Abstract
Background
Healthcare workers can suffer from occupational stress as a result of lack of skills, organisational factors, and low social support at work. This may lead to distress, burnout and psychosomatic problems, and deterioration in quality of life and service provision.
Objectives
To evaluate the effectiveness of work‐ and person‐directed interventions compared to no intervention or alternative interventions in preventing stress at work in healthcare workers.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE, PsycINFO, CINAHL, NIOSHTIC‐2 and Web of Science up to November 2013.
Selection criteria
Randomised controlled trials (RCTs) of interventions aimed at preventing psychological stress in healthcare workers. For organisational interventions, interrupted time‐series and controlled before‐and‐after (CBA) studies were also eligible.
Data collection and analysis
Two review authors independently extracted data and assessed trial quality. We used Standardised Mean Differences (SMDs) where authors of trials used different scales to measure stress or burnout. We combined studies that were similar in meta‐analyses. We used the GRADE system to rate the quality of the evidence.
Main results
In this update, we added 39 studies, making a total of 58 studies (54 RCTs and four CBA studies), with 7188 participants. We categorised interventions as cognitive‐behavioural training (CBT) (n = 14), mental and physical relaxation (n = 21), combined CBT and relaxation (n = 6) and organisational interventions (n = 20). Follow‐up was less than one month in 24 studies, one to six in 22 studies and more than six months in 12 studies. We categorised outcomes as stress, anxiety or general health.
There was low‐quality evidence that CBT with or without relaxation was no more effective in reducing stress symptoms than no intervention at one month follow‐up in six studies (SMD ‐0.27 (95% Confidence Interval (CI) ‐0.66 to 0.13; 332 participants). But at one to six months follow‐up in seven studies (SMD ‐0.38, 95% CI ‐0.59 to ‐0.16; 549 participants, 13% relative risk reduction), and at more than six months follow‐up in two studies (SMD ‐1.04, 95% CI ‐1.37 to ‐0.70; 157 participants) CBT with or without relaxation reduced stress more than no intervention.
CBT interventions did not lead to a considerably greater effect than an alternative intervention, in three studies.
Physical relaxation (e.g. massage) was more effective in reducing stress than no intervention at one month follow‐up in four studies (SMD ‐0.48, 95% CI ‐0.89 to ‐0.08; 97 participants) and at one to six months follow‐up in six studies (SMD ‐0.47; 95% CI ‐0.70 to ‐0.24; 316 participants). Two studies did not find a considerable difference in stress between massage and taking extra breaks.
Mental relaxation (e.g. meditation) led to similar stress symptom levels as no intervention at one to six months follow‐up in six studies (SMD ‐0.50, 95% CI ‐1.15 to 0.15; 205 participants) but to less stress in one study at more than six months follow‐up. One study showed that mental relaxation reduced stress more effectively than attending a course on theory analysis and another that it was more effective than just relaxing in a chair.
Organisational interventions consisted of changes in working conditions, organising support, changing care, increasing communication skills and changing work schedules. Changing work schedules (from continuous to having weekend breaks and from a four‐week to a two‐week schedule) reduced stress with SMD ‐0.55 (95% CI ‐0.84 to ‐0.25; 2 trials, 180 participants). Other organisational interventions were not more effective than no intervention or an alternative intervention.
We graded the quality of the evidence for all but one comparison as low. For CBT this was due to the possibility of publication bias, and for the other comparisons to a lack of precision and risk of bias. Only for relaxation versus no intervention was the evidence of moderate quality.
Authors' conclusions
There is low‐quality evidence that CBT and mental and physical relaxation reduce stress more than no intervention but not more than alternative interventions. There is also low‐quality evidence that changing work schedules may lead to a reduction of stress. Other organisational interventions have no effect on stress levels. More randomised controlled trials are needed with at least 120 participants that compare the intervention to a placebo‐like intervention. Organisational interventions need better focus on reduction of specific stressors.
Plain language summary
Preventing occupational stress in healthcare workers
Background
Healthcare workers suffer from work‐related or occupational stress. Often this is because healthcare workers face high expectations and they may not have enough time, skills and social support at work. This can lead to severe distress, burnout or physical illness. In the end, healthcare workers may be unable to provide high quality healthcare services. Stress and burnout can also be costly because affected healthcare workers take sick leave and may even change jobs.
We evaluated how well different ways to prevent healthcare workers' stress or burnout work.
Study characteristics
We included 58 studies that included altogether 7188 participants. Fiftyfour of the included studies were randomised controlled studies and four were non‐randomised studies. We categorised the interventions as either cognitive‐behavioural training, mental and physical relaxation, or organisational changes.
Key findings and quality of the evidence
Cognitive‐behavioural interventions
According to six studies, there was low‐quality evidence that cognitive‐behavioural training decreased stress with about 13% when compared to no intervention and when measured at follow‐up periods ranging from less than a month up to two years. It is unclear how relevant this reduction is for a person with stress. The results were similar when cognitive‐behavioural training was combined with relaxation. However, in three studies, stress levels were similar after a cognitive‐behavioural training course compared to other training that was not focused on stress management but on the content of care.
Mental and physical relaxation interventions
In 17 studies there was low‐ to moderate‐quality evidence that both mental and physical relaxation led to a reduction of 23% in stress levels compared to no intervention.
Organisational interventions
Organisational interventions were aimed at changing working conditions in 20 studies, improving support or mentoring in six studies, changing content of care in four studies, improving communication skills in one study and improving work schedules in two studies. Shorter or interrupted work schedules reduced stress levels in two studies but there was no clear benefit of any of the other organisational interventions.
Conclusions
We conclude that cognitive‐behavioural training as well as mental and physical relaxation all reduce stress moderately. Changing work schedules can also reduce stress, but other organisational interventions have no clear effects. We need randomised studies with at least 120 participants and preferably a single component intervention. Organisational interventions need to be better focused on addressing specific factors that cause stress.
Summary of findings
Background
Healthcare workers can suffer from work‐related or occupational stress as a result of organisational factors and an imbalance of demands, skills and social support at work, or any combination of these. Under some conditions this can lead to severe distress, burnout or psychosomatic diseases, and the resulting deterioration in quality of life and service provision (Weinberg 2000).
Description of the condition
'Burnout' has been defined as a persistent, negative, work‐related state of mind in 'normal' individuals that is primarily characterised by exhaustion, which is accompanied by distress, a sense of reduced effectiveness, decreased motivation, and the development of dysfunctional attitudes and behaviours at work. This psychological condition develops gradually but may remain unnoticed for a long time for the individual involved. It results from a misfit between intentions and reality at the job. Often burnout is self‐perpetuating because of inadequate coping strategies that are associated with the syndrome (Schaufeli 2003). Burnout and occupational stress are both considered to result from exposure to stressors at work, the effects of which are mediated by personal coping or the ability to deal with environmental stressors at a personal level (Cooper 2001; Schaufeli 2003). Burnout is considered here as a specific form of psychological stress and not as a clinical diagnosis (Firth‐Cozens 1999). The economic impact of such conditions is high, as can be inferred from data on absenteeism and turnover (Jacobson 1996; Raiger 2005). More than 10% of total claims for occupational diseases are attributed to stress at work (Williamson 1994). There are a variety of stress factors in the workplace of healthcare workers that have been shown to increase the risk of distress and burnout, such as increasing workload, emotional response to contact with suffering and dying patients, and organisational problems and conflicts (Payne 1987; McNeely 2005). In addition, many studies have shown that levels of dissatisfaction, distress and burnout at work are quite high in healthcare workers (Deckard 1994; Karasek 1992; Maslach 1982; Raiger 2005; Ramirez 1996).
Description of the intervention
Work‐related stress and burnout can be addressed with one or more of the following approaches: teaching cognitive‐behavioural techniques, engaging in mental or physical relaxation or by changing the organisation of work.
How the intervention might work
Cognitive‐behavioural techniques work by providing new ways to feel, think and act in stressful situations. Mental and physical relaxation techniques divert attention away from unpleasant stressful thoughts and feelings and build resilience. Organisational interventions can prevent stressful events from occurring or the feeling of stress or burnout from developing by adjusting work practices so that they match and make use of workers' capabilities better.
Why it is important to do this review
An extensive number of reviews have been published on the effectiveness of interventions to prevent or treat stress (DeFrank 1987; Lamontagne 2007; Murphy 1995; Van der Hek 1997; Van der Klink 2001). However, apart from Jones 2000b and Mimura 2003, there are no other reviews that focus specifically on interventions directed at stress prevention in healthcare workers. According to the Fifth European Working Conditions Survey (Eurofound 2012), the healthcare sector rates the highest on two important potential causes of work stress: hiding one's own emotions and adverse social behaviour, with 'mental health at risk' at an intermediate level compared with other sectors. In the UK, the healthcare sector has the highest estimated prevalence rate of work‐related stress (HSE 2013).
Because the characteristics of interventions designed for healthcare workers may be different from those of other occupations, the aim of this review is to determine the effectiveness of interventions to reduce stress specifically in healthcare workers. This is a fully updated version of the review that we first published in 2006.
Objectives
To evaluate the effectiveness of work‐ and person‐directed interventions compared to no intervention or alternative interventions in preventing stress at work in healthcare workers.
Methods
Criteria for considering studies for this review
Types of studies
For interventions directed at persons or the person/work interface such as relaxation or cognitive‐behavioural interventions, we considered only randomised controlled trials.
For work‐directed interventions such as organisational changes (see Types of interventions) it is usually unfeasible to randomise study participants because the interventions are usually executed at the environmental or group level. This can be overcome by using the cluster‐randomised design where workplaces or departments are randomised to the intervention or control groups. However, as this is a difficult and fairly new design, we also considered additional study designs for inclusion that allow for environmental interventions at the group level: controlled before‐and‐after studies (otherwise known as prospective cohort studies or quasi‐experimental studies) and interrupted time‐series. The interrupted time‐series design is defined by the Cochrane Effective Practice and Organisation of Care Review Group as a series of at least three outcome measurements before and at least three after the implementation of an intervention (EPOC 2013).
Types of participants
We included studies in which the interventions were directed at workers who had not actively sought help for conditions such as burnout, depression or anxiety disorder. This included interventions directed at healthcare workers officially employed in any healthcare setting or at student nurses or physicians otherwise in training to become a professional who were also doing clinical work. This excluded studies in which the participants were simply caregivers and were not employed by a healthcare organisation.
Types of interventions
We included studies with any kind of intervention aimed at preventing or reducing stress arising from work. 'Prevention' is defined as an intervention directed at healthy individuals not diagnosed with a specific disease.
We categorised interventions into three groups:
1. Cognitive‐behavioural interventions that aim to change the way in which participants think, feel and consequently behave in stressful situations.
2. Relaxation interventions that aim to induce a state of mental or bodily calmness, or both, to counteract the agitation caused by stress. This can be achieved by, for example, being a passive recipient of a massage or by actively performing various exercises. Thus focus is directed towards a specific relaxing activity and away from the unpleasant thoughts and feelings associated with stress.
3. Organisational interventions that are measures to change resources, the working environment, work tasks or working methods. The intention here is to prevent or decrease stress by ensuring that workers are better equipped to deal with the tasks associated with their jobs.
Some authors also distinguish multimodal interventions that consist of cognitive‐behavioural interventions combined with, for example, relaxation. We considered it more informative to describe such studies as combining cognitive‐behavioural interventions with relaxation.
For all kinds of interventions we included studies with both non‐intervention controls and with one or more alternative interventions as a control group.
In the previous version of this review (Marine 2006) we categorised interventions as person‐ and work‐directed. We think the new categorisation is more informative.
Types of outcome measures
Primary outcomes
As the primary outcome we considered all validated self‐report questionnaires measuring occupational stress or burnout. These included measures such as: Maslach Burnout Inventory (MBI) (Maslach 1982), the Nursing Stress Scale (Gray‐Toft 1981) and Karasek's Job Content Questionnaire (Karasek 1998).
Secondary outcomes
As secondary outcomes we considered all outcome measures of the detrimental effects of stress or burnout. These included measures such as: (a) Psychological symptoms: anxiety and depression, such as the State‐Trait Anxiety Inventory (Spielberger 1970), General Health Questionnaire (Goldberg 1991), Beck Depression Inventory (Beck 1961); (b) Physical symptoms and physiological parameters: for example, hormone levels such as prolactin, corticosteroids or others; (c) Measures on the cost effectiveness of interventions, such as incremental cost‐effectiveness ratios (ICERs), incremental cost‐per‐QALY (quality‐adjusted life year) and cost‐benefit ratios.
We considered the effects on the following time‐scales: (i) Up to one month (ii) From one month to six months (iii) Over six months
We deemed all other outcomes that do not measure stress or its effects on individuals beyond the scope of this review and thus we excluded them from analyses. Examples of excluded outcomes are: coping skills, knowledge or attitude change, work performance, patient satisfaction and claims from clients, employee absenteeism and turnover.
Search methods for identification of studies
Electronic searches
The original systematic searches: (a) MEDLINE/PubMed (1966 ‐ May 2005) (b) PsycINFO/Ovid (1967 ‐ May 2005) (c) Cochrane Depression, Anxiety and Neurosis Group (CCDAN) Specialised registry (last search: February 2002) (d) Cochrane Occupational Health Field (COHF) Specialised registry (last search: May 2005) The updated systematic searches:
(a) Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library, 2013, Issue 11 (November)) (b) MEDLINE/PubMed (1966 ‐ November 2013) (c) EMBASE.COM (1986 ‐ November 2013) (d) PsycINFO/ProQuest (1967 ‐ November 2013) (e) CINAHL/EBSCO (1981 ‐ November 2013) (f) NIOSHTIC‐2 (1900 ‐ December 2013) (g) Web of Science (1988 ‐ November 2013)
Searching other resources
Reference lists We carefully examined the reference lists from articles and reviews for any additional eligible studies.
Handsearching We handsearched all issues of Work & Stress between January 1987 and November 2013.
Data collection and analysis
Selection of studies
Two review authors (JR, JV) independently selected the studies to include in the review according to the inclusion criteria. If there was any disagreement concerning the inclusion of a study, we discussed this jointly, and where necessary a third review author (AM or CS) resolved the disagreement.
Data extraction and management
We conducted the extraction of data by using a made‐to‐measure data extraction form filled in independently by two review authors (JR and JV or AM and CS) for each study. (a) If studies used a cross‐over design we used the results from just after the implementation of the intervention in the intervention group, compared to the results in the concurrent waiting‐list control group. (b) If studies compared more than one active intervention we chose the most intensive intervention to enter into the meta‐analysis.
Assessment of risk of bias in included studies
We used the following items to assess risk of bias in the included studies: adequate sequence generation, allocation concealment, incomplete outcome data addressed and selective outcome reporting. We did not use items on blinding because none of the studies could blind participants or intervention providers, and all primary outcomes were from self‐reported questionnaires.
Measures of treatment effect
We plotted the results of each trial as means and standard deviations (SDs) for continuous outcomes. Because in many cases different instruments were used to measure stress, we transformed the means into standardised mean differences (SMDs) or effect sizes. Because these outcomes are difficult to interpret for clinical use, we also reported the means and standard deviations for the most‐used stress‐measurement instrument and the MBI.
In many cases multiple similar outcome measures were used or an instrument had several sub‐scales but no summary measure. In case of multiple similar outcomes, we chose the outcome which we deemed to best represent a measure of stress in healthcare workers, such as the Nursing Stress Scale (Gray‐Toft 1981) instead of, for example, the Perceived Stress Scale (Cohen 1983). When study authors used subscales such as with the MBI (Maslach 1996), we chose the subscale that in our view best represented stress, such as the emotional exhaustion scale of the MBI (Maslach 1996) or the effort subscale of the Effort Reward Imbalance Questionnaire (Siegrist 2004).
Unit of analysis issues
For studies that employed a cluster‐randomised design and that reported sufficient data to be included in the meta‐analysis and that did not make an allowance for the design effect, we calculated the design effect based on a fairly large assumed intra‐cluster correlation of 0.10. Even though we did not find information for the intra‐cluster correlation for these types of studies we assumed that 0.10 would be a realistic estimate. We based this assumption by analogy on studies about implementation research (Campbell 2001). We followed the methods stated in the Cochrane Handbook for Systematic Reviews of Interventions (Cochrane Handbook, Higgins 2011) for the calculations: design effect = 1+(M‐1)*ICC, where M is the average cluster size and ICC is the intra‐cluster correlation coefficient.
For studies with multiple study‐arms, we decided which was the least extensive intervention and compared all other arms to that intervention only, to prevent increasing the number of comparisons. When more than one arm of an intervention was included in the same comparison, we divided the number of control participants in two and used half of the control participants for each intervention arm to prevent double‐counting.
For studies with a cross‐over design we judged if a sufficient wash‐out period was used in the study design. We expected that the effects of most stress‐management interventions would extend over longer periods of time, and for these types of studies we only used data from before the washout period. For studies where a more immediate effect would be expected, such as in studies that evaluated working schedules, we accepted that with a reasonable washout period the results of the second period could also be used.
Dealing with missing data
Where necessary, we sought missing statistical data (means and standard deviations) from authors. We received unpublished statistical data from the authors of the following studies: Cohen‐Katz 2005; Ketelaar 2013; Gärtner 2013; Jones 2000a; McElligott 2003; Moody 2013; Oman 2006. The first author of Bittman 2003 did not wish to share their data and the first author of Ewers 2002 did not have the data anymore. The authors of Razavi 1993 referred us to the results of Delvaux 2004 instead. The author of Rowe 2006 reported that after baseline they had only measured MBI, which explains the apparent selective reporting.
When standard deviations (SDs) were not reported we calculated them from other reported values according to the methods stated in the Cochrane Handbook (Higgins 2011). For West 1984 we took the means and SDs that resulted from the post hoc comparisons in the repeated measures analyses. For Norvell 1987, we took the post‐treatment values and calculated SDs based on the P value. We calculated a t‐value from this P value even though the authors used a Mann‐Whitney U test. For Shapiro 2005, we took the post‐treatment values and the F‐value reported by the authors. We calculated a t‐value and subsequent SDs by taking the square root of the F‐value as the t‐value. For Tsai 1993, we took the post‐treatment values from the figure reporting the results of the repeated measures analysis. We took the reported P value belonging to the repeated measures analysis as if it had resulted from a t‐test and calculated the SDs based on this t‐value. For Ewers 2002, we took the post‐treatment scores and the P values belonging to the independent t‐tests to calculate a t‐value and subsequently SDs. For Martins 2011, we imputed the average of the SDs from the other studies in the same comparison.
Assessment of heterogeneity
We assessed first if studies were clinically homogeneous, i.e. sufficiently similar regarding their participants, interventions, control condition, outcome and follow‐up time to be combined in one comparison. Then we assessed statistical heterogeneity with the I² statistic. We deemed an I² value of more than 50% to indicate considerable heterogeneity.
Assessment of reporting biases
We avoided reporting bias by including studies and not articles. If multiple articles reported reported results from a single study, we consolidated all the data from all articles under one study ID only. We avoided language bias by including studies in any language. The Cochrane Handbook (Higgins 2011) recommends assessing publication bias with funnel plots when there are at least ten studies in a comparison. However, as this recommended cut‐off is arbitrary, we assessed publication bias with funnel plots in comparisons containing five or more studies.
Data synthesis
We combined studies that we deemed sufficiently similar regarding participants, intervention, control, outcome and follow‐up time in one comparison.
We pooled the results statistically when the outcomes were similar concepts, such as perceived stress. Because many different instruments were used, we used standardised mean differences (SMDs) to combine the stress‐related outcomes in the meta‐analysis.Not all instruments used one summary score but presented the results of various subscales. In cases where there was no summary measure, we chose the subscale that best represented a measure of stress. For example, for this analysis, we used only the emotional exhaustion subscale of the Maslach Burnout Inventory. In this way, we considered the various stress scales to measure the same concept.
To better enable the interpretation of these results we recalculated the pooled SMD back into a mean difference for the emotional exhaustion subscale of the MBI by dividing the SMD by an estimation of standard deviation. For this estimation we used the median value of the SDs of the control group in the studies that evaluated this intervention and used the MBI.
If there was little or no statistical heterogeneity in a comparison, we pooled the results using a fixed‐effect model. If the I² statistic was more than 50% we combined the study results using a random‐effects model.
Subgroup analysis and investigation of heterogeneity
Since various occupational groups of healthcare workers have different work content, their stress levels could be different and also the effect of interventions. We therefore evaluated the effect in nurses, physicians, and other health professionals like physiotherapists in subgroups if available in the same comparison.
When substantial heterogeneity was present in a comparison as indicated by I² greater than 50%, we tried to find an explanation. In our opinion, the most likely explanation is that there are data input errors.
Sensitivity analysis
To assess the effect of risk of bias on the pooled results, we performed a sensitivity analysis in which we excluded studies with a high risk of bias and assessed whether this changed the results appreciably.
Results
Description of studies
Results of the search
From the initial set of references found with the original systematic searches conducted in 2005, we identified a set of 51 potentially eligible studies (Figure 1). We scrutinised these further, and excluded 31 studies, leaving a total of 20 studies. However, we noticed that two studies actually reported separate sets of results of a single study so we included them as one study and henceforth refer to it as Lökk 2000. Thus, the original sample consisted of 19 studies. The first updated systematic searches conducted in 2008 yielded a set of 8623 references, after excluding duplicates, of which 5334 covered the period of the original search. Screening these references for eligibility resulted in 17 of the 19 studies already included in the original sample and an additional 30 potentially eligible studies for the period covered by the original search. This showed that the original search had not been sensitive enough. The first updated search in 2008 yielded another 34 potential studies that had been published since 2005. Other sources resulted in another six potential studies. We scrutinised the full‐text articles of these 70 new potentially eligible studies with regard to our inclusion and exclusion criteria. Altogether we excluded 56 studies, leaving a total of 14 new studies. However, one of these new studies (Rowe 2006) actually reported new follow‐up data for an earlier study (Rowe 1999). Because the more recent article reported the results of all measurements starting from baseline, we used these data and thus included the study only once. The systematic searches have since been updated three times, in November 2010, May 2012 and November 2013. These yielded altogether 9646 references, excluding duplicates. We assessed 100 full text articles for eligibility and excluded 76. This left 24 new studies. Put together, via four rounds of systematic searches conducted in 2008, 2010, 2012 and 2013, we have identified altogether 58 studies that fulfilled our inclusion criteria and 212 that did not and that we summarily excluded. In addition, we located three ongoing studies (Gomez‐Gascon 2013; Niks 2013; Spoor 2010) for which we could not find published outcome data.
1.
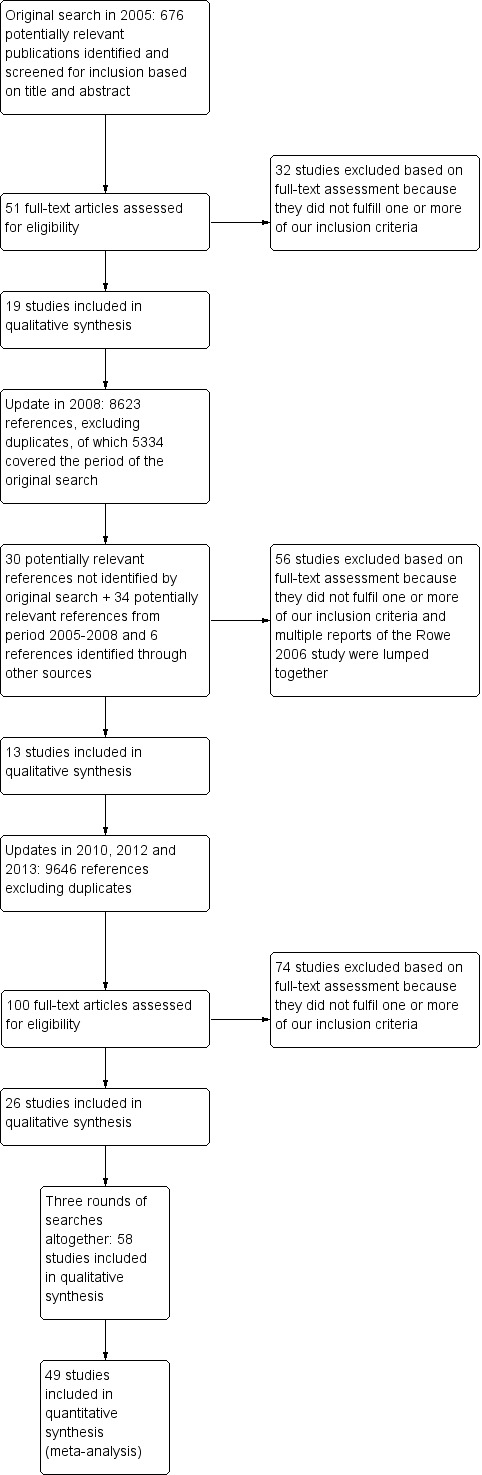
Study flow diagram.
We sought additional information regarding study details and statistical data or both from 18 authors and we received it from 12. Eight of the authors provided data that had not been published in their articles which enabled us to enter two of these studies into the meta‐analyses.
Included studies
Study designs Of the 58 included studies, 42 were randomised controlled trials, eight were cluster‐randomised trials, four were cross‐over studies and four were controlled before‐and‐after studies of a work‐directed intervention.
Six of the eight included cluster‐randomised trials had a unit of analysis error. In other words, these studies ignored the clustering of the data in their analysis. Hence we had to adjust the data accordingly. See Unit of analysis issues for the formula we used to calculate the design effect based on average cluster size (M) and an intra‐cluster correlation coefficient. We calculated the design effect as 2.01 for the Jensen 2006 study (19 clusters, M = 11.05); 2.2 for the Lökk 2000 study (2 clusters, M = 13); 2.73 for the Schrijnemaekers 2003 study (16 clusters, M = 18.3); 1.72 for the Proctor 1998 study (12 clusters, M = 8.2), 2.7 for Uchiyama 2013 (24 clusters, M = 18.08) and 1.42 for Ketelaar 2013 (58 clusters, M = 5.17). We used the design effect to reduce the number of participants in both intervention and control groups if we were able to use quantitative outcome data in meta‐analyses.
For the four cross‐over studies we wanted to use data from the first period only for Bittman 2003 and Lai 2011, but the studies did not provide these and thus could not contribute to the analysis. Von Baeyer 1983 reported the results of the first period separately and we included these. Lucas 2012 studied the immediate effect of different working schedules and used a washout period of four weeks between the intervention and the control period, which seemed reasonable. For this study we included the post‐intervention results of all participants.
We were aiming also to include studies with interrupted time‐series designs but the final sample contained none of these.
Country and time period Twelve of the included studies had been conducted before the year 2000, 22 between the years 2000 and 2010, and 24 in 2010 or later. Nineteen studies had been carried out in Europe, another 24 in North America, eight in Asia, three in the Middle East, two in South America and two in Australia.
Type of settings and participants Altogether 39 of the included studies had been conducted in hospitals, eight in residential care homes for the elderly or the disabled, seven in mixed healthcare settings, three in a secure unit and one in a nursing school. Thirty‐five studies included exclusively nurses (including all institutions), 15 included all healthcare staff, but usually the majority of the staff were nurses and only a small fraction (about 5%) were physicians, six studies exclusively included physicians and two included either physiotherapists or respiratory therapists.
Sample sizes The total number of participants was 7188, with 3592 in various intervention groups and 3596 in control groups. The number of participants was less than 20 in five studies, more than 20 but less than 60 in 27 studies, more than 60 but less than 300 in 20 studies, and more than 300 in six studies.
Interventions
Thirteen study‐arms (Delvaux 2004; Gardner CBT 2005; Gardner Coping 2005; Ketelaar 2013; Gärtner 2013; Günüsen 2010; Jensen 2006; Kwok 2012; Lee 1994; Lökk 2000; Martins 2011; Rowe 2006; Yamagishi 2008) examined cognitive‐behavioural interventions.
Six studies (Jones 2000a; Norvell 1987; Reynolds 1993; Sood 2011; Von Baeyer 1983; West 1984) assessed a combination of cognitive‐behavioural elements and relaxation.
Twenty‐two study‐arms examined relaxation interventions. We categorised relaxation interventions as: physical: Bittman 2003; Brennan 2006; Griffith 2008; Hansen 2006; Kurebayashi 2012; Lai 2011; Lemaire 2011; McElligott 2003; Palumbo 2012; Saganha 2012; Tsai 1993; Yazdani 2010; Yung 2004; and mental relaxation: Cohen‐Katz 2005; Klatt 2012; Mackenzie 2006; Moody 2013; Oman 2006; Shapiro 2005; Stanton 1988.
Twenty‐one study‐arms examined the effectiveness of organisational interventions. Of these, six tried to improve working conditions with or without the participation of workers (Bourbonnais 2011; Le Blanc 2007; Melchior 1996; Proctor 1998; Romig 2012; Uchiyama 2013). Another seven organised some kind of support, for example peer support groups, to discuss problems at work that increase stress (Carson 1999; Günüsen 2010; Heaney 1995; Leiter 2011; Li 2011; Peterson 2008; Salles 2013). Four studies evaluated the introduction of special care models such as emotion‐oriented care training (Finnema 2005; Razavi 1993; Redhead 2011; Schrijnemaekers 2003). Two studies evaluated the effect of different work schedules on stress (Ali 2011; Lucas 2012), one assessed the effect of improving nurses' knowledge about serious mental illness on stress (Ewers 2002) and another evaluated the effect of communication skills training on stress (Ghazavi 2010).
Type of control group (no intervention versus other active or 'passive' interventions) Almost all (45) of the included studies used a no‐intervention or waiting‐list control group.
