Abstract
Recent global commitments to shift responsibility for Neglected Tropical Disease (NTD) control to affected countries reflect a renewed emphasis on sustainability, away from aid-dependency. This calls for a better understanding of how domestic stakeholders perceive investments in different strategies for NTD control. Soil transmitted helminths (STH) are among the NTDs targeted for elimination as a public health problem by international agencies through mass drug administration, provided periodically to at-risk population groups, often using drugs donated by pharmaceutical companies. This study was conducted in Kenya at a time when responsibilities for long running STH programmes were transitioning from external to national and sub-national agencies. Following an initial assessment in which we identified key domestic stakeholders and reviewed relevant scientific and government documents, the perspectives of stakeholders working in health, education, community engagement and sanitation were investigated through semi-structured interviews with national level policymakers, county level policymakers, and frontline implementers in one high-STH burden county, Kwale. Our conceptual framework on sustainability traced a progression in thinking, from ensuring financial stability through the technical ability to adapt to changing circumstances, and ultimately to a situation where a programme is prioritised by domestic policymakers because empowered communities demand it. It was clear from our interviews that most Kenyan stakeholders sought to be at the final stage in this progression. Interviewees criticised long-term investment in mass drug administration, the approach favoured predominantly by external agencies, for failing to address underlying causes of STH. Instead they identified three synergistic priority areas for investment: changes in institutional structures and culture to reduce working in silos; building community demand for and ownership; and increased policymaker engagement on underlying socioeconomic and environmental causes of STH. Although challenging to implement, the shift in responsibility from external agencies to domestic stakeholders may lead to emergence of new strategic directions.
Keywords: Sustainability, Aid-dependency, Neglected Tropical Diseases, Elimination, Kenya
Introduction
Neglected Tropical Diseases (NTDs) have, at last, reached the mainstream global development agenda with the Sustainable Development Goals now containing a target (3.3.5) to reduce the ‘number of people requiring interventions against neglected tropical diseases’ [1]. This is the culmination of a transition, over several decades, from a series of largely separate programmes seeking to control these diseases, to co-ordinated policies to eliminate them where possible. Important steps along this path included a WHO Roadmap, published in 2012, that set targets for ‘control, prevention, elimination and eradication of NTDs’ [2]. This was soon followed by the London Declaration to control or eliminate ten NTDs by 2020 [3], bringing together global health and developmental organizations, donor agencies, and the pharmaceutical industry. The main strategy favoured by the WHO Roadmap and London Declaration for the five NTDs amenable to ‘preventive chemotherapy’ was mass drug administration (MDA) provided periodically to at-risk population groups.
The MDA programmes are reliant upon medicines mostly donated by multinational pharmaceutical companies, with strict coverage targets considered to be key programmatic performance indicator [4]. Although MDA has been positioned as a low-cost ‘rapid impact package’, implementation is not always straightforward [5–8]. For intestinal worm infections, also known as soil transmitted helminths (STH), treatment campaigns have often but not exclusively been delivered through schools, which provide easy access to children, the population group at greater risk of morbidity. In 2017, the WHO expanded its recommendation for MDA to also include pre-school children, adolescent girls, women of reproductive age and pregnant women to control the morbidity associated with STH [9]. This expansion helps to address concerns that treating only school-aged children misses a large number of those at risk of infection [10–12], but the suggested policy change poses major implementation challenges, given the lack of delivery platforms to reach the general population in many settings. Furthermore, mass treatment does not prevent reinfection from contaminated soil, so it is likely that treatment gains would not be maintained over the longer term without investment in a much wider programme that addresses improvements in sanitation and hygiene behaviours [11, 13, 14].
Consequently, while the offers by pharmaceutical companies to donate drugs for MDA make such programmes seem attractive, they fail to address weaknesses in infrastructure critical to sustaining implementation, the maintenance of support from policymakers and communities in affected countries, and broader socioeconomic and environmental causes of STH. This recognition has led the WHO and experts in NTD control to call on national governments to take ownership of NTD programmes from the donor agencies now leading them [15, 16]. Thus, a resolution at the 66th World Health Assembly, in 2013, called on Member States to ensure country ownership of prevention, control, elimination and eradication programmes and for international partners to play a smaller role focusing on targeted funding support [16]. Other policy documents also emphasised that while control of NTDs in low resource settings can be supported by, resources invested by external agencies, they should not be driven indefinitely by them [2]. This has profound implications for policymakers in countries with a high NTD burden and a high dependency on external agencies given that the transfer of responsibility from external agencies often occurs in the context of constrained domestic capacity for implementation, reduced technical support, and ongoing wider transactional relationships with the donors from whom they are taking over [17].
While the diverse perspectives of those in the international community, both researchers and policy makers, are well documented, rather less attention has been given to investigating the views of stakeholders in the countries affected about what should be prioritised to achieve sustained impact (which, in the case of STH, would be elimination of ongoing transmission). This question has become critical considering the push to transfer responsibility for NTD programmes from external agencies to domestic stakeholders. The limited available evidence indicates that the various stakeholderssuch as domestic policymakers, funders, healthcare providers, teachers and community members – may have different perspectives on priorities for investment [18, 19], according to what they value most, with ample scope for potential conflicts of interest. For example, donors may seek to reduce dependence on the financial assistance they provide whereas health programme staff may be most concerned about maintaining their jobs and beneficiaries may think mainly about continuation or expansion of services [20]. An analysis of domestic stakeholders working in HIV programmes in six countries illustrated differences in preferred strategies such as prioritization (of specific population sub-groups or interventions), efficiency improvements and mobilisation of national resources [21]. Given the shift in power and responsibility for NTD programmes away from international partners and to national and subnational policymakers, understanding their priorities for investment in health is essential. Different strategic directions may emerge as countries shift from aid dependence to domestically driven strategies.
This paper examines the experience of one country, Kenya, which has already made considerable progress in implementing STH control programmes. The country has an estimated 9.4 million pre-school and school-aged children living in areas with endemic STH [22]. In 2009, Kenya was among the first countries to launch a national school-based deworming (SBD) programme based on preventive chemotherapy. It did so within the framework of an international partnership, including funding from the national government, involvement by the Ministries of Health and Education, and technical support and drugs from Deworm the World initiative and the Partnership for Child Development [23]. By 2012, the Kenyan Ministries of Health and Education had started to implement work in four regions (Western, Nyanza, Rift Valley and Coast) known to have a high prevalence of STH [24] and, by 2017, were treating over 6 million children. Now, extension of preventive chemotherapy to adults is being considered, drawing lessons from the TUMIKIA cluster randomised controlled trial [25], in which the two of the intervention arms include annual or twice annual deworming of the entire population using community health volunteers. The programme has also been supported extensively by international partners, although it is intended that the government of Kenya will continue the programme if it is shown to be effective [26].
