA | NA |
| 28 | NA | NA | NA | NA | NA | NA | ||||
| 3 | 1947 | Patterson [29] | 1 | NA | NA | NA | NA | NA | NA | NA |
| 4 | 1949 | Foote [30] | 1 | NA | NA | dead | NA | NA | metastasis | NA |
| 5 | 1949 | Fajers [5] | 5 | 27 | NA | NA | RIGHT | NA | NA | NA |
| 35 | NA | NA | LEFT | NA | NA | NA | ||||
| 50 | NA | NA | LEFT | NA | NA | NA | ||||
| 45 | NA | NA | RIGHT | NA | NA | NA | ||||
| 58 | NA | Na | RIGHT | NA | NA | NA | ||||
| 6 | 1958 | Reynolds [31] | 1 | 45 | NO | 6 alive | RIGHT | papillary epithelioid | NA | LARGE MASS HYDROCELE |
| 7 | 1968 | Kozlowski [32] | 1 | 63 | NA | NA | spermatic cord | biphasic | NA | MASS |
| 8 | 1968 | Abell [9] | 2 | 78 | NA | 45 dead | NA | biphasic | metastasis | NA |
| 70 | NA | 16 dead | NA | biphasic | metastasis | NA | ||||
| 9 | 1969 | Kasdon [33] | 2 | 58 | NA | 36 dead | RIGHT | papillary epithelioid | 12 | HYDROCELE |
| 72 | NA | 36 recurrence | RIGHT | papillary epithelioId | 5 | HYDROCELE | ||||
| 10 | 1969 | Arlen [34] | 1 | 40 | NA | 216 | LEFT spermatic cord | NA | metastasis | MASS |
| 11 | 1973 | Johnson [35] | 1 | 23 | NA | 3 | RIGHT | papillary epithelioid | 3 alive | SWELLING AND MILD DISCOMFORT |
| 12 | 1975 | Fishelovitch [36] | 1 | 60 | NA | 12 alive | LEFT | papillary epithelioid | NO | SWELLING, HYDROCELE |
| 13 | 1976 | Fligiel [37] | 1 | 68 | pipe insulator for 40 years (pleural plaque) | 20 dead | RIGHT | papillary epithelioid | NA | PAIN AND SWELLING |
| 14 | 1976 | Pugh [38] | 2 | NA | NO | 48 alive | NA | papillary epithelioid | NO | HYDROCELE |
| NA | NO | 84 | NA | papillary epithelioid | 84 recurrence | HYDROCELE | ||||
| 15 | 1976 | Pizzolato [39] | 1 | 57 | Sugar raffinery worker | 41 dead | RIGHT | papillary epithelioid | 12 recurrence | URETHRAL STRUCTURE, SECONDARY URINARY EXTRAVASION WITH URETHRITIS AND RECURRENT INGUINAL HERNIA |
| 16 | 1977 | Eimoto [40] | 1 | 35 | NO | 2 dead | LEFT | fibrous | NA | SWELLING |
| 17 | 1977 | Tuttle [41] | 1 | 37 | NA | NA | RIGHT spermatic cord | fibrous | NA | MASS |
| 18 | 1978 | Sinha [42] | 1 | 65 | NA | 24 alive | RIGHT | papillary epithelioid | NA | SWELLING |
| 19 | 1978 | Jaffe [43] | 1 | 77 | NO | 12 dead | LEFT | papillary epithelioid | Local recurrence | SWELLING |
| 20 | 1981 | Benisch [44] | 1 | 64 | NO | 8 | SCROTUM NA | fibrous | NO | MASS |
| 21 | 1981 | Kossow [14] | 1 | 50 | NA | 24 NED | RIGHT | papillary epithelioid | NO | MASS |
| 22 | 1981 | Blitzer [45] | 1 | 74 | NA | 30 | LEFT spermatic cord | NA | NO | PAINLESS, MASS |
| 23 | 1982 | Japko [46] | 1 | 30 | Insulator for 8 years | 6 NED | RIGHT | Biphasic | NO | SWELLING |
| 24 | 1982 | Chen [47] | 1 | 64 | NA | 30 dead | RIGHT | Biphasic | 24 recurrence | SWELLING |
| 25 | 1982 | Hollands [48] | 1 | 63 | NA | 24 | RIGHT TESTIS | Biphasic | 12 recurrence | HYDROCELE, SWELLING |
| 26 | 1982 | Slaysman [49] | 1 | 20 | NA Maffucci Syndrome | NA | bilateral | papillary epithelioid | Recurrence bilateral | SWELLING |
| 27 | 1983 | Zidar [50] | 1 | 63 | NA | 32 | NA | papillary epithelioid | NA | NA |
| 28 | 1983 | Mc Donald [51] | 2 | 21 | NA | 24 | RIGHT HEMI-SCROTUM bilateral | papillary epithelioid | 24 recurrence | PAINFUL GRADUAL ENLARGMENT |
| 29 | NA | 20 NED | RIGHT HEMI-SCROTUM | papillary epithelioid | NO 20 | PAINFUL GRADUAL ENLARGMENT | ||||
| 29 | 1983 | Van Der Rhee [52] | 1 | 86 | NO | 36 dead | LEFT HEMI-SCROTUM | papillary epithelioid | 12 recurrence | HAEMATOSCROTUM |
| 30 | 1984 | Antman [53] | 6 | 58 | pipefitter | 60 | LEFT INGUINAL | papillary solid polypoid tissue | 60 metastasis | HYDROCELE, INGUINAL HERNIA |
| 73 | shipyard plumber for 25 years | 33 dead | RIGHT | papillary epithelioid | 12 metastasis | HYDROCELE | ||||
| 23 | NA | 180 | LEFT | NA | 180 metastasis | SLOWLY ENLARGEMENT | ||||
| 63 | machinist for 20 years | 48 dead | LEFT | papillary epithelioid | 4 metastasis | MASS | ||||
| 52 | NO | 24 dead | RIGHT | papillary epithelioid | 14 metastasis | MASS | ||||
| 43 | construction worker for 16 years | 48 NED | RIGHT | papillary epithelioid | NO | EPIDIDIMITE | ||||
| 31 | 1984 | Yamanishi [54] | 1 | 34 | NA | 6 | RIGHT | biphasic | NO | MASS |
| 32 | 1984 | Khan [55] | 1 | 42 | NO | 9 dead | RIGHT epididymis | biphasic | 6 metastasis | PAINFULL, SWELLING |
| 33 | 1985 | Vakalikos [56] | 1 | 26 | NA | 12 NED | RIGHT | papillary pseudotu-bular | NO 12 | SWELLING INGUINAL |
| 34 | 1985 | Ehya [57] | 1 | 63 | NA | 52 | LEFT | papillary epithelioid | 50 metastasis | HYDROCELE |
| 35 | 1986 | Karunaharan [58] | 1 | 40 | plastic fenolica worker for 20 years | 14 dead | RIGHT | glandular structure papillary epithelioid | 9 metastasis 12 local recurrence | IRREGULAR MASS |
| 36 | 1986 | Petersen [59] | 1 | 51 | NA | 30 | NA | NA | 30 alive recurrence | NA |
| 37 | 1987 | Cartwright [60] | 1 | 49 | NA | 4 | RIGHT | papillary epithelioid | 24 metastasis | HYDROCELE |
| 38 | 1987 | Fitzmaurice [61] | 1 | 72 | NA | 18 NED | LEFT | papillary epithelioid | NO 18 | SWELLING |
| 39 | 1988 | Linn [62] | 1 | 20 | NA | NA | LEFT | papillary epithelioid | NA | PAIN, SWELLING |
| 40 | 1988 | Prescott [63] | 1 | 61 | Pleural plaques | 21 dead | LEFT |
Biphasic papillary, pseudo-glandular component |
8 Local recurrence metastasis |
HYDROCELE |
| 41 | 1988 | Velasco [64] | 1 | 14 | NA | 24 | LEFT | papillary epithelioid | NO 24 | ABDOMINAL MASS |
| 42 | 1989 | Tyagi [65] | 1 | 79 | Shipyard worker | 24 dead | LEFT | papillary epithelioid | metastasis | SWELLING |
| 43 | 1989 | Grove [27] | 66 | Carpenter for 10 years | 42 | RIGHT | papillary epithelioid |
24 metastasis 42 alive local recurrence |
SWELLING HYDROCELE |
|
| 79 | NO | 60 dead | RIGHT | epithelial papillary | 60 Prostatic metastasis | MASS | ||||
| 58 | NO | 108 NED | LEFT | Tubule papillary | 108 NED | HYDROCELE | ||||
| 44 | 1990 | Kamiya [66] | 1 | 32 | NO | 5 | LEFT | papillary | NO 5 | ELASTIC AND INDOLENT TUMOR |
| 45 | 1990 | Smith [67] | 1 | 57 | NO | alive | LEFT | papillary epithelioid | 48 Local recurrence metastasis | SWELLING |
| 46 | 1990 | Carp [23] | 1 | 54 | NO | 64 dead | LEFT | papillary epithelioid | 38 Local recurrence metastasis | MASS |
| 47 | 1991 | Kuwabara [68] | 1 | 60 | NO | 65 dead | RIGHT | Biphasic | 60 metastasis | SWELLING |
| 48 | 1992 | Pfister [69] | 1 | 7 | NA | 16 | LEFT | papillary epithelioid | NO 16 | SWELLING |
| 49 | 1992 | Adler [70] | 1 | 62 | occupational | 12 | RIGHT | NA | NO 12 | PAINFUL ENLARGEMENT |
| 50 | 1992 | Serio(7 [71] | 1 | 69 | railway cleaner for 10 years | 10 | LEFT | tubulo-papillary | NO 10 | SWELLING |
| 51 | 1992 | Noble [72] | 1 | 62 | NA | NA | LEFT | papillary epithelioid | NA | SWELLING, HYDROCELE |
| 52 | 1992 | Fields [73] | 1 | 91 | Steel industry worker indirect exposure | NA | NA | Biphasic | NA | SWELLING |
| 53 | 1994 | Moch [74] | 1 | 80 | NO | 25 NED | RIGHT | papillary epithelioid | NO | PAINLESS SWELLING |
| 54 | 1994 | Saw [75] | 1 | 63 | Occupational for 7 years [20] | 6 | LEFT | Biphasic | NO 6 | HYDROCELE |
| 55 | 1994 | Reynard [76] | 1 | 76 | NA | NA | RIGHT | tubulo-glandular | 1 recurrence | PAINLESS SWELLING |
| 56 | 1994 | Wenger [77] | 1 | 25 | NA | NA | RIGHT | NA | NA | PAINFUL MASS |
| 57 | 1994 | Watanabe [78] | 1 | 67 | Insulator for 17 years asbestosis | 10 dead | LEFT | biphasic | multifocal | NA |
| 58 | 1995 | Amin [79] | 1 | 59 | NO | 189 | RIGHT | papillary epithelioid | NO 188 | PAINLESS SWELLING |
| 59 | 1995 | Magoha [80] | 1 | NA | NA | NA | NA | fibrous | NA | NA |
| 60 | 1995 |
Huncharek [81] |
1 | 45 | insulator Electrical power plant | 144 | RIGHT | epithelial | NO | PAINLESS MASS |
| 61 | 1995 | Umekawa [82] | 1 | 67 | NO | 8 dead | RIGHT | epithelial | 6 metastasis | SWELLING |
| 62 | 1995 | Eden [83] | 2 | 62 | NO | 6 | LEFT | NA | NO 6 | HYDROCELE |
| 76 | Chemist for 10 years | 27 alive | LEFT | epithelial | 6 recurrence | HYDROCELE | ||||
| 63 | 1995 | Joseph [84] | 1 | 26 | NA | NA | LEFT | NA | NA | TWO PINK TO-PURPLE NODULES |
| 64 | 1995 | Lopez [85] | 1 | 47 | NA | 36 | NA | papillary epithelioid | NO 36 | HYDROCELE |
| 65 | 1995 | Jones [86] | 11 | 75 | NA | Lost follow up | NA | epithelial | NA | HYDROCELE |
| 12 | NA | 12 ned | NA | epithelial | NO 12 | HYDROCELE | ||||
| 39 | NO | 3 | NA | epithelial | NA | PARATESTICULAR MASS | ||||
| 50 | NO | 24 | NA | epithelial | 24 local recurrence | HYDROCELE | ||||
| 41 | NO | 3 | NA | biphasic | NA | PARATESTICULAR MASS | ||||
| 65 | NA | 180 | NA | biphasic | 180 metastasis | PARATESTICULAR MASS | ||||
| 76 | pipe fitter for 10 years | 48 dead | NA | biphasic | NA | HYDROCELE | ||||
| 58 | NA | 36 dead | NA | biphasic | NA | HYDROCELE | ||||
| 67 | NO | 3 | NA | biphasic | NA | PARATESTICULAR MASS | ||||
| 70 | NA | 48 dead | NA | epithelial | NA | HYDROCELE | ||||
| 42 | NA | 24 | NA | epithelial | Alive with disease | HYDROCELE | ||||
| 66 | 1996 | Ahmed [87] | 1 | 80 | dock worker for 10 years | 24 dead | LEFT | papillary epithelioid | 3 local recurrence | HYDROCELE |
| 67 | 1996 | Ascoli [88] | 1 | 55 | Insulator | 6 | RIGHT | biphasic | NA | SWELLING |
| 68 | 1996 | Mathew [89] | 2 | 70 | NA | 3 dead | LEFT | NA | spinal metastasis | SWELLING |
| 58 | NA | 2 dead | RIGHT | NA | spinal metastasis | ENLARGMENT | ||||
| 69 | 1997 | Berti [90] | 1 | 75 | NO | 15 | LEFT | papillary epithelioid | NO 15 | HYDROCELE |
| 70 | 1997 | Agapitos [91] | 2 | 60 | NA | 20 | LEFT | biphasic | NA | SWELLING |
| 84 | NA | 10 | LEFT | biphasic | NO 10 | HYDROCELE | ||||
| 71 | 1997 | Khan [92] | 1 | 6 | NA | 24 | BILATERAL | papillary epithelioid | NO 24 | HYDROCELE |
| 72 | 1998 | Gupta SC [93] | 1 | 36 | NO | 10 | RIGHT | papillary epithelioid | 1,5 metastasis | HYDROCELE |
| 73 | 1998 | Lee [94] | 2 | 45 | NA | 4 | RIGHT | NA | 4 metastasis | HYDROCELE |
| 66 | NA | 6 | LEFT | papillary epithelioid | NO 6 | HYDROCELE | ||||
| 74 | 1998 | Plas [95] | 1 | 14 | NO | 12 | RIGHT | papillary epithelioid | NO 12 | ENLARGEMENT |
| 75 | 1999 | Kanazawa [96] | 1 | 38 | maintenance air conditioning system for 20 years | 156 | BILATERAL | epithelial | 36 local recurrence | INGUINAL HERNIA |
| 76 | 1999 | Harmse [97] | 1 | 70 | NO | 120 | RIGHT | epithelial | NA | MASS |
| 77 | 1999 | Gupta NP [98] | 2 | 69 | NA | 18 dead | RIGHT | biphasic | metastasis | SWELLING |
| 51 | NA | 5 dead | LEFT | biphasic | metastasis | ENLARGEMENT | ||||
| 78 | 2000 | Fujisaki [99] | 1 | 32 | NO | 36 | RIGHT | epithelial | NO 36 | SWELLING |
| 79 | 2000 | Poggi [100] | 1 | 47 | NA | 8 | RIGHT | epithelial | NA | PARATESTICULAR MASS |
| 80 | 2000 | Attanoos [13] | 3 | 71 | dockyard crane driver for 20 years (ASBESTOS BODIES) | NA | RIGHT | biphasic | NA | HYDROCELE |
| 77 | NO | 50 | LEFT | epithelial | NA | MASS | ||||
| 33 | NO | 37 | LEFT | epithelial | NA | MASS | ||||