Eleven studies compared an active intervention to a 'passive' intervention aiming to control for the Hawthorne effect, etc. (Brennan 2006; Carson 1999; Finnema 2005; Jensen 2006; Lai 2011; Lee 1994; Lökk 2000; Moyle 2013; McElligott 2003; Salles 2013; Tsai 1993).
Two studies (Ali 2011; Lucas 2012) compared only active interventions, that is, different work schedules with one another.
Multiple Intervention Arms
Seven studies (Gardner CBT 2005; Gärtner 2013; Günüsen 2010; Kurebayashi 2012; Rowe 2006; West 1984; Yung 2004) compared one or more active stress management interventions. Gardner CBT 2005 included an arm with CBT content and an arm aimed at improving coping with stress with relaxation and other individual self‐management interventions (time management, assertion, problem‐solving, etc.). We used both arms in different subgroups. Ketelaar 2013 and Gärtner 2013 evaluated two interventions with a similar content but with different modes of providing the intervention. We therefore combined those in the same comparison and again halved the numbers in the control group. Günüsen 2010 provided a coping and work support intervention and these were entered in separate comparisons. With Kurebayashi 2012, we entered both interventions in the same comparison of physical relaxation. West 1984 had five study arms but finally reported data only on one study arm versus a no‐intervention or no‐effect condition. We used this as an intervention versus no‐intervention comparison.
Outcomes
Altogether 21 studies used the Maslach Burnout Inventory (MBI) or one of its subscales as their main outcome measure. However, the MBI was only reported as a sum score in Shapiro 2005, and we used the Perceived Stress Scale (PSS) for that study instead of the MBI. Six studies used the Perceived Stress Scale (Brennan 2006; Griffith 2008; Lee 1994; Li 2011; Palumbo 2012; Sood 2011). Four studies used their own definition of burnout (Ali 2011; Bourbonnais 2011; Romig 2012; Salles 2013). Two studies used the Nurse Stress Scale (Delvaux 2004; Razavi 1993). Two studies used the General Health Questionnaire (GHQ) (Reynolds 1993; Yung 2004) and another two used the Profile of Moods States (POMS) (Bittman 2003; Moyle 2013). Two studies used their own developed stress scale (Ghazavi 2010; Lemaire 2011). The other outcome measures were each used by one study only: 4‐dimension complaint checklist (Ketelaar 2013), Brief Job Stress Questionaire (Yamagishi 2008), Depression Anxiety Stress Scale (Yazdani 2010), Derogatis Stress Profile (Jones 2000a), Effort Reward Imbalance Questionnaire (Uchiyama 2013), Job Stress Questionnaire (Hansen 2006), The Mental Health Professional Stress Scale (Gardner CBT 2005), Nurse Stress Checklist (see Benoliel 1990) (Tsai 1993), Occupational Stress Indicator (see Cooper 1988) (Proctor 1998), Organisation and Stress Scale (Finnema 2005), The General Nordic Questionnaire for Psychological and Social Factors at Work (QPS Nordic) (Peterson 2008), Symptom Checklist‐90 (see Derogatis 1976; Derogatis 1983) (Heaney 1995), Somatic Stress (Kwok 2012), Stress Profile (Stanton 1988), Stress Symptom Checklist (Kurebayashi 2012), Structured Stress Questionnaire (Lökk 2000), and Stress Visual Analogue Scale (Lai 2011). Two studies measured only anxiety (McElligott 2003; Von Baeyer 1983).
Altogether 22 studies used more than one of the stress measures listed above.
None of the studies measured the cost effectiveness of interventions.
Follow‐up (i)Short‐Term: There were 24 studies in which the last outcome measurement was either at the end of the intervention (Ewers 2002; Finnema 2005; Ghazavi 2010; Griffith 2008; Hansen 2006; Kurebayashi 2012; Lai 2011; Lemaire 2011; Li 2011; Lucas 2012; Mackenzie 2006; Martins 2011; McElligott 2003; Moyle 2013; Norvell 1987; Palumbo 2012; Proctor 1998; Saganha 2012; Shapiro 2005; Sood 2011; Von Baeyer 1983; Yamagishi 2008) or at less than a month after intervention (Brennan 2006; Tsai 1993).
(ii) Medium‐Term: In another 22 studies the last follow‐up measurement was between one and six months after intervention (Bittman 2003; Carson 1999; Cohen‐Katz 2005; Delvaux 2004; Gardner CBT 2005; Günüsen 2010; Heaney 1995; Klatt 2012; Kwok 2012; Le Blanc 2007; Lee 1994; Leiter 2011; Lökk 2000; Moody 2013; Oman 2006; Razavi 1993; Reynolds 1993; Romig 2012; Salles 2013; West 1984; Yazdani 2010; Yung 2004).
(iii) Long Term: There were also 12 studies in which the last follow‐up measurement was at six months after intervention or later (Ali 2011; Bourbonnais 2011; Jensen 2006; Jones 2000a; Ketelaar 2013; Melchior 1996; Peterson 2008; Redhead 2011; Rowe 2006; Schrijnemaekers 2003; Stanton 1988; Uchiyama 2013).
Excluded studies
Excluded studies
The main reasons for excluding studies from this review were the following, as illustrated by selected examples of each category (see Characteristics of excluded studies):
No control group: Andersen 2010; Cohen 2005; Elo 2000; Michie 1992; Petterson 2006; Schaufeli 1995; Yamagishi 2007.
Non‐randomised study design and intervention directed at persons or the person/work interface: Bourbonnais 2006a; Holt 2006; Michie 1994; Petterson 1998; Young 2001; Zimber 2001.
No intervention aimed at preventing or treating stress or burnout: Bourbonnais 2006b; Brinkborg 2011; Cámara Conde 2009; Ridge 2011; Wetzel 2011.
The intervention is primarily aimed at people with dementia at a care home and not the staff caring for them, although the effects were measured also for the latter: Baldelli 2004.
No primary outcome measure of stress or burnout: Bay 2010; Lai 2012; Pipe 2009; Saadat 2012; Sharif 2013; Villani 2012.
Participants were not healthcare workers or nursing students with clinical duties: Drain 1991.
Participants were nursing students but did not have clinical duties: Johansson 1991; Russler 1991; Sharif 2004.
Participants were victims of assault and deemed not healthy as per inclusion criteria: Nhiwatiwa 2003.
Participants had been diagnosed with burnout syndrome: Diaz‐Rodriguez 2011a; Diaz‐Rodriguez 2011b.
Risk of bias in included studies
In general, most studies were of low methodological quality, with at least several items that we judged to put them at a high risk of bias (Figure 2). We judged only one study (Günüsen 2010) to be at low risk of bias in randomisation, allocation concealment, incomplete data, selective reporting or other risks of bias. Blinding was consistently problematic in all studies because self report was used to assess stress levels as the outcome and the providers could not be blinded to the intervention. We therefore did not use this item to make a distinction between studies at high or low risk of bias.
2.
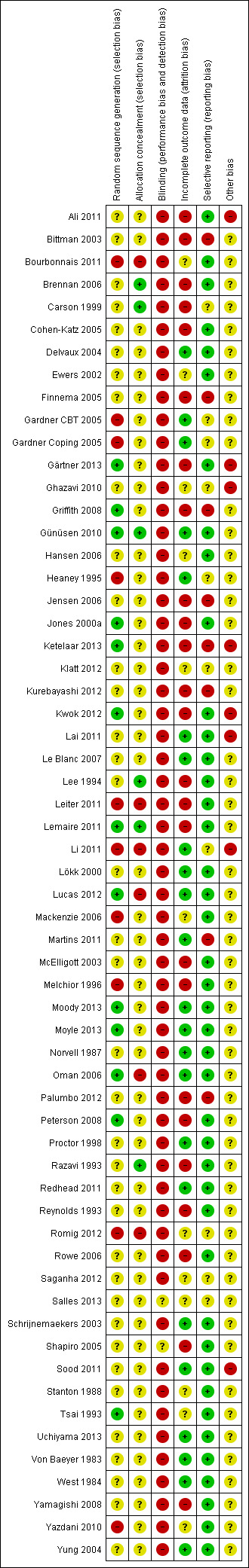
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Only 12 out of the 58 studies clearly described the method for generating random numbers, with the newer studies being better in this regard than the older studies. It is still surprising to note that most studies just describe the whole process as "We randomised participants". The large number of studies that did not report details prevented us from asking all authors to provide better information. Details of allocation concealment were lacking even more often, with only six studies giving an adequate description. Even though many other risks of bias are difficult to avoid in stress management studies, these items can clearly be improved for any study. The fact that a minority of studies reported sufficient detail and content to justify an assessment of low risk of bias means that it is feasible for all.
Blinding
We considered the reporting of stress by questionnaires as an outcome assessment that could be biased by knowledge of the intervention. We judged that it could be possible that a participant in the intervention group, knowing that they have gone through a six‐week course of stress management, would rate their stress symptoms more favourably than a person in the control group. This would create an overestimation of the effect of the intervention. Very few authors mentioned that blinding could be an issue, but said also that they thought that blinding is impossible here. We agree that this is not possible but that does not eliminate the risk of bias and we therefore rated all studies with self reports as being at high risk of bias.
Incomplete outcome data
The loss of participants was mostly low. However, 12 studies (Brennan 2006; Carson 1999; Finnema 2005; Ketelaar 2013; Gärtner 2013; Griffith 2008; Jensen 2006; McElligott 2003; Melchior 1996; Palumbo 2012; Peterson 2008; Tsai 1993) suffered a loss exceeding 20% of the initial sample. These were labelled as being at high risk of bias. Also one study (Bittman 2003) reported the reasons for participants not completing the study but not separately for the two groups. As the reasons listed were not entirely random (e.g. poor attendance and refusal to participate) we judged this study to be at high risk of attrition bias. In six studies (Jones 2000a; Lee 1994; Razavi 1993; Reynolds 1993; Rowe 2006; Shapiro 2005) results were analysed only for participants who provided complete data sets. We labelled these studies as being at high risk of bias. In two studies (Mackenzie 2006; Stanton 1988) it was unclear whether any participants dropped out and the studies were therefore labelled as being at unclear risk of bias.
Selective reporting
In the absence of a protocol, it is difficult to judge if outcomes are reported as planned. If the authors mentioned a protocol, we checked the protocol. If there was no mention of a protocol we judged if the methods and results sections reported the same outcomes. In most (41) of the studies all outcomes were reported as planned and consequently we judged them as being at low risk of bias. In one study (Carson 1999) two of the outcomes (Minnesota Job Satisfaction scale and the Cooper Coping Skills scale) were administered but their results were not reported. We judged this to be a sign of a high risk of bias. In two studies (Gardner CBT 2005; Jensen 2006) only significant differences were reported, which we also took to be a sign of a high risk of bias. In Finnema 2005 the results for nursing assistants consisted of covariance analyses that were not prespecified and because of this we judged the study to be at high risk of bias. In Rowe 2006 authors report only the results of the Maslach Burnout Inventory (MBI) at each follow‐up point, but when we made contact the author explained that this was the plan all along. We therefore assessed the study as being at low risk of bias.
Other potential sources of bias
There were several risks of bias that came up in addition to the risks mentioned above, such as an unclear washout period in a cross‐over trial (Lai 2011), very low compliance with the intervention (Ketelaar 2013) or a loosely validated outcome measure (Ghazavi 2010). If we found nothing else then we left the other potential source of bias as unclear in the 'Risk of bias' tool.
Effects of interventions
Summary of findings for the main comparison. Cognitive‐behavioural intervention compared to no Intervention for reducing stress.
| Cognitive‐behavioural intervention compared to no Intervention for reducing stress | ||||||
| Patient or population: Healthcare workers Settings: Health Care Intervention: Cognitive‐behavioural intervention Comparison: No Intervention (SMD) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No Intervention | Cognitive‐behavioural intervention | |||||
| Stress 1 Month Various Measurement Instruments Follow‐up: 0 ‐ 1 month | The median stress level across all control groups across all follow‐up times was 24.33 points on the Emotional Exhaustion subscale of the Maslach Burnout Inventory¹ | The mean stress level at 1 month in the intervention groups was 1.22 points lower (2.98 lower to 0.59 higher). | SMD ‐0.27 (‐0.66 to 0.13) | 332 (6 studies) | ⊕⊕⊝⊝ low²,³ | This meta‐analysis was back transformed to the EE subscale of the MBI by using the median SD of the EE scale across control groups. |
| Stress 1 ‐ 6 months Various Instruments. Scale from: 0 to 2. Follow‐up: 1 ‐ 6 months | The median stress level across all control groups across all follow‐up times was 24.33 points on the Emotional Exhaustion subscale of the Maslach Burnout Inventory¹ | The mean stress at 1 ‐ 6 months in the intervention groups was 1.83 points lower (0.77 to 2.85 lower). | SMD ‐0.38 (‐0.59 to ‐0.16) | 549 (8 studies) | ⊕⊕⊝⊝ low²,³ |
This meta‐analysis was back transformed to the EE subscale of the MBI by using the median SD of the EE scale across control groups. |
| Stress > 6 months Various Instruments Follow‐up: > 6 months | The median stress level across all control groups across all follow‐up times was 24.33 points on the Emotional Exhaustion subscale of the Maslach Burnout Inventory¹ | The mean stress at more than 6 months in the intervention groups was 11.34 points lower (4.47 to 14.94 lower) | SMD ‐1.04 (‐1.37 to ‐0.70) | 157 (2 studies) | ⊕⊕⊝⊝ low²,³ |
This meta‐analysis was back transformed to the EE subscale of the MBI by using the median SD of the EE scale across control groups. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 This was the median from the control groups of all studies that measured the effect of CBT vs. no intervention on Emotional Exhaustion with the same scale. 2 Most studies were at a high risk of bias 3 Publication bias detected with funnel plot
Summary of findings 2. Relaxation compared to no intervention (SMD) for reducing stress.
| Relaxation compared to no intervention (SMD) for | ||||||
| Patient or population: Healthcare workers Settings: Health care Intervention: Relaxation Comparison: No intervention (SMD) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| no intervention (SMD) | Relaxation | |||||
| Stress 1 month | The median stress level across all control groups across all follow‐up times was 22.17 points on the Emotional Exhaustion subscale of the Maslach Burnout Inventory¹ | The mean stress at 1 month in the intervention groups was 2.14 points lower (0.36 to 3.96 lower). | SMD ‐0.48 (‐0.89 to ‐0.08) | 97 (4 studies) | ⊕⊕⊝⊝ low |
This meta‐analysis was back transformed to the EE subscale of the MBI by using the median SD of the EE scale across control groups. |
| Stress 1 ‐ 6 months | The median stress level across all control groups across all follow‐up times was 22.17 points on the Emotional Exhaustion subscale of the Maslach Burnout Inventory¹ | The mean stress at 1 ‐ 6 months in the intervention groups was 4.84 points lower (2.37 to 6.92 lower). | SMD ‐0.49 (‐0.78 to ‐0.21) | 521 (12 studies) | ⊕⊕⊕⊝ moderate |
This meta‐analysis was back transformed to the EE subscale of the MBI by using the median SD of the EE scale across control groups. |
| Stress > 6 months | The median stress level across all control groups across all follow‐up times was 22.17 points on the Emotional Exhaustion subscale of the Maslach Burnout Inventory¹ | The mean stress at > 6 months in the intervention groups was 5.67 points lower (3.39 to 7.95 lower). | SMD ‐1.89 (‐2.65 to ‐1.13) | 40 (1 study) | ⊕⊕⊝⊝ low |
This result was back transformed to the EE subscale of the MBI by using the median SD of the EE scale across control groups. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 This was the median from the control groups of all studies that measured the effect of relaxation vs. no intervention on Emotional Exhaustion with the same scale.
Cognitive‐behavioural interventions
1. Cognitive‐behavioural intervention vs. no intervention
1.1. Any stress‐related outcome (Follow‐up to one month)
1.1.1 Cognitive‐behavioural intervention only vs. no intervention
We could combine the results of four studies (Gardner CBT 2005; Martins 2011; Rowe 2006; Yamagishi 2008) (Analysis 1.1; 248 participants ). There was a standardised mean difference (SMD) of ‐0.25 (95% confidence interval (CI) ‐0.60 to 0.11) showing no difference in stress between the cognitive‐behavioural training (CBT) intervention and no intervention at up to one month follow‐up. The meta‐analysis of this subgroup did not have considerable heterogeneity (I² = 43%).
1.1. Analysis.
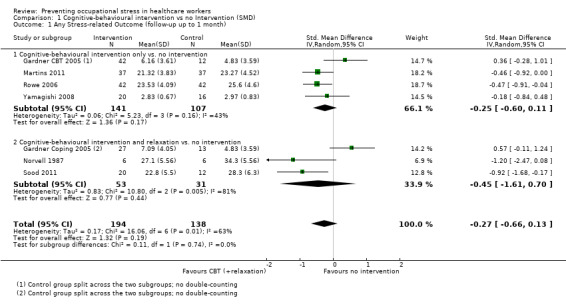
Comparison 1 Cognitive‐behavioural intervention vs no Intervention (SMD), Outcome 1 Any Stress‐related Outcome (follow‐up up to 1 month).
1.1.2 Cognitive‐behavioural intervention and relaxation vs. no intervention
According to three studies (Gardner Coping 2005; Norvell 1987; Sood 2011) stress levels were similar for the combined cognitive‐behavioural plus relaxation intervention when compared with no intervention at up to one month follow‐up (SMD ‐0.45; 95% CI ‐1.61 to 0.70; Analysis 1.1; 84 participants).
When the above seven studies are combined, stress levels are similar following cognitive‐behavioural intervention with or without relaxation and no intervention (SMD ‐0.27; 95% CI ‐0.66 to 0.13) at up to one month follow‐up (Analysis 1.1). Because of the sizeable heterogeneity (I² = 81%) caused by Gardner Coping 2005, we employed the random effects model in this meta‐analysis.
The funnel plot revealed a lack of studies in the right lower quadrant of the funnel where the small negative studies would be expected, indicating that there could be publication bias (Figure 3). The meta‐analysis combining both subgroups also suffered from considerable heterogeneity (I² = 63%) that was entirely due to Gardner Coping 2005.
3.
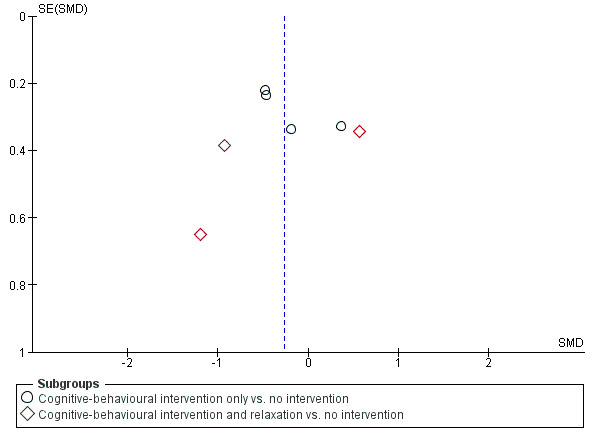
Funnel plot of comparison: 1 Cognitive‐behavioural intervention vs no Intervention (SMD), outcome: 1.1 Any Stress‐related Outcome (follow‐up up to 1 month).
1.2 Any stress‐related outcome (Follow‐up from one to six months)
1.2.1 Cognitive‐behavioural intervention only vs. no intervention
According to six studies (Delvaux 2004; Ketelaar 2013; Gärtner 2013; Günüsen 2010; Kwok 2012; Rowe 2006), a cognitive‐behavioural intervention decreased stress more than no intervention (SMD ‐0.28; 95% CI ‐0.47 to ‐0.09; 439 participants) at one to six months follow‐up (Analysis 1.2).
1.2. Analysis.
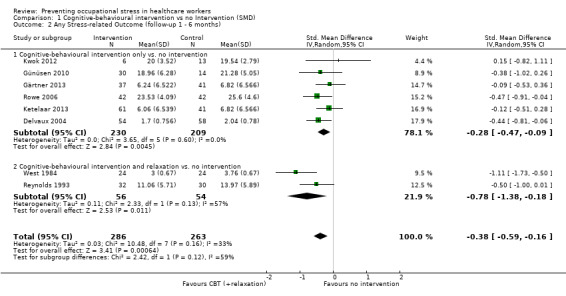
Comparison 1 Cognitive‐behavioural intervention vs no Intervention (SMD), Outcome 2 Any Stress‐related Outcome (follow‐up 1 ‐ 6 months).
1.2.2 Cognitive‐behavioural intervention and relaxation vs. no intervention
Another two studies (Reynolds 1993; West 1984) showed that cognitive‐behavioural intervention combined with relaxation decreased stress more than no intervention (SMD ‐0.78; 95% CI ‐1.38 to ‐0.18; 110 participants) at one to six months follow‐up (Analysis 1.2).
When the above eight studies are combined, cognitive‐behavioural intervention with or without relaxation reduces stress when compared to no intervention (SMD ‐0.38; 95% CI ‐0.59 to ‐0.16) at one to six months follow‐up (Analysis 1.2).
Also here the funnel plot indicated the potential presence of publication bias (Figure 4). There was some heterogeneity (I² = 33%) that could be explained by the greater effect in studies that combined CBT with relaxation.
4.
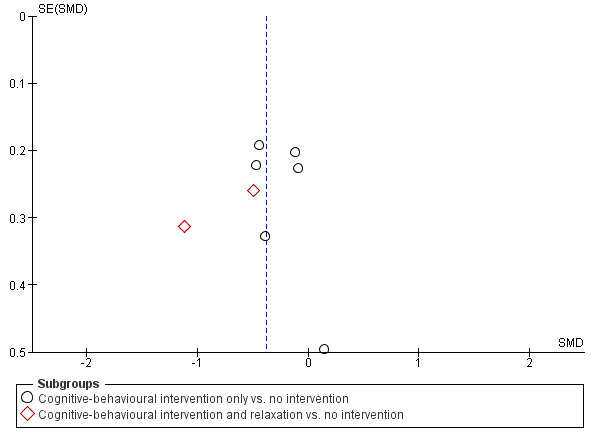
Funnel plot of comparison: 1 Cognitive‐behavioural intervention vs no Intervention (SMD), outcome: 1.2 Any Stress‐related Outcome (follow‐up 1 ‐ 6 months).
1.3 Any stress‐related outcome (Follow‐up more than six months)
1.3.1 Cognitive‐behavioural intervention with or without relaxation vs. no intervention
One study (Rowe 2006) showed that a cognitive‐behavioural intervention decreased stress more than no intervention (SMD ‐1.18; 95% CI ‐1.64 to ‐0.71; 84 participants) at more than six months follow‐up (Analysis 1.3). The intervention consisted of refresher courses at regular intervals and the effect was measured at two‐year follow‐up.
1.3. Analysis.
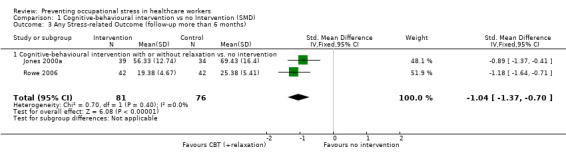
Comparison 1 Cognitive‐behavioural intervention vs no Intervention (SMD), Outcome 3 Any Stress‐related Outcome (follow‐up more than 6 months).
The results of another study (Jones 2000a) favoured a cognitive‐behavioural intervention combined with relaxation in reducing stress when compared to no intervention (SMD ‐0.89; 95% CI ‐1.37 to ‐0.41; 73 participants) at more than six months follow‐up (Analysis 1.3).
When the above two studies are combined, cognitive‐behavioural intervention with or without relaxation appears to reduce stress when compared to no intervention (SMD ‐1.04; 95% CI ‐1.37 to ‐0.70) at more than six months follow‐up (Analysis 1.3). Given the lack of heterogeneity in results (I² = 0%), we employed the fixed‐effect model in this meta‐analysis.
1.4 Anxiety (Follow‐up to one month)
Both state and trait anxiety decreased in the CBT plus relaxation intervention studies (Jones 2000a; Von Baeyer 1983; West 1984; 135 participants) more than after no intervention: mean difference (MD) ‐11.07; 95% CI ‐18.39 to ‐3.75 and MD ‐8.36; 95% CI ‐10.02 to ‐6.70 at one month follow‐up (Analysis 1.4).
1.4. Analysis.
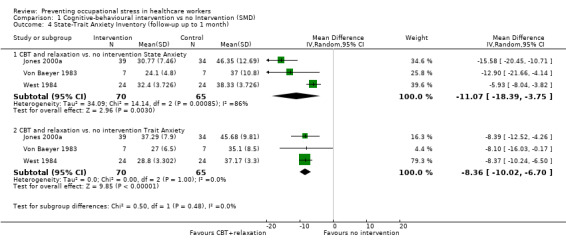
Comparison 1 Cognitive‐behavioural intervention vs no Intervention (SMD), Outcome 4 State‐Trait Anxiety Inventory (follow‐up up to 1 month).
1.5 Anxiety (Follow‐up one to six months)
Also at six months follow‐up there was a similar difference for both state and trait anxiety between CBT plus relaxation (Jones 2000a; 73 participants) and no intervention in one study: MD ‐8.05; 95% CI ‐12.10 to ‐4.00; and MD ‐6.00; 95% CI ‐10.30 to ‐1.70 at one to six months follow‐up (Analysis 1.5).
1.5. Analysis.
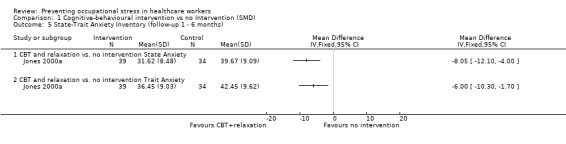
Comparison 1 Cognitive‐behavioural intervention vs no Intervention (SMD), Outcome 5 State‐Trait Anxiety Inventory (follow‐up 1 ‐ 6 months).
1.6 General Health Questionnaire (FU up to one month)
There was no effect in one study of CBT plus relaxation on the General Health Questionnaire score compared to no intervention (Gardner CBT 2005) (MD 0.29; 95% CI ‐1.96 to 2.54; 27 participants) (Analysis 1.6).
1.6. Analysis.
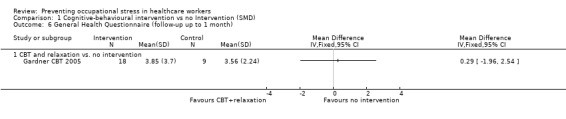
Comparison 1 Cognitive‐behavioural intervention vs no Intervention (SMD), Outcome 6 General Health Questionnaire (follow‐up up to 1 month).
2. Cognitive‐behavioural intervention vs. non‐stress‐management intervention
2.1 Any stress scale (Follow‐up from one to six months)
Two studies (Lee 1994; Lökk 2000) measured the effects of a cognitive‐behavioural intervention on decreasing stress when compared to an alternative intervention (computer training or passive attendance of psychologist at staff meetings) by using different stress measures with one to six months follow‐up. The stress levels after the intervention and the control condition were similar (SMD ‐0.54 95% CI ‐1.16 to 0.08; 83 participants) (Analysis 2.1). Given the differences in interventions and outcome measures, we employed the random effects model in this meta‐analysis.
2.1. Analysis.
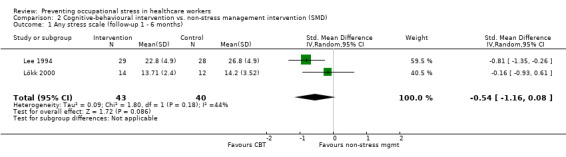
Comparison 2 Cognitive‐behavioural intervention vs. non‐stress management intervention (SMD), Outcome 1 Any stress scale (follow‐up 1 ‐ 6 months).
2.2 Any stress scale (Follow‐up more than six months)
One study (Jensen 2006) did not find a considerable effect of a cognitive‐behavioural intervention compared to an alternative intervention (lessons of the participant's own choice on e.g. skin care, proper treatment of a person with diabetes, work and asthma, and safety procedures in chemicals handling) on decreasing stress at more than six months follow‐up (SMD 0.03; 95% CI ‐0.53 to ‐0.59; 49 participants) (Analysis 2.2).
2.2. Analysis.
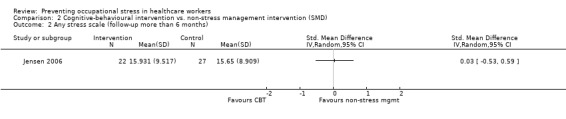
Comparison 2 Cognitive‐behavioural intervention vs. non‐stress management intervention (SMD), Outcome 2 Any stress scale (follow‐up more than 6 months).
2.3 Anxiety (Follow‐up one to six months)
One study measured anxiety but did not find a considerable effect on anxiety of CBT compared to an alternative intervention (MD ‐0.12; 95% CI ‐1.94 to 1.70; 26 participants) (Analysis 2.3).
2.3. Analysis.
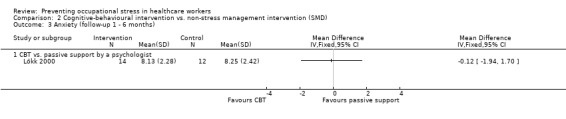
Comparison 2 Cognitive‐behavioural intervention vs. non‐stress management intervention (SMD), Outcome 3 Anxiety (follow‐up 1 ‐ 6 months).
Relaxation interventions
3. Relaxation vs. no intervention
3.1 Any stress outcome (Follow‐up to one month)
3.1.1 Physical relaxation vs. no intervention
Four studies (Hansen 2006; Lemaire 2011; Palumbo 2012; Saganha 2012) compared physical relaxation with no intervention at decreasing stress at up to a month follow‐up. The pooled SMD (‐0.48; 95% CI ‐0.89 to ‐0.08; 97 participants) favoured physical relaxation and there was no heterogeneity (Analysis 3.1).
