Abstract
Since the description of femoroacetabular impingement (FAI) by Ganz in 2003, our understanding of the pathophysiology, management options, and outcomes has evolved and literature continues to be generated on this condition at a rapid rate. FAI has been identified as a primary source of hip pain as well as a generator of secondary osteoarthritis. Improvements in the radiographic detection of cam and pincer morphologies as well as a better understanding of the structural impact of these morphologies have led to improved preoperative planning. Advancements in hip arthroscopy techniques have also led to a higher rate of arthroscopic management of this condition over the initially described open surgical dislocation technique. While arthroscopic management of this condition has become the most common form of surgical management for FAI, inadequate bony resection has been shown to be a frequent source of revision surgery. Therefore, roles for open surgical dislocation and combined mini-open approaches remain, particularly in cases where concern for the inability to fully access the morphology arthroscopically exists.
Keywords: impingement, hip pain, femur impingement, acetabular impingement, cam lesion, pincer lesion
Background
Over the past 20 years, femoroacetabular impingement (FAI) syndrome has emerged as a source of pre-arthritic hip pain as well as a source of secondary hip osteoarthritis (OA). While early work dating back to 1936 had speculated that abnormal proximal femur and acetabular anatomy could lead to OA, it was not until the work by Ganz et al in 2003 that the term FAI was coined and identified as a leading source of early OA.1–3 Ganz et al proposed FAI as a “mechanism for the development of early osteoarthritis for most nondysplastic hips” based on their clinical experience performing and analyzing over 600 surgical hip dislocations.4 They described both proximal femoral lesions (“cam” lesions) and acetabular rim lesions (“pincer” lesions) as contributing factors to early OA and initial treatment involved an open surgical hip dislocation through a trochanteric flip approach with femoral and/or acetabular osteotomy.
Since 2003, extensive research around FAI has been published and our understanding of the condition has substantially evolved. A systematic review in 2014 demonstrated a 5-fold increase in publications related to FAI from 2005 to 2010.5 Advancements in pathophysiology, imaging, management, and outcomes have all been demonstrated and continue to grow. Here, we present a review of the literature regarding the current understanding of FAI pathophysiology, physical exam, imaging, nonoperative management, operative management, and outcomes.
Pathophysiology
FAI involves a spectrum of structural morphologies that contribute to a misshapen hip joint which can lead to eccentric loading, breakdown of intra-articular structures, pain, and early osteoarthritis.6,7 FAI is defined as:
abnormal contact between the proximal femur and acetabular rim that occurs during terminal motion of the hip leading to lesions of the acetabular labrum and/or the adjacent acetabular cartilage.8
Three different types of impingement have been identified including cam (femoral), pincer (acetabular), and combined. While initially these were referred to as lesions and/or deformities, in 2015, Frank et al performed a systematic review of asymptomatic volunteers and found that in 2114 asymptomatic hips, 37% demonstrated a cam deformity, and 67% demonstrated a pincer deformity. This has led us to favor the terms cam and/or pincer “morphology” over the term “lesion” given it prevalence in the asymptomatic population.9 Furthermore, FAI should not be used synonymously with cam or pincer morphology but rather used to refer to patients with symptomatic cam, pincer, or combined morphologies.
Cam morphology refers to the loss of sphericity at the femoral head–neck junction which leads to a decrease in the head–neck ratio resulting in impingement.6,7 Pincer morphology refers to an excessive prominence of the anterolateral rim of the acetabulum resulting in impingement. The cam morphology is most commonly located along the anterosuperior aspect of the proximal femur which generates damage to the anterolateral acetabular articular cartilage with repetitive deep flexion and internal rotation.10 The pincer morphology results in compression of the labrum between the prominent rim of the acetabulum and the femoral neck during deep flexion. Beck et al found that in cam impingement, the shear forces on the articular cartilage lead to chondral injury and delamination with relative preservation of the labrum in the early stages. When progression to a labral tear does occur, it is typically a detachment from the transition-zone cartilage rather than an intrasubstance tear.10 This is in contrast with pincer morphology which was found to initially result in injury to the anterosuperior labrum including degeneration, ossification, and tearing.7,10
Epidemiology
With the increasing awareness of femoroacetabular impingement as a source of hip pain, it is being diagnosed in patients ranging from early childhood through late adulthood. Cam morphology is most commonly seen in young active male patients while pincer morphology is most commonly seen in middle-aged women.11 Clohisy et al performed a multicenter prospective longitudinal cohort study to assess the epidemiology of FAI morphologies and found that in 1130 hips reviewed, 47.6% demonstrated cam morphology, 44.5% combined morphology, and 7.9% had pincer morphologies.12
The origin of FAI is likely multifactorial including both a genetic predisposition and activity-related risk factors. Pollard et al looked at genetics as a source of this morphology through analysis of siblings and did find a correlation including a relative risk of 2.8 and 2.0 for cam-type and pincer type deformities, respectively.13 Other studies have demonstrated a higher rate of FAI in elite athletes compared to the general population and further analysis of adolescent athletes, in particular, have actually shown that cam deformities can be generated through sport activities and increase in size through the time of physeal closure.14,15
Presentation
FAI typically initially present as an insidious onset of anterior groin pain that is exacerbated with rigorous activities such as sports or prolonged walking.4 Patients may report pain with deep flexion or self-describe the positions that generate impingement. When asked where they are having pain the patient may display a “C” sign in which the patient’s hand is cupped above the greater trochanter with the fingers gripping into the anterior groin.7 Often, the presentation is vague and requires a high index of suspicion, a thorough physical exam, and proper imaging studies to identify the morphology.