| 81 | 2000 | Ferri [101] | 1 | 64 | NA | 36 | NA | epithelial | NA | OSTRUZIONE CERVICO-URETRALE |
| 82 | 2001 |
Wolanske [102] |
1 | 71 | NO | 3 | RIGHT | NA | NO 3 | NODLE |
| 83 | 2001 | Sebbag [103] | 2 | 34 | NO | 62 alive | LEFT | epithelial | NO 6O | INGUINAL MASS |
| 19 | NO | 24 dead | LEFT | epithelial | 11 recurrence | SCROTAL MASS | ||||
| 84 | 2001 | Gurdal [104] | 1 | 67 | NO | 30 | RIGHT | epithelial | 24 recurrence | HYDROCELE RECIDIVANTE |
| 85 | 2002 | Abe [105] | 1 | 81 | NO | 12 dead | LEFT | epithelial | 7 metastasis | HYDROCELE |
| 86 | 2002 | Bruno [106] | 1 | 85 | NO | NA | RIGHT HEMI-SCROTUM | epithelial | NA | SWELLING |
| 87 | 2002 |
Iczkowski [107] |
1 | 71 | NO | 26 dead | LEFT HEMI-SCROTUM | epithelial | 19 liver metastasis | PAINFULL SWELLING |
| 88 | 2003 | Black [108] | 1 | 67 | NA | 36 dead | RIGHT | epithelial | 3 recurrence | HYDROCELE |
| 89 | 2003 | Garcia de Jalon [109] | 1 | 78 | carpenter | 3 | RIGHT | tubulo-papillary | 3 metastasis | INCREASE IN THE VOLUME THE TESTIS |
| 90 | 2004 | Pelzer [110] | 1 | 21 | NO | 24 | BILATERAL | epithelial | NA | RECURRENT PAIN |
| 91 | 2004 | Sawada [111] | 1 | 48 | NO | 72 | RIGHT | biphasic | NO 72 | SWELLING |
| 92 | 2004 | Mishra [112] | 1 | 75 | NA | NA | NA | NA | NA | NA |
| 93 | 2004 | Shimada [113] | 1 | 64 | NO | 18 | RIGHT | biphasic80% sarco-matoid | NO | SWELLING |
| 94 | 2005 | Wang [114] | 1 | 81 | NO | NA | RIGHT | tubulo-papillary | NA | SCROTAL MASS |
| 95 | 2005 | Gorini [115] | 2 | 67 | maintenance of locomotives for 30 years [42] | 24 | LEFT | epithelial | NO 24 | MASS |
| 80 | maintenance of tractors for 6 years [67] | 24 | RIGHT | biphasic | NA | SWELLING | ||||
| 96 | 2005 | Spiess [116] (no individual data) | 5 | 57-83 | 4 | 5-68 (4 dead 1 disease free survival 68) | NA | NA | Metastasis in 4 cases | NA |
| 97 | 2006 |
Van Apeldoorn [117] |
1 | 83 | NO but with pleural thickening at CT | 1 dead | RIGHT | epithelial | liver metastasis |
SCROTAL ENLARGEMENT Chyluria |
| 98 | 2006 | Schure [118] | 3 | 45 | NO | 48 | LEFT | NA | NO 48 | SWELLING |
| 35 | NO | 4 dead | LEFT | NA | 2 metastasis | MASS INGUINO-SCROTAL | ||||
| 26 | NO | 18 | LEFT | NA | NO 18 | INGUINAL MASS | ||||
| 99 | 2006 |
Winstanley [119] |
18 | 54 | NO | 12 dead | RIGHT | NA | NA | FOLLOWING A FALL |
| 56 | Dockyard worker | 60 | NA | NA | 60 metastasis | SOVRAPUBIC MASS | ||||
| 59 | NO | 24 dead | LEFT | NA | NA | RECURRENT HYDROCELE | ||||
| 52 | NO | 48 | LEFT | NA | NO 48 | RECURRENT HYDROCELE | ||||
| 49 | NA | 24 | NA | NA | NO 24 | HYDROCELE | ||||
| 79 | NA | 1 | LEFT | NA | NO 1 | HYDROCELE | ||||
| 70 | NA | 12 dead | RIGHT | NA | NA | BLOOD STAINED HYDROCELE | ||||
| 62 | NA | 24 dead | LEFT | NA | NO | RECURRENT HYDROCELE | ||||
| 45 | NA | 6 | LEFT | NA | NO 6 | SWELLING TESTICULAR | ||||
| 65 | NA | 60 | RIGHT | NA | NO 60 | HYDROCELE | ||||
| 75 | NO | 36 | LEFT | NA | NA | HYDROCELE | ||||
| 73 | NO | 12 dead | LEFT | NA | 12 metastasis | TESTICULAR SWELLING | ||||
| 45 | NA | 72 | NA | NA | NO 72 | NA | ||||
| 58 | NO | 36 | LEFT | NA | NO 36 | HYDROCELE HISTORY E YEARS | ||||
| NA | NA | NA | NA | NA | NA | NA | ||||
| NA | NA | NA | NA | NA | NA | NA | ||||
| NA | NA | NA | NA | NA | NA | NA | ||||
| NA | NO | NA | NA | NA | NA | NA | ||||
| 100 | 2007 | Al Qahtani [120] | 1 | 39 | NA | 84 | LEFT | NA | NO 84 | HYDROCELE |
| 101 | 2007 | Liguori [121] | 1 | 68 | NA | 70 | LEFT | epithelial | 24 recurrence | INGUINAL MASS |
| 102 | 2007 | Guney [122] | 1 | 45 | NO | 3 | RIGHT | papillary | NO 3 | TESTICULAR MASS |
| 103 | 2008 | Boyum [123] | 1 | 60 | NO | 23 | LEFT | biphasic | NA |
SCROTAL SWELLING RECURRENT EPIDIDYMITIS |
| 104 | 2008 | Candura [124] | 1 | 38 | petrochemical worker for 16 years | 15 | RIGHT | epithelial | NO 15 | HYDROCELE |
| 105 | 2008 | Mathur [125] | 2 | 65 | Farmer | NA | LEFT | papillary | NA | SWELLING |
| 60 | NA | NA | RIGHT | epithelial | NA | SWELLING | ||||
| 106 | 2008 | Ikegami [126] | 1 | 67 | Painting worker | 26 dead | RIGHT | epithelial | 24 liver metastasis | PAINLESS SWELLING |
| 107 | 2008 | Barui [127] | 1 | 42 | NO | NA | RIGHT | tubulo-papillary | NA | SCROTAL MASS |
| 108 | 2008 | Goel [128] | 1 | 65 | Farmer | 72 | LEFT | epithelial | NA | PAINLESS SWELLING |
| 109 | 2009 | Al Salam [129] | 1 | 83 | NO | NA | LEFT | epithelial | NA | SCROTAL SWELLING |
| 110 | 2009 | Baccheta [130] | 1 | 63 | NO | 30 dead | RIGHT | epithelial | NA | NA |
| 111 | 2009 | Chen [131] | 1 | 67 | Occupational [40] | 7 | RIGHT | biphasic | NO 7 | RIGHT HYDROCELE AND LONG-STANDING BILATERAL HYDROCELE |
| 112 | 2009 | De Lima [132] | 1 | 15 | NO | 12 | RIGHT | epithelial | PAINLESS INCREASE IN SCROTUM VOLUME | |
| 113 | 2010 |
Brimo MUMP [11] |
8 | 43 | NA | 108 alive | NA |
papillary tubulo papillary |
108 NED | HYDROCELE |
| 49 | NA | 24 alive | NA |
papillary tubulo papillary |
24 NED | HYDROCELE | ||||
| 73 | NA | 8 alive | NA |
papillary tubulo papillary |
8 NED | HYDROCELE | ||||
| 34 | NA | 36 alive | NA |
papillary tubulo papillary |
36 NED | SCROTAL MASS | ||||
| 61 | NA | 60 dead | NA |
papillary tubulo papillary |
18 NED | HYDROCELE | ||||
| 53 | NA | 564 dead | NA |
papillary tubulo papillary |
564 | HYDROCELE | ||||
| 57 | NA | NA | NA |
papillary tubulo papillary |
NA | HYDROCELE | ||||
| 50 | NA | NA | NA |
papillary tubulo papillary |
NA | HYDROCELE | ||||
| 114 | 2010 |
Aggarwal [133] |
1 | 75 | NA | 76 dead | LEFT | NA | 30 recurrence | SCROTAL ENLARGEMENT |
| 115 | 2010 | Bisceglia [134] | 1 | 74 | NO | 101 | RIGHT | tubulo-papillary | 24 recurrence | TESTICULAR PAIN |
| 116 | 2010 | Klaassen [135] | 1 | 37 | NO | 6 | LEFT | papillary epitheliode | 6 NO | MASS |
| 117 | 2011 | Trpkov [12]MUMP | 1 | 57 | NO | 72 NED | NA | papillary epitheliode | NO | HYDROCELE |
| 118 | 2011 | Gupta R [136] | 1 | 80 | NA | NA | RIGHT |
tubulo- papillary |
NA | SWELLING OF 3 YEARS DURATION |
| 119 | 2011 | Park [137] | 1 | 65 | Foundry worker for 4 years | 6 dead | LEFT | papillary | 3 recurrence | PALPABLE MASS |
| 120 | 2011 | Grey Venyo [138] | 1 | 69 | NO | NA | LEFT | epithelial | 2 recurrence | SWELLING |
| 121 | 2011 | Bass [139] | 1 | 64 | worked on a naval vessel | 44 alive | LEFT | papillary | 20 recurrence | SCROTAL SWELLING |
| 122 | 2012 | Ahmed [140] | 1 | 78 | NO | 6 | RIGHT | epithelioid | NO 6 | PAINFUL SWELLING |
| 123 | 2012 | Whan Doo [141] | 1 | 36 | NO | 1 | RIGHT | NA | NO 1 | PAINLESS SWELLING |
| 124 | 2012 |
Abdelrahman [142] |
1 | 54 | Farmer | NA | RIGHT | biphasic | NA | SWELLING |
| 125 | 2012 | Esen [143] | 1 | 38 | NO | 26 | LEFT | epitheloid | NO 26 | PAIN AND SWELLING |
| 126 | 2012 | Bo Hai [144] | 6 | 26 | NO | 24 | LEFT spermatic cord | epithelial | NO 24 | SPERMATIC CORD MASS |
| 67 | NO | 24 | LEFT | epithelial | Local recurrence | SCROTAL MASS, BILATERAL HYDROCELE | ||||
| 57 | NO | 24 |
RIGHT spermatic cord |
epithelial | Local recurrence | MASS | ||||
| 46 | YES | 24 dead | LEFT | epithelial | DOD | ACUTE APPENDIX, TESTIS PAIN | ||||
| 78 | NO | 24 | LEFT | epithelial | Local recurrence | SCROTAL MASS, BILATERAL HYDROCELE | ||||
| 76 | YES | 24 dead | LEFT | epithelial | DOD | SCROTAL MASS | ||||
| 127 | 2012 | Priester [145] | 1 | 71 | NA | 24 dead | RIGHT | epithelial | 17 recurrence | HYDROCELE |
| 128 | 2012 | Heng Yen [146] | 1 | 53 | NO | 36 | LEFT | tubulopapillary | NO 36 | RECURRENT EPIDIDYMITIS, HYDROCELE |
| 129 | 2012 | Mrinakova [147] | 1 | 20 | environmental | 41 | LEFT TESTIS | papillary | NO 41 | PAINLESS HYDROCELE |
| 130 | 2012 | Mensi [148] | 13 | 72 | NA | 8 | RIGHT | epithelial | NA | HYDROCELE AND ENLARGEMENT |
| 73 | Familial for 4 years | 44 | LEFT | biphasic | NA | HYDROCELE | ||||
| 76 | Occupational maintenace worker for 32 years | 9 | LEFT | epithelial | NA | SCROTAL HERNIA | ||||
| 80 | Household for 11 years | 18 | RIGHT | biphasic | NA | HYDROCELE | ||||
| 60 | NA | 15 | RIGHT | epithelial | NA | INGUINAL-SCROTAL HERNIA | ||||
| 82 | Occupational spinner for 32 years | 25 | LEFT | sarcomatous | NA | TESTICULAR MASS | ||||
| 38 | Occupational maintenace worker for 16 years | 33 | RIGHT | epithelial | NA | TESTICULAR PAIN AND SPERMATIC CORD TORSION | ||||
| 69 | NA | 52 | LEFT | desmoplastic | NA | HYDROCELE | ||||
| 85 | NA | 14 | LEFT | poorly differentation | NA | HYDROCELE | ||||
| 69 | NA | 39 | LEFT | sarcomatous | NA | TESTICULAR MASS | ||||
| 76 | Occupatonal textile worker for 11 years | 42 | RIGHT | epithelial | NA | HYDROCELE | ||||
| 77 | Occupational bricklayer for 24 years | 8 | LEFT | epithelial | NA | HYDROCELE | ||||
| 74 | Occupatonal bricklayer for 28 years | 6 | LEFT | epithelial | NA | TESTICULAR MASS, HYDROCELE | ||||
| 131 | 2012 | Vijayan [149] | 1 | 89 | Familial (son asbestosis) | 3 dead | LEFT | papillary | 1 recurrence | SWELLING |
| 132 | 2012 | Shelton [150] | 1 | NA | NA | NA | NA | tubulo papillary | NA | NA |
| 133 | 2012 | Gemba no individual data [151] | 5 | na | 3 /5 (construction, shipbuilding, steel production) | NA | NA | NA | NA | NA |
| 134 | 2013 |
Busto Martin [152] |
1 | 61 | NO | 120 | RIGHT | biphasic | NO 120 | INCREASE OF RIGHT SCROTUM SIZE WITH PAIN |
| 135 | 2013 | Gkentzis [153] | 1 | 55 | NA | NA | LEFT | epitheliod | 24 recurrence | MASS PALPABLE |
| 136 | 2013 | Weng [154] | 1 | 28 | NO | 12 | LEFT |
tubulo papillary |
NO 12 | SCROTAL TENDERNESS AND SWELLING |
| 137 | 2013 | Meng [155] | 1 | 45 | NO | 6 alive NED | LEFT | epitheliod | NO | MASS |
| 138 | 2013 | Rajan [156] | 1 | 18 | NA | 14 dead | LEFT | papillary,multycistic | 10 metastasis | SCROTAL PAIN AND SWELLLING |
| 139 | 2013 | MeisenKothen [157] | 9 | 60 | Occupational asbestos cement pipe and domestic for 10 years [53] | 15 dead | RIGHT | NA | 15 recurrence | NA |
| 70 | Familial domestic occupational mechanic for 30 years [64] | 46 alive | RIGHT | epithelioid | NO 46 | NA | ||||
| 59 | Domestic occupational US navy railroad [48] | 71 alive | RIGHT | epithelioid | NO 71 | MASS | ||||
| 44 | Occupational mining worker for 24 years [26] | 14 dead |
RIGHT Spermatic cord |
epithelioid | 14 DOD | NA | ||||
| 74 | occupational shipping industry for 30 years [58] | 54 dead | RIGHT | biphasic | 24 recurrence | INGUINAL MASS | ||||
| 63 | Occupational automobile manufacturing for 8 years [48] | 1 dead | RIGHT | ephitelioid | 1 metastasis | NA | ||||
| 51 | Hobby and occupational asbestos cement pipe for 7 years [41] | 54 alive | LEFT | epithelioid | NO 54 | HYDROCELE | ||||
| 51 | Occupational petrochemical plant worker and hobby for [31] | 43 alive | RIGHT | NA | NO 43 | NA | ||||
| 65 | Occupational mechanic and hobby for 23 years [49] | 39 | LEFT | epithelioid | NO 39 | NA | ||||
| 140 | 2014 | Lin Nei Hsu [158] | 1 | 76 | 50 years house environmental residential | 8 | RIGHT | biphasic | NO | SWELLING |
