Abstract
Background
Dysmenorrhoea (occurrence of painful menstrual cramps of uterine origin) is a common gynaecological condition. The character of pain from musculoskeletal dysfunction can be very similar to gynaecological pain by presenting cyclicly and being altered by hormonal changes associated with menstruation. Medical treatment for dysmenorrhoea usually comprises anti‐inflammatory drugs, oral contraceptives, or surgical intervention. Spinal manipulation is a non‐medical intervention. It has been suggested that manipulation of the vertebrae may increase spinal mobility thus improving pelvic blood supply and facilitating pain relief.
Objectives
To determine the safety and efficacy of spinal manipulative interventions for the treatment of dysmenorrhoea when compared to each other, placebo, no treatment, or other medical treatment.
Search methods
In this update we searched the Cochrane Menstrual Disorders and Subfertility Group Trials Register (May 2009), CENTRAL (to second quarter, 2009), MEDLINE (1966 to May 2009), EMBASE (1980 to May 2009), CINAHL (1982 to May 2009), and PsycINFO (1806 to May 2009). Citation lists of review articles and included trials were examined.
Selection criteria
Any randomised controlled trials (RCTs) including spinal manipulative interventions (for example chiropractic, osteopathy, or manipulative physiotherapy) versus each other, placebo, no treatment, or another medical treatment were considered. Exclusion criteria were mild or infrequent dysmenorrhoea or dysmenorrhoea from an intrauterine device (IUD).
Data collection and analysis
Two trials of high velocity, low amplitude (HVLA) manipulation and one trial of the Toftness technique were included. Quality assessment and data extraction were performed independently by two review authors. No data were suitable for meta‐analysis. Data were therefore reported as descriptive data. The outcome measures were pain relief or pain intensity and adverse effects.
Main results
Results from HVLA manipulation suggested that the technique was no more effective than sham manipulation for the treatment of dysmenorrhoea. One small trial indicated a difference in favour of HVLA manipulation however the one trial with an adequate sample size found no difference between HVLA and sham manipulation. There was no difference in adverse effects. The Toftness technique appeared more effective than sham treatment in one small trial but no conclusions could be made due to the size and other methodological limitations of the trial.
Authors' conclusions
There is no evidence to suggest that spinal manipulation is effective in the treatment of dysmenorrhoea. In the one trial reporting on adverse effects there was no greater risk of such events with spinal compared with sham manipulation.
Keywords: Female; Humans; Manipulation, Spinal; Dysmenorrhea; Dysmenorrhea/therapy; Pelvis; Pelvis/blood supply; Randomized Controlled Trials as Topic
Spinal manipulation for painful periods
Painful menstrual periods (dysmenorrhoea) are caused by cramps in the uterus (womb). One of the non‐drug options for dysmenorrhoea is spinal manipulation (using the hands to put pressure on certain parts of the back bone). This procedure is sometimes offered by physiotherapists, osteopaths or chiropractors. As dysmenorrhoea may be caused by restricted blood flow, manipulating the lower spine could improve blood flow to the pelvic area. The review of trials found no evidence that spinal manipulation relieves dysmenorrhoea.
Background
Description of the condition
Dysmenorrhoea refers to the occurrence of painful menstrual cramps of uterine origin. It is a common gynaecological condition that can affect as many as 50% of women, 10% of these women suffer severely enough to render them incapacitated for one to three days each menstrual cycle (Dawood 1990). This situation not only has a significant affect on quality of life and personal health but also has a global economic impact. In the US alone it is estimated that the annual economic loss is 600 million work hours and two billion dollars (Dawood 1984).
Dysmenorrhoea is commonly defined under two subcategories. When the pelvic pain is associated with an identifiable pathological condition, such as endometriosis or ovarian cysts, it is considered to be secondary dysmenorrhoea. In contrast, menstrual pain without organic pathology is considered to be primary dysmenorrhoea (Lichten 1987). The initial onset of primary dysmenorrhoea is usually at or shortly after (six to 12 months) menarche, when ovulatory cycles are established. The pain duration is commonly eight to 72 hours and is typically associated with the onset of menstrual flow. In contrast, secondary dysmenorrhoea is more likely to occur years after the onset of menarche and can occur premenstrually as well as during menstruation.
There are many methodological problems associated with quantifying and grading the pain of dysmenorrhoea. Assessment instruments used in quantifying dysmenorrhoea are based on women's self reporting, which may be subject to bias. Simple numerical rating scales (that is, one to five) or verbal rating scales (that is, mild, moderate, or severe) are common tools in rating pain such as with dysmenorrhoea. A similar tool that is more sensitive is the visual analogue scale (VAS) (Huskisson 1983). The VAS is a commonly used scale in pain assessment due to its simplicity and reliability; however, it is only a uni‐dimensional measure and is, therefore, limited in application (Melzack 1994). Multi‐dimensional scales such as the Menstrual Distress Questionnaire (Moos 1968) and the Menstrual Symptom Questionnaire (Chesney 1975) have also been developed; however, both have been criticised for being based on unrepresentative samples and for problems with validity (Lewis 198383). Generally speaking, if a woman seeks relief from pain a diagnosis of dysmenorrhoea may be justified regardless of the grading system used to assess her level of pain (Ylikorkala 1978).
The aetiology of primary dysmenorrhoea has been the source of considerable debate and is still not completely certain. Experimental and clinical research has identified the overproduction of uterine prostaglandins as a substantial contributing factor to the painful cramps that are the major symptom of dysmenorrhoea (Rosenwaks 1980). Overproduction of vasopressin, a hormone that stimulates contraction of muscular tissue, has also been identified as a contributing factor to dysmenorrhoea (Stromberg 1984).
Description of the intervention
Medical treatments such as non‐steroidal anti‐inflammatory drugs (NSAIDs) or oral contraceptive pills (OCPs) are common therapies for dysmenorrhoea as they both act by reducing myometrial activity. Surgical interruption of the sympathetic pelvic nerve pathways is also used as treatment to diminish uterine pain (Perez 1990). The efficacy of conventional treatments such as NSAIDs is considerable however the failure rate can still be as high as 20% to 25%, and there are also a number of associated adverse effects (Dawood 1985; Henzl 1985).
Many women seek alternatives to conventional medical treatments. The use of complementary or alternative therapy has become popular with both consumers and mainstream medical practitioners. Their definition is deliberately broad as what are considered complementary practices in one country could be conventional therapies in another. Studies suggest that between 30% to 50% of the adult population in industrialised nations use some form of complementary therapy to prevent or treat health‐related problems (Astin 1998a).
Physical or manipulative treatments have some of the highest rates of physician referral and practice among the many forms of complementary therapy (Astin 1998a). One popular treatment modality is spinal manipulation therapy. There is controversy about its use to treat visceral conditions (conditions related to the internal organs) such as dysmenorrhoea (Jamison 1992). A case study of treatment with spinal manipulation has demonstrated effective management of dysmenorrhoea (Liebl 1990).
The Toftness technique is a 'low‐force' chiropractic technique. The basic premise is that the nervous system has an electromagnetic energy associated with normal function. When the nervous system is not functioning normally, that is when there is a subluxation, the electromagnetic energy is abnormal. The chiropractor aims to identify the subluxation and remove it through adjustment.