3.1. Analysis.
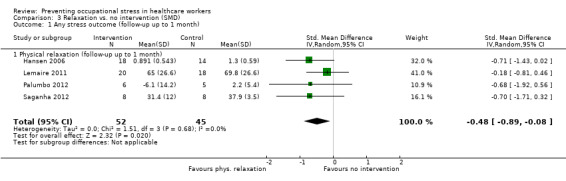
Comparison 3 Relaxation vs. no intervention (SMD), Outcome 1 Any stress outcome (follow‐up up to 1 month).
3.2 Any stress outcome (Follow‐up from one to six months)
3.2.1 Mental relaxation vs. no intervention
Six studies (Cohen‐Katz 2005; Mackenzie 2006; Moody 2013; Oman 2006; Shapiro 2005; Stanton 1988) found that mental relaxation was not more effective than no intervention at decreasing stress (SMD ‐0.50; 95% CI ‐1.15 to 0.15; 205 participants) at one to six months follow‐up (Analysis 3.2).
3.2. Analysis.
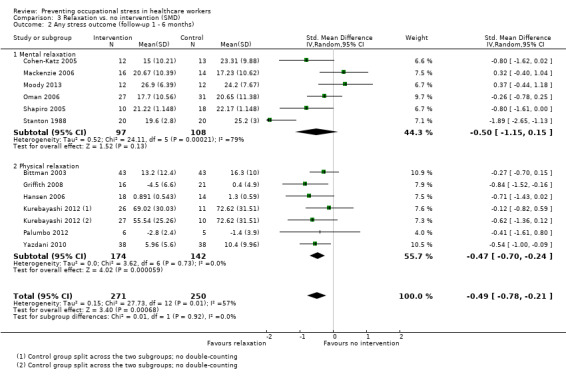
Comparison 3 Relaxation vs. no intervention (SMD), Outcome 2 Any stress outcome (follow‐up 1 ‐ 6 months).
3.2.2 Physical relaxation vs. no intervention
Six studies (7 comparisons) (Bittman 2003; Griffith 2008; Hansen 2006; Kurebayashi 2012 (two arms); Palumbo 2012; Yazdani 2010) found that physical relaxation was more effective than no intervention at decreasing stress (SMD ‐0.47; 95% CI ‐0.70 to ‐0.24; 316 participants) at one to six months follow‐up (Analysis 3.2)
Pooling the results of both mental and physical relaxation gives a SMD of ‐0.49 (95% CI ‐0.78 to ‐0.21) but with substantial heterogeneity (I² = 57%), which is mostly due to the oldest study (Stanton 1988). If we remove this outlier study from the meta‐analysis, the magnitude of effect reduces to SMD ‐0.38 ; 95% CI ‐0.59 to ‐0.17) whilst bringing I² value down to 18%. The funnel plot does not indicate publication bias (Figure 5)
5.
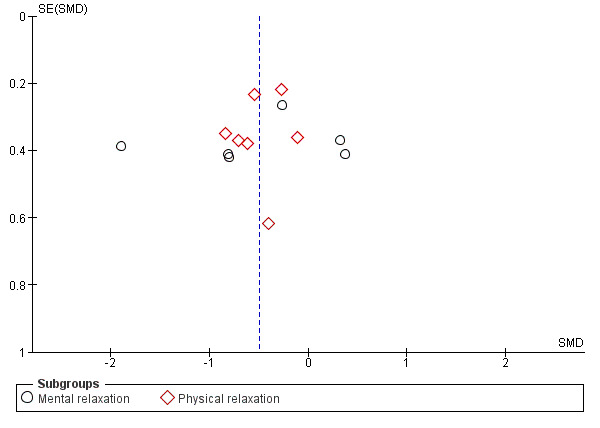
Funnel plot of comparison: 3 Relaxation vs. no intervention (SMD), outcome: 3.2 Any stress outcome (follow‐up 1 ‐ 6 months).
3.3 Any stress outcome (Follow‐up more than 6 months)
3.3.1 Mental relaxation vs. no intervention
According to one study (Stanton 1988) mental relaxation was more effective than no intervention at decreasing stress (SMD ‐1.89; 95% CI ‐2.65 to ‐1.13; 40 participants) at more than six months follow‐up (Analysis 3.3).
3.3. Analysis.
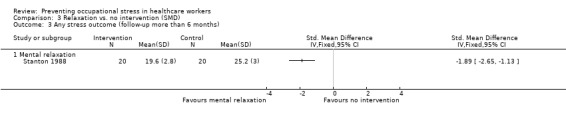
Comparison 3 Relaxation vs. no intervention (SMD), Outcome 3 Any stress outcome (follow‐up more than 6 months).
3.4 Any anxiety outcome (Follow‐up time from 1 to 6 months)
3.4.1 Mental relaxation vs. no intervention
One study (Yung 2004; 65 participants) found a difference in State Anxiety between participants in the control group and participants that received a cognitive relaxation intervention (Analysis 3.4), but not on Trait Anxiety (Analysis 3.5)
3.4. Analysis.
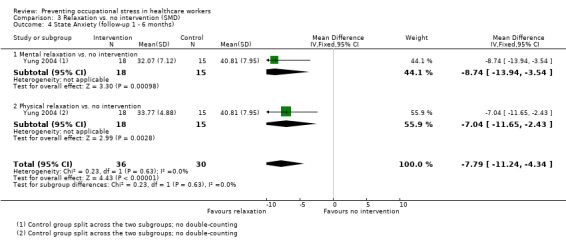
Comparison 3 Relaxation vs. no intervention (SMD), Outcome 4 State Anxiety (follow‐up 1 ‐ 6 months).
3.5. Analysis.
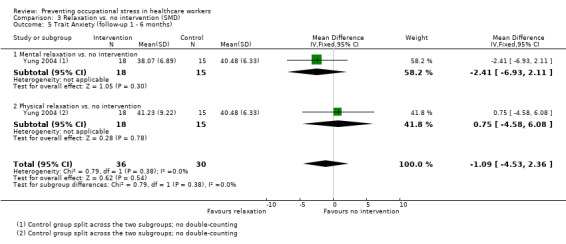
Comparison 3 Relaxation vs. no intervention (SMD), Outcome 5 Trait Anxiety (follow‐up 1 ‐ 6 months).
3.4.2 Physical relaxation vs. no intervention
The same study (Yung 2004) also found a difference in State Anxiety between participants in the control group and participants that received a stretch‐release relaxation intervention (Analysis 3.4), but again not on Trait Anxiety (Analysis 3.5).
However, when we combined the data from the two interventions (making sure we included control group data only once), we found that relaxation decreased State Anxiety when compared to no intervention (SMD ‐7.79; 95% CI ‐11.24 to ‐4.34) at one to six months follow‐up (Analysis 3.4) but not Trait Anxiety (SMD ‐1.09; 95% CI ‐4.53 to 2.36) (Analysis 3.5).
4. Relaxation vs. other intervention
4.1 Any stress outcome
4.1.1 Mental relaxation vs. in‐service education (Follow‐up from one to six months)
One study (Tsai 1993) showed that mental relaxation reduced stress more effectively than attending a course on theory analysis (SMD ‐0.61; 95% CI ‐0.97 to ‐0.24; 122 participants) when measured at five weeks after the intervention (Analysis 4.1).
4.1. Analysis.
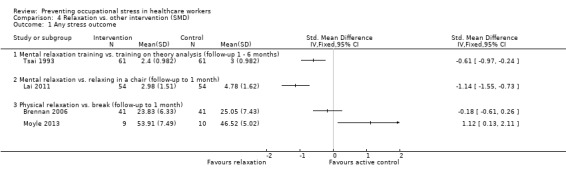
Comparison 4 Relaxation vs. other intervention (SMD), Outcome 1 Any stress outcome.
4.1.2 Mental relaxation versus relaxing in a chair (Follow‐up to one month)
Lai 2011 found listening to music more effective in reducing stress levels than just relaxing in a chair (SMD ‐1.14; 95% CI ‐1.55 to ‐0.73; 108 participants) (Analysis 4.1)
4.1.3 Physical relaxation vs. a break (Follow‐up to one month)
Another study (Brennan 2006; 82 participants ) found similar stress levels in participants that were given a 10‐minute massage and in those that took a self‐directed 10‐minute break when measured directly following the intervention. Moyle 2013 compared foot‐massage to silent resting under similar conditions and found resting to be more effective but there were only 19 participants (Analysis 4.1)
4.2 Any anxiety outcome
4.2.1 Physical relaxation vs. standard touch therapy
One study (McElligott 2003) did not find a significant difference in anxiety between participants who had received AMMA therapeutic massage and those who had received the control procedure where the practitioners only held their hands on certain areas of the participants' bodies (SMD ‐0.17; 95% CI ‐1.15 to 0.82; 18 participants) (Analysis 4.2).
4.2. Analysis.
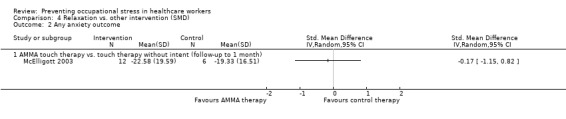
Comparison 4 Relaxation vs. other intervention (SMD), Outcome 2 Any anxiety outcome.
4.3 General Health Questionnaire
Tsai 1993 did not find a reduction in the score of the General Health Questionnaire (SMD ‐0.28; 95% CI ‐0.63 to 0.08; 122 participants) after mental relaxation compared to training in theory analysis (Analysis 4.3).
4.3. Analysis.
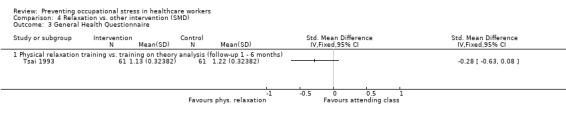
Comparison 4 Relaxation vs. other intervention (SMD), Outcome 3 General Health Questionnaire.
Organisational interventions
5. Organisational intervention vs. no intervention
5.1 Any stress‐related outcome (Follow‐up to one month)
5.1.1 Support interventions vs. no intervention
Li 2011 ( 49 participants) organised a peer‐support mentoring scheme among nurses and did not find a substantive difference between the intervention and no‐intervention control group (SMD ‐0.35; 95% CI ‐0.95 to 0.24) (Analysis 5.1). Salles 2013 reported beneficial effects on 'rates of burnout' in an RCT of an intervention aimed at preventing surgery residents from leaving the specialty by providing them with anecdotes on career choices from their seniors. Despite trying to contact the authors, we were not able to get enough information to include this study in the meta‐analysis.
5.1. Analysis.
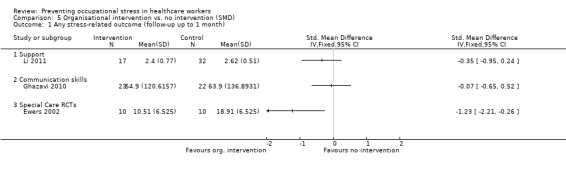
Comparison 5 Organisational intervention vs. no intervention (SMD), Outcome 1 Any stress‐related outcome (follow‐up up to 1 month).
5.1.2 Communication skills versus no intervention
Another study (Ghazavi 2010) compared the training of communication skills with the no‐intervention control group but did not find a difference at short‐term follow‐up (SMD ‐0.07; 95% CI ‐0.65 to 0.52; 45 participants)(Analysis 5.1).
5.1.3 Special care vs. no intervention
Ewers 2002 evaluated a special training programme called 'psychosocial intervention training' aimed at better handling of behaviorally problematic patients, and found a significant improvement in stress levels after the programme (SMD ‐1.23; 95% CI ‐2.21 to ‐0.26; 20 participants) (Analysis 5.1).
5.1.4 Changing working conditions vs. no intervention
Romig 2012 evaluated the use of telemedicine to decrease the work load of intensivists working at the Intensive Care Unit, but did not find a statistically significant change in the questions used to measure burnout. Because of the lack of reported data we could not include the study in a meta‐analysis. Proctor 1998 evaluated a training programme to improve work but did not find an effect on any of the six subscales of the occupational stress indicator. We could not combine these six subscales into one outcome and therefore could not include this study in the meta‐analysis.
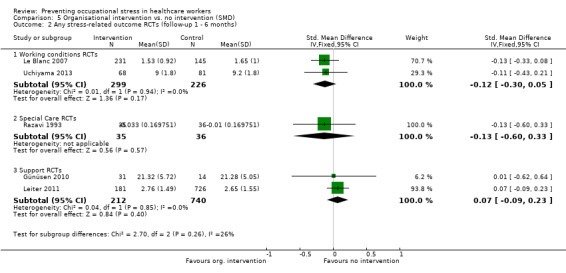
5.2 Any stress‐related outcome (Follow‐up one to six months)
5.2.1 Changing working conditions vs. no intervention
Two studies (Le Blanc 2007; Uchiyama 2013) compared an intensive participatory programme of improving psychosocial working conditions with no intervention, but there was no considerable effect on stress levels in the meta‐analysis (SMD ‐0.12; 95% CI ‐0.30 to 0.05; 525 participants) (Analysis 5.2).
5.2. Analysis.
Comparison 5 Organisational intervention vs. no intervention (SMD), Outcome 2 Any stress‐related outcome RCTs (follow‐up 1 ‐ 6 months).
5.2.2 Special care vs. no intervention
One study introduced special care (Razavi 1993) based on a 24‐hour training programme but did not find an effect on stress levels compared to no intervention (SMD ‐0.13; 95% CI ‐0.60 to 0.33; 71 participants) (Analysis 5.2).
5.2.3 Support organisation vs. no intervention
Two studies (Günüsen 2010; Leiter 2011) organised peer support to ameliorate psychosocial stressors but did not find a considerable effect on stress levels (SMD 0.07; 95% CI ‐0.09 to 0.23; 952 participants) (Analysis 5.2). One other RCT (Heaney 1995) found that the intervention did not significantly improve psychological well‐being measured as depressive symptoms and somatization compared to the no‐intervention control group. The study could not be included in the meta‐analysis because the authors reported only regression coefficients,
5.3 Any stress‐related outcome (Follow‐up more than six months)
5.3.1. Changing working conditions vs. no intervention: RCT
Melchior 1996 improved quality of care in an RCT but there was no considerable effect on stress levels compared to no intervention (SMD ‐0.23; 95% CI ‐0.55 to 0.09; 161 participants) (Analysis 5.3).
5.3. Analysis.
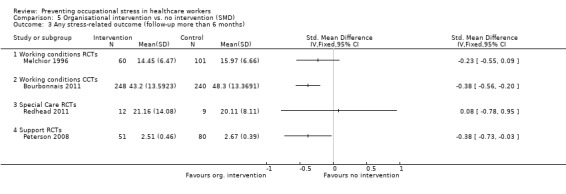
Comparison 5 Organisational intervention vs. no intervention (SMD), Outcome 3 Any stress‐related outcome (follow‐up more than 6 months).
5.3.2 Changing working conditions vs. no intervention: CCT:
Another study (Bourbonnais 2011) compared an intervention programme aimed at reducing psychosocial stressors at work with no intervention in a non‐randomised controlled design and found a lower level of stress at three years' follow‐up (SMD ‐0.38; 95% CI ‐0.56 to ‐0.20; 488 participants) (Analysis 5.3).
5.3.3 Special Care vs. no intervention
Redhead 2011 organised special care for managing symptoms in patients but the stress levels in staff were similar in the no‐intervention control group (SMD 0.08; 95% CI ‐0.78 to 0.95; 21 participants) (Analysis 5.3). Another study (Schrijnemaekers 2003) evaluated emotion‐oriented care for professional caregivers in homes for elderly persons. Due to a lack of detail in reporting of the data, we could not include the study in the meta‐analysis. At twelve months follow‐up, they reported a non‐significant difference between intervention and control group of 1.85 score points on the emotional exhaustion subscale of the Maslach Burnout Inventory (range 0 ‐ 48) in favour of the intervention group. For depersonalisation the score difference was 0.55 score points and also non‐significant. For personal accomplishment the score difference was 1.46 in favour of the intervention group and this was statistically significant.
5.3.4 Support vs. no intervention
In one RCT (Peterson 2008), the organisation of peer‐support groups led to a decrease of stress levels compared to no intervention (SMD ‐0.38; 95% CI ‐0.73 to ‐0.03; 131 participants) (Analysis 5.3)) at long‐term follow‐up. The same study found an increase on The Short Form Health Survey (SF‐36) score (MD 7.40; 95% CI 0.79 to 14.01) (Analysis 5.4).
5.4. Analysis.
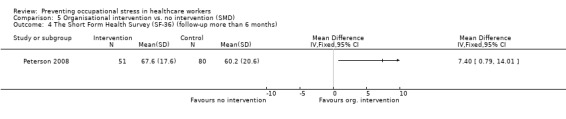
Comparison 5 Organisational intervention vs. no intervention (SMD), Outcome 4 The Short Form Health Survey (SF‐36) (follow‐up more than 6 months).
6. Organisational intervention vs. other intervention
6.1 Any stress‐related outcome (Follow‐up time up to one month)
6.1.1 Special care vs. usual care
One study (Finnema 2005) found similar levels of nurses' stress following the implementation of integrated emotion‐oriented care vs. care as usual (SMD 0.07; 95% CI ‐0.60 to 0.75; 46 participants) (Analysis 6.1).
6.1. Analysis.
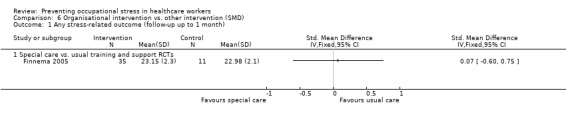
Comparison 6 Organisational intervention vs. other intervention (SMD), Outcome 1 Any stress‐related outcome (follow‐up up to 1 month).
6.2 Any stress‐related outcome (Follow‐up from one to six months)
6.2.1 Support intervention vs. feedback only
One study (Carson 1999) compared a course underlining the importance of social support as a key coping strategy when dealing with stress to only giving participants feedback on their baseline stress questionnaire results. They found similar levels of stress following the intervention and feedback only (SMD 0.53; 95% CI ‐0.02 to 1.08; 53 participants) (Analysis 6.2).
6.2. Analysis.
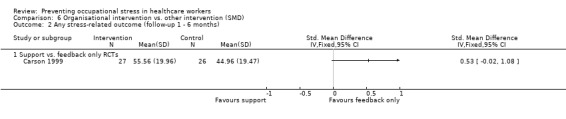
Comparison 6 Organisational intervention vs. other intervention (SMD), Outcome 2 Any stress‐related outcome (follow‐up 1 ‐ 6 months).
6.3 Any stress‐related outcome (Follow‐up time more than six months)
6.3.1 Shorter vs. longer working schedules
Ali 2011 compared a work schedule with weekend breaks to a continuous schedule among intensive care staff, and Lucas 2012 compared a two‐week with a four‐week schedule among resident physicians. We combined the results of the two studies because the interventions had a similar objective and they both measured emotional exhaustion as an outcome, even though it was measured in different ways. The results showed that the shorter schedule reduced stress (SMD ‐0.55; 95% CI ‐0.84 to ‐0.25; 180 participants) (Analysis 6.3).
6.3. Analysis.
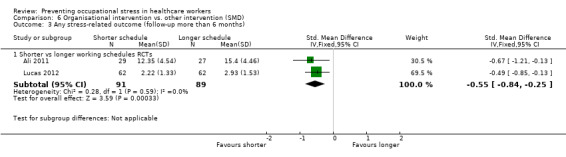
Comparison 6 Organisational intervention vs. other intervention (SMD), Outcome 3 Any stress‐related outcome (follow‐up more than 6 months).
6.4 General Health Questionnaire
Carson 1999 measured whether support decreased the score on the GHQ more than after feedback only, but results were similar in both groups (MD ‐0.57; 95% CI ‐3.34 to 2.20; 53 participants) (Analysis 6.4). Finnema 2005 also found no difference on the GHQ after introducing special care compared to care as usual (MD ‐4.48; 95% CI ‐10.46 to 1.50; 47 participants) .
6.4. Analysis.
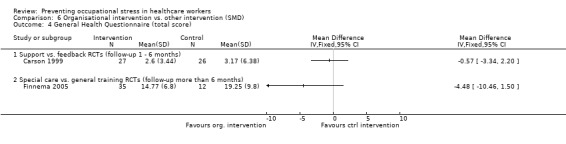
Comparison 6 Organisational intervention vs. other intervention (SMD), Outcome 4 General Health Questionnaire (total score).
GRADE assessment
For all major comparisons we made an assessment of the quality of the evidence. The arguments on which our decisions were based are given in Table 3 for the major comparisons which included more than three studies. For all the other comparisons, with fewer than three studies and fewer than 400 participants we decided to downgrade by two levels, because of risk of bias and imprecision, to low‐quality evidence.
1. GRADE assessment.
| Comparison | Risk of Bias | Inconsistency | Indirectness | Imprecision |
Publication Bias |
Level of Evidence |
|
CBT vs no intervention 1 mo follow‐up |
5 out of 6 studies high risk of bias: 1 level down |
I² = 64%: no downgrading |
No | 332 participants No downgrading |
Yes in funnel plot: 1 level down |
Low Quality |
|
CBT vs no intervention 1 ‐ 6 mo follow‐up |
5 out of 8 studies high risk of bias: 1 level down |
I² = 54%: no downgrading |
No | 549 participants No downgrading |
Yes in funnel plot: 1 level down |
Low Quality |
|
CBT vs no intervention > 6 months follow‐up |
2 studies high risk of bias: 1 level down |
I² = 38%: no downgrading |
No | 157 participants 1 level down |
Not apparent | Low Quality |
|
Relaxation vs no intervention 1 mo follow‐up |
3 out 4 studies high risk of bias: 1 level down |
I² = 0%: no downgrading |
No | 97 participants 1 level down |
Not apparent | Low Quality |
|
Relaxation vs no intervention 1 ‐ 6 mo follow‐up |
10 out of 13 studies high risk of bias: 1 level down |
I² = 57%: no downgrading |
No | 521 participants no downgrading |
Not apparent | Moderate Quality |
|
Relaxation vs no intervention > 6 mo follow‐up |
1 study: no downgrading |
N/A | No | 40 participants 2 levels down |
Not apparent | Low Quality |
Sensitivity analysis
Influence of study risk of bias
We defined low‐quality studies as those that had one or more domains at high risk of bias or no domain with a low risk of bias (i.e. all domains had an unclear or high risk of bias). We ignored the blinding issues here, because this applied similarly to all studies. This left us with 40 low‐quality studies, 17 moderate‐quality studies and one high‐quality study (Günüsen 2010).
Removing low‐quality studies from the comparison of CBT versus no intervention left only one study at less than one month follow‐up (Norvell 1987); the SMD was ‐1.20 (95% CI ‐2.47 to 0.08), i.e. substantially greater than with low‐quality studies included (SMD ‐0.25; 95% CI ‐0.60 to 0.11). Doing the same with the comparison at one to six months follow‐up left three studies (Delvaux 2004; Günüsen 2010; West 1984) with an SMD of ‐0.62 (95% CI ‐1.04 to ‐0.19), compared with SMD ‐0.28 (95% CI ‐0.47 to ‐0.09) across six studies. At six months' follow‐up there was only one study, so no sensitivity analysis was possible.
Removing low‐quality studies from the comparison relaxation versus no intervention left only one study at one month follow‐up, with an SMD of ‐0.71 (95% CI ‐1.43 to 0.02), compared with SMD ‐0.48 (95% CI ‐0.89 to ‐0.08) across four studies. At one to six months follow‐up, there were three studies left (Hansen 2006; Moody 2013; Stanton 1988) with an SMD of ‐0.79 (95% CI ‐1.23 to ‐0.35), compared to an SMD of ‐0.49 (95% CI ‐1.15 to 0.15) across 12 studies. Heterogeneity, however, remained high, with an I² of 88%, due to the presence of one study with a large effect (Stanton 1988). At six months follow‐up there was again only one study and thus sensitivity analysis was not possible.
For all the other comparisons there were too few studies to meaningfully re‐analyse the findings.
Influence of similarity of stress measurement instruments assumption
We checked the assumption that various stress measurement instruments measure the same stress concept and can be pooled with SMDs. We redid the analyses with only those studies that measured stress with the MBI. For CBT versus no intervention with a follow‐up of one month, there were two studies that could be included which showed significant improvements in emotional exhaustion (Analysis 7.1). However, the results on the other two subscales depersonalisation and lack of personal accomplishment were too heterogeneous to combine (Analysis 7.1). At medium‐term follow‐up there were two studies that could be included and that showed positive results for emotional exhaustion, non‐significant results for depersonalisation and for the lack of personal accomplishment subscale the results were too heterogeneous to combine (Analysis 7.2). The results for CBT including relaxation showed a decrease in emotional exhaustion but not for personal accomplishment. Results for the depersonalisation were not reported in these studies (Analysis 8.1). In the long‐term comparison of CBT versus another intervention, in one study, none of the scales showed significant differences (Analysis 9.1). Relaxation did not show beneficial effects on any of the subscales but an increase in the score on lack of personal accomplishment compared to no intervention at one to six months follow‐up (Analysis 10.1). Organisational interventions compared to no intervention showed favourable effects on the emotional exhaustion and depersonalisation subscales but not on the personal accomplishment subscale at less than a month's follow‐up (Analysis 11.1). At one to six months' follow‐up however, effects were non‐significant on the emotional exhaustion and depersonalisation subscales and the results were too heterogeneous to combine in meta‐analysis (Analysis 11.2). At more than six months' follow‐up, organisational interventions again yielded favourable effects on the emotional exhaustion and depersonalisation subscales but not on lack of personal accomplishment (Analysis 11.3). However, the one study that could not be included in the meta‐analyses (Schrijnemaekers 2003) yielded a significant effect on the personal accomplishment scale but not on the two other scales at the end of 12 months follow‐up. There was only one study that compared an organisation intervention with an alternative intervention and the results did not reach significance on any of the three subscales of the MBI (Analysis 12.1).
7.1. Analysis.
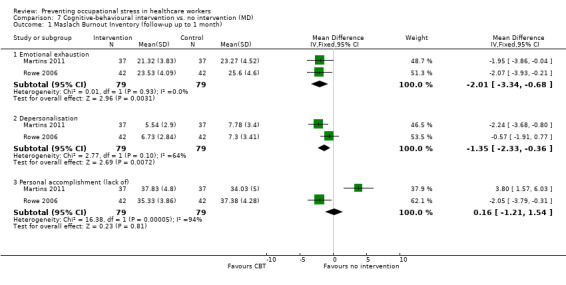
Comparison 7 Cognitive‐behavioural intervention vs. no intervention (MD), Outcome 1 Maslach Burnout Inventory (follow‐up up to 1 month).
7.2. Analysis.
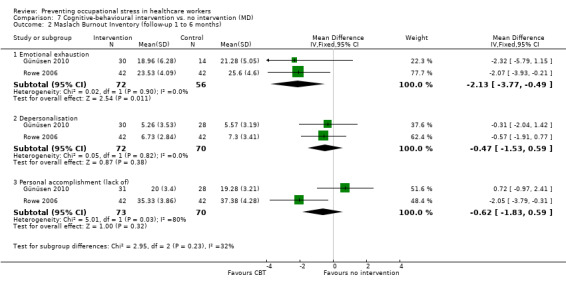
Comparison 7 Cognitive‐behavioural intervention vs. no intervention (MD), Outcome 2 Maslach Burnout Inventory (follow‐up 1 to 6 months).
8.1. Analysis.
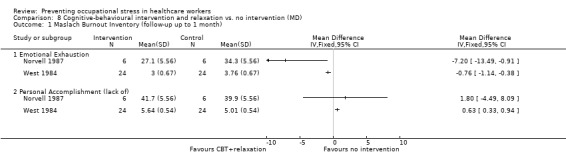
Comparison 8 Cognitive‐behavioural intervention and relaxation vs. no intervention (MD), Outcome 1 Maslach Burnout Inventory (follow‐up up to 1 month).
9.1. Analysis.
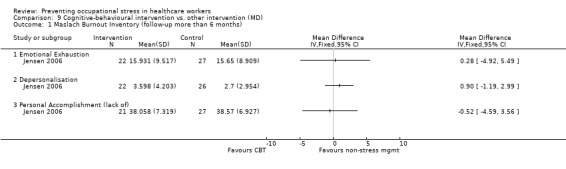
Comparison 9 Cognitive‐behavioural intervention vs. other intervention (MD), Outcome 1 Maslach Burnout Inventory (follow‐up more than 6 months).
10.1. Analysis.
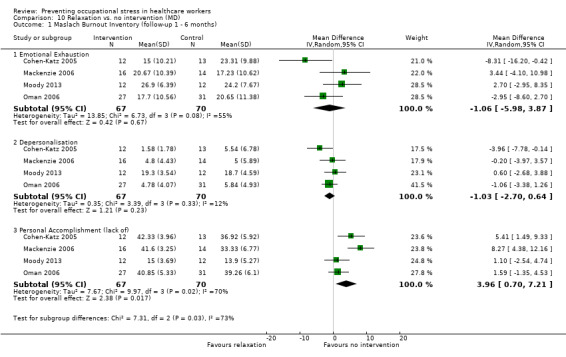
Comparison 10 Relaxation vs. no intervention (MD), Outcome 1 Maslach Burnout Inventory (follow‐up 1 ‐ 6 months).
