Although the presence of focal lesions in 18F-fluo-rodeoxygluocse (FDG) positron emission tomography (PET)/computed tomography (CT) is associated with adverse outcome in multiple myeloma, data on diffuse bone marrow infiltration are lacking. In the current prospective study we investigated the prognostic significance of quantitative 18F-FDG PET/CT parameters in patients with multiple myeloma undergoing high-dose chemotherapy followed by autologous stem cell transplantation. We found that the reference bone marrow-derived PET/CT parameters maximum standardized uptake value (SUVmax), fractional blood volume (VB), phosphorylation rate (k3) and influx (Ki) prior to therapy adversely affected the patients’ progression-free survival. These results suggest that, apart from the presence of focal lesions in PET/CT, quantitative 18F-FDG parameters from reference bone marrow can predict survival of patients with multiple myeloma. 18F-FDG PET/CT is a valuable investigation in the initial work-up and response evaluation in multiple myeloma.1–3
The vast majority of PET/CT studies are performed as whole-body scans based on static images acquired 60 min after injection of 18F-FDG. The acquisition of dynamic, quantitative data offers the opportunity to measure 18F-FDG kinetics.4 Our group has previously shown that bone marrow plasma cell infiltration in multiple myeloma correlates with 18F-FDG quantitative parameters.5 In the current study we investigated for the first time the prognostic significance of quantitative parameters derived from dynamic PET/CT in reference bone marrow (from the os ilium) as well as focal lesions in patients with newly diagnosed, symptomatic multiple myeloma.
Forty-eight consecutive patients with previously untreated multiple myeloma were included in this prospective study. Twenty-two patients (45.8%) were enrolled in the prospective GMMG MM5 phase III trial,6 while 26 patients (54.2%) were treated outside the MM5 trial with comparable treatment regimens. All patients underwent autologous stem cell transplantation.
As described previously, PET/CT data acquisition consisted of dynamic acquisition over the lower abdomen and pelvis for 60 min, and whole body, static PET/CT acquisition.5
Qualitative analysis of the PET/CT data led to the identification of four distribution patterns: (i) a negative pattern, without pathological tracer accumulation; (ii) a focal pattern, with focal areas of increased 18F-FDG in lesions; (iii) a diffuse pattern, with intense, diffuse tracer uptake in the bone marrow; and (iv) a mixed pattern, with a combination of diffuse bone marrow uptake and focal lesions.
Semi-quantitative and quantitative evaluation of the PET/CT data was performed in reference bone marrow and the hottest focal lesion in each patient. The semi-quantitative assessment was based on calculation of the SUV according to the formula: SUV = tissue concentration (Bq/mL)/(injected dose (Bq)/body weight (g). The quantitative evaluation of dynamic 18F-FDG PET/CT was based on a two-tissue compartment model, with methods used previously by our group.7–9 The application of this model leads to the extraction of the kinetic parameters K1, k2, k3 and k4 as well as influx (Ki), which describe specific molecular processes: k1 and k2 reflect the carrier-mediated transport of 18F-FDG from plasma to tissue and vice versa, while k3 and k4 represent the phosphorylation and dephosphorylation rates of the radiotracer. Influx (Ki) is derived from the equation = (K1 x k3)/(k2 + k3).7,9
Fluorescence in situ hybridization was performed as described previously.10 Cytogenetic data were available for 41 patients (85%), with high-risk cytogenetic abnormalities being detected in 9/41 patients (22%). The study endpoint was progression-free survival. Details regarding statistical methods are described in the Online Supplement.
Qualitative PET/CT analysis revealed that 12 patients (25%) had no pathological findings (negative pattern), while the remaining 36 patients (75%) had a pathological PET pattern (focal, n=12; diffuse, n=8; mixed, n=16) (Online Supplementary Figure S1). Of the nine patients with high-risk cytogenetic abnormalities, eight (89%) had a pathological PET pattern, while one (11%) was PET-negative. The descriptive statistics of the calculated PET parameters are presented in Online Supplementary Table S1.
Information on progression-free survival was available for 47/48 patients. The median follow-up was 55.6 months (95% confidence interval: 53.2 - 63.8 months). Twenty-nine patients (62%) showed progression and the median progression-free survival was 43.0 months.
First, we aimed to validate established prognostic PET parameters - namely the presence of more than three focal lesions, SUVmax >4.2 and the presence of extramedullary disease.4 We found that these parameters were indeed associated with an adverse progression-free survival in our cohort (Online Supplementary Table S2).