How the intervention might work
There are several rationales for the use of musculoskeletal manipulation to treat dysmenorrhoea. The parasympathetic and sympathetic pelvic nerve pathways are closely associated with the spinal vertebrae, in particular the second to fourth sacral segments and the 10th thoracic to the second lumbar segments (Jamison 1992). One hypothesis is that mechanical dysfunction in these vertebrae causes decreased spinal mobility. This could affect the sympathetic nerve supply to the blood vessels supplying the pelvic viscera (internal organs) leading to dysmenorrhoea as a result of vasoconstriction (constriction of blood vessels). Manipulation of these vertebrae increases spinal mobility and may improve pelvic blood supply through an influence on the autonomic nerve supply to the blood vessels (Hitchcock 1976). Another hypothesis is that dysmenorrhoea is referred pain arising from musculoskeletal structures that share the same pelvic nerve pathways. Referred pain from the lumbar spine, pelvis, and hips may be responsible for the pelvic pain and other symptoms associated with dysmenorrhoea; vertebrae, joint capsules, ligaments, discs and muscle groups are all structures supplied by the pelvic nerve roots (Baker 1993). The character of pain from musculoskeletal dysfunction can be very similar to gynaecological pain and can present as cyclic pain as it can also be altered by hormonal influences and the changes associated with menstruation (Baker 1993). The value of any treatment is also dependent on the possible adverse effects associated with the treatment. Severe adverse reactions including death and paralysis can occur with spinal manipulation (Assendelft 1996) however these extreme effects are usually related to cervical spinal manipulation and occur at the rate of one in one million cervical spine manipulations (Hurwitz 1996). Manipulation of the lower spine, the area that would commonly be targeted in dysmenorrhoea, is associated with much lower risks; fractures and cauda equina syndrome (nerve compression) are the most serious reactions (Assendelft 1996).
Why it is important to do this review
Perceived efficacy is the most salient factor in a person's decision to use complementary and alternative medicine (CAM), such as spinal manipulation, yet this efficacy is usually based on word of mouth or single case studies (Astin 1998b). This systematic review aims to compare all randomised controlled trials of spinal manipulative interventions as treatment for dysmenorrhoea to determine their safety and efficacy.
Objectives
To determine the safety and efficacy of spinal manipulative interventions for the treatment of dysmenorrhoea when compared to each other, placebo, no treatment, or other medical treatment.
Methods
Criteria for considering studies for this review
Types of studies
Any randomised controlled trials (RCTs) that use spinal manipulation for the treatment of primary or secondary dysmenorrhoea. Cross‐over trials were excluded as once the spinal manipulation has been done it can not be reversed and, therefore, the effect inevitably carries over into the next cycle.
Types of participants
Inclusion criteria Participants in the trials must have met all the following inclusion criteria for the trial to be included in the review.
Women of reproductive age.
Women with moderate to severe primary dysmenorrhoea (pain that did not respond well to mild analgesics or affected daily activity) or women with secondary dysmenorrhoea of identifiable pathology that occurred in the majority of menstrual cycles.
Exclusion criteria If participants in the trial met any of the following exclusion criteria the trial was not included in the review.
Women with mild dysmenorrhoea (mild pain that responded well to analgesics).
Women with irregular or infrequent menstrual cycles (outside of the typical range of a 21 to 35 day cycle).
Women using an intrauterine contraceptive device ( IUD) or taking an oral contraceptive pill (OCP).
Types of interventions
Any RCTs including spinal manipulative interventions (for example, chiropractic, osteopathy, or manipulative physiotherapy) versus each other, placebo, no treatment, or another medical treatment were considered.
Types of outcome measures
Primary outcomes
(1) Pain relief (measured by a visual analogue scale (VAS), other pain scales, as a dichotomous outcome ( that is, pain relief achieved: yes or no), or as descriptive data). (2) Overall improvement in dysmenorrhoea (measured by change in dysmenorrhoeic symptoms, treatment effectiveness either self reported or observed, quality of life scales or other similar measures). (3) Adverse effects from treatment (incidence of side effects and type of side effects).
Secondary outcomes
(1) Requirements for additional medication (measured as the proportion of women requiring analgesics additional to their assigned treatment). (2) Restriction of daily life activities (measured as the proportion of women who reported activity restriction). (3) Absence from work or school (measured as the proportion of women reporting absences from work or school; and also as hours or days of absence, as a more selective measure).
Search methods for identification of studies
Electronic searches
All reports which described (or might have described) RCTs of spinal manipulation in the treatment of dysmenorrhoea were obtained using the following search strategies.
(1) We searched the Menstrual Disorders and Subfertility Group Trials Register (May 2009) for any trials with dysmenorrhoea or dysmenorrhoea in the title, abstract, or keyword sections (refer to Appendix 4).
The search found 387 references, seven involving spinal manipulation techniques. Three of these were trials that could be included (Hondras 1999; Kokjohn 1992; Snyder 1996). Two references were duplicates of the data in other trials, one a letter describing a trial and the other an unpublished version of the Hondras data.
(2) The search was adapted for other databases by using text words instead of subject headings and by removing the methodological terms from the search string.
Search results
MEDLINE (refer to Appendix 1): 41 references found, two were RCTs (Hondras 1999; Kokjohn 1992) EMBASE (refer to Appendix 2 ): 176 references found, two were RCTs (Hondras 1999; Kokjohn 1992) PsycINFO (refer to Appendix 5): six references found, one was an RCT (Hondras 1999)
(3) The Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library) was searched (Appendix 3).
The search found seven references: three were trials (Hondras 1999; Kokjohn 1992; Snyder 1996), one was a duplicate of a trial, one was an unpublished version of the Hondras data, and two were not relevant.
(4) We searched the metaRegister of Controlled Trials, which is a major international searchable database of ongoing randomised controlled trials in all areas of healthcare built by combining registers held by public, charitable, and commercial sponsors of trials (http://controlled‐trials.com/mrct/) (searched 18th March 2004). We searched for any trials with dysmenorrhoea or dysmenorrhoea as a keyword.
The search generated 26 references, however none were relevant.
(5) The Cochrane Complementary Medicine Field Register of controlled trials (CISCOM) was searched for any trials with dysmenorrhoea or dysmenorrhoea in the title, abstract, or keyword fields for the original review. No additional references to RCTs were found.
Searching other resources
The citation lists of relevant publications, review articles, abstracts of scientific meetings, and included studies were searched. No additional references to RCTs were found.
Data collection and analysis
Selection of studies
The selection of trials for inclusion in the review was performed by two review authors (MW, PM) after employing the search strategy described.
Data extraction and management
Data were extracted from eligible studies using a data extraction form designed by the authors. Where studies had multiple publications, the main trial report was used as the reference and additional details supplemented from secondary papers.
All assessments of the quality of trials were performed independently by two review authors (MW, WH) as was the data extraction (MW, TJ). Any discrepancies were to be resolved by a third review author (WH or TJ) but this was unnecessary. Additional information on trial methodology or original trial data were sought from the principal authors of two trials (Snyder 1996; Thomason 1979) as aspects of the methodology were unclear or the data were in a form that was unsuitable for meta‐analysis. Prof M Kilmore kindly supplied original data from the Boesler trial (Boesler 1993).
Included trials were analysed for the quality criteria and methodological details. This information is presented in the table of 'Characteristics of included studies and provides a context for discussing the reliability of results.
Assessment of risk of bias in included studies
The included studies were assessed for risk of bias using the Cochrane risk of bias assessment tool to assess sequence generation; allocation concealment; blinding of participants, providers, and outcome assessors; completeness of outcome data; selective outcome reporting; and other potential sources of bias. The conclusions of this analysis are presented in the 'Risk of bias' figures Figure 1; Figure 2 . If sufficient studies were identified a funnel plot was to be created to assess publication bias.
Figure 1.
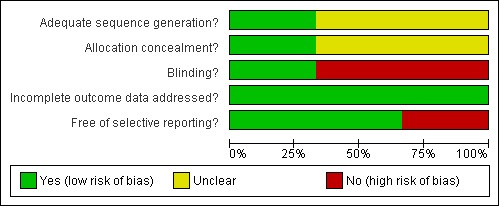
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
Figure 2.