It is not clear, however, what strategies for STH control Kenyan policymakers will support if they take on full programme ownership, particularly as they must commit limited internal resources. Health reforms implemented in Kenya between 2010 and 2013 have devolved responsibility for management and delivery of services from central government to 47 newly created semi-autonomous counties. This has coincided with a decline in external donor funding [27]. The new county administrations thus face considerable challenges in managing resource allocation across numerous competing heath priorities [28], as does the national Ministry of Health, which is now tasked with policymaking and technical support [27]. In light of the shifting responsibilities for financing and implementation of NTD programmes, we investigate perspectives of Kenyan stakeholders working at the national, county, sub-county and community level, about priority areas for investment that they believe will lead to the control of STH.
Theorising dependency and stakeholder views on the goals of investments in health for sustained impact
We first summarise key elements of the literature on aid dependence and how this can constrain the extent to which domestic stakeholders’ goals and priorities influence national health programmes. Following this, we outline three ways in which the goals of investment in health to achieve sustained impact have been conceptualised in the literature; these conceptualisations will be compared with views of domestic stakeholders through our qualitative investigation. Investment in health programmes is shaped by a complex intersection of institutional and political interests[29]. Governments and non-governmental organisations (NGOs) in Low and Middle-Income Countries (LMICs) often depend on external agencies for financial resources or technical expertise. Funding often moves along an ‘aid chain’ – as exemplified by the Deworm the World Initiative in Kenya – originating from large funding agencies and moving through an intermediary NGO based in Northern countries [31]. With their control of scarce resources, external agencies acquire power to influence goals and strategies of programmes they invest in, with their goals sometimes differing substantially from those of domestic policymakers [32, 33].
This model has been supported by some commentators, based largely on epistemic claims of expertise and technical capacity to deliver policy-optimal outcomes [34]. The validity – and sufficiency – of such claims are, however, subject to growing critique, particularly because of a shift in the balance between external and domestic investment in health [35, 36]. Indeed, some theories explain why external agencies, by their very nature, do not possess superior technical expertise on health and development. Thus, Lindenberg and Bryant highlight two concerns of domestic stakeholders tasked with implementing strategies largely designed by external agencies [37]. Firstly, those strategies are often developed in very different contexts from those in which they will be implemented and so may be misaligned with local cultures and institutions [38]. Secondly, under pressure from donor governments or other funders, external agencies often favour easily quantifiable results, rather than addressing the complex underlying causes of the problem.
Recent commitments, described above, to transfer responsibility for NTD programmes to national governments have, at their core, an emphasis on sustainability by reducing aid-dependency [17, 39]. The importance of sustainability is recognised by most external agencies, even if they take differing approaches to conceptualising the desired health outcomes of investments. Sustainability is commonly described in terms of benefits from an intervention or policy which continue into the future [30, 40–43]. These concepts are evolving. Three broad conceptualisations of desirable outcomes or benefits can be identified and are summarised in Table 1. These provide the basis of our analytical framework.
Table 1. Differing stakeholder views of strategies to achieve long term improvements in health [40, 51, 73].
| What should be maintained? | Definitions | Stakeholder Discipline/Approach | Illustrative references |
|---|---|---|---|
| 1. Financial self-sufficiency of the health programme |
|
International assistance and development [views of external agencies providing resources] | Lafond, 1995 |
|
Health promotion/[enabling people to increase control over, and improve, their health] | Hanson et al, 2005 | |
|
Public Health | Bowman, 2008 | |
| 2. Institutional changes |
|
Complex systems [taking into account structural complexity owing to interconnectedness of systems] | Greenhalgh, 2012 |
|
Programme planning [ensuring elements are in place to meet stakeholder needs] | Johnson et al 2004 | |
| 3. Community empowerment or ownership |
|
Community development [focusing on processes enabling affected communities to take action] | Bennett at al, 2011 |
| A combination of the above | Complex systems/Organisational theory | Nelson et al 2007 | |
The first draws on ideas from the 1990s, when the international assistance discourse saw success in terms of being financially self-sufficient to continue running a specific health programme (point 1 in Table 1)[44]. This was interpreted as meaning that recipients could continue a programme initiated by the donor using their own resources[43]. Thus, reducing aid-dependency and sustainability was conceived primarily in financial terms. Others such, as Hanson et al. argued for a broader concept than simply sustaining a programme, and included sustaining the programme’s outcomes, such as improved health, in their conceptualisation of sustainability [45]. This later developed to include the ability of communities to adapt the programme in ways that enabled it to remain operational [46]. The second draws on the literature on complex systems and on management and argues for sustaining something much broader than a single programme, such as embedded changes in cultures or structures of institutions (point 2 in table 1)[47, 48]. Meanwhile, the third concept, developed by researchers taking a community perspective, conceives sustainability primarily as the empowerment of communities (point 3 in Table 1), to enable them to demand actions to improve health over the long term and shape the programmes available to them [18, 19, 49]. Finally, these three conceptualisations have been combined to create a comprehensive definition of sustainability [50]
Methods
Our study included national level policymakers based in Nairobi and stakeholders in Kwale county, a setting which exemplifies ongoing challenges with sustainability of STH control programmes. Kwale is one of the poorest counties in Kenya, lying in the coastal region south of Mombasa. It has successfully implemented school-based deworming since 2009,[56] and has a mixed and interrupted experience of community-based mass drug administration for lymphatic filariasis since 2005.[57, 58] It is also the location of the TUMIKIA project, which is investigating the potential of wider MDA to entire communities as a strategy to interrupt STH transmission [25].
Prior to initiating this study, a detailed documentary and literature review was conducted. The purpose of the review was to identify plans for sustainability formulated by different institutions, including plans to continue the programme or exit. Abstracts and executive summaries were reviewed for relevance to the research question. Full texts were obtained where relevant. Our final selection comprised 13 sources (eight peer-reviewed papers [23, 56, 59–63] and five government reports for the ministries of health and education [58, 64–67]. Each document was then analysed to identify references to sustainability, continuity or long-term planning of STH programme development over time.
