Abstract
Background and Objectives:
Although primary care clinicians provide >60% of U.S. asthma care, no nationally representative study has examined variation in adherence among primary care groups to four cornerstone domains of the Expert Panel Report-3 asthma guidelines: assessment/monitoring, patient education, environmental assessment, and medications. We used the 2012 National Asthma Survey of Physicians: National Ambulatory Medical Care Survey to compare adherence by family/general medicine practitioners (FM/GM), internists, pediatricians and Community Health Center mid-level clinicians (CHC).
Methods:
Adherence was self-reported (n=1,355 clinicians). Adjusted odds of almost always adhering to each recommendation (≥75% of the time) were estimated controlling for clinician/practice characteristics, and agreement and self-efficacy with guideline recommendations.
Results:
A higher percentage of pediatricians adhered to most assessment/monitoring recommendations compared to FM/GM and other groups (e.g., 71.6% [SE 4.0] almost always assessed daytime symptoms versus 50.6% [SE 5.1]-51.1% [SE 5.8], t-test P<.05) but low percentages from all groups almost always performed spirometry (6.8% [SE 2.0]-16.8% [SE 4.7]). Pediatricians were more likely to provide asthma action/treatment plans than FM/GM and internists. Internists were more likely to assess school/work triggers than pediatricians and CHC (environmental assessment). All groups prescribed inhaled corticosteroids for daily control (84.0% [SE 3.7]-90.7% [SE 2.5]) (medications). In adjusted analyses, pediatric specialty, high self-efficacy and frequent specialist referral were associated with high adherence.
Conclusions:
Pediatricians were more likely to report high adherence than other clinicians. Self-efficacy and frequent referral were also associated with adherence. Adherence was higher for history-taking recommendations and lower for recommendations involving patient education, equipment and expertise.
Introduction
Primary care clinicians are the front-line providers for US asthma patients. Of the approximately 15 million non-emergent ambulatory asthma visits made annually, over 60% occur in primary care settings.1,2 The Expert Panel Report-3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma3 highlighted four evidence-based cornerstone components of asthma care: assessment/monitoring, patient education, control of environmental factors and pharmacologic treatment. Efforts to increase guideline implementation have ranged from public education campaigns4 to a guideline implementation report.5 Despite multifaceted efforts, clinician adherence to guideline recommendations has been low for many reasons (e.g., lack of self-efficacy and/or agreement with guidelines, guideline complexity, patient characteristics, organization barriers, reimbursement, and burnout).6–20 However, no previous study has compared similarities and differences in adherence between primary care groups for the four major components of the guidelines. A review found that a minority of studies involved pediatric health care providers and called for studies applicable across the health care provider spectrum.21 Understanding the variation and similarities in practice between guideline components and differential uptake between primary care provider groups can inform future interventions to increase implementation.
The 2012 National Asthma Survey of Physicians (NAS): National Ambulatory Medical Care Survey (NAMCS), a one-time provider questionnaire supplement to the National Center for Health Statistics’s (NCHS) NAMCS, was designed to assess clinician agreement, self-efficacy (belief in one’s own ability to execute specific tasks to achieve performance goals) and adherence with EPR-3 recommendations among a nationally representative sample of clinicians. NAS data were released in 2017. A previous analysis of the NAS assessed differences in guideline adherence between primary care clinicians and asthma specialists.22 This study focuses on assessing and comparing adherence to the four cornerstone components of the guidelines among 4 major primary care clinician groups: family/general medicine (FM/GM), internal medicine (IM), pediatrics, and Community Health Center (CHC) mid-level clinicians. We hypothesized that guideline adherence differed among primary care clinician groups and was associated with differences in clinician agreement with guideline recommendations and self-efficacy with performing guideline-based care.7,8,14
Methods
Data Source and Study Population
The annually-conducted NAMCS 23 provides nationally representative data about patient visit and provider characteristics and includes two sampling frames. The office-based frame includes non-federally employed physicians engaged in office-based patient care per the American Medical Association or the American Osteopathic Association. The Community Health Centers (CHC) frame includes physicians and mid-level practitioners (i.e., physician assistants, nurse practitioners, and nurse midwives) from sampled CHCs. The 2012 NAS was a one-time clinician questionnaire supplement to NAMCS and included clinicians in both NAMCS frames who responded affirmatively to: “Do you treat patients with asthma?”23,24 The NCHS Institutional Review Board approved the NAS and informed consent was obtained from participating clinicians.
The unweighted and weighted NAS response rates were 38% and 28%, respectively, similar to or higher than other national physician surveys.25 Demographic information included clinician age and sex. Clinician race/ethnicity and board certification were not available. Practice characteristics included census region, urbanization level, ownership, age of patient population, and asthma patient volume. Of the 1,726 respondents, 304 specialists were excluded as well as 67 primary care clinicians with missing information and those with non-clinical roles (4.7% of primary care respondents). The final sample size was 1,355.
Guideline adherence, agreement and self-efficacy
Guideline recommendations were categorized into four components: assessment/monitoring, patient education, control of environmental factors, and pharmacologic treatment (see Supplemental Table E1). Self-reported adherence was evaluated by the percentage of asthma visits in which each recommendation was followed (“almost always”, ≥75%; “often”, 25–74%; “sometimes”, 1–24%; “never”, 0%). The “sometimes” and “never” categories were combined due to low response frequencies. Clinicians were also asked about the frequency of patient concerns and confusion about medications. The results were dichotomized to “almost always/often” versus “sometimes/never” due to low frequencies of “almost always” responses. While these outcomes are not guideline recommendations, responses can be considered an indicator of perceived need for patient education.
To assess how adherence was associated with guideline agreement and self-efficacy, we constructed two dichotomous index variables (see Supplemental Table E2). The survey included five questions each on agreement and self-efficacy. In general, for each of the questions, nearly or more than half of clinicians either strongly agreed with the guideline recommendation (with the exception of provision of asthma action plans for which 31% strongly agreed) or reported that they were very confident at performing the recommendation (with the exception of using spirometry of which 37% reported being very confident). To construct an index that could meaningfully discern agreement or self-efficacy, we dichotomized between the top category and others. The agreement index variable was categorized as a clinician response of “strongly agree” versus all other responses (“agree,” “neutral,” “disagree” and “strongly disagree”) to all five questions about guideline agreement. Similarly, the self-efficacy index variable was defined as “very confident” versus all other responses (“somewhat confident,” “not at all confident” and “NA/do not perform”) to all five self-efficacy questions.
Statistical Analysis
National estimates were calculated using NAS sample weights that accounted for the probability of selection and non-response. Standard error (SE) estimation accounted for the complex survey design. Analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC) and SUDAAN 11.0 (Research Triangle Institute). A relative standard error >30% (SE/estimate) indicates low precision. Differences between primary care clinician groups across response categories were assessed using chi-square tests. When chi-square testing indicated statistically significant differences across groups, t-tests were performed to test pairwise differences in the proportion reporting high adherence (“almost always” performing a recommendation), and in the reported use of a medication for a specific indication.