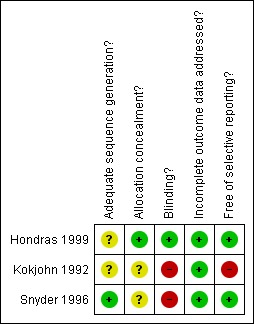
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Measures of treatment effect
The main planned analyses were comparisons between different types of spinal manipulation; spinal manipulation versus placebo, control, or no treatment; and spinal manipulation versus other medical treatments. It was later decided to evaluate the data from different manipulative techniques separately as the authors deemed it inappropriate to combine data when treatments were dramatically different. One included trial used the Toftness technique as the intervention (Snyder 1996). This technique was considerably different from the high velocity, low amplitude manipulative techniques used in the other three trials, therefore the two treatments were considered separately in the analysis.
Statistical analysis was performed in accordance with the guidelines for statistical analysis developed by the Menstrual Disorders and Subfertility Group. It was the intention of the review authors to pool the outcomes, where possible. Due to the lack of trials no data were pooled. For dichotomous data (that is, outcomes that are either present or not, such as pain relief) the data were summarised as the number of people who experienced the event or outcome in each comparison group and the total number in each group.
For continuous data (for example, pain measured on a visual analogue scale (VAS)) the data were summarised as the number of people in each group, the mean value for the outcome in each group and the standard deviation for each mean. No meta‐analysis could be conducted as there was only one trial for each outcome.
For one study, standard errors were converted to standard deviations (standard error x square root of n (where n = group sample size)) for the outcome of mean change from baseline for 100 mm VAS pain scores so that a mean difference (MD) could be calculated (Hondras 1999).
Unit of analysis issues
The primary analysis was per woman randomised. Cross‐over trials were excluded as the effects of spinal manipulation can not be reversed and are therefore likely to be carried over into the next cycle. One of the studies was excluded as the chiropractors and not the patients were randomised (Boesler 1993).
Dealing with missing data
Data were examined on an intention‐to‐treat principle, where possible. Where data were missing the original authors were contacted to try to obtain this information.
Assessment of heterogeneity
It was the intention of the review authors to examine heterogeneity between the results of different studies by inspecting the scatter in the data points and the overlap in their confidence intervals and, more formally, by checking the results of the Chi2 tests. However this was not possible due to the lack of pooled data.
Assessment of reporting biases
In order to minimise the potential impact of publication bias a comprehensive search for eligible studies was conducted. There were insufficient studies to be able to produce a funnel plot to assess publication bias.
Data synthesis
Data were presented in the following comparisons.
High velocity, low amplitude (HVLA) manipulation versus control on:
pain relief or intensity;
adverse effects.
Toftness technique versus control on:
pain intensity.
Subgroup analysis and investigation of heterogeneity
Due to the limited amount of evidence, no subgroup analyses were conducted.
Sensitivity analysis
A priori, it was planned to perform sensitivity analyses of results to look at the possible contribution of differences in: (1) trial design, especially the type of manipulation and control used; (2) methodological quality, with only trials of high quality compared to all trials; (3) methods of assessing dysmenorrhoeic pain, with the use of VAS compared to other scales. These analyses were not possible as only five trials were included, which is an inadequate number for these type of analyses.
Results
Description of studies
Results of the search
We included three studies in the review. Two studies were excluded from the update: the chiropractors were randomised rather than the participants; the trial was not truly randomised.
Included studies
Three trials followed a strict parallel‐group design in which one group received manipulative treatment and the other group a sham or control treatment (Hondras 1999; Kokjohn 1992; Snyder 1996).
All the trials took place in chiropractic and osteopathic clinics and all were performed in the United States. Two studies mentioned the source of their participants: two used local advertisements (Hondras 1999; Kokjohn 1992), and one also used referrals from practitioners (chiropractors) or gynaecologists (Kokjohn 1992).
All the included participants in the trials had dysmenorrhoea. The trialist's specifically mentioned primary dysmenorrhoea in addition to the exclusion of pelvic pathology (Hondras 1999; Kokjohn 1992; Snyder 1996). One trial mentioned the use of both a gynaecological and chiropractic examination to confirm the diagnosis of primary dysmenorrhoea (Hondras 1999). Common exclusion criteria were pre‐existing back trauma or pain, pelvic abnormality or pathology, and the use of an IUD or oral contraceptives. The age of participants ranged from 17 to 45 years.
Two of the included trials used similar high velocity, low amplitude (HVLA) rotation manipulation techniques. These treatments involved multiple level manipulations in the sideline position with joints manipulated in the physiological end range (Hondras 1999; Kokjohn 1992). One trial used a very different technique, the Toftness system, which involved a sensometer and spinal adjustment using a hand pressure applicator (Snyder 1996). The trials compared the manipulative treatment to some type of sham manipulative procedure (Hondras 1999; Kokjohn 1992; Snyder 1996).
In general, spinal manipulative treatment regimens varied greatly. More specific details on the treatment type, duration, and timing used by each included trial are summarised below.
Hondras 1999 Treatment: following pretreatment with superficial effleurage (massage) for three to five minutes, spinal manipulative therapy (SMT) using high velocity, short‐lever, low amplitude (greater than 750 N) thrust to vertebral levels from the 10th thoracic vertebrae to the fifth lumbar vertebrae (T10 to L5) and the sacroiliac joints (the joints between the hip and sacrum). Participants were positioned lying on their side with their bottom leg straight and their top hip and leg flexed. Control: a low‐force mimic (LFM) manoeuvre intended as a sham procedure as it appeared very similar to SMT. Sham manipulation was delivered to the left lumbar second to third vertebral level. A high velocity, short‐lever, low amplitude thrust (of not more than 400 N) was administered however the posture of the participant (both hips and both knees flexed) was such that the mechanical effect of the manipulation was substantially reduced. Duration and timing: cycle one was the baseline; treatment was performed on day one of cycle two for one treatment; three treatments were performed seven to 10 days preceding menses for cycles three and four, treatment was also performed on the first day of menses in cycles three and four.
Kokjohn 1992 Treatment: high velocity, low amplitude manipulation to clinically relevant vertebral levels from the 10th thoracic vertebrae to the fifth lumbar vertebrae, the sacral curve (T10 to L5‐S1) and the sacroiliac joints (the joints between the hip and sacrum). Participants were positioned lying on their side with their bottom leg straight and their top hip and leg flexed. Control: sham manipulation to midline base of the sacrum. A high velocity, short‐lever, low amplitude thrust was administered however the posture of the participant (with both hips and knees flexed), the offsetting of the leg movement to the thrust, and the midrange position of the joint was such that the mechanical torque of the manipulation was substantially reduced. Duration: one treatment only, on first day of menstrual cycle.
Snyder 1996 Treatment: Toftness system of chiropractic adjusting, a low force technique which uses a sensometer to detect abnormal electromagnetic radiation to determine which sites to adjust. Adjustment was delivered using a metered, hand‐held pressure applicator. Control: used the same basic procedure as the treatment group however adjustments were made at sites distinct from sites identified by the sensometer, otherwise the same contact and amount of force was used. Duration: three consecutive cycles, adjustments began on day one of menstrual flow and were received daily until the last day of menstrual flow. No more than 27 adjustments were allowed in the 90‐day treatment period. Women were monitored for three months after treatment. If loss of pain was experienced after the first cycle of treatment then no more adjustments were given, if pain was exacerbated then the participant was dropped from the trial.