The documentary analysis also identified key actors involved in institutional efforts to promote sustainability. This guided us to preliminary conversations with agencies implementing STH control, to understand the structures, processes and the roles of different stakeholders. A purposive sampling method was then used to recruit key informants for in-depth interviews, based on their close involvement with deworming in Kenya, either as those making decisions on resource allocation for deworming and other public health programmes, or as deworming programme implementers. We then added further stakeholders mentioned as influential during the initial interviews. In total, we conducted 29 face-to-face, in-depth interviews with three broad categories of key informants (table 2). These were national level policymakers (health, education, water and sanitation) (n=5); county and sub-county level policymakers (n=13) identified as key to current implementation and future fund allocation decisions and leading the departments of public health, water and sanitation, community engagement, nutrition, NTDs, administration and education; and frontline implementers (n=11), including teachers, Community Health Workers, and community mobilisers.
Table 2. Summary of participants included in the study.
| Stakeholder group | Number of interviewees | Coding |
|---|---|---|
| National level policymakers | 5 | NHP |
| County and sub-county level policymakers | 13 | County Health Policymaker = CHP (9) County Education Policymaker = ED (5) |
| Implementers | 11 | Community health worker = CHW (7) Teachers = T (3) Community Mobiliser = CM (1) |
Interviews with healthcare workers and teachers were conducted by a native Kenyan female researcher with training and experience in qualitative research methods (MN, MSc), in English or Swahili depending on the interviewee’s preference. Interviews with policymakers and county-level managers working in the health and education sector were conducted jointly by MN and a researcher with international experience in qualitative ‘elite’ policy interviews (MSK, PhD), in English. All participants were approached prior to the interviews by a phone call or email. Interviews lasted between 20 and 60 minutes, were conducted in the participant’s workplace and no participants who were approached refused to participate. Data were collected between October 2016 and March 2017, using a piloted topic guide seeking views on current and ideal goals for investments that would lead to long-term (sustainable) control of STH in Kenya. We focused specifically on the question ‘what should be sustained’ and for what purpose. All interviews were recorded with permission, and audio recordings were transcribed verbatim and translated into English by native Kenyans fluent in English when required.
We conducted a thematic analysis – involving a search for themes that emerge as being important to the description of the phenomenon – employing an interpretive approach. The analysis was conducted manually. Identified themes were supported by excerpts from the raw data, to ensure that interpretation was directly linked to participants’ narratives. Two members of the research team (MSK, DB) independently identified themes emerging directly from the data. Codes were then compared between researchers and collated into potential themes and subthemes, using an iterative consensus decision-making process. Following this, one researcher (MSK) coded each transcript line by line [68] using a coding frame linked to the conceptualisations of sustainability identified in Table 1. Initial categories were compared with subsequent ones and refined until all the data were sorted, employing the constant comparison technique [69]. Reporting followed consolidated criteria for reporting qualitative research (COREQ) [70].
Results
We first present our analysis of interviews and documents in relation to the three conceptualisations of sustainability found in the literature. These involved, variously, sustaining: a specific health programme; institutional changes; or community empowerment/ownership. We then summarise views about investments to sustain domestic policymaker attention that emerged directly from the data (table 3).
Table 3. Comparison of findings about Kenyan stakeholders’ views on strategies for STH control with common conceptualisations of sustainability used by external agencies.
| Aims of sustainability efforts (following the conceptual framework) | Conceptualisation | Perspectives from Kenyan stakeholders |
|---|---|---|
| Sustaining a specific health programme | Policy, programme or intervention continued through use of internal resources with minimal external input Capacity to adapt or replace intervention/policy |
Opposing view of benefits to invest in; conceptualised in terms of decreasing need (over time) for ongoing investments in an intervention/policy owing to impact on addressing underlying causes of disease Adaptation based on community and domestic policymaker input considered important at design stage rather than only as part of evolution of an externally designed intervention/policy |
| Sustaining institutional changes | Integration of intervention/policy into routine operations or existing organisational structures Changes in culture of institutions |
Change in institutional structure and culture was seen as a key goal, but not with the aim of sustaining a specific intervention/policy. Investments to change siloed working and encourage cross-sectoral engagement were associated with sustained gains |
| Sustaining community empowerment or ownership | Community demand for intervention or policy Community empowerment |
Identified as a critical are to invest in to ensure sustainability of an intervention/policy because it results in community resource mobilisation and community demand which influences policy setting |
| Sustaining policy maker engagement [Additional factor emerging from data] | Improved priority setting and health policy design by policymakers such that important interventions are given financial and political attention | To encourage long-term investment and attention to a priority health issues by domestic policymakers, advocacy directed at policymakers and community demand was considered essential |
1. Sustainability conceived as the financial self-sufficiency of the specific health programme
Although external agencies often focus on whether a disease control intervention or programme –such as school- or community-based deworming – is carried on after external funding has ended, this was not seen as a worthwhile goal in itself by the majority of Kenyan stakeholders interviewed. There were two predominant views on the value of preventive chemotherapy interventions. Seven national and county level policymakers viewed MDA as justified if it was a temporary measure, in combination with strategies to tackle root causes of disease. Another view was that other wider health-related goals should be prioritised instead of focusing investments primarily on MDA.
A concept of sustainability in terms of delivering a disease-specific programme focused on preventive chemotherapy was criticised for neglecting the underlying causes of ill health, which require ongoing investment (4 x CHW; 4 x CHP; 1 x CM; 3 x ED; 2 x NHP). Indeed, many interviewees, working in health and education at national, county and community level, expressed strong views that specific interventions should not need to be continued in their current format over a prolonged period, as effective strategies should gradually reduce or eliminate the health problem (1 x NHP; 2 x CHP; 1 x CHW; 3 x ED).
Several interviewees (3 x-CHP; 1 x NHP; 1 x ED) felt that investments in medication programmes that fail to address underlying causes of ill health are of limited use, even as a short-term strategy. Five interviewees, from different backgrounds, voiced concerns about what happens outside of months when deworming tablets were provided, noting how the underlying causes of infection remain (2 x CHP; 1 x NHP; 1 x ED).
So what happens after 3 months, after 4 months, 6 months you go do an assessment, it’s still there, and children are infected. The environment remains the same, people are still defecating in the open, and people are still eating contaminated food and all those aspects… (NHP)
The view that mass drug administration-based interventions should not be the leading approach to improve STH outcomes (and health) was common. Even those who believed that deworming could be useful in the short term argued that greater emphasis should be placed on the underlying (behavioural and environmental) causes of ill health and the implied focus on immediate rather than long term health gains. Supporters of measures that address underlying environmental and socioeconomic determinants of STH, working at the county level, used strong language and stark illustrations to convey their feelings (2 x CHW; 2 x CHP; 1 x ED), with county level policymakers describing deworming as fight[ing] the fire (1-CHP) and a cycle of failure (CHP).