Physical exam
Young patients presenting with hip pain can make for a difficult diagnosis and require a thorough physical exam to elucidate the underlying pathology. When assessing the patient’s hip range of motion, typically, decreased internal rotation is noticed secondary to alterations in the bony architecture of the hip.7 It should also be noted that some patients may have decreased internal rotation with the hip flexed to 90° without actually having clinical impingement. If patients present with a symptomatic hip, the range of motion should be compared to the contralateral side as the morphology of the bony hip deformity is often present bilaterally.7
There have been many described physical exam tests to help with the diagnosis of FAI, several of which are outlined below. Often times, a diagnosis of FAI is difficult to be elicited by a single test. Although these tests may suggest FAI to a clinician, it has been shown that physical exam tests alone are not sufficient enough to readily confirm or exclude FAI as a diagnosis.16
The anterior impingement test is performed by flexing the hip to 90°, adducting and internally rotating the hip. With this test, the anterior femoral neck impinges upon the anterosuperior acetabulum which results in reproduction of the pain seen in femoroacetabular impingement. This test has been shown to have high specificity and positive predictive value for intra-articular hip pathology.17,18 The posterior impingement test can elicit posterior impingement and is performed with the patient supine on the exam table, the leg is maximally extended and externally rotated resulting in posterior hip pain. Global pathology or over coverage may result in a positive posterior impingement test.
The FABER test of the hip is performed with the patient lying supine and the hip is placed into the figure of four position with the hip flexed, abducted, and externally rotated with the contralateral pelvic being stabilized. A downward, external rotation force is applied to the leg being tested and the distance from the ipsilateral knee to the exam table is measured. This distance is compared to the distance on the contralateral side. This test is considered positive if there is any difference in the distance between either hip. Maslowski et al showed the FABER test to have high sensitivity (81%) and low specificity (25%) for intra-articular hip pathology.19
Internal rotation over pressure (IROP test) is performed with the patient lying supine and the affected leg is brought into flexion and internal rotation with an axial force directed through the knee. A positive test produces pain. Maslowski et al showed high sensitivity (88%) and low specificity (17%) with this test for intra-articular hip pathology.19
Lateral rim impingement test is performed by taking the affected leg from flexion to extension with the leg abducted and externally rotated. Reproduction of pain signifies a positive test.
Scour test is performed with the patient flexing the affected hip to approximately 90°. An axial force is applied to the leg, and the hip is abducted and externally rotated, the leg is then taken to adduction and internal rotation. Pain or diminished motion represents a positive test. This test has been shown to have low sensitivity and specificity for FAI in the literature.19
Stinchfield test may also be positive in FAI and is performed with the affected leg raised to approximately 45° and the patient resists a downward force with reproduction of pain signifying a positive test. This test has been shown to have low sensitivity and specificity for FAI in the literature.16
When examining a patient with suspected FAI, the clinician should keep in mind some conditions can mimic FAI such as trochanteric bursitis, athletic pubalgia, snapping hip syndrome, tight IT band, flexor muscle strain, hip subluxation in hip dysplasia, soft tissue tumors, and femoral neck stress fractures.
Imaging
If the symptoms and exam suggest FAI may be present, then imaging can be considered. Typically, radiographs are obtained first. Standard imaging includes anteroposterior (AP) radiograph of the pelvis and lateral view of the involved hip. It should be noted that it is very important for the AP view to be well balanced in terms of rotation and tilt (Figure 1). Proper rotation is seen with the tip of the coccyx being in line with the pubic symphysis. Proper tilt is confirmed by the tip of the coccyx being approximately 1–2 cm from the superior border of the pubic symphysis. Radiographs can provide valuable information to the clinician in regards to a patient’s hip pain. The presence or absence of signs of arthritis should be noted by the physician.
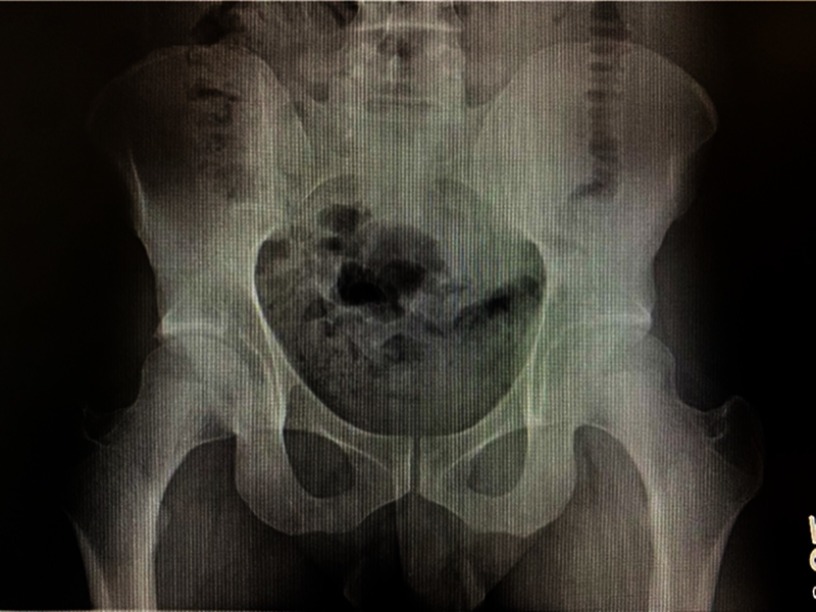
Figure 1.
Anteroposterior pelvis radiograph in good position and orientation.