Excluded studies
Two trials were excluded. In the trial by Boesler (1993) the chiropractors were randomised rather than the women (Boesler 1993); the second (Thomason 1979) performed 'randomisation' by asking participants to select one of three cards marked with M (manipulation), an A (activator sham), or a C (control). This was considered to be inadequate concealment of allocation. The uneven numbers of participants in each group: manipulation (n = 8), sham manipulation (n = 1), and control (n = 2) highlighted the inadequacies of this method of randomisation.
Risk of bias in included studies
Allocation
All three trials stated they were randomised controlled trials.
One trial were given a score of A for adequate allocation concealment as it used sealed, opaque, sequentially numbered envelopes to allocate treatments (Hondras 1999). The remaining trials were given a score of B for unclear allocation concealment as no details were given on allocation or randomisation of participants (Kokjohn 1992; Snyder 1996).
Blinding
In one included trial the outcome assessors were blinded to the treatment received and the participants were potentially blind due to the use of a sham treatment that was very similar to the real manipulative treatment (Hondras 1999), therefore the trial was potentially double blind. Another trial claimed to be single blind due to the use of a sham manipulation technique. The participants were unaware which was the real manipulative treatment and which was the sham treatment; in addition, the investigators delivering the treatment were unaware of the participants' clinical outcome measures (Snyder 1996). The other trial gave no details regarding the use of blinding.
One of the included trials made no mention of the naivety of their participants to spinal manipulation (Kokjohn 1992), which is an important aspect in successful blinding of sham manipulation. Only one trial clearly stated that all included participants were naive to the manipulation technique used (Snyder 1996), although one trial informally assessed the extent of blinding by asking women if they thought they had received real manipulation. The majority thought they had (Hondras 1999).
Incomplete outcome data
None of the trials performed an intention‐to‐treat analysis. There was no mention of participants withdrawing or dropping out in one trial (Kokjohn 1992). One trial reported that 13% of participants (4/30) dropped out but no reasons were given (Snyder 1996). The other trial reported that 2% (3/138) of participants dropped out after two cycles of treatment: one due to pregnancy, one received other treatment from a chiropractor so was excluded, and one refused to travel for treatment (Hondras 1999).
Selective reporting
There were no issues for discussion here.
Other potential sources of bias
Physical treatment regimens are particularly difficult to administer consistently and there are additional problems associated with the use of placebo or sham techniques. Summarised below are details on how the included trials dealt with treatment consistency and the use of placebo or sham therapies. For additional information on trial characteristics see the table Characteristics of included studies
Hondras 1999 Four chiropractic doctors delivered the majority of treatments, however a total of 14 clinicians delivered treatments. Initially all clinicians were trained in both procedures and retraining occurred at regular intervals throughout the study although how often was not specified. The sham treatment used was a very similar procedure to the experimental treatment and all other factors of the procedure were kept consistent (the only difference was posture and the force applied). The authors suggested that their sham procedure may have been too similar to the treatment to elicit an adequate comparison. Overall, the consistency of treatment appeared adequate however the number of clinicians delivering treatments seems high.
Kokjohn 1992 All participants were treated only once, on day one of their cycle. No information was presented regarding consistency of treatment. The trial reported that the clinically relevant vertebral levels would be manipulated; however, no information was presented on how this differed among participants. The measurement of outcomes occurred directly after treatment, therefore, no information was reported on whether the treatment effects lasted longer than one hour post‐treatment. The sham treatment used was the same as that used in the Hondras trial and appeared to be adequate. This sham treatment was perhaps too similar to the manipulative treatment and the amount of force used may still have had a therapeutic effect.
Snyder 1996 The number of treatments received varied for each individual. No information was given on the consistency of treatment or which parts of the spine were manipulated, there was also potential for inconsistency in the way the sensometer was applied. The sham treatment was exactly the same as the experimental treatment but was performed in areas distinct from those identified by the sensometer.
All of the included studies originated in the United States, which may therefore be a source of bias as many other countries are accepting of complementary and alternative medicines.
Effects of interventions
High velocity, low amplitude spinal manipulation Two of the included trials used high velocity, low amplitude (HVLA) manipulation as treatment. The outcome of pain intensity or pain relief was reported in a different way by each of the trials therefore it was not possible to combine the results of the trials. One small trial comparing HVLA manipulation with sham treatment (n = 44) expressed pain as a 10 cm VAS pain intensity score (with high scores representing more pain) after one treatment and one cycle (Kokjohn 1992). This trial indicated a significant difference between active and sham treatment in favour of HVLA manipulation (MD ‐1.41, 95% CI ‐2.55 to ‐0.27). The second trial (n = 137) reported pain data as the mean change in 100 mm VAS pain scores from baseline (Hondras 1999). This trial showed that pain scores for the HVLA treatment group had not dropped significantly more than for the sham treatment group after one treatment in one cycle (MD 2.08, 95% CI ‐3.20 to 7.36).
Only one trial (n = 138) reported the number of adverse effects experienced (Hondras 1999). Results showed no significant differences in the adverse effects experienced by participants in the HVLA and sham treatment groups after one cycle of treatment (Peto OR 1.51, 95% CI 0.25 to 8.95).
Toftness technique of spinal manipulation One trial (n = 26) compared the Toftness technique of manipulation with sham manipulation (Snyder 1996). Pain was reported as pain intensity on a 10 cm VAS (with high scores representing more pain) after three months treatment and at six months follow up. After three months treatment the sham manipulation participants had significantly lower pain scores (MD 2.20, 95% CI 1.38 to 3.02), however at the six‐month follow up there was a significant difference in favour of the Toftness manipulation group (MD ‐1.40, 95% CI ‐2.21 to ‐0.59).
Discussion
Summary of main results
This review aimed to assess the efficacy and safety of spinal manipulation for the treatment of primary and secondary dysmenorrhoea. Despite the popularity of complementary therapies, especially chiropractic treatment, there is a general lack of well‐designed research to evaluate the effectiveness of manipulation for specific conditions.
Three trials of spinal manipulation were identified. High velocity, low amplitude (HVLA) manipulation, a common manipulative technique, was the subject of two trials with a combined total of 183 participants. The Toftness technique, a little known technique that utilises a metered, hand‐held pressure applicator was the subject of one trial with 30 participants. A meta‐analysis combining results from all the trials was not feasible due to differences in the measurement, timing and reporting of pain outcomes and because only one trial was available for each outcome. Therefore results were reported with dichotomous, continuous or descriptive data separately.
HVLA manipulation was shown to be no more effective than sham manipulation (one trial, n = 44) although both treatments reduced the level of pain experienced. While the smaller trial indicated a difference in pain relief in favour of HVLA manipulation, the one trial with an adequate sample size (n = 137) and the best methodological rating found no difference between HVLA and sham treatments.
Results showed no significant differences in the adverse effects experienced by participants in the HVLA and sham treatment groups after one cycle of treatment. Overall there were few withdrawals from treatment but reporting of adverse events was not considered by most of the studies and it was not clear that the data presented in the studies reflected a comprehensive assessment of adverse events.
The Toftness technique was shown to be more effective than sham treatment at six months follow up, by one small trial, however three months following treatment the sham group had less pain. No strong conclusion can be made due to the small size of the single trial and other methodological considerations. There was a large difference in pain scores between the treatment and sham groups at baseline that may have had an impact on the results.
Additional outcome measures were reported by some of the included trials. Two trials reported a decrease in the circulating plasma levels of prostaglandin F2 alpha (Hondras 1999; Kokjohn 1992). Over production of this prostaglandin has been shown to be a substantial contributing factor to the painful cramps associated with dysmenorrhoea. The decrease occurred in conjunction with a decrease in pain and at the same rate in both the HVLA and sham manipulation treatment groups, with no difference in prostaglandin levels between the two groups.