| 141 | 2014 | Gomes da Fonseca [159] | 1 | 62 | NO | 5 dead | LEFT | epithelioid | 3 metastasis | ENLARGEMENT |
| 142 | 2014 | Stradella [160] | 1 | 51 | Possible occupational | NA | RIGHT | biphasic | NA | HYDROCELE |
| 143 | 2014 | Yang [161] | 1 | 68 | Farmer | 6 | RIGHT | epithelioid | NO | PAINFUL |
| 144 | 2015 | Akin [162] | 1 | 49 | NO | 48 | LEFT | papillary | NA | TESTICULAR MASS |
| 145 | 2015 | Bandyopadhyay [163] | 1 | 40 | Farmer | NA | NA | papillary | NA | SCROTAL SWELLING |
| 146 | 2015 |
Jankovichova [164] |
1 | 67 | Environmental residential roof eternit and occupational lorry driver construction material | 44 | LEFT | epithelioid | 14 local recurrence | HYDROCELE |
| 147 | 2015 | Silverio [165] | 1 | 82 | NA | NA | NA | NA | NA | NA |
| 148 | 2015 | D’Antonio [166] | 1 | 80 | Occupational railway workers | 12 | RIGHT spermatic cord |
tubulo- papillarymm |
NO 12 | PAINLESS MASS |
| 149 | 2015 | Segura [167] Gonzales | 1 | 58 | NO | 6 | LEFT | epithelioid | NO 6 | SWELLING |
| 150 | 2015 | Alesawi [168] | 1 | 69 | NO | 12 | RIGHT |
tubulo- papillary |
NO 12 | HYDROCELE |
| 151 | 2016 | Hispan [169] | 1 | 93 | Occupational aluminum factory for 40 years | NA | LEFT |
tubulo- papillary |
NA cutaneous metastasis | MUTIPLE NODULES |
| 152 | 2016 |
Mrinakova [170] |
2 | 67 | Occupational environmental | 62 | LEFT |
tubulo- papillary |
24 recurrence | HYDROCELE |
| 20 | environmental | 91 | LEFT | epithelioid | NO 91 | HYDROCELE | ||||
| 153 | 2016 | Ahmed [171] | 1 | 45 | Occupaional truck driver | NA | spermatic cord | biphasic | NA | SWELLING |
| 154 | 2016 |
Andresen [172] |
1 | 60 | Occupational | 27 | RIGHT | NA | 24 recurrence |
SWELLING hydrocele |
| 155 | 2016 | Serio [173] | 2 | 77 | Occupational machines ship | 44 dead | LEFT | epithelioid | 26 recurrence | SWELLING |
| 82 | NO | 63 dead | LEFT | epithelioid | 53 recurrence | hydrocele | ||||
| 156 | 2016 |
Bertolotto [174] |
7 | 64 | NA | NA | RIGHT | epithelioid | NA | SCROTAL ENLARGEMENT |
| 60 | NA | 66 | LEFT | epithelioid | NO 66 | MASS | ||||
| 65 | NA | 132 dead | LEFT | epithelioid | NA | SCROTAL ENLARGEMENT | ||||
| 70 | NA | 24 dead | RIGHT | epithelioid | NA | SCROTAL ENLARGEMENT | ||||
| 82 | NA | 6 | RIGHT | epithelioid | NO 6 | PALPABLE MASS | ||||
| 63 | NA | NA | BILATERAL | NA | NA | SCROTAL ENLARGEMENT | ||||
| 75 | NA | NA | RIGHT | NA | NA | PALPABLE MASS | ||||
| 157 | 2017 | Zhang [175] | 1 | 50 | NA | 24 | LEFT | biphasic | NO 24 | PAINLESS ENLARGEMENT |
| 158 | 2017 | Arda [176] | 1 | 84 | NA | NA | LEFT | epithelioid | NO | SCROTAL SWELLING |
| 159 | 2017 |
Recabal [177] No individual data |
15 | 39-66 | 2/15 | 42 median | NA | papillary | NA | NA |
| 160 | 2017 | Shaikh [178] | 1 | 65 | NO | 24 | BILATERAL | biphasic | NO 24 | BILATERAL PAINLESS SCROTAL SWELLING |
| 161 | 2017 | An [179] | 7 | 74 | NO | NA | NA | biphasic | NA | HYDROCELE |
| 67 | YES | 47 | NA | biphasic | NO 47 | SCROTAL MASS | ||||
| 58 | NO | 65 | NA | epithelioid | NO 65 | SPERMATOCELE | ||||
| 43 | NO | 14 | NA | epithelioid | 14 recurrence | SCROTAL MASS | ||||
| 47 | NO | 155 | NA | NA | NO 155 | HYDROCELE | ||||
| 85 | YES | 19 | NA | epithelioid | NO 19 | HYDROCELE | ||||
| 71 | NO | 15 | NA | NA | NO 15 | HYDROCELE | ||||
| 162 | 2017 |
Maheshwari [180] |
1 | 20 | NO | 16 dead | LEFT | NA | NA | SCROTAL SWELLING |
| 163 | 2018 | Abello [181] | 1 | 80 | NO | 26 | RIGHT | biphasic | 24 recurrence | PAINLESS TESTICULAR MASS |
| 164 | 2018 | Trenti [182] | 1 | 40 | NO | 72 NED | LEFT |
tubulo- papillary epithelioid |
72 NED | HYDROCELE |
| 165 | 2018 | Zhang [183] | 1 | 65 | NO | 72 alive | LEFT | NA | 72 metastasis | HYDROCELE BILATERAL |
| 2018 | Current cases | 4 | 75 | Occupational foundry worker for 4 years [46] | 141 alive | LEFT |
tubulo- papillary epithelioid |
No | MASS HYDROCELE | |
| 77 |
Occupational asbestos cement worker for 23 years asbestosis pleural plaques [45] |
2 dead | LEFT |
tubulo- papillary epithelioid |
2 metastasis | MASS | ||||
| 78 | Occupational ship machinist ship then reclaimed for 3 years [58] | 40 dead | LEFT |
tubulo- papillary epithelioid |
cardiopath | MASS | ||||
| 63 | Occupational mason cutting plates eternit trucker for 14 years [41] | 3 alive | LEFT |
tubulo- papillary epithelioid |
Recent case 3 months alive | MASS HYDROCELE |
LEGEND: NA not available, NED no evidence of disease, DOD dead of disease, CT computer tomography, MUMP mesothelioma uncertain malignant potential
Watenabe (1994)) [79] and Ascoli (1996) [89] reported two cases of multifocal mesothelioma; the subjects both had occupational exposure as insulators. Individual data were not available in three papers: Spiess (2005) [117], Gemba (2012) [152] and Recabal (2017) [178] which present case series.
Our cases were retrieved from the Apulian malignant mesothelioma register Cor Apulia (Cor-operating centre regional), established in 1993 as a part of the ReNaM-Italian national mesothelioma register. The Apulia mesothelioma register collects data on all incident cases of mesothelioma (pleura, pericardium, peritoneum and tunica vaginalis testis) from 1993 to date.
The regional register according to the national guidelines [185], using a standardized questionnaire and with direct interviews with patients or their relatives, obtained occupational and residential-environmental histories, lifestyle habits and the hobbies of the patients. Similarly, the best evidence of histological diagnosis, follow-up data and vital status of each patient were recorded.
Results
Since, in 1943, a confusing nomenclature arose, and in 1945 Golden and Ash [18] introduced the term “adenomatoid tumours”, De Klerk and Nime [186] reported in 1975 that, from 1912 to 1975, two hundred three cases of adenomatoid tumours (malignant adenomatoid tumours) of testicular and paratesticular tissues were reported in the English language literature. Therefore, Bisceglia (Bisceglia 2010) [135] reported fewer than 250 cases of testicular and paratesticular mesothelioma, Jankovichova reported approximately 250 cases, and Mrinakova reported approximately 300 cases [165, 171]. All of these cases comprised and could be categorized as MM, WDPM and MUMP or MLMP.
In our review, we found 289 cases of MMTVT (Table 1). The last four cases reported in Table 1 were cases currently found in the Apulia regional registry of the mesothelioma, so the total number of cases reported is here 293.
Among the 289 cases reported here from the literature, the main features are summarized in Table 2.
Table 2.
289 MMTVT main features: age at diagnosis, side, histologic type, clinical presentation, duration of follow up, recurrence, asbestos exposure
| Number of cases | % | |
|---|---|---|
| Age at diagnosis | ||
| 1-30 | 27 | 9.3 |
| 31-40 | 24 | 8.3 |
| 41-50 | 32 | 11.07 |
| 51-60 | 43 | 14.8 |
| 61-70 | 64 | 22.1 |
| 71-80 | 48 | 16.6 |
| 81- | 17 | 5.8 |
| NA(not available) | 34 | 11.7 |
| Total | 289 | 100 |
| Laterality | ||
| Right testis | 92 | 31.8 |
| Left testis | 104 | 35.9 |
| Bilateral | 6 | 2.07 |
| Others (spermatic cord, scrotum, epididymis, ecc.) | 7 | 2.4 |
| NA | 80 | 27.6 |
| Total | 289 | 100 |
| Histologic type | ||
| Epithelial | 155 | 53.6 |
| Biphasic | 45 | 15.5 |
| Sarcomatous | 5 | 1.7 |
| NA | 84 | 29.06 |
| Total | 289 | 100 |
| Clinical presentation | ||
| Mass | 55 | 19.03 |
| Hydrocele | 84 | 29.06 |
| Swelling | 79 | 27.3 |
| Others (inguinal hernia, pain, hematoscrotum,ecc.) | 15 | 5.1 |
| NA | 56 | 19.3 |
| Total | 289 | 100 |
| Duration of follow up in months | ||
| 2-12 | 66 | 22.8 |
| 13-36 | 88 | 30.04 |
| 37-60 | 27 | 9.3 |
| 61-96 | 21 | 7.2 |
| 97-132 | 6 | 2.07 |
| 133-564 | 7 | 2.4 |
| NA | 74 | 25.6 |
| Total | 289 | 100 |
| Recurrence | ||
| Metastasis | 23 | 7.9 |
| Multifocal | 53 | 18.3 |
| No | 110 | 38.06 |
| NA | 103 | 35.6 |
| Total | 289 | 100 |
| Asbestos exposure | ||
| Yes | 80 | 27.6 |
| No | 88 | 30.4 |
| NA | 121 | 41.8 |
| Total | 289 | 100 |
The characteristics of our cases are reported in Table 1 and summarized in Table 3; the age at diagnosis ranged from 63 to 78 years old, with an average age of 73.2 years old; the clinical onset was a mass, and only two cases also had hydroceles; all of the cases involved the left testicle. All of the patients underwent surgery (orchidectomy), and the histological types were epithelioid. IHC (immunohistochemistry) was always performed with calretinin, HBME1, CK AE1/AE3, EMA positive (Figs. 1, 2, and 3).
Table 3.
Four MMTVT cases from the Apulia mesothelioma register
| Case number | Year of diagnosis | Age years | Clinical diagnosis | Histological diagnosis | IHC | Survival months | Exposure reliable professional | Duration of exposure Years- calendar years | Latency years |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2006 | 75 | CAT | mm epithelioid with papillary tubule aspects | Calretinine+++, HBME1+++ | 141 | foundry worker | 4 (1960-63) | 46 |
| 2 | 2009 | 77 | CAT ecocolordoppler | mm epithelioid with papillary and microcystic aspects | Calretinine +++,CK AE1/AE3+++, vimentine+++, WT1 (80%) KI67(8%) nuclear grade 2, IM:3x10HPF | 2 | asbestos cement worker | 21 (1964-85) | 45 |
| 3 | 2009 | 78 | CAT ecocolordoppler | mm epithelioid papillary tubule growth pattern solid and focally clear cell presence psammomatous bodies | Calretinine +++, CK AE1/AE3+++,EMA +++, HMBE1 +++, WT1+++ > 25% nuclear grade 2,3 IM:5x10HPF | 40 | naval machinist | 3 (1951-53) | 58 |
| 4 | 2018 | 63 | CAT | mm epithelioid papillary (70%) and solid (30%) tubule growth pattern | Calretinine +++,CK AE1/AE3+++,HMBE1 +++, WT1(90%)KI67 10% papillary tubulum component and 40% solid component | 3 | bricklayer cutting plates eternit and trucker | 14 (1977-90) | 41 |
Fig. 1.

Case number 4 Gross examination, lardaceous superficial thickening of the tunica albuginea
Fig. 2.
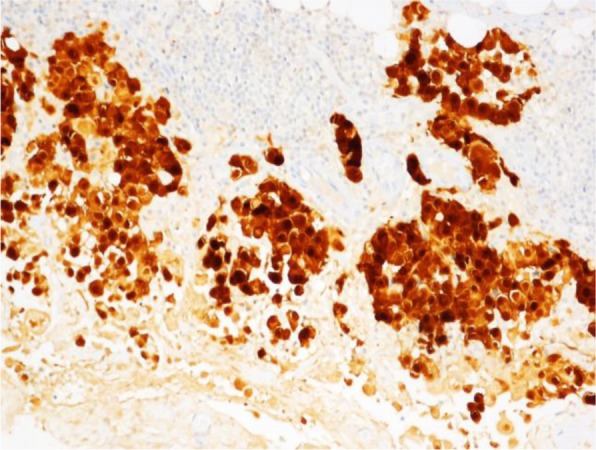
Case number 4. Microscopic examination, pseudopapillary epithelioid neoplastic proliferation wrapping around the testicular parenchyma. Diffuse immunopositivity for calretinin antigen (× 200)
Fig. 3.
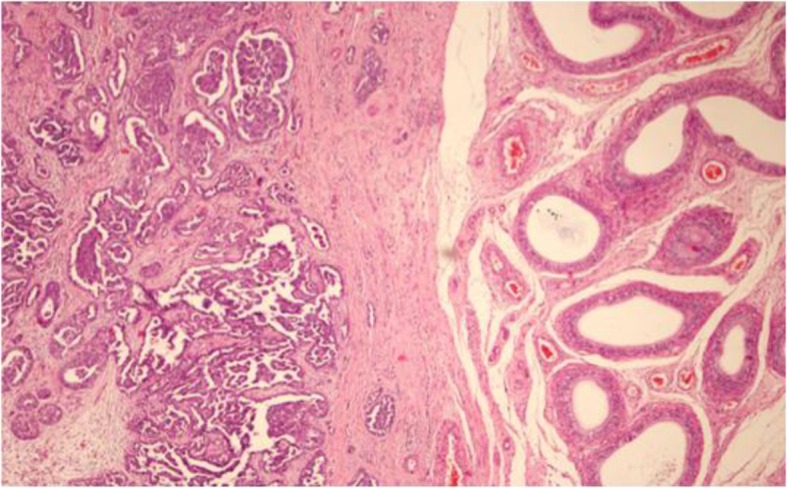
Case number 4. Microscopic examination, pseudopapillary epithelioid neoplastic proliferation wrapping around the testicular parenchyma (H&E, X100)
All of our cases were directly interviewed, and asbestos exposure was documented. Two patients had pleural plaques found on computerized axial tomography (CAT) examination. At the last date of follow-up, in September 2018, two patients were alive and two were dead: one died of disease metastasis, and the other died of cardiopathy. The median survival was 46.7 months (range 2-141), the latency period was a mean of 47.5 years (range 41-58), and the duration of asbestos exposure had a mean of 10.5 years (range 2-21).