A separate logistic regression model was used for each recommendation to examine associations with guideline adherence. Outcome variables (adherence to each given recommendation) were dichotomized to “almost always” versus all other responses. Records with missing responses for the outcome (0.01%−2.0%) were excluded from each model. 26 Multivariable models were constructed a priori and included the two index variables for agreement and self-efficacy. As a sensitivity analysis, agreement for individual guideline items was assessed in logistic regression analysis when the agreement question matched the guideline recommendation (spirometry and AAP provision). Additional covariates included clinician group, clinician age group (<40, 40–59, 60+ years), clinician sex, practice region (Northeast, Midwest, South, West), urbanicity (large metro, medium/small metro, non-metro), and referral frequency to asthma specialists (almost always versus often/sometimes/never). While recommendations about specialist referral are included in the EPR-3 guidelines, it is one of many topics outside of the four cornerstones of management. We considered referral behavior as a proxy measure for clinician decision-making and patient population characteristics for which no data were available. A previous analysis of primary care providers showed that low rates of allergy testing referral were correlated with factors that indicate lack of familiarity with asthma or with the guidelines (low outpatient asthma volume, being a resident in training, low familiarity with specific guideline components).8 Another past study showed that perceived indications for specialty referral did not align with guideline-recommended reasons for specialist referral, and that referral decisions (higher referral among family practice physicians) and clinical practice (higher likelihood of diagnostic testing by family practice physicians) differed between primary care groups.9 In a sensitivity analysis, responses to questions about patient concerns and confusion were included in the regression model for AAP provision. Average weekly asthma patient volume (2.5% missing) was excluded from final models due to lack of statistical significance and lack of confounding.
Results
Participant and practice characteristics are shown in Table 1. Compared to physicians, CHC mid-level practitioners were younger, more likely to be female, and to practice in non-metropolitan areas. Overall, there was low prevalence of strong agreement with the guidelines (11.6%) which was driven by low levels of strong agreement that asthma action plans are effective (29.6%) and that spirometry is essential for diagnosis (35.4%) versus higher prevalence of strong agreement about efficacy of ICS (48.1%), the need for 6-month follow up visits (48.5%) and the need to assess severity to determine initial treatment (50.1%) (Table E3). Pediatricians were more likely to report higher asthma patient volume. Referral frequency was similar between groups. However, agreement and self-efficacy with guideline recommendations differed between primary care groups. Lower percentages of FM/GM expressed strong overall agreement with the guidelines (7.7%) compared to internists and CHC mild-level providers (16.4% and 17.4%, respectively). FM/GM and internists were more likely to report high self-efficacy with guideline recommendations (20.0% and 35.8%, respectively) compared to 12.6% of pediatricians and 8.7% of CHC mid-level providers. These differences stemmed from lower percentages of clinicians with high self-efficacy with spirometry among pediatricians (20.3%) and CHC mid-level providers (21.2%) versus 42.0% FM/GM and 51.8% internists (Table E3).
Table 1:
Characteristics of Primary Care Clinicians, 2012 National Asthma Survey of Physicians (weighted %, SE)
| n | Total | Family/General Medicine (n=524) |
Internal Medicine (n=196) |
Pediatrics (n=302) |
CHC Mid- level Clinicians (n=333) |
Chi- square p- value |
|
|---|---|---|---|---|---|---|---|
| Total | 1355 | 100 (0.0) | 40.4 (2.2) | 26.0 (2.4) | 24.6 (1.9) | 9.0 (0.6) | |
| Provider age (years)a | |||||||
| <40 | 334 | 16.2 (1.5) | 14.4 (2.3) | 7.6 (2.9)† | 18.1 (3.2) | 44.2 (5.0) | <.001 |
| 40–59 | 748 | 59.9 (2.3) | 57.2 (3.5) | 69.6 (5.3) | 60.5 (4.2) | 42.7 (4.4) | |
| 60+ | 273 | 23.9 (2.1) | 28.5 (3.3) | 22.8 (4.8) | 21.4 (3.6) | 13.1 (2.7) | |
| Provider sexa,b | |||||||
| Female | 700 | 41.8 (2.2) | 35.4 (3.4) | 28.4 (4.6) | 51.6 (4.2) | 83.5 (2.8) | <.001 |
| Male | 655 | 58.2 (2.2) | 64.6 (3.4) | 71.6 (4.6) | 48.4 (4.2) | 16.5 (2.8) | |
| Census region | |||||||
| Northeast | 192 | 20.0 (1.0) | 16.4 (2.6) | 23.0 (4.1) | 24.1 (2.8) | 16.3 (2.7) | .110 |
| Midwest | 338 | 19.9 (0.8) | 25.1 (2.2) | 15.9 (3.2) | 15.9 (2.1) | 18.9 (2.4) | |
| South | 463 | 30.2 (1.0) | 27.3 (2.4) | 30.7 (4.3) | 36.2 (3.5) | 25.2 (2.6) | |
| West | 362 | 29.9 (1.1) | 31.2 (2.9) | 30.4 (5.4) | 23.8 (3.8) | 39.6 (3.7) | |
| Level of urbanizationa,c | |||||||
| Large Metro | 562 | 56.2 (2.1) | 49.3 (3.2) | 68.9 (4.8) | 61.0 (4.1) | 39.4 (5.1) | <.001 |
| Medium/Small Metro | 443 | 29.0 (2.0) | 30.6 (2.9) | 22.8 (4.5) | 29.9 (3.9) | 34.3 (5.2) | |
| Non-metro | 350 | 14.8 (1.2) | 20.1 (2.4) | 8.3 (2.1) | 9.2 (2.0) | 26.3 (3.7) | |
| Asthma patient volumed (#/week) | |||||||
| <3 | 267 | 20.7 (2.0) | 22.4 (2.9) | 31.7 (5.5) | 7.8 (1.7) | 16.5 (3.1) | <.001 |