…from my view even giving drug is not necessary we should do prevention awareness before even giving drugs. (CHP)
The current prioritisation of short term goals, such as reduced worm load following deworming activities, requiring year on year investment but not planning for a long-term impact or addressing underlying causes, was repeatedly criticised:
Because for how long are we going to take the tablets? I think we should look at measures of prevention. (ED)
While the scientific papers we analysed mention sustainability in passing or not at all, the five government reports noted sustainability as a core policy issue. The first National School Health Strategy Implementation Plan defined long-term continuation of the STH-control programme as its overarching mission[64]. This was the only government document that framed sustainability as a progression towards addressing determinants of ill-health, such as safe and adequate water supply, sanitation and nutrition. However, sustainability was operationalised mainly in terms of sustainable nutrition in schools, with little explicit link to health sector deworming initiatives. The revised Strategic Plan also defined sustainability of NTD programmes as one of four strategic priorities[58]. Here the focus was on financial and operational sustainability, with proposed strategies seen mainly as a means to make the MDA programme cheaper and more efficient to run and scale up.
2. Sustainability conceived as achievement of institutional change
Many interviewees highlighted the critical importance of institutional change. A common thread was that change should involve evolution of fundamental structures and processes, and investment in such transformations was perceived to be a priority. However, the nature of the changes that were advocated varied. First, cultural and structural changes in institutions were valued if they removed silos that impede effective collaboration from those within and outside health institutions. They did not simply want institutional changes that allow incorporation of a specific programme into routine operations (in line with management theory-based conceptualisations of sustainability and the National School-Based Deworming Programme’s vision of having MDA institutionalised and integrated within the Ministry’s structures and processes[58, 67]). Second, interviewees perceived that vested interests of stakeholders perpetuate the curative-focused and silo-based approaches pursued by institutions supporting the NTD response.
Examples of desired institutional changes to sustain health gains, highlighted by many different interviewees, included measures to promote collaboration between those working in different disease-specific programmes and bureaucratic sub-divisions (2 x NHP; 2 x CHP; 1 x ED, 1 x CHW). Another area of major change was in enabling the engagement of health stakeholders with sectors outside health, such as nutrition and water and sanitation (2 x NHP, 1x CHP, 1 x ED).
But everybody is going his own way and those are the issues. We assume that health means medical and we want to hand over all things (to health departments). But when we look at it (we see) that it can been done together with people outside ministry of health, but we don’t engage them. (NHP)
The need for synergies between structures and institutional processes, in health and beyond, was emphasised not only by national and county level policymakers but also by health and education staff working at the frontline and in the 2nd National School Health Implementation Plan[58]. Five community health workers highlighted scope for cost saving from better coordination and integration of different aspects of service delivery, linked to notions of sustainability.
Likewise, three county policymakers in the education sector argued for a system that enables health and education to work together on multiple issues, for example related to implementing school-based health interventions. Thus, the views on the frontline were aligned with views of stakeholders involved in policy development.
Several interviewees identified potential to improve collaboration with the private sector and across different government departments. Opportunities included attracting new sources of income, from private or community-led financing (1 x NHP; 1 x ED), building on existing data collection and service delivery platforms or other efficiency measures (NHP), and changing the mindset of health policy-makers who focus predominantly on biomedical aspects of disease while neglecting the role of broader socioeconomic or environmental factors (1 x CHP; 1 x NHP)
So what we are actually talking about is a plan to improve on the efficiency of delivery, utilize the existing stakeholders within government and outside the government so that we have a very cheap delivery package that is affordable to us as we move in to sustainability. (NHP)
The second main aspect of this theme was the perception that vested interests perpetuated the perceived dominance of disease-specific, curative interventions at the expense of preventive efforts. Specifically, several interviewees pointed to the role of the pharmaceutical industry, encouraging national and international policy makers to prioritise interventions based on drug delivery rather than addressing causes of illness (2 x NHP; 2 x CHP; 1 x ED). Respondents discussed openly the self-interest of domestic decision makers, such as financial benefits from engaging with pharmaceutical companies (2 x NHP; 1 x CHP):
…the drug manufacturers want to sell their products and will convince you that the best option is to buy the drugs and have people treated… (NHP)
How long will Kwale county and Kenya as a country be for drugs and building goodwill for Kenyans to buy drugs from to these companies that are giving free drugs? It is not sustainable at a community level standpoint. (CHP)
Other interviewees believed that the silos created by vertical disease control programmes were perpetuated to allow programme managers to retain their jobs (2 x NHP; 1 x CHP). It was also felt by some interviewees working at the county level that the Kenyan health system contained skewed institutional priorities, in which curative and preventive services had to compete for funding, with the former attracting the majority of resources (2 x CHP; 1 x CHW).
3. Sustainability conceived as achievement of community empowerment and ownership of STH control interventions
Many respondents saw the promotion of community demand for and ownership of health improvements as a means of sustaining improvements in health (3 x CHP; 2 x CHW, 16; 3 x ED, 1 x NHP), for three reasons. First, healthy behaviours would reduce disease incidence, reducing the need for curative services (1 x NHP; 2 x CHP; 2 x CHW; 2 x ED).
If we health educate our community they will be enlightened, they will know what to do for them to stay healthy and that will be good, rather than pumping drugs in hospital which means we need our community just to be in sick beds. (CHW)
Second, it was felt that community members will invest their own resources where they see issues important to them being addressed by health interventions or policies, gradually reducing the need for interventions funded solely by the health sector (4 x CHP; 4 x CHW; 1 x ED); this concept was conveyed by those working in health at the county level but was not an issue raised by those working at the national level. Finally, county level policy makers also considered those actions demanded by communities as more likely to attract investment by politicians seeking re-election. Thus, investments in empowering communities could result in long-terms shifts in political priorities for health (3 x CHP).
The pitfalls of investing in curative interventions without creating community demand for them were highlighted by several implementers in health and education. These included refusals of communities to participate in interventions (3 x CHW) and reliance of service delivery staff – healthcare workers or teachers – on incentives for running programmes (2 x ED; 1 x T).
…you see some teachers are funny because they are not happy they make sure that we have a lot of wastage, dropping these tablets and all that… it’s a way of expressing a point but the health teacher (who is provided a financial incentive) becomes so committed unlike the other teachers who are just doing it because they were told and they have to do. (ED)
Several interviewees from different groups (1 x CHW; 1 x T) believed that a greater understanding of the importance of SBD as a means to improve health and school performance will result in increased demand for SBD among communities members, teachers and policymakers in the education sector.
