Abstract
Clinical reasoning is a complex cognitive process that is essential to evaluate and manage a patient’s medical problem. The aim of this paper was to provide a critical review of the research literature on clinical reasoning theories and models. To conduct our study, we applied the process of conducting a literature review in four stages in accordance with the approach of Carnwell and Daly. First, we defined the scope of the review as being limited to clinical reasoning theories and models in medical education. In the second stage, we conducted a search based on related words in PubMed, Google Scholar, PsycINFO, ERIC, ScienceDirect and Web of Science databases. In the third stage, we classified the results of the review into three categories, and in the fourth stage, we concluded and informed further studies. Based on the inclusion and exclusion criteria, 31 articles were eligible to be reviewed. Three theories and two models were recognized and classified into three categories. Several theories and models have been proposed in relation to clinical reasoning, but it seems that these theories and models could only explain part of this complex process and not the whole process. Therefore, to fulfill this gap, it may be helpful to build a Meta-model or Meta-theory, which unified all the models, and theories of clinical reasoning.
Keywords: clinical reasoning, medical education, review
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
Clinical reasoning is a complex cognitive process that is essential to evaluate and manage a patient’s medical problem.1 It includes the diagnosis of the patient problem, making a therapeutic decision and estimating the prognosis for the patient.2 In describing the importance of clinical reasoning, it has been acknowledged that clinical reasoning is the central part of physician competence,3 and stands at the heart of the clinical practice,4 it has an important role in physicians’ abilities to make diagnoses and decisions.1 Clinical reasoning has been the subject of academic and scientific research for decades;5 and its theoretical underpinning has been studied from different perspectives.6 Clinical reasoning is a challenging, promising, complex, multidimensional, mostly invisible,7 and poorly understood process.8 Researchers have explored its nature since 1980,9 but due to the lack of theoretical models, it remains vague. Most used theoretical models have limited explanatory power, and are based on certain assumptions about what constitutes clinical reasoning.10 In the literature of clinical reasoning, several competing theories and models have been raised.1,11–13 Although most of the theoretical contributions on clinical reasoning belong to the 20th century, proposing new models are well continued into the 21st century, for example, Haring and her colleagues proposed a conceptual model for expert judgment of clinical reasoning of medical students.14 However, there is no general agreement as to which of these is the best.15 The purpose of this paper is to provide a critical review of the research literature on clinical reasoning theories and models and present a comprehensive view of main models and theories of clinical reasoning in medical education. A clearer understanding of clinical reasoning models and theories help medical teachers for teaching, planning, and assessment of clinical reasoning. This paper tries to clarify the current knowledge regarding the clinical reasoning models and theories and present a classification of the main theories and models.
Materials and methods
Grant noted, “A critical review aims to demonstrate that the writer has extensively researched the literature and critically evaluated its quality.”16 It included a degree of analysis and conceptual innovation.16 In this study, we applied the process of conducting a literature review according to Carnwell and Daly.17 They proposed a “four-stage” method that included: 1) “Defining the scope of the review,” 2) “Identifying and selecting the sources of relevant information,” 3) “Organizing the results of the review into categories,” and 4) “Concluding and informing further studies.”17
Step 1: defining the scope of the review
The scope of this review was limited to the main clinical reasoning theories and models proposed in medical education literature. We concentrated our review on published works in scholarly journals between the years 1970 and 2018.
Step 2: identifying and selecting the sources of relevant information
At this stage, each of the two reviewers conducted a separate search based on keywords – “clinical reasoning,” “diagnostic reasoning,” “clinical reasoning theory,” “clinical reasoning model,” “script theory,” “hypothetico–deductive model,” “cognitive continuum theory,” and “dual processing theory” – in PubMed, Google Scholar, PsycINFO, ERIC, ScienceDirect and Web of Science databases. The results were pooled and extensive literature were found (n=305) which was from 1970 to 2018, but due to lack of access to the full text of some articles, and after removing duplicated studies, the title and abstract of articles from 1974 up to 2018 have been reviewed by researchers (n=170) (Table 1).
Table 1.
Scientific studies about clinical reasoning that has been title and abstract reviewed
| First decade | Second decade | Third decade | Fourth decade | Fifth decade |
|---|---|---|---|---|
| Feinstein (1974)41 Rubin (1975)42 Elstein et al (1978)43 Elstein & Bordage (1979)44 |
Kraytman et al (1981)45 Feltovich et.al (1984)46 Kuipers & Kassirer (1984)47 Schmidt & de Volder (1984)23 McGuire (1985)48 Patel et al (1986)19 Barrows et al (1987)31 Case et al (1988)32 Hamm (1988)39 Groen & Patel et al (1988)49 Girotto & Legrenzi (1989)50 |
Elstein et al (1990)18 Joseph & Patel (1990)51 Patel et al (1990)52 Norman et al (1990)53 Schmidt et al (1990)25 Ericsson (1991)54 Kaufman (1991)55 Mattingly (1991)56 Custers et al (1992)57 Evans & Patel (1992)58 Florance (1992)59 Henny Boshuizen et al (1992)60 Higgs (1992)20 Arocha et al (1993)61 Hassebrock et al (1993)62 Patel et al (1993)63 Schmidt et al (1993)64 Higgs (1993)65 Joseph Arocha et al (1993)66 Bordage (1994)67 Elstein (1994)22 Patel et al (1994)68 Jones (1995)69 Joseph Arocha & Patel (1995)70 Custers (1995)71 Custers et al (1996)26,28 Hammond (1996)38 Mandin et al (1997)30 Van de Wiel (1997)72 Allen et al (1998)73 Chang & Bordage (1998)74 Charlin et al (1998)75 Custers et al (1998)24 Cuthbert (1999)76 Kaufman et al (1999)77 Round (1999)78 |
Charlin et al (2000)12 Carter & Robinson (2001)79 Harries & Harries (2001)80 Round (2001)6 Elstein & Schwarz (2002)81 Nendaz (2002)82 Patel et al (2002)83 Bleakley et al (2003)84 Coderre et al (2003)85 Norman & Eva (2003)86 Eshach & Bitterman (2003)87 Groves et al (2003)88 Hardin (2003)89 Charlin &Van der Vleuten (2004)90 Eva (2004)91 Rikers et al (2004)92 Verkoeijen et.al (2004)93 Holyoak & Morrison (2005)21 Norman (2005)3 Tamayo-Sarver (2005)94 Anderson (2006)95 Bowen (2006)96 Eva & Cunnington (2006)97 Loftus (2006)5 Montgomery (2006)98 Novak et al (2006)99 Thornton (2006)100 Auclair (2007)101 Schmidt & Rikers (2007)102 Norman et al (2007)11 Banning(2008)103 Evans (2008)13 Harasym et al (2008)29 Heiberg (2008)104 Higgs (2008)7 Humbert (2008)105 |
Aleluia et al (2010)113 Corcoran (2010)114 Mariasin (2010)115 Lee et al (2010)116 Omana et al (2010)117 Wilhelmsson (2010)118 Thomson et al(2010)8 Amini et al (2011)119 Durning (2011)120 Franklin et.al.(2011)121 Pelaccia et al (2011)1 Thomson et al (2011)8 Adams (2012)122 Ashoorion et al (2012)123 Van Bruggen (2012)124 Charlin et al (2012)125 Demirören & Palaoğlu (2012)126 Braude (2012)127 Braude (2012)128 Khatami et al (2012)129 Lucchiari & Pravettoni (2012)10 Loftus (2012)4 Marcum (2012)34 Nouh et al (2012)130 Shaban (2012)131 Adams (2013)9 Custers (2013)40 Audétat et al (2013)132 Da Silva (2013)133 Evans & Stanovich (2013)36 Gigante (2013)134 Kriewaldt (2013)135 Lubarsky et al (2013)136 Munshi et al (2013)137 Smith (2013)138 Weiss et al (2013)139 Ilgen et al (2013)140 |
| Noreen et al (2008)106 Vertue & Haig (2008)107 Braude(2009)108 Bissessur et al (2009)109 Carrière et al (2009)110 Croskerry (2009)35,37 Elstein (2009)33 Stempsey (2009)15 Rehder & Woo Kim (2009)111 Vosniadou (2009)112 |
Bowen & Ilgen (2014)141 Delany & Golding (2014)142 Freiwald et al (2014)143 Geisler et al (2014)144 Gordon (2014)145 Holmboe & Durning (2014)146 Hrynchak et al (2014)147 Hochberg et al (2014)148,149 Monajemi (2014)150 Roots (2014)151 Salkeld (2014)152 Smith et al (2014)153 Capaldi (2015)154 Custers (2015)27 Gaba (2015)155 Islam et al (2015)156 Lafleur & Leppink (2015)157 Lubarsky et al (2015)158 Park et al (2015)159 Lisk (2016)160 McBee et al (2016)161 Gruppen (2017)162 Haring et al (2017)14 Jarodzka et al (2017)163 Norman et.al (2017)164 Ten Cate et.al (2017)165 Zamani et al (2017)166 Bowen & ten Cate (2018)167 Custers (2018)168 Daly (2018)2 King et al (2018)169 Keemink et al (2018)170 Lopes et al (2018)171 Yazdani & Hoseini (2017)172 Yazdani et al (2018)173 Higgs et al (2018)174 |
Then, the articles that presented theories or models of clinical reasoning in medicine or provided evidence in relation to them were selected to full-text study. Studies were eligible for this critical review if they presented a model or a theory of clinical reasoning, or related critiqued models and theories or the studies that add some features to the theories and models of clinical reasoning (n=47). The inclusion criteria of selecting studies were: 1) published articles in English and Persian and 2) published articles in the field of medicine. Studies were excluded if they provided clinical reasoning models or theories in other fields (like nursing and optometry), examined the clinical reasoning in the field of artificial intelligence (like clinical decision support systems), and/or examined brain biology and brain functions (like fMRI studies).