In FAI, patients may have over coverage of the anterior superior acetabulum which is referred to as a pincer lesion. The pincer lesion can then impinge on the femoral neck. Acetabular retroversion has been associated with this over coverage. Radiographically, acetabular retroversion is suggested by a crossover sign. The crossover sign has been shown to be the most cited radiographic sign used to assess for pincer type impingement, although recent literature has suggested the crossover sign may overestimate acetabular retroversion.20 Acetabular retroversion may also be suggested by a shallow posterior wall. Radiographically, this appears as the border of the posterior wall lying medially to the center of rotation of the femoral head. A prominent ischial spine is another radiographic sign that can be seen with acetabular retroversion. These radiographic findings have been shown in the literature to have only moderate intra-observer reliability.21
Global over coverage of the acetabulum can be seen with coxa profunda and acetabular protrusio and may be associated with pincer type impingement. Coxa profunda is suggested if the floor of the acetabular fossa is medial to the ilioischial line. Additionally, a false profile view can show anterior acetabulum over coverage. Recent studies have suggested coxa profunda can be a normal finding in patients and is not necessary nor sufficient to diagnose pincer type impingement.22 Radiographically, acetabular protrusio is seen when the femoral head is medial to the ilioischial line. Protrusio is important to note on pre operative radiographs as it has been shown to be associated with worse outcomes following surgical intervention for FAI.23
When evaluating the acetabulum, lateral center-edge angle (LCE) is measured by the angle formed from a line from the center of the femoral head to the lateral edge of the acetabulum and a vertical reference line from the center of the femoral head. Although there is controversy regarding the threshold values for this angle, it has been suggested that between 35° and 40° may suggest pincer type impingement and any value >40° may suggest protrusio.20 The LCE has been shown to have high inter-observer reliability and has been shown to correlate with pincer type impingement.24,25
Acetabular index is defined by the angle of a line from the medial to the lateral edge of the acetabulum and a horizontal reference. Tannast et al suggested a normal range of 3°–13° for acetabular index.26 Values less than 3° suggest acetabular over coverage.26
Cam lesions are often seen in patients with FAI and are represented by a convex lesion on the anterosuperior portion at the femoral head–neck junction where there is typically a concave slope. Evaluation of the femur for cam lesions should include AP and lateral views of the involved hip. (Figures 1 and 2). Some controversy exists about the optimal lateral radiograph. Cross-table lateral and Dunn views are popular views to evaluate the sphericity of the femoral head. Meyer et al showed that a Dunn view in 45° or 90° of flexion and a cross-table lateral in internal rotation best show the femoral head/neck junction.27 It should be noted that because of the variability of the shape and location of a cam lesion, no radiograph is consistently reliable and may not show the extent of a cam lesion.
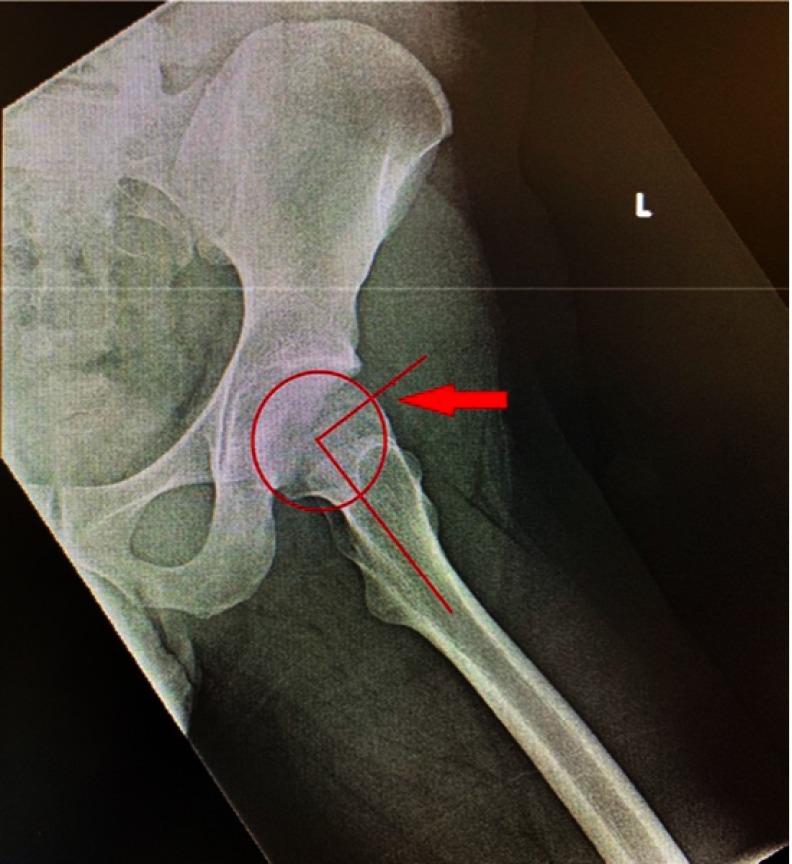
Figure 2.
A lateral radiograph demonstrates a prominent head–neck junction, indicating a CAM lesion (arrow). The alpha angle is 85 degrees.
When evaluating a cam lesion radiographically, the classic “pistol grip” deformity is seen on the AP radiograph. The alpha angle is typically used to quantitate the severity of the cam lesion. On a lateral view, a circle is drawn around the femoral head, a line is drawn down the axis of the femoral neck, and a second line is drawn from the center of the femoral head to the point where the femoral head is outside of the circle (Figure 2). Notzli et al showed a value above 50° is associated with cam lesion impingement in FAI.28 Femoral head–neck offset is another measurement used to define cam lesions and is the distance between a parallel line down the center of the femoral neck and a parallel line that passes through the point where the femoral head–neck contour exceeds the femoral head radius divided by the diameter of the femoral head.29 A ratio of less than 0.17 is suggestive of a cam deformity.