It is important that the users (schools) start demanding for it as a routine service, but it is usually the ministry of health who seem to see the need of having the children dewormed. The ministry of education does not seem to understand the importance of deworming the children. I think it should be demand driven by the ministry of education. (CHP)
Again, there was a mismatch between the interviews and the government documents that addressed sustainability. Community engagement and ownership was only briefly mentioned, and primarily as a tool to improve coverage rather than empowering communities to assume a more substantial role.
4. Sustainability conceived as improved methods of priority setting and design of health policy design
Several interviewees argued for investing in measures that would influence the priorities of domestic policy-makers, something not identified in the literature summarised in Table 1 (2 x NHP, 3 x CHP; 1 x ED; 1 x T). The National Strategic Plan for Control of NTDs instead mentioned tools to guide effective policy and programme implementation rather than improving the capacity of domestic policymakers in relation to policy setting.
Some interviewees saw advocacy for neglected health issues (including NTDs) as important for sustainability because it would allow for continued pressure on policy makers to address these issues, and potentially influence future investment decisions: Explaining why he saw long-term advocacy as important, one national policymaker said:
But there is one aspect that we tend to forget about and it is the aspect of making noise… You have to keep on being heard so that you even make some of the target audience uncomfortable and just for the purposes of trying to have some peace they have to listen to what you are saying… in the absence of funding we are also trying to make sure that we get heard. (NHP)
While two national policymakers argued for advocacy at the national level, a county health policymaker also emphasised the importance of local campaigns, as politicians want to get re-elected. He went on to explain that the desire for re-election drives the focus on visible, curative health investments but also that there are situations where investment in stimulating community demand for health systems strengthening has altered political priorities at the county level:
That brings me back to what we did in 2014-15, where we mobilized the community… From that engagement, the demand for dispensaries and ambulances reduced versus the demand for support for the CHVs in terms of the stipend, transport and issues on public sanitation. That actually greatly influenced the budgetary allocation. (CHP)
Interviewees explained that politicians’ prioritisation of health issues could also be influenced by new evidence and, for this, data systems that facilitate evidence-based decision making by policymakers were seen as an ‘extremely important’ investment (NHP) with long-term benefits (T). Deworming was cited as an example where evidence of the disease burden influenced policymaker prioritisation:
…findings from different studies and researches that have brought to light that worm infestation in school going children is a big problem and this has enabled action to be taken. (CHP)
Finally, a county education official argued that devolution, whereby local health policymakers assumed greater power, was having a positive impact because local policymakers had experienced health such as deworming first hand.
Discussion
The growing emphasis on country ownership of health programmes to ensure sustainability and reduced aid-dependency is challenging the power and legitimacy of external agencies in influencing priorities for NTD programmes in LMICs. Our case study of STH control in Kenya, conducted at a time when responsibilities for funding and implementation were shifting from external to national and sub-national stakeholders, revealed important differences in opinions about priorities and strategies for control of STH.
Our conceptual framework for understanding sustainability traced a progression in thinking, from ensuring financial stability through the technical ability to adapt to changing circumstances, and ultimately to a situation where it is maintained because empowered communities demand it. The clearly expressed view by most of our interviewees was that they sought to be at the final stage in this progression. Simply maintaining a programme that controls but fails to eradicate an important threat to health was seen as being unambitious and, ultimately, unsustainable, especially when there are grounds for believing that, with sufficient effort, eradication should be possible. This view was widespread even though the eventual eradication of STH could have implications for those engaged in regular treatment cycles. Indeed, there was widespread recognition that this would threaten some vested interests, specifically pharmaceutical manufacturers. Although we could not examine it in detail, it is likely that other vested interests play a part in the institutional fragmentation identified by many interviewees as a barrier to more effective action.
Importantly, the wider social and environmental determinants of health were well recognised by those interviewed. Yet this was not the case in the documentary evidence we reviewed, most of which failed to operationalise sustainability and, where it did, focused on sustaining the current far from adequate model. There was a marked contrast in consideration of broader social determinants of health between government documents and interviewees; the former tended to present to narrower concepts of programmatic sustainability. However, there were some indications of a shift in consideration of sustainability with education ministry led annual evaluations of the deworming programme over time. The first two evaluations note the central role of sustainability as a programme objective across both health and educational sector without providing details on operationalisation[65, 66], while the third year evaluation includes a more detailed framework and a cascade of actions [67].
What is especially notable is how those interviewed were unconvinced by the existing external agency-led preventive chemotherapy strategy for STH control. This is consistent with earlier research reporting differences between international and domestic stakeholders in their motivations for and approaches to improving health [20, 33]. However, the interviewees were influenced not only by the perceived failure of the existing model to work and, especially, to address the underlying causes of ill health. As noted above, the current strategy was also criticised as promoting the financial interests of pharmaceutical companies and their allies in the international policy community above those of the Kenyan people, consistent with ‘development of underdevelopment’ theories [52].
Moving forward, our findings suggest that a domestically led STH control programme could, if free from vested interests (a major assumption that we could not test and which is likely to be challenging), look quite different from what exists currently. It would involve breaking down barriers between institutions, with their different structures and cultures, so that policies would no longer be fragmented in silos. There would be effective community-led demand for and ownership of policies, which would be likely to include preventive chemotherapy and improved sanitation. Importantly, those policy makers at national and county level whom we interviewed saw community demand as important for making things happen, not least because it feeds into the agendas of politicians seeking election. There would also be increased political attention to the underlying socioeconomic and environmental causes of STH. Perhaps most important, these changes were not viewed as independent of each other. Rather, they were viewed as different elements of a co-ordinated approach, in which each area reinforces the others.
These views of Kenyan stakeholders from different sectors and at different administrative levels are consistent with emerging views on strategies required to achieve the Sustainable Development Goals (SDGs). Buse and Hawkes argue that success requires a paradigm shift in addressing key global health challenges, through leadership aimed at intersectoral coherence with coordinated action on the social, economic, political and legal drivers of health, shifting the focus from treatment to prevention through locally-led, politically-tuned approaches to deliver a far broader agenda [71]. And these ideas are not new. The importance of taking a holistic view to infectious disease control policies, and the perils of biomedically framed, disease-specific approaches that neglect socioeconomic determinants of health (often favoured by external agencies), was highlighted Porter et al almost two decades ago [72]. What is new is that the shift in responsibility for health programmes from external agencies to those who live and work in affected countries may, if our findings are borne out in other countries, and if the necessary cultural and organisational changes can be achieved, make this vision possible.