Step 3: organizing the results of the review into categories
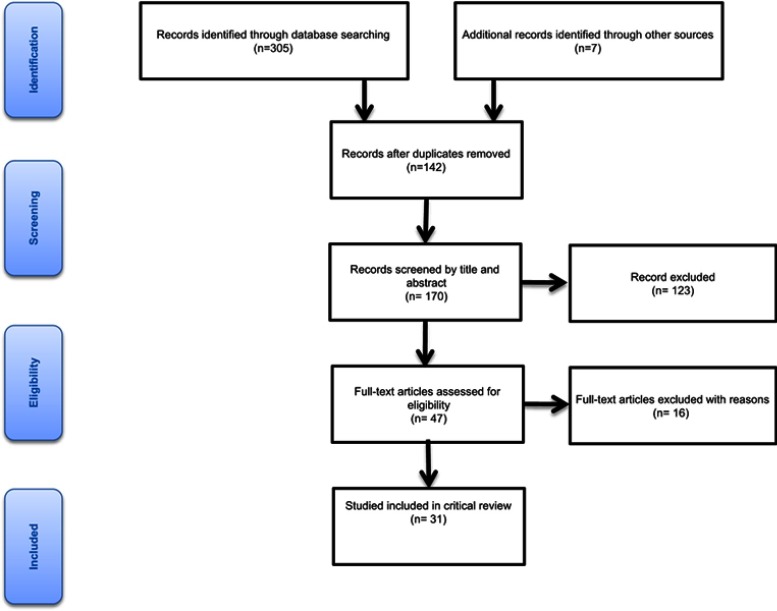
After excluding irrelevant studies, a total of 31 documents were initially selected for review which is shown in PRISMA flowchart below (Figure 1).
Figure 1.
PRISMA flowchart.
Models and theories which were extracted from studies, classified to three categories and each category, based on Carnwel and Daly approach, reviewed in three steps: first, we present a summary of the models and theories, and then reflect other author’s views and finally, we present our view (Table 2).17 If a model or theory explains about the process of clinical reasoning our first category owns it while models and theories which clarified the formation of knowledge structures and their application during the clinical reasoning process belongs to the second category, and our third category consisted models and theories which consider more than one processing modes of clinical reasoning.
Table 2.
The list of 31 related literatures that included in the review
| Category no. | Theory/model | Author | Year | Aspects related to supporting/criticizing the model |
|---|---|---|---|---|
| First category: theories and models based on the process of clinical reasoning | Hypothetico-deductive model | Elstein | 199018 | The description of the hypothetico-deductive model The advantages of hypothetico-deductive model |
| Patel | 198619 | Lack of consistency of hypothetico-deductive model with other domains | ||
| Higgs | 199220 | Clinical reasoning process is not sequential | ||
| Charlin | 200012 | Unfamiliarity of psychological mechanisms involved in this model | ||
| Holyoak | 200521 | No differentiation between novice and expert clinical reasoning | ||
| Loftus | 20065 | Clarification of the role of hypothesis in clinical reasoning process | ||
| Higgs | 20087 | Adequate description of the process of clinical reasoning | ||
| Elstein | 199422 | Application of hypotheses for framing of clinical problems | ||
| Second category: theories and models based on the knowledge structure | Illness script theory | Schmidt | 198423 | The description of the illness script theory Formation and development of the illness script |
| Custers | 199824 | The description of the illness script theory | ||
| Schmidt | 199025 | The structure of illness script Formation and development of the illness script |
||
| Custers | 199626 | The structure of illness script | ||
| Custers | 201527 | Script concordance test Formation and development of the illness script |
||
| Custers | 199628 | The structure of illness script | ||
| Harasym | 200829 | Formation and development of the illness script | ||
| Mandin | 199730 | Distinction between the concept of the script and the schema | ||
| Pattern recognition model | Barrows | 198731 | The description of the model | |
| Case S | 198732 | It used by experienced practitioners | ||
| Norman | 200711 | The most usual form of nonanalytic processes | ||
| Elstein | 200933 | Unanswered questions about pattern recognition model | ||
| Marcum | 201234 | The complexity of cognitive processes involved in clinical reasoning to be ignored. | ||
| Higgs | 20087 | Pattern recognition model examined in limited field of expertise. | ||
| Third category: compilation theories and mode | Dual processing theory | Evans | 200836 | The description of the theory |
| Croskerry | 200935 | Advantages of this theory | ||
| Croskerry | 200937 | Proposing a model based on dual processing theory | ||
| Pelaccia | 20111 | Clarification of the place of pattern recognition and hypothetico-deductive models in dual processing theory. | ||
| Evans | 201336 | Criticized this theory in five major themes | ||
| Lucchiari | 201210 | Models based on dual processing theory | ||
| Cognitive continuum | Hammond | 199638 | The description of the theory | |
| Hamm | 198839 | The description of the theory | ||
| Custers | 201340 | Advantages of this theory |
Results
First category: theories and models based on the process of clinical reasoning
This category includes the models and theories that explain the clinical reasoning process, between models and theories that we reviewed, only hypothetico-deductive model was eligible to get placed in the first category as the most reputed model that explains the clinical reasoning process. This model was proposed by Elstein (1978), and, according to this model, the physicians primarily generate a limited number of diagnostic hypotheses or problem formulations in the process of solving a diagnostic problem and then testing them. These hypotheses guide further patient information.18,19 Unlike the findings of hypothetico-deductive model that claim: “primarily generated and tested hypotheses by expert and novice are the same,” Patel believed that it is not consistent in other domains, like physics.19
Higgs argued that this model posits the idea that the process of clinical reasoning is largely a sequential process.20 Charlin pointed out that the psychological mechanisms involved in the generation and testing of relevant hypotheses are unfamiliar,12 and Holyoak argued that this model does not distinguish between novice and expert clinical reasoning strategies.21 Loftus believed that the collected information and the way they interpreted, distorted by the used hypothesis.5 This model as an adequate description of the process of clinical reasoning has challenged by the case specificity findings.7
Nevertheless, some researchers defend hypothetico-deductive model, Elstein argued that the small set of solutions that generated in this model transformed an unstructured problem to structured one and it is an effective way to solve diagnostic problems.18 This model is recommended by medical experts as a useful reasoning strategy for medical students.22 Hypothetico-deductive model is applicable when data are vague or reveal over time,22 and is a representation of clinical reasoning.20 This model represents a description of the mental processes used by physicians and has repeatedly been validated by empirical studies and is the basis for modern clinical education.12
Hypothetico-deductive model assumes the physician starts hypothesizing after collecting patient information and then tests hypotheses, while we believe the physician starts hypothesizing initially from his/her clinical encounter. The initial hypotheses can be strong or weak, depending on whether the physician is an expert or novice, the difference between the novice and the expert lies in the quality of the hypotheses they made. Therefore, since the initial hypothesis of an expert has good quality, hypothesis testing will be fast and efficient. The simplicity of this model in describing the process of clinical reasoning is both strength and the weakness of it, as a strength, because it simply portrays the start point of the process of clinical reasoning so it can be used to design the teaching plan and evaluate clinical reasoning. As a weakness, because it considers the process of diagnostic reasoning very simple, while even for a novice, this process does not occur so easily, and other factors (such as the individual’s knowledge structure, the context, the health system, etc.) affect the process of clinical reasoning, but this model does not consider these factors.