Magnetic resonance imaging
Magnetic resonance imaging (MRI) is often used in the pre operative evaluation of patients with FAI. When considering MRI for evaluation of FAI, physicians should consider MRI with intra-articular gadolinium (MRA) as this provides intra-articular contrast which allows better sensitivity for evaluating and detecting intra-articular pathology, especially with 1.5 Tesla MRIs. Additionally, injection of long-acting anesthetic with the contrast can provide useful information for the physician depending on if the patient experiences relief of their symptoms after the injection. If the physician has access to a 3.0 Tesla MRI, then contrast may not be necessary to visualize intra-articular pathology as the 3.0 Tesla MRI has been shown to be at least equivalent and possibly superior to 1.5 Tesla MRA for identifying hip pathology.30
MRI/MRA allows for evaluation of pathology associated with FAI that is unable to be seen on radiographs. Labral lesions are common with FAI and are able to be evaluated with MRI/MRA (Figure 3A). Cartilage lesions are also common in FAI and can be seen and characterized by MRI/MRA, with a higher sensitivity of detection with MRA.29 Bony morphology of the acetabulum and femur can also be evaluated with MRI/MRA (Figure 3B).
Figure 3.

(A) MR arthrogram of the left hip demonstrating a labral tear (arrow). (B) MR arthrogram of the left hip demonstrating a large cam lesion (arrow).
Non operative management
Conservative management of FAI has been described in the literature. Emara et al showed short-term improvement with adapting of activities of daily living to a safe range of motion as to avoid impingement.31 Asymptomatic patients should be treated with conservative management with follow-up for the development of impingement symptoms. In patients who have mild symptoms, early conservative management can be considered with an emphasis on physical therapy and activity modification.32 With physical therapy, focus should be on improving core strength and identifying and improving any decompensatory disorders secondary to compensation for chronic impingement.7 Identifying and modifying any activities that cause impingement, such as squats, is crucial for conservative management of FAI. Patients with severe FAI or athletes who may not be able to modify their activities in a way to prevent impingement should be identified early by physicians as they may fail conservative management leading to continued symptomatology and potentially deleterious effects on the joint.
Operative management
Indication for surgical management for FAI is a complicated issue for surgeons. Literature has shown there is inconsistency regarding indications for surgery.33 Some commonly cited reasons for proceeding with surgery include failure of non operative management, symptoms and pain for greater than 6 months, series of positive special tests, signs of FAI on radiographs, MRI and/or CT scans.33 For hip arthroscopy, an absolute contraindication includes joint space narrowing <2 mm. Relative contraindications for surgery include osteoarthritis of the hip, advanced age, ligamentous laxity and morbid obesity.34–36 It should be discussed with patients prior to surgery that due to the diagnosis of FAI, they may develop further progression which could lead to osteoarthritis necessitating a total hip arthroplasty in the future.
Open surgical hip dislocation
Open surgical hip dislocation was the first described surgical treatment of FAI and was once considered the “gold standard”.37 This approach has shown good results in the literature. Nwachukwu et al showed in a recent systematic review that patients who underwent open hip dislocation had equivalent medium-term survival rates when compared to hip arthroscopy.38 Open hip dislocation has advantages when compared to other approaches in that it provides 360° visualization of the femoral head and acetabulum thus allowing the surgeon to address all pathology associated with FAI and allows for templating of the femoral aspect to allow for precise sphericity.37 It is a larger operation when compared to other techniques and has been shown to result in more blood loss, more extensive soft tissue dissection, increased blood loss and longer rehabilitation when compared to mini-open and arthroscopic techniques. It requires a trochanteric osteotomy which may result in nonunion and hardware pain.37
Combined approach (mini-open arthroscopic assisted)
With this technique, the intra-articular pathology associated with FAI is addressed arthroscopically. The cam lesion is then addressed via a mini-open approach thus avoiding the need for a trochanteric osteotomy. This approach is efficacious in that it has been shown to improve hip scores postoperatively. Laude et al showed an improvement in the non-arthritic hip score (NAHS) by 29.1 points.39 Ribas et al also showed improvement in WOMAC scores in patients with Tonnis grade 1–2 following mini-open treatment.40 In regards to high-performance level activities, Tokish et al showed a low rate of return to military active duty following mini-open arthroscopic assisted treatment of FAI.41 A recent meta-analysis was done which showed the combined approach was associated with increased complication rate and increased revision surgery rate when compared to arthroscopy and open hip dislocation. Lateral femoral cutaneous nerve neuropraxia was higher in the combined approach when compared to arthroscopy and open hip dislocation. The most common reason for revision surgery was continued pain.37
Arthroscopy
Arthroscopic treatment of FAI provides a less invasive option and has become a very popular surgical option. Griffin et al showed, in a multicenter randomized trial, the patients undergoing hip arthroscopy improved to a greater degree than patients who did physical therapy.42 When treating patients arthroscopically, the articular and labral components can be addressed through the central compartment, whereas the cam lesion is typically more peripherally located and can be addressed through the peripheral compartment. Arthroscopic treatment has been shown to be very effective at treating the pathology associated with FAI. Byrd and Jones reported on 200 patients who underwent hip arthroscopy for FAI and found an average increase of 20 points in the Harris hip score.43 In a recent meta-analysis of 1981 hips, Minkara et al showed that after hip arthroscopy, 87.7% of the patients returned to sport after surgery with any increase in Hip Outcome Score by 41.7 points and modified Harris hip score by 24.4 points.44 O’Connor et al showed a return to sports rate of 84.6% in their meta-analysis of 1442 hips in 1296 patients with an increase of modified Harris hip score by nearly 20 points.45 Adolescent patients have also been found to benefit from hip arthroscopy. Byrd et al also showed arthroscopy resulted in a 25.4-point increase in Harris hip score in adolescent patients.46 Botser et al showed that patients who underwent hip arthroscopy had a higher rate of return to sport in professional athletes than patients who underwent open hip dislocation.37
In patients with labral tears, labral repair has been shown to have improved outcomes when compared to labral debridement.47,48 Thus, we recommend labral repair for labral tears when able to be performed. As technology continues to evolve, various techniques have been proposed for labral repair; however, there has been no consensus for optimal repair technique. When treating these patients, in addition to labral repair, adequate acetabuloplasty must also be performed in order to address the underlying pincer pathology.49 Cam lesion bony resection is also a very important component of surgical intervention (Figure 4A and B). As shown by previous studies, inadequate bony resection is a common reason for revision surgery.50,51 For larger pincer lesions, often times the labrum must be detached in order to fully address the underlying pathology.52 In patients who do not have sufficient labrum, an evolving treatment option that has been shown to have success is labral reconstruction.53–55
Figure 4.