11.1. Analysis.
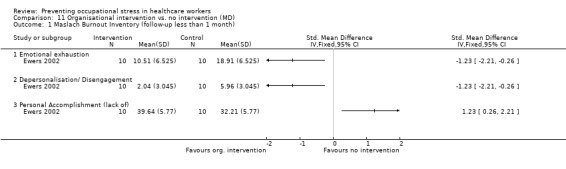
Comparison 11 Organisational intervention vs. no intervention (MD), Outcome 1 Maslach Burnout Inventory (follow‐up less than 1 month).
11.2. Analysis.
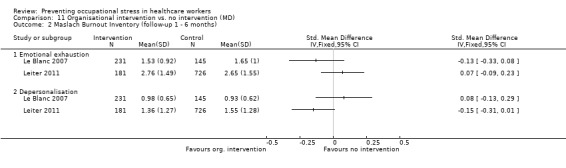
Comparison 11 Organisational intervention vs. no intervention (MD), Outcome 2 Maslach Burnout Inventory (follow‐up 1 ‐ 6 months).
11.3. Analysis.
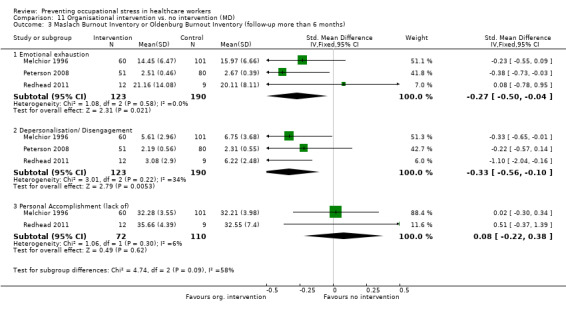
Comparison 11 Organisational intervention vs. no intervention (MD), Outcome 3 Maslach Burnout Inventory or Oldenburg Burnout Inventory (follow‐up more than 6 months).
12.1. Analysis.
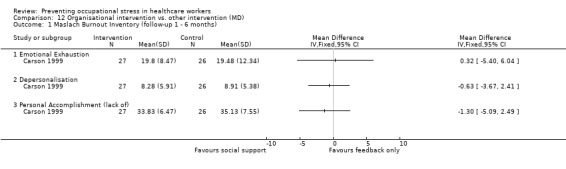
Comparison 12 Organisational intervention vs. other intervention (MD), Outcome 1 Maslach Burnout Inventory (follow‐up 1 ‐ 6 months).
All in all, this analysis shows that meta‐analysis results are similar when combining all stress‐related measures or when using the emotional exhaustion or the depersonalisation subscale, but not when using the personal accomplishment subscale. It could be that it is more difficult to change someone's score on the personal accomplishment subscale with an intervention. Another possible explanation is that with healthcare workers this domain is the least affected to begin with.
Subgroup analysis and explanation of heterogeneity
Since working conditions differ considerable between various occupations in health care, we analysed if there were differences in the effects of CBT and relaxation between various occupations. We did so only for comparisons with sufficient studies: CBT vs. no intervention and relaxation vs. no intervention (Analysis 13.1; Analysis 13.2; Analysis 14.1; Analysis 14.2). We ignored the previous subgroups in the CBT and relaxation intervention categories and divided the studies according to the occupation of the participants into nurses, physicians, all staff and other healthcare professionals. There were no differences between these subgroups. Within the subgroups however, there was still considerable statistical heterogeneity. We therefore do not think that the occupation of the participants explains statistical heterogeneity between studies.
13.1. Analysis.
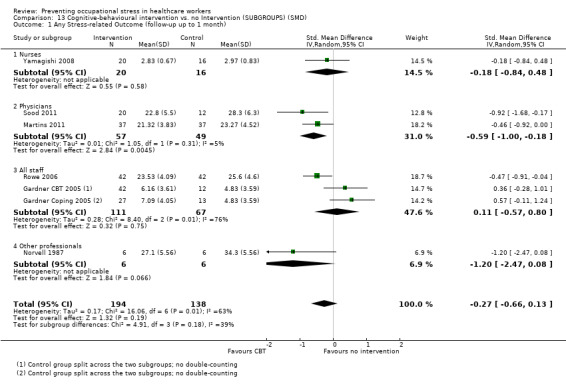
Comparison 13 Cognitive‐behavioural intervention vs. no Intervention (SUBGROUPS) (SMD), Outcome 1 Any Stress‐related Outcome (follow‐up up to 1 month).
13.2. Analysis.
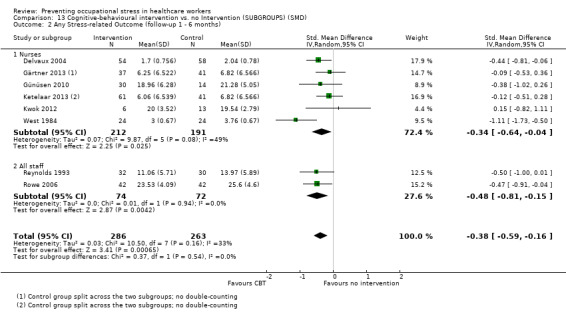
Comparison 13 Cognitive‐behavioural intervention vs. no Intervention (SUBGROUPS) (SMD), Outcome 2 Any Stress‐related Outcome (follow‐up 1 ‐ 6 months).
14.1. Analysis.
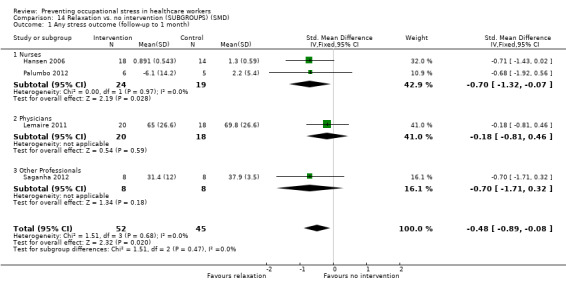
Comparison 14 Relaxation vs. no intervention (SUBGROUPS) (SMD), Outcome 1 Any stress outcome (follow‐up to 1 month).
14.2. Analysis.
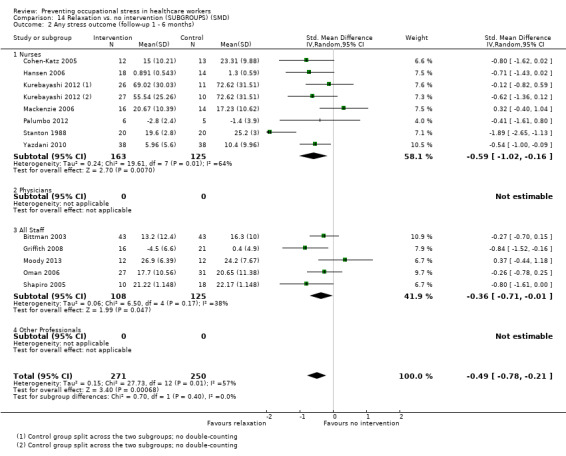
Comparison 14 Relaxation vs. no intervention (SUBGROUPS) (SMD), Outcome 2 Any stress outcome (follow‐up 1 ‐ 6 months).
Discussion
Summary of main results
We found low‐quality evidence that cognitive‐behavioural training (CBT) interventions with or without relaxation techniques in healthcare workers reduce the levels of burnout symptoms when compared to no intervention at one to six months in eight studies of 549 people (standardised mean difference (SMD) ‐0.38) and more than six months follow‐up in two studies of 157 people (SMD ‐1.04). At less than one month of follow‐up the difference was not significant. This was not influenced by excluding low‐quality studies nor by types of participants.
Translated back to the emotional exhaustion (EE) subscale of the Maslach Burnout Inventory (MBI), and assuming a standard deviation (SD) of 7.1 (the median of all intervention and control groups that used the MBI EE subscale), an SMD of ‐0.38 means a decrease in the intervention group of 2.7 score points on the EE subscale of the MBI. The median of all control groups' score on this scale of the MBI was 21. Thus the intervention decreases the stress levels by 13% (95% confidence interval (CI) 5% to 20%). Since no clinically or minimally important differences are known for the MBI, this can probably be best considered a modest effect. For comparisons of CBT with other active interventions, there were no considerable differences. It was difficult to draw conclusions because controls varied and most were used in single studies only.
With relaxation interventions the reductions in stress levels were comparable with those of CBT. There was low‐ to moderate‐quality evidence that stress levels remained lower at one month follow‐up, in four studies of 97 people (SMD ‐0.48), at one to six months in 12 studies of 521 people (SMD ‐0.49) and at more than six months in one study of 40 people (SMD ‐1.89). There were no significant differences between physical relaxation such as massage or mental relaxation such as mindfulness meditation. Comparisons of relaxation versus other interventions were difficult to judge because the control groups varied and could not be pooled. The results were at best inconsistent.
There was low‐quality evidence in two studies that changing work schedules reduced stress levels. Other organisational interventions did not lead to considerable reductions of stress levels at any of the three follow‐up times. This conclusion, however, is mostly based on single studies only.
Overall completeness and applicability of evidence
Studies have been performed in many countries and almost all continents except for Africa. Even though we did not perform a specific subgroup analysis, It does not seem that there are differences in effect between different cultures. Chinese relaxation techniques like Qigong are equally applicable in Europe, and conversely CBT seems to lead to effects in Japanese nurses similar to those in US nurses.
Studies have been performed in various healthcare occupations. In the previous version of this review, stress management interventions were almost exclusively studied in nurses, but now a few studies have also been conducted with physicians. We believe that this is important because it is conceivable that the interventions would have a different effect among physicians. We did a formal subgroup analysis of the effect in various healthcare occupations. There were no differences in effect between the subgroups but the power of the test to detect these differences is low.
Recently, the number of studies has increased enormously, with the majority of studies having been published after 2010. This means that the evidence is recent and well applicable to current healthcare situations.
A wide range of person‐directed interventions has been studied, from aroma therapy, massage, music‐making and Qigong to more formal CBT techniques that address the relation between thoughts and emotions. Also when it comes to organisational interventions, a wide range has been studied, varying from the creation of support groups to changing the content of care.
As to the outcomes, it is unclear what the main aim of the interventions is. For example, the MBI discerns three specific aspects of burnout: emotional exhaustion, depersonalisation and lack of personal accomplishment. It is unclear if the various interventions aim to prevent specific aspects of burnout or if they aim only to reduce emotional exhaustion.
Quality of the evidence
The quality of the evidence that we found was not very high. Some studies applied rigorous methods but contended with attrition problems. Most randomised controlled trials (RCTs) had fewer than 120 participants, especially those that examined relaxation techniques. For a SMD of ‐0.38 and using Lehr's formula, a sample size of 110 is sufficient to find a significant difference with P < 0.05 and 80% power (Petrie 2006). Reporting quality was low, with most studies not reporting adequately on random number generation or allocation concealment. We assumed that outcomes that were measured by questionnaire were reported blind to the researchers but we could not be certain about this assumption.
In many studies, it seems that healthcare workers themselves are most interested in the effects of stress management interventions on themselves and their colleagues. This does not always lead to the best quality studies. Formal power calculations are often missing and the personnel of one single department are randomised into an intervention and a control group. Given the great interest in stress prevention in healthcare staff, it would be good if those setting up new studies were better educated on how to design and conduct studies so that risk of bias is minimised.
Even though we found significant results, it is not possible to say how this is related to the clinical relevance of the changes achieved in the studies. With the MBI (Maslach 1996), for example, there is no generally accepted change that would be regarded as clinically relevant. We contacted the authors of the questionnaire but they could not help clarify this issue for us.
Potential biases in the review process
We assumed that the various stress measurement instruments measured the same aspect of perceived stress. There is some evidence that the emotional exhaustion scale of the MBI can be replaced by a single‐item question on self‐defined burnout (Rohland 2004). Given that we found considerable heterogeneity between studies, this assumption is not supported by the evidence. However, we also presented the results separately for studies that used the MBI, and presented the results as the original scales of the MBI, not transformed into SMDs. Even though only a fraction of all the studies could be included, this analysis showed similar results. We therefore believe that the results based on SMDs are reliable.
We had to categorise the interventions ourselves. There is no major framework available for categorising preventive stress interventions. We believe that the main categorisation into person‐ and work‐directed interventions is useful because it is considerably more difficult to change organisational structures or to introduce new organisational elements than to organise an individual stress management course. However, many interventions such as organising peer support groups or mentoring schemes are difficult to classify as either person‐ or work‐directed interventions. If the categorisation of the interventions had been different, then the results could also have changed. However, we do not think that this would have affected our main conclusions based on CBT, relaxation and organisational interventions.
We took follow‐up times into account when pooling the various study results. This led to a spread of studies over various follow‐up times. With different categories of follow‐up times, the comparisons would have been different and possibly also the results. Resources to evaluate the effects of these assumptions were lacking. We do not know how different effects of stress management interventions are at various follow‐up times. It could be that combining all studies with a follow‐up longer than one month is also sensible. We believe that a more conservative approach is warranted if no clear evidence for similar effects is available.
We included reports of studies in all languages and therefore believe that there is no language bias in our review.
We assessed publication bias based on fairly small samples of studies (seven, eight and 13 respectively) and we downgraded the level of evidence in two comparisons based on suspicion of publication bias. As The Cochrane Handbook (Higgins 2011) recommends using a minimum of ten studies to assess publication bias, this may have led to a too conservative estimate of the quality of the evidence.
Agreements and disagreements with other studies or reviews
Reviews on stress prevention in nurses
When compared to older reviews such as Mimura 2003, our review, even though it used more rigorous inclusion criteria, only accepting randomised controlled trials for person‐directed interventions, found 51 more trials. Where Mimura 2003 refrained from drawing clear conclusions based on the studies found, we could make better inferences. Jones 2000b reviewed studies in nurses and student nurses but only for the time period 1992 to 1999, and is mainly narrative. Gilbody 2006 reviewed interventions to improve the morale of staff, restricted to mental healthcare workers only. It reached more or less the same conclusion as our review, even though the number of studies included was fewer and they used a wider range of outcome measures and study designs. Paris 2010 reviewed intervention effectiveness in mental healthcare workers but they located only two non‐randomised intervention studies. They conclude that many strategies to prevent burnout that are mentioned in the literature have not been evaluated, such as the introduction of competitive salaries, financial and non‐financial incentives, opportunities for promotion and career advancement, increased staffing levels, clear job descriptions or expectations, and open‐door policies with management. For other possible interventions that they mention we found evidence in our review: training staff on self‐care strategies, additional clinical supervision and mentoring, routine assessment of burnout, flexible work schedules, social events and informal support as well as in‐service training. Galbraith 2011 studied intervention effects in student nurses. The review located 16 studies and concluded that relaxation and skills for changing maladaptive cognitions were effective. In addition, the authors concluded that interventions that promoted skills to reduce stressors were also successful but that there was no effect on academic performance. They agree with our conclusions that the design of stress interventions should be more driven by theory. Pulido‐Martos 2012 reviewed 23 studies on sources of stress in student nurses and found that, in addition to stress from academic performance, students perceived stress from clinical situations such as fear of unknown situations, mistakes with patients or handling of technical equipment. It is unclear if current interventions would also address these factors, even though better individual stress‐management in general would probably also work in these situations.
Reviews on stress prevention in all occupations
The quality of the evidence that we found was also better than Michie 2003 found, as their sample consisted almost entirely of cross‐sectional studies. Another review by Van der Klink 2001 involved a meta‐analysis of interventions to prevent or treat stress in all occupations. In line with the results of this version of our review, Van der Klink 2001 concluded that there was no evidence in favour of work‐directed interventions. Richardson 2008 performed a systematic review and meta‐analysis of RCTs of stress management interventions in any occupation. They found 36 studies and pooled all of them, resulting in an SMD of 0.526 (95% CI 0.36 to 0.69). In their analysis, cognitive‐behavioral programmes produced larger effects than other types of interventions. Treatment length, outcome type, and occupation did not reveal significant variations in effect size by intervention type. These results are comparable with ours but we found that the effects of relaxation and CBT were similar. The review missed many studies performed in health care because the authors did not search MEDLINE.Theirs was the only review that assessed publication bias. Using the trim‐and‐fill method they found only a weak indication of publication bias for CBT studies. Awa 2010 reviewed, up until 2007, 25 intervention studies aimed at preventing burnout. They included all before‐and‐after evaluations but only with burnout‐like outcome measures such as the MBI. They concluded that person‐directed interventions reduced burnout in the short term (six months or less), while a combination of both person‐ and organisation‐directed interventions had longer‐lasting positive effects (12 months and over). In all cases, positive intervention effects diminished over the course of time. These conclusions are not clear from our review. This could be due to the different categorisation of interventions, but also to the fact that the authors did not perform meta‐analysis. Chiesa 2009 identified 10 studies that evaluated mindfulness‐based stress reduction and found that mindfulness‐based interventions are effective in reducing stress. Based on one study they concluded, in line with our review, that mindfulness‐based interventions produced effects similar to physical relaxation. They rated the quality of the evidence as low and proposed to compare mindfulness‐based interventions with other non‐specific interventions. Malgorzata 2010 gave a general overview of organisational interventions aimed at reducing stress, but this was not a systematic review.
Overviews of systematic reviews
Günthner 2010 gave an overview of systematic reviews on stress management as burnout prevention. They conclude that CBT is the most effective intervention even though they did not perform a network meta‐analysis. They concluded that booster sessions are beneficial. Bhui 2012 also gave a narrative overview of the effectiveness of individual, organisational and mixed interventions on mental health based on 23 systematic reviews. They concluded that meta‐analyses found a greater effect size of individual interventions on individual outcomes. Organisational interventions showed mixed evidence of benefit. In contrast to our review, they found that cognitive‐behavioural programmes produced larger effects at the individual level compared with other interventions. They did not address the possibility of publication bias.
It seems therefore that no review has covered all recent studies on stress management in healthcare staff published after 2010. Most of the other reviews did not examine the possibility of publication bias favouring beneficial results. Compared to other reviews, our conclusions are more tentative.
Authors' conclusions
Implications for practice.
There is low‐quality evidence that cognitive‐behavioural training with or without relaxation leads to modest decreases in stress levels (relative risk reduction 13%; 95% CI 5% to 20%) compared to no intervention. Low‐quality evidence shows that similar reductions can be achieved by relaxation techniques, either physical such as massage or mental such as mindfulness, also compared to no intervention. There is low‐quality evidence that changing working schedules reduces stress levels. Organisational changes such as improving work conditions, organising support or organising special care models do not lead to considerable effects on stress levels, but this finding is based only on one or two studies each.
Implications for research.
Randomised trials of better quality are needed. Studies should have at least 60 participants in each arm to avoid a small‐studies effect. Cross‐over studies are best avoided because it is unclear if a washout period can prevent contamination and how long such a period should be. Cluster‐randomised trials should adjust their results for the clustering effect and report the cluster‐coefficients. Attrition bias should be avoided by reducing dropout and by the use of better methods of imputation of missing values. Follow‐up time should be at least one year, to be sure that results of the intervention are lasting.
Studies in physicians are lacking.
Stress‐management, preferably of one clear category, should be compared with a placebo‐like active control and both options should be offered as being equal to prevent bias from self report.
Better theoretical underpinning is needed of how organisational interventions would lead to an individual stress reduction. The interventions could also be more focused on specific stressors such as work schedules.
A better validation of the main outcome measures such as the Maslach Burnout Inventory (MBI) is needed. Initially, a study into the development of a minimal relevant or clinically relevant difference is necessary to be better able to judge results from trials. It would also help to interpret the findings if the three subscales of the MBI could be combined in a summary score. If this is not possible then there should be a clear formulation of which dimensions of the MBI should be improved by the intervention. Studies should not include more than one primary outcome stress measurement, to prevent false‐positive findings based on multiple outcome measurement.
The quality of reporting (random number generation, allocation concealment, blinding) should be improved.
Feedback
Mistake in reporting length of follow‐up, 16 January 2015
Summary
Name: Paul Landsbergis
Email Address: paul.landsbergis@downstate.edu
Affiliation: SUNY Downstate School of Public Health
Comment: I have just read your excellent review of studies stress prevention among health care workers in the Cochrane Collaboration 2014. In this paper you write:
"5.3.2 Changing working conditions vs. no intervention: CCT: Another study (Bourbonnais 2011) compared an intervention programme aimed at reducing psychosocial stressors at work with no intervention in a non‐randomised controlled design and found a lower level of stress at one month follow‐up (SMD ‐0.38; 95%CI ‐0.56 to ‐0.20; 488 participants) (Analysis 5.3)."
However, you have included the Bourbonnais study (and rightly so) in the category of "5.3 Any stress‐related outcome (Follow‐up more than six months)". The 2011 paper reports results from a 3‐year follow‐up of the intervention and control hospitals. Therefore, I am wondering if perhaps the phrasing in the paragraph "lower level of stress at one month follow‐up" is a typographical error?
I agree with the conflict of interest statement below:
I certify that I have no affiliations with or involvement in any organization or entity with a financial interest in the subject matter of my feedback.
Reply
Thank you for your comment. We read the article again and we saw that you are correct.
We corrected the text in the Results section, under comparison 5.3.2. Now it says: "Another study (Bourbonnais 2011) compared an intervention programme aimed at reducing psychosocial stressors at work with no intervention in a non‐randomised controlled design and found a lower level of stress at three years' follow‐up (SMD ‐0.38; 95% CI ‐0.56 to ‐0.20; 488 participants) (Analysis 5.3)."
Contributors
Jani Ruotsalainen, Jos Verbeek
Mistake in reporting results of a general health measure, 28 January 2015
Summary
Name: Ulla Peterson
Email Address: ulla.peterson@lnu.se
Comment: The sentence on page 22: "However, the same study found an increase in symptoms on the General Health Questionnaire (MD 7.40; 95% CI 0.79 to 14.01) (Analysis 5.4)." is not consistent with the result presented in the article Peterson et al. (2008). As stated in that article: "Vitality and general health were assessed using the Short Form Health Survey (SF‐36; Sullivan et al. 1994, 1995, Sullivan & Karlsson 1998). The vitality score, which consist of 4 items, measures the frequency with which the respondent feels full of life and has a lot of energy, or feels tired and worn out. The general health score measures perceived general health status and consists of 5 items. The scales were transformed to a 0–100 scale using a transformation formula where 100 represents best possible health status." The result therefore shows an increase in self‐rated health rather than an increase in symptoms after participation in reflecting peer‐support groups.
I agree with the conflict of interest statement below:
I certify that I have no affiliations with or involvement in any organization or entity with a financial interest in the subject matter of my feedback.
Reply
Thank you for your comment. We read the article again and we saw that you are correct.
We switched the graph labels in analysis 5.4 around so that now the left side of the forest plot favours no intervention and the right side favours intervention. This means that the intervention group experienced an increase in health, rather than of symptoms, and that is a good thing.
We also corrected the text in the Results section, under comparison 5.3.4. Now it says: "The same study found an increase on The Short Form Health Survey (SF‐36) score (MD 7.40; 95% CI 0.79 to 14.01) (Analysis 5.4)."
Contributors
Jani Ruotsalainen, Jos Verbeek
What's new
| Date | Event | Description |
|---|---|---|
| 31 March 2015 | Amended | We received feedback from Paul Landsbergis and Ulla Peterson saying we had reported results of two included studies wrong. With Bourbonnais 2011, the mistake was a typo in the effects of interventions text describing length of follow‐up being less than a month when it was in fact three years. We corrected the text accordingly. With Peterson 2008, we had erroneously labelled an outcome as having been the General Health Questionnaire when the authors had actually used the Short Form Health Survey (SF‐36). We had also mistakenly reported the result as favouring no intervention because we had understood it meaning an increase in symptoms when in fact it favoured the organisational intervention group by showing an increase in general health. We switched the forest plot labels around and corrected the text, thus fixing the problem. |
| 31 March 2015 | Feedback has been incorporated | We appended the comments sent by Paul Landsbergis and Ulla Peterson verbatim into the Feedback section and also explained there how we amended the review. |
| 5 December 2014 | Amended | Corrected a small error (18% to 13%) in the PLS. |
| 9 July 2014 | New citation required and conclusions have changed | We added 38 studies and reorganised the analyses to be more informative. |
| 30 October 2013 | New search has been performed | We updated the review and merged it with the review entitled Preventive staff‐support interventions for health workers by Brian van Wyk and Victoria Pillay‐van Wyk because of considerable overlap. |
| 4 November 2008 | Amended | Converted to new review format. |
History
Protocol first published: Issue 2, 2000 Review first published: Issue 4, 2006
| Date | Event | Description |
|---|---|---|
| 21 August 2006 | New citation required and conclusions have changed | Substantive amendment |
Notes
The title of this review has changed from Effectiveness of occupational stress management programmes to Preventing occupational stress in healthcare workers. The review entitled Preventive staff‐support interventions for health workers by Brian van Wyk and Victoria Pillay‐van Wyk has been merged with this review and therefore will not be updated separately.
Acknowledgements
We thank Merja Jauhiainen, at the time the Cochrane Occupational Health Field Trials Search Coordinator, for completely rebuilding the systematic searches to replace the ones run for the first published version of this review. We thank the Cochrane Occupational Safety and Health Review Group's Trials Search Co‐ordinator Leena Isotalo for conducting the many rounds of update searches. We thank Brian Lucas, Lone Donbæk Jensen, Ulla Peterson, Veron Schrijnemaekers, Andrea Martins, Ingalill Rahm Hallberg, Dirk von Dierendonck, Martyn Jones, Deborah McElligott, Michelle Rowe and Joanne Cohen‐Katz for providing further information about their studies and Albert Westergren for kindly facilitating contact with one of the authors. We thank Joan Martí and to Hugh McGuire for their support in identifying studies for this review. We thank Marjo Pulliainen for performing study selection on a study published in Finnish (Elo 2000). We thank Brian van Wyk and Victoria Pillay‐van Wyk for their work on their review titled Preventive staff‐support interventions for health workers (van Wyk 2010) that we merged with this review. We thank Johannes Siegrist, Diego Montano, Steven Pryjmachuk, Anneli Ojajärvi, Kaisa Neuvonen and Jukka Vuori for their valuable comments and Malcolm Sim for his worthy contribution as stand‐in Co‐ordinating Editor. Finally, we thank Kate Cahill for copy editing the text.