Second category: theories and models based on the knowledge structure
For this category, we considered theories and models that explain the formation of knowledge structures in the clinical reasoning process, by this description and the inclusion criteria just one theory and one model of clinical reasoning gain eligibility to include, the “illness script theory” and the “pattern recognition model.”
The illness script theory proposed by Barrows and Feltovich consists of three components: 1) enabling conditions, 2) fault, and 3) consequences.23 The first component is the factors such as age, sex, current medication, previous medical history, occupation, risk behavior, hereditary, and environment affect the probability of someone gets a disease, are the patient’s contextual and background factors that refer to “Enabling conditions.” These “Enabling conditions” can cause the latter pathophysiological malfunctioning that called “fault” which is the second component of illness script. Consequences of this fault are complaints, signs, and symptoms that consist of the third component.24 Illness scripts are the list-like structures,25 which conceptualized as a specific representation of clinical knowledge.26 Script concordance test designed according to this theory.27
While we were studying about Illness script theory, we realized that we could categorize studies into two broad groups. The first group is the studies that deal with the concept of the script, the schema, and the illness script, and their features, distinctions, and components (Table 3).24,26–28
Table 3.
The studies that deal with the concept of “script,” “schema,” and “illness script,” and their features, distinctions, and components
The second group deals with the formation and development of the illness script during the acquisition of expertise and changes in the physician’s knowledge structure (Table 4).23,25,26,29
Table 4.
The studies that deal with the formation and development of “illness script” during the acquisition of expertise and changes in the physician’s knowledge structure
The first group of studies also looked at the distinction between the concept of the script and the schema, but this distinction was not clear in the literature. The schemas and scripts are stored in long-term memory.30
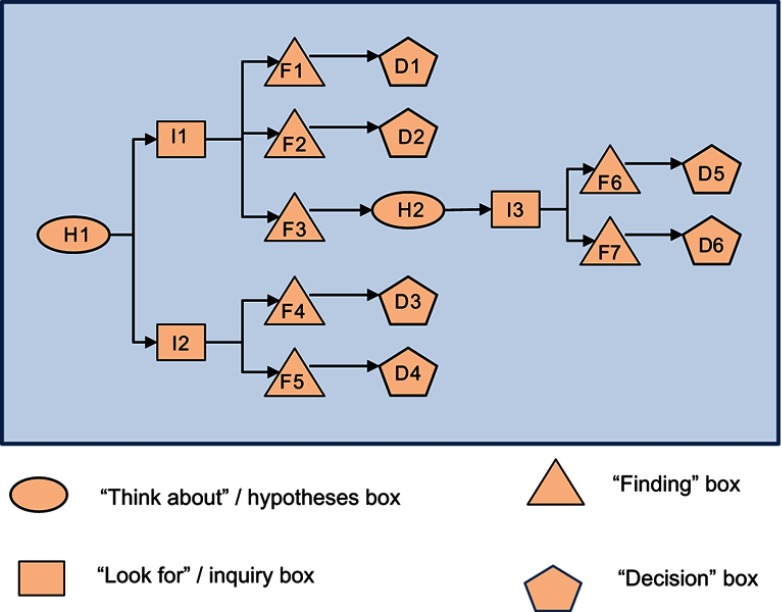
Schema as a knowledge structure has an “if/then” formatting and occurs sequentially, in the sense that this sequence divided into two branches: “if” and “then,” so we can claim out that its format is algorithmic. This algorithm starts with a hypothesis in a person’s mind or something that a person thinks about and then continues with inquiries and searches that a physician has performed and then with the findings that a physician has reached, and finish with the decisions that he/she has finally taken (Figure 2).
Figure 2.
Generic flow of events in a typical schema. D1: Decision No 1; D5: Decision No 6; F1: Finding No 1; F5: Finding No 5; H1: Hypothesis No 1; H2: Hypothesis No 2; I1: Inquiry No 1; I3: Inquiry No 3.
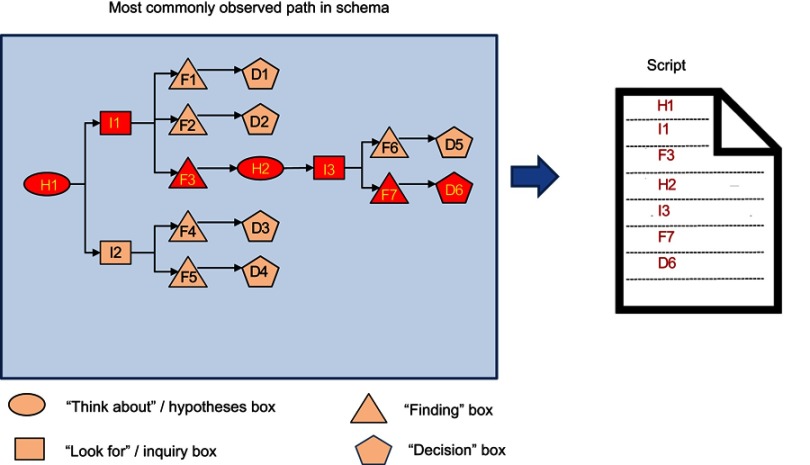
In terms of the structure of the script, we also agree with Schmidt’s view that the scripts are list-like structures, but unlike Charlin, who believed that “the script describes the structure of clinical knowledge,” we believe that the script is not necessarily the structure of clinical knowledge, but a knowledge structure that has clinical applications. The script is schemas for common situations, which include a packet or a list of expectations of what people see or do at a given location. The schemas and scripts are stored in long-term memory, and if physicians encounter a clinical case that matches with them, they will retrieve it from long-term memory and move it to short-term memory (Figure 3).
Figure 3.
Script as a routinized pathway of previously used schema. D1: Decision No 1; D5: Decision No 6; F1: Finding No 1; F5: Finding No 5; H1: Hypothesis No 1; H2: Hypothesis No 2; I1: Inquiry No 1; I3: Inquiry No 3.
Pattern recognition model
In the pattern recognition model, a physician directly compares the pattern of the patient’s problem with disease patterns and if found them similar to each other, then select the pattern that matches it.31 Experienced practitioners often use pattern recognition to achieve a medical diagnosis.32 Norman and his colleagues argue that pattern recognition is the most usual form of nonanalytic processes.11 However, Elstein proposed some questions about this model, as followed:
When dose a person use a pattern recognition model?
When is this method preferable to the hypothetico-deductive method?
What guarantees that the choice of a pattern or an illness script is correct?
What happens if the pattern or script stored in the knowledge base is wrong?33
This model considers the complexity of cognitive processes involved in clinical reasoning to be insignificant.34
Based on the definition of the pattern recognition model, it only mentions the existence of patterns in mind, but does not explain how the construction of these patterns occurred. The studies which designed to prove that the pattern recognition model happens in reality are in a limited field of expertise, like radiology, dermatology, and pathology. 7 So the pattern recognition model is not extendable to all medical specialties.