Qualitative, whole-body PET/CT evaluation showed that the median progression-free survival for patients with a pathological 18F-FDG distribution pattern (focal, diffuse, or mixed) was 34.7 months, while that of patients with a physiological 18F-FDG distribution pattern was not reached (P=0.07) (Online Supplementary Figure S2). In detail, the median progression-free survival was 28.6 months for patients with the mixed pattern, 42.0 months for those with the focal pattern, while the median progression-free survival was not reached in patients with the diffuse bone marrow pattern (P=0.05).
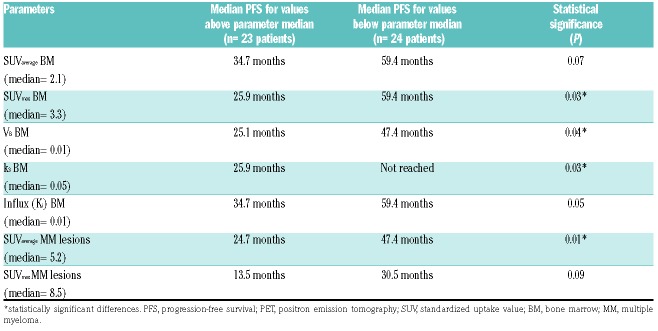
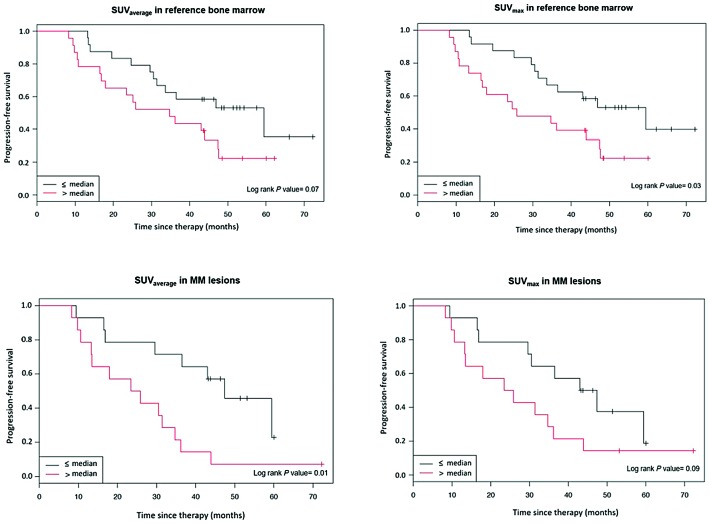
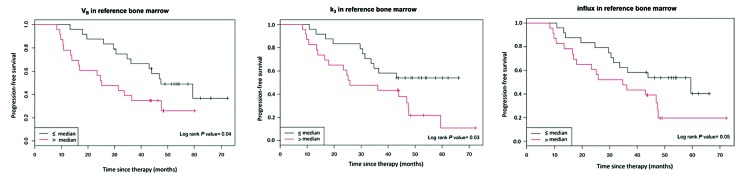
For the survival analyses, semi-quantitative and quantitative PET parameters were dichotomized at the median. According to this dichotomization, survival was shorter in patients with SUVmax, VB, k3 and influx (Ki) values in the bone marrow and SUVaverage in focal lesions above the median compared to those with values below the median (Table 1, Figures 1 and 2). Optimal cutoffs were identified using maximally selected rank statistics: univariate analysis revealed that SUVmax >4.0, VB >0.001, k3 >0.038 and influx (Ki) >0.015 in reference bone marrow as well as SUVmax >6.8 in myeloma lesions, were associated with shorter progression-free survival. Multivariate Cox regression analysis accounting for high-risk cytogenetic abnormalities showed that high SUVmax and VB in bone marrow were associated with shorter progression-free survival (Online Supplementary Table S3).
Table 1.
Relationship of semi-quantitative and quantitative positron emission tomography parameters, dichotomized at their median values, with progression-free survival.
Figure 1.
Progression-free survival according to standardized uptake values from reference bone marrow and multiple myeloma lesions. SUV: standardized uptake value; MM: multiple myeloma.
Figure 2.
Progression-free survival according to quantitative (kinetic) positron emission tomography parameters from reference bone marrow. VB: fractional blood volume; k3: phosphorylation rate.