(A) Anteroposterior radiography of left hip demonstrating post resection of cam lesion (arrow). (B) Lateral radiograph of the same patient with clear evidence of large cam lesion excision (arrow).
In addition to higher rate of return to play, when compared to open hip dislocation, patients who underwent hip arthroscopy have been shown to return to sport earlier.37 Time to return following hip arthroscopy has not been well established in the literature. O’Connor et al showed that the average time to return to play was 7.4 months following surgery. In the same meta-analysis, O’Connor et al showed that the majority of studies produced recommended protocol for return to play between 3 and 4 months postoperatively.45 The discrepancy was felt to be secondary to heterogeneous patient population with protocols and study designs catered more for athletic populations rather than recreational or non-athletic patients. Currently, return to play protocols have high variability from surgeon to surgeon and there is no validated functional assessment for return to play following hip arthroscopy.
Management of the capsule is a topic that has been debated in the literature. Several studies have shown that capsular repair results in improved stability and improved function following hip arthroscopy. Frank et al showed that patients who had complete capsular repair had higher sport specific outcomes when compared to patients who had partial repair of the capsule. Additionally, there was a 13% revision rate in patients undergoing partial repair and a 0% revision rate in the complete capsular repair group.56 Wylie et al reported on 33 patients who required revision hip arthroscopy due to symptomatic instability after no capsular repair was done at the time of the index procedure. Following capsular repair at the time of revision, all patients had improvement in patient-reported outcomes at two years.57 Ortiz-Declet et al, in a systematic review, suggested that routine capsular closure may result in superior outcomes compared to unrepaired capsulotomy. They also suggest that in patients with signs or symptoms of instability, capsular plication may result in improved outcomes.58 Additionally, multiple biomechanical studies have shown the importance of hip capsule integrity for the stability of the hip joint.59–63 In patients with deficient capsule, capsular reconstruction has been described to improve stability. Fagotti et al showed that capsular reconstruction with iliotibial band allograft had better outcomes at 25 months when compared to dermal allograft.64
Hip arthroscopy has been shown in the literature to have a lower complication rate when compared to mini-open and open surgical dislocation.38,65 Recently, Larson et al showed, in a prospective trial, a complication rate of 8.3% following hip arthroscopy. They noted most common complications included lateral femoral cutaneous nerve neuropraxia, pudendal nerve neuropraxia, chondral injury, labral injury and heterotopic ossification. In their study, they showed the complication rate was higher in female patients and longer surgical and traction times with over 60 mins resulting in significantly increased complication rate.66
Summary
In the last decade, we have learned that the pathology around the femur-neck junction, rim of the acetabulum is real and it may be associated with labral and cartilage pathologies as well. Physical exam findings, radiographs and advanced imaging allow to delineate the pathology better and helps to plan the operative treatment more appropriately. Although conservative management can be an early option, literature has shown that patients undergoing hip arthroscopy for FAI have improved outcomes. If labral tears are encountered, current literature suggests repairing the tears results in better outcomes. Additionally, the underlying cam and pincer lesion pathology should be addressed with bony resection. Current literature also supports capsular repair which provides a stabilizer to the hip joint. If labrum or capsule is insufficient, reconstruction of these structures can be entertained.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Smith-Petersen MN. The classic: treatment of malum coxae senilis, old slipped upper femoral epiphysis, intrapelvic protrusion of the acetabulum, and coxa plana by means of acetabuloplasty. 1936. Clin Orthop Relat Res. 2009;467(3):608–615. doi: 10.1007/s11999-008-0670-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murray RO. The aetiology of primary osteoarthritis of the hip. Br J Radiol. 1965;38(455):810–824. doi: 10.1259/0007-1285-38-455-810 [DOI] [PubMed] [Google Scholar]
- 3.Solomon L. Patterns of osteoarthritis of the hip. J Bone Joint Surg Br. 1976;58(2):176–183. [DOI] [PubMed] [Google Scholar]
- 4.Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. [DOI] [PubMed] [Google Scholar]