Third category: compilation theories and model
Some of the included documents were about “dual processing” and “cognitive continuum” theories that explain two modes of reasoning – “analytical” and “non-analytical,” these modes are the characteristics of both first and second category, so we cannot involve them in one of them, therefore they form our third category.
The dual-processing theories commonly have two different processing modes in which they refer to: System 1 and System 2.13 System 1 described as a fast, automatic and intuitive mode, which shares similarities through perception, while System 2 is slow and analytic mode that applies rules without inferring emotions.7
Croskerry believed that dual-processing theory is an applicable model in multiple domains of health care like decision-making and it can be useful in teaching decision theory or in making a platform to future research.35 Pelaccia et al noted that in the framework of this theory, the pattern recognition and hypothetico-deductive models are the basis of the intuitive system and the analytic system, respectively.1
Evans and Stanovich criticized this theory in five major themes: 1) various theorists have proposed multiple and vague definitions for this theory, 2) there is no consistency in associated attribute clusters with dual systems, 3) distinctions are referred to the continuum of processing and not to discrete processing; 4) the apparent dual-process phenomenon can present by single-process accounts; and 5) the evidence base for the dual-processing theory is ambiguous or unconvincing.36
In the reviewing of the literature, we found out that some of the researchers established their models based on dual-processing theory like Marcum,34 Croskerry,35,37 and Lucchiari and Pravettoni.10
Dual-processing theory employs many of the seemingly contradictory features that have been proposed for clinical reasoning in the literature (such as fast, slow, reflective, etc.). It seems that, in reality, a physician does not use just intuitive or analytic systems and the mind of physician operates in the space between them, while the dual-processing theory ignores this.
The theories and models that have been proposed following this theory have led to the introduction of cognitive concepts such as metacognition and perception and their role in the process of clinical reasoning. This theory has relatively clarified the role of emotions and their place of influence in the process of clinical reasoning, and has also contributed to clarifying the concept of intuition in clinical reasoning.
The second theory that has placed in third categories is cognitive continuum, as Hammond claimed, this theory considered two poles, an intuitive cognition and an analytical cognition, in which various modes or forms of cognition have relational order on a continuum, and this assumption rejected the dual-processing approach.38 Hamm believed, this theory does not explain the information processing that is the basis of analysis and intuition, but based on analytical and intuitive cognitive attributes it gives us various techniques in describing cognitive modes. Also, he believed that this theory did not offer an instruction about thinking analytically or intuitively, and it just presented a general framework. Cognitive continuum theory described the features of cognition and their correlation with the characteristics of the task.39 Custers noted that this theory illustrates the cognitive processes and the cognitive tasks on a continuum, and this theory can be used to provide advice on how to structure clinical tasks in an educational setting.40 In criticizing cognitive continuum theory, we did totally agree with Hamm and Custers.
Conclusion
The present study was conducted to critically review theories and models of clinical reasoning that have often been raised in the medical education literature within five decades (1970–2018). Several theories and models presented in relation to clinical reasoning and it seems that they can explain only part of the complex process, but not the whole process. For example, the models and theories of the first category in our study just address the process of clinical reasoning and do not pay attention to knowledge structures and cognition; in the second category, they just focused on knowledge structures and their formations during clinical reasoning process and do not clarify the process of clinical reasoning. In addition, the dual processing and cognitive continuum theories that form the third category just covered the cognition part of the clinical reasoning. Therefore, to fulfill this gap, it may be helpful to build a Meta-model or Meta-theory, which unified all the models, and theories of clinical reasoning. Although our focus was on the main models and theories of clinical reasoning in the field of medical education, but we acknowledge that there are other models and theories of clinical reasoning in the literature and their absence can be the bias of this study.
Acknowledgment
This work was part of a PhD dissertation, funded and financially supported by the Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Pelaccia T, Tardif J, Triby E, Charlin B. An analysis of clinical reasoning through a recent and comprehensive approach: the dual-process theory. Med educ online. 2011;16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Daly P. A concise guide to clinical reasoning. J Eval Clin Pract. 2018;24(5):966–972. [DOI] [PubMed] [Google Scholar]
- 3.Norman G. Research in clinical reasoning: past history and current trends. Med educ. 2005;39(4):418–427. [DOI] [PubMed] [Google Scholar]
- 4.Loftus S. Rethinking clinical reasoning: time for a dialogical turn. Med educ. 2012;46(12):1174–1178. [DOI] [PubMed] [Google Scholar]
- 5.Loftus SF. Language in Clinical Reasoning: Learning and Using the Language of Collective Clinical Decision Making.Sydney, Australia: University of Sydney. 2006 [Google Scholar]
- 6.Round A. Introduction to clinical reasoning. J Eval Clin Pract. 2001. [DOI] [PubMed] [Google Scholar]
- 7.Higgs J, Jones M, Loftus S, Christensen N. Clinical Reasoning in the Health Professions. 3rd ed. Philadelphia, PA: Elsevier Health Sciences; 2008. [Google Scholar]
- 8.Thomson O, Petty N, J, Moore A. Clinical reasoning in osteopathy e More than just principles? Int J Osteopath Med. 2011;14: 71–76. [Google Scholar]
- 9.Adams L. Clinical Reasoning and Causal Attribution in Medical Diagnosis.Thesis. University of Plymouth; 2013. [Google Scholar]
- 10.Lucchiari C, Pravettoni G. Cognitive balanced model: a conceptual scheme of diagnostic decision making. J Eval Clin Pract. 2012;18(1):82–88. [DOI] [PubMed] [Google Scholar]
- 11.Norman G, Young M, Brooks L. Non‐analytical models of clinical reasoning: the role of experience. Med educ. 2007;41(12):1140–1145. [DOI] [PubMed] [Google Scholar]
- 12.Charlin B, Tardif J, Boshuizen H. Scripts and medical diagnostic knowledge: theory and applications for clinical reasoning instruction and research. Acad Med. 2000;75(2):182–190. [DOI] [PubMed] [Google Scholar]
- 13.Evans JSB. Dual-processing accounts of reasoning, judgment, and social cognition. Annu. Rev. Psychol. 2008;59:255–278. [DOI] [PubMed] [Google Scholar]
- 14.Haring CM, et al. Observable phenomena that reveal medical students' clinical reasoning ability during expert assessment of their history taking: a qualitative study. . BMC med educ. 2017;17(1):147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stempsey WE. Clinical reasoning: new challenges. Theor Med Bioeth. 2009;30(3):173–179. [DOI] [PubMed] [Google Scholar]