| 3–12 | 740 | 48.3 (2.2) | 52.3 (3.6) | 41.8 (5.1) | 48.0 (4.2) | 49.9 (4.3) | |
| 13+ | 241 | 19.3 (1.9) | 14.9 (2.6) | 10.4 (3.5)† | 34.7 (4.3) | 22.9 (4.6) | |
| missing | 107 | 11.7 (1.8) | 10.5 (2.6) | 16.1 (5.0)† | 9.6 (3.0)† | 10.7 (3.6)† | |
| Referral frequency to specialist | |||||||
| Always (>75% of time) | 90 | 8.0 (1.4) | 6.1 (1.6) | 12.1 (4.1)† | 7.5 (2.5)† | 6.3 (2.2)† | .370 |
| Often (25-<75% of time) | 387 | 29.5 (2.1) | 25.9 (3.0) | 30.0 (5.3) | 34.1 (4.0) | 31.5 (4.6) | |
| Sometimes/never (<25%) | 878 | 62.5 (2.3) | 68.0 (3.2) | 57.9 (5.7) | 58.4 (4.2) | 62.2 (4.8) | |
| Agreement indexe | |||||||
| Strongly agree | 179 | 11.6 (1.4) | 7.7 (1.4) | 16.4 (3.8) | 10.8 (2.7) | 17.4 (3.8) | .050 |
| All other responses | 1176 | 88.4 (1.6) | 92.3 (1.4) | 83.6 (3.8) | 89.2 (2.7) | 82.6 (3.8) | |
| Self-efficacy indexc,f | |||||||
| Very confident | 261 | 21.3 (2.2) | 20.0 (2.8) | 35.8 (5.8) | 12.6 (2.5) | 8.7 (2.3) | <.001 |
| All other responses | 1094 | 78.7 (2.2) | 80.0 (2.8) | 64.2 (5.8) | 87.4 (2.5) | 91.3 (2.3) | |
Relative standard error >30%
Notes: CHC: Community Health Center; SE: standard error
Source: National Center for Health Statistics, 2012 National Asthma Survey of Physicians: National Ambulatory Medical Care Survey
CHC significantly different than all other categories, t-test P<.05
Pediatrics significantly different than all other categories, t-test P<.05
FM/GM significantly different than all other categories, t-test P<.05
Pediatrics significantly different than FM/GM, internists, t-test P<.05
FM/GM significantly different than internists, CHC, t-test P<.05
Internists significantly different than all other categories, t-test P<.05
Guideline component 1: assessing/monitoring
Adherence to assessment/monitoring recommendations differed between primary care groups (Table 2). Pediatricians were generally more likely to report almost always asking about individual components of asthma control compared to each of the other primary care groups, including the ability to engage in normal activities, daytime symptoms and nighttime symptoms (63.1%−71.6% of pediatricians versus 42.6%−51.1% of other clinician groups). High adherence was lower among CHC midlevel providers compared to other groups for asking about patient perception of control. Low percentages of all primary care groups reported use of a control assessment tool (6.4%−20.6%). Pediatricians were more likely than FM/GM and internists to almost always ask about rescue inhaler use frequency. For the two recommendations involving assessing risk frequency, pediatricians reported higher rates of “almost always” asking about oral steroid use frequency and ED visit frequency than FM/GM and CHC midlevel providers. For recommendations involving objective assessment and monitoring, only 5.7% to 12.2% of clinicians reported almost always asking about peak flow results, and only 6.8% to 16.8% reported almost always performing spirometry in patients who were able to perform this test. More than half of clinicians almost always assessed daily controller use among patients with persistent asthma, but adherence with inhaler technique assessment ranged between 13.6% (FM/GM, internists) and 23.0% (pediatricians).
Table 2:
Percent of primary care clinicians reporting assessing/monitoring asthma severity & control: Guideline component 1
| Family/General Medicine | Internal Medicine | Pediatrics | CHC Mid-level Clinicians | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Almost always |
Often | Someti mes/ Never |
Almost always |
Often | Someti mes /Never |
Almost always |
Often | Someti mes/ Never |
Almost always |
Often | Someti mes/ Never |
Chi- square p-value |
|
| Assessment of impairment frequency, weighted % (SE) | ||||||||||||||
| Document asthma control | 1276 | 31.7 (3.5) | 43.1 (3.5) | 25.2 (3.3) | 27.1 (4.7) | 50.4 (5.9) | 22.5 (5.2) | 37.2 (4.2) | 43.8 (4.4) | 19.0 (3.6) | 34.5 (5.1) | 36.9 (4.8) | 28.5 (4.3) | 0.47 |
| Ask about ability engage in normal activities | 1343 | 42.6 (3.5) | 42.2 (3.5) | 15.2 (2.8) | 43.2 (5.8) | 44.4 (5.6) | 12.4 (3.2) | 63.1a (4.1) | 29.5 (3.9) | 7.4 (1.8) | 43.5 (4.7) | 36.6 (4.5) | 19.9 (4.1) | 0.006 |
| Ask about frequency of daytime symptoms | 1348 | 50.6 (3.4) | 42.9 (3.6) | 6.5 (1.9) | 51.1 (5.8) | 38.9 (5.6) | 10.1 (3.0) | 71.6a (4.0) | 23.0 (3.7) | 5.4† (2.2) | 50.6 (5.1) | 36.0 (4.5) | 13.4 (3.6) | 0.004 |
| Ask about frequency of nighttime awakening | 1346 | 47.8 (3.6) | 36.6 (3.5) | 15.7 (2.8) | 47.2 (5.8) | 31.0 (5.0) | 21.9 (4.8) | 70.0a (4.0) | 25.7 (3.9) | 4.3 (1.4) | 49.6 (4.8) | 32.7 (4.5) | 17.7 (3.8) | <0.001 |
| Ask about perception of control | 1344 | 54.4 (3.6) | 31.8 (3.2) | 13.8 (2.9) | 43.9 (5.7) | 42.2 (5.6) | 14.0 (4.1) | 55.8 (4.3) | 23.7 (3.2) | 20.5 (3.8) | 33.9b (4.5) | 42.2 (4.5) | 23.9 (4.2) | 0.016 |
| Use control assessment tool | 1344 | 12.1 (2.4) | 13.3 (2.5) | 74.5 (3.2) | 6.4† (2.1) | 20.6 (5.0) | 73.0 (5.2) | 20.6a (3.5) | 18.1 (3.3) | 61.3 (4.2) | 13.0 (3.9) | 13.0 (2.9) | 74.0 (4.4) | 0.021 |
| Ask about frequency rescue inhaler | 1347 | 69.8 (3.4) | 28.0 (3.4) | 2.2† (1.0) | 67.4 (5.1) | 23.0 (4.3) | 9.6† (3.5) | 81.4c (3.1) | 18.0 (3.1) | 0.7† (0.4) | 71.5 (4.5) | 21.9 (3.8) | 6.6† (3.2) | 0.011 |
| Assessment of risk frequency, weighted % (SE) | ||||||||||||||