So far, PET/CT studies have been restricted to either descriptive analyses of infiltration patterns or semi-quantitative analysis of parameters derived from focal lesions. In the current study we investigated the prognostic significance of quantitative parameters derived from dynamic PET/CT of the iliac crest, in an attempt to investigate the impact of diffuse bone marrow infiltration for the first time. We were able to demonstrate that fractional blood volume (VB), phosphorylation rate (k3) and influx rate (Ki) of reference bone marrow, as well as the widely used SUVmax, are associated with adverse outcome after autologous stem cell transplantation. These results are significant, since they are derived from reference bone marrow routinely used for biopsies and aspirates, rather than from focal lesions, as used in previous studies.4,11 We therefore show, for the first time, that apart from lesion-related indices, quantitative bone marrow 18F-FDG parameters predict survival in multiple myeloma.
There are ongoing attempts to objectify PET/CT interpretation as well as treatment response evaluation in MM.12,13 However, the analyses are restricted to descriptive evaluations of 18F-FDG-avid focal lesions and relative tracer uptake in comparison to that in reference organs such as the liver. The widespread application of absolute SUV cutoff values suffers from the variability introduced by the use of different imaging devices, software and measurement methods. Our findings highlight that quantitative methods add significant predictive information for the outcome of patients with multiple myeloma. Quantitative measurements of PET tracer kinetics do not require assumptions regarding relative tracer uptake in comparison to that in other reference organs, thus reducing intra-and inter-observer variability.
Previous findings from our group might explain the biological background of the observed effects, since kinetic parameters (influx, K1) and SUV from reference bone marrow correlated significantly with the degree of bone marrow plasma cell infiltration.5 Furthermore, they are in line with the findings of another study investigating treatment response in patients with multiple myeloma undergoing high-dose chemotherapy and autologous stem cell transplantation. In that study, all patients responded to therapy with at least partial remission and at the same time the bone marrow-derived PET parameters SUV, K1, and influx also decreased significantly, indicating the potential for using quantitative, dynamic PET/CT values to evaluate treatment response.9 Taking the previous results in consideration and given the growing interest in the role of PET/CT for imaging minimal residual disease,13,14 it could be suggested that quantitative, dynamic 18F-FDG PET/CT data might play a future role in defining minimal residual disease negativity. However, the lack of follow-up PET/CT for therapy response evaluation and its possible correlation with baseline PET/CT parameters does not yet allow definitive conclusions to be drawn.
Apart from the dynamic PET/CT studies, we also performed whole-body, static PET/CT imaging and confirmed that patients with the established adverse parameters of more than three focal lesions, SUVmax> 4.2 and extramedullary disease4,15 have shorter progression-free survival. Furthermore, compared to the groups with focal, diffuse or negative tracer uptake patterns, patients with a combination of focal and diffuse uptake had the shortest progression-free survival, which is in agreement with a previous finding that patients with a mixed 18F-FDG uptake pattern had the highest degree of bone marrow plasma cell infiltration.5
The major limitation of this work is the relatively small number of patients studied. This can be, however, justified, given the longer acquisition time of dynamic PET scanning, which is a necessity if real quantitative/kinetic data are to be acquired. Other limitations include the fact that dynamic sequences were performed only in the lower abdomen and pelvis, and the lack of histological confirmation of the 18F-FDG-avid focal lesions. The advent of new PET/CT scanners will facilitate the use of dynamic PET protocols and reduce acquisition times. Furthermore, we will perform image-guided biopsies in the future to molecularly characterize PET-positive focal lesions.
Taken together there are three major findings from our study. First, we confirm the prognostic significance of previously established PET risk factors. Second, we demonstrate that the application of dynamic PET/CT is feasible and identifies patients with adverse outcome after autologous stem cell transplantation. Lastly, we show for the first time that not only quantitative parameters from focal lesions, but also those from reference bone marrow samples are associated with adverse outcome in multiple myeloma.
Footnotes
Information on authorship, contributions, and financial & other disclosures was provided by the authors and is available with the online version of this article at www.haematologica.org.