These outcomes were used by the authors of the trials as an attempt to provide an objective measure of the efficacy of spinal manipulation. Although these measures add to our overall knowledge about the effects of spinal manipulation, physiological measures are not necessarily related to the pain levels experienced by dysmenorrhoeic women and are surrogate endpoints.
Overall completeness and applicability of evidence
There is too limited evidence identified to be able to generalise the findings.
Quality of the evidence
The review identified three RCTs. Due to the limited number of studies and the variety of outcomes used the authors of the review were unable to pool data for analysis and therefore the evidence is limited.
Blinding An important aspect when using placebo or sham treatments as controls is the participants' previous experience with treatment. To be successful in maintaining blinding, the participants entering the trial need to be naive to the treatment being offered. This is especially the case for spinal manipulation where the sham treatment differs intrinsically from the real treatment in order to avoid a therapeutic effect. Therefore, single blinding (of the participant) is considered difficult with the use of sham manipulation as a control and infeasible if the control is a different type of treatment, for example spinal manipulation versus a placebo pill.
Double blinding (blinding of both the participant and the treatment provider) in physical therapies is also generally considered impossible as the treatment provider needs to physically deliver the treatment or placebo. Spinal manipulation involves correction of the alignment of and restoration of mobility to select spinal vertebrae chosen for therapeutic effect and therefore needs to be performed by a skilled practitioner. As a result, it is probably impossible to perform a true double‐blind trial of spinal manipulation although blinding of the participant and outcome assessors should be used, if possible.
Potential biases in the review process
Standardisation of treatment Treatment providers perform physical therapies with variations. Treatment is often individually tailored to each participant's set of symptoms. Even if this is not the case different therapists vary the duration of treatment, the exact placement of manipulation along the spine, the force of manipulation, the types of manoeuvres, the frequency of treatments, timing of treatments in the cycle, and the number of treatments performed. These are all factors that make it difficult to assess the overall efficacy of spinal manipulation. The impact of these factors on treatment outcomes is not clear as these types of variations between practitioners of spinal manipulation can also be found in conventional medicine.
Use of sham manipulation A difficult issue in all randomised controlled trials of physical therapies is what to use as a control or placebo treatment. To adequately control for all the factors that may contribute to the treatment effect, a comparable placebo treatment rather than a waiting list control or a no‐treatment control is preferable. Study designs based on a sham treatment effectively control for any influence associated with the doctor‐patient interaction as the procedures can be performed through use of an identical protocol, in the same clinical setting, and by the same practitioner.
There are a number of techniques used as placebo for spinal manipulation. The main principle is to use a non‐therapeutic level of torque in the sham treatment. Therefore, peak forces delivered to the participants during sham manipulation thrust are substantially less than the peak forces delivered during true spinal manipulation therapy. Two common techniques for sham manipulation are where thrust is administered but the posture of the participant is such that the mechanical torque of the manipulation is substantially reduced; or through the use of an activator‐adjusting tool which can make spinal adjustments using spring recoil, where the spring is set so no force is exerted.
There is no guarantee that using sham manipulation will have no effect. The activator‐adjusting tool has been criticised as being an inadequate sham technique as force is still delivered even when the spring is set to zero (Harman 2000). The Hondras trial also acknowledged that their technique of sham manipulation (different patient position to lessen torque) may not have been an adequate placebo. In the attempt to ensure blinding of the participants, it is possible the sham manipulation techniques used by the trials included in this review may have had an unintended therapeutic effect. In most cases sham manipulation occurred in a slightly different area or with less force applied but it is unknown if these were sufficient differences for the intended sham treatments to be ineffective in relieving pain.
Other methodological issues In the trials included in this review there were many differences in treatment schedules. Some treatments were scheduled during menses; however one trial also used pre‐emptive treatment carried out at another time in the menstrual cycle. These different approaches could affect the outcome measures.
Agreements and disagreements with other studies or reviews
This review indicated that there was no evidence to suggest that spinal manipulation was effective in treating dysmenorrhoea.
Authors' conclusions
Overall, there is no evidence to suggest that spinal manipulation is effective in the treatment of dysmenorrhoea. In the one trial detailing adverse effects there was no greater risk of these effects with spinal manipulation than there is with sham manipulation.
Although the nature of physical therapy makes it difficult to blind participants to the intervention, future trials should maintain blinding for all outcome assessments. In addition, future trials should incorporate participants who are naive to spinal manipulation and should assess at the end of the trial the degree of participant blinding that occurred. Because trials involving sham manipulation may underestimate the actual benefit of spinal manipulation therapy, future trials should consider including a third arm, a no‐treatment control group.
Another important aspect is the use of standardised outcomes (that is, VAS pain scales) and adequate reporting of these measures. Baseline characteristics should be reported along with standard deviations (for continuous variables) and the number of participants in each category (for categorical variables), and for every follow up measure.
It is not anticipated that further research will emerge that will alter the findings of this review. It has therefore been decided that this review will not be updated again.
Acknowledgements
The authors acknowledge the helpful comments of those who refereed previous versions of this review and Anita Ballantyne for help with searching for trials. Special thanks are also due to Prof M Kilmore for kindly supplying original trial data, and the editorial base of the Cochrane Menstrual Disorders and Subfertility Group. The authors also acknowledge Dr Julie Brown for her assistance in updating the review in 2009.