Appendices
Appendix 1. Medline / Pubmed search strategy
25.11.2013
#1 "Health Personnel"[Majr] OR "health personnel"[tiab] OR "health care personnel"[tw] OR "healthcare personnel"[tw] OR "health care worker"[tw] OR "health care workers"[tw] OR "healthcare worker"[tw] OR "healthcare workers"[tw] OR "health worker"[tw] OR "health workers"[tw] OR "health professional"[tw] OR "health professionals"[tw] OR "health care professional"[tw] OR "health care professionals"[tw] OR "healthcare professional"[tw] OR "healthcare professionals"[tw] OR "medical care personnel"[tw] OR nurse[tiab] OR nurses[tiab] OR nursing[tw] OR physician[tiab] OR physicians[tiab]
#2 "Burnout, Professional"[Mesh] OR burnout[tiab] OR "psychological workload"[tw]
#3 "Stress, Psychological"[Mesh] OR "Anxiety"[Mesh:NoExp] OR "Depression"[Mesh] OR anxie*[tw] OR anxious*[tw] OR depress*[tw] OR stress*[tw] OR strain[tw] OR burden*[tw] OR "psychological load"[tw]
#4 work[tw] OR works*[tw] OR work'*[tw] OR worka*[tw] OR worke*[tw]OR workg*[tw] OR worki*[tw] OR workl*[tw] OR workp*[tw] OR occupation*[tw] OR job[tw] OR jobs [tw] OR employee*[tw]
#5 #3 AND #4
#6 (program* [tw] OR "prevention and control" [sh]) AND (occupational [tw] OR worker* [tw])
#7 (randomized controlled trial[pt] OR controlled clinical trial[pt] OR randomized controlled trials[mh] OR random allocation[mh] OR double‐blind method[mh] OR single‐blind method[mh] OR clinical trial[pt] OR clinical trials[mh] OR "clinical trial"[tw] OR ((singl*[tw] OR doubl*[tw] OR trebl*[tw] OR tripl*[tw]) AND (mask*[tw] OR blind*[tw])) OR "latin square"[tw] OR placebos[mh] OR placebo*[tw] OR random*[tw] OR research design[mh:noexp] OR comparative study[pt] OR evaluation studies as topic[mh] OR evaluation studies[pt] OR follow‐up studies[mh] OR prospective studies[mh] OR cross‐over studies[mh] OR control*[tw] OR prospectiv*[tw] OR volunteer*[tw]) NOT (animal[mh] NOT human[mh])
#8 "Costs and Cost Analysis"[Mesh] OR "economics"[MeSH Subheading] OR econom*[tiab] OR cost[tw] OR costs[tw]
#9 #1 AND (#2 OR #5) AND (#6 OR #7 OR #8)
Appendix 2. PsycINFO (ProQuest) search strategy
26.11.2013
#9 limit 8 to yr="2008 ‐Current"
#8 3 and 7
#7 4 or 5 or 6
#6 ((occupational or work or worker or workers or working or workplace or worksite or job) and (stress or strain or anxiety or anxious or depressive or depression or burden)).mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures]
#5 ("job stress" or burnout or "burn out").mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures]
#4 "Occupational Stress"/
#3 #1 or #2
#2 ("healthcare personnel" or "health care worker" or "health care workers" or "healthcare worker" or "healthcare workers" or "health worker" or "health workers" or "health professional" or "health professionals" or "healthcare professional" or "healthcare professionals" or nurses or nursing or physician or physicians or "medical care personnel").mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures]
#1 "Health Personnel"/ or "Allied Health Personnel"/ or "Medical Personnel"/ or "Mental Health Personnel"/
Appendix 3. NIOSHTIC‐2 search strategy
23.5.2012
DC{OUNIOS} AND GW{stress or burnout or strain or depress* or anxiety or anxious or burden or burn out} and GW{health care or healthcare* or health personnel or physician or physicians or nurse or nurses or nursing} and GW{random* or clinical or control* or double‐blind* or single‐blind* or placebo* or comparativ* or evaluat* or follow‐up* or cross‐over* or prospectiv*} and UD{> 201010}
2.12.2013
DC{OUNIOS} and GW{stress or burnout or strain or depress* or anxiety or anxious or burden or burn out} and GW{health care or healthcare* or health personnel or physician or physicians or nurse or nurses or nursing} and GW{random* or clinical or control* or double‐blind* or single‐blind* or placebo* or comparativ* or evaluat* or follow‐up* or cross‐over* or prospectiv*} and UD{> 201201}
Appendix 4. CENTRAL search strategy
2.12.2013
#1 burnout OR "burn out" OR "occupational stress" OR "job stress" OR "work stress" OR "work strain" #2 (occupational stress) OR (job stress) OR (work stress) OR (work strain)
#3" health personnel" OR "healthcare personnel" OR "health care worker" OR "healthcare worker" OR "health worker" OR "health workers" OR "health professional" OR "health care professional"
#4 (nurse OR nurses OR nursing OR physician OR physicians):ti,ab,kw
#5 (#1 OR #2)
#6 (#3 OR #4)
#7 (#5 AND #6)
Appendix 5. CINAHL (EBSCO) search strategy
23.5.2012
#1 (MM "Health Personnel")
#2 TX "healthcare personnel" OR "health care worker" OR "health care workers" OR "healthcare worker" OR "healthcare workers" OR "health worker" OR "health workers" OR "health professional" OR "health professionals" OR "healthcare professional" OR "healthcare professionals"
#3 TI nurses OR nursing OR physician OR physicians OR "medical care personnel"
#4 AB nurses OR nursing OR physician OR physicians OR "medical care personnel"
#5 MH "Burnout, Professional"
#6 MH "Stress, Occupational"
#7 #1 or #2 OR #3 or #4
#8 "job stress" OR burnout OR "burn out"
#9 (occupational OR work OR worker OR workers OR working OR workplace OR worksite OR job) and (stress OR strain OR anxiety OR anxious OR depressive OR depression OR burden)
#10 #5 OR #6 OR #8 OR #9
#11 #7 AND #10
#12 random* OR clinical* OR control* OR double‐blind* OR single‐blind* OR placebo* OR comparativ* OR evaluat* OR follow‐up* OR cross‐over* OR prospectiv* OR volunteer*
#13 #11 AND #12
#14 #11 and #12 (Limiters ‐ Published Date from: 20101101‐20120531; Exclude MEDLINE records)
27.11.2013
#1 MM "Health Personnel"
#2 TX "healthcare personnel" OR "health care worker" OR "health care workers" OR "healthcare worker" OR "healthcare workers" OR "health worker" OR "health workers" OR "health professional" OR "health professionals" OR "healthcare professional" OR "healthcare professionals"
#3 TI nurses OR nursing OR physician OR physicians OR "medical care personnel"
#4 AB nurses OR nursing OR physician OR physicians OR "medical care personnel"
#5 MH "Burnout, Professional"
#6 MH "Stress, Occupational"
#7 S1 OR #2 OR #3 OR #4
#8 job stress OR burnout OR "burn out"
#9 (occupational OR work OR worker OR workers OR working OR workplace OR worksite OR job) and (stress OR strain OR anxiety OR anxious OR depressive OR depression OR burden)
#10 #5 OR #6 OR #8 OR #9
#11 #7 AND #10
#12 random* OR clinical* OR control* OR double‐blind* OR single‐blind* OR placebo* OR comparativ* OR evaluat* OR follow‐up* OR cross‐over* OR prospectiv* OR volunteer*
#13 #11 AND #12
#14 #11 AND #12 (Limiters ‐ Published Date: 20120101‐20131231; Exclude MEDLINE records)
Appendix 6. Web of Science search strategy
21.11.2013 (* = Databases=SCI‐EXPANDED, SSCI, A&HCI Timespan=All years)
#1 TS=("health personnel" OR "health care personnel" OR "healthcare personnel" OR "health care worker" OR "health care workers" OR "healthcare worker" OR "healthcare workers" OR "health worker" OR "health workers") *
#2 TS=("health professional" OR "health professionals" OR "health care professional" OR "health care professionals" OR "healthcare professional") *
#3 TS=("healthcare professionals" OR "medical care personnel") *
#4 #3 OR #2 OR #1 *
# 5 TS=(burnout OR "psychological workload") *
# 6 TS=(stress OR anxiety OR depression OR anxious OR depressive OR strain OR burden OR "psychological load") AND TS=(work OR works OR worker OR workers OR workplace OR worksite OR occupation OR occupational OR job OR jobs OR employee OR employees) *
#7 #6 OR #5 *
#8 #7 AND TS=(physician OR physicians OR nurse OR nurses OR nursing) *
#9 #7 AND #4 *
#10 #9 OR #8 *
#11 TS=(program* OR prevention OR control) AND TS=(occupational OR worker*) *
#12 #11 AND #10 *
#13 #10 AND TS=("randomized controlled trial" OR "controlled clinical trial" OR "randomized controlled trials" OR "random allocation" OR "double‐blind" OR "single‐blind" OR "clinical trial" OR "clinical trials" OR ((singl* OR doubl* OR trebl* OR tripl*) AND (mask* OR blind*)) OR "latin square" OR placebos OR placebo OR random* OR "comparative study" OR "evaluation studies" OR "follow‐up" OR "cross‐over" OR control* OR prospectiv* OR volunteer*) *
#14 #13 OR #12 *
#15 #14 (Databases=SCI‐EXPANDED, SSCI, A&HCI Timespan=2012‐2013)
Data and analyses
Comparison 1. Cognitive‐behavioural intervention vs no Intervention (SMD).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Any Stress‐related Outcome (follow‐up up to 1 month) | 7 | 332 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.66, 0.13] |
| 1.1 Cognitive‐behavioural intervention only vs. no intervention | 4 | 248 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.60, 0.11] |
| 1.2 Cognitive‐behavioural intervention and relaxation vs. no intervention | 3 | 84 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐1.61, 0.70] |
| 2 Any Stress‐related Outcome (follow‐up 1 ‐ 6 months) | 8 | 549 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.59, ‐0.16] |
| 2.1 Cognitive‐behavioural intervention only vs. no intervention | 6 | 439 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.47, ‐0.09] |
| 2.2 Cognitive‐behavioural intervention and relaxation vs. no intervention | 2 | 110 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.78 [‐1.38, ‐0.18] |
| 3 Any Stress‐related Outcome (follow‐up more than 6 months) | 2 | 157 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.04 [‐1.37, ‐0.70] |
| 3.1 Cognitive‐behavioural intervention with or without relaxation vs. no intervention | 2 | 157 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.04 [‐1.37, ‐0.70] |
| 4 State‐Trait Anxiety Inventory (follow‐up up to 1 month) | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 CBT and relaxation vs. no intervention State Anxiety | 3 | 135 | Mean Difference (IV, Random, 95% CI) | ‐11.07 [‐18.39, ‐3.75] |
| 4.2 CBT and relaxation vs. no intervention Trait Anxiety | 3 | 135 | Mean Difference (IV, Random, 95% CI) | ‐8.36 [‐10.02, ‐6.70] |
| 5 State‐Trait Anxiety Inventory (follow‐up 1 ‐ 6 months) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 CBT and relaxation vs. no intervention State Anxiety | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 CBT and relaxation vs. no intervention Trait Anxiety | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 General Health Questionnaire (follow‐up up to 1 month) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 CBT and relaxation vs. no intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 2. Cognitive‐behavioural intervention vs. non‐stress management intervention (SMD).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Any stress scale (follow‐up 1 ‐ 6 months) | 2 | 83 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.54 [‐1.16, 0.08] |
| 2 Any stress scale (follow‐up more than 6 months) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3 Anxiety (follow‐up 1 ‐ 6 months) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 CBT vs. passive support by a psychologist | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 3. Relaxation vs. no intervention (SMD).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Any stress outcome (follow‐up up to 1 month) | 4 | 97 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐0.89, ‐0.08] |
| 1.1 Physical relaxation (follow‐up up to 1 month) | 4 | 97 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐0.89, ‐0.08] |
| 2 Any stress outcome (follow‐up 1 ‐ 6 months) | 12 | 521 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐0.78, ‐0.21] |
| 2.1 Mental relaxation | 6 | 205 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐1.15, 0.15] |
| 2.2 Physical relaxation | 6 | 316 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.47 [‐0.70, ‐0.24] |
| 3 Any stress outcome (follow‐up more than 6 months) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Mental relaxation | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 State Anxiety (follow‐up 1 ‐ 6 months) | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | ‐7.79 [‐11.24, ‐4.34] |
| 4.1 Mental relaxation vs. no intervention | 1 | 33 | Mean Difference (IV, Fixed, 95% CI) | ‐8.74 [‐13.94, ‐3.54] |
| 4.2 Physical relaxation vs. no intervention | 1 | 33 | Mean Difference (IV, Fixed, 95% CI) | ‐7.04 [‐11.65, ‐2.43] |
| 5 Trait Anxiety (follow‐up 1 ‐ 6 months) | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | ‐1.09 [‐4.53, 2.36] |
| 5.1 Mental relaxation vs. no intervention | 1 | 33 | Mean Difference (IV, Fixed, 95% CI) | ‐2.41 [‐6.93, 2.11] |
| 5.2 Physical relaxation vs. no intervention | 1 | 33 | Mean Difference (IV, Fixed, 95% CI) | 0.75 [‐4.58, 6.08] |
| 6 General Health (follow‐up 1 ‐ 6 months) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Mental relaxation vs. no intervention | 1 | 33 | Mean Difference (IV, Fixed, 95% CI) | ‐7.10 [‐11.39, ‐2.81] |
| 6.2 Physical relaxation vs. no intervention | 2 | 70 | Mean Difference (IV, Fixed, 95% CI) | ‐3.22 [‐6.53, 0.08] |
3.6. Analysis.
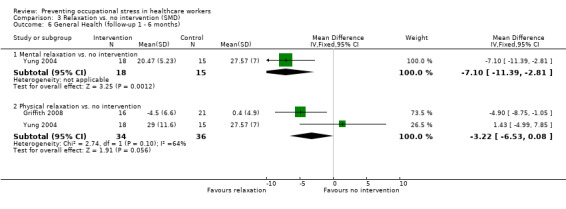
Comparison 3 Relaxation vs. no intervention (SMD), Outcome 6 General Health (follow‐up 1 ‐ 6 months).
Comparison 4. Relaxation vs. other intervention (SMD).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Any stress outcome | 4 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Mental relaxation training vs. training on theory analysis (follow‐up 1 ‐ 6 months) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Mental relaxation vs. relaxing in a chair (follow‐up to 1 month) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Physical relaxation vs. break (follow‐up to 1 month) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Any anxiety outcome | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 AMMA touch therapy vs. touch therapy without intent (follow‐up to 1 month) | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 General Health Questionnaire | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Physical relaxation training vs. training on theory analysis (follow‐up 1 ‐ 6 months) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 5. Organisational intervention vs. no intervention (SMD).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Any stress‐related outcome (follow‐up up to 1 month) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Support | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Communication skills | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Special Care RCTs | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Any stress‐related outcome RCTs (follow‐up 1 ‐ 6 months) | 5 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Working conditions RCTs | 2 | 525 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.12 [‐0.30, 0.05] |
| 2.2 Special Care RCTs | 1 | 71 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.13 [‐0.60, 0.33] |
| 2.3 Support RCTs | 2 | 952 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.09, 0.23] |
| 3 Any stress‐related outcome (follow‐up more than 6 months) | 4 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Working conditions RCTs | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Working conditions CCTs | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Special Care RCTs | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.4 Support RCTs | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 The Short Form Health Survey (SF‐36) (follow‐up more than 6 months) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 6. Organisational intervention vs. other intervention (SMD).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Any stress‐related outcome (follow‐up up to 1 month) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Special care vs. usual training and support RCTs | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Any stress‐related outcome (follow‐up 1 ‐ 6 months) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Support vs. feedback only RCTs | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Any stress‐related outcome (follow‐up more than 6 months) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Shorter vs longer working schedules RCTs | 2 | 180 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.55 [‐0.84, ‐0.25] |
| 4 General Health Questionnaire (total score) | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Support vs. feedback RCTs (follow‐up 1 ‐ 6 months) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Special care vs. general training RCTs (follow‐up more than 6 months) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 7. Cognitive‐behavioural intervention vs. no intervention (MD).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Maslach Burnout Inventory (follow‐up up to 1 month) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Emotional exhaustion | 2 | 158 | Mean Difference (IV, Fixed, 95% CI) | ‐2.01 [‐3.34, ‐0.68] |
| 1.2 Depersonalisation | 2 | 158 | Mean Difference (IV, Fixed, 95% CI) | ‐1.35 [‐2.33, ‐0.36] |
| 1.3 Personal accomplishment (lack of) | 2 | 158 | Mean Difference (IV, Fixed, 95% CI) | 0.16 [‐1.21, 1.54] |
| 2 Maslach Burnout Inventory (follow‐up 1 to 6 months) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Emotional exhaustion | 2 | 128 | Mean Difference (IV, Fixed, 95% CI) | ‐2.13 [‐3.77, ‐0.49] |
| 2.2 Depersonalisation | 2 | 142 | Mean Difference (IV, Fixed, 95% CI) | ‐0.47 [‐1.53, 0.59] |
| 2.3 Personal accomplishment (lack of) | 2 | 143 | Mean Difference (IV, Fixed, 95% CI) | ‐0.62 [‐1.83, 0.59] |
Comparison 8. Cognitive‐behavioural intervention and relaxation vs. no intervention (MD).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Maslach Burnout Inventory (follow‐up up to 1 month) | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Emotional Exhaustion | 2 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Personal Accomplishment (lack of) | 2 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 9. Cognitive‐behavioural intervention vs. other intervention (MD).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Maslach Burnout Inventory (follow‐up more than 6 months) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Emotional Exhaustion | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Depersonalisation | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Personal Accomplishment (lack of) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 10. Relaxation vs. no intervention (MD).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Maslach Burnout Inventory (follow‐up 1 ‐ 6 months) | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Emotional Exhaustion | 4 | 137 | Mean Difference (IV, Random, 95% CI) | ‐1.06 [‐5.98, 3.87] |
| 1.2 Depersonalisation | 4 | 137 | Mean Difference (IV, Random, 95% CI) | ‐1.03 [‐2.70, 0.64] |
| 1.3 Personal Accomplishment (lack of) | 4 | 137 | Mean Difference (IV, Random, 95% CI) | 3.96 [0.70, 7.21] |
Comparison 11. Organisational intervention vs. no intervention (MD).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Maslach Burnout Inventory (follow‐up less than 1 month) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Emotional exhaustion | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Depersonalisation/ Disengagement | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Personal Accomplishment (lack of) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Maslach Burnout Inventory (follow‐up 1 ‐ 6 months) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Emotional exhaustion | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Depersonalisation | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Maslach Burnout Inventory or Oldenburg Burnout Inventory (follow‐up more than 6 months) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Emotional exhaustion | 3 | 313 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.27 [‐0.50, ‐0.04] |
| 3.2 Depersonalisation/ Disengagement | 3 | 313 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.33 [‐0.56, ‐0.10] |
| 3.3 Personal Accomplishment (lack of) | 2 | 182 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐0.22, 0.38] |
Comparison 12. Organisational intervention vs. other intervention (MD).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Maslach Burnout Inventory (follow‐up 1 ‐ 6 months) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Emotional Exhaustion | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Depersonalisation | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Personal Accomplishment (lack of) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 13. Cognitive‐behavioural intervention vs. no Intervention (SUBGROUPS) (SMD).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Any Stress‐related Outcome (follow‐up up to 1 month) | 7 | 332 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.66, 0.13] |
| 1.1 Nurses | 1 | 36 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.84, 0.48] |
| 1.2 Physicians | 2 | 106 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.59 [‐1.00, ‐0.18] |
| 1.3 All staff | 3 | 178 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.57, 0.80] |
| 1.4 Other professionals | 1 | 12 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.20 [‐2.47, 0.08] |
| 2 Any Stress‐related Outcome (follow‐up 1 ‐ 6 months) | 8 | 549 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.59, ‐0.16] |
| 2.1 Nurses | 6 | 403 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.64, ‐0.04] |
| 2.2 All staff | 2 | 146 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐0.81, ‐0.15] |
Comparison 14. Relaxation vs. no intervention (SUBGROUPS) (SMD).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Any stress outcome (follow‐up to 1 month) | 4 | 97 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.48 [‐0.89, ‐0.08] |
| 1.1 Nurses | 2 | 43 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.70 [‐1.32, ‐0.07] |
| 1.2 Physicians | 1 | 38 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.18 [‐0.81, 0.46] |
| 1.3 Other Professionals | 1 | 16 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.70 [‐1.71, 0.32] |
| 2 Any stress outcome (follow‐up 1 ‐ 6 months) | 12 | 521 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐0.78, ‐0.21] |
| 2.1 Nurses | 7 | 288 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.59 [‐1.02, ‐0.16] |
| 2.2 Physicians | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 All Staff | 5 | 233 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.71, ‐0.01] |
| 2.4 Other Professionals | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ali 2011.
| Methods | RCT, Canada | |
| Participants | Physicians at 5 medical ICUs in academic medical hospitals in USA. Age 41 ± 6 years, Sex 76% men, Experience 8 ± ‐6 years. N = 39 | |
| Interventions | Experimental: Interrupted work schedule (IS) in which the weekends were taken over by someone else; Control: In the continuous schedule (CS) one intensivist was responsible for 14 days; duration 9 months. 14 participants took IS only, 12 took CS only and 13 alternated both schedules; effectively comparing 27 IS schedules with 25 CS schedules | |
| Outcomes | Burnout (on a scale from 5 ‐ 25) based on 5 questions similar to the MBI EE‐scale from the National Study of the Changing Workforce, a survey of United States workers performed by the Families and Work Institute, and formerly by the U.S. Department of Labor; also Job distress (on a scale from 6 ‐ 30) was measured but we did not use that scale. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Sites were randomized between CS‐IS‐CS and IS‐CS‐IS patterns" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 2 units dropped out after randomisation and the authors made no attempt to account for this |
| Selective reporting (reporting bias) | Low risk | There was no difference between Methods and Results. |
| Other bias | High risk | There were many more physicians in one of the intervention arms. |
Bittman 2003.
| Methods | Cross‐over study, USA | |
| Participants | 112 randomly selected staff of a retirement community | |
| Interventions | 1) Experimental: Recreational music‐making: 6 consecutive weekly 1‐hour sessions of playing drums and percussion instruments with Clavinova accompaniment (typically to a familiar tune) and non‐verbal expression (by playing the drums) in direct response to questions that were intended to inspire deep thought, contemplation and mutual respect. 2) Control: No intervention | |
| Outcomes | MBI, POMS | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "All subjects were randomly assigned to Group A or Group B (mean 10.6 subjects/group) based upon the crossover design." (p.3) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Reasons for not completing the study reported but not separately for the 2 groups. |
| Selective reporting (reporting bias) | High risk | All outcomes reported but no report about cross‐over interim analysis or use of proper t‐tests |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Bourbonnais 2011.
| Methods | Controlled clinical trial, Canada | |
| Participants | "The study population was composed of all care‐providing personnel in the experimental (n = 674) and control hospitals (n = 894), both of which offer general and specialised short‐term care. The population included all healthcare professionals in direct contact with patients (nurses and beneficiary attendants)." (p. 480). Of these, 467 participants remained at follow‐up (247 in the intervention group and 220 in the control group). | |
| Interventions | "The intervention was defined as changes undertaken by the hospital to reduce adverse psychosocial factors in the workplace. Solutions proposed by the intervention team and adopted by the nursing department as well as any other objective change introduced with the explicit goal (or actual consequence) of improving one of the four targeted psychosocial factors were considered part of the intervention." (p. 480) | |
| Outcomes | Client burnout, work burnout, personal burnout and psychological distress. In addition, the authors measured several intermediary outcomes such as psychological demands and decision latitude. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "This research used a before‐and‐after quasi‐experimental design with a control group." (p. 480) |
| Allocation concealment (selection bias) | High risk | There was no allocation concealment. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Low risk | All the measured outcomes were reported. |
| Other bias | Unclear risk | "It is difficult to identify which aspect of the intervention was responsible for the outcomes observed. In fact, even if the qualitative part of the study allowed to gather detailed information on what changes were made, still the design of the study was not experimental and as in most intervention research, changes in the workplace were beyond the researchers’ control." (pp. 483 ‐ 4) |
Brennan 2006.
| Methods | RCT, USA | |
| Participants | Nurses with at least 6 months full‐time bedside nursing in a hospital setting. Those who regularly receive massage therapy on their own as well as anyone with medical reasons for not being able to have chair massage were excluded. | |
| Interventions | 1) Experimental: Massage: application to the back, neck, shoulders, arms and hands. Techniques used were effleurage, petrissage, friction, vibration and compression. One 30‐minute session per person over 4 days 2) Control: 10‐minute self‐directed break | |
| Outcomes | The Perceived Stress Scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. |
| Allocation concealment (selection bias) | Low risk | "Sample size was 82 participants, randomly assigned to the massage group or the control group per a randomization schedule developed by a biostatistician who worked for the hospital but was not on the study team" (p. 337) |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "A total of 60 follow‐up surveys were completed, a 73% return rate" (p.339) |
| Selective reporting (reporting bias) | Low risk | There was only one outcome measured and reported. |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Carson 1999.
| Methods | RCT, UK | |
| Participants | 53 mental health nurses from 2 hospitals | |
| Interventions | 1) Experimental: Social support intervention: 5 consecutive weekly sessions of a minimum of 2 hours of group exercises underlining the importance of social support as key coping strategy when dealing with stress. 2) Control: Feedback only | |
| Outcomes | The DeVilliers Carson Leary Stress Scale, The General Health Questionnaire (GHQ‐28), The MBI | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "After allocation using sealed envelopes with random permuted blocks..." (p.33) |
| Allocation concealment (selection bias) | Low risk | "After allocation using sealed envelopes with random permuted blocks..." (p.33) |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "Attrition rates were similar in both conditions, at around 30%." (p. 31). Intention‐to‐treat analysis was not used. |
| Selective reporting (reporting bias) | Unclear risk | "...the Minnesota Job Satisfaction scale (Weiss et al., 1967) and the Cooper Coping Skills scale (Cooper et al., 1988b) were administered at Time 1 and Time 2." (p. 34) The results of these 2 outcomes were not reported. |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Cohen‐Katz 2005.
| Methods | RCT, USA | |
| Participants | 25 nurses, pastoral care, respiratory therapy and social work personnel | |
| Interventions | 1) Experimental: Mindfulness‐based stress reduction programme: 8‐week program with approximately 2.5 hours teaching per week and homework practice with audiotapes for six days a week. Group sessions included teaching on topics such as communication skills, stress reactivity and self‐compassion and experiential exercises to help participants integrate these concepts. 2) Control: No intervention | |
| Outcomes | MBI, Brief Symptom Inventory | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Participants were then randomly assigned to the treatment group or the wait‐list control group." (p.27) |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 2/14 in the treatment group did not return completed inventories and were not taken into consideration in the analyses. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Delvaux 2004.
| Methods | RCT, Belgium | |
| Participants | 115 oncology nurses | |
| Interventions | 1) Experimental: Psychological Training Program: 3 weeks of training (each week including 5 consecutive days) and 1 week for the consecutive 3 months. Programme included 30‐hour theoretical information and 75 hours of role‐playing and experiential exchanges. The programme was designed to decrease nurses' professional stress levels, to improve nurses' attitudes and communication skills. 2) Control: No intervention | |
| Outcomes | Nursing Stress Scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Every time 20 nurses were enrolled, the nurses were randomly allocated to a training group (TG) or to a control group (CG). |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Only 1 participant dropped out of the intervention group and none from the control group. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Ewers 2002.
| Methods | RCT, UK | |
| Participants | 20 forensic mental health nurses | |
| Interventions | 1) Experimental:Psychosocial Intervention Training: 20 days of training with the aim to improve nurses' knowledge about serious mental illness and attitude towards patients and thus decrease subjective burnout. Training duration 6 months. The training helps clinicians to conceptualise their patients' problems within a more empathic framework and trains them in the skills to intervene effectively. Thus self efficacy may increase and jobs may be perceived as more rewarding. 2) Control: No intervention | |
| Outcomes | MBI directly after training | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The 20 staff who volunteered for the PSI training were randomly allocated to either the experimental PSI training group (n=10) or a waiting list control group (n=10). The sample was stratified by ward, sex and day/night duty, thus subjects in each group represented all grades of staff and all wards." (p. 473) |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Presumably all participants completed all measurements as no data reported on dropouts. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Finnema 2005.
| Methods | RCT, Netherlands | |
| Participants | 99 nursing assistants | |
| Interventions | 1) Experimental: Integrated emotion‐oriented care: Basic training course of 2 days with an intermediary period of 2 weeks for homework (for all staff members on intervention wards) addressing staff members' own experience, phases of ego‐experience of the demented residents and the application of (non‐)verbal empathic skills Advanced course of 7 days spread out over 7 ‐ 8 months for 5 people from each intervention ward and an Adviser course of 10 days over 9 months for 1 person from each intervention ward. 2) Control: Training and support in giving usual care |
|
| Outcomes | The Organization and Stress Scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "A pretest‐posttest control group design with matched groups (randomized clinical trial) was used" (p. 331) |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "During the experimental period 25 nursing assistants dropped out due to: illness (11), pregnancy (2), and transfer (9). In three cases questionnaires were missing. Data analysis was carried out on 99 'complete' cases. Drop‐out did not differ between the groups..." (p. 333) |
| Selective reporting (reporting bias) | High risk | For nursing assistants results consist of covariance analyses that were not prespecified. |
| Other bias | Unclear risk | We did not any indications of other sources of bias. |
Gardner CBT 2005.
| Methods | RCT, UK | |
| Participants | 138 NHS employees who had contact with patients. 30% were nurses, 37% were care assistants, 20% were psychologists, speech therapists, physiotherapists or social workers, and 3% were doctors. The rest (10%) were administrative staff. | |
| Interventions | 1) Experimental 1: Cognitive therapy techniques training: participants attended 3 weekly 3½‐hour workshops. Participants in both intervention groups received didactic teaching in the concepts of stress and burnout and the physical and mental signs of stress. The cognitive groups also received teaching and practice in the cognitive model, identification of negative automatic thoughts, thought challenging, beliefs and attitudes, positive self talk, distraction and relaxation using imagery. These were packaged together as all involve the employment of cognitive strategies to influence thinking, emotions and well‐being. N = 57 2) Experimental 2: Behavioural coping skills training: 3 weekly 3½‐hour workshops of teaching and practice in time management, assertion, problem solving, goal planning, healthy lifestyles, Type A and Type B behaviours and progressive muscular relaxation. These were packaged together as all stress the importance of changing behaviour so as to improve one's work environment and relationships, as well as general health and well‐being. N = 44 3) Control: No intervention. N = 37 | |
| Outcomes | The Mental Health Professional Stress Scale, The General Health Questionnaire (GHQ‐12), Ways of Coping Scale, Support Questionnaire | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Random assignment of staff to various groups was not always feasible due to organizational constraints, staff availability and some participants requesting early intervention. Some staff were assigned to groups (and hence condition) according to their work location." (p. 141) |
| Allocation concealment (selection bias) | Unclear risk | "Randomization was achieved by putting 16 proposed courses into a hat (8 cognitive and 8 coping) and drawing them out one by one. The order in which they came out determined the order in which they were delivered."... "In the event 14 courses ran and it was fortunate that courses 15 and 16 would have been one of each condition, coping and cognitive. Date and venue thus determined the condition, and participants did not know which course they were allocated to until they arrived." (p. 141) |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "To assess for attrition bias, comparisons were made between those participants who dropped out of the study and those who were retained on factors thought to bias the results. Independent t tests and chi‐squared tests showed no significant differences between those who dropped out of the study and those who remained." (p. 145) |
| Selective reporting (reporting bias) | Unclear risk | "Table III. Means and standard deviations and significance levels using one‐way ANOVA for all variables where significant differences were found." (p. 146) |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Gardner Coping 2005.