Discussion
MMTVT is a rare neoplasm that constitutes 0.3-5% of all mesothelioma cases with a mortality rate of 53% at 2 years following diagnosis [176].
Pathogenesis predisposing factors are described as local trauma, herniorrhaphy, long-term hydrocele or spermatocele [129, 187–189], venereal diseases and ionizing radiation [96, 99].
The tunica vaginalis has a common embryological origin with the visceral pleura, peritoneum and pericardium [187]. Relative to histogenesis in the past, four embryologic hypotheses have been considered: endothelium, epithelial, mesonephric and mesothelial hypotheses [42]. Early writers believed that this tumour had a lymphangiomatous origin because the predominance of labyrinthine channels lined by seemingly flat endothelial cells embedded in a reticular stroma, subsequent microscopic investigations excluded the endothelial origin due to the presence of vacuolated cuboidal and columnar cells. [42].
The mesothelial character was supported by electron microscopic studies [190]. The tunica vaginalis develops from evagination of the peritoneum during fetal life, and it is an embryonic extension of the peritoneal mesothelium, resulting from the descent of the testis through the abdominal wall via the inguinal canal into the scrotum [68]. The epithelial lining of the urogenital tract has mesodermal (mesothelial) origin [191], and the mesothelium has the ability to differentiate into fibroblasts and mesonephric tubular structures, or rather, the mesothelial cells could have a multipotent evolution; they can differentiate in an epithelial or a fibroblastic direction [33, 192, 193]. The mesothelial hypothesis was also corroborated by the occurrence in a patient affected by Maffucci’s syndrome, a mesenchymal disease [50].
To date, there is agreement regarding some of the main features of this disease as shown below; moreover, it is difficult to diagnose preoperatively.
Symptomatology
MMTVT can be asymptomatic for a long time. Hydrocele, scrotal mass, a lack of pain, inguinal hernia, spermatocele, testicular torsion, previous herniorrhaphy, and post-traumatic injury are all possible clinical manifestations of the disease [147]. Long asymptomatic intervals from initial presentation to clinical recurrence have been reported [54], moreover, MMTVT might mimic epididymitis [147] .
Diagnosis
Computed tomography, ultrasound, ultrasonography (colour Doppler sonography), and cytological examination of the hydrocele fluid by sonographically guided fine-needle aspiration (FNA) [128, 137, 164] have been performed, although some authors [169, 173] do not agree with these methods due to the low sensitivity of cytology and the potential risk of metastasis, instead using gross pathology images and magnetic resonance imaging.
Macroscopic appearance gross findings
A firm painless scrotal mass [194], numerous small papillary lesions or multiple nodules studded on the internal surface of the hydrocele sac, diffuse thickening of the tunica vaginalis [195], and a solid coat around the tunica vaginalis with variable features.
Microscopic appearance findings
Malignant character is demonstrated by the growth pattern, cytological alterations, extensive tissue invasion, and metastases to the lymph nodes; early diagnosis is by cytologic examination of the hydrocele fluid. Nuclear atypia, mitotic activity, with a stroma invasion infiltrative pattern. Cellular nuclear pleomorphism and papillary configuration are signs of lethal potential [52]. An infiltrative pattern of growth with increased cellularity nuclear pleomorphism and high mitotic rate and stromal invasion [105, 195]. Large lymphoid cells with clear or slightly eosinophilic cytoplasm with large strongly atypical polymorphic nuclei and a great number of mitoses; epithelioid features with papillary growth, papillary tubules, and solid growth in invasive foci [196].
Histologically, it can be of three histologic types
Epithelial (papillary, tubuloalveolar-glandular or solid) [99], fibrosarcomatous or mesenchymal; biphasic; or mixed, associated with the papillary architecture with stromal invasion. Hallmarks of mesothelioma are epithelial cuboidal cells with microvilli, basement membranes, filaments and desmosomes [197].The criteria for malignancy are nuclear pleomorphism, mitotic activity and stromal invasion [13, 198, 199].
Histochemical-immunohistochemical features
IHC (immunohistochemistry) shows the presence of both cytokeratin and vimentin, suggesting the diagnosis of mesothelioma. Positive staining for cytokeratin, vimentin and Ema (epithelial membrane antigen), with negative staining for Cea carcinoembryonic antigen, Leu–M1, and cytokeratin 20 CKL20. Epithelial membrane antigen and factor VIII are strongly suggestive for the diagnosis of MM; mesothelioma-related markers include calretinin, thrombomodulin, CK5/6 (pleural), WT1 (Wilms tumour antibody), D2-40, CK7 (tunica vaginalis) [120, 162, 188, 198], CD20 +, and calretinin + [196, 200].
Electron microscopy
The microvilli are elongated and develop complex throughout the tumour; there are well-defined, mature desmosomes through the interdigitating portions of the cytoplasmatic membrane, and numerous cytoplasmatic filaments are observed [104, 151, 188]. In 2009, the International Mesothelioma Interest Group (IMIG) [201]) recommended IHC as the gold standard for the diagnosis of MM, instead of electron microscopy.
Ultrasonography [103]
The most common sonographic finding is the presence of heterogeneous nodular or papillary masses of the tunica vaginalis associated with a hydrocele or hypoechoic hydrocele with heterogeneous masses of increased echogenicity at the periphery [74, 115, 187, 202]. Lesions are closely related to the tunica vaginalis [196].
Laterality
Most cases are unilateral on presentation, while only a few cases of bilateral MMTVT have been reported [131]; in the present review, we found only six cases (2.03%) with reported bilateral disease [50, 93, 97, 111, 175, 179].The case reported by Slaysman (1982) [50] occurred in a young man of 20 years old affected by Maffucci syndrome.
Distant spread usually occurs via lymphatics; the retroperitoneal nodes are the most common site of metastasis, while spinal metastasis was described by Mathew (1996) [90] and cutaneous metastasis has also been reported [34, 53, 61, 170].
The differential diagnosis includes mesothelial hyperplasia, adenomatoid tumour, benign papillary mesothelioma, borderline serous papillary tumours, serous carcinomas, carcinoma of the rete testis or epididymis and metastatic adenocarcinoma [26, 99, 188, 203]. Because of potential misdiagnosis, the best evidence for definitive diagnosis requires a panel of HIC markers [145, 198, 203].
The prognosis is poor. While MM of the pleura and peritoneum has an extremely poor prognosis, MMTVT has a better prognosis, but the natural history of this tumour suggests an aggressive behaviour, with a survival rate of less than 50% 2 years after diagnosis [176].Early diagnosis is of great importance for treatment and long-term survival, especially in young men [156, 160].
Treatment
A multidisciplinary approach of radical orchiectomy and retroperitoneal node dissection is the best choice for cases of this disease. Chemotherapy can be useful for regression of disseminated disease, although to date, because of the rarity of this disease, no statistically significant studies or large series are available to assess the role of adjuvant therapy (chemo- and radiotherapy) [204]. Long-term follow-up over 5 years is needed because late recurrence is not rare and, to date, an aggressive surgical approach is necessary to achieve a cure because of potential late recurrence or metastasis. Many authors have emphasized the importance of considering this tumour in men with scrotal masses and hydroceles [54], even in the absence of asbestos exposure [115, 122, 123]. Lifelong follow-up and management in a multidisciplinary setting are recommended [161, 168, 171].
Similarly, our review, which considered only malignant mesotheliomas in the English literature, as reported by the authors of the examined articles due to the temporal evolution of the histological classification of this pathology, as already noted, does not confirm the total number of cases as reported in previous reviews [149] including approximately 250 cases.
Another limitation of this review is that no best evidence of diagnosis from early articles and no best evidence of asbestos exposure are available.
The histologic prevalent pattern is epithelial (53.6%of all cases), followed by a mixed biphasic pattern in 15.5% and a fibrous sarcomatoid variant in 1.7%. The more frequent age at presentation ranges from 61 to 80 years old (38.7%). Hydrocele was present in 29.06% of the cases described and swelling in 27.3%. Two cases [79, 89] were not primary tumours but of multifocal origin, and the pleura and peritoneum were involved in two patients with heavy exposure to an insulator.
Only 4.4% of cases had a follow-up of over 8 years. Sixty-six patients died of disease progression with an average survival of 24.2 months (range1-76); two cases with a long duration of follow-up died after 132 and 564 months; ultimately, the prognosis remains poor with only rare long-term survivors. The overall recurrence rate (recurrence or metastasis) was 26.2%, predominantly within the first 2 years of follow-up. Both cases reported by Mathew (1996) [90] presented spinal metastasis, and the case reported by Hispan (2016) [170] presented cutaneous metastasis. Finally, in the papers by Spiess (2005) [117], Gemba (2012) [152] and Recabal (2017) [178], no individual data were reported. In previous reviews, a statistically significant correlation was reported between survival with age < 60 years old and organ-confined disease at diagnosis [74, 202]. Assessment of prognostic parameters revealed a significant correlation of the patient’s age with survival [96]. Radical inguinal orchiectomy might contribute to a better prognosis [112]. Due to the possibility of late tumour recurrence reported in 2.7% [96], lifelong follow-up can be recommended and should be offered to the patient because of the metastatic potential of the tumour; in fact, recurrence can occur as late as 15 years postoperatively [123, 205].
Regarding risk factors, the only causal factor so far ascertained is asbestos exposure, and exposure to different asbestos-containing materials is the only well-documented risk factor [87, 96], as stated by IARC (international agency on cancer research) (2012) [1], although information about exposure might not always have been adequate. Nevertheless, there are authors who do not agree with the absence, until today, of analytical case-control epidemiologic studies to test this relationship [189].
Asbestos is an ascertained carcinogen [1] in the development of mesotheliomas. It is necessary to bear in mind that it is ubiquitous not only in the workplace but also in the general environment [206]. The first study reporting an MMTVT case, diagnosed in 1969, with asbestos exposure was published in 1976 by Fligiei and Kaneko [38] in a pipe insulator exposed for 40 years. In the same year, Pizzolato and Lamberty [40] reported a case in a sugar refinery worker. Since the first case of MMTVT described in 1976 by Fligiel and Kaneko (Fligiel 1976 [38], it has been supposed that the asbestos fibres from the lung can reach the tunica vaginalis by a lymphatic or bloodstream route [207, 208]. Mirabella (1991) [209], in his review of the literature, reported eleven cases with occupational asbestos exposure. In the review by Jones (1995) [87] of a total of 63 cases, 48% had histories of asbestos exposure, while in Mensi’s report (2012) [149], 61% of cases had asbestos exposure.
Overall, asbestos exposure was investigated only in 58% of all cases reported in this review, while in 41.8%, these data were not available. Notably, in many reports, there was no anamnestic reconstruction of any asbestos exposure.
A history of direct occupational, environmental or family asbestos exposure is found in 27.6% of these cases. Among these cases (80 cases) 12.5% reported generic occupational exposure the others 87.5% have a documented history of asbestos exposure. Among the latter there are insulators, dock workers, steel industry workers, farmers, shipyard workers and other different occupations in sectors known to involve asbestos exposure. To be noted there are four cases with environmental exposure, six with household, family or hobby exposure and five cases with or without declared exposure but with pleural plaques or asbestos bodies.
The duration of asbestos exposure is recorded in 108 articles of the 165 reviewed (65.45%). In these articles 50 ascertained the exposure (30.30%) while in 58 articles it was excluded (35.15%).
The duration of exposure is between 4 and 50 years, for occupational exposures only the range is 4-40 years. For the new employment cases presented here the range is 3-23 years.
The true incidence of asbestos exposure in these reported MMTVT cases is underestimated because of insufficient information, especially for the earlier cases and case series described until the beginning of the 2000s, when the scientific community became aware of the risk factors for this disease represented by asbestos exposure [158]. Similarly, because of the long latency period, even over decades, poor patient recall in the reconstruction of asbestos exposure and occupational histories or the patient being unaware of using materials containing asbestos [171], until now, the quality of these data was quite unclear, which might have caused the majority of MMTVT cases to date appearing to be idiopathic, and there is no accurate assessment of asbestos exposure association. However, latency in Antman’s (1984)) [54] case series ranged from 16 to 40 years. The higher incidence of MMTVT among older patients is related to longer exposure to asbestos with a latency range of 10-40 years. A positive history of asbestos exposure or asbestos-containing materials constitutes a risk for the development of an MMTVT and should be monitored [123].
The Apulia mesothelioma registry recorded 4 cases of MMTVT from 1993 to 2018, accounting for 0.3% of all MM cases reported in the regional register during this period. This percentage is consistent with the national Renam data (0.28%) from the national Italian mesothelioma registry [2]. The age at diagnosis was an average of 73 years old, and the mean survival (46 months) was consistent with that reported in the literature [188]. The family histories and clinical-medical histories of the patients were unremarkable. None of our patients underwent chemotherapy or radiotherapy cycles after orchidectomy. The Renam data [2] showed that more than 59% of MMTVT cases had asbestos exposure. Our four cases, all with occupational exposure, had a latency of 47 years and an exposure length of 10.5 years, and these data are concordant with the descriptions in the literature of the aetiological role of asbestos in the pathogenesis of MM [3, 13, 206]. The accurate diagnosis of primary malignant MMTVT and occupational anamnesis are helpful for medicolegal compensation considerations, especially for the cases associated with asbestos exposure [13]. The case described here was referred to the Italian workers’ compensation authority (Inail - National Insurance Institution for Occupational Accidents).
Recently, many studies have demonstrated molecular changes in MM with multiple chromosomal alterations [184, 210–214]. Chromosomal abnormalities in cases of MMTVT were described for the first time by Serio (Serio 2016) [174]in two cases with comparative genomic hybridization (CGH) findings. The two cases showed several gains and losses, in particular, identical lost regions at 1p13.3 → q21.1; 19q13.42; 21q22.2; and 22q12.2 (tumour suppressor gene NF2). Jean (Jean 2012) [215] hypothesized that NF2 regulates cell growth function, and its inactivation could be related to tumour progression and patient survival. We are deepening the study of these new cases, all with ascertained exposure to asbestos, to understand whether there are specific DNA copy number changes in MMTVT and investigating the relative genes involved to define whether they are or are not the same as those reported in pleural MM, particularly in relation to asbestos exposure, and whether they might be useful in elucidating tumorigenesis and predicting prognosis.
Conclusions
Although this systematic review shows that only 27.6% of the cases reported in this long period of time (1943-2018) had asbestos exposure must be underlined that in 41.8% of the cases in the literature exposure to asbestos is not investigated. In our opinion, to establish a broad consensus on the causal relationship between asbestos and MMTVT in the scientific community, we will need to analyze these relationships with analytical epidemiological studies. A case control study on the data from the national mesothelioma registry is under way in Italy, together with molecular epidemiological studies.
Acknowledgements
The authors thank Mr. Alberto Amenduni for his help in retrieving articles.