- 16.Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26(2):91–108. [DOI] [PubMed] [Google Scholar]
- 17.Carnwell R, Daly W. Strategies for the construction of a critical review of the literature. Nurse Educ Pract. 2001;1(2):57–63. [DOI] [PubMed] [Google Scholar]
- 18.Elstein AS, Shulman LS, Sprafka SA. Medical problem solving a ten-year retrospective. Eval Health Prof. 1990;13(1):5–36. [Google Scholar]
- 19.Patel VL, Groen GJ. Knowledge based solution strategies in medical reasoning. Cogn Sci. 1986;10(1):91–116. [Google Scholar]
- 20.Higgs J. Developing clinical reasoning competencies. Physiotherapy. 1992;78(8):575–581. [Google Scholar]
- 21.Holyoak KJ, Morrison R. The Cambridge Handbook of Thinking and Reasoning. Cambridge, UK: Cambridge University Press; ; 2005. [Google Scholar]
- 22.Elstein AS. What goes around comes around: return of the hypothetico‐deductive strategy. TEACH LEARN MED: An International Journal. 1994;6(2):121–123. [Google Scholar]
- 23.Schmidt HG, de Volder ML. Tutorials in Problem-based Learning: New Directions in Training for the Health Professions. 1st International Symposium. Van Gorcum; ; 1984. [Google Scholar]
- 24.Custers EJ, Boshuizen HP, Schmidt HG. The role of illness scripts in the development of medical diagnostic expertise: Results from an interview study. Cogn Instr. 1998;16(4):367–398. [Google Scholar]
- 25.Schmidt H, Norman G, Boshuizen H. A cognitive perspective on medical expertise: theory and implication [published erratum appears in Acad Med 1992 Apr; 67 (4): 287]. Acad med. 1990;65(10):611–621. [DOI] [PubMed] [Google Scholar]
- 26.Custers EJ, Boshuizen HP, Schmidt HG. The influence of medical expertise, case typicality, and illness script component on case processing and disease probability estimates. Mem Cognit. 1996;24(3):384–399. [DOI] [PubMed] [Google Scholar]
- 27.Custers EJ. Thirty years of illness scripts: Theoretical origins and practical applications. Med teach. 2015;37(5):457–462. [DOI] [PubMed] [Google Scholar]
- 28.Custers E, Regehr G, Norman GR. Mental representations of medical diagnostic knowledge: a review. Acad Med. 1996;71(10):S55–61. [DOI] [PubMed] [Google Scholar]
- 29.Harasym PH, Tsai T-C, Hemmati P. Current trends in developing medical students' critical thinking abilities. Kaohsiung J Med Sci. 2008;24(7):341–355. [DOI] [PubMed] [Google Scholar]
- 30.Mandin H, Jones A, Woloschuk W, Harasym P. Helping students learn to think like experts when solving clinical problems. Acad med: journal of the Association of American Medical Colleges. 1997;72(3):173–179. [DOI] [PubMed] [Google Scholar]
- 31.Barrows HS, Feltovich PJ. The clinical reasoning process. Med Educ. 1987;21(2):86–91. [DOI] [PubMed] [Google Scholar]
- 32.Case S, Swanson D, Stillman P Evaluating diagnostic pattern recognition: the psychometric characteristics of a new item format. Paper presented at: Research in medical education: proceedings of the … annual Conference. Conference on Research in Medical Education; United States: Whashington, DC; : 1987. [PubMed] [Google Scholar]
- 33.Elstein AS. Thinking about diagnostic thinking: a 30-year perspective. Adv Health Sci Educ Theory Pract. 2009;14(1):7–18. [DOI] [PubMed] [Google Scholar]
- 34.Marcum JA. An integrated model of clinical reasoning: dual‐process theory of cognition and metacognition. J Eval Clin Pract. 2012;18(5):954–961. [DOI] [PubMed] [Google Scholar]
- 35.Croskerry P. Clinical cognition and diagnostic error: applications of a dual process model of reasoning. Adv Health Sci Educ. 2009;14(1):27–35. [DOI] [PubMed] [Google Scholar]
- 36.Evans JSB, Stanovich KE. Dual-process theories of higher cognition advancing the debate. Perspect Psychol Sci. 2013;8(3):223–241. [DOI] [PubMed] [Google Scholar]
- 37.Croskerry P. A universal model of diagnostic reasoning. Acad med. 2009;84(8):1022–1028. [DOI] [PubMed] [Google Scholar]
- 38.Hammond KR. Human Judgment and Social Policy: Irreducible Uncertainty, Inevitable Error, Unavoidable Injustice. New York: Oxford University Press; : 1996. [Google Scholar]
- 39.Hamm RM. Clinical intuition and clinical analysis: expertise and the cognitive continuum In: Professional Judgment: A Reader in Clinical Decision Making. Cambridge, UK: Cambridge University Press; 1988:78–105. [Google Scholar]
- 40.Custers EJ. Medical education and cognitive continuum theory: an alternative perspective on medical problem solving and clinical reasoning. Acad Med. 2013;88(8):1074–1080. [DOI] [PubMed] [Google Scholar]
- 41.Feinstein AR. An analysis of diagnostic reasoning. 3. The construction of clinical algorithms. Yale J Biol Med. 1974;47(1):5. [PMC free article] [PubMed] [Google Scholar]
- 42.Rubin AD. Hypothesis formation and evaluation in medical diagnosis. 1975. Available from: https://dspace.mit.edu/handle/1721.1/6919. [Google Scholar]
- 43.Elstein AS, Shulman LS, Sprafka SA. Medical problem solving an analysis of clinical reasoning. Cambridge,US: Harvard University Press; 1978. [Google Scholar]
- 44.Elstein A, Bordage G. Psychology or clinical reasoning. Stone G, Cohen F, Adler N, editors. Health psychology: a handbook. San Francisco: Jossey-Bass. 1979:335-367. [Google Scholar]
- 45.Kraytman M. The preparation of medical students in our country: some clinical observations. Acta clinica Belgica. 1981;36(5):223–226. [DOI] [PubMed] [Google Scholar]
- 46.Feltovich PJ, Patel VL. The Pursuit of Understanding in Clinical Reasoning. 1984. [Google Scholar]
- 47.Kuipers B, Kassirer JP. Causal reasoning in medicine: analysis of a protocol. Cogn Sci. 1984;8(4):363–385. [Google Scholar]
- 48.McGuire CH. Medical problem-solving: a critique of the literature. J Med Educ.1985: 60(8):587–95 [PubMed] [Google Scholar]
- 49.Groen GJ, Patel VL. The relationship between comprehension and reasoning in medical expertise In: In Chi M. T. H., Glaser R., & Farr M. J. (Eds.), The nature of expertise . Hillsdale, NJ, US: Lawrence Erlbaum Associates, Inc1988: 287–310 [Google Scholar]
- 50.Girotto V, Legrenzi P. Mental representation and hypothetico-deductive reasoning: The case of the THOG problem. Psychol Res. 1989;51(3):129–135. [DOI] [PubMed] [Google Scholar]
- 51.Joseph G-M, Patel VL. Domain knowledge and hypothesis genenation in diagnostic reasoning. Med Decis Making. 1990;10(1):31–44. [DOI] [PubMed] [Google Scholar]
- 52.Patel VL, Groen GJ, Arocha JF. Medical expertise as a function of task difficulty. Mem Cognit. 1990;18(4):394–406. [DOI] [PubMed] [Google Scholar]
- 53.Norman GG, Patel V, Schmidt HH. Clinical inquiry and scientific inquiry. Med educ. 1990;24(4):396–399. [DOI] [PubMed] [Google Scholar]
- 54.Ericsson KA, Smith J. Toward a general theory of expertise: Prospects and limits. New York, US: Cambridge University Press; 1991. [Google Scholar]
- 55.Kaufman SG. A Formal Theory of Spatial Reasoning. In Allen J, Fikes RE, Sandewall E..Principles of Knowledge Representation and Reasoning: Proceedings of the Second International Conference. Morgan Kaufmann Publishers: 1991. [Google Scholar]
- 56.Mattingly C. The narrative nature of clinical reasoning. Am J Occup Ther. 1991;45(11):998–1005. [DOI] [PubMed] [Google Scholar]
- 57.Custers EJ. The Relationship between Medical Expertise and the Development of Illness-Scripts. 1992-Apr. Belgium; Netherlands [Google Scholar]
- 58.Evans C, Kakas AC. Reasoning Hypothetico-deductive. Paper presented at: Fifth Generation Computer Systems; 1992. Tokyo, Japan [Google Scholar]
- 59.Florance V. Medical knowledge for clinical problem solving: a structural analysis of clinical questions. Bull Med Libr Assoc. 1992;80(2):140. [PMC free article] [PubMed] [Google Scholar]