- 5.Yeung M, Khan M, Schrieber VM, et al. Global Discrepancies in the diagnosis, surgical management, and investigation of femoroacetabular impingement. Arthroscopy. 2014;30:1625–1633. doi: 10.1016/j.arthro.2014.06.008 [DOI] [PubMed] [Google Scholar]
- 6.Bedi A, Kelly BT. Femoroacetabular impingement. J Bone Joint Surg. 2013;95:82–92. doi: 10.2106/JBJS.K.01219 [DOI] [PubMed] [Google Scholar]
- 7.Byrd JW. Femoroacetabular Impingement in Athletes. Am J Sports Med. 2014;42:737–751. doi: 10.1177/0363546513499136 [DOI] [PubMed] [Google Scholar]
- 8.Nepple JJ, Clohisy JC; ANCHOR study group members. Evolution of femoroacetabular impingement treatment: the ANCHOR experience. Am J Orthop. 2017;46(1):28–34. [PubMed] [Google Scholar]
- 9.Frank JM, Harris JD, Erickson BJ, et al. Prevalence of femoroacetabular impingement imaging findings in asymptomatic volunteers: a systematic review. Arthroscopy. 2015;31(6):1199–1204. doi: 10.1016/j.arthro.2014.11.042 [DOI] [PubMed] [Google Scholar]
- 10.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012–1018. doi: 10.1302/0301-620X.87B7.15203 [DOI] [PubMed] [Google Scholar]
- 11.Ganz R, Leunig M, Leunig-Ganz K, Harris W. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466(2):264–272. doi: 10.1007/s11999-007-0060-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clohisy J, Baca G, Beaule P, et al. Descriptive epidemiology of femoroacetabular impingement: a North American cohort of patients undergoing surgery. Am J Sports Med. 2013;41(6):1348–1356. doi: 10.1177/0363546513488861 [DOI] [PubMed] [Google Scholar]
- 13.Pollard TC, Villar RN, Norton MR, et al. Genetic influences in the aetiology of femoroacetabular impingement: a sibling study. J Bone Joint Surg Br. 2010;92(2):209–216. doi: 10.1302/0301-620X.92B2.22850 [DOI] [PubMed] [Google Scholar]
- 14.Agricola R, Bessems J, Ginai A, et al. The development of Cam-type deformity in adolescent and young male soccer players. Am J Sports Med. 2012;40(5):1099–1106. doi: 10.1177/0363546512438381 [DOI] [PubMed] [Google Scholar]
- 15.Zadpoor A. Etiology of femoroacetabular impingement in athletes: a review of recent findings. Sports Med. 2015;45(8):1097–1106. doi: 10.1007/s40279-015-0339-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tijssen M, van Cingel R, Willemsen L, de Visser E. Diagnostics of femoroacetabular impingement and labral pathology of the hip: a systematic review of the accuracy and validity of physical tests. Arthroscopy. 2012;28(6):860–871. doi: 10.1016/j.arthro.2011.12.004 [DOI] [PubMed] [Google Scholar]
- 17.Troelsen A, Mechlenburg I, Gelineck J, Bolvig L, Jacobsen S, Søballe K. What is the role of clinical tests and ultrasound in acetabular labral tear diagnostics? Acta Orthop. 2009;80:314–318. doi: 10.3109/17453670902988402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hananouchi T, Yasui Y, Yamamoto K, Toritsuka Y, Ohzono K. Anterior impingement test for labral lesions has high positive predictive value. Clin Orthop Relat Res. 2012;470(12):3524–3529. doi: 10.1007/s11999-012-2450-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maslowski E, Sullivan W, Forster Harwood J. The diagnostic validity of hip provocation maneuvers to detect intra-articular hip pathology. Pm R. 2010;2:174–181. doi: 10.1016/j.pmrj.2010.01.014 [DOI] [PubMed] [Google Scholar]
- 20.Rhee C, Le Francois T, Byrd JWT, Glazebrook M, Wong I. Radiographic diagnosis of pincer-type femoroacetabular impingement: a systematic review. Orthop J Sports Med. 2017;5(5):232596711770830. doi: 10.1177/2325967117708307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kappe T, Kocak T, Neuerburg C, et al. Reliability of radiographic signs for acetabular retroversion. Int Orthop. 2011;35:817–821. doi: 10.1007/s00264-010-1035-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nepple JJ, Riggs CN, Ross JR, Clohisy JC. Clinical presentation and disease characteristics of femoroacetabular impingement are sex-dependent. J Bone Joint Surg Am. 2014;96(20):1683–1689. doi: 10.2106/JBJS.M.01320 [DOI] [PubMed] [Google Scholar]
- 23.Hanke MS, Steppacher SD, Zurmühle CA, Siebenrock KA, Tannast M. Hips with protrusio acetabuli are at increased risk for failure after femoroacetabular impingement surgery: a 10-year followup. Clin Orthop Relat Res. 2016;474(10):2168–2180. doi: 10.1007/s11999-016-4918-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kutty S, Schneider P, Faris P, et al. Reliability and predictability of the centre-edge angle in the assessment of pincer femoroacetabular impingement. Int Orthop. 2012;36(3):505–510. doi: 10.1007/s00264-011-1302-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stelzeneder D, Hingsammer A, Bixby SD, Kim YJ. Can radiographic morphometric parameters for the hip be assessed on MRI? Clin Orthop Relat Res. 2013;471(3):989–999. doi: 10.1007/s11999-012-2654-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tannast M, Hanke MS, Zheng G, Steppacher SD, Siebenrock KA. What are the radiographic reference values for acetabular under- and overcoverage? Clin Orthop Relat Res. 2015;473(4):1234–1246. doi: 10.1007/s11999-014-4038-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res. 2006;445:181–185. doi: 10.1097/01.blo.0000201168.72388.24 [DOI] [PubMed] [Google Scholar]