Abbreviations
- CAT
Computerized axial tomography
- CGH
Comparative genomic hybridization
- COR
Operating centre regional
- FNA
Fine needle aspiration
- IARC
International agency on cancer research
- IHC
Immunohistochemistry
- IMIG
International mesothelioma interest group
- MLMP
Mesothelioma low malignant potential
- MM
Malignant mesotelioma
- MMTVT
Malignant mesothelioma tunica vaginalis testis
- MUMP
Mesothelioma uncertain malignant potential
- NA
Not available
- ReNaM
National mesothelioma register
- WDPM
Well differentiated papillary mesotheloma
- WHO
World Health Organization
Authors’ contributions
LV, was involved in study design, data interpretation, analysis, draft and reviewed the manuscript, DC was involved in study design, recovery of data from the regional registry of mesotheliomas, data interpretation, analysis, draft and reviewed the manuscript, MCD, LDEM and AC conducted literature search, GMF reviewed the draft, GS made histological diagnoses and reviewed the draft. All authors read and approved the final manuscript.
Funding
This work was supported with the ordinary funds of the University Aldo Moro of Bari.
Availability of data and materials
The dataset and articles used and analyzed during the study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declared that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Giovanni Maria Ferri and Gabriella Serio contributed equally to this work.
Contributor Information
Luigi Vimercati, Phone: 39-80-5478256, Email: luigi.vimercati@uniba.it.
Domenica Cavone, Email: domenica.cavone@uniba.it.
Maria Celeste Delfino, Email: maria.delfino@uniba.it.
Luigi De Maria, Email: luigi.demaria@uniba.it.
Antonio Caputi, Email: antonio.caputi@uniba.it.
Giovanni Maria Ferri, Email: giovannimaria.ferri@uniba.it.
Gabriella Serio, Email: gabriella.serio1@uniba.it.
References
- 1.IARC International Agency for Research on Cancer (IARC) Arsenic, metals, fibres, and dusts. IARC working group on the evaluation of carcinogenic risks to humans. IARC Monogr Eval Carcinog Risks Hum. 2012;100(Pt. C):11–465. [PMC free article] [PubMed] [Google Scholar]
- 2.RENAM Registro Nazionale Mesotelomi Sesto rapporto. Il registro nazionale dei mesoteliomi: Inail; 2018. https://www.inail.it/cs/internet/docs/alg-pubbl-registro-nazionale-mesoteliomi-6-rapporto.pdf
- 3.Attanoos RL, Gibbs AR. Pathology of malignant mesothelioma. Histopathology. 1977;30:403–418. doi: 10.1046/j.1365-2559.1997.5460776.x. [DOI] [PubMed] [Google Scholar]
- 4.Evans N. Mesotheliomas of the uterine and tubal serosa and the tunica vaginalis testis: report of four cases. Am J Pathol. 1943;19(3):461–471. [PMC free article] [PubMed] [Google Scholar]
- 5.Fajers CM. Mesotheliomas of the genital tract; a report of five new cases and a survey of the literature. Acta Pathol Microbiol Scand. 1949;26(1):1–23. doi: 10.1111/j.1699-0463.1949.tb03142.x. [DOI] [PubMed] [Google Scholar]
- 6.Dixon FJ, Moore RA. Tumors of the testicle. Acta Unio Int Contra Cancrum. 1952;8(2):310–315. [PubMed] [Google Scholar]
- 7.Longo T, Zanaboni A. Contribution to the knowledge of the so-called mesothelioma of the epididymis. Minerva Urol. 1959;11:225–237. [PubMed] [Google Scholar]
- 8.Söderström J, Liedberg CF. Malignant "adenomatoid" tumour of the epididymis. Acta Pathol Microbiol Scand. 1966;67(2):165–168. doi: 10.1111/apm.1966.67.2.165. [DOI] [PubMed] [Google Scholar]
- 9.Abell MR, Holtz F. Testicular and paratesticular neoplasms in patients 60 years of age and older. Cancer. 1968;21(5):852–870. doi: 10.1002/1097-0142(196805)21:5<852::AID-CNCR2820210509>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 10.Rankin NE. Adenomatoid tumours of the epididymis and tunica albuginea; two cases. Br J Urol. 1956;28(2):187–193. doi: 10.1111/j.1464-410X.1956.tb04754.x. [DOI] [PubMed] [Google Scholar]
- 11.Brimo F, Illei PB, Epstein JI. Mesothelioma of the tunica vaginalis: a series of eight cases with uncertain malignant potential. Mod Pathol. 2010;23(8):1165–1172. doi: 10.1038/modpathol.2010.113. [DOI] [PubMed] [Google Scholar]
- 12.Trpkov K, Barr R, Kulaga A, Yilmaz A. Mesothelioma of tunica vaginalis of "uncertain malignant potential" - an evolving concept: case report and review of the literature. Diagn Pathol. 2011;6:78. doi: 10.1186/1746-1596-6-78.Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Attanoos RL, Gibbs AR. Primary malignant gonadal mesotheliomas and asbestos. Histopathology. 2000;37(2):150–159. doi: 10.1046/j.1365-2559.2000.00942.x. [DOI] [PubMed] [Google Scholar]
- 14.Kossow AS, McCann LS. Malignant mesothelioma of the testicular tunic. J Urol. 1981;126(2):272–274. doi: 10.1016/S0022-5347(17)54473-0. [DOI] [PubMed] [Google Scholar]
- 15.Naegeli T. Virchows Arch. 1912;208:364. doi: 10.1007/BF01991207. [DOI] [Google Scholar]
- 16.Sakaguchi Y. Virchows Arch. 1912;208:364. doi: 10.1007/BF01991207. [DOI] [Google Scholar]
- 17.Thompson GJ. Tumors of the spermatic cord, epididymis and testicular tunics. Review of literature and report of forty-one additional cases. Surg Gynecol Obstet. 1936;62:712. [Google Scholar]
- 18.Golden A, Ash JE. Adenomatoid tumors of the genital tract. Am J Pathol. 1945;21(1):63–79. [PMC free article] [PubMed] [Google Scholar]
- 19.Lee MJ, Jr, Dockerty MB, Thompson GJ, Waugh JM. Benign mesotheliomas (adenomatoid tumors) of the genital tract. Proc Staff Meet Mayo Clin. 1950;25(25):665–672. [PubMed] [Google Scholar]
- 20.Bailey GN, Willis RA, Wilson JV. A case of adenocarcinoma of the appendix testis. J Pathol Bacteriol. 1955;69(1-2):326–328. doi: 10.1002/path.1700690142. [DOI] [PubMed] [Google Scholar]
- 21.Barbera V, Rubino M. Papillary mesothelioma of the tunica vaginalis. Cancer. 1957;10(1):183–189. doi: 10.1002/1097-0142(195701/02)10:1<183::AID-CNCR2820100127>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 22.Marcus JB, Lynn JA. Ultrastructural comparson of an adenomatpoid tumor, lymphangoma, hemangioma and mesothelioma. Cancer. 1970;25:171–175. doi: 10.1002/1097-0142(197001)25:1<171::AID-CNCR2820250125>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 23.Carp NZ, Petersen RO, Kusiak JF, Greenberg RE. Malignant mesothelioma of the tunica vaginalis testis. J Urol. 1990;144(6):1475–1478. doi: 10.1016/S0022-5347(17)39773-2. [DOI] [PubMed] [Google Scholar]
- 24.WHO World Health Organization . Classification of Tumours of the urinary system and male genital organs. 2016. [Google Scholar]
- 25.Battifora H, Kopinski MI. Distinction of mesothelioma from adenocarcinoma. An immunohistochemical approach. Cancer. 1985;55(8):1679–1685. doi: 10.1002/1097-0142(19850415)55:8<1679::AID-CNCR2820550812>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 26.Colecchia M, Mikuz G, Algaba F. Rare tumors of the testis and mesothelial proliferation in the tunica vaginalis. Tumori. 2012;98(2):270–273. doi: 10.1700/1088.11942. [DOI] [PubMed] [Google Scholar]
- 27.Ramirez Sevilla C, Admella Salvador C, Feliu Canaleta J, Llopis Manzanera J, Barranco Sanz MA, Romero Martin JA, Bernal SS. Two case reports of benign testicular mesothelioma and review of the literature. Case Rep Oncol Med. 2017;2017:5419635. doi: 10.1155/2017/5419635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grove A, Jensen ML, Donna A. Mesotheliomas of the tunica vaginalis testis and hernial sacs. Virchows Arch A Pathol Anat Histopathol. 1989;415(3):283–292. doi: 10.1007/BF00724916. [DOI] [PubMed] [Google Scholar]
- 29.Robinson JN. Benign tumours of epididymis and tunica vaginalis. Brit J Urol. 1945;17(2):68–69. doi: 10.1111/j.1464-410X.1945.tb10558.x. [DOI] [Google Scholar]
- 30.Patterson TC, Mogg RA. A case of mesothelioma of the epididymis. Brit J Surg. 1947;34(136):427–429. doi: 10.1002/bjs.18003413619. [DOI] [PubMed] [Google Scholar]
- 31.Foote NC. Testicular tumors. N Y State J Med. 1949;49(3):284–286. [PubMed] [Google Scholar]
- 32.Reynolds CL., Jr Multiple mesotheliomas of the hydrocele sac: a case report. J Urol. 1958;79(1):134–137. doi: 10.1016/S0022-5347(17)66246-3. [DOI] [PubMed] [Google Scholar]
- 33.Kozlowski H, Zoltowska A. Mesothelioma of spermatic cord. Neoplasma. 1968;15(1):97–100. [PubMed] [Google Scholar]
- 34.Kasdon EJ. Malignant mesothelioma of the tunica vaginalis propria testis. Report of two cases. Cancer. 1969;23(5):1144–1150. doi: 10.1002/1097-0142(196905)23:5<1144::AID-CNCR2820230520>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 35.Arlen M, Grabstald H, Whitmore WF., Jr Malignant tumors of the spermatic cord. Cancer. 1969;23(3):525–532. doi: 10.1002/1097-0142(196903)23:3<525::AID-CNCR2820230302>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 36.Johnson DE, Fuerst DE, Gallager HS. Mesothelioma of the tunica vaginalis. South Med J. 1973;66(11):1295–1297. doi: 10.1097/00007611-197311000-00023. [DOI] [PubMed] [Google Scholar]
- 37.Fishelovitch J, Meiraz D, Keinan Z, Green I. Malignant mesothelioma of the testicular tunica vaginalis. Br J Urol. 1975;47(2):208. doi: 10.1111/j.1464-410X.1975.tb03949.x. [DOI] [PubMed] [Google Scholar]
- 38.Fligiel Z, Kaneko M. Malignant mesothelioma of the tunica vaginalis propria testis in a patient with asbestos exposure. A case report. Cancer. 1976;37(3):1478–1484. doi: 10.1002/1097-0142(197603)37:3<1478::AID-CNCR2820370333>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 39.Pugh RCB. Pathology of the testis. Oxford, London, Edinburgh, Melbourne: Blackwell scientific publications; 1976. [Google Scholar]
- 40.Pizzolato P, Lamberty J. Mesothelioma of spermatic cord: electron microscopic and histochemical characteristics of its mucopolysaccharides. Urology. 1976;8(4):403–408. doi: 10.1016/0090-4295(76)90502-1. [DOI] [PubMed] [Google Scholar]
- 41.Eimoto T, Inoue I. Malignant fibrous mesothelioma of the tunica vaginalis: a histologic and ultrastructural study. Cancer. 1977;39(5):2059–2066. doi: 10.1002/1097-0142(197705)39:5<2059::AID-CNCR2820390523>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 42.Tuttle JP, Jr, Rous SN, Harrold MW. Mesotheliomas of spermatic cord. Urology. 1977;10(5):466–468. doi: 10.1016/0090-4295(77)90141-8. [DOI] [PubMed] [Google Scholar]
- 43.Sinha AP. Neoplasms of tunica vaginalis. Br J Urol. 1978;50(6):424. doi: 10.1111/j.1464-410X.1978.tb04224.x. [DOI] [PubMed] [Google Scholar]
- 44.Jaffe J, Roth JA, Carter H. Malignant papillary mesothelioma of tunica vaginalis testis. Urology. 1978;11(6):647–650. doi: 10.1016/0090-4295(78)90023-7. [DOI] [PubMed] [Google Scholar]
- 45.Benisch B, Peison B, Sobel HJ, Marquet E. Fibrous mesotheliomas(pseudofibroma) of the scrotal sac: a light and ultrastructural study. Cancer. 1981;47(4):731–735. doi: 10.1002/1097-0142(19810215)47:4<731::AID-CNCR2820470418>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 46.Blitzer PH, Dosoretz DE, Proppe KH, Shipley WU. Treatment of malignant tumors of the spermatic cord: a study of 10 cases and a review of the literature. J Urol. 1981;126(5):611–614. doi: 10.1016/S0022-5347(17)54650-9. [DOI] [PubMed] [Google Scholar]
- 47.Japko L, Horta AA, Schreiber K, Mitsudo S, Karwa GL, Singh G, Koss LG. Malignant mesothelioma of the tunica vaginalis testis: report of first case with preoperative diagnosis. Cancer. 1982;49(1):119–127. doi: 10.1002/1097-0142(19820101)49:1<119::AID-CNCR2820490123>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 48.Chen KT, Arhelger RB, Flam MS, Hanson JH. Malignant mesothelioma of tunica vaginalis testis. Urology. 1982;20(3):316–319. doi: 10.1016/0090-4295(82)90652-5. [DOI] [PubMed] [Google Scholar]
- 49.Hollands MJ, Dottori V, Nash AG. Malignant mesothelioma of the tunica vaginalis testis. Eur Urol. 1982;8(2):121–122. doi: 10.1159/000473493. [DOI] [PubMed] [Google Scholar]
- 50.Slaysman ML, McDonald RE, Gormley WT. Mesothelioma of the male genital tract in a patient with Maffucci's syndrome. South Med J. 1982;75(8):1007–1010. doi: 10.1097/00007611-198208000-00022. [DOI] [PubMed] [Google Scholar]
- 51.Zidar BL, Pugh RP, Schiffer LM, Raju RN, Vaidya KA, Bloom RL, Horne D, Baker LH. Treatment of six cases of mesothelioma with doxorubicin and cisplatin. Cancer. 1983;52(10):1788–1791. doi: 10.1002/1097-0142(19831115)52:10<1788::AID-CNCR2820521005>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 52.McDonald RE, Sago AL, Novicki DE, Bagnall JW. Paratesticular mesotheliomas. J Urol. 1983;130(2):360–361. doi: 10.1016/S0022-5347(17)51150-7. [DOI] [PubMed] [Google Scholar]
- 53.van der Rhee HJ, van Vloten WA, Scheffer E, Zwartendijk J. Cutaneous manifestations of malignant mesothelioma of the tunica vaginalis testis. J Cutan Pathol. 1983;10(3):213–216. doi: 10.1111/j.1600-0560.1983.tb00329.x. [DOI] [PubMed] [Google Scholar]
- 54.Antman K, Cohen S, Dimitrov NV, Green M, Muggia F. Malignant mesothelioma of the tunica vaginalis testis. J Clin Oncol. 1984;2(5):447–451. doi: 10.1200/JCO.1984.2.5.447. [DOI] [PubMed] [Google Scholar]
- 55.Yamanishi T, Wakisaka M, Ito H, Matsuzaki O, Nagao K, Shimazaki J. Malignant mesothelioma of the tunica vaginalis testis. Eur Urol. 1984;10(3):207–209. doi: 10.1159/000463789. [DOI] [PubMed] [Google Scholar]
- 56.Khan AR, Min B, Chai SW, Englander LS. Biphasic malignant mesothelioma (malignant adenomatoid tumor) of paratesticular tissue. Urology. 1984;24(1):82–84. doi: 10.1016/0090-4295(84)90397-2. [DOI] [PubMed] [Google Scholar]