| Ask about oral steroid frequency | 1347 | 49.1 (3.6) | 35.7 (3.4) | 15.3 (2.9) | 52.2 (5.7) | 36.6 (5.2) | 11.2† (3.6) | 65.9d (4.2) | 28.2 (3.9) | 6.0† (2.3) | 38.4 (4.7) | 39.3 (4.7) | 22.3 (4.3) | 0.010 |
| Ask about ED visit frequency | 1348 | 50.2 (3.6) | 29.0 (3.1) | 20.8 (3.3) | 57.8 (5.4) | 33.7 (5.0) | 8.5† (2.8) | 65.4d (4.2) | 27.2 (3.9) | 7.4† (2.7) | 47.4 (4.9) | 30.5 (4.1) | 22.1 (4.5) | 0.004 |
| Objective assessment and monitoring, weighted % (SE) | ||||||||||||||
| Ask about peak flow results | 1346 | 8.6 (1.9) | 27.5 (3.2) | 64.0 (3.4) | 10.4† (3.4) | 30.7 (5.4) | 58.9 (5.7) | 12.2 (2.6) | 13.6 (2.4) | 74.2 (3.3) | 5.7† (2.3) | 10.7 (2.8) | 83.6 (3.5) | 0.002 |
| Perform spirometry | 1330 | 6.8 (2.0) | 25.4 (2.8) | 67.8 (3.2) | 16.8 (4.7) | 30.8 (5.2) | 52.4 (5.7) | 10.0 (2.2) | 20.6 (3.5) | 69.4 (3.9) | 8.1† (2.5) | 16.3 (3.2) | 75.5 (3.8) | 0.025 |
| Ongoing monitoring frequency, weighted % (SE) | ||||||||||||||
| Assess daily controller use persistent asthma | 1348 | 60.1 (3.5) | 33.3 (3.4) | 6.6 (1.6) | 56.8 (5.6) | 29.2 (4.9) | 14.0† (4.2) | 61.3 (4.4) | 34.3 (4.3) | 4.5† (1.8) | 59.8 (4.9) | 29.0 (4.1) | 11.2† (3.5) | 0.25 |
| Repeated assessment of inhaler technique | 1349 | 13.6 (2.5) | 36.2 (3.5) | 50.3 (3.6) | 13.6 (3.5) | 41.2 (5.7) | 45.2 (5.5) | 23.0e (3.4) | 41.4 (4.3) | 35.6 (4.1) | 17.2 (4.6) | 36.5 (4.8) | 46.3 (5.2) | 0.18 |
Relative standard error >30%
Significantly higher compared to other clinician groups (t-test p-value <.05)
Significantly lower compared to FM/GM and pediatrics (t-test p-value<.05)
Significantly higher compared to FM/GM and internists (t-test p-value <.05)
Significantly higher compared to FM/GM and CHC (t-test p-value <.05)
Significantly higher compared to FM/GM (t-test p-value <.05)
Notes: Adherence categories: Almost always (≥75% of the time), Often (25-<75%), Sometimes (1–24%), Never (0%); CHC: Community Health Center; ED: emergency department; SE: standard error
Source: National Center for Health Statistics, 2012 National Asthma Survey of Physicians: National Ambulatory Medical Care Survey
Adjusted odds ratios (AORs) of almost always adhering to these 13 assessment/monitoring recommendations are shown in Figure 1 for primary care group, frequency of patient referral to asthma specialists, guideline agreement, and self-efficacy (see Table E4 for additional covariates). Solid symbols denote AORs with 95% confidence intervals that exclude 1.0. Pediatricians’ higher reported adherence was still apparent after controlling for covariates (first vertical panel). Clinicians who reported almost always referring asthma patients for specialty care had higher odds of high adherence to several recommendations (second panel). Strong agreement with guideline recommendations was significantly associated with high adherence only to asking about rescue medication use frequency (third panel). In a sensitivity analysis of spirometry performance, strong agreement with spirometry recommendations in particular was analyzed in place of the overall agreement index and was found to be associated with high adherence to spirometry (AOR 3.6, 95%CI 1.6, 7.8) while results for the remaining covariates did not vary significantly from the main model (data not shown). High self-efficacy was associated with higher odds of high adherence to all 13 recommendations (fourth panel). In general, clinician age group, sex, and practice location were not associated with higher guideline adherence (Table E4).
Figure 1.
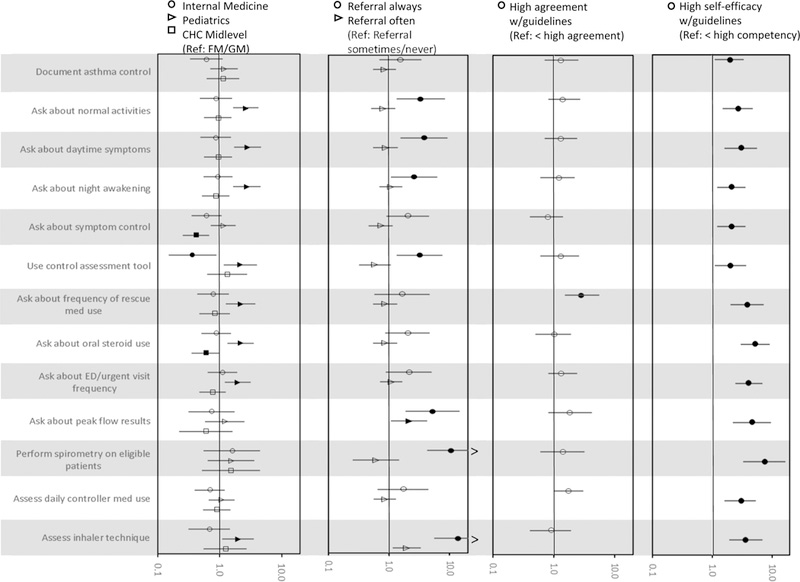
Adjusted OR, 95%CI of “almost always” adhering to assessment and monitoring recommendations, Guideline component 1
Notes: Solid symbols denote AOR with 95% confidence interval excluding 1.0. AORs are on the logarithmic scale with a, maximum value of 20. Confidence intervals ending with an open arrow denote confidence limits that exceed the scale, Source: 2012 National Asthma Survey of Physicians: National Ambulatory Medical Care Survey
Guideline component 2: Patient education
Higher percentages of pediatricians reported almost always providing an AAP, (26.8%, SE 3.6) compared to FM/GM (11.9%, SE 2.4) and internists (10.1%, SE 3.2). CHC mid-level clinicians had adherence similar to pediatricians, (20.3%, SE 4.3) but a pairwise comparison was not significant (data not shown). Pediatrics, frequent specialist referral and high self-efficacy, but not strong agreement, were associated with higher adjusted odds of almost always providing an AAP (Figure 2 top panel). In a sensitivity analysis, we replaced the overall agreement index in the model with strong agreement with AAP recommendations, and found an association with high adherence to AAP provision (AOR 2.8, 95% CI 1.6, 4.8). The results for the remaining covariates did not vary significantly from the main model (data not shown).
Figure 2.
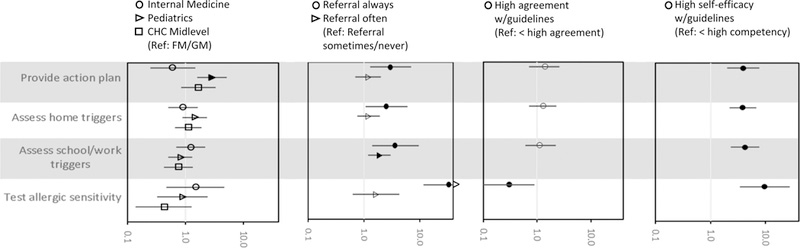
Adjusted odds of reported adherence to 4 guideline recommendations for environmental assessment, by specialist referral frequency, perceived, competency with guidelines, agreement with guidelines and primary care specialty, National Asthma Survey of Physicians
Notes: Solid symbols denote AORs with 95% confidence interval excluding 1.0. The AORs are on the logarithmic scale with a maximum value, of 40. Confidence intervals with open an arrow denote confidence limits that exceed the scale.