Appendices
Appendix 1. MEDLINE search strategy
1 exp Menstruation Disturbances/ (21391) 2 pelvic pain.mp. or Pelvic Pain/ (4569) 3 (pelvi$ adj4 pain$).mp. (5193) 4 dysmenorrhea.mp. or Dysmenorrhea/ (3494) 5 (pain$ adj4 menstrua$).mp. (695) 6 (pain$ adj4 period$).mp. (2125) 7 menstrual disorder$.mp. (1052) 8 exp Endometriosis/ (12995) 9 Endometriosis.tw. (11365) 10 or/1‐9 (42461) 11 Manipulation, Chiropractic/ or Chiropractic/ or chiropractic.tw. (3773) 12 osteopath$.tw. (3107) 13 Osteopathic Medicine/ (2202) 14 (spin$ adj4 manipulat$).tw. (1086) 15 orthopedic manipulation.mp. or Manipulation, Orthopedic/ (3035) 16 spinal manipulation.mp. or Manipulation, Spinal/ (1141) 17 Physical Therapy Modalities/ or physical therapy.mp. or "Physical Therapy (Specialty)"/ (25080) 18 (manual adj2 therap$).mp. (762) 19 or/11‐18 (35660) 20 19 and 10 (187) 21 randomized controlled trial.pt. (270142) 22 controlled clinical trial.pt. (79146) 23 randomized.ab. (180138) 24 placebo.tw. (115093) 25 clinical trials as topic.sh. (142914) 26 randomly.ab. (130694) 27 trial.ti. (78660) 28 (crossover or cross‐over or cross over).tw. (42679) 29 or/21‐28 (640027) 30 (animals not (humans and animals)).sh. (3276464) 31 29 not 30 (592741) 32 31 and 20 (46) 33 (2006$ or 2007$ or 2008$ or 2009$).ed. (2375017) 34 33 and 32 (13) 35 from 34 keep 1‐13 (13)
Appendix 2. EMBASE search strategy
1 exp Menstruation Disorder/ (23821) 2 pelvic pain.mp. or exp Pelvis Pain Syndrome/ (5659) 3 (pelvi$ adj4 pain$).mp. (6822) 4 dysmenorrhea.mp. or DYSMENORRHEA/ (3991) 5 (pain$ adj4 menstrua$).mp. (1060) 6 exp Endometriosis/ (11040) 7 Endometriosis.tw. (9534) 8 (pain$ adj4 period$).mp. (1990) 9 or/1‐8 (41741) 10 chiropractic.mp. or Manipulative Medicine/ (7058) 11 osteopath$.mp. (2471) 12 spine manipulation/ or spinal manipulation.mp. (559) 13 orthopedic.mp. or ORTHOPEDICS/ (24501) 14 exp orthopedics/ or exp orthotics/ (5043) 15 (manipulat$ adj4 spin$).mp. (1577) 16 physical therapy.mp. or Physiotherapy/ (24853) 17 (manual adj2 therapy).mp. (757) 18 or/10‐17 (56817) 19 9 and 18 (509) 20 Controlled study/ or randomized controlled trial/ (2899215) 21 double blind procedure/ (72374) 22 single blind procedure/ (8152) 23 crossover procedure/ (21275) 24 drug comparison/ (81258) 25 placebo/ (126465) 26 random$.ti,ab,hw,tn,mf. (438069) 27 latin square.ti,ab,hw,tn,mf. (1130) 28 crossover.ti,ab,hw,tn,mf. (36587) 29 cross‐over.ti,ab,hw,tn,mf. (12303) 30 placebo$.ti,ab,hw,tn,mf. (177798) 31 ((doubl$ or singl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).ti,ab,hw,tn,mf. (118808) 32 (comparative adj5 trial$).ti,ab,hw,tn,mf. (16000) 33 (clinical adj5 trial$).ti,ab,hw,tn,mf. (608295) 34 or/20‐33 (3434891) 35 nonhuman/ (3221437) 36 animal/ not (human/ and animal/) (14488) 37 or/35‐36 (3225137) 38 34 not 37 (2029152) 39 19 and 38 (210) 40 limit 39 to yr="2008 ‐Current" (31) 41 from 40 keep 1‐31 (31)
Appendix 3. CENTRAL search strategy
1 exp Menstruation Disturbances/ (1070) 2 pelvic pain.mp. or Pelvic Pain/ (360) 3 (pelvi$ adj4 pain$).mp. (441) 4 dysmenorrhea.mp. or Dysmenorrhea/ (512) 5 (pain$ adj4 menstrua$).mp. (165) 6 (pain$ adj4 period$).mp. (1387) 7 menstrual disorder$.mp. (30) 8 exp Endometriosis/ (368) 9 Endometriosis.tw. (622) 10 or/1‐9 (3634) 11 Manipulation, Chiropractic/ or Chiropractic/ or chiropractic.tw. (383) 12 osteopath$.tw. (101) 13 Osteopathic Medicine/ (15) 14 (spin$ adj4 manipulat$).tw. (243) 15 orthopedic manipulation.mp. or Manipulation, Orthopedic/ (168) 16 spinal manipulation.mp. or Manipulation, Spinal/ (247) 17 Physical Therapy Modalities/ or physical therapy.mp. or "Physical Therapy (Specialty)"/ (2072) 18 (manual adj2 therap$).mp. (218) 19 or/11‐18 (2871) 20 19 and 10 (63) 21 limit 20 to yr="2006 ‐Current" (14) 22 from 21 keep 1‐14 (14)
Appendix 4. Menstrual Disorders and Subfertility Group (MDSG) search terms
MDSG search strings for MW526
Keywords CONTAINS "dysmenorrhea" or "Dysmenorrhea‐Symptoms" or "dysmenorrhoea" or "pain‐dysmenorrhea" or "menstrual pain" or "menstrual cramps" or "pelvic pain" or "*Endometriosis", "*Endometriosis" or "Pain‐abdominal" or "pain‐endometriosis" or "pain‐dyspareunia" or "pain‐pelvic"
AND
Keywords CONTAINS "manual therapy"or "manipulation"or "spinal manipulation"or "Chiropractic"or "Osteopathy"or"physiotherapy"or "spinal" or Title CONTAINS "manual therapy"or "manipulation"or "spinal manipulation"or "Chiropractic"or "Osteopathy"or"physiotherapy"or "spinal"
Appendix 5. PsycINFO search strategy
1 exp Menstruation Disturbances/ (0) 2 pelvic pain.mp. or Pelvic Pain/ (256) 3 (pelvi$ adj4 pain$).mp. (284) 4 dysmenorrhea.mp. or Dysmenorrhea/ (241) 5 (pain$ adj4 menstrua$).mp. (153) 6 (pain$ adj4 period$).mp. (324) 7 menstrual disorder$.mp. (308) 8 exp Endometriosis/ (0) 9 Endometriosis.tw. (98) 10 or/1‐9 (1267) 11 Manipulation, Chiropractic/ or Chiropractic/ or chiropractic.tw. (133) 12 osteopath$.tw. (130) 13 Osteopathic Medicine/ (39) 14 (spin$ adj4 manipulat$).tw. (44) 15 orthopedic manipulation.mp. or Manipulation, Orthopedic/ (1) 16 spinal manipulation.mp. or Manipulation, Spinal/ (17) 17 Physical Therapy Modalities/ or physical therapy.mp. or "Physical Therapy (Specialty)"/ (1704) 18 (manual adj2 therap$).mp. (224) 19 or/11‐18 (2178) 20 19 and 10 (10) 21 limit 20 to yr="2006 ‐Current" (6) 22 from 21 keep 1‐6 (6)
Data and analyses
Comparison 1.
High velocity, low amplitude (HVLA) manipulation versus control
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain intensity (10cm VAS) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 HVLA versus sham treatment | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | ‐1.41 [‐2.55, ‐0.27] |
| 2 Pain relief or intensity ‐ descriptive data | Other data | No numeric data | ||
| 2.1 HVLA versus sham treatment | Other data | No numeric data | ||
| 3 Change in pain intensity from baseline ‐ 100mm VAS | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 HVLA versus sham treatment | 1 | 137 | Mean Difference (IV, Fixed, 95% CI) | 2.08 [‐3.20, 7.36] |
| 4 Adverse effects | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 4.1 HVLA versus sham treatment | 1 | 138 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.51 [0.25, 8.95] |
Analysis 1.1.
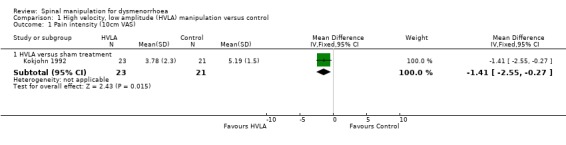
Comparison 1 High velocity, low amplitude (HVLA) manipulation versus control, Outcome 1 Pain intensity (10cm VAS).
Analysis 1.2.
Comparison 1 High velocity, low amplitude (HVLA) manipulation versus control, Outcome 2 Pain relief or intensity ‐ descriptive data.
Pain relief or intensity ‐ descriptive data
| Study | Pain scale used | n | results | conclusions |
|---|---|---|---|---|
| HVLA versus sham treatment | ||||
| Hondras 1999 | Pain 100mm VAS (0=none) mean change in VAS scores from baseline (std error) | Cycle 1: HVLA = 69 Sham = 66 Cycle 2: HVLA = 68 Control = 69 | HVLA: 10.09 (1.84) Sham: 8.01 (1.96) | A two‐sample t‐test was used by the trial to compare pre and post scores but no indication was given of significance values. |
Analysis 1.3.
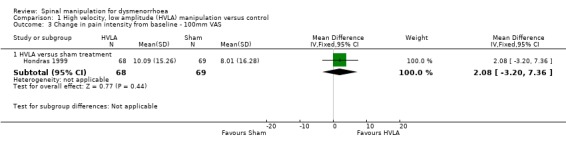
Comparison 1 High velocity, low amplitude (HVLA) manipulation versus control, Outcome 3 Change in pain intensity from baseline ‐ 100mm VAS.
Analysis 1.4.