- 57.Vakalikos I, Destouni E, Valassis K, Eftichiadou C, Charalambopoulos A, Salem N. Malignant mesothelioma of testicular tunica. J Surg Oncol. 1985;29(4):264. doi: 10.1002/jso.2930290415. [DOI] [PubMed] [Google Scholar]
- 58.Ehya H. Cytology of mesothelioma of the tunica vaginalis metastatic to the lung. Acta Cytol. 1985;29(1):79–84. [PubMed] [Google Scholar]
- 59.Karunaharan T. Malignant mesothelioma of the tunica vaginalis in an asbestos worker. J R Coll Surg Edinb. 1986;31(4):253–254. [PubMed] [Google Scholar]
- 60.Petersen RO. Urologic Pathology. Philadelphia: J.B. Lippincott Company; 1986. [Google Scholar]
- 61.Cartwright LE, Steinman HK. Malignant papillary mesothelioma of the tunica vaginalis testes: cutaneous metastases showing pagetoid epidermal invasion. J Am Acad Dermatol. 1987;17(5 Pt 2):887–890. doi: 10.1016/S0190-9622(87)70275-8. [DOI] [PubMed] [Google Scholar]
- 62.Fitzmaurice H, Hotiana MZ, Crucioli V. Malignant mesothelioma of the tunica vaginalis testis. Br J Urol. 1987;60(2):184. doi: 10.1111/j.1464-410X.1987.tb04966.x. [DOI] [PubMed] [Google Scholar]
- 63.Linn R, Moskovitz B, Bolkier M, Munichor M, Levin DR. Paratesticular papillary mesothelioma. Urol Int. 1988;43(1):60–61. doi: 10.1159/000281306. [DOI] [PubMed] [Google Scholar]
- 64.Prescott S, Taylor RE, Sclare G, Busuttil A. Malignant mesothelioma of the tunica vaginalis testis: a case report. J Urol. 1988;140(3):623–624. doi: 10.1016/S0022-5347(17)41741-1. [DOI] [PubMed] [Google Scholar]
- 65.Velasco AL, Ophoven J, Priest JR, Brennom WS. Paratesticular malignant mesothelioma associated with abdominoscrotal hydrocele. J Pediatr Surg. 1988;23(11):1065–1067. doi: 10.1016/S0022-3468(88)80034-4. [DOI] [PubMed] [Google Scholar]
- 66.Tyagi G, Munn CS, Kiser LC, Wetzner SM, Tarabulcy E. Malignant mesothelioma of tunica vaginalis testis. Urology. 1989;34(2):102–104. doi: 10.1016/0090-4295(89)90174-X. [DOI] [PubMed] [Google Scholar]
- 67.Kamiya M, Eimoto T. Malignant mesothelioma of the tunica vaginalis. Pathol Res Pract. 1990;186(5):680–684. doi: 10.1016/S0344-0338(11)80233-5. [DOI] [PubMed] [Google Scholar]
- 68.Smith JJ, 3rd, Malone MJ, Geffin J, Silverman ML, Libertino JA. Retroperitoneal lymph node dissection in malignant mesothelioma of tunica vaginalis testis. J Urol. 1990;144(5):1242–1243. doi: 10.1016/S0022-5347(17)39706-9. [DOI] [PubMed] [Google Scholar]
- 69.Kuwabara H, Uda H, Sakamoto H, Sato A. Malignant mesothelioma of the tunica vaginalis testis. Report of a case and review of the literature. Acta Pathol Jpn. 1991;41(11):857–863. doi: 10.1111/j.1440-1827.1991.tb01630.x. [DOI] [PubMed] [Google Scholar]
- 70.Pfister M, Sáez D, Celeste F. Sonographic appearance of malignant mesothelioma of the tunica vaginalis testis in a child. J Clin Ultrasound. 1992;20(2):129–131. doi: 10.1002/jcu.1870200208. [DOI] [PubMed] [Google Scholar]
- 71.Adler BD, Kelsey PJ. Malignant mesothelioma of the tunica vaginalis testis. Australas Radiol. 1992;36(1):29–30. doi: 10.1111/j.1440-1673.1992.tb03068.x. [DOI] [PubMed] [Google Scholar]
- 72.Serio G, Ceppi M, Fonte A, Martinazzi M. Malignant mesothelioma of the testicular tunica vaginalis. Eur Urol. 1992;21(2):174–176. doi: 10.1159/000474830. [DOI] [PubMed] [Google Scholar]
- 73.Noble JG, Watkins A, Chappell ME, Heath AD. Mesothelioma of the tunica vaginalis of the testis. Br J Urol. 1992;70(3):328–329. doi: 10.1111/j.1464-410X.1992.tb15743.x. [DOI] [PubMed] [Google Scholar]
- 74.Fields JM, Russell SA, Andrew SM. Case report: ultrasound appearances of a malignant mesothelioma of the tunica vaginalis testis. Clin Radiol. 1992;46(2):128–130. doi: 10.1016/S0009-9260(05)80318-6. [DOI] [PubMed] [Google Scholar]
- 75.Moch H, Ohnacker H, Epper R, Gudat F, Mihatsch MJ. A new case of malignant mesothelioma of the tunica vaginalis testis. Immunohistochemistry in comparison with an adenomatoid tumor of the testis. Pathol Res Pract. 1994;190(4):400–404. doi: 10.1016/S0344-0338(11)80414-0. [DOI] [PubMed] [Google Scholar]
- 76.Saw KC, Barker TH, Khalil KH, Gaches CG. Biphasic malignant mesothelioma of the tunica vaginalis testis. Br J Urol. 1994;74(3):381–382. doi: 10.1111/j.1464-410X.1994.tb16634.x. [DOI] [PubMed] [Google Scholar]
- 77.Reynard JM, Hasan N, Baithun SI, Newman L, Lord MG. Malignant mesothelioma of the tunica vaginalis testis. Br J Urol. 1994;74(3):389–390. doi: 10.1111/j.1464-410X.1994.tb16640.x. [DOI] [PubMed] [Google Scholar]
- 78.Wenger MC, Cohen AJ, Greensite F. Thymic rebound in a patient with scrotal mesothelioma. J Thorac Imaging. 1994;9(3):145–147. doi: 10.1097/00005382-199422000-00005. [DOI] [PubMed] [Google Scholar]
- 79.Watanabe M, Kimura N, Kato M, Iwami D, Takahashi M, Nagura H. An autopsy case of malignant mesothelioma associated with asbestosis. Pathol Int. 1994;44(10-11):785–792. doi: 10.1111/j.1440-1827.1994.tb02927.x. [DOI] [PubMed] [Google Scholar]
- 80.Amin R. Case report: malignant mesothelioma of the tunica vaginalis testis--an indolent course. Br J Radiol. 1995;68(813):1025–1027. doi: 10.1259/0007-1285-68-813-1025. [DOI] [PubMed] [Google Scholar]
- 81.Magoha GA. Testicular cancer in Nigerians. East Afr Med J. 1995;72(9):554–556. [PubMed] [Google Scholar]
- 82.Huncharek M, Klassen M, Christiani D. Mesothelioma of the tunica vaginalis testis with possible occupational asbestos exposure. Br J Urol. 1995;75(5):679–680. doi: 10.1111/j.1464-410X.1995.tb07437.x. [DOI] [PubMed] [Google Scholar]
- 83.Umekawa T, Kurita T. Treatment of mesothelioma of the tunica vaginalis testis. Urol Int. 1995;55(4):215–217. doi: 10.1159/000282790. [DOI] [PubMed] [Google Scholar]
- 84.Eden CG, Bettochi C, Coker CB, Yates-Bell AJ, Pryor JP. Malignant mesothelioma of the tunica vaginalis. J Urol. 1995;153(3 Pt 2):1053–1054. [PubMed] [Google Scholar]
- 85.Joseph AK, Tschen JA, Sekula SA, Sudduth SH. Purpuric nodules along a surgical scar. Metastatic malignant mesothelioma of the tunica vaginalis testis. Arch Dermatol. 1995;131(4):484–485. doi: 10.1001/archderm.131.4.484. [DOI] [PubMed] [Google Scholar]
- 86.Lopez JI, Angulo JC, Ibañez T. Combined therapy in a case of malignant mesothelioma of the tunica vaginalis testis. Scand J Urol Nephrol. 1995;29(3):361–364. doi: 10.3109/00365599509180593. [DOI] [PubMed] [Google Scholar]
- 87.Jones MA, Young RH, Scully RE. Malignant mesothelioma of the tunica vaginalis.A clinicopathologic analysis of 11 cases with review of the literature. Am J Surg Pathol. 1995;19(7):815–825. doi: 10.1097/00000478-199507000-00010. [DOI] [PubMed] [Google Scholar]
- 88.Ahmed M, Chari R, Mufi GR, Azzopardi A. Malignant mesothelioma of the tunica vaginalis testis diagnosed by aspiration cytology--a case report with review of literature. Int Urol Nephrol. 1996;28(6):793–796. doi: 10.1007/BF02550729. [DOI] [PubMed] [Google Scholar]
- 89.Ascoli V, Facciolo F, Rahimi S, Scalzo CC, Nardi F. Concomitant malignant mesothelioma of the pleura, peritoneum, and tunica vaginalis testis. Diagn Cytopathol. 1996;14(3):243–248. doi: 10.1002/(SICI)1097-0339(199604)14:3<243::AID-DC9>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 90.Mathew BS, Jyothirmayi R, Nair MK. Case report: malignant mesothelioma of tunica vaginalis testis presenting with spinal metastasis--report of two cases. Br J Radiol. 1996;69(827):1067–1068. doi: 10.1259/0007-1285-69-827-1067. [DOI] [PubMed] [Google Scholar]
- 91.Berti E, Schiaffino E, Minervini MS, Longo G, Schmid C. Primary malignant mesothelioma of the tunica vaginalis of the testis. Immunohistochemistry and electron microscopy. Pathology. 1997;29(1):96–99. doi: 10.1080/00313029700169654. [DOI] [PubMed] [Google Scholar]
- 92.Agapitos E, Pavlopoulos PM, Marinos E, Doutsias A, Davaris P. Malignant mesothelioma of the tunica vaginalis testis: an immunohistochemical and bultrastructural study of two cases. Br J Urol. 1997;80(2):345–346. doi: 10.1046/j.1464-410X.1997.00287.x. [DOI] [PubMed] [Google Scholar]
- 93.Khan MA, Puri P, Devaney D. Mesothelioma of tunica vaginalis testis in a child. J Urol. 1997;158(1):198–199. doi: 10.1097/00005392-199707000-00070. [DOI] [PubMed] [Google Scholar]
- 94.Gupta SC, Gupta AK, Misra V, Singh PA. Pre-operative diagnosis of malignant mesothelioma of tunica vaginalis testis by hydrocele fluid cytology. Eur J Surg Oncol. 1998;24(2):153–154. doi: 10.1016/S0748-7983(98)91771-1. [DOI] [PubMed] [Google Scholar]
- 95.Lee M, Gaffney EF, Sweeney JP, McDermott TE, Butler MR, Thornhill JA. Mesothelioma of the tunica vaginalis--beware of the malignant hydrocoele. Ir Med J. 1998;91(2):64–65. [PubMed] [Google Scholar]
- 96.Plas E, Riedl CR, Pflüger H. Malignant mesothelioma of the tunica vaginalis testis: review of the literature and assessment of prognostic parameters. Cancer. 1998;83(12):2437–2446. doi: 10.1002/(SICI)1097-0142(19981215)83:12<2437::AID-CNCR6>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 97.Kanazawa S, Nagae T, Fujiwara T, Fujiki R, Mukai N, Sugihara Y, Yamaguchi N, Ohtani H, Higami Y, Ikeda T, Tsunoda T. Malignant mesothelioma of the tunica vaginalis testis: report of a case. Surg Today. 1999;29(10):1106–10. doi: 10.1007/s005950050654. [DOI] [PubMed] [Google Scholar]
- 98.Harmse JL, Evans AT, Windsor PM. Malignant mesothelioma of the tunica vaginalis: a case with an unusually indolent course following radical orchidectomy and radiotherapy. Br J Radiol. 1999;72(857):502–504. doi: 10.1259/bjr.72.857.10505018. [DOI] [PubMed] [Google Scholar]
- 99.Gupta NP, Agrawal AK, Sood S, Hemal AK, Nair M. Malignant mesothelioma of the tunica vaginalis testis: a report of two cases and review of literature. J Surg Oncol. 1999;70(4):251–254. doi: 10.1002/(SICI)1096-9098(199904)70:4<251::AID-JSO10>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 100.Fujisaki M, Tokuda Y, Sato S, Fujiyama C, Matsuo Y, Sugihara H, Masaki Z. Case of mesothelioma of the tunica vaginalis testis with characteristic findings on ultrasonography and magnetic resonance imaging. Int J Urol. 2000;7(11):427–430. doi: 10.1046/j.1442-2042.2000.00225.x. [DOI] [PubMed] [Google Scholar]
- 101.Poggi A, Longo F, Mansueto G, Scirocchi R, De Petris L, Gemma D, Borgomastro A, Marchei P. A case of mesothelioma of the tunica vaginalis testis, with involvement of the pleura and peritoneum. Tumori. 2000;86(3):256–257. doi: 10.1177/030089160008600315. [DOI] [PubMed] [Google Scholar]
- 102.Ferri E, Azzolini N, Sebastio N, Salsi P, Meli S, Cortellini P. Unusual case of mesothelioma of the tunica vaginalis associated with prostatic adenocarcinoma. Minerva Urol Nefrol. 2000;52(1):33–35. [PubMed] [Google Scholar]
- 103.Wolanske K, Nino-Murcia M. Malignant mesothelioma of the tunica vaginalis testis: atypical sonographic appearance. J Ultrasound Med. 2001;20(1):69–72. doi: 10.7863/jum.2001.20.1.69. [DOI] [PubMed] [Google Scholar]
- 104.Sebbag G, Hui Y, Shmookler BM, Sugarbaker PH. Malignant Mesothelioma of the male genital tract: report of two cases. Urol Oncol. 2001;6:261–264. doi: 10.1016/S1078-1439(01)00123-5. [DOI] [Google Scholar]
- 105.Gürdal M, Erol A. Malignant mesothelioma of tunica vaginalis testis associated with long-lasting hydrocele: could hydrocele be an etiological factor? Int Urol Nephrol. 2001;32(4):687–689. doi: 10.1023/A:1014433203297. [DOI] [PubMed] [Google Scholar]
- 106.Abe K, Kato N, Miki K, Nimura S, Suzuki M, Kiyota H, Onodera S, Oishi Y. Malignant mesothelioma of testicular tunica vaginalis. Int J Urol. 2002;9(10):602–603. doi: 10.1046/j.1442-2042.2002.00521.x. [DOI] [PubMed] [Google Scholar]
- 107.Bruno C, Minniti S, Procacci C. Diagnosis of malignant mesothelioma of the tunica vaginalis testis by ultrasound-guided fine-needle aspiration. J Clin Ultrasound. 2002;30(3):181–183. doi: 10.1002/jcu.10045. [DOI] [PubMed] [Google Scholar]
- 108.Iczkowski KA, Katz G, Zander DS, Clapp WL. Malignant mesothelioma of tunica vaginalis testis: a fatal case with liver metastasis. J Urol. 2002;167(2 Pt1):645–646. doi: 10.1016/S0022-5347(01)69106-7. [DOI] [PubMed] [Google Scholar]
- 109.Black PC, Lange PH, Takayama TK. Extensive palliative surgery for advanced mesothelioma of the tunica vaginalis. Urology. 2003;62(4):748. doi: 10.1016/S0090-4295(03)00673-3. [DOI] [PubMed] [Google Scholar]
- 110.García de Jalón A, Gil P, Azúa-Romeo J, Borque A, Sancho C, Rioja LA. Malignant mesothelioma of the tunica vaginalis. Report of a case without risk factors and review of the literature. Int Urol Nephrol. 2003;35(1):59–62. doi: 10.1023/A:1025952129438. [DOI] [PubMed] [Google Scholar]
- 111.Pelzer A, Akkad T, Herwig R, Rogatsch H, Pinggera GM, Bartsch G, Rehder P. Synchronous bilateral malignant mesothelioma of tunica vaginalis testis: early diagnosis. Urology. 2004;64(5):1031. doi: 10.1016/j.urology.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 112.Sawada K, Inoue K, Ishihara T, Kurabayashi A, Moriki T, Shuin T. Multicystic malignant mesothelioma of the tunica vaginalis with an unusually indolent clinical course. Hinyokika Kiyo. 2004;50(7):511–513. [PubMed] [Google Scholar]
- 113.Mishra A, Shet T. Clear cell mesothelioma of the testis with deciduoid areas--a case report. Indian J Pathol Microbiol. 2004;47(4):544–546. [PubMed] [Google Scholar]
- 114.Shimada S, Ono K, Suzuki Y, Mori N. Malignant mesothelioma of the tunica vaginalis testis: a case with a predominant sarcomatous component. Pathol Int. 2004;54(12):930–934. doi: 10.1111/j.1440-1827.2004.01774.x. [DOI] [PubMed] [Google Scholar]