Our findings should be considered in light of several limitations to our research. We studied one Kenyan county, Kwale, identified as an appropriate case-study because of its high STH prevalence and the presence of external agencies focus on STH control programmes in the county. However, the views of the stakeholders interviewed may have been influenced by specific experiences of local STH programmes which may be atypical and further studies in other counties would help to indicate how representative our findings are of subnational stakeholders in Kenya more broadly. We anticipate that those with a stake in policy at community and county levels based in regions where STH is a less salient issue may be less sensitised to issues around MDA and may take different views. We also recognise that the views of stakeholders may have been shaped by their personal experiences, including those with other disease-specific programmes and individual external agencies operating in Kenya rather than linked specifically to STH. Although we were able to interview some of the most senior national policymakers in three sectors, we acknowledge the number of national interviewees was relatively small (five), and that additional interviews with deputies of the senior policymakers we approached in health, education and water and sanitation would have allowed us to be more confident about the consistency of our findings. The scope of this study did not extend to cover a parallel, in-depth investigation of views’ of external agencies operating in Kenya; this would be a useful topic for further research. While our findings are encouraging, suggesting that domestic leadership may be more likely to address the fundamental causes of this problem, we cannot know whether they will succeed in realising their vision in the future. As was noted, there are powerful vested interests with a stake in the status quo, able to exert hidden power. Finally, without further research, our findings cannot necessarily be generalised to other countries in Africa or low income countries elsewhere, where understanding of the problem and systems of accountability may differ.
Conclusion
The most obvious conclusion from our study is one that should not need to be said. Those designing a development programme should speak to those implementing it on the ground and affected by it. We concur with Tesh [51], who has argued that divergent views between international and domestic actors on priorities for investment in health may be driven by differing underlying assumptions about the causes of disease and optimal control measures but differ in that while Tesh considers these beliefs are often subconscious, we found that Kenyan stakeholders had conscious reasons to differ. Our investigation of Kenyan domestic stakeholders’ views revealed that they did not consider sustainability simply in terms of maintaining or integrating into routine operations an external agency-led preventive chemotherapy strategy. Crucially, the domestic views took a broad approach for addressing underlying drivers of STH - which they felt required including changes in institutional structures, policymaking and community - that is consistent with more recent thinking internationally about sustainability. Although such changes are extremely challenges to implement, especially in light of contending vested interests, the shift in responsibility for health programmes from external agencies to those who live and work in affected countries may result in new strategic directions emerging.
Research highlights.
Sustainability was not conceptualised as self-sufficiency to continue a programme
Mass drug administration criticised for neglecting root causes of worm infestation
Kenyan stakeholders linked sustainability to building community demand for health
Community demand was seen as a precursor to increased political attention
As Kenyan stakeholders lead on NTD control, investment strategies may change
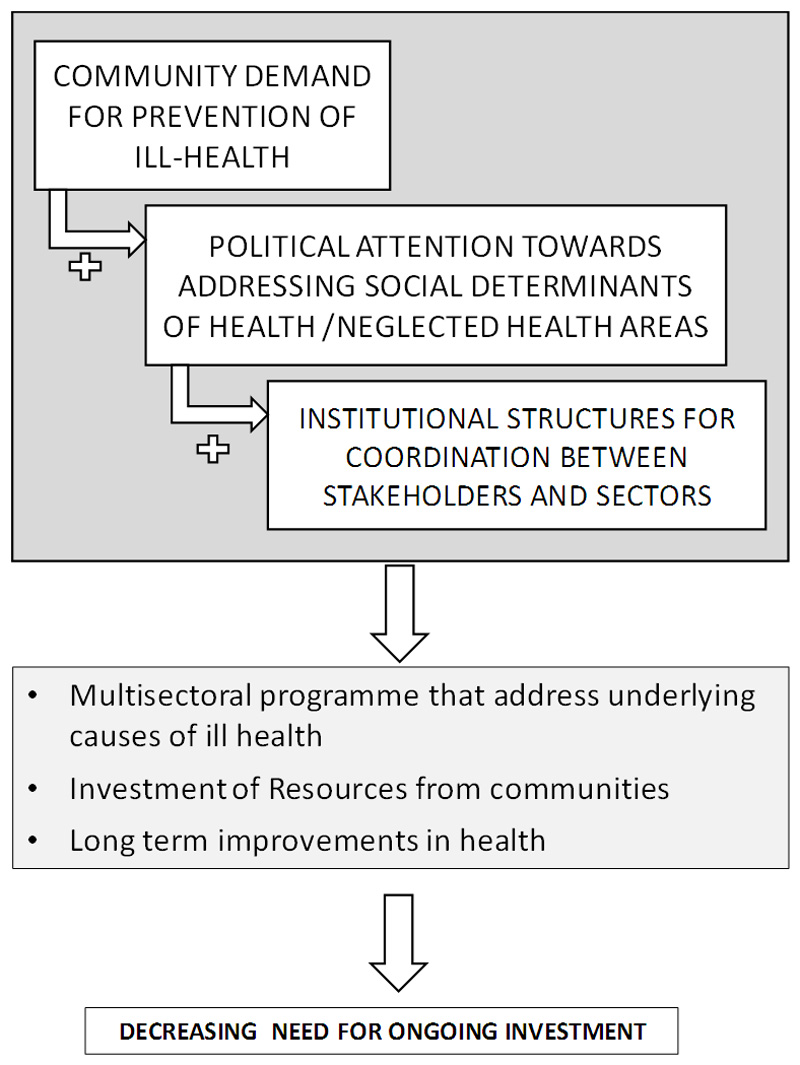
Figure 1. Kenyan stakeholders′ views on how investments can lead to sustained impact on health.
References
- 1.United Nations. [5th March 2018];Sustainable Development Goals. 2018 Available from: http://www.un.org/sustainabledevelopment/sustainable-development-goals/.
- 2.World Health Organization. Accelerating work to overcome the global impact of neglected tropical diseases: a roadmap for implementation: executive summary. 2012 [Google Scholar]
- 3.World Health Organization. Implementing the WHO Roadmap on neglected tropical diseases – partners celebrate five years of collaboration. [4th March 2018]; Available from: http://www.who.int/neglected_diseases/news/WHO_Roadmap_five_years_of_collaboration/en/.
- 4.Uniting to combat Neglected Tropical Diseases. Available from: http://unitingtocombatntds.org/reports/5th-report/.