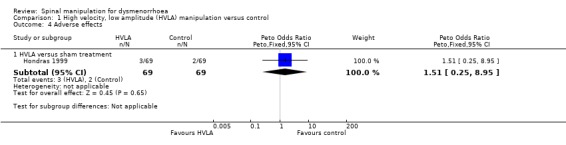
Comparison 1 High velocity, low amplitude (HVLA) manipulation versus control, Outcome 4 Adverse effects.
Comparison 2.
Toftness technique versus control
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain intensity (10cm VAS) at three months | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Toftness versus Sham treatment | 1 | 26 | Mean Difference (IV, Fixed, 95% CI) | 2.20 [1.38, 3.02] |
| 2 Pain intensity (10cm VAS) at six months | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Toftness versus Sham treatment | 1 | 26 | Mean Difference (IV, Fixed, 95% CI) | ‐1.40 [‐2.21, ‐0.59] |
Analysis 2.1.
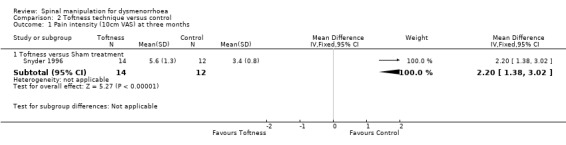
Comparison 2 Toftness technique versus control, Outcome 1 Pain intensity (10cm VAS) at three months.
Analysis 2.2.
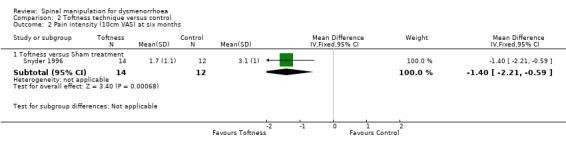
Comparison 2 Toftness technique versus control, Outcome 2 Pain intensity (10cm VAS) at six months.
What's new
| Date | Event | Description |
|---|---|---|
| 27 July 2009 | Review declared as stable | No new studies have been identified and the results of the review are unlikely to change. Therefore it has been decided to no longer update this review. Some studies previously included have been removed from the review as they were not randomised trials. |
History
Protocol first published: Issue 2, 2000 Review first published: Issue 1, 2002
| Date | Event | Description |
|---|---|---|
| 23 June 2009 | New search has been performed | New searches run and no new studies identified. Review reformatted to RevMan 5 requirements. One previous study excluded. |
| 6 November 2008 | Amended | Converted to new review format. |
| 29 April 2006 | New citation required and conclusions have changed | Substantive amendment |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Trial design: randomised clinical trial. Randomisation and allocation: random allocation using sealed, opaque sequentially numbered envelopes. Blinding: single blinding, observer was blind to treatment received and women were potentially blind as the LMF (sham) treatment appeared similar to the treatment procedure. Number of participants: 138 women randomised, all completed cycles 1‐2, then 3 lost to follow up (1 pregnancy, 1 refused to travel, 1 received treatment from a chiropractor). | |
| Participants | Inclusion: regular cycles; moderate to severe primary dysmenorrhoea; chiropractic and gynaecological examinations. Exclusion: IUD, OCP or NSAID use; organic pathology; recent hormone use; pre‐existing lower back pain. Age: 18 to 45 years Source: local newspaper advertisements. Location: chiropractic centre in Chicago, USA. | |
| Interventions | Treatment: spinal manipulative therapy (SMT); high velocity, short‐lever, low amplitude thrust to vertebral levels from T10 to L5 and the sacroiliac joints. Control: LFM manoeuvre, intended as a sham procedure as it appeared very similar to STM. Treatments performed by licensed chiropractors who rehearsed manoeuvres for reliability and were periodically retrained. Duration: cycle 1 was baseline; treatment performed on day 1 of cycle 2 for one treatment; 3 treatments performed in 7‐10 days preceding menses for cycles 3 and 4, treatment also performed on 1st day of menses in cycle 3 and 4. | |
| Outcomes | Visual analogue scale (VAS 10 cm) for pain intensity before and 1 hour after treatment (including baseline cycle). Moos Menstrual Distress Questionnaire on days 1 and 4 of cycles before and after treatment. Side effects. Blood samples for prostaglandin levels. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Random allocation, no details |
| Allocation concealment? | Low risk | Allocation using sealed, opaque sequentially numbered envelopes |
| Blinding? All outcomes | Low risk | Single blinding, observer was blind to treatment received and women were potentially blind as the LMF (sham) treatment appeared similar to the treatment procedure |
| Incomplete outcome data addressed? All outcomes | Low risk | 3 lost to follow up (1 pregnancy, 1 refused to travel, 1 received treatment from a chiropractor) |
| Free of selective reporting? | Low risk | All relevant outcomes discussed |
| Methods | Trial design: randomised clinical trial. Randomisation and allocation: no details on allocation concealment. Blinding: no details on blinding. Number of participants: 45 women randomised, 24 in treatment, 21 in control. | |
| Participants | Inclusion: history of primary dysmenorrhoea beginning within 2 years of menarche; regular cycle; moderate, severe or disabling dysmenorrhoea in each cycle, beginning day before or at onset of flow. Exclusion: excluded if any pelvic abnormality, endometriosis, use of birth control pills or IUD, or contraindications to spinal manipulation. Women also asked not to use analgesics during study and to abstain from exercise or intercourse 24 hr prior to treatment. Age: 20‐40 (mean 30.3) years. Source: recruited from local community by advertisements or referrals from chiropractors or gynaecologists. Location: chiropractic clinic in Chicago, USA. | |
| Interventions | Treatment: high velocity low amplitude manipulation to clinically relevant vertebral and sacroiliac joints. Control: sham manipulation to midline base of sacrum. Duration: one treatment only. | |
| Outcomes | VAS for abdominal pain. VAS for back pain. MDQ for menstrual distress. All scales assessed 15 min before and 60 min after treatment. Blood samples for KD PGF2α. | |
| Notes | Outcome measurement rather limited temporally. No information on whether effects lasted longer than 1 hr post‐treatment. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | No details |
| Allocation concealment? | Unclear risk | No details |
| Blinding? All outcomes | High risk | No details of blinding |
| Incomplete outcome data addressed? All outcomes | Low risk | All participants accounted for |
| Free of selective reporting? | High risk | Outcome measurement rather limited temporally. No info on whether effects lasted longer than 1 hr post‐treatment |
| Methods | Trial design: single blind randomised controlled clinical trial. Randomisation and allocation: allocation was by a random number generator and block 2 design without stratification. Blinding: no details on blinding. Number of participants: 30 women randomised, 26 analysed;1 from treatment group and 3 from sham group dropped out or lost to follow up. | |
| Participants | Inclusion: had a history of primary dysmenorrhoea for at least 1 year, menstrual pain beginning day before or just after onset of menstrual flow, moderate to severe pain, regular cycle. Exclusion: over age 50 years; history of endometriosis, pelvic inflammatory disease, or other pelvic organic pathology; using IUD; also needed to refrain from other chiropractic care during the course of the study. Age: means 26.1(4.5) and 27.1(6.2) years. | |
| Interventions | Treatment: Toftness system of chiropractic adjusting, low force technique which uses a sensometer to detect electromagnetic radiation and determine which sites to adjust. Control: same procedure however adjustments made at a site distinct from that identified by the sensometer. Duration: 3 consecutive cycles, adjustments began on day 1 of menstrual flow and received daily until last day of menstrual flow, no more than 27 adjustments in the 90 day treatment period. Then women monitored for 3 months after treatment. If loss of pain experienced after first cycle no more adjustments were given, if pain exacerbated women were dropped from the trial. | |
| Outcomes | MDQ completed on first day of every cycle: 5‐point scale for 18 questions. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Randomisation was by a random number generator and block 2 design without stratification |
| Allocation concealment? | Unclear risk | B‐unclear |
| Blinding? All outcomes | High risk | No evidence of blinding |
| Incomplete outcome data addressed? All outcomes | Low risk | 26 analysed,1 from treatment group and 3 from sham group dropped out or lost to follow up |
| Free of selective reporting? | Low risk | All relevant outcomes reported |
LFM: low‐force mimic manoeuvre
MDQ: Menstrual Distress Questionnaire
SMT: spinal manipulative therapy
VAS: visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Boesler 1993 | Study randomised chiropractors and not participants. |
| Thomason 1979 | Participants not truly randomised. They were asked to select one of three cards. |
Contributions of authors
Michelle Proctor: took the lead in writing the protocol and review, performed initial searches of databases for trials, was involved in selecting trials for inclusion, performed independent data extraction and quality assessment of the included trials, and was responsible for statistical analysis and interpretation of the data. Wayne Hing: performed independent quality assessment; added clinical expertise to the description of studies section, methodological quality section, and the discussion; and commented on drafts of the review. Trina Johnson: commented on drafts of the protocol and review, performed independent data extraction, and added clinical expertise to the discussion. Patricia Murphy: assisted in writing the protocol, was involved in selecting trials for inclusion, and commented on drafts of the protocol and review.