- 28.Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84(4):556–560. [DOI] [PubMed] [Google Scholar]
- 29.Albers CE, Wambeek N, Hanke MS, Schmaranzer F, Prosser GH, Yates PJ. Imaging of femoroacetabular impingement-current concepts. J Hip Preserv Surg. 2016;3(4):245–261. doi: 10.1093/jhps/hnw035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chopra A, Grainger AJ, Dube B, et al. Comparative reliability and diagnostic performance of conventional 3T magnetic resonance imaging and 1.5T magnetic resonance arthrography for the evaluation of internal derangement of the hip. Eur Radiol. 2017;28(3):963–971. doi: 10.1007/s00330-017-5069-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Emara K, Samir W, Motasem ELH, Ghafar KA. Conservative treatment for mild femoroacetabular impingement. J Orthop Surg (Hong Kong). 2011;19(1):41–45. doi: 10.1177/230949901101900109 [DOI] [PubMed] [Google Scholar]
- 32.Wall PD, Fernandez M, Griffin DR, Foster NE. Nonoperative treatment for femoroacetabular impingement: a systematic review of the literature. Pm R. 2013;5(5):418–426. doi: 10.1016/j.pmrj.2013.02.005 [DOI] [PubMed] [Google Scholar]
- 33.Ayeni OR, Wong I, Chien T, Musahl V, Kelly BT, Bhandari M. Surgical indications for arthroscopic management of femoroacetabular impingement. Arthroscopy. 2012;28(8):1170–1179. doi: 10.1016/j.arthro.2012.01.010 [DOI] [PubMed] [Google Scholar]
- 34.Zaltz I, Kelly BT, Larson CM, Leunig M, Bedi A. Surgical treatment of femoroacetabular impingement: what are the limits of hip arthroscopy? Arthroscopy. 2014;30(1):99–110. doi: 10.1016/j.arthro.2013.10.005 [DOI] [PubMed] [Google Scholar]
- 35.Philippon MJ, Schroder E, Souza BG, Briggs KK. Hip arthroscopy for femoroacetabular impingement in adults aged 50 years or older. Arthroscopy. 2014;28(1):59–65. doi: 10.1016/j.arthro.2011.07.004 [DOI] [PubMed] [Google Scholar]
- 36.Philippon MJ, Briggs KK, Yen YM, Kuppersmith DA. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br. 2009;91(1):16–23. doi: 10.1302/0301-620X.91B1.21329 [DOI] [PubMed] [Google Scholar]
- 37.Botser IB, Smith TW Jr, Nasser R, Domb BG. Open surgical dislocation versus arthroscopy for femoroacetabular impingement: a comparison of clinical outcomes. Arthroscopy. 2011;27(2):270–278. doi: 10.1016/j.arthro.2010.11.008 [DOI] [PubMed] [Google Scholar]
- 38.Nwachukwu BU, Rebolledo BJ, McCormick F, Rosas S, Harris JD, Kelly BT. Arthroscopic versus open treatment of femoroacetabular impingement: a systematic review of medium- to long-term outcomes. Am J Sports Med. 2016;44(4):1062–1068. doi: 10.1177/0363546515587719 [DOI] [PubMed] [Google Scholar]
- 39.Laude F, Sariali E, Nogier A. Femoroacetabular impingement treatment using arthroscopy and anterior approach. Clin Orthop Relat Res. 2009;467(3):747–752. doi: 10.1007/s11999-008-0656-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ribas M, Marín-Peña OR, Regenbrecht B, De La Torre B, Vilarrubias JM. Hip osteoplasty by an anterior minimally invasive approach for active patients with femoroacetabular impingement. Hip Int. 2007;17(2):91–98. [DOI] [PubMed] [Google Scholar]
- 41.Tokish J, Ernat J, Song D, Brugman S, Lee G. Return to duty after mini-open arthropscopic-assisted treatment of femoral acetabular impingement in an active duty military population. Arthroscopy. (SS-37). 2013;29(6):e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Griffin DR, Dickenson EJ, Wall PDH, et al.; FASHion Study Group. Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): a multicentre randomised controlled trial. Lancet. 2018;391(10136):2225–2235. doi: 10.1016/S0140-6736(18)31202-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Byrd JW, Jones KS, Arthroscopic management of femoroacetabular impingement in athletes. Am J Sports Med. 2011;39(Suppl):7S–13S. doi: 10.1177/0363546511404144 [DOI] [PubMed] [Google Scholar]
- 44.Minkara AA, Westermann RW, Rosneck J, Lynch TS. Systematic review and meta-analysis of outcomes after hip arthroscopy in femoroacetabular impingement. Am J Sports Med. 2019;47(2):488–500. [DOI] [PubMed] [Google Scholar]
- 45.O’Connor M, Minkara AA, Westermann RW, Rosneck J, Lynch TS. Return to play after hip arthroscopy: a systematic review and meta-analysis. Am J Sports Med. 2018;46(11):2780–2788. doi: 10.1177/0363546518759731 [DOI] [PubMed] [Google Scholar]
- 46.Byrd JW, Jones KS, Gwathmey FW. Arthroscopic management of femoroacetabular impingement in adolescents. Arthroscopy. 2016;32(9):1800–1806. doi: 10.1016/j.arthro.2016.02.019 [DOI] [PubMed] [Google Scholar]
- 47.Larson CM, Giveans MR. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25:369–376. doi: 10.1016/j.arthro.2008.12.014 [DOI] [PubMed] [Google Scholar]