- 5.Kisoka WJ, et al. community members' perceptions of mass drug administration for control of Lymphatic Filariasis in rural and urban Tanzania. J Biosoc Sci. 2016;48(1):94–112. doi: 10.1017/S0021932015000024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Addiss D. The 6th Meeting of the Global Alliance to Eliminate Lymphatic Filariasis: A half-time review of lymphatic filariasis elimination and its integration with the control of other neglected tropical diseases. Parasit Vectors. 2010;3:100. doi: 10.1186/1756-3305-3-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krentel A, et al. Review of the factors influencing the motivation of community drug distributors towards the control and elimination of neglected tropical diseases (NTDs) PLoS Negl Trop Dis. 2017;11(12):e0006065. doi: 10.1371/journal.pntd.0006065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Humphries D, et al. The promise and pitfalls of mass drug administration to control intestinal helminth infections. Curr Opin Infect Dis. 2012;25(5):584–9. doi: 10.1097/QCO.0b013e328357e4cf. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. 2017. Guideline: preventive chemotherapy to control soil-transmitted helminth infections in at-risk population groups. Available from: http://apps.who.int/iris/bitstream/10665/258983/1/9789241550116-eng.pdf?ua=1. [PubMed] [Google Scholar]
- 10.Anderson RM, et al. How effective is school-based deworming for the community-wide control of soil-transmitted helminths? PLoS Negl Trop Dis. 2013;7(2):e2027. doi: 10.1371/journal.pntd.0002027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anderson R, Truscott J, Hollingsworth TD. The coverage and frequency of mass drug administration required to eliminate persistent transmission of soil-transmitted helminths. Philos Trans R Soc Lond B Biol Sci. 2014;369(1645):20130435. doi: 10.1098/rstb.2013.0435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Truscott JE, et al. Can chemotherapy alone eliminate the transmission of soil transmitted helminths? Parasit Vectors. 2014;7:266. doi: 10.1186/1756-3305-7-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Campbell SJ, et al. Tailoring Water, Sanitation, and Hygiene (WASH) Targets for Soil-Transmitted Helminthiasis and Schistosomiasis Control. Trends Parasitol. 2018;34(1):53–63. doi: 10.1016/j.pt.2017.09.004. [DOI] [PubMed] [Google Scholar]
- 14.Boisson S, et al. Water, sanitation and hygiene for accelerating and sustaining progress on neglected tropical diseases: a new Global Strategy 2015-20. Int Health. 2016;8(Suppl 1):i19–21. doi: 10.1093/inthealth/ihv073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hotez PJ, et al. Rescuing the bottom billion through control of neglected tropical diseases. Lancet. 2009;373(9674):1570–5. doi: 10.1016/S0140-6736(09)60233-6. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization. Neglected Tropical Diseases (132 Session Agenda Item 9.2) 2013 Jan 28th; Available from: http://apps.who.int/gb/ebwha/pdf_files/EB132/B132_R7-en.pdf.
- 17.Ooms G, Hammonds R. Correcting globalisation in health: transnational entitlements versus the ethical imperative of reducing aid-dependency. Public Health Ethics. 2008;1(2):154–170. [Google Scholar]
- 18.Moucheraud C, et al. Sustainability of health information systems: a three-country qualitative study in southern Africa. BMC health services research. 2017;17(1):23. doi: 10.1186/s12913-016-1971-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Askell-Williams H. Perspectives from teachers and school leaders about long-term sustainability: A challenge for mental health promotion initiatives in educational settings. 2017 [Google Scholar]
- 20.Merson MH, Black RE, Mills AJ. Global health. Jones & Bartlett Publishers; 2012. [Google Scholar]
- 21.Katz I, et al. Lessons learned from stakeholder-driven sustainability analysis of six national HIV programmes. Health policy and planning. 2013;29(3):379–387. doi: 10.1093/heapol/czt024. [DOI] [PubMed] [Google Scholar]
- 22.World health Organization. Neglected Tropical Diseases: PCT databank. Available from: http://www.who.int/neglected_diseases/preventive_chemotherapy/sth/en/.
- 23.Mwandawiro CS, et al. Monitoring and evaluating the impact of national school-based deworming in Kenya: study design and baseline results. Parasit Vectors. 2013;6:198. doi: 10.1186/1756-3305-6-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Okoyo C, et al. Monitoring the impact of a national school based deworming programme on soil-transmitted helminths in Kenya: the first three years, 2012 – 2014. Parasites & Vectors. 2016;9:408. doi: 10.1186/s13071-016-1679-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brooker SJ, et al. Interrupting transmission of soil-transmitted helminths: a study protocol for cluster randomised trials evaluating alternative treatment strategies and delivery systems in Kenya. BMJ Open. 2015;5(10):e008950. doi: 10.1136/bmjopen-2015-008950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Global Atlas of Helminth Infections. TUMIKIA Project. Available from: http://www.thiswormyworld.org/tumikia-project.
- 27.Ministry of Health. National Health Accounts 2012/2013. Nairobi: 2015. [Google Scholar]
- 28.Tsofa B, et al. How does decentralisation affect health sector planning and financial management? A case study of early effects of devolution on Kilifi County, Kenya. International Journal for Equity in Health. 2017;16:151. doi: 10.1186/s12939-017-0649-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pfeffer J, Gerald RS. The external control of organizations: A resource dependence perspective. New York: Harper & Row; 1978. [Google Scholar]
- 30.Rauh K. NGOs, foreign donors, and organizational processes: passive NGO recipients or strategic actors? McGill Sociological Review. 2010;1:29. [Google Scholar]
- 31.Oller SD. Power relations in the financial aid chain. Development. 2006;49(2):34–39. [Google Scholar]
- 32.Chambers R, Pettit J. Shifting power to make a difference. Inclusive aid: Changing power and relationships in international development. 2004:137–162. [Google Scholar]
- 33.Khan MS, et al. How do external donors influence national health policy processes? Experiences of domestic policy actors in Cambodia and Pakistan. Health policy and planning. 2017 doi: 10.1093/heapol/czx145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Scholte JA. Towards greater legitimacy in global governance. Review of International Political Economy. 2011;18(1):110–120. [Google Scholar]
- 35.Bernstein S. Legitimacy in intergovernmental and non-state global governance. Review of International Political Economy. 2011;18(1):17–51. [Google Scholar]
- 36.Mügge D. Limits of legitimacy and the primacy of politics in financial governance. Review of International Political Economy. 2011;18(1):52–74. [Google Scholar]
- 37.Lindenberg M, Bryant C. Going global: Transforming relief and development NGOs. Kumarian Press; Bloomfield, CT: 2001. [Google Scholar]