See Table E5 for results for additional covariates.
Source: 2012 National Asthma Survey of Physicians: National Ambulatory Medical Care Survey
Clinicians in all groups reported encountering patient misunderstanding, concerns, and confusion (Figure 3). There was group variation, however, with responses ranging from about 35% reporting misunderstanding “almost always” or “often” (FM/GM and IM) to ~50% (pediatricians and CHC mid-level clinicians). Pediatricians more often reported patient/parental concern about long-term side effects of ICS compared to FM/GM or internists. More than half of FM/GM (60.5%), pediatricians (69.0%), and CHC mid-level providers (80.2%) reported that patients/parents were “often” or “almost always” confused about differences between rescue and control medications. In an additional sensitivity analysis, responses of patient medication concerns and confusion were included as covariates in the AAP provision logistic regression model. Only almost always/often encountering patient confusion between relief and controller medications approached a significant association with high adherence with AAP provision (AOR 1.8, 95% CI, 1.0, 3.2) and results for remaining covariates remained similar to those from the main model (data not shown).
Figure 3.
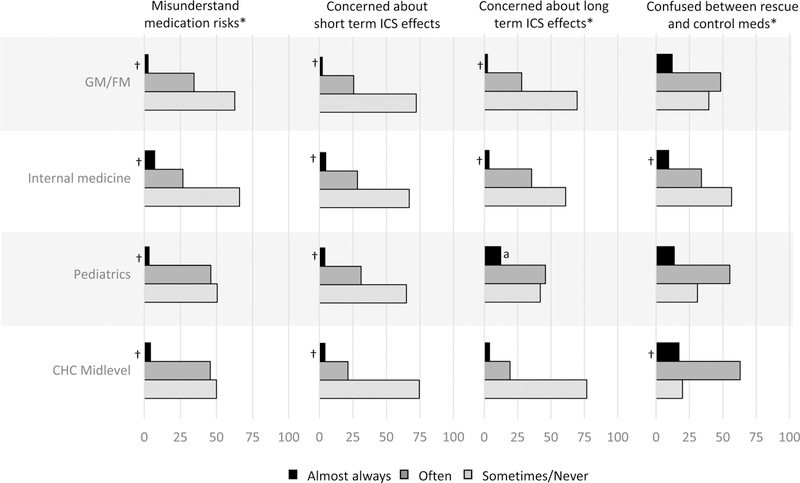
Percent of primary care clinicians who reported patient misunderstanding and concerns about asthma medications: Guideline, component 2
* Statistically significant difference between primary care specialty groups.
† Relative standard error >30%
a Significantly higher compared to all other clinician groups (t‐test p‐value<.05)
Notes: Adherence categories: Adherence categories: Almost always (>75% of the time), Often (25‐<75%), Sometimes/Never (<25% of the time)
Guideline component 3: assess and control environmental factors
There was no significant difference between primary care groups in reported adherence to assessing asthma triggers in the home (Table 3). However, internists were more likely than pediatricians or CHC midlevel providers to almost always assess asthma triggers in the school or workplace. Most primary care clinicians did not routinely test for allergic sensitivity.
Table 3.
Adherence with guideline-recommended measures to assess environmental factors: Guideline component 3 (weighted %, SE)
| Family/General Medicine | Internal Medicine | Pediatrics | CHC Mid-level Clinicians | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Almost always |
Often | Someti mes/ Never |
Almost always |
Often | Someti mes /Never |
Almost always |
Often | Someti mes/ Never |
Almost always |
Often | Someti mes/ Never |
Chi- square p-value |
|
| Assess home triggers | 1350 | 36.4 (3.4) | 46.7 (3.6) | 16.9 (2.7) | 40.2 (5.7) | 39.4 (5.4) | 20.4 (4.5) | 43.7 (4.3 ) | 38.6 (4.3) | 17.7 (3.6) | 38.2 (5.0) | 45.3 (4.7) | 16.6 (3.8) | 0.74 |
| Assess school or workplace triggers | 1355 | 33.1 (3.2) | 41.2 (3.5) | 25.7 (3.2) | 45.3 (5.7) | 33.6 (5.1) | 21.1 (4.5) | 29.6 (3.7) | 38.5 (4.2) | 32.0 (4.0) | 24.6 (4.0) | 46.4 (4.5) | 29.0 (4.6) | 0.08 |
| Test for allergic sensitivity | 1339 | 5.5 (1.5) | 15.2 (2.8) | 79.3 (3.0) | 10.7† (4.2) | 16.0 (4.0) | 73.4 (5.2) | 5.6† (1.8) | 26.0 (3.9) | 68.4 (4.1) | 3.1† (1.6) | 11.9 (3.4) | 85.0 (3.6) | 0.12 |
Relative standard error >30%
Notes: Adherence categories: Almost always (≥75% of the time), Often (25-<75%), Sometimes/Never (<25%)
Source: National Center for Health Statistics, 2012 National Asthma Survey of Physicians: National Ambulatory Medical Care Survey
Figure 2 shows AORs for “almost always” adhering to environmental recommendations (bottom three rows, see Table E5 for remaining covariates). A high frequency of specialist referral and high self-efficacy were associated with greater odds of assessing environmental factors. For example, clinicians who reported “almost always” referring patients to asthma specialists had an AOR of 3.6 (95% CI 1.4, 9.6) of assessing school/workplace triggers compared to those never or sometimes referred patients, and those with high self-efficacy had an AOR of 3.8 (95% CI 2.2, 6.8) compared to those with lower than high self-efficacy. There was no significant association between primary care group and high adherence with assessing school/workplace triggers in adjusted analyses.
Guideline component 4: pharmacologic treatment
Asthma medication prescription generally followed guideline recommended indications (Figure 4). ICS were prescribed for daily long-term control by 84.0% or higher among all clinician groups. Short and long course oral steroids were prescribed predominantly for acute exacerbations and difficult to control asthma, respectively. Pediatricians were less likely to use long course oral steroids than other groups. Omalizumab and methylxanthines were rarely used for difficult to control asthma among all groups, and pediatricians were more likely to report never using these medications compared to other groups. Anticholinergics were used for all indications, but less frequently by pediatricians for daily long-term control and add-on daily control therapy. Pediatricians were more likely to report never using LABA and LABA/ICS combinations compared to each of the other clinician groups, and CHC midlevel providers were more likely to never use these medications compared to internists. Nearly all clinicians reported prescribing short acting beta agonists for acute exacerbations.