- 60.Boshuizen HP, Schmidt HG. On the role of biomedical knowledge in clinical reasoning by experts, intermediates and novices. Cogn Sci. 1992;16(2):153–184. [Google Scholar]
- 61.Arocha JF, Patel VL, Patel YC. Hypothesis generation and the coordination of theory and evidence in novice diagnostic reasoning. Med Decis Making. 1993;13(3):198–211. [DOI] [PubMed] [Google Scholar]
- 62.Hassebrock F, Johnson PE, Bullemer P, Fox PW, Moller JH. When less is more: Representation and selective memory in expert problem solving. Am J Psychol. 1993:155–189. [PubMed] [Google Scholar]
- 63.Patel VL, Groen GJ, Norman GR. Reasoning and instruction in medical curricula. Cogn Instr. 1993;10(4):335–378. [Google Scholar]
- 64.Schmidt HG, Boshuizen HP. On acquiring expertise in medicine. Educ Psychol Rev. 1993;5(3):205–221. [Google Scholar]
- 65.Higgs J. A programme for developing clinical reasoning skills in graduate physiotherapists. Med teach. 1993;15(2–3):195–205. [DOI] [PubMed] [Google Scholar]
- 66.Arocha JF, Patel VL, Patel YC. Hypothesis generation and the coordination of theory and evidence in novice diagnostic reasoning. Med Decis Making: an international journal of the Society for Medical Decision Making. Jul-Sep 1993;13(3):198–211. [DOI] [PubMed] [Google Scholar]
- 67.Bordage G. Elaborated knowledge: a key to successful diagnostic thinking. Acad Med. 1994. [DOI] [PubMed] [Google Scholar]
- 68.Patel V, Arocha JF, Kaufman D. Diagnostic reasoning and medical expertise.In Medin, DL Advances in Research and Theory . 1994;31(C):187–252. [Google Scholar]
- 69.Jones M. Clinical reasoning and pain. Man Ther. 1995;1(1):17–24. [DOI] [PubMed] [Google Scholar]
- 70.Arocha JF, Patel VL. Novice diagnostic reasoning in medicine: accounting for evidence. J Learn Sci. 1995;4(4):355–384. [Google Scholar]
- 71.Custers EJFM. The development and function of illness scripts: studies on the structure of medical diagnostic knowledge. Thesis. Maastricht University; 1995. [Google Scholar]
- 72.Van de Wiel M. Knowledge encapsulation:Studies on the deve;opment of medical expertise. thesis.Maastricht university, 1997. [Google Scholar]
- 73.Allen VG, Arocha JF, Patel VL. Evaluating evidence against diagnostic hypotheses in clinical decision making by students, residents and physicians. Int J Med Inform. Aug-Sep 1998;51(2–3):91–105. [DOI] [PubMed] [Google Scholar]
- 74.Chang RW, Bordage G, Connell KJ. COGNITION, CONFIDENCE, AND CLINICAL SKILLS: the importance of early problem representation during case presentations. Acad Med. 1998;73(10):S109–111. [DOI] [PubMed] [Google Scholar]
- 75.Charlin B. Script questionnaires: their use for assessment of diagnostic knowledge in radiology. Med Teach. 1998;20(6):567–571. [Google Scholar]
- 76.Cuthbert L, Duboulay, B., Teather, D., Teather, B., Sharples, M., & Duboulay, G. . Expert/novice differences in diagnostic medical cognition-A review of the literature. University of Sussex Cognitive Science Research paper CSRP #508, Feb. 1999, ISSN 1350–3162. [Google Scholar]
- 77.Kaufman DR, Kushniruk AW, Yale JF, Patel VL. Conceptual knowledge and decision strategies in relation to hypercholesterolemia and coronary heart disease. Int J Med Inform. November 1999;55(3):159–177. [DOI] [PubMed] [Google Scholar]
- 78.Round AP. Teaching clinical reasoning--a preliminary controlled study. Med Educ. July 1999;33(7):480–483. [DOI] [PubMed] [Google Scholar]
- 79.Carter MA, & Robinson, S. S. A narrative approach to the clinical reasoning process in pediatric intensive care: The story of Matthew. J Med Humanit. 2001;22(3):173–194. [Google Scholar]
- 80.Harries PA, Harries C. Studying clinical reasoning, part 2: Applying social judgement theory. Br J Occup Ther. 2001;64(6):285–292. [Google Scholar]
- 81.Elstein AS, Schwartz A. Clinical problem solving and diagnostic decision making: selective review of the cognitive literature. BMJ (Clinical research ed.). March 23 2002;324(7339):729–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nendaz MR, Bordage G. Promoting diagnostic problem representation. Med Educ. August 2002;36(8):760–766. [DOI] [PubMed] [Google Scholar]
- 83.Patel VL, Arocha JF, Kushniruk AW. Patients' and physicians' understanding of health and biomedical concepts: relationship to the design of EMR systems. J Biomed Inform. February 2002;35(1):8–16. [DOI] [PubMed] [Google Scholar]
- 84.Bleakley A, Farrow R, Gould D, Marshall R. Making sense of clinical reasoning: judgement and the evidence of the senses. Med Educ. June 2003;37(6):544–552. [DOI] [PubMed] [Google Scholar]
- 85.Coderre S, Mandin H, Harasym PH, Fick GH. Diagnostic reasoning strategies and diagnostic success. Med Educ. August 2003;37(8):695–703. [DOI] [PubMed] [Google Scholar]
- 86.Norman GR, Eva KW. Doggie diagnosis, diagnostic success and diagnostic reasoning strategies: an alternative view. Med Educ. August 2003;37(8):676–677. [DOI] [PubMed] [Google Scholar]
- 87.Eshach H, Bitterman H. From case-based reasoning to problem-based learning. Acad Med: journal of the Association of American Medical Colleges. May 2003;78(5):491–496. [DOI] [PubMed] [Google Scholar]
- 88.Groves M, O'Rourke P, Alexander H. Clinical reasoning: the relative contribution of identification, interpretation and hypothesis errors to misdiagnosis. Med Teach. November 2003;25(6):621–625. [DOI] [PubMed] [Google Scholar]
- 89.Hardin LE. Research in medical problem solving: a review. J Vet Med Educ. Fall 2003;30(3):230–235. [DOI] [PubMed] [Google Scholar]
- 90.Charlin B, van der Vleuten C. Standardized assessment of reasoning in contexts of uncertainty: the script concordance approach. Eval Health Prof. September 2004;27(3):304–319. [DOI] [PubMed] [Google Scholar]
- 91.Eva KW. What every teacher needs to know about clinical reasoning. Med Educ. January 2005;39(1):98–106. [DOI] [PubMed] [Google Scholar]
- 92.Rikers RM, Van Gerven PW, Schmidt HG. Cognitive load theory as a tool for expertise development. Instr Sci. 2004;32(1–2):173–182. [Google Scholar]
- 93.Verkoeijen PP, Rikers RM, Schmidt HG, van de Wiel MW, Kooman JP. Case representation by medical experts, intermediates and novices for laboratory data presented with or without a clinical context. Med Educ. June 2004;38(6):617–627. [DOI] [PubMed] [Google Scholar]
- 94.Tamayo-Sarver JH, Dawson NV, Hinze SW, Cydulka RK, Wigton RS, Baker DW. Rapid clinical decisions in context: a theoretical model to understand physicians’ decision-making with an application to racial/ethnic treatment disparities Health Care Services, Racial and Ethnic Minorities and Underserved Populations: Patient and Provider Perspectives: Emerald Group Publishing Limited; 2005:183–213. [Google Scholar]
- 95.Anderson KJ. Factors affecting the development of undergraduate medical students' clinical reasoning ability. Thesis. The university Adelaide. 2006. [Google Scholar]
- 96.Bowen JL. Educational strategies to promote clinical diagnostic reasoning. N Engl J Med. November 23 2006;355(21):2217–2225. [DOI] [PubMed] [Google Scholar]
- 97.Eva KW, Cunnington JP. The difficulty with experience: does practice increase susceptibility to premature closure? J Contin Educ Health Prof. Summer 2006;26(3):192–198. [DOI] [PubMed] [Google Scholar]
- 98.Mongtomery K. How doctors think: Clinical judgment and the practice of medicine. Oxford, United states: New York: Oxford University Press; 2005. [Google Scholar]