| Methods | RCT, UK | |
| Participants | 138 NHS employees who had contact with patients. 30% were nurses, 37% were care assistants, 20% were psychologists, speech therapists, physiotherapists or social workers, and 3% were doctors. The rest (10%) were administrative staff. | |
| Interventions | 1) Experimental 1: Cognitive therapy techniques training: participants attended 3 weekly 3½‐hour workshops. Participants in both intervention groups received didactic teaching in the concepts of stress and burnout and the physical and mental signs of stress. The cognitive groups also received teaching and practice in the cognitive model, identification of negative automatic thoughts, thought challenging, beliefs and attitudes, positive self talk, distraction and relaxation using imagery. These were packaged together as all involve the employment of cognitive strategies to influence thinking, emotions and well‐being. N = 57 2) Experimental 2: Behavioural coping skills training: 3 weekly 3½‐hour workshops of teaching and practice in time management, assertion, problem solving, goal planning, healthy lifestyles, Type A and Type B behaviours and progressive muscular relaxation. These were packaged together as all stress the importance of changing behaviour so as to improve one's work environment and relationships, as well as general health and well‐being. N = 44 3) Control: No intervention. N = 37 | |
| Outcomes | The Mental Health Professional Stress Scale, The General Health Questionnaire (GHQ‐12), Ways of Coping Scale, Support Questionnaire | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Random assignment of staff to various groups was not always feasible due to organizational constraints, staff availability and some participants requesting early intervention. Some staff were assigned to groups (and hence condition) according to their work location." (p. 141) |
| Allocation concealment (selection bias) | Unclear risk | "Randomization was achieved by putting 16 proposed courses into a hat (8 cognitive and 8 coping) and drawing them out one by one. The order in which they came out determined the order in which they were delivered."... "In the event 14 courses ran and it was fortunate that courses 15 and 16 would have been one of each condition, coping and cognitive. Date and venue thus determined the condition, and participants did not know which course they were allocated to until they arrived." (p. 141) |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "To assess for attrition bias, comparisons were made between those participants who dropped out of the study and those who were retained on factors thought to bias the results. Independent t tests and chi‐squared tests showed no significant differences between those who dropped out of the study and those who remained." (p. 145) |
| Selective reporting (reporting bias) | Unclear risk | "Table III. Means and standard deviations and significance levels using one‐way ANOVA for all variables where significant differences were found." (p. 146) |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Ghazavi 2010.
| Methods | RCT, Iran | |
| Participants | 45 male and female nurses with B. Sc. of nursing, who exclusively worked in emergency or acute, chronic, or specialised male and female wards of psychiatry, and who scored less than 150 on the Holms and Rahe stress scale. 66.7% were married, 73.3% were on rotating shifts, and 55.4% were in the age range of 25 ‐ 30. | |
| Interventions | 1) Experimental: Communication skills training for 6 hours over 3 weeks 2) Control: No intervention |
|
| Outcomes | A stress questionnaire designed by the researcher. The questionnaire was based on Tuft‐Anderson’s questionnaire, psychiatric nurses occupational stress scale (PNOSS), and an opinion poll of some nurses working in psychiatry wards about the sources of their stress. " To determine the validity of the questionnaire designed by the researcher, it was revised and approved by five faculty members of psychiatric nursing, one PhD of nursing, three psychiatric nurses, two psychiatrists, and six psychologists." (p. 397) "The questionnaire consisted of 34 questions, on a four point scale, ranging from 0 to 3, in which 0 implied no stress, 1 mild stress, 2 moderate stress, and 3 high stress. Thus, the highest and the lowest possible scores of the questionnaire were 102 and zero, respectively. The questionnaire covered six fields; nine items on coping with threatening cases, four items on shortage of resources, nine items on personnel conflicts, five items on planning issues, four items on working load, and three items on un‐preparedness for the occupational stress of psychiatric wards. Obtaining scores equal to or less than 30 was interpreted as low stress, while stress score of 40‐62, and 63 and above indicated moderate and high stress, respectively." (p. 397) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "the participants were randomly assigned to two groups; experiment and control. According to the random number table, of the 23 participants in the experiment group, four (17.4%) and 19 (82.6%) were from Noor and Farabi hospitals, respectively, while of the 22 participants in the control group, 10 (45.5%) and 12 (54.5%) were from Noor and Farabi hospitals, respectively." (p. 397) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The authors do not report about participants dropping out. |
| Selective reporting (reporting bias) | Unclear risk | The authors report the results of their stress questionnaire only as group means and t‐test P values. |
| Other bias | High risk | The only outcome measure the authors used was of their own devising and it was validated only by revision and approval by colleagues. |
Griffith 2008.
| Methods | RCT, USA | |
| Participants | 50 employees of the Denver Veterans Affairs Medical Center | |
| Interventions | 1) Experimental: Qigong exercise: participants assigned to the exercise group attended a 1‐hour, noon qigong class twice weekly and were asked to practice independently for 30 minutes on non‐class days with the aid of a DVD demonstrating the instructor performing the exercises. Classes were taught by a senior apprentice in qigong with over 17 years’ experience in qigong. In addition, participants were provided a manual that outlined the acupuncture meridians and the rationale for the exercises. During class sessions, participants practised movements until they experienced a sensation of stretching or pressure in the targeted acupuncture points. The qigong movements were synchronised with specific breathing patterns, and participants were instructed to inhale and exhale fully at a comfortable rate, with a target respiratory rate of 6 breaths or fewer per minute. 2) Control: No intervention | |
| Outcomes | Perceived Stress Scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Fifty (50) subjects, 39 females and 11 males, were matched for gender and then randomized (25 in each treatment group) through the use of computer‐generated numbers (SYSTAT12.0 for Windows, Cranes Software, 2007, Bangalore, India)." (p. 940) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self‐report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "There were no significant differences in numbers of withdrawals between study groups" (p.940) This statement seems counterfactual as the intervention group lost 36% and the control group lost 16% of their participants before follow‐up. In the intervention group 5 (25%) stopped attending and in the control group one participant started mindfulness training. ITT analysis was not used. |
| Selective reporting (reporting bias) | High risk | Authors only report change values. |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Gärtner 2013.
| Methods | Cluster‐RCT, Netherlands | |
| Participants | Nurses on wards of an academic hospital were screened for work and health problems: Experimental: 29 wards, 591 participants of which 151 screened positive Control: 28 wards, 561 participants of which 161 screened positive. Experimental: 17% Control 22% men, > 45 years age Experimental 51% Control 46%, > 10 years of experience Experimental 51% Control 41% | |
| Interventions | 1) Experimental: All who screened positive were referred to Occupational Health Physician (OHP). Participants who were screened as positive were invited for a face‐to‐face preventive consultation with their occupational physician. The consultation was voluntary, and workers could reschedule or cancel it if they wished. Supervisors were not informed about the screening results or about the invitation for and content of the preventive consultation of any employee. The 7‐step protocol for OHPs closely followed occupational physicians’ care as usual for consultations initiated by the employee in contrast to the compulsory consultation in the context of absenteeism. Occupational physicians received 3 hours of training from the researchers on the use of the protocol. (CBT) 2) Control: Waiting list: In the control arm. Participants filled out the baseline questionnaire; however, results of the screening‐questionnaires were not to be reported back to participants, and no further interventions were advised at baseline. As compensation, participants in the control arm received their personal screening results together with a tailored choice for a self‐help EMH intervention six months after baseline. |
|
| Outcomes | The study's primary outcome was help‐seeking behaviour; we used secondary outcomes: distress from the Dutch 4DKL, anxiety and depression from Brief Symptom Inventory | |
| Notes | We got the following data for the distress scale of the 4DKL at 6 months follow‐up for the group who screened positive from author K Nieuwenhuijsen: Experimental: N = 86 6.24 ± 6.52 Control: N = 116 6.82 ± 6.57 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | " Randomization was performed at the ward level (n = 86). Randomization sequences with a block size of three were generated with Nquery Advisor (Statistical Solutions, Ltd, Cork, Ireland) by one researcher (K.N.) who was not involved in the recruitment" |
| Allocation concealment (selection bias) | Unclear risk | Not blinded |
| Blinding (performance bias and detection bias) All outcomes | High risk | Providers not blinded, outcome self‐reported measures of stress |
| Incomplete outcome data (attrition bias) All outcomes | High risk | At 3 months lost to follow‐up: Experimental 37% / Control 30%; at 6 months Experimental 46% / Contr 34% |
| Selective reporting (reporting bias) | Low risk | All outcomes reported that were announced in protocol |
| Other bias | High risk | Compliance very low: 34% of those invited visited their OHP |
Günüsen 2010.
| Methods | RCT, Turkey | |
| Participants | " All of the nurses (n = 227) were invited to complete the Maslach Burnout Inventory (MBI) developed by Maslach & Jackson (1981). Those who completed the questionnaire and received a score on emotional exhaustion higher than the median score for all nurses were invited to participate in the burnout reduction intervention." (p. 487) 108 nurses were randomised to one of three conditions. |
|
| Interventions | 1) Coping training (N = 36) "The group that received coping training consisted of two groups, each group consisting of 18 people. In the first week, the concept of stress was explained to the nurses, and coping methods used by the nurses in stressful conditions were discussed. In the second session, basic communication skills on the stress level were discussed. In the third session, cognitive coping methods were presented theoretically. In the fourth session, cognitive distortions found among nurses and methods for coping with these distortions were discussed. In the fifth session, the problem‐solving method was theoretically explained to the nurses. In the sixth session, stressful situations that the nurses encounter were discussed and resolved by means of the problem solving method. In the seventh session, problems that the nurses had difficulty coping with were discussed by utilizing the skills learned during the course of the programme." (p. 488) 2) Support group (N = 36) "...the support group consisted of three groups, each group consisting of 12 people. The nurses talked about the most frequently encountered stressors in the workplace and expressed their feelings towards their jobs. At the beginning of each session, the nurses expressed their feelings related to difficult situations at the workplace. Then, a problem chosen by the nurses was attempted to be solved by using reflective cycle steps. Researchers provided information when needed. Possible solution methods were discussed in the groups, and the nurses were advised to use these methods in their daily lives. The nurses shared their difficult and favourable times and also exchanged recommendations with each other." (p. 488) 3) Control: No intervention (N = 36) |
|
| Outcomes | MBI | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Random allocation was concealed by using a system of sequentially numbered, opaque, sealed envelopes containing the computer‐generated random allocation, which had been drawn up by a statistician. During the randomization, the researchers and the participants did not know the groups to which they would be allocated." (p. 487) |
| Allocation concealment (selection bias) | Low risk | See above |
| Blinding (performance bias and detection bias) All outcomes | High risk | "No blinding was applied to the participants and the researchers." (p. 487) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Intention‐to‐treat analysis was used because of sample loss." (p. 487) |
| Selective reporting (reporting bias) | Low risk | The authors only measured and adequately reported results of the MBI. |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Hansen 2006.
| Methods | RCT, Norway | |
| Participants | 32 nurses working at 2 psychiatric hospitals | |
| Interventions | 1) Experimental: Full‐body massage: 6 consecutive weekly 90‐minute full‐body aromatherapy massages. 2) Control: No intervention | |
| Outcomes | Cooper's Job Stress Questionnaire | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Thirty‐five subjects registered for the study and were randomised by drawing numbers, to either a treatment group (n = 18) or a control group." (p. 91) |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not reported, self‐report blinding not possible |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "Three persons dropped out from the control group, two moved to other parts of Norway and one went on vacation" (p. 91) |
| Selective reporting (reporting bias) | Low risk | There was only one outcome measure and its results were reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Heaney 1995.
| Methods | RCT, USA | |
| Participants | 1375 direct care staff and home managers | |
| Interventions | 1) Experimental: Caregiver support programme (CSP): 6 4 ‐ 5‐hour group training sessions for the house manager and 1 direct care staff person from each intervention group home (train the trainer approach) of participatory problem‐solving skills, influencing decision making and how to mobilise support from others at work. 2) Control: No intervention | |
| Outcomes | Social support, Organisational climate, SCL‐90‐R, Confidence in coping ability | |
| Notes | The study results are reported only as regression coefficients and thereby could not be entered into meta‐analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Half of the group homes within each participating agency were then randomly assigned to receive the CSP (the experimental group), and the other half did not (the control group). If an agency had an odd number of homes, the extra home was assigned to the experimental group." (p. 338) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Employees who were randomized into the experimental group but who had no exposure to the CSP were included in the analyses as members of the experimental group." (p. 342) |
| Selective reporting (reporting bias) | Unclear risk | Results reported only as regression coefficients |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Jensen 2006.
| Methods | cluster‐RCT, Denmark | |
| Participants | 210 eldercare workers | |
| Interventions | 1) Experimental 1: Stress Management Intervention: The SMI was developed to address the work stress in health care with particular attention to prevention of burnout and development of strategies for stress management. Training occurred over 20 weeks, with group sessions every 2 weeks, and each session lasting 2 hours. Between sessions, the participants were given assignments concerning implementation of the programme in daily practice. 2) Experimemtal 2:Transfer Technique Intervention: The TTI was based on the Stockholm training concept, which aims to reduce the biomechanical load on the back, minimise work in asymmetric postures, and prevent sudden unexpected loads. Training in the TTI arm was a combination of practical classroom education (24 hours for each worker) and instruction at the work site. There were 11 instructors who belonged to the 7 groups in the TTI arm, with 1 – 2 persons in each group who received 30 hours of education during the initial phase of the study. 3) Control: Reference Programme consisting of lessons of the participants' own choice in matters unrelated to the intervention programmes but of the same duration as the active intervention lessons (e.g. on skin care, proper treatment of a person with diabetes, etc.) | |
| Outcomes | MBI (results not reported in article but obtained directly from author) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomization was performed at group level because the intervention programs were meant to involve the employee as a group during education and implementation. The assignment to the different intervention programs was balanced to secure representation of all 3 programs in each of the wards." (p.1762) |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "We observed no differences in age and number of years occupied in health care and mean intensity of LBP during the past year between participants who remained in the study and participants who dropped out." (p.1762) |
| Selective reporting (reporting bias) | High risk | Results data for the MBI, Setterlind's Stress Scores and rating of social support were not reported because they were not statistically significantly different between groups. "...[N]o significant changes were found in either of the intervention arms in ... the Maslach Burnout Inventory, the Setterlind stress scores, or the rating of social support (data not shown)" (p. 1765) |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Jones 2000a.
| Methods | RCT, UK | |
| Participants | 79 student nurses reporting significant levels of affective distress at screen | |
| Interventions | 1) Experimental: Multi‐modal stress management: 6 2‐hour sessions about coping skills: self monitoring of distress symptoms, use of problem‐solving strategies to change situations, situational reappraisal, time‐ and self‐management skills, relaxation skills and applying all this in real‐life settings. The presentation of an element of a 6‐session relaxation intervention completed each session. The aim of the relaxation programme was to enable the student to relax in a non‐threatening situation in 30 seconds and for the student to generalise this "applied relaxation" coping skill in real‐life situations. Relaxation techniques taught were: progressive muscle relaxation, release‐only relaxation, rapid relaxation, autogenic relaxation and meditation. In addition, strategies described as having an interface/organisational focus were included. using participant experience as a focus, problem solving in a group setting centred on the reduction of work‐family stress, the facilitation of an increase in perceived influence and maximisation of awareness and uptake of available organisational supports. 2) Control: No intervention | |
| Outcomes | Derogatis Stress profile, Beck & Srivastava Stress Inventory, GHQ, STAI, BDI, ways of coping, absenteeism | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Students were randomly allocated to experimental and control groups. Odd and even integers read from random number tables were used to assign experimental and control group membership respectively." (p. 692) |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "This [Attrition from the stress management intervention] was low and comparable between groups with only 6 and 7% of control and experimental participants leaving the study by 3 month follow‐up. Data from students who attended 4 sessions and provided three complete sets of data at times 1‐3, we included in the analytic procedures employed." (p. 693) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Ketelaar 2013.
| Methods | Cluster‐RCT, Netherlands | |
| Participants | Nurses on wards of an academic hospital were screened for work and health problems: Experimental: 29 wards, 579 participants of which 139 screened positive Control: 29 wards, 561 participants of which 161 screened positive. Experimental 17% Control 22% men, > 45 years age Experimental 51% Control 46%, > 10 years of experience Experimental 51% Control 41% | |
| Interventions | 1) Experimental: Participants received personalised feedback on their screening results immediately after filling out the baseline questionnaire, both onscreen and in an e‐mail. The personalised feedback was followed by an invitation for a tailored offer of self‐help EMH interventions, on the basis of an algorithm based on the specific symptoms and the work‐relatedness of the symptoms. Participants were mostly offered a choice of 2 ‐ 3 EMH interventions to leave room for personal preferences. Participants who screened negative on all mental health complaints were invited to follow an EMH intervention aimed at enhancing and retaining their mental fitness. The EMH interventions are self‐help interventions on the Internet aimed at reducing specific mental health complaints or enhancing well‐being. The interventions are mainly based on the principles of cognitive behavioural therapy and combine a variety of aspects, e.g. providing information and advice, weekly assignments, the option of keeping a diary and a forum to get in contact with others who have similar complaints. The EMH interventions were developed as stand‐alone interventions by the Trimbos Institute (CBT) 2) Control: Waiting list: In the control arm. Participants filled out the baseline questionnaire; however, results of the screening questionnaires were not to be reported back to participants, and no further interventions were advised at baseline. As compensation, participants in the control arm received their personal screening results together with a tailored choice for a self‐help e‐mental health intervention six months after baseline. |
|
| Outcomes | The study used work‐functioning as the primary outcome: we used the distress part of the Dutch 4DKL as stress outcome; anxiety and depression were also measured but not reported | |
| Notes | We got the following data from author S. Ketelaar: Distress measure with 4DKL at 6 months follow‐up for the group who screened positive: Experimental: N = 52 6.06 ± 6.54; Control: N = 116 6.82 ± 6.5.7 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | In order to guarantee allocation concealment, randomisation was performed by 1 researcher (KN) who was not involved in the practical recruitment of employees, using the computer software program Nquery Advisor with a block size of 3. |
| Allocation concealment (selection bias) | Unclear risk | see above |
| Blinding (performance bias and detection bias) All outcomes | High risk | Providers and participants not blinded; outcome self‐reported stress |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Experimental: 80/178 = 44% lost to follow‐up; Control: 71/211 = 34% lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Anxiety and Depression not reported |
| Other bias | High risk | Compliance with the intervention was extremely low |
Klatt 2012.
| Methods | RCT of individuals, USA | |
| Participants | Personnell of a surgical intensive care unit of a large university hospital (n = 32); 69% nurses, 88% women, age average 44 yrs, experience 12 ± 10 yrs | |
| Interventions | 1) Experimental: A pragmatic low‐dose mindfullness‐based worksite intervention, on‐site 1 hour before shift change during 8 weeks 2) Control: waiting list control |
|
| Outcomes | Depression Anxiety Stress Scale (DASS‐21) and salivary alpha‐amylase; work satisfaction | |
| Notes | Based on abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "..were randomized to intervention or wait‐list control groups, stratified by gender.." |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | Not reported |
| Other bias | Unclear risk | Based on abstract only |
Kurebayashi 2012.
| Methods | RCT, Brazil | |
| Participants | 75 nurses at the Teaching Hospital of the University of São Paulo. "In order to define the sample of participants, the authors used the Stress Inventory or Stress Symptoms List – SSL. This instrument was applied to all subjects who agreed to participate in the study (N=109); however, only subjects who achieved mean (29 to 60 points), high (61 to 120 points) or very high (>120 points) scores were included in the sample; 75 of them completed the study. As for the distribution of the participants, 22 subjects were placed in the Control Group, 27 in the Needles Group and 26 in the Seeds Group." (p. 88) "The inclusion criteria were: belonging to the nursing team; voluntary participation in the study with avaiability to attend the sessions; obtaining a minimum SSL score at mean, high and very high stress level; not being pregnant. The authors excluded from the sample all the subjects who went on vacation or medical leave after the beginning of the study; did not show up to the session or gave up due to adverse effects, and those who had low SSL score." (p. 88) |
|
| Interventions | 1) Experimental 1: Auriculotherapy (form of acupuncture performed on the ears) with needles (n = 27) 2) Experimental 2: Auriculotherapy with seeds (n = 26) 3) Control: No intervention(n = 22) "The intervention groups received eight sessions (one session a week), with duration of 5 to 10 minutes each session, on the Shenmen, Kidney and Brainstem points. The first two points have calmative properties and the kidney point has energetic function. After the location of the reactive points with a point locator, the ear auricle was hygienized with cotton and ethyl alcohol 70% and, then, semi‐permanent needles were applied or seeds were fixed with adhesive plaster, according to the intervention group. In the group of auriculo therapy with seeds, mustard seeds were used and the participants were instructed to stimulate them three times a day, for 15 times, with moderate pressure. The volunteers were instructed to remove the needles or seeds 24 hours before the session and, in case there was any discomfort, itching or signs of allergy, they should remove them before that." (p. 88) |
|
| Outcomes | Stress Symptoms List | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "This randomized controlled clinical experiment was performed with three groups..." (p. 88) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding was not possible |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "...there was a loss of 34 subjects during the study. Seven professionals went on vacation after the beginning of the study and two on medical leave; 12 missed the session because they had forgotten it, due to traffic problems or the difficulty to reschedule it and seven did not show up for the first session. One participant gave up due to adverse effects, in this case, nightmares, and five exclusions were due to low score (1), not belonging to the nursing team (3), and not filling out properly the questionnaires (1)." (p. 89) The authors do not report how the dropouts were distributed among the study groups. |
| Selective reporting (reporting bias) | High risk | The authors present data separately for participants who had had high SSL scores to begin with in table 2 but not at all for participants with a moderate SSL score. |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Kwok 2012.
| Methods | RCT, Hong Kong | |
| Participants | 38 nurses. "All ED nurses who met the following inclusion criteria were invited to participate in the MEDI program: (a) currently employed ED nurse and (b) Cantonese‐English speaking" (p. 20) "Exclusionary criteria were as follows: (a) substantial drug or alcohol abuse problems, (b) current suicidal ideation, (c) the presence of psychotic symptoms, or (d) currently taking psychiatric medication." (p. 20) | |
| Interventions | 1) Experimental: MEDI intervention (n = 18) "The MEDI program is a combination of four crucial components: to pay attention to each moment with non‐judgemental manner (Mindfulness), to regulate intense emotions (Emotion regulation), to tolerate emotional distress when change is sluggish or implausible (Distress toleration) and to be more efficient in resolving interpersonal conflicts (Interpersonal effectiveness)." (p. 13) "...the MEDI program, which included four sessions, 1.5h each concerning mindfulness, emotion regulation, distress tolerance, and interpersonal effectiveness." (p. 24) 2) Control: No intervention (n = 20) |
|
| Outcomes | MPSS‐R consisting of 4 subscales; OS = Occupational Stress, JD = Job Dissatisfaction, NPA = Negative patient attitude and SS = Somatic Stress. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...two groups were formed: (a) MEDI treatment (n=18) and (b) no treatment control (n=20) based on each participant blindly drawing a number from an envelope (1 = MEDI group and 2 = control condition)." (p. 32) |
| Allocation concealment (selection bias) | Unclear risk | Authors do not report if allocation was concealed |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding of participants (also outcome assessors of self‐report measures) and intervention providers was not possible. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Participants were "[e]xcluded from analysis due to drop out". (p. 32) |
| Selective reporting (reporting bias) | Low risk | All measured outcomes were reported. |
| Other bias | High risk | The dropout rate was 50% of the original sample (12/18 in intervention group and 7/20 in control group). |
Lai 2011.
| Methods | Cross‐over study, Taiwan | |
| Participants | 54 newly‐employed nurses who had been in their job for less than one year. "The 54 participants were all female with a mean age of 23.4 (SD = 2.46). Only one participant was married. The majority were registered nurses (n = 49, 90.7%), with no past clinical experience (n = 42, 77.8%) and most had graduated from junior college (n = 40, 74.1%)." (p. 2419) "To qualify for participation in the study, participants were required to: (1) have normal hearing without the use of any hearing aid; 2) have been employed full‐time as a nurse for <1 year; (3) be between 20 and 40 years of age; (4) have a self‐rated VAS 0‐10 stress score of ≥6 and (5) weigh between 45 and 70 kg." (p. 2416) "Exclusion criteria included: (1) current or past abnormalities in endocrinology or metabolism (Lavie et al. 2009); (2) pregnancy; (3) chronic organic disease; (4) medicine, alcohol or tobacco use; (5) those who have experienced a major stressful event in the past 6 months (The Social Readjustment Rating Scale) (Holmes & Rahe 1967); and (6) those receiving physical training (Schulz et al. 2004)." (p. 2416) |
|
| Interventions | "Interventions consisted of an alternating music and chair rest or chair rest and music sequence" (p. 2416) The procedure took one hour and 20 minutes to complete. It started with 30 minutes listening to music whilst seated, followed by a 20‐minute washout during which participants "...were asked to get up and move around while the researcher made conversation with the participant based on a standardized chatting guideline about the daily leisure activities and interests participants had outlined beforehand" and finally participants rested whilst seated for another 30 minutes. Half the participants were randomised to receive the interventions the other way round. | |
| Outcomes | Self‐perceived stress on a 10 cm VAS, Heart rate, mean arterial pressure and finger temperature. | |
| Notes | Authors could not be traced for inquiries | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "A randomized controlled crossover clinical trial was used to examine the effectiveness of music on stress reduction." (p. 2416) |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not reported but not possible. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Apparently there were no dropouts so all data are accounted for. |
| Selective reporting (reporting bias) | Low risk | All the measured outcomes were reported. |
| Other bias | High risk | The cross‐over design may be a source of bias. It is impossible to say if a 20‐minute washout is enough. |
Le Blanc 2007.
| Methods | Cluster‐RCT, Netherlands | |
| Participants | 664 staff members of 29 oncology wards of 18 general hospitals. Participants were physicians, nurses and radiotherapy assistants. | |
| Interventions | 1) Experimental: Take Care! stress management training: 6 monthly 3‐hour sessions about 1) working mechanisms of job stress and feedback on work situation survey 2) emergence and preservation of unwanted collective behaviour 3) communication 4) building a social support network 5) balancing job‐related investments and outcomes. Participants formed teams that collectively designed, implemented, evaluated and reformulated plans of action to cope with most important stressors in their work situation. 2) Control: No intervention | |
| Outcomes | MBI, Social support scale, Participation in decision making scale, Job control scale, Quantitative job demands scale and Emotional job demands scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Nine experimental wards were randomly selected from the total number of 29 wards participating in this study; the remaining 20 wards served as controls" (p. 215) |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "An analysis of the dropout pattern ... revealed that panel attrition was the dominant pattern, with a group of 54 respondents who were missing at T2 but returned at T3. Given this pattern, we created a variable indicating whether a person was missing at T2 but not at T1 and T3. Next, we performed a multivariate analysis of variance to check whether this specific group differed from the remaining participants... No significant differences emerged... which suggests that panel attrition was not selective." (p. 217) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Lee 1994.
| Methods | RCT, Taiwan | |
| Participants | 60 hospital nurses suffering from either: insomnia, headache or gastrointestinal discomfort | |
| Interventions | 1) Experimental: Assertiveness training: 6 2‐hour sessions on Monday, Wednesday and Friday at 2pm ‐ 4pm on t2consecutive weeks. The contents of sessions included the concept of beliefs and negative self‐statements, building a positive belief system, applying assertion to clinical settings and developing group and self‐reinforcement support systems. 2) Control: Traditional in‐service programme about computer applications in nursing | |
| Outcomes | Perceived Stress Scale, Rathus Assertiveness Schedule | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Subjects were randomly assigned to one of two treatments: assertiveness training (AT) or alternate treatment control (ATC), which served as a control and contained updated knowledge of new computer technology for in patient settings." (p. 419) |
| Allocation concealment (selection bias) | Low risk | "Subjects admitted to the study agreed to random treatment assignment and a 2‐month commitment to the study. However, the subjects did not know whether they would receive treatment or control procedures during that time." (p. 425) |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "Of the respondents who initially chose to participate, three did not complete the study and were not included in the data analysis due to their failure to attend all sessions, failure to complete the questionnaire, or decision to leave hospital employment." (p. 425) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Leiter 2011.
| Methods | Controlled Clinical Trial, Canada | |
| Participants | "At Time 1, 1,173 health care workers in three district health authorities in Nova Scotia and two hospitals in Ontario completed a survey (n 262 in the intervention units and n 911 in the contrast units). Participants were predominantly female (n 1,009, 86.0%; male: n 139, 11.8%; 25 not responding), with an average age of 42.54 years (SD 10.12). Their employment status varied, including full‐time (n 833, 71.0%), part‐time (n 232, 19.8%), casual (n 85, 7.2%), and temporary (n 8, 0.7%) employment, with 15 not responding. The occupational categories with the highest response rates included registered nurses (RNs; n 607, 51.7%), registered psychiatric nurses (RPNs; n 74, 6.3%), ward clerks (n 52, 4.4%), physicians (n 46, 3.9%) and licensed practical nurses (LPNs; n 42, 3.6%). They worked in their current hospital for varying lengths: fewer than 6 months (25, 2.1%), 6–24 months (68, 5.8%), 2–5 years (247, 21.1%), 6–10 years (207, 17.6%), 11–15 years (124, 10.6%), 16–20 years (151, 12.9%), 21–30 years (190, 16.2%), and more than 30 years (50, 4.3%), with 111 not responding. At Time 2, 907 health care workers completed the survey (n 181 in intervention units; n 726 in contrast units), for a response rate of 28.6%. Four hundred seventy‐two participants completed surveys both at Time 1 and Time 2. At Time 2, participants were predominantly female (n 793, 87.4%; male: n 96, 10.6%, 18 not responding), with an average age of 42.27 years (SD 10.60). Their employment status varied, including full‐time (n 645, 71.0%), part‐time (n 177, 19.6%), casual (n 56, 6.1%), and temporary (n 13; 1.4%) employment, with 16 not responding. The occupational categories with the highest response rates included RNs (n 464, 51.3%), physicians (n 43, 4.8%), ward clerks (n 43, 4.8%), RPNs (n 41, 4.5%), and LPNs (n 33, 3.7%). They worked in their current hospital for varying lengths: fewer than 6 months (16, 1.8%), 6–24 months (78, 8.6%), 2–5 years (137, 15.2%), 6–10 years (133, 14.7%), 11–15 years (70, 7.7%), 16–20 years (101, 11.2%), 21–30 years (160, 17.7%), and more than 30 years (44, 4.9%), with 168 not responding. Employees who described their position as temporary (Time 1, n 8; Time 2, n 13) were dropped from the analysis." (p. 1262) | |
| Interventions | 1) Experimental: CREW intervention The CREW (Civility, Respect and Engagement at Work) intervention consisted of an introductory period, six months of weekly meetings led by a facilitator "CREW is a process designed to enhance civility among colleagues within the USA VHA. Employees met with coworkers on their units on a weekly or biweekly basis to work on effective interpersonal interactions at work. Trained facilitators assist these groups by providing guidance on the basis of their expertise in group facilitation and knowledge of effective work group communication." 2) Control: No intervention |
|
| Outcomes | The Emotional Exhaustion and Cynicism subscales of the MBI‐General Survey | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not randomised |
| Allocation concealment (selection bias) | High risk | Not concealed |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not blinded, not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The authors are not at all concerned with the fact that only 40% of participants that responded at time 1 (pre‐intervention) did so again at time 2 (post‐intervention) |
| Selective reporting (reporting bias) | Low risk | The authors report results for all outcomes listed in the Methods section. |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Lemaire 2011.