Figure 4:
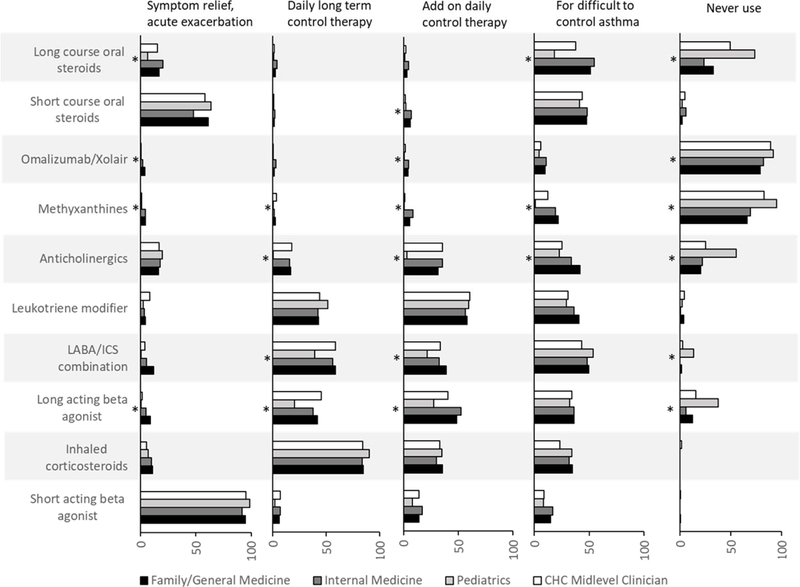
Reported use of medication by indication, by primary care group: Guideline component 4
* Statistically significant difference between primary care specialty group
Source: National Asthma Survey of Physicians: National Ambulatory Medical Care Survey
Discussion
Implementation of the EPR-3 guidelines is a healthcare and public health priority.5,27 Adherence by primary care clinicians is particularly important because they manage the majority of asthma visits,1,2 and guideline utilization improves asthma outcomes.28–31 A previous analysis demonstrated that adherence and self-efficacy were higher among asthma specialists compared to primary care clinicians but did not assess differences among different primary care clinician groups.22 Higher percentages of pediatricians reported high adherence with assessment/monitoring and asthma action plan recommendations, but were less likely to use controller medications other than inhaled corticosteroids. Similarities between groups were also observed. More than half of FM/GM, pediatricians and CHC mid-level providers reported patient confusion between rescue and control medications. Among all primary care groups, adherence was higher for recommendations involving history taking compared to those requiring iterative evaluation and objective assessment. Similar patterns of lower adherence for more resource-intensive recommendations have been observed in previous studies.7–9,11–20 Adherence was associated with high self-efficacy and frequent referral to asthma specialists. However, adherence was generally not associated with level of overall agreement with the guidelines which was low for all primary care groups. The index measure of agreement used in this study established a high threshold in that it required strong agreement with all five components assessed. It is likely that the association between agreement and adherence is more nuanced: as seen for AAP provision and spirometry, agreement with those specific guideline recommendations is associated with adherence to those items. Thus, providing evidence of efficacy for key guideline recommendations to clinicians and facilitating implementation (e.g., time, reimbursement) may be important to increasing adherence, especially for resource intensive items. While the findings highlight challenges, national-level data provide helpful information for ongoing efforts to improve guideline adherence and areas for additional research.
Over 50% of clinicians reported almost always adhering to specific assessment/monitoring recommendations involving history taking. Cabana et al. demonstrated that vague, global assessment of asthma control led to overestimation of good control, and concluded that assessing specific individual components is necessary to determine control status and the appropriate level of therapy.32 Pediatricians were generally more likely to report almost always adhering to individual assessment/monitoring recommendations, but they were not more likely to report strong agreement or high self-efficacy with guideline recommendations. However, asthma prevalence is higher in children than adults, and asthma is one of the most common chronic childhood conditions. Of visits to primary care clinicians, the majority are likely to be made to pediatricians,33 and in the NAS, pediatricians reported the highest asthma patient volume. Yet, patient volume may be only part of the difference between primary care groups—there are also fewer chronic diseases among children demanding clinician attention. Clinicians treating adults face a much larger number of chronic conditions with coinciding guidelines and comorbidities. Thus, clinicians who primarily treat children may be more familiar with asthma guideline-based management because asthma is one of the major chronic conditions they encounter.
Low adherence was observed for provision of written AAPs, agreeing with previous studies.5,8,9,12,13,15 AAPs are as much a clinician care coordination tool as a patient education tool—triggers, symptoms, and medication choice/dosage must all be understood and formulated to complete an AAP.5 AAPs are correlated with increased follow-up after emergency care, 28,34 adherence to preventive medication,28 and lower adverse outcomes,35 although others have questioned their added effectiveness in children who received other asthma education.36 High adherence to AAP provision was more likely among pediatricians, clinicians with frequent patient referrals to specialists, and those with high self-efficacy. A sensitivity analysis showed a significant association between AAP provision and agreement with this specific recommendation. Another sensitivity analysis showed that among patient concerns and confusions encountered, only confusion between rescue and controller medications was associated with AAP provision. It is unknown if encountering confusion spurred provision of an AAP, if such confusion was more likely to be uncovered when providing AAPs to patients, or both.
All clinician groups reported lower rates of high adherence with peak flow monitoring, spirometry and assessment of inhaler technique. These items involve assessment beyond history taking and/or require equipment that may be unavailable in a primary care setting. Similar patterns of lower adherence for more resource-intensive recommendations have been observed.7–9,11–20 Nevertheless, the feasibility of completing moderate-to-high levels of technical adequacy and accurate interpretation of spirometry in family medicine settings has previously been demonstrated,37 and the importance of objective monitoring in the diagnosis and management of asthma in primary care continues to be affirmed.14,38 Despite feasibility, studies report providers citing lack of training and expertise in performing and interpreting spirometry as barriers,14,16,39 and thus self-efficacy could be an important barrier to spirometry in particular. In addition, our sensitivity analysis showed that strong agreement with the necessity of spirometry was associated with adherence to spirometry recommendations. A nationally representative study reported that a high percentage of clinicians ever used spirometry (68% primary care physicians and 88% specialists).15 These much higher percentages compared to NAS are likely due to questionnaire differences—the NAS asked clinicians in what percentage of asthma visits they performed recommended guideline actions, a more narrow scope than “ever” using these tools. The EPR-3 guidelines recommend spirometry at least every 1–2 years, during periods of loss of asthma control, and as indicated by clinical severity.3 However, even considering this periodic recommended use, less than half of NAS respondents reported using spirometry >25% of the time.
ICS prescription for long-term asthma control is a key recommendation (84% or higher among all groups used ICS for daily long-term control). Previous studies reported 62–70% of clinicians regularly prescribed ICS but did not directly assess clinical indications.8,19 Previous studies reported concerns about ICS side effects9 and low adherence among primary care providers versus specialists.15,40 Sustained efforts to increase ICS use5 may have addressed barriers and concerns. Pediatricians and CHC mid-level providers were more likely to report never using other controller medications (long course oral steroids, omalizumab, methylxanthines, anticholinergics and LABA). Although a 2010 Food and Drug Administration statement recommended LABA use only in combination with ICS and efficacy and safety of LABA/ICS therapy in children has been demonstrated,41 safety concerns at the time of the survey could have resulted in avoidance of LABA in any form among clinicians treating children.