- 99.Novak K, Mandin H, Wilcox E, McLaughlin K. Using a conceptual framework during learning attenuates the loss of expert-type knowledge structure. BMC Med Educ. July 18 2006;6:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Thornton T. Tacit knowledge as the unifying factor in evidence based medicine and clinical judgement. PHILOS ETHICS HUM ME. March 17 2006;1(1):E2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Auclair F. Problem formulation by medical students: an observation study. BMC med educ. June 17 2007;7:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Schmidt HG, Rikers RM. How expertise develops in medicine: knowledge encapsulation and illness script formation. Med Educ. December 2007;41(12):1133–1139. [DOI] [PubMed] [Google Scholar]
- 103.Banning M. A review of clinical decision making: models and current research. J Clin Nurs. January 2008;17(2):187–195. [DOI] [PubMed] [Google Scholar]
- 104.Heiberg Engel PJ. Tacit knowledge and visual expertise in medical diagnostic reasoning: implications for medical education. Med Teach. 2008;30(7):e184–188. [DOI] [PubMed] [Google Scholar]
- 105.Humbert A. 15 Assessing the Clinical Reasoning Skills of Emergency Medicine Clerkship Students Using a Script Concordance Test. Acad Emerg Med. 2008;15:S230–S231. [DOI] [PubMed] [Google Scholar]
- 106.Facione NC, Facione PA. Critical thinking and clinical judgment Critical thinking and clinical reasoning in the health sciences: A teaching anthology. US, Millbrae, California Academic Press, 2008:1–13. [Google Scholar]
- 107.Vertue FM, Haig BD. An abductive perspective on clinical reasoning and case formulation. J Clin Psychol. September 2008;64(9):1046–1068. [DOI] [PubMed] [Google Scholar]
- 108.Braude HD. Clinical intuition versus statistics: different modes of tacit knowledge in clinical epidemiology and evidence-based medicine. Theor Med Bioeth. 2009;30(3):181–198. [DOI] [PubMed] [Google Scholar]
- 109.Bissessur SW, Geijteman EC, Al-Dulaimy M, et al. Therapeutic reasoning: from hiatus to hypothetical model. J Eval Clin Pract. December 2009;15(6):985–989. [DOI] [PubMed] [Google Scholar]
- 110.Carriere B, Gagnon R, Charlin B, Downing S, Bordage G. Assessing clinical reasoning in pediatric emergency medicine: validity evidence for a Script Concordance Test. Annals of emergency medicine. May 2009;53(5):647–652. [DOI] [PubMed] [Google Scholar]
- 111.Rehder B, Kim S. Classification as diagnostic reasoning. Mem Cognit. 2009;37(6):715–729. [DOI] [PubMed] [Google Scholar]
- 112.Vosniadou S. International handbook of research on conceptual change. United states: New York. Routledge; 2009. [Google Scholar]
- 113.Aleluia IM, Carvalho PM, Jr., Menezes MS. A way to assess students' clinical reasoning. Med Educ. November 2010;44(11):1145–1146. [DOI] [PubMed] [Google Scholar]
- 114.Corcoran J, Walsh J. Clinical assessment and diagnosis in social work practice. Oxford, United states: New York: Oxford University; 2010. [Google Scholar]
- 115.Mariasin M. Novice, Generalist, and Expert Reasoning During Clinical Case Explanation: A Propositional Assessment of Knowledge Utilization and Application, thesis.University of Waterloo; 2010. [Google Scholar]
- 116.Lee A, Joynt GM, Lee AK, et al. Using illness scripts to teach clinical reasoning skills to medical students. Fam Med. 2010;42(4):255–261. [PubMed] [Google Scholar]
- 117.Elizondo-Omana RE, Morales-Gomez JA, Morquecho-Espinoza O, et al. Teaching skills to promote clinical reasoning in early basic science courses. Anat Sci Educ. Sep-Oct 2010;3(5):267–271. [DOI] [PubMed] [Google Scholar]
- 118.Wilhelmsson N. From basic science knowledge to clinical understanding. Thesis. Karolinska Institutet,2010. [Google Scholar]
- 119.Amini M, Moghadami M, Kojuri J, et al. An innovative method to assess clinical reasoning skills: Clinical reasoning tests in the second national medical science Olympiad in Iran. BMC Res Notes. October 17 2011;4:418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Durning S, Artino AR, Jr., Pangaro L, van der Vleuten CP, Schuwirth L. Context and clinical reasoning: understanding the perspective of the expert's voice. Med Educ. September 2011;45(9):927–938. [DOI] [PubMed] [Google Scholar]
- 121.Franklin A, Liu Y, Li Z, et al. Opportunistic decision making and complexity in emergency care. J Biomed Inform. Jun 2011;44(3):469–476. [DOI] [PubMed] [Google Scholar]
- 122.Adams JR, Elwyn G, Legare F, Frosch DL. Communicating with physicians about medical decisions: a reluctance to disagree. Arch Intern Med. August 13 2012;172(15):1184–1186. [DOI] [PubMed] [Google Scholar]
- 123.Ashoorion V, Liaghatdar MJ, Adibi P. What variables can influence clinical reasoning? J Res Med Sci: the official journal of Isfahan University of Medical Sciences. 2012;17(12):1170. [PMC free article] [PubMed] [Google Scholar]
- 124.van Bruggen L, Manrique-van Woudenbergh M, Spierenburg E, Vos J. Preferred question types for computer-based assessment of clinical reasoning: a literature study. Perspect Med Educ. November 2012;1(4):162–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Charlin B, Lubarsky S, Millette B, et al. Clinical reasoning processes: unravelling complexity through graphical representation. Med Educ. May 2012;46(5):454–463. [DOI] [PubMed] [Google Scholar]
- 126.Demirören M, Palaoğlu Ö. Assessment of Medical Student’s Clinical Reasoning Skills in the Problem Based Learning-Integrated Curriculum. J Ankara Univ Fac Med. 2012, 65 (2) [Google Scholar]
- 127.Braude HD. Intuition in medicine: A philosophical defense of clinical reasoning. US: Chicago: University of Chicago Press; 2012. [Google Scholar]
- 128.Braude HD. Conciliating cognition and consciousness: the perceptual foundations of clinical reasoning. J Eval Clin Pract. 2012;18(5):945–950. [DOI] [PubMed] [Google Scholar]
- 129.Khatami S, MacEntee MI, Pratt DD, Collins JB. Clinical reasoning in dentistry: a conceptual framework for dental education. J Dent Educ. September 2012;76(9):1116–1128. [PubMed] [Google Scholar]
- 130.Nouh T, Boutros M, Gagnon R, et al. The script concordance test as a measure of clinical reasoning: a national validation study. Am J Surg. April 2012;203(4):530–534. [DOI] [PubMed] [Google Scholar]
- 131.Shaban R. Theories of clinical judgment and decision-making: A review of the theoretical literature. AJP. 2015;3(1). [Google Scholar]
- 132.Audetat MC, Laurin S, Sanche G, et al. Clinical reasoning difficulties: a taxonomy for clinical teachers. Med Teach. 2013;35(3):e984–989. [DOI] [PubMed] [Google Scholar]
- 133.Da Silva A. Clinical reasoning development in medical students: An educational and transcultural comparative study, PhD thesis, University of; 2013. [Google Scholar]
- 134.Gigante J. Teaching Clinical Reasoning Skills to Help your Learners “Get” the Diagnosis. Pediat Therapeut, 2013;3(4). [Google Scholar]
- 135.Kriewaldt J, Turnidge D. Conceptualising an approach to clinical reasoning in the education profession. AJTE. 2013;38(6):7. [Google Scholar]
- 136.Lubarsky S, Dory V, Duggan P, Gagnon R, Charlin B. Script concordance testing: from theory to practice: AMEE guide no. 75. Med Teach. 2013;35(3):184–193. [DOI] [PubMed] [Google Scholar]
- 137.Munshi FM, AlJarallah BM, Harasym PH. Problem Solving Strategy and Diagnostic Performance at Three Expertise Levels: Does the Problem Solving Approach Matter? J Health Educ Res Dev. 2013. [Google Scholar]
- 138.Smith M, Loftus S, Levett-Jones T. Teaching clinical reasoningIn: Loftus, S., Gerzina, T., Higgs, J., Smith, M., & Duffy, E. Educating Health Professionals: Dordrecht, Netherlands: SensePublishers; 2013:269–276. [Google Scholar]
- 139.Weiss MJ, Bhanji F, Fontela PS, Razack SI. A preliminary study of the impact of a handover cognitive aid on clinical reasoning and information transfer. Med Educ. August 2013;47(8):832–841. [DOI] [PubMed] [Google Scholar]