- 38.Allen T, Parker M. Deworming delusions? Mass drug administration in East African schools. Journal of biosocial science. 2016;48(S1):S116–S147. doi: 10.1017/S0021932016000171. [DOI] [PubMed] [Google Scholar]
- 39.Preble C, Tupy ML. Trade, Not Aid. 2005 >Reason Online Available from: https://www.cato.org/publications/commentary/trade-not-aid. [Google Scholar]
- 40.Gruen RL, et al. Sustainability science: an integrated approach for health-programme planning. Lancet. 2008;372(9649):1579–89. doi: 10.1016/S0140-6736(08)61659-1. [DOI] [PubMed] [Google Scholar]
- 41.Shigayeva A, Coker RJ. Communicable disease control programmes and health systems: an analytical approach to sustainability. Health Policy Plan. 2015;30(3):368–85. doi: 10.1093/heapol/czu005. [DOI] [PubMed] [Google Scholar]
- 42.Lee H. Sustainability in International Aid Programs; Identification of Working Concepts of Sustainability and Its Contributing Factors. Int'l J Soc Sci Stud. 2017;5:7. [Google Scholar]
- 43.Bossert TJ. Can they get along without us? Sustainability of donor-supported health projects in Central America and Africa. Soc Sci Med. 1990;30(9):1015–23. doi: 10.1016/0277-9536(90)90148-l. [DOI] [PubMed] [Google Scholar]
- 44.LaFond A. Sustaining primary health care. Earthscan; 1995. [Google Scholar]
- 45.Hanson D, et al. The injury iceberg: an ecological approach to planning sustainable community safety interventions. Health Promotion Journal of Australia. 2005;16(1):5–10. doi: 10.1071/he05005. [DOI] [PubMed] [Google Scholar]
- 46.Bowman CC, et al. Measuring persistence of implementation: QUERI Series. Implementation Science. 2008;3(1):21. doi: 10.1186/1748-5908-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Greenhalgh T, et al. “If we build it will it, stay?” A case study of the sustainability of whole-system change in London. 3. Vol. 90. Milbank Quarterly; 2012. pp. 516–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Johnson K, et al. Building capacity and sustainable prevention innovations: a sustainability planning model. Evaluation and program planning. 2004;27(2):135–149. [Google Scholar]
- 49.Bennett S, et al. Sustainability of donor programs: evaluating and informing the transition of a large HIV prevention program in India to local ownership. Global Health Action. 2011;4 doi: 10.3402/gha.v4i0.7360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nelson DE, et al. Successfully maintaining program funding during trying times: lessons from tobacco control programs in five states. J Public Health Manag Pract. 2007;13(6):612–20. doi: 10.1097/01.PHH.0000296138.48929.45. [DOI] [PubMed] [Google Scholar]
- 51.Tesh SN. Hidden arguments: Political ideology and disease prevention policy. Rutgers University Press; 1988. [Google Scholar]
- 52.Frank AG. The development of underdevelopment. New England Free Press; Boston, MA: 1966. [Google Scholar]
- 53.Ferraro V. Dependency theory: An introduction. The development economics reader. 2008;12(2):58–64. [Google Scholar]
- 54.Owusu F. Pragmatism and the gradual shift from dependency to neoliberalism: The World Bank, African leaders and development policy in Africa. World Development. 2003;31(10):1655–1672. [Google Scholar]
- 55.Harrison G. Neoliberal Africa: The impact of global social engineering. London: Zed Books; 2013. [Google Scholar]
- 56.Okoyo C, et al. Monitoring the impact of a national school based deworming programme on soil-transmitted helminths in Kenya: the first three years, 2012 - 2014. Parasit Vectors. 2016;9(1):408. doi: 10.1186/s13071-016-1679-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Njomo DW, et al. The role of personal opinions and experiences in compliance with mass drug administration for lymphatic filariasis elimination in Kenya. PLoS One. 2012;7(11):e48395. doi: 10.1371/journal.pone.0048395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ministry of Health. The 2nd Kenya National Strategic Plan For control of Neglected Tropical Diseases 2016 – 2020. Revised edition. Nairobi: Ministry of Health; 2017. [Google Scholar]
- 59.Suchdev PS, et al. Soil-transmitted helminth infection and nutritional status among urban slum children in Kenya. Am J Trop Med Hyg. 2014;90(2):299–305. doi: 10.4269/ajtmh.13-0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mwinzi PN, et al. Integrated community-directed intervention for schistosomiasis and soil transmitted helminths in western Kenya - a pilot study. Parasit Vectors. 2012;5:182. doi: 10.1186/1756-3305-5-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Njenga SM, et al. Adult population as potential reservoir of NTD infections in rural villages of Kwale district, Coastal Kenya: implications for preventive chemotherapy interventions policy. Parasit Vectors. 2011;4:175. doi: 10.1186/1756-3305-4-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Freeman MC, et al. Associations between school- and household-level water, sanitation and hygiene conditions and soil-transmitted helminth infection among Kenyan school children. Parasit Vectors. 2015;8:412. doi: 10.1186/s13071-015-1024-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Davis SM, et al. Soil-transmitted helminths in pre-school-aged and school-aged children in an urban slum: a cross-sectional study of prevalence, distribution, and associated exposures. Am J Trop Med Hyg. 2014;91(5):1002–10. doi: 10.4269/ajtmh.14-0060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ministry Of Public Health And Sanitation And Ministry Of Education. National School Health Strategy Implementation Plan 2010-2015 [Google Scholar]
- 65.Ministry of Education, S.a.T., and Ministry of Health. Kenya National School-Based Deworming Programme Year 1 (2012-2013) Results [Google Scholar]
- 66.Ministry of Education, S.a.T., and Ministry of Health. Kenya National School-Based Deworming Programme Year 2 Report (April 2013 - March 2014) [Google Scholar]
- 67.Ministry of Education, S.a.T., and Ministry of Health. Kenya National School-Based Deworming Programme. Year 3 Report (2014 – 2015) [Google Scholar]
- 68.Saldaña J. The coding manual for qualitative researchers. Sage; 2015. [Google Scholar]
- 69.Glaser BG, Strauss AL, Strutzel E. The discovery of grounded theory; strategies for qualitative research. Nursing research. 1968;17(4):364. [Google Scholar]
- 70.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 71.Buse K, Hawkes S. Health in the sustainable development goals: ready for a paradigm shift? Globalization and health. 2015;11(1):13. doi: 10.1186/s12992-015-0098-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Porter J, Ogden J, Pronyk P. Infectious disease policy: towards the production of health. Health Policy and Planning. 1999;14(4):322–328. doi: 10.1093/heapol/14.4.322. [DOI] [PubMed] [Google Scholar]
- 73.Scheirer MA. Is sustainability possible? A review and commentary on empirical studies of program sustainability. American Journal of Evaluation. 2005;26(3):320–347. [Google Scholar]