- 115.Wang MT, Mak CW, Tzeng WS, Chen JC, Chang JM, Lin CN. Malignant mesothelioma of the tunica vaginalis testis: unusual sonographic appearance. J Clin Ultrasound. 2005;33(8):418–420. doi: 10.1002/jcu.20140. [DOI] [PubMed] [Google Scholar]
- 116.Gorini G, Pinelli M, Sforza V, Simi U, Rinnovati A, Zocchi G. Mesothelioma of the tunica vaginalis testis: report of 2 cases with asbestos occupational exposure. Int J Surg Pathol. 2005;13(2):211–214. doi: 10.1177/106689690501300214. [DOI] [PubMed] [Google Scholar]
- 117.Spiess PE, Tuziak T, Kassouf W, Grossman HB, Czerniak B. Malignant mesothelioma of the tunica vaginalis. Urology. 2005;66(2):397–401. doi: 10.1016/j.urology.2005.03.012. [DOI] [PubMed] [Google Scholar]
- 118.van Apeldoorn MJ, Rustemeijer C, Voerman BJ, Peterse J. Mesothelioma of thetunica vaginalis complicated by chyluria. J Clin Oncol. 2006;24(33):5329–5330. doi: 10.1200/JCO.2006.07.6596. [DOI] [PubMed] [Google Scholar]
- 119.Schure PJ, van Dalen KC, Ruitenberg HM, van Dalen T. Mesothelioma of thetunica vaginalis testis: a rare malignancy mimicking more common inguino-scrotal masses. J Surg Oncol. 2006;94(2):162–164. doi: 10.1002/jso.20428. [DOI] [PubMed] [Google Scholar]
- 120.Winstanley AM, Landon G, Berney D, Minhas S, Fisher C, Parkinson MC. The immunohistochemical profile of malignant mesotheliomas of the tunica vaginalis: a study of 20 cases. Am J Surg Pathol. 2006;30(1):1–6. doi: 10.1097/01.pas.0000178094.07513.71. [DOI] [PubMed] [Google Scholar]
- 121.Al-Qahtani M, Morris B, Dawood S, Onerheim R. Malignant mesothelioma of the tunica vaginalis. Can J Urol. 2007;14(2):3514–3517. [PubMed] [Google Scholar]
- 122.Liguori G, Garaffa G, Trombetta C, Bussani R, Bucci S, Belgrano E. Inguinal recurrence of malignant mesothelioma of the tunica vaginalis: one case report with delayed recurrence and review of the literature. Asian J Androl. 2007;9(6):859–860. doi: 10.1111/j.1745-7262.2007.00266.x. [DOI] [PubMed] [Google Scholar]
- 123.Guney N, Basaran M, Karayigit E, Müslümanoglu A, Guney S, Kilicaslan I, Gulbarut S. Malignant mesothelioma of the tunica vaginalis testis: a case report and review of the literature. Med Oncol. 2007;24(4):449–452. doi: 10.1007/s12032-007-0010-3. [DOI] [PubMed] [Google Scholar]
- 124.Boyum J, Wasserman NF. Malignant mesothelioma of the tunica vaginalis testis: a case illustrating Doppler color flow imaging and its potential for preoperative diagnosis. J Ultrasound Med. 2008;27(8):1249–1255. doi: 10.7863/jum.2008.27.8.1249. [DOI] [PubMed] [Google Scholar]
- 125.Candura SM, Canto A, Amatu A, Gerardini M, Stella G, Mensi M, Poggi G. Malignant mesothelioma of the tunica vaginalis testis in a petrochemical worker exposed to asbestos. Anticancer Res. 2008;28(2B):1365–1368. [PubMed] [Google Scholar]
- 126.Mathur SR, Aron M, Gupta R, Sharma MC, Arora VK. Malignant mesothelioma of tunica vaginalis: a report of 2 cases with preoperative cytologic diagnosis. Acta Cytol. 2008;52(6):740–743. doi: 10.1159/000325635. [DOI] [PubMed] [Google Scholar]
- 127.Ikegami Y, Kawai N, Tozawa K, Hayashi Y, Kohri K. Malignant mesothelioma of the tunica vaginalis testis related to recent asbestos. Int J Urol. 2008;15(6):560–561. doi: 10.1111/j.1442-2042.2008.02036.x. [DOI] [PubMed] [Google Scholar]
- 128.Barui GN, Karmakar R, Sinha A, Bhattacharya A. J Cytol. 2008;25-2:76–77. doi: 10.4103/0970-9371.42457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Goel A, Agrawal A, Gupta R, Hari S, Dey AB. Malignant mesothelioma of the tunica vaginalis of the testis without exposure to asbestos. Cases J. 2008;1(1):310. doi: 10.1186/1757-1626-1-310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Al-Salam S, Hammad FT, Salman MA, AlAshari M. Expression of Wilms tumor-1 protein and CD 138 in malignant mesothelioma of the tunica vaginalis. Pathol Res Pract. 2009;205(11):797–800. doi: 10.1016/j.prp.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 131.Bacchetta J, Ranchère D, Dijoud F, Droz JP. Mesothelioma of the testis and nephrotic syndrome: a case report. J Med Case Reports. 2009;3:7248. doi: 10.1186/1752-1947-3-7248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Chen JL, Hsu YH. Malignant mesothelioma of the tunica vaginalis testis: a case report and literature review. Kaohsiung J Med Sci. 2009;25(2):77–81. doi: 10.1016/S1607-551X(09)70044-0. [DOI] [PubMed] [Google Scholar]
- 133.de Lima GR, de Oliveira VP, Reis PH, Pinheiro FG, Lima MV, Gonzaga-Silva LF. A rare case of malignant hydrocele in a young patient. J Pediatr Urol. 2009;5(3):243–245. doi: 10.1016/j.jpurol.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 134.Aggarwal P, Sidana A, Mustafa S, Rodriguez R. Preoperative diagnosis of malignant mesothelioma of the tunica vaginalis using Doppler ultrasound. Urology. 2010;75(2):251–252. doi: 10.1016/j.urology.2009.07.1275. [DOI] [PubMed] [Google Scholar]
- 135.Bisceglia M, Dor DB, Carosi I, Vairo M, Pasquinelli G. Paratesticular mesothelioma. Report of a case with comprehensive review of literature. Adv Anat Pathol. 2010;17(1):53–70. doi: 10.1097/PAP.0b013e3181c66fbc. [DOI] [PubMed] [Google Scholar]
- 136.Klaassen Z, Lehrhoff BJ. Malignant mesothelioma of the tunica vaginalis testis: a rare , enigmatic tumor. Uro Today Int J. 2010;3(6). 10.3834/uij.1944-5784.2010.12.12.
- 137.Gupta R, Dey P, Vasishtha RK. Fine needle aspiration cytology in malignant mesothelioma of the tunica vaginalis testis. Cytopathology. 2011;22(1):66–68. doi: 10.1111/j.1365-2303.2010.00764.x. [DOI] [PubMed] [Google Scholar]
- 138.Park YJ, Kong HJ, Jang HC, Shin HS, Oh HK, Park JS. Malignant mesothelioma of the spermatic cord. Korean J Urol. 2011;52(3):225–229. doi: 10.4111/kju.2011.52.3.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Grey Venyo A, Costello BC. Malignant mesotelioma of tunica vaginalis testis complicating a hydrocele. Webmedcentral Urol. 2011;2(10):WMC002309. [Google Scholar]
- 140.Bass L, Hegeman TW. Multiple primary cancers including mesothelioma of the tunica vaginalis: case report and literature review with primary care focus. J Am Osteopath Assoc. 2011;111(8):483–486. [PubMed] [Google Scholar]
- 141.Ahmed S, Menon S, Desai S. Epithelioid malignant mesothelioma of tunica vaginalis with deciduoid features: an unusual malignancy clinically masquerading an inguinal hernia. Indian J Pathol Microbiol. 2012;55(1):89–91. doi: 10.4103/0377-4929.94868. [DOI] [PubMed] [Google Scholar]
- 142.Doo SW, Cho KH, Kim JS, Yang WJ, Choi IH, Lee DW, Hong SS, Song YS. Radiologicfindings of mesothelioma at the tunica vaginalis. Urology. 2012;80(1):e3–e5. doi: 10.1016/j.urology.2012.02.050. [DOI] [PubMed] [Google Scholar]
- 143.Abdelrahman M, Dowling C, O'Connor K, Mayer N, Kiely E. Malignant mesothelioma of the tunica vaginalis. J Surg Case Rep. 2012;2012(5):2. doi: 10.1093/jscr/2012.5.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Esen T, Acar O, Peker K, Sarman K, Musaoglu A, Tefekli A. Malignant mesothelioma of the tunica vaginalis: presenting with intermittent scrotal pain and hydrocele. Case Rep Med. 2012;2012:189170. doi: 10.1155/2012/189170.Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Hai B, Yang Y, Xiao Y, Li B, Chen C. Diagnosis and prognosis of malignant mesothelioma of the tunica vaginalis testis. Can Urol Assoc J. 2012;6(6):E238–E241. doi: 10.5489/cuaj.10200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Priester P, Kopecký J, Prošvicová J, Petera J, Zoul Z, Slováček L. Cutaneous recurrence of malignant mesothelioma of the tunica vaginalis testis: a rare case report. Onkologie. 2012;35(1-2):46–48. doi: 10.1159/000335884. [DOI] [PubMed] [Google Scholar]
- 147.Yen CH, Lee CT, Su CJ, Lo HC. Malignant mesothelioma of the tunica vaginalis testis: a malignancy associated with recurrent epididymitis? World J Surg Oncol. 2012;10:238. doi: 10.1186/1477-7819-10-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Mrinakova B, Ondrus D, Kajo K, Kunderlik M, Tkacova M, Ondrusova M. Paratesticular mesothelioma in young age. Case report. Klin Onkol. 2012;25(4):290–293. [PubMed] [Google Scholar]
- 149.Mensi C, Pellegatta M, Sieno C, Consonni D, Riboldi L, Bertazzi PA. Mesothelioma of tunica vaginalis testis and asbestos exposure. BJU Int. 2012;110(4):533–537. doi: 10.1111/j.1464-410X.2012.10932.x. [DOI] [PubMed] [Google Scholar]
- 150.Vijayan S, Carr R, Strachan J. Primary and secondary mesothelioma of the tunica vaginalis: a comparative case study. BJUI. 2012, 23/02/2012. 10.1002/BJUIw-2011-127-web.
- 151.Shelton D, Dalal N. Mesothelioma of the tunica vaginalis with BerEp4 and LeuM1 expression: identification of cytoplasmic tonofilaments by electron microscopy is a key diagnostic feature. J Clin Pathol. 2012;65(10):958–959. doi: 10.1136/jclinpath-2012-200845. [DOI] [PubMed] [Google Scholar]
- 152.Gemba K, Fujimoto N, Kato K, Aoe K, Takeshima Y, Inai K, Kishimoto T. National survey of malignant mesothelioma and asbestos exposure in Japan. Cancer Sci. 2012;103(3):483–490. doi: 10.1111/j.1349-7006.2011.02165.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Busto Martin L, Portela Pereira P, Sacristan Lista F, Busto Castañon L. Mesothelioma of the tunica vaginalis. Case report. Arch Esp Urol. 2013;66(4):384–388. [PubMed] [Google Scholar]
- 154.Gkentzis A, Sawalem K, Husain J. An unusual case of paratesticular mesothelioma on the site of previously excised epididymal adenomatoid tumour. Int J Surg Case Rep. 2013;4(5):460–462. doi: 10.1016/j.ijscr.2013.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Weng CH, Ho PY, Chen CK, Tsai WK. Incidentally discovered malignant mesothelioma of the tunica vaginalis. J Formos Med Assoc. 2013;112(1):57–58. doi: 10.1016/j.jfma.2011.08.024. [DOI] [PubMed] [Google Scholar]
- 156.Meng X, Guzzo TJ, Bing Z. Malignant mesotheliomas in spermatic cords: reports of two cases and a brief review of literature. Rare Tumors. 2013;5(1):e4. doi: 10.4081/rt.2013.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Rajan V, Nandhakumar R, Shanmugasundaram S, Ravi R, Natarajan S, Mohan G, Nanjundappan PM. Paratesticular malignant mesothelioma - a rare case presentation. Indian J Surg. 2013;75(Suppl 1):174–176. doi: 10.1007/s12262-012-0573-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Meisenkothen C, Finkelstein MM. Asbestos exposure and malignant mesothelioma of the tunica vaginalis testis:case series and review of the literature. OA Case Rep. 2013;2(2):17. [Google Scholar]
- 159.Hsu LN, Sung MT, Chiang PH. Paratesticular malignant mesothelioma in a patient exposed to asbestos for more than 50 years. Kaohsiung J Med Sci. 2014;30(10):537–538. doi: 10.1016/j.kjms.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 160.da Fonseca LG, Marques DF, Takahashi TK, Aguiar FN, Ravanini JN, Saragiotto DF. Malignant paratesticular mesothelioma. Autops Case Rep. 2014;4(1):45–51. doi: 10.4322/acr.2014.007.eCollection2014Jan-Mar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Stradella A, Conde-Gallego E, Escalera-Almendros CA, Durán-Martínez I. Malignant mesothelioma of tunica vaginalis. Actas Urol Esp. 2014;38(1):68–69. doi: 10.1016/j.acuro.2013.02.017. [DOI] [PubMed] [Google Scholar]
- 162.Yang LH, Yu JH, Xu HT, Lin XY, Liu Y, Miao Y, Wang L, Fan CF, Jiang GY, Ding SL, Li G, Wang EH. Mesothelioma of the tunica vaginalis testis with prominent adenomatoid features: a case report. Int J Clin Exp Pathol. 2014;7(10):7082–7087. [PMC free article] [PubMed] [Google Scholar]
- 163.Akin Y, Bassorgun I, Basara I, Yucel S. Malignant mesothelioma of tunica vaginalis: an extremely rare case presenting without risk factors. Singapore Med J. 2015;56(3):e53–e55. doi: 10.11622/smedj.2015053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Bandyopadhyay A, Bhattacharya S, Konar K. Preoperative cytological diagnosis of malignant mesothelioma of tunica vaginalis. Diagn Cytopathol. 2015;43(10):850–854. doi: 10.1002/dc.23325. [DOI] [PubMed] [Google Scholar]
- 165.Jankovichova T, Jankovich M, Ondrus D, Kajo K, Dubravicky J, Breza J. Extremely rare tumour--malignant mesothelioma of tunica vaginalis testis. Bratisl Lek Listy. 2015;116(9):574–576. doi: 10.4149/bll_2015_111. [DOI] [PubMed] [Google Scholar]
- 166.Silverio PC, Schoofs F, Iselin CE, Tille JC. Fourteen-year experience with the intraoperative frozen section examination of testicular lesion in a tertiary university center. Ann Diagn Pathol. 2015;19(3):99–102. doi: 10.1016/j.anndiagpath.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 167.D'Antonio A, Mastella F, Colucci A, Silvestre G. Malignant mesothelioma of spermatic cord in an elderly man with a history of Asbestos exposure. Urology. 2016;87:e1–e3. doi: 10.1016/j.urology.2015.09.020. [DOI] [PubMed] [Google Scholar]
- 168.Segura-González M, Urias-Rocha J, Castelán-Pedraza J. Malignant mesothelioma of the tunica vaginalis: a rare neoplasm--case report and literature review. Clin Genitourin Cancer. 2015;13(6):e401–e405. doi: 10.1016/j.clgc.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 169.Alesawi AM, Levesque J, Fradet V. Malignant mesothelioma of the tunica vaginalis testis: comprehensive review of literature and acse report. JCU. 2015;8(2):147–52. 10.1177/2051415813511082uro.sagepub.com.