| Methods | RCT, Canada | |
| Participants | 40 staff physicians practising in an urban tertiary care centre "We excluded potential participants who screened positive for major depression with the 9‐item Patient Health Questionnaire (PHQ‐9) depression scale and referred them to the provincial physician wellness support program." (p. 155) |
|
| Interventions | 1) Experimental: Biofeedback‐based stress management (n = 21). "Participants allocated to the intervention group received a brochure describing the provincial physician wellness support program; were given a biofeedback device and participated in an individual training session to learn the quick coherence technique and how to use the device, with an offer of optional follow‐up instruction; and were given a prescription to use the stress management tool during study days 0 to 28 for 5 minutes at least three times daily. A research assistant contacted each participant in the intervention group twice weekly to measure stress and well‐being, heart rate and blood pressure; to document their adherence to using the stress management tool; and to record a 3‐minute biofeedback session using the emWavePC software." (p. 156) "Participants allocated to the control group received the same brochure describing the provincial physician wellness support program and were contacted twice weekly by a research assistant to measure stress and well‐being, heart rate and blood pressure." (p. 156) "The biofeedback‐based stress management tool used in our study consisted of a combination of rhythmic breathing, self‐generated positive emotion and a biofeedback device to reinforce positive physiological change when dealing with stress." (p. 155) 2) Control: (n = 19) Brochure only |
|
| Outcomes | Perceived stress measured on "...a multiple‐item scale developed by the research team and intended to measure global perceptions of stress and also to capture occupation‐specific stress that is particularly relevant to physicians" The survey included 15 items from the Perceived Stress Scale and 25 selected items from the Personal and Organizational Quality Assessment–Revised (POQA‐R) questionnaire. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "We used a computer program to generate a random allocation sequence for assigning participants to either the control or the intervention group, with stratification by sex to ensure parity within groups." (p. 155) |
| Allocation concealment (selection bias) | Low risk | "Participants’ allocation to the control or intervention group was concealed until after the research assistant and/or the co‐investigators had confirmed eligibility criteria and received informed consent." (p. 155) |
| Blinding (performance bias and detection bias) All outcomes | High risk | "Given the nature of the intervention and the outcome measures, the study was not blinded." (p. 155) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "We limited calculation of mean change in stress score to participants for whom data were complete, as this value was calculated by subtracting, for each participant, the score on day 0 from the score on day 28, and then reporting the mean of these differences." (p. 157) |
| Selective reporting (reporting bias) | Low risk | All outcomes listed in Methods were reported. |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Li 2011.
| Methods | Controlled Clinical Trial, Taiwan | |
| Participants | 49 junior nursing students engaged in a medical‐surgical rotation from a university. "The experimental groups consisted of mentor and mentee students; each mentor was paired with one mentee. The mentors were recruited students who had received medical–surgical experience before entering university. They also have a junior college nursing certification and a Registered Nursing license (n = 17). The mentees (n = 17) have had no prior medical–surgical clinical practice experience. The control groups consisted only of students who had no medical or surgical clinical practice experience (n = 32). The control group and experimental group were assigned in two different clinical settings at different time in order to minimize within‐group influence and its interference with the research." (p. 205) | |
| Interventions | 1) Experimental: Peer mentoring intervention, 3 days per week for 4 weeks (n = 17). "The mentors were selected from the mentee’s class. The mentors were all informed in advance about the aim and process of this study. They were volunteers and were requested to be motivated, self‐confident, enthusiastic and open, especially when dealing with mentees. They were supposed to be the role models for their mentee when taking care of patients or interacting with the clinical teacher and medical staff. The mentor also played a psychosocial role, for example, listening to the mentees’ complaints,sharing their pre clinical practice experience and generally giving all‐round support." (p. 205) "Mentors were coached and supervised by the clinical teacher to make sure of the accuracy and reliability of their knowledge when they first practiced their nursing skills on an actual patient. After that, mentors could assist mentees in some basic and non‐intervened nursing skills, such as naso‐gastric tube care and mouth care, which had been taught in school lectures. Mentors and mentees could also learn to understand each other’s patients through communicating with the patients and discussing with the medical staff. They were able to converse with each other at least once a week during the rotation. In addition, after work, they gave support through correspondence, over the telephone or e‐mail." (p. 205) 2) Control: (n = 32) No intervention |
|
| Outcomes | The Perceived Stress Scale (PSS) Total score | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "The control group and experimental group were assigned in two different clinical settings at different time in order to minimize within‐group influence and its interference with the research." (p. 205) |
| Allocation concealment (selection bias) | High risk | Allocation was not concealed. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Apparently none of the participants dropped out. |
| Selective reporting (reporting bias) | Unclear risk | The study recruited 34 students in the experimental group (17 mentors and 17 mentees) but the authors report outcome data only for 17 of these, presumably the mentees. |
| Other bias | High risk | The authors state that "… gender will be a confounding variable in this study" (206) |
Lucas 2012.
| Methods | Cluster‐randomised cross‐over non‐inferiority trial, USA | |
| Participants | 62 hospital physicians | |
| Interventions | 1) Experimental: 2‐week hypothesised to be least stressful 2) Control: 4‐week rotations to improve education and supervisor relation | |
| Outcomes | Burnout was measured with a questionnaire that contained: "...8 items from Minimizing Error, Maximizing Outcomes...and 4 items from the short version of the Perceived Stress Scale. Emotional exhaustion... was measured using 9 items from the Maslach Burnout Inventory Human Services Survey and a single‐item measure from the National Job Burnout Survey that uses a personal definition of burnout." (p. 2201) We used the MBI emotional exhaustion scale. The study´s primary outcome was patient re‐hospitalisation. |
|
| Notes | The authors kindly provided the continuous outcomes for the MBI scale. We used the data at physician level not at work schedule level. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "After dividing each attending physician’s year‐long service commitment into 4‐week segments, we used a computerized random‐number generator to block randomize these 4‐week segments (as single 4‐week or paired 2‐week rotations) using block sizes of 2, the number of rotation types." (eAppendix) |
| Allocation concealment (selection bias) | High risk | Not concealed |
| Blinding (performance bias and detection bias) All outcomes | High risk | "Attending physicians were not blinded to their rotation assignments because the year long rotation schedule was distributed 3 months before the study commenced. Attending physicians, trainees, and patients were, nonetheless, blinded to the study hypothesis." (p. 2200‐2201) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were very little missing data. "A severity assessment from a 2‐week rotation was missing from one attending physician who had completed 5 other assessments after 2‐week rotations." |
| Selective reporting (reporting bias) | Low risk | All outcomes listed in the Methods section were reported. |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Lökk 2000.
| Methods | Cluster‐RCT, Sweden | |
| Participants | 26 health care personnel in a geriatric hospital | |
| Interventions | 1) Experimental: Support and advice from a psychologist: 1 hour every second week for 20 weeks regarding knowledge about stressors, relaxation techniques, life style factors and physiological, cognitive, emotional and behavioural stress reactions. Participants were encouraged to alter reaction patterns and to discuss and test new alternative patterns and enhance own work conditions and increase self control over work processes. 2) Control: Passive attendance of psychologist in staff meetings | |
| Outcomes | A structured made‐to‐measure stress questionnaire | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The wards were randomly allocated to be either intervention (I) or control (C) ward" (p. 80) |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "There were no dropouts during the study period" (p. 81) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Mackenzie 2006.
| Methods | RCT, Canada | |
| Participants | 30 nurses and nurse aides working in a large urban geriatric teaching hospital | |
| Interventions | 1) Experimental: Mindfulness‐based stress reduction programme: 4 30‐minute group sessions including didactic section and experiential exercises. Participants also received a CD or audiocassette of guided exercises and a manual with the help of which they were instructed to practise for at least 10 minutes per day 5 days per week. 2) Control: No intervention | |
| Outcomes | MBI, Smith Relaxation Dispositions Inventory | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Nurses and nurse aides were recruited from long‐term and complex continuing care units in a large urban geriatric teaching hospital and randomly assigned to intervention or wait‐list control groups. Because the study was conducted during the summer, however, several exceptions were made to accommodate participants' vacation schedules and additional control participants were recruited." (p. 106) |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It is unclear if any participants dropped out |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Martins 2011.
| Methods | RCT, Argentina | |
| Participants | 74 hospital paediatric resident physicians. " A total of 81% were female; the mean age was 27.3±1.4 years; 57% were working in inpatient areas, 35% in the outpatient clinic, and 8% in the intensive care unit." " A comparison of the characteristics of both groups (experimental and control) revealed no significant differences." (p. 494) | |
| Interventions | 1) Experimental: Self‐care workshop intervention (n = 37). "The experimental group received a brief intervention consisting of two 2.5‐hour workshops directed by mental health professionals, which covered repercussions of
burnout syndrome on professional activity, recognition of risk indicators for burnout syndrome, and tools to cope (identification of strengths, coping behaviors, preventive and self‐care behaviors)." (p. 494) 2) Control: (n = 37) No intervention |
|
| Outcomes | MBI | |
| Notes | It is unclear why 43 (37%) out of the available 117 resident physicians did not participate in the study. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "After administration of the questionnaire, subjects were randomly assigned to one of the two study groups." (p. 494) |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants could not be blinded regarding group allocation. Also as outcome measurement was by self report, there was no blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Apparently no participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | The authors do not report standard deviations with the mean MBI subscale scores. |
| Other bias | Unclear risk | It is unclear if these 74 were all the participants or only those that could be followed up. |
McElligott 2003.
| Methods | RCT, USA | |
| Participants | 20 nurses working at a tertiary care centre | |
| Interventions | 1) Experimental: AMMA therapy: 4 weekly 45‐minute treatments consisting of circular digital pressure along particular Chinese energy channels on the head, chest, arms, hands, feet, abdomen, legs and back. "It is performed while the practitioner is using intent to remove blockages from the energy channels, as well as pressure on designated "points" or areas of the body." (p. 20) 2) Control: a standardised touch therapy protocol that was: "...designed to sequentially mimic AMMA treatment. It did not include pressure, intent, or digital motion used in AMMA Therapy. "Intent" is defined as the conscious awareness of being in the present moment to help facilitate the healing process. In an attempt to control for intent, the nurses were instructed to hold their hands on certain areas of participants' bodies and to count to 60." (p. 20) | |
| Outcomes | VAS of anxiety, blood pressure, heart rate, pulse oximetry, skin temperature | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The first 30 names of eligible participants were randomly and equally divided into control (receiving mock treatments) and experimental (receiving authentic AMMA treatment) groups." (p. 19) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "Three participants from each group withdrew from the study before receiving treatments. One control group practitioner withdrew from the study as it began and the four participants in that group were unable to reschedule with another practitioner." (p. 19) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Melchior 1996.
| Methods | RCT,Netherlands | |
| Participants | 161 psychiatric nurses in long‐stay settings | |
| Interventions | 1) Experimental: Support and advice given by nurse managers or quality care co‐ordinators: Participants were assigned to patients as primary nurses and given advice by nurse managers or quality care co‐ordinators and they followed a training programme about communication skills over a year. 2) Control: No intervention | |
| Outcomes | MBI | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Random sampling was used to select 492 nurses to complete the questionnaires." (p. 696) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "Two main problems were encountered in this study, namely a high drop‐out rate largely due to job turnover among nurses, and the imitation of the intervention by the control group." (p. 697) A total of 51.6% of the participants dropped out during the study |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Moody 2013.
| Methods | RCT with individual participants, USA | |
| Participants | Paediatric oncology staff (50% nurses, 20% physicians); Experimental 23 Control 24; Men: Experimental 30% Control 8%; Age: not reported; stated to be equal; Experience: > 10 yrs Experimental 48% Control 46% | |
| Interventions | 1) Experimental: 8 weeks of didactic and experiential mindfulness education via a structured, skills‐training course delivered in a group setting at their hospital. The course included 1 initial 6‐hour session; 6 weekly 1‐hour follow‐up sessions; and a final 3‐hour wrap‐up session (15 hours total class time) 2) Control: No intervention |
|
| Outcomes | MBI; Percieved Stress Scale | |
| Notes | Authors provided extra data: SDs of MBI at follow‐up: Experimental: EE: 7.67; DP: 3.54; PA 3.69 Control: EE: 6.39; DP: 4.59; PA: 5.27 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Using a computer‐generated random numbers schema in blocks of 10 |
| Allocation concealment (selection bias) | Unclear risk | Participants were stratified according to their respective professions and randomised to a mindfulness‐based course (intervention) or no intervention (control) |
| Blinding (performance bias and detection bias) All outcomes | High risk | Study not blinded, outcome self report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants reported outcomes |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in the Methods reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Moyle 2013.
| Methods | RCT with individual participants in parallel groups, Australia | |
| Participants | Nurses and assistant nurses in dementia care; 100% women; Age 49 yrs ± 11 yrs; > 10 yrs experience 10%; Experimental n = 9 Control n = 10 | |
| Interventions | 1) Experimental: The intervention was a foot massage delivered by 1 of 2 research assistants trained by an expert certified therapist in the massage technique. In each session, participants received a standardised 5‐minute massage on each foot (10‐minute in total), involving the application of light pressure with long, gliding, rhythmical strokes of the entire foot and ankle, and toe and ankle rotation, flexion and extension [16 ‐ 19]. Unscented Sorbolene (8 ‐ 10 mls) was applied as a lubricant for the massage. 2 ) Control: In the silent resting control sessions participants sat silently with their eyes closed and legs slightly elevated on a beanbag for 10 minutes. A trained research assistant stayed outside the room for the 10‐min period. The purpose of the silent resting condition was to help isolate whether any observed effects were because of the foot massage specifically, or because the participant received special attention and had the opportunity to be away from the work environment for a quiet time. |
|
| Outcomes | Profile of Mood States‐ Bipolar (POMS‐Bipolar); systolic and diastolic blood pressure | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "used a computer program to undertake the permuted‐block randomization process, with block sizes set at six" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Provider and participants not blinded. Outcome self‐reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participant‐outcome data reported |
| Selective reporting (reporting bias) | Low risk | No protocol, but all outcomes from Method section reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Norvell 1987.
| Methods | RCT, USA | |
| Participants | 12 respiratory therapists | |
| Interventions | 1) Experimental: Stress management programme: 8 weekly group sessions on average 60 minutes and a manual containing homework assignments to be completed between sessions. Topics covered were deep muscle relaxation, cognitive‐behavioural exercises to identify and examine stressful situations, replacing negative thoughts and emotions with adaptive rational cognitions, effective communication skills, social support networks and problem‐solving skills, physical fitness, nutrition and weight management and maintenance of behaviour change. 2) Control: No intervention | |
| Outcomes | MBI, C‐H Inventory of Phys Symptoms, The Hassles Scale, The Uplifts Scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The 12 participating employees were randomly assigned to one of two conditions: 6 to an 8‐week stress management programme and 6 to a wait‐list control group." (p. 120) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no dropouts because of small sample size |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Oman 2006.
| Methods | RCT, USA | |
| Participants | 58 staff members (64% nurses, 12% physicians and 24% other) of a large hospital | |
| Interventions | 1) Experimental: Eight‐Point Program Spiritual Skills Training: 8 weekly 2‐hour training sessions about meditation skills (passage meditation, mantram repetition, slowing down, focused attention, training the senses, putting others first, spiritual association and inspirational reading). 2) Control: No intervention | |
| Outcomes | Perceived Stress Scale, MBI, Medical Outcomes Study | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Details of randomisation were provided in a separate supplement to the article: "While participants were completing pretests, individuals were randomly assigned to treatment (n = 30) or wait‐list control (n = 31). Computer pre‐generated 1:1 random assignment tables had been prepared by the lead investigator for each potential number of registering participants, up to 60, for each session (precise number of registrants could not be anticipated). At each session, as participants completed pretests, their consent forms were rapidly assembled in an arbitrary order and given sequential numbers by the lead investigator or the main instructor. The total number of received consent forms dictated the appropriate random assignment table, which dictated how to separate the numbered consent forms into two groups." (p. S4) |
| Allocation concealment (selection bias) | High risk | "Immediately following pretest, participants were informed of their group assignment. One or two weeks later, those in the treatment condition began the eight week training, meeting together in one large group." (p. S4) |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Selected characteristics of the 58 final participants included in the intention‐to‐treat analysis are displayed in Table 1" (p. 715) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Palumbo 2012.
| Methods | RCT, USA | |
| Participants | 14 registered or licensed practical female nurses aged 49 years and older who were currently employed at an academic medical centre full‐time or part‐time in a staff nurse position that involved lifting patients. | |
| Interventions | 1) Experimental: Tai Chi: onsite Tai Chi classes once a week and to practise on their own for 10 minutes each day at least 4 days per week for 15 weeks. Each Tai Chi class lasted 45 minutes, with 10 minutes of breathing exercises, followed by 30 minutes of Tai Chi practice, and ended with 5 minutes of visualisation and cool‐down exercises. 2) Control: No intervention | |
| Outcomes | Nursing Stress Scale, Perceived Stress Scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 3/14 participants dropped out. No imputation of data |
| Selective reporting (reporting bias) | High risk | Only change values were reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Peterson 2008.
| Methods | RCT, Sweden | |
| Participants | 131 healthcare workers who scored above the 75th percentile on the exhaustion dimension of the Oldenburg Burnout Inventory | |
| Interventions | 1) Experimental: Reflecting peer‐support group: 10 2‐hour weekly sessions where participants discussed and reflected with colleagues about work‐related stress and burnout, provided mutual support for each other, compared experiences and set individual goals to find out alternative ways to handle perceived stressful situations. The sessions started with a short 10‐minute guided relaxation. 2) Control: No intervention | |
| Outcomes | The General Nordic Questionnaire for Psychological and Social Factors at Work (QPS Nordic), Oldenburg Burnout Inventory, The Hospital Anxiety and Depression Scale, The Short Form Health Survey (SF‐36) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The randomization procedure was performed by a statistician using the Statistical Analysis Software, version 8.2." (p. 508) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Altogether 27% of participants dropped out during follow‐up and the reasons for the control group participants leaving were not known |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Proctor 1998.
| Methods | Cluster‐randomised trial, UK | |
| Participants | 98 care staff in residential nursing homes | |
| Interventions | 1) Experimental: Developing knowledge and skills and individual programme planning: 7 hour‐long seminars over a period of 6 months about the theoretical basis of organic and functional disorders experienced in old age and approaches to care and activities in residential settings. The second part of the training schedule consisted of weekly visits to intervention homes by an experienced psychiatric nurse who trained staff in behavioural management of residents by developing individual care programmes for them. 2) Control: No intervention | |
| Outcomes | The Occupational Stress Indicator, GHQ | |
| Notes | Measurements were completed at baseline and immediately following the 6‐month intervention. We accounted for the design effect (participants randomised in clusters but analysed as individuals) by dividing the number of participants by the calculated design effect of 1.143. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Ten residential care homes and two nursing homes participated in the study and were matched into pairs according to size and accreditation status. One of each pair of homes was then randomised to one of two groups by computer." (p. 3) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "There was no survivor effect due to staff attrition on any of the measures completed; missing data were replaced by the last known assessment carried forward." (p. 5) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Razavi 1993.
| Methods | RCT, Belgium and France | |
| Participants | 72 oncology nurses | |
| Interventions | 1) Experimental: a 24‐h Psychological Training Program: 8 3‐hour sessions weekly in groups of 6 participants about issues related to patient care, healthcare professionals' problems and family care. Each session began with a case presentation (75 mins) and was followed by a role‐playing exercise with videotaped feedback (75 mins). The role‐playing exercises were themed: information during the diagnostic phase, pain control, support during chemotherapy, euthanasia request, healthcare professional‐family collusion and family problems. The last session included a presentation of theoretical information and and assessment of the programme. 2) Control: No intervention | |
| Outcomes | The Nursing Stress Scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "A randomised group design was used in which nurse candidates for a P.T.P [psychological training program] were allocated to a P.T.P. group or to a 4‐month waiting list group. Subjects were randomised separately in the different institutions in order to allocate 6 subjects to the training program and 6 subjects to the waiting list in each consecutive group of 12 eligible subjects in an institution. (p. 1858) |
| Allocation concealment (selection bias) | Low risk | "The randomised interventions were indicated by opening a sealed envelope once subjects satisfied the inclusion criteria of the study" (p. 1858) |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "After initial contact one subject was unable to continue participation in the training. Two subjects belonging to the waiting list group and one to the trained group refused to participate in the role‐playing exercise. These subjects were excluded from the data analysis." (p. 1860) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Redhead 2011.
| Methods | RCT, UK | |
| Participants | 42 nurses working in a low‐secure mental health unit (LSU). Inclusion criteria: working on the LSU for a minimum of 35 hours and having direct contact with service users. Exclusion criteria: having been previously trained in Psychosocial Intervention. "A total of 79 nursing staff worked on the LSU. Forty‐two (58%) volunteered to participate in the study and provided informed consent. Of the remaining 37 staff, none actively refused but eight were on sick leave, 23 were unable to be released by their managers to attend the training and six were excluded as they had previously been trained in PSI." (p. 61) "There were no significant differences at baseline between the experimental and control groups in terms of age, gender, clinical area or qualification." (p. 62) |
|
| Interventions | 1) Experimental: Psychosocial intervention training (12 qualified and 10 unqualified nurses). "Nurses allocated to the experimental group attended a PSI [Psychosocial Intervention] training programme which was delivered in a meeting room within the LSU. As the learning outcomes for qualified and unqualified staff were different, they were trained on separate courses. The training programme for qualified staff consisted of 16 half‐day sessions delivered over 8 months. The content covered a broad range of PSI including cognitive behavioural approaches for managing symptoms..." " The training for unqualified staff was delivered in 8 half‐day sessions and focused on understanding symptom related behaviours, relationship formation and helping services users to cope with symptoms..." "Teaching sessions were supplemented by small group supervision..." (p. 61) 2) Control: No intervention control (9 qualified and 11 unqualified nurses) |
|
| Outcomes | The MBI | |
| Notes | From reference list: Doyle 2007 ‐ check for inclusion | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "A randomized controlled design was adopted with nurses who volunteered to participate being allocated to either the experimental PSI training group or a waiting list control group." (p. 60) |
| Allocation concealment (selection bias) | Unclear risk | Not reported if group allocation was concealed |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants could not be blinded regarding group allocation. Also as outcome measurement was by self report, there was no blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Apparently no participants were lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | The authors report all results for outcome measures listed in the Methods section |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Reynolds 1993.
| Methods | RCT, UK | |
| Participants | 62 health service workers | |
| Interventions | 1) Experimental: Stress Management Training (SMT): 6 weekly 2‐hour sessions of didactic learning, practice of techniques, group exercises and discussion. Topics covered were: nature, signs, causes and symptoms of stress, progressive muscular relaxation, relationship difficulties at home and work, assertiveness techniques, cognitive appraisal and reappraisal, time‐management and goal‐setting skills and emotions and seeking social support. 2) Control: No intervention | |
| Outcomes | General Health Questionnaire (GHQ‐12) used to obtain a score labelled psychological distress | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The main features of the overall study design include random allocation of groups to receive SMT either immediately or after a waiting period." (p. 329) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only the data for those participants (62/92) who had completed the full set of assessment questionnaires were used in the analyses |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Romig 2012.
| Methods | Controlled before‐and‐after study, USA | |
| Participants | ICU nurses, Experimental n = 27 (out of 70) Control n = 11 (out of 65), age, experience, gender not reported | |
| Interventions | 1) Experimental: Introduction of tele‐medicine: remote access to more patients by 1 physician and 1 nurse tele‐ICU, 11 week experiment 2) Control: no intervention |
|
| Outcomes | Safety attitudes Questionnaire contains questions about burn out such as 'I feel burnout by my work' | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not randomised |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding of providers or participants; outcome self‐reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Small number of all staff participated in questionnaires |
| Selective reporting (reporting bias) | Unclear risk | All outcomes that were in the Methods section are reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Rowe 2006.
| Methods | RCT, USA | |
| Participants | 108 healthcare professionals (42 nurses, 24 hospital/clinical staff, 10 physicians/surgeons, 15 administrators, 9 psychologists/counselors/social workers and 8 health educators) | |
| Interventions | 1) Experimental 1: Stress management/adaptive coping training: 6 weekly 90‐minute sessions. Purpose of sessions was to develop problem‐focused strategies when addressing problems that generally have solutions and emotion‐focused strategies when solutions are not available. Participants practised employing these strategies in small groups (6 ‐ 8 people) on real‐life problems faced recently in the work environment. 2) Experimental 2: Stress management/adaptive coping training, with 1‐hour refresher sessions at 5 months, 11 months and 17 months 3) Control: No intervention | |
| Outcomes | MBI, Stress Assessment Inventory, State‐Trait Anxiety Inventory | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Of those willing, approximately 40% (N=126) were randomly selected and assigned to 3 groups..." (p. 606) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No imputation used or last observation carried forward |
| Selective reporting (reporting bias) | Low risk | Only MBI measured and reported at each follow‐up point but the author explained when contacted that this was always the plan. |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Saganha 2012.
| Methods | RCT with individual participants, Portugal | |
| Participants | Physiotherapists scoring more than 26 on Emotional Exhaustion subscale of MBI out of 106 screened with MBI, and not familiar with Qigong; Experimental n = 8 Control n = 8 | |
| Interventions | 1) Experimental: Qigong exercise: posture, breathing and mind focus; classes 20 min/day 1 week; self treatment 2X / day 2 weeks, total 3 weeks 2) Control: Waiting list for 3 weeks; after that they got the treatment as well |
|
| Outcomes | MBI | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "the design was a prospective randomized controlled study" |
| Allocation concealment (selection bias) | Unclear risk | "the design was a prospective randomized controlled study" |
| Blinding (performance bias and detection bias) All outcomes | High risk | Providers and participants not blinded; outcome self‐reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Outcomes for all participants reported |
| Selective reporting (reporting bias) | Unclear risk | Baseline data not reported for the RCT group only |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Salles 2013.
| Methods | RCT with individual participants, USA | |
| Participants | Resident surgeons in various specialties, Experimental n = ? Control n = ?, n = 35 total | |
| Interventions | 1) Experimental: Reading about challenges that seniors had faced as part of the training programme 2) Control: Reading about ethical issues that seniors had faced |
|
| Outcomes | Burn‐out | |
| Notes | Author did not respond to inquiries | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "We utilized a randomized, controlled trial.." |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | Not clear if these were all outcomes |
| Other bias | Unclear risk | Abstract only with information missing; authors have not replied to inquiries |
Schrijnemaekers 2003.
| Methods | Cluster‐randomised trial, Netherlands | |
| Participants | 300 professional caregivers in homes for elderly persons | |
| Interventions | 1) Experimental: Emotion‐oriented care training, clinical lessons and supervision meetings: 1‐hour clinical lesson, 6‐day training programme with 4 days at a 2‐week interval and last 2 days at a 4‐week interval. The participants were taught about the dementia syndrome and various care models for communicating with elderly people with dementia (e.g. reality orientation, validation and reminiscence), inequality of the resident‐caregiver relation, understanding the residents' perception of the environment and the attitude and (non‐)verbal communication of staff towards the resident. Intervention homes also received 3 half‐day supervision meetings to support the implementation of emotion‐oriented care. 2) Control: No intervention | |
| Outcomes | MBI, Job satisfaction | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomization was performed on the level of homes. ...within each pair, one home was randomly assigned to the intervention or control group, and the home was assigned to the alternate state." (p. S51) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Missing values on items that were part of a scale or subscale were replaced according to the "mean value of valid subtests" principle (i.e. replacement by the mean value calculated from the valid item scores of the [sub‐] scale obtained for the same subject at the same time point). This replacement strategy was only used if less than 25% of the items of a scale or subscale had missing values." (p. S52) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Shapiro 2005.
| Methods | RCT, USA | |
| Participants | 38 healthcare professionals including physicians, nurses, social workers, physical therapists and psychologists | |
| Interventions | 1) Experimental: Mindfulness‐Based Stress Reduction programme: 8 weekly 2‐hour training sessions about employing the techniques involved in sitting meditation, body scan, hatha yoga, 3‐minute breathing space (a "minimeditation") and a "loving kindness" meditation. 2) Control: No intervention | |
| Outcomes | MBI, Perceived Stress Scale, Brief Symptom Inventory | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Participants were randomly assigned to an 8‐week MBSR group or a wait‐list control group." (p. 167) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "Owing to the pilot nature of this study and the small sample size, we did not perform intention‐to‐treat analyses but compared only those participants who did not drop out" (p. 169) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Sood 2011.