References
- 1.Cavo M, Terpos E, Nanni C, et al. Role of 18F-FDG PET/CT in the diagnosis and management of multiple myeloma and other plasma cell disorders: a consensus statement by the International Myeloma Working Group. Lancet Oncol. 2017;18(4):e206–e217. [DOI] [PubMed] [Google Scholar]
- 2.Bartel TB, Haessler J, Brown TL, et al. F18-fluorodeoxyglucose positron emission tomography in the context of other imaging techniques and prognostic factors in multiple myeloma. Blood. 2009;114(10):2068–2076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zamagni E, Patriarca F, Nanni C, et al. Prognostic relevance of 18-F FDG PET/CT in newly diagnosed multiple myeloma patients treated with up-front autologous transplantation. Blood. 2011;118(23):5989–5995. [DOI] [PubMed] [Google Scholar]
- 4.Phelps ME, Huang SC, Hoffman EJ, et al. Tomographic measurement of local cerebral glucose metabolic rate in humans with (F-18)2-fluo-ro-2-deoxy-D-glucose: validation of method. Ann Neurol. 1979;6(5):371–388. [DOI] [PubMed] [Google Scholar]
- 5.Sachpekidis C, Mai EK, Goldschmidt H, et al. 18F-FDG dynamic PET/CT in patients with multiple myeloma: patterns of tracer uptake and correlation with bone marrow plasma cell infiltration rate. Clin Nucl Med. 2015;40(6):e300–307. [DOI] [PubMed] [Google Scholar]
- 6.Goldschmidt H, Mai EK, Dürig J, et al. Response-adapted lenalido-mide maintenance in newly diagnosed, transplant-eligible multiple myeloma: results from the multicenter phase III GMMG-MM5 trial. Blood. 2017; 130(Suppl 1):400. [Google Scholar]
- 7.Sokoloff L, Smith CB. Basic principles underlying radioisotopic methods for assay of biochemical processes in vivo. In: Greitz T, Ingvar DH, Widén L, editors. The Metabolism of the Human Brain Studied with Positron Emission Tomography. New York: Raven Press; 1983;p.123–148. [Google Scholar]
- 8.Pan L, Cheng C, Haberkorn U, Dimitrakopoulou-Strauss A. Machine learning-based kinetic modeling: a robust and reproducible solution for quantitative analysis of dynamic PET data. Phys Med Biol. 2017; 62(9):3566–3581. [DOI] [PubMed] [Google Scholar]
- 9.Sachpekidis C, Hillengass J, Goldschmidt H, et al. Treatment response evaluation with 18F-FDG PET/CT and 18F-NaF PET/CT in multiple myeloma patients undergoing high-dose chemotherapy and autologous stem cell transplantation. Eur J Nucl Med Mol Imaging. 2017;44(1):50–62. [DOI] [PubMed] [Google Scholar]
- 10.Neben K, Lokhorst HM, Jauch A, et al. Administration of bortezomib before and after autologous stem cell transplantation improves outcome in multiple myeloma patients with deletion 17p. Blood. 2012; 119(4):940–948. [DOI] [PubMed] [Google Scholar]
- 11.Haznedar R, Akı SZ, Akdemir OU, et al. Value of 18F-fluo-rodeoxyglucose uptake in positron emission tomography/computed tomography in predicting survival in multiple myeloma. Eur J Nucl Med Mol Imaging. 2011;38(6):1046–1053. [DOI] [PubMed] [Google Scholar]
- 12.Nanni C, Versari A, Chauvie S, et al. Interpretation criteria for FDG PET/CT in multiple myeloma (IMPeTUs): final results. IMPeTUs (Italian myeloma criteria for PET USe). Eur J Nucl Med Mol Imaging. 2018;45(5):712–719. [DOI] [PubMed] [Google Scholar]
- 13.Zamagni E, Nanni C, Dozza L, et al. Standardization of 18F-FDG PET/CT according to Deauville criteria for MRD evaluation in newly diagnosed transplant eligible multiple myeloma patients: joined analysis of two prospective randomized phase III trials. Blood 2018. 132:257 (Suppl 1). Accessed December 28 2018 Retrieved from http://www.bloodjournal.org/content/132/Suppl_1/257. [Google Scholar]
- 14.Zamagni E, Tacchetti P, Terragna C, Cavo M. Multiple myeloma: disease response assessment. Expert Rev Hematol. 2016;9(9):831–837. [DOI] [PubMed] [Google Scholar]
- 15.Tirumani SH, Sakellis C, Jacene H, et al. Role of FDG-PET/CT in extramedullary multiple myeloma: correlation of FDG-PET/CT findings with clinical outcome. Clin Nucl Med. 2016;41(1):e7–13. [DOI] [PubMed] [Google Scholar]