- 170.Hispán P, Pascual JC, González I, Bravo D, Peiró G. Cutaneous metastases from malignant mesothelioma of the tunica vaginalis testis. Am J Dermatopathol. 2016;38(3):222–225. doi: 10.1097/DAD.0000000000000369. [DOI] [PubMed] [Google Scholar]
- 171.Mrinakova B, Kajo K, Ondrusova M, Simo J, Ondrus D. Malignant mesothelioma of the tunica vaginalis testis. A Clinicopathologic analysis of two cases with a review of the literature. Klin Onkol. 2016;29(5):369–374. doi: 10.14735/amko2016369. [DOI] [PubMed] [Google Scholar]
- 172.Ahmed Z, Singh S, Mangal A, Mittal A. Primary malignant mesothelioma of the spermatic cord. BMJ Case Rep. 2016;2016. 10.1136/bcr-2016-214602. [DOI] [PMC free article] [PubMed]
- 173.Andresen ED, Henning G, Uhlman MA, Gupta A. Malignant mesothelioma of the tunica vaginalis: a rare case report and description of multimodal treatment. Can J Urol. 2016;23(6):8585–8589. [PubMed] [Google Scholar]
- 174.Serio G, Pagliarulo V, Marzullo A, et al. Molecular changes of malignant mesothelioma in the testis and their impact on prognosis: analyses of two cases. Int J Clin Exp Pathol. 2016;9(7):7658–7667. [Google Scholar]
- 175.Bertolotto M, Boulay-Coletta I, Butini R, Dudea SM, Grenier N, Oltmanns G, Ramchandani P, Stein MW, Valentino M, Derchi LE. Imaging of mesothelioma of tunica vaginalis testis. Eur Radiol. 2016;26(3):631–638. doi: 10.1007/s00330-015-3887-9. [DOI] [PubMed] [Google Scholar]
- 176.Zhang N, Fu N, Peng S, Luo X. Malignant mesothelioma of the tunica vaginalis testis: a case report and literature review. Mol Clin Oncol. 2017;7(6):1053–1056. doi: 10.3892/mco.2017.1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Arda E, Arıkan MG, Cetin G, Kuyumcuoğlu U, Usta U. Malignant mesothelioma of tunica vaginalis testis: macroscopic and microscopic features of a very rare malignancy. Cureus. 2017;9(11):e1860. doi: 10.7759/cureus.1860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Recabal P, Rosenzweig B, Bazzi WM, Carver BS, Sheinfeld J. Malignant mesothelioma of the tunica vaginalis testis: outcomes following surgical management beyond radical orchiectomy. Urology. 2017;107:166–170. doi: 10.1016/j.urology.2017.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Shaikh AA, Naik KV, Shetty SN, Ansari NN, Babhale PS. Bilateral malignant mesothelioma of tunica vaginalis a case report on rare presentation. Urol Case Rep. 2017;14:53–55. doi: 10.1016/j.eucr.2017.06.006.eCollection2017Sep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.An JY, Kim D, Tanakchi S, Semerjian AM, Thomas A, Boyle SL, Hassan R, Metwalli AR. Clinical features and outcomes of tunica vaginalis mesothelioma: a case series from the National Institutes of Health. Clin Genitourin Cancer. 2017;15(5):e871–e875. doi: 10.1016/j.clgc.2017.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Maheshwari PN, Abiola OO, Wagaskar VG, Oswal AT. Hydrocele with a surprise: Malignant mesothelioma of the tunica vaginalis - Case report and review of literature. Urol Ann. 2017;9(1):110–112. doi: 10.4103/0974-7796.198877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Abello Alejandro, Steinkeler Jennifer, Das Anurag K. A Bilateral Metachronous Mesothelioma of the Tunica Vaginalis. Urology. 2018;120:e1–e2. doi: 10.1016/j.urology.2018.07.003. [DOI] [PubMed] [Google Scholar]
- 183.Trenti E, Palermo SM, D'Elia C, Comploj E, Pycha A, Carella R, Pycha A. Malignant mesothelioma of tunica vaginalis testis: report of a very rare case with review of the literature. Arch Ital Urol Androl. 2018;90(3):212–214. doi: 10.4081/aiua.2018.3.212. [DOI] [PubMed] [Google Scholar]
- 184.Zhang S, Zhang Q, Sun Q, Tang J, Chen J, Ji N, Zheng Y, Fang F, Lei W, Li P, Zhang N. Genome evolution analysis of recurrent testicular malignant mesothelioma by whole-genome sequencing. Cell Physiol Biochem. 2018;45(1):163–174. doi: 10.1159/000486355. [DOI] [PubMed] [Google Scholar]
- 185.Nesti M, Adamoli S, Ammirabile F, et al. Guidelines for the identification and definition of malignant mesothelioma cases and the transmission to Ispesl by regional operating centres, monograph. Rome: ISPESL; 2003. [Google Scholar]
- 186.de Klerk DP, Nime F. Adenomatoid tumors (mesothelioma) of testicular and paratesticular tissue. Urology. 1975;6(5):635–641. doi: 10.1016/0090-4295(75)90521-X. [DOI] [PubMed] [Google Scholar]
- 187.Garriga V, Serrano A, Marin A, Medrano S, Roson N, Pruna X. US of the tunica vaginalis testis: anatomic relationships and pathologic conditions. Radiographics. 2009;29(7):2017–2032. doi: 10.1148/rg.297095040. [DOI] [PubMed] [Google Scholar]
- 188.Chekol SS, Sun CC. Malignant mesothelioma of the tunica vaginalis testis: diagnostic studies and differential diagnosis. Arch Pathol Lab Med. 2012;136(1):113–117. doi: 10.5858/arpa.2010-0550-RS. [DOI] [PubMed] [Google Scholar]
- 189.Mezei G, Chang ET, Mowat FS, Moolgavkar SH. Epidemiology of mesothelioma of the pericardium and tunica vaginalis testis. Ann Epidemiol. 2017;27(5):348–359.e11. doi: 10.1016/j.annepidem.2017.04.001. [DOI] [PubMed] [Google Scholar]
- 190.Mackay B, Bennington JL, Skoglund RW. The adenomatoid tumor: fine structural evidence for a mesothelial origin. Cancer. 1971;27(1):109–115. doi: 10.1002/1097-0142(197101)27:1<109::AID-CNCR2820270116>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 191.Ham AW. Histology 2nd ed. Philadelphia: J.B. Lippincott Co; 1953. pp. 163–164. [Google Scholar]
- 192.Stavridess A, Hutcheson JB. Benign mesotheliomas of testicular appendages: a morphologic and histochemical study of seven cases and review of theories of histogenesis. J Urol. 1960;83:448–453. doi: 10.1016/S0022-5347(17)65736-7. [DOI] [PubMed] [Google Scholar]
- 193.Holland JM. Multiple mesothelial cystis of the parietal tunica vaginalis testis: case report. J Urol. 1962;87(6):903–905. doi: 10.1016/S0022-5347(17)65065-1. [DOI] [PubMed] [Google Scholar]
- 194.Amin MB. Selected other problematic testicular and paratesticular lesions: rete testis neoplasms and pseudotumors, mesothelial lesions and secondary tumors. Mod Pathol. 2005;18(Suppl 2):S131–S145. doi: 10.1038/modpathol.3800314. [DOI] [PubMed] [Google Scholar]
- 195.Lloreta-Trull J. Extrathoracic mesothelial proliferations and their mimics. Ultrastruct Pathol. 2006;30(1):37–51. doi: 10.1080/01913120500313200. [DOI] [PubMed] [Google Scholar]
- 196.Vagnoni V, Brunocilla E, Schiavina R, Borghesi M, Passaretti G, Gentile G, Fiorentino M, Martorana G. Inguinal canal tumors of adulthood. Anticancer Res. 2013;33(6):2361–2368. [PubMed] [Google Scholar]
- 197.Mikuz G, Höpfel-Kreiner I. Papillary mesothelioma of the tunica vaginalis propria testis. Case report and ultrastructural study. Virchows Arch A Pathol Anat Histol. 1982;396(2):231–238. doi: 10.1007/BF00431244. [DOI] [PubMed] [Google Scholar]
- 198.Anchala PR, Dhir R, Parwani AV, Zynger DL. Immunohistochemical profile of paratesticular serous papillary adenocarcinoma and tunica vaginalis facilitates distinction from malignant mesothelioma. Int J Surg Pathol. 2011;19(5):692–698. doi: 10.1177/1066896909337504. [DOI] [PubMed] [Google Scholar]
- 199.Tan WK, Tan MY, Tan WS, Gan SC, Pathmanathan R, Tan HM, Tan WP. Well-differentiated papillary mesothelioma of the tunica vaginalis: case report and systematic review of literature. Clin Genitourin Cancer. 2016;14(4):e435–e439. doi: 10.1016/j.clgc.2016.03.007. [DOI] [PubMed] [Google Scholar]
- 200.Perez-Ordonez B, Srigley JR. Mesothelial lesions of the paratesticular region. Semin Diagn Pathol. 2000;17(4):294–306. [PubMed] [Google Scholar]
- 201.Husain AN, Colby TV, Ordóñez NG, Krausz T, Borczuk A, Cagle PT, Chirieac LR, Churg A, Galateau-Salle F, Gibbs AR, Gown AM, Hammar SP, Litzky LA, Roggli VL, Travis WD, Wick MR. Guidelines for pathologic diagnosis of malignant mesothelioma: a consensus statement from the international mesothelioma interest group. Arch Pathol Lab Med. 2009;133(8):1317–1331. doi: 10.1043/1543-2165-133.8.1317. [DOI] [PubMed] [Google Scholar]
- 202.Khoubehi B, Mishra V, Ali M, Motiwala H, Karim O. Adult paratesticular tumours. BJU Int. 2002;90(7):707–715. doi: 10.1046/j.1464-410X.2002.02992.x. [DOI] [PubMed] [Google Scholar]
- 203.Churg A, Galateau-Salle F. The separation of benign and malignant mesothelial proliferations. Arch Pathol Lab Med. 2012;136(10):1217–1226. doi: 10.5858/arpa.2012-0112-RA. [DOI] [PubMed] [Google Scholar]
- 204.Gupta NP, Kumar R. Malignant gonadal mesothelioma. Curr Treat Options Oncol. 2002;3(5):363–367. doi: 10.1007/s11864-002-0001-8. [DOI] [PubMed] [Google Scholar]
- 205.Frias-Kletecka MC, MacLennan GT. Mesothelioma of the tunica vaginalis. J Urol. 2007;178(4 Pt 1):1489. doi: 10.1016/j.juro.2007.07.067. [DOI] [PubMed] [Google Scholar]
- 206.Vimercati L, Cavone D, Lovreglio P, De Maria L, Caputi A, Ferri GM, Serio G. Environmental asbestos exposure and mesothelioma cases in Bari, Apulia region, southern Italy: a national interest site for land reclamation. Environ Sci Pollut Res Int. 2018;25(16):15692–15701. doi: 10.1007/s11356-018-1618-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Hillerdal G. The pathogenesis of pleural plaques and pulmonary asbestosis: possibilities and impossibilities. Eur J Respir Dis. 1980;61(3):129–138. [PubMed] [Google Scholar]
- 208.Miserocchi G, Sancini G, Mantegazza F, Chiappino G. Translocation pathways for inhaled asbestos fibers. Environ Health. 2008;7:4. doi: 10.1186/1476-069X-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Mirabella F. Malignant mesothelioma of the tunica vaginalis of the testis.Here again asbestos? Minerva Med. 1991;82(11):765–770. [PubMed] [Google Scholar]
- 210.Musti M, Kettunen E, Dragonieri S, Lindholm P, Cavone D, Serio G, Knuutila S. Cytogenetic and molecular genetic changes in malignant mesothelioma. Cancer Genet Cytogenet. 2006;170(1):9–15. doi: 10.1016/j.cancergencyto.2006.04.011. [DOI] [PubMed] [Google Scholar]
- 211.Serio Gabriella, Pezzuto Federica, Marzullo Andrea, Scattone Anna, Cavone Domenica, Punzi Alessandra, Fortarezza Francesco, Gentile Mattia, Buonadonna Antonia, Barbareschi Mattia, Vimercati Luigi. Peritoneal Mesothelioma with Residential Asbestos Exposure. Report of a Case with Long Survival (Seventeen Years) Analyzed by Cgh-Array. International Journal of Molecular Sciences. 2017;18(8):1818. doi: 10.3390/ijms18081818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Serio G, Vimercati L, Pennella A, Gentile M, Cavone D, Buonadonna AL, Scattone A, Fortarezza F, De Palma A, Marzullo A. Genomic changes of chromosomes 8p23.1 and 1q21: novel mutations in malignant mesothelioma. Lung Cancer. 2018;126:106–111. doi: 10.1016/j.lungcan.2018.10.012. [DOI] [PubMed] [Google Scholar]
- 213.De Rienzo A, Testa JR. Malignant mesotelioma. Atlas Genet Cytogenet Oncol Haematol. 2018;22(9):403–406. [Google Scholar]
- 214.Dipalma N, Luisi V, Di Serio F, Fontana A, Maggiolini P, Licchelli B, Mera E, Bisceglia L, Galise I, Loizzi M, Pizzigallo MA, Molinini R, Vimercati L. Biomarkers in malignant mesothelioma: diagnostic and prognostic role of soluble mesothelin-related peptide. Int J Biol Markers. 2011;26(3):160–165. doi: 10.5301/JBM.2011.8614. [DOI] [PubMed] [Google Scholar]
- 215.Jean D, Daubriac J, Le Pimpec-Barthes F, Galateau-Salle F, Jaurand MC. Molecular changes in mesothelioma with an impact on prognosis and treatment. Arch Pathol Lab Med. 2012;136(3):277–293. doi: 10.5858/arpa.2011-0215-RA. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset and articles used and analyzed during the study are available from the corresponding author on reasonable request.