High self-efficacy with guideline recommendations and frequent patient referral to asthma specialists were associated with guideline adherence, but while high self-efficacy differed between clinician groups, it did not completely explain differences in adherence. Pediatricians had lower self-efficacy compared to internal medicine and family/general medicine clinicians despite the higher rate of adherence. Focusing guideline implementation efforts on self-efficacy could potentially improve adherence across all groups, but perhaps not address the differences in uptake of guideline recommendations between primary care clinician groups. Self-efficacy—confidence in implementing a goal-directed behavior—has been hypothesized to increase adherence 6,7,39 but may not be sufficient.6 A study of primary care physician adherence with COPD spirometry recommendations found low adherence despite high agreement and self-efficacy.39 A major barrier was lack of onsite equipment. Another study of asthma guidelines found that self-efficacy was necessary but not sufficient to increase guideline implementation.6 It is likely that observed associations with self-efficacy are sensitive to the measurement of this concept and that heterogeneity in the findings of the impact of perceived confidence should be expected. Referral behavior likely has a complex association with guideline adherence. EPR-3 guidelines recommend referral for life-threatening exacerbations, difficult to control asthma, atypical signs/symptoms or uncertain diagnosis, and high risk (oral steroids or hospitalization).3 Studies have reported high referral rates for life-threatening asthma events (>90%), whereas referral rates for other types of high-risk patients, including those with difficult to control asthma and uncertain diagnosis, have been lower (40–50%).9,12 Another aspect of referral behavior is the clinician’s patient population profile. One study found that lower outpatient asthma volume was associated with lower rates of allergy testing referral.8 Furthermore, low access to specialists has been associated with low income and may be an indicator of health care resources and quality.42
The NAS provided nationally representative data on the four EPR-3 cornerstone components with sufficient sample size, and thus allowed comparison of primary care clinician groups. Nevertheless, clinician self-report of adherence is a limitation and raises the possibility of recall bias and social desirability bias. While high adherence rates in this study to medications and environmental assessment were similar to those in a study assessing adherence using medical records,19 adherence to other items such as AAP provision were higher in this study, suggesting possible over-reporting. Nevertheless, the general magnitudes of adherence were similar (i.e., highest for medications, lower for items requiring documentation and patient education). The NAS did not collect visit-level data and patient characteristics such as age, race/ethnicity or disease severity. The NAS was not designed to assess other aspects of care, such as criteria for referral or patient population characteristics (e.g., asthma severity). In addition, the NAS included clinicians treating pediatric and adult populations. Other researchers have noted that pediatric healthcare involves aspects different than adult care, including a different natural history of asthma and caregiver structure. However, they conclude that the EPR-3 guidelines provide uniform cornerstone recommendations for patients of all ages.21 Detailed probing of familiarity, ambivalence and outcome expectancy with EPR-3 recommendations was not included in the NAS. Previous studies found high awareness of the asthma guidelines,7–9 although familiarity with specific recommendations was lower.8
Conclusions
Variation in implementation of recommended asthma care exists between primary care groups. High adherence was more likely to be reported by pediatricians for assessment/monitoring and patient education. There was no difference between clinician groups with high adherence to environmental assessment and medication prescription for acute exacerbations and long-term control. This survey also demonstrated higher adherence to guideline recommendations among all groups that could be considered “low hanging fruit”—those involving history taking. Recommendations requiring additional equipment, training and patient education had lower rates of high adherence. Future research could examine interventions to enhance adherence to resource-intensive recommendations, the potentially nuanced role of self-efficacy, and clinical decision-making underlying referral behavior.
Supplementary Material
Abbreviations:
- AAP
Asthma Action Plan
- CHC
Community Health Center
- EPR-3
Expert Panel Report-3
- FM/GM
family/general medicine
- ICS
Inhaled corticosteroids
- IM
internal medicine
- LABA
Long acting beta agonist
- NAMCS
National Ambulatory Medical Care Survey
- NAS
National Asthma Survey of Physicians
- RSE
relative standard error
- SE
standard error
References
- 1.Schappert SM, Rechtsteiner EA. Ambulatory medical care utilization estimates for 2007. Vital Health Stat 13. 2011(169):1–38. [PubMed] [Google Scholar]
- 2.National Center for Health Statistics. 2009–2010 Combined Year Tables: Table 1. Annual number and percent distribution of ambulatory care visits by setting type according to diagnosis group. 2010; https://www.cdc.gov/nchs/ahcd/web_tables.htm. Accessed 06/19/2018.
- 3.National Asthma Education and Prevention Program. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. National Heart, Lung, and Blood Institute, National Institutes of Health; August 28, 2007. 2007. [Google Scholar]
- 4.U.S. Environmental Protection Agency. If you have a child with asthma, you’re not alone. 2001; https://nepis.epa.gov/Exe/tiff2png.cgi/000002C7.PNG?-r+75+-g+7+D%3A%5CZYFILES%5CINDEX%20DATA%5C00THRU05%5CTIFF%5C00000266%5C000002C7.TIF. Accessed January 12, 2018.