- 140.Ilgen JS, Bowen JL, McIntyre LA, et al. Comparing diagnostic performance and the utility of clinical vignette-based assessment under testing conditions designed to encourage either automatic or analytic thought. Acad Med. October 2013;88(10):1545–1551. [DOI] [PubMed] [Google Scholar]
- 141.Bowen L. J, S. Ilgen J. Now You See It, Now You Don't: What Thinking Aloud Tells Us About Clinical Reasoning. J Grad Med Educ. 2014;6(4):783–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Delany C, Golding C. Teaching clinical reasoning by making thinking visible: an action research project with allied health clinical educators. BMC Med Educ. January 30 2014;14:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Freiwald T, Salimi M, Khaljani E, Harendza S. Pattern recognition as a concept for multiple-choice questions in a national licensing exam. BMC Med Educ. 2014;14(1):232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Geisler PR, Hummel C, Piebes S. Evaluating evidence-informed clinical reasoning proficiency in oral practical examinations. Athl Train Educ J. 2014;9(1):43–48. [Google Scholar]
- 145.Gordon M. Manual of nursing diagnosis. Jones & Bartlett Publishers; 2014. [Google Scholar]
- 146.Holmboe ES, Durning SJ. Assessing clinical reasoning: moving from in vitro to in vivo. Diagnosis (Berlin, Germany). January 1 2014;1(1):111–117. [DOI] [PubMed] [Google Scholar]
- 147.Hrynchak P, Takahashi SG, Nayer M. Key-feature questions for assessment of clinical reasoning: a literature review. Med Educ. September 2014;48(9):870–883. [DOI] [PubMed] [Google Scholar]
- 148.Hochberg L, Alm CO, Rantanen EM, DeLong CM, Haake A. Decision style in a clinical reasoning corpus. Proceedings of BioNLP 2014. USA. Baltimore, Maryland 2014:83–87. [Google Scholar]
- 149.Hochberg L, Alm CO, Rantanen EM, Yu Q, DeLong CM, Haake A. Towards automatic annotation of clinical decision-making style Paper presented at: Proceedings of LAW VIII-The 8th Linguistic Annotation Workshop. Ireland, Dublin, 2014. [Google Scholar]
- 150.The Monajemi A. Role of Biomedical Knowledge in Clinical Reasoning: Bridging the Gap between Two Theories. IJBMC. 2014;1(2):102–106. [Google Scholar]
- 151.Roots, S. A. Clinical reasoning in osteopathy: an investigation of diagnostic hypothesis generation for patients with acute low back pain . Thesis. Unitec Institute of Technology; 2014. [Google Scholar]
- 152.Salkeld EJ. Framework negotiations: diagnostic insights among alternative medical practitioners participating in integrative medicine case conferences. Med Anthropol Q. March 2014;28(1):44–65. [DOI] [PubMed] [Google Scholar]
- 153.Smith CS, Hill W, Francovich C, et al. Diagnostic Reasoning across the Medical Education Continuum. Healthcare (Basel, Switzerland). July 15 2014;2(3):253–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Capaldi VF, Durning SJ, Pangaro LN, Ber R. The clinical integrative puzzle for teaching and assessing clinical reasoning: preliminary feasibility, reliability, and validity evidence. Mil Med. April 2015;180(4 Suppl):54–60. [DOI] [PubMed] [Google Scholar]
- 155.Teaching Clinical Gaba A. Judgment: A Review with Consideration of Applications for Health Professions. Open Nutr J. 2015;9(1). [Google Scholar]
- 156.Islam R, Weir CR, Jones M, Del Fiol G, Samore MH. Understanding complex clinical reasoning in infectious diseases for improving clinical decision support design. BMC Med Inform Decis Mak. November 30 2015;15:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Lafleur A, Cote L, Leppink J. Influences of OSCE design on students' diagnostic reasoning. Med Educ. February 2015;49(2):203–214. [DOI] [PubMed] [Google Scholar]
- 158.Lubarsky S, Dory V, Audetat MC, Custers E, Charlin B. Using script theory to cultivate illness script formation and clinical reasoning in health professions education. Can Med Educ J. 2015;6(2):e61–70. [PMC free article] [PubMed] [Google Scholar]
- 159.Park WB, Kang SH, Lee YS, Myung SJ. Does Objective Structured Clinical Examinations Score Reflect the Clinical Reasoning Ability of Medical Students? Am J Med Sci. Jul 2015;350(1):64–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Lisk K, Agur AM, Woods NN. Exploring cognitive integration of basic science and its effect on diagnostic reasoning in novices. Perspect Med Educ. June 2016;5(3):147–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.McBee E, Ratcliffe T, Goldszmidt M, et al. Clinical Reasoning Tasks and Resident Physicians: What Do They Reason About? Acad Med : journal of the Association of American Medical Colleges. Jul 2016;91(7):1022–1028. [DOI] [PubMed] [Google Scholar]
- 162.Gruppen LD. Clinical Reasoning: Defining It, Teaching It, Assessing It, Studying It. West J Emerg Med. January 2017;18(1):4–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Jarodzka H, Boshuizen HP. Unboxing the Black Box of Visual Expertise in Medicine. Frontline learn research. 2017;5(3):167–183. [Google Scholar]
- 164.Norman GR, Monteiro SD, Sherbino J, Ilgen JS, Schmidt HG, Mamede S. The Causes of Errors in Clinical Reasoning: Cognitive Biases, Knowledge Deficits, and Dual Process Thinking Acad Med: journal of the Association of American Medical Colleges. Jan 2017;92(1):23–30. [DOI] [PubMed] [Google Scholar]
- 165.ten Cate O, Durning SJ. Understanding Clinical Reasoning from Multiple Perspectives: A Conceptual and Theoretical Overview In: ten Cate O, Custers E, Durning SJ, eds. Principles and Practice of Case-based Clinical Reasoning Education: A Method for Preclinical Students. Switzerlan, Cham, Springer: 2018:35–46. [Google Scholar]
- 166.Zamani S, Amini M, Masoumi SZ, Delavari S, Namaki MJ, Kojuri J. The comparison of the key feature of clinical reasoning and multiple choice examinations in clinical decision makings ability. Biomed Re. 2017;28(3):1115–1119. [Google Scholar]
- 167.Bowen JL, ten Cate O. Prerequisites for Learning Clinical Reasoning In: ten Cate O, Custers E, Durning SJ, eds. Principles and Practice of Case-based Clinical Reasoning Education: A Method for Preclinical Students. Switzerlan, Cham, Springer: 2018:47–63. [PubMed] [Google Scholar]
- 168.Custers EJ. Training Clinical Reasoning: Historical and Theoretical BackgroundIn: In: ten Cate O, Custers E, Durning SJ, eds. Principles and Practice of Case-based Clinical Reasoning Education: A Method for Preclinical Students. Switzerlan, Cham, Springer; 2018:21–33. [PubMed] [Google Scholar]
- 169.King L, Kremser S, Deam P, et al. Clinical reasoning in osteopathy: Experiences of novice and experienced practitioners. INT J OSTEOPATH MED. 2018;28:12–19. [Google Scholar]
- 170.Keemink Y, Custers E, van Dijk S, Ten Cate O. Illness script development in pre-clinical education through case-based clinical reasoning training. Int J Med Educ. February 9 2018;9:35–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Lopes HF, Polson NG. Bayesian hypothesis testing: Redux. Cornel university.arXiv preprint arXiv:1808.08491. 2018. [Google Scholar]
- 172.Yazdani S, Abardeh MH. Clinical Reasoning in Medicine: A Concept Analysis. JMED. 2017;16(3). [Google Scholar]
- 173.Yazdani S, Hosseinzadeh M, Hosseini F. Models of clinical reasoning with a focus on general practice: A critical review. J Adv Med Educ Prof. October 2017;5(4):177–184. [PMC free article] [PubMed] [Google Scholar]
- 174.Higgs J. Judgment and reasoning in professional contexts. In: Lanzer, P. ed., 2018. Textbook of Catheter-Based Cardiovascular Interventions: A Knowledge-Based Approach. Springer. 2018:15–25. [Google Scholar]