- 48.Ayeni OR, Adamich J, Farrokhyar F, et al. Surgical management of labral tears during femoroacetabular impingement surgery: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):756–762. doi: 10.1007/s00167-014-2886-8 [DOI] [PubMed] [Google Scholar]
- 49.Redmond JM, El Bitar YF, Gupta A, Stake CE, Vemula SP, Domb BG. Arthroscopic acetabuloplasty and labral refixation without labral detachment. Am J Sports Med. 2015;43(1):105–112. doi: 10.1177/0363546514555330 [DOI] [PubMed] [Google Scholar]
- 50.Philippon MJ, Schenker ML, Briggs KK, Kuppersmith DA, Maxwell RB, Stubbs AJ. Revision hip arthroscopy. Am J Sports Med. 2007;35:1918–1921. doi: 10.1177/0363546507305097 [DOI] [PubMed] [Google Scholar]
- 51.Heyworth BE, Shindle MK, Voos JE, Rudzki JR, Kelly BT. Radiologic and intraoperative findings in revision hip arthroscopy. Arthroscopy. 2007;23:1295–1302. doi: 10.1016/j.arthro.2007.09.015 [DOI] [PubMed] [Google Scholar]
- 52.Chow RM, Krych AJ, Levy BA. Arthroscopic acetabular rim resection in the treatment of femoroacetabular impingement. Arthrosc Tech. 2013;2(4):e327–e331. doi: 10.1016/j.eats.2013.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.White BJ, Herzog MM. Labral reconstruction: when to perform and how. Front Surg. 2015;2:27. doi: 10.3389/fsurg.2015.00027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.White BJ, Stapleford AB, Hawkes TK, Finger MJ, Herzog MM. Allograft use in arthroscopic labral reconstruction of the hip: minimum 2-year follow-up with front-to-back fixation technique. Arthroscopy. 2016;32(1):26–32. doi: 10.1016/j.arthro.2015.07.016 [DOI] [PubMed] [Google Scholar]
- 55.Locks R, Chahla J, Bolia IK, Briggs KK, Philippon MJ. Outcomes following arthroscopic hip segmental labral reconstruction using autologous capsule tissue or indirect head of the rectus tendon. J. Hip Preserv Surg. 2018;5(1):73–77. doi: 10.1093/jhps/hnx033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Frank RM, Lee S, Bush-Joseph CA, Kelly BT, Salata MJ, Nho SJ. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: a comparative matched-pair analysis. Am J Sports Med. 2014;42:2634–2642. doi: 10.1177/0363546514548017 [DOI] [PubMed] [Google Scholar]
- 57.Wylie JD, Beckmann JT, Maak TG, Aoki SK. Arthroscopic capsular repair for symptomatic hip instability after previous hip arthroscopic surgery. Am J Sports Med. 2016;44:39–45. doi: 10.1177/0363546515608162 [DOI] [PubMed] [Google Scholar]
- 58.Ortiz-Declet V, Mu B, Chen AW, et al. Should the capsule be repaired or plicated after hip arthroscopy for labral tears associated with femoroacetabular impingement or instability? A systematic review. Arthroscopy. 2018;34(1):303–318. doi: 10.1016/j.arthro.2017.06.030 [DOI] [PubMed] [Google Scholar]
- 59.Bayne CO, Stanley R, Simon P, et al. Effect of capsulotomy on hip stability—a consideration during hip arthroscopy. Am J Orthop. 2014;43:160–165. [PubMed] [Google Scholar]
- 60.Myers CA, Register BC, Lertwanich P, et al. Role of the acetabular labrum and the iliofemoral ligament in hip stability: an in vitro biplane fluoroscopy study. Am J Sports Med. 2011;39:85S–91S. doi: 10.1177/0363546511412161 [DOI] [PubMed] [Google Scholar]
- 61.Abrams GD, Hart MA, Takami K, et al. Biomechanical evaluation of capsulotomy, capsulectomy, and capsular repair on hip rotation. Arthroscopy. 2015;31:1511–1517. doi: 10.1016/j.arthro.2015.02.031 [DOI] [PubMed] [Google Scholar]
- 62.Smith MV, Costic RS, Allaire R, Schilling PL, Sekiya JK. A biomechanical analysis of the soft tissue and osseous constraints of the hip joint. Knee Surg Sports Traumatol Arthrosc. 2014;22:946–952. doi: 10.1007/s00167-012-2255-4 [DOI] [PubMed] [Google Scholar]
- 63.van Arkel RJ, Amis AA, Cobb JP, Jeffers JR. The capsular ligaments provide more hip rotational restraint than the acetabular labrum and the ligamentum teres: an experimental study. Bone Joint J. 2015;97-B:484–491. doi: 10.1302/0301-620X.97B9.35263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fagotti L, Soares E, Bolia IK, Briggs KK, Philippon MJ. Early outcomes after arthroscopic hip capsular reconstruction using iliotibial band allograft versus dermal allograft. Arthroscopy. 2019;35(3):778–786. doi: 10.1016/j.arthro.2018.10.110 [DOI] [PubMed] [Google Scholar]
- 65.Matsuda DK, Carlisle JC, Arthurs SC, Wiekrs CH, Phillipon MJ. Comparative systematic review of the open dislocation, mini-open, and arthroscopic surgeries for femuroacetabular impingement. Arthroscopy. 2011;27(2):252–269. doi: 10.1016/j.arthro.2010.09.011 [DOI] [PubMed] [Google Scholar]
- 66.Larson CM, Clohisy JC, Beaulé PE, et al.; ANCHOR Study Group. Intraoperative and early postoperative complications after hip arthroscopic surgery: a prospective multicenter trial utilizing a validated grading scheme. Am J Sports Med. 2016;44(9):2292–2298. doi: 10.1177/0363546516650885 [DOI] [PubMed] [Google Scholar]