Julie Brown conducted the update in 2009, reformatted the review, and removed two previously included trials which have subsequently been excluded.
Sources of support
Internal sources
University of Auckland, School of Medicine, Auckland, New Zealand.
External sources
Princess of Wales Memorial Trust Fund administered by the Mercia Barnes Fund, New Zealand.
Declarations of interest
None known
Stable (no update expected for reasons given in 'What's new')
References
References to studies included in this review
- Hondras MA, Long CR, Brennan PC. Spinal manipulation therapy versus a low force mimic maneuver for women with primary dysmenorrhea: a randomized, observer‐blinded clinical trial. Pain 1999;81(1‐2):105‐14. [DOI] [PubMed] [Google Scholar]
- Kokjohn K, Schmid DM, Triano JJ, Brennan PC. The effect of spinal manipulation on pain and prostaglandin levels in women with primary dysmenorrhea. Journal of Manipulative and Physiological Therapeutics 1992;15(5):279‐85. [PubMed] [Google Scholar]
- Snyder BJ, Sanders GE. Evaluation of the Toftness system of chiropractic adjusting for subjects with chronic back pain, chronic tension headaches, or primary dysmenorrhea. Chiropractic Techniques 1996;8(1):3‐9. [Google Scholar]
References to studies excluded from this review
- Boesler D, Warner M, Alpers A, Finnerty EP, Kilmore MA. Efficacy of high‐velocity low‐amplitude manipulative technique in subjects with low‐back pain during menstrual cramping. Journal of the American Osteopathic Association 1993;93(2):203‐14. [PubMed] [Google Scholar]
- Thomason PR, Fisher BL, Carpenter PA, Fike GL. Effectiveness of spinal manipulative therapy in treatment of primary dysmenorrhea: A pilot study. Journal of Manipulative and Physiological Therapeutics 1979;2(3):140‐5. [Google Scholar]
Additional references
- Assendelft WJ, Bouter LM, Knipschild PG. Complications of spinal manipulation: a comprehensive review of the literature. Journal of Family Practice 1996;42(5):475‐80. [PubMed] [Google Scholar]
- Astin JA, Marie A, Pelletier KR, Hansen E, Haskell WL. A review of the incorporation of complementary and alternative medicine by mainstream physicians. Archives of Internal Medicine 1998;158(21):2303‐10. [DOI] [PubMed] [Google Scholar]
- Astin JA. Why patients use alternative medicine: Results of a national study. JAMA 1998;279(19):1548‐53. [DOI] [PubMed] [Google Scholar]
- Baker PK. Musculoskeletal origins of chronic pelvic pain: diagnosis and treatment. Obstetrics and Gynecology Clinics of North America 1993;20(4):719‐42. [PubMed] [Google Scholar]
- Chesney MA, Tasto DL. The development of the Menstrual Symptom Questionnaire. Behaviour Research and Therapy 1975;13:237‐44. [DOI] [PubMed] [Google Scholar]
- Dawood MY. Ibuprofen and dysmenorrhea. American Journal of Medicine 1984;77(1A):87‐94. [DOI] [PubMed] [Google Scholar]
- Dawood MY. Dysmenorrhea. Pain and Analgesia 1985;1:20. [Google Scholar]
- Dawood MY. Dysmenorrhea. Clinical Obstetrics and Gynecology 1990;33(1):168‐78. [DOI] [PubMed] [Google Scholar]
- Harman RD. Preliminary study of the effects of a placebo chiropractic treatment with sham adjustments. Journal of Manipulative and Physiological Therapeutics 2000;23(4):294. [DOI] [PubMed] [Google Scholar]
- Henzl MR. Dysmenorrhea: Achievements and challenge. Sexual Medicine Today 1985;9:8‐12. [Google Scholar]
- Hitchcock ME. The manipulative approach to the management of primary dysmenorrhea. The Journal of the American Osteopathic Association 1976;75(10):909‐18. [PubMed] [Google Scholar]
- Hurwitz EL, Aker PD, Adams AH, Meeker WC, Shekelle PG. Manipulation and mobilisation of the cervical spine. A systematic review of the literature. Spine 1996;21:1746‐59. [DOI] [PubMed] [Google Scholar]
- Huskisson EE. Visual analogue scales. In: Melzack R editor(s). Pain measurement and assessment. New York: Raven Press, 1983:33‐7. [Google Scholar]
- Jamison JR, McEwen AP, Thomas SJ. Chiropractic adjustment in the management of visceral conditions: A critical appraisal. Journal of Manipulative and Physiological Therapeutics 1992;15(3):171‐80. [PubMed] [Google Scholar]
- Lewis RJ, Wasserman E, Denney NW, Gerrard M. The etiology and treatment of primary dysmenorrhea: a review. Clinical Psychology Review 1983;3:371‐89. [Google Scholar]
- Lichten EM, Bombard J. Surgical treatment of primary dysmenorrhea with laparoscopic uterine nerve ablation. Journal of Reproductive Medicine 1987;32:37‐41. [PubMed] [Google Scholar]
- Liebl NA, Butler LM. A chiropractic approach to the treatment of dysmenorrhoea. Journal of Manipulative and Physiological Therapeutics 1990;13(3):101‐6. [PubMed] [Google Scholar]
- Melzack R, Katz J. Pain measurement in persons in pain. In: Wall PD, Melzack R editor(s). Textbook of Pain. 3rd Edition. London: Churchill Livingstone, 1994:337‐51. [Google Scholar]
- Moos RH. The development of a menstrual distress questionnaire. Psychosomatic Medicine 1968;30(6):853‐67. [DOI] [PubMed] [Google Scholar]
- Perez JJ. Laparoscopic presacral neurectomy. Results of the first 25 cases. Journal of Reproductive Medicine 1990;35(6):625‐30. [PubMed] [Google Scholar]
- Rosenwaks Z, Seegar‐Jones G. Menstrual pain: its origin and pathogensis. Journal of Reproductive Medicine 1980;25 Suppl(4):207‐12. [PubMed] [Google Scholar]
- Stromberg P, Akerlund M, Forsling ML, Granstrom E, Kindahl H. Vasopressin and prostaglandins in premenstrual pain and primary dysmenorrhea. Acta Obstetricia et Gynecologica Scandinavica 1984;63(6):533‐8. [DOI] [PubMed] [Google Scholar]
- Ylikorkala O, Dawood MY. New concepts in dysmenorrhea. American Journal of Obstetrics and Gynecology 1978;130(7):833‐47. [DOI] [PubMed] [Google Scholar]