| Methods | RCT, USA | |
| Participants | 40 physicians working at Mayo Clinic Rochester "Inclusion criteria were: (1) being a faculty member of the DOM and (2) being able and willing to participate. Exclusion criteria were: (1) recent (within the past 6 months) psychotic episode or (2) clinically significant acute unstable neurological, psychiatric, hepatic, renal, cardiovascular, or respiratory disease that prevented participation in the study." (p. 859) "Mean age of the participants in the active arm (46.8 ± 8.3 years) was comparable to the control arm (50.2 ± 5.7 years). Gender distribution was comparable across the two arms (55% vs 50% males in the active and control arm, respectively)." (p. 859) |
|
| Interventions | 1) Experimental: Stress Management and Resiliency Training (SMART) programme (n = 20). "The study intervention was a single 90‐min session training in the SMART program. The SMART program has been adapted from Attention and Interpretation Therapy (AIT). AIT is a structured therapy developed at the Mayo Clinic to decrease stress and enhance resilience. AIT addresses two aspects of human experience, attention and interpretation." "AIT guides learners to delay judgment and pay greater attention to the novelty of the world. Complementing attention training is instruction to help participants direct their interpretations away from fixed prejudices toward a more flexible disposition while cultivating skills such as gratitude, compassion, acceptance, forgiveness, and higher meaning." " Participants were also offered an optional 30–60 min follow‐up session depending on individual needs. (p. 859) 2) Control: No intervention control (n = 20) |
|
| Outcomes | Perceived Stress Scale, Smith Anxiety Scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "After obtaining the informed consent, physicians were randomly assigned to one of two groups ‐ an active arm or a wait‐list control arm." (p. 859) |
| Allocation concealment (selection bias) | Unclear risk | The authors do not report if they concealed allocation |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants could not be blinded regarding group allocation. Also as outcome measurement was by self report, there was no blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Apparently there were no dropouts |
| Selective reporting (reporting bias) | Low risk | The authors report all results for outcome measures listed in the Methods section. |
| Other bias | High risk | "Eight participants (all in the control arm) declined to participate after randomization and prior to filling out any assessments because of scheduling issues" (p. 860) |
Stanton 1988.
| Methods | RCT, Australia | |
| Participants | 40 trained hospital nurses who complained being overstressed | |
| Interventions | 1) Experimental: Ego‐enhancement training: 1 50‐minute session and 3 20‐minute sessions 1 week apart of training in the techniques of: physical relaxation, mental calmness, disposing of "rubbish", removal of a barrier and enjoyment of a special place. 2) Control: No intervention | |
| Outcomes | Stress Profile | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "In the first stage of the experiment the nurses were matched on their Profile scores, one member of each pair being allocated at random to either a non‐treatment control group or an experimental group experiencing four treatment sessions" (p. 318) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It is unclear if any participants dropped out |
| Selective reporting (reporting bias) | Low risk | Only 1 outcome measure used and reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Tsai 1993.
| Methods | RCT, Taiwan | |
| Participants | 137 nurses | |
| Interventions | 1) Experimental: Training about stress at work, relaxation, breathing, imagery and meditation: 1 90‐minute session in each of 2 weeks and 1 follow‐up session in the 5th week. Training covered: sources of stress at work, relaxation as a coping method and meditation including breathing exercise and imagery that emphasised the underlying cognitive process of meditation. 2) Control: Traditional in‐service education about theory analysis | |
| Outcomes | Nurse Stress Checklist, Chinese General Health Questionnaire | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "For each unit, a coin was thrown to select which nurse from this unit would be assigned to either the experimental or control group." (p. 56) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It is unclear if any participants dropped out |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Uchiyama 2013.
| Methods | Cluster‐RCT of hospital wards, Japan | |
| Participants | Nurses (n = 434) in 24 units in 2 general hospitals ; Experimental: 11 units with 183 nurses; Control: 13 units with 218 nurses; Gender: all women; Age: Experimental: 33 yrs ± 10 yrs; Control: 32 yrs ± 9 yrs Experience: Experimental: 11 yrs ± 8 yrs; Control: 10 yrs ± 9 yrs | |
| Interventions | 1) Experimental: Participatory psychosocial work environment improvement programme with varying elements over 6 months per unit; first 3 months development, last 3 months implementation 2) Control: No intervention |
|
| Outcomes | CES‐Depression, Job Content Questionnaire, Effort Reward Imbalance‐Questionnaire | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation of the intervention group and the wait list control group was conducted at the unit level after stratification by hospital and department nature (outpatient/inpatient) and carried out by a person who was not involved in the intervention or evaluation |
| Allocation concealment (selection bias) | Unclear risk | See above; not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Providers and participants not blinded; outcome self‐reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Experimental: 168/183 = 91% follow‐up; Control: 193/218 = 89% follow‐up |
| Selective reporting (reporting bias) | Low risk | No protocol but all outcomes from Methods reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Von Baeyer 1983.
| Methods | Cross‐over study, Canada | |
| Participants | 14 nurses in a burn treatment unit | |
| Interventions | 1) Experimental: Cognitive‐behavioural stress management training: 3 individual 1‐hour sessions over a period of 5 ‐ 8 days with a minimum of 2 days and a maximum of 5 days between sessions. Topics covered in the 1st session were: a conceptualisation of stress, situational stressors, psychological appraisal and physiological arousal. This was followed by training in relaxation and deep breathing. In the 2nd session participants were taught cognitive strategies for reducing stress (e.g. thought stopping, attention diversion and engaging in coping self‐statements). In the 3rd session the trainer modelled the use of stress management techniques in a role‐played burn treatment situation. Participants were also given a 4‐page outline of stress management techniques to read. 2) Control: No intervention | |
| Outcomes | STAI | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Subjects were randomly assigned to one of two groups." (p. 115) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "One nurse chose not to attend the third session of stress management training, but all fourteen subjects were involved in data collection procedures throughout the forty‐three day study period." (p. 114) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
West 1984.
| Methods | RCT, USA | |
| Participants | 60 acute care hospital nurses | |
| Interventions | 1) Experimental: 4 weeks of Stress Inoculation (SI) training divided as: i) Education‐only group (Ed) weekly 30‐minute sessions of information about anxiety, stress and coping skills and practice of self‐monitoring of stress producing events (n = 12) ii) Education + coping skills group (CS), 4 weekly 60‐minute sessions including education plus CS. CS: relaxation training, assertive skill training, cognitive restructuring and time‐management instruction (n = 12) iii) Education + exposure group (Ex) 4 weekly 60‐minute including education plus simulated stress‐producing situations via role play (n = 12) iv) Education + coping skills + exposure group (SI) 60‐minute sessions twice a week during 4 weeks including all the above (n = 12) 2) Control: No intervention (n = 12) |
|
| Outcomes | MBI (used frequency and intensity separately for each subscale); we used Emotional Exhaustion intensity scores. Job‐Related Tension Index, Life Satisfaction Index, STAI, Rathus Assertiveness Schedule, systolic and diastolic blood pressure | |
| Notes | Results are only presented for the group including CS (n = 24) versus education plus no‐intervention (n = 24) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "...60 registered nurses... were stratified on the basis of work shift and randomly assigned to 1 of 6 counselors and one of five treatment conditions." (p. 212) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "No subject attrition occurred at posttesting." (p. 213) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Yamagishi 2008.
| Methods | RCT, Japan | |
| Participants | 60 shift work nurses | |
| Interventions | 1) Experimental: Web‐based career identity training: 1 60‐minute training session that covered the definition of career identity, cognition of participants' own career identity, characteristics of nurses' career identity and career goal management and planning. 2) Control: No intervention | |
| Outcomes | Brief Job Stress Questionnaire | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The 60 participants were randomly allocated into the intervention and control groups by the hospital" (p. 191) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 60 nurses were randomised to intervention and control and after 3 weeks at post‐intervention measurement only 36 (60%) remained |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Yazdani 2010.
| Methods | RCT, Iran | |
| Participants | 76 nursing students "The study population included all male and female nursing students who were studying in Isfahan Nursing and Midwifery university in 2010‐2011, in the second and third years (third, fourth, fifth and sixth semesters). 72 [sic] students were randomly assigned to two groups using the list of students studying in the second and third year in 2010‐2011 and based on the odd and even numbers." (p. 210) "The groups were heterogeneous in terms of gender..." (p. 210) |
|
| Interventions | 1) Experimental: Stress management training (n = 38). "[F]irst group (n=38) trained stress management training program (8 two hours sessions, twice a week). And second group (n = 38) did not received [sic] training." (p. 210) The stress management program consisted of: information about stress, gradual muscle relaxation and its implementation with mental imagery, consequences and physical symptoms of stress, relaxation and imagery and training and diaphragm breathing practices, linking thoughts and emotions and familiarity with cognitive errors, discussion about relaxation exercises and replacement of logical thoughts and personal stress management program. 2) Control: no intervention (n = 38) |
|
| Outcomes | DASS‐42: Depression, Anxiety and Stress Scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "...students were randomly assigned to two groups using the list of students studying in the second and third year in 2010‐2011 and based on the odd and even numbers." (p. 210) |
| Allocation concealment (selection bias) | Unclear risk | Not reported if group allocation was concealed |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants could not be blinded regarding group allocation. Also as outcome measurement was by self report, there was no blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It is difficult to tell if some participants were lost to follow‐up or not as the authors give three separate numbers for the amount of participants. "This study was a parallel ‐group randomized quasi‐experimental trial...on 68 Bs nursing students.", " 72 students were randomly assigned..." and "Finally seventy‐six subjects elected among them." (p. 210) |
| Selective reporting (reporting bias) | Low risk | The study had only one outcome and its results are all reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Yung 2004.
| Methods | RCT, China | |
| Participants | 65 nurse managers | |
| Interventions | 1) Experimental 1: Cognitive relaxation: participants were asked to imagine the relaxation of different muscle groups. 2) Experimental 2: Stretch‐release relaxation: training guided by the model of Stretch Relaxation developed by Carlson and Collins (1990) which focused on the stretching and relaxation of muscle groups. Unlike the popular progressive relaxation exercise which involves the tensing and relaxing of muscle groups, stretch‐release relaxation is less strenuous. Muscle relaxation exercise, based upon the stretching of muscle groups, incorporates the beneficial effects of muscle sensation contrast with accompanied reductions in muscle activity from the stretch procedure resulting in relaxation. 3) Control: No intervention | |
| Outcomes | C‐STAI, C‐GHQ | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Of the 65 participants, 35 were randomly assigned to the experimental condition and the remaining 30 were put to the control condition. Subsequently, the 35 subjects assigned to the experimental condition were randomly allocated to the stretch‐release relaxation (n = 17) and cognitive relaxation (n = 18) groups." (p. 256) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible, self report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "All participants including the TC [test control] group were assessed again in a follow‐up session after 1 month." (p. 258) We assume this means that there were no dropouts |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
4DKL: De Vierdimensionale Klachtenlijst (Four Dimensional Symptom Questionnaire ‐ 4DSQ) BDI: Beck Depression Inventory DP: Depersonalisation EE: Emotional Exhaustion EMH: e‐mental health GHQ: General health questionnaire ICU: intensive care unit LSU: low‐secure unit MBI: Maslach burnout inventory MPSS‐R: Medical Personnel Stress Survey‐Revised PA: Personal Accomplishment (lack of) POMS: Profile of Mood States RCT: randomised controlled trial SCL‐90‐R: Symptom Checklist 90 Revised STAI: State‐trait anxiety inventory VAS: visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Andersen 2010 | The study is uncontrolled. |
| Baldelli 2004 | The intervention is primarily aimed at demented patients at a care home and not the staff caring for them, although the effects were measured also for the latter. |
| Bay 2010 | The study does not employ a primary outcome measure of stress or burnout. |
| Beddoe 2004 | The study is uncontrolled. |
| Bormann 2006 | The study is uncontrolled. |
| Bost 2006 | The study does not employ a primary outcome measure of stress or burnout. |
| Bourbonnais 2006a | The study is non‐randomised by design and the intervention is directed at persons or the person/work interface. |
| Bourbonnais 2006b | There is no intervention aimed at preventing or treating stress or burnout. |
| Brinkborg 2011 | There is no intervention aimed at preventing or treating stress or burnout. |
| Bruneau 2004 | The study is uncontrolled. |
| Cohen 2005 | The study is uncontrolled. |
| Cooke 2007 | The study is uncontrolled. |
| Cuneo 2011 | The study is uncontrolled. |
| Cutshall 2011 | The study is uncontrolled. |
| Cámara Conde 2009 | There is no intervention aimed at preventing or treating stress or burnout. |
| Davis 2005 | The study is uncontrolled. |
| Diaz‐Rodriguez 2011a | Participants were diagnosed with burnout. |
| Diaz‐Rodriguez 2011b | Participants were diagnosed with burnout. |
| Drain 1991 | The participants of the study are not healthcare personnel or nursing students with clinical duties. |
| Dunn 2007 | The study is non‐randomised by design. |
| Edmonds 2012 | The study is non‐randomised by design. In the first wave all participants received intervention. In the second wave half were randomised to receive a booster session. |
| Elo 2000 | The study is uncontrolled. |
| Freedy 1994 | The study is non‐randomised by design. |
| Galantino 2005 | The study is uncontrolled. |
| Gorter 2001 | The study is non‐randomised by design. |
| Holt 2006 | The study is non‐randomised by design and the intervention is directed at persons or the person/work interface. |
| Isaksson Rø 2008 | The study is non‐randomised by design. |
| Isaksson Rø 2010 | The study is non‐randomised by design. |
| Italia 2008 | The study is non‐randomised by design. |
| Johansson 1991 | The participants are nursing students but do not have clinical duties. |
| Ju 2006 | There is no intervention aimed at preventing or treating stress or burnout. |
| Kendall 2005 | The study is uncontrolled. |
| Keyes 1988 | The study is non‐randomised by design. |
| Koivu 2012 | The study is non‐randomised by design. |
| Kushnir 1994 | The study is uncontrolled. |
| Kushnir 1998 | The study is non‐randomised by design. The measurements in the comparison group were done a year later than in the intervention group. |
| Lai 2012 | The study does not employ a primary outcome measure of stress or burnout. |
| Lewis 1990 | The study is uncontrolled. |
| McCue 1991 | The study is non‐randomised by design. |
| Michie 1992 | The study is uncontrolled. |
| Michie 1994 | The study is non‐randomised by design and the intervention is directed at persons or the person/work interface. |
| Moeini 2011 | The study is non‐randomised by design. |
| Murphy 1983 | The study is non‐randomised by design. |
| Newsome 2010 | The study is uncontrolled. |
| Newton 2006 | The study is uncontrolled. |
| Nhiwatiwa 2003 | The participants were victims of assault and deemed not healthy as per inclusion criteria. |
| Nooryan 2011 | The study is non‐randomised by design. |
| Nooryan 2012 | The study is non‐randomised by design. |
| Orly 2011 | The study is non‐randomised by design. |
| Ortega Ruiz 2008 | The study is uncontrolled. |
| Panda 2010 | The study is non‐randomised by design. |
| Pemberton 2008 | The study is uncontrolled. |
| Petterson 1998 | The study is non‐randomised by design and the intervention is directed at persons or the person/work interface. |
| Petterson 2006 | The study is uncontrolled. |
| Pipe 2009 | The study does not employ a primary outcome measure of stress or burnout. |
| Poulin 2008 | The study is non‐randomised by design. |
| Prasad 2011 | The study is uncontrolled. |
| Ridge 2011 | There is no intervention aimed at preventing or treating stress or burnout. The article only presents the design of an intervention and not an assessment of its implementation. |
| Russler 1991 | The participants are nursing students but do not have clinical duties. |
| Saadat 2012 | The study does not employ a primary outcome measure of stress or burnout. |
| Salyers 2011 | The study is non‐randomised by design. |
| Sarid 2010 | The study is uncontrolled. |
| Schaufeli 1995 | The study is uncontrolled. |
| Shanafelt 2014 | The study is non‐randomised by design. |
| Sharif 2004 | The participants are nursing students but do not have clinical duties. |
| Sharif 2013 | The study does not employ a primary outcome measure of stress or burnout. |
| Tang 2010 | The study is uncontrolled. |
| Taylor 2001 | The study does not employ a primary outcome measure of stress or burnout. |
| Te Brake 2001 | The study is non‐randomised by design. |
| Van Dierendonck 1998 | The study is non‐randomised by design. |
| Villani 2011 | The study does not employ a primary outcome measure of stress or burnout. |
| Villani 2012 | The study does not employ a primary outcome measure of stress or burnout. |
| Wassel 1993 | The study is uncontrolled. |
| Wetzel 2011 | There is no intervention aimed at preventing or treating stress or burnout. |
| Winefield 1998 | The study is uncontrolled. |
| Yamagishi 2007 | The study is uncontrolled. |
| Yong 2011 | The study is non‐randomised by design. |
| Young 2001 | The study is non‐randomised by design and the intervention is directed at persons or the person/work interface. |
| Zimber 2001 | The study is non‐randomised by design and the intervention is directed at persons or the person/work interface. |
Characteristics of studies awaiting assessment [ordered by study ID]
Khaghanizadeh 2008.
| Methods | Comparative study |
| Participants | Nurses |
| Interventions | Imagery? |
| Outcomes | MBI |
| Notes | in Persian awaiting translation |
Ruehl 2013.
| Methods | RCT |
| Participants | nurses |
| Interventions | CBT |
| Outcomes | |
| Notes | dissertation |
CBT: Cognitive behavioural training MBI: Maslach burnout inventory
Characteristics of ongoing studies [ordered by study ID]
Gomez‐Gascon 2013.
| Trial name or title | ClinicalTrials.gov Identifier: NCT01870154 |
| Methods | RCT |
| Participants | Primary care health professionals |
| Interventions | Education about burnout |
| Outcomes | MBI‐EE |
| Starting date | ? |
| Contact information | Gomez‐Gascon, Tomas |
| Notes | Spain |
Niks 2013.
| Trial name or title | DISCovery |
| Methods | Controlled before‐and‐after study |
| Participants | Health Care Workers |
| Interventions | Organisational changes |
| Outcomes | MBI among many others |
| Starting date | |
| Contact information | i.m.w.niks@tue.nl |
| Notes |
Spoor 2010.
| Trial name or title | Direct Project |
| Methods | Controlled before‐and‐after study |
| Participants | 8 wards with nursing home staff |
| Interventions | Interventions to increase job resources and recovery opportunities and performance outcomes in nursing homes |
| Outcomes | Job‐related health, well‐being, |
| Starting date | 2010? |
| Contact information | e.m.b.spoor@tue.nl |
| Notes | Netherlands |
EE: emotional exhaustion MBI: Maslach burnout inventory
Differences between protocol and review
In the previous version of this review (Marine 2006) we categorised interventions as person‐ and work‐directed. We think the new categorisation into cognitive‐behavioural, mental and physical relaxation and organisational interventions is more informative.
Contributions of authors
Jani Ruotsalainen, Albert Mariné, Jos Verbeek and Consol Serra screened the systematic search results for potential new studies to include. Jani Ruotsalainen, Albert Mariné, Consol Serra and Jos Verbeek extracted data from new included studies and also assessed the risk of bias of the previously included studies. Jani Ruotsalainen and Jos Verbeek rebuilt the comparisons and ran the analyses. Jos Verbeek and Jani Ruotsalainen wrote the first draft of the updated review text. All authors commented on the draft. Jani Ruotsalainen is the guarantor of the review.
Sources of support
Internal sources
Cochrane Occupational Safety and Health Review Group, Finland.
Finnish Institute of Occupational Health, Finland.
Corporació Parc Taulí (Sabadell), Spain.
Network of Centers for Research on Epidemiology and Public Health, Spain.
External sources
Ministry of Social Affairs and Health, Finland.
Declarations of interest
Jani Ruotsalainen: None known.
Jos Verbeek: None known.
Consol Serra: None known.
Albert Marine: None known.
New search for studies and content updated (conclusions changed), comment added to review
References
References to studies included in this review
Ali 2011 {published data only}
- Ali NA, Hammersley J, Hoffmann SP, O'Brien JM Jr, Phillips GS, Rashkin M, et al. Continuity of care in intensive care units: a cluster‐randomized trial of intensivist staffing. American Journal of Respiratory and Critical Care Medicine 2011;184(7):803‐8. [DOI] [PubMed] [Google Scholar]
Bittman 2003 {published data only}
- Bittman B, Bruhn KT, Stevens C, Westengard J, Umbach PO. Recreational music‐making: a cost‐effective group interdisciplinary strategy for reducing burnout and improving mood states in long‐term care workers. Advances in Mind‐Body Medicine 2003;19(3‐4):4‐15. [PubMed] [Google Scholar]
Bourbonnais 2011 {published data only}
- Bourbonnais R, Brisson C, Vinet A, Vézina M, Abdous B, Gaudet M. Effectiveness of a participative intervention on psychosocial work factors to prevent mental health problems in a hospital setting. Occupational and Environmental Medicine 2006;63(5):335‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourbonnais R, Brisson C, Vinet A, Vézina M, Lower A. Development and implementation of a participative intervention to improve the psychosocial work environment and mental health in an acute care hospital. Occupational and Environmental Medicine 2006;63(5):326‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourbonnais R, Brisson C, Vézina M. Long‐term effects of an intervention on psychosocial work factors among healthcare professionals in a hospital setting. Occupational and Environmental Medicine 2011;68(7):479‐86. [DOI] [PubMed] [Google Scholar]
Brennan 2006 {published data only}
- Brennan MK, DeBate RD. The effect of chair massage on stress perception of hospital bedside. Journal of Bodywork and Movement Therapies 2006;10(4):335‐42. [Google Scholar]
Carson 1999 {published data only}
- Carson J, Cavagin J, Bunclark J, Maal S, Gournay K, Kuipers E, et al. Effective communication in mental health nurses: did social support save the psychiatric nurse?. NT Research 1999;4:31‐42. [Google Scholar]
Cohen‐Katz 2005 {unpublished data only}
- Cohen‐Katz J, Wiley SD, Capuano T, Baker DM, Kimmel S, Shapiro S. The effects of mindfulness‐based stress reduction on nurse stress and burnout, Part II: A quantitative and qualitative study. Holistic Nursing Practice 2005;19(1):26‐35. [DOI] [PubMed] [Google Scholar]
Delvaux 2004 {published data only}
- Delvaux N, Razavi D, Marchal S, Bredart A, Farvacques C, Slachmuylder JL. Effects of a 105 hours psychological training program on attitudes, communication skills and occupational stress in oncology: a randomised study. British Journal of Cancer 2004;90(1):106‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ewers 2002 {published data only}
- Ewers P, Bradshaw T, McGovern J, Ewers B. Does training in psychosocial interventions reduce burnout rates in forensic nurses?. Journal of Advanced Nursing 2002;37(5):470‐6. [DOI] [PubMed] [Google Scholar]
Finnema 2005 {published data only}
- Finnema E, Droes RM, Ettema T, Ooms M, Ader H, Ribbe M, et al. The effect of integrated emotion‐oriented care versus usual care on elderly persons with dementia in the nursing home and on nursing assistants: a randomized clinical trial. International Journal of Geriatric Psychiatry 2005;20(4):330‐43. [DOI] [PubMed] [Google Scholar]
Gardner CBT 2005 {published data only}
- Gardner B, Rose J, Mason O, Tyler P, Cushway D. Cognitive therapy and behavioural coping in the management of work‐related stress: An intervention study. Work and Stress 2005;19(2):137‐52. [Google Scholar]
Gardner Coping 2005 {published data only}
- Gardner B, Rose J, Mason O, Tyler P, Cushway D. Cognitive therapy and behavioural coping in the management of work‐related stress: An intervention study. Work and Stress 2005;19(2):137‐52. [Google Scholar]
Gärtner 2013 {published data only}
- Gärtner FR, Nieuwenhuijsen K, Ketelaar SM, Dijk FJH, Sluiter JK. The Mental Vitality @ Work Study: effectiveness of a mental module for workers E‐health surveillance for nurses and allied health care professionals on their help‐seeking behavior. Journal of Occupational and Environmental Medicine 2013;55(10):1219‐29. [DOI] [PubMed] [Google Scholar]
- Ketelaar SM, Gärtner FR, Bolier L, Smeets O, Nieuwenhuijsen K, Sluiter JK. Mental Vitality @ Work‐‐a workers' health surveillance mental module for nurses and allied health care professionals: process evaluation of a randomized controlled trial. Journal of Occupational and Environmental Medicine 2013;55(5):563‐71. [DOI] [PubMed] [Google Scholar]
Ghazavi 2010 {published data only}
- Ghazavi Z, Lohrasbi F, Mehrabi T. Effect of communication skill training using group psycho‐education method on the stress level of psychiatry ward nurses. Iranian Journal of Nursing and Midwifery Research 2010;15(Suppl 1):395‐400. [PMC free article] [PubMed] [Google Scholar]
Griffith 2008 {published data only}
- Griffith JM, Hasley JP, Liu H, Severn DG, Conner LH, Adler LE. Qigong stress reduction in hospital staff. Journal of Alternative and Complementary Medicine 2008;14(8):939‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Günüsen 2010 {published data only}
- Gunusen N, Ustun B. An RCT of coping and support groups to reduce burnout among nurses. International Nursing Review 2010;57(4):485‐92. [DOI] [PubMed] [Google Scholar]
Hansen 2006 {published data only}
- Hansen TM, Hansen B, Ringdal GI. Does aromatherapy massage reduce job‐related stress? Results from a randomised, controlled trial. International Journal of Aromatherapy 2006;16:89‐94. [Google Scholar]
Heaney 1995 {published data only}
- Heaney CA, Price RH, Rafferty J. Increasing coping resources at work: a field experiment to increase social support, improve work team functioning, and enhance employee mental health. Journal of Organizational Behavior 1995;16:335‐52. [Google Scholar]
Jensen 2006 {published data only}
- Jensen LD, Gonge H, Jors E, Ryom P, Foldspang A, Christensen MA, et al. Prevention of low back pain in female eldercare workers: randomized controlled work site trial. Spine 2006;31(16):1761‐9. [PUBMED: 16845347] [DOI] [PubMed] [Google Scholar]
Jones 2000a {published data only}
- Jones MC, Johnston DW. Evaluating the impact of a worksite stress management programme for distressed students: a randomised controlled trial. Psychology and Health 2000;15:689‐706. [Google Scholar]
Ketelaar 2013 {published data only}
- Ketelaar SM, Gärtner FR, Bolier L, Smeets O, Nieuwenhuijsen K, Sluiter JK. Mental Vitality @ Work‐‐a workers' health surveillance mental module for nurses and allied health care professionals: process evaluation of a randomized controlled tTrial. Journal of Occupational and Environmental Medicine 2013;55(5):563‐71. [DOI] [PubMed] [Google Scholar]
- Ketelaar SM, Nieuwenhuijsen K, Gärtner FR, Bolier L, Smeets O, Sluiter JK. Effect of an E‐mental health approach to workers' health surveillance versus control group on work functioning of hospital employees: a cluster‐RCT. PLoS ONE 2013; Vol. 8, issue 9. [DOI] [PMC free article] [PubMed]
Klatt 2012 {published data only}
- Klatt M, Steinberg B, Marks D, Duchemin A. Changes in physiological and psychological markers of stress in hospital personnel after a low‐dose mindfulness‐based worksite intervention. BMC Complementary and Alternative Medicine 2012;12(Suppl 1):O16. [Google Scholar]
Kurebayashi 2012 {published data only}
Kwok 2012 {published data only}
- Kwok WO. The effects of an intervention program (medi) on reducing occupational stress in emergency department nurses. Dissertation Abstracts International: Section B: The Sciences and Engineering 2012; Vol. 72, issue 7‐B:3963.
Lai 2011 {published data only}
- Lai HL, Li YM. The effect of music on biochemical markers and self‐perceived stress among first‐line nurses: a randomized controlled crossover trial. Journal of Advanced Nursing 2011;67(11):2414‐24. [DOI] [PubMed] [Google Scholar]
Le Blanc 2007 {published data only}
- Blanc PM, Hox JJ, Schaufeli WB, Taris TW, Peeters MC. Take care! The evaluation of a team‐based burnout intervention program for oncology care providers. Journal of Appled Psychology 2007;92(1):213‐27. [DOI] [PubMed] [Google Scholar]
Lee 1994 {published data only}
- Lee S, Crockett MS. Effect of assertiveness training on levels of stress and assertiveness experienced by nurses in Taiwan, Republic of China. Issues in Mental Health Nursing 1994;15(4):419‐32. [DOI] [PubMed] [Google Scholar]
Leiter 2011 {published data only}
- Leiter MP, Laschinger HK, Day A, Oore DG. The impact of civility interventions on employee social behavior, distress, and attitudes. The Journal of Applied Psychology 2011;96(6):1258‐74. [DOI] [PubMed] [Google Scholar]
Lemaire 2011 {published data only}
- Lemaire JB, Wallace JE, Lewin AM, Grood J, Schaefer JP. The effect of a biofeedback‐based stress management tool on physician stress: a randomized controlled clinical trial. Open Medicine 2011;5(4):e154‐65. [PMC free article] [PubMed] [Google Scholar]
Li 2011 {published data only}
- Li HC, Wang LS, Lin YH, Lee I. The effect of a peer‐mentoring strategy on student nurse stress reduction in clinical practice. International Nursing