- 5.National Asthma Education and Prevention Program. Guidelines Implementation Panel Report for: Expert Panel Report 3—Guidelines for the Diagnosis and Management of Asthma. National Institutes of Health;2008. NIH Publication No. 09–6147. [Google Scholar]
- 6.Cloutier MM, Tennen H, Wakefield DB, Brazil K, Hall CB. Improving clinician self-efficacy does not increase asthma guideline use by primary care clinicians. Academic pediatrics. 2012;12(4):312–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cabana MD, Rand CS, Becher OJ, Rubin HR. Reasons for pediatrician nonadherence to asthma guidelines. Archives of pediatrics & adolescent medicine. 2001;155(9):1057–1062. [DOI] [PubMed] [Google Scholar]
- 8.Wisnivesky JP, Lorenzo J, Lyn-Cook R, et al. Barriers to adherence to asthma management guidelines among inner-city primary care providers. Annals of allergy, asthma & immunology : official publication of the American College of Allergy, Asthma, & Immunology. 2008;101(3):264–270. [DOI] [PubMed] [Google Scholar]
- 9.Finkelstein JA, Lozano P, Shulruff R, et al. Self-reported physician practices for children with asthma: are national guidelines followed? Pediatrics. 2000;106(4 Suppl):886–896. [PubMed] [Google Scholar]
- 10.Cloutier MM. Asthma management programs for primary care providers: increasing adherence to asthma guidelines. Current opinion in allergy and clinical immunology. 2016;16(2):142–147. [DOI] [PubMed] [Google Scholar]
- 11.Cabana MD, Bruckman D, Meister K, Bradley JF, Clark N. Documentation of asthma severity in pediatric outpatient clinics. Clin Pediatr (Phila). 2003;42(2):121–125. [DOI] [PubMed] [Google Scholar]
- 12.Boulet LP, Devlin H, O’Donnell DE. The Physicians’ Practice Assessment Questionnaire on asthma and COPD. Respiratory medicine. 2011;105(1):8–14. [DOI] [PubMed] [Google Scholar]
- 13.Diette GB, Skinner EA, Markson LE, et al. Consistency of care with national guidelines for children with asthma in managed care. The Journal of pediatrics. 2001;138(1):59–64. [DOI] [PubMed] [Google Scholar]
- 14.Dombkowski KJ, Hassan F, Wasilevich EA, Clark SJ. Spirometry use among pediatric primary care physicians. Pediatrics. 2010;126(4):682–687. [DOI] [PubMed] [Google Scholar]
- 15.Janson S, Weiss K. A national survey of asthma knowledge and practices among specialists and primary care physicians. The Journal of asthma : official journal of the Association for the Care of Asthma. 2004;41(3):343–348. [DOI] [PubMed] [Google Scholar]
- 16.O’Dowd LC, Fife D, Tenhave T, Panettieri RA, Jr. Attitudes of physicians toward objective measures of airway function in asthma. Am J Med. 2003;114(5):391–396. [DOI] [PubMed] [Google Scholar]
- 17.Sokol KC, Sharma G, Lin YL, Goldblum RM. Choosing wisely: adherence by physicians to recommended use of spirometry in the diagnosis and management of adult asthma. Am J Med. 2015;128(5):502–508. [DOI] [PubMed] [Google Scholar]
- 18.Tumiel-Berhalter LM, Watkins R. The impact of provider knowledge and attitudes toward national asthma guidelines on self-reported implementation of guidelines. The Journal of asthma : official journal of the Association for the Care of Asthma. 2006;43(8):625–628. [DOI] [PubMed] [Google Scholar]
- 19.Yawn BP, Rank MA, Cabana MD, Wollan PC, Juhn YJ. Adherence to Asthma Guidelines in Children, Tweens, and Adults in Primary Care Settings: A Practice-Based Network Assessment. Mayo Clin Proc. 2016;91(4):411–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yee AB, Fagnano M, Halterman JS. Preventive asthma care delivery in the primary care office: missed opportunities for children with persistent asthma symptoms. Academic pediatrics. 2013;13(2):98–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Okelo SO, Butz AM, Sharma R, et al. Interventions to modify health care provider adherence to asthma guidelines: a systematic review. Pediatrics. 2013;132(3):517–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cloutier MM, Salo PM, Akinbami LJ, et al. Clinician Agreement, Self-efficacy, and Adherence with the Guidelines for the Diagnosis and Management of Asthma. The journal of allergy and clinical immunology In practice. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Center for Health Statistics Division of Health Care Statistics. 2012 NAMCS micro-data file documentation. 2016; August 21, 2015:ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NAMCS/doc2012.pdf.
- 24.National Center for Health Statistics Division of Health Care Statistics. Physician Induction Interview Sample Card. 2012; OMB No. 0920–0234:https://www.cdc.gov/nchs/data/ahcd/2012_NAMCS_Physician_Induction_Interview_Sample_Card.pdf. Accessed May 22, 2017.
- 25.The College of Family Phyisicians of Canada CMA, Royal College,. National Physician Survey: 2014 Response Rates. 2014; http://nationalphysiciansurvey.ca/surveys/2014-survey/response-rates/. Accessed July 9, 2017.
- 26.Knol MJ, Janssen KJ, Donders AR, et al. Unpredictable bias when using the missing indicator method or complete case analysis for missing confounder values: an empirical example. J Clin Epidemiol. 2010;63(7):728–736. [DOI] [PubMed] [Google Scholar]
- 27.National Center for Environmental Health CfDCaP. CDC’s National Asthma Control Program. 2018; https://www.cdc.gov/asthma/nacp.htm. Accessed February 17,2018.
- 28.Ducharme FM, Zemek RL, Chalut D, et al. Written action plan in pediatric emergency room improves asthma prescribing, adherence, and control. American journal of respiratory and critical care medicine. 2011;183(2):195–203. [DOI] [PubMed] [Google Scholar]
- 29.Wu AW, Young Y, Skinner EA, et al. Quality of care and outcomes of adults with asthma treated by specialists and generalists in managed care. Arch Intern Med. 2001;161(21):2554–2560. [DOI] [PubMed] [Google Scholar]
- 30.Janson SL, McGrath KW, Covington JK, Cheng SC, Boushey HA. Individualized asthma self-management improves medication adherence and markers of asthma control. The Journal of allergy and clinical immunology. 2009;123(4):840–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Williams LK, Pladevall M, Xi H, et al. Relationship between adherence to inhaled corticosteroids and poor outcomes among adults with asthma. The Journal of allergy and clinical immunology. 2004;114(6):1288–1293. [DOI] [PubMed] [Google Scholar]
- 32.Cabana MD, Slish KK, Nan B, Lin X, Clark NM. Asking the correct questions to assess asthma symptoms. Clin Pediatr (Phila). 2005;44(4):319–325. [DOI] [PubMed] [Google Scholar]
- 33.Burt CW, Knapp DE. Ambulatory care visits for asthma: United States, 1993–94. Advance data. 1996(277):1. [PubMed] [Google Scholar]
- 34.Butz AM, Halterman J, Bellin M, et al. Improving preventive care in high risk children with asthma: lessons learned. The Journal of asthma : official journal of the Association for the Care of Asthma. 2014;51(5):498–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gibson PG, Powell H. Written action plans for asthma: an evidence-based review of the key components. Thorax. 2004;59(2):94–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kelso JM. Do Written Asthma Action Plans Improve Outcomes? Pediatr Allergy Immunol Pulmonol. 2016;29(1):2–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yawn BP, Enright PL, Lemanske RF Jr., et al. Spirometry can be done in family physicians’ offices and alters clinical decisions in management of asthma and COPD. Chest. 2007;132(4):1162–1168. [DOI] [PubMed] [Google Scholar]
- 38.Derom E, van Weel C, Liistro G, et al. Primary care spirometry. The European respiratory journal. 2008;31(1):197–203. [DOI] [PubMed] [Google Scholar]
- 39.Salinas GD, Williamson JC, Kalhan R, et al. Barriers to adherence to chronic obstructive pulmonary disease guidelines by primary care physicians. Int J Chron Obstruct Pulmon Dis. 2011;6:171–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Diette GB, Skinner EA, Nguyen TT, Markson L, Clark BD, Wu AW. Comparison of quality of care by specialist and generalist physicians as usual source of asthma care for children. Pediatrics. 2001;108(2):432–437. [DOI] [PubMed] [Google Scholar]
- 41.Xia Y, Kelton CM, Xue L, Guo JJ, Bian B, Wigle PR. Safety of long-acting beta agonists and inhaled corticosteroids in children and adolescents with asthma. Ther Adv Drug Saf. 2013;4(6):254–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Flores G, Snowden-Bridon C, Torres S, et al. Urban minority children with asthma: substantial morbidity, compromised quality and access to specialists, and the importance of poverty and specialty care. The Journal of asthma : official journal of the Association for the Care of Asthma. 2009;46(4):392–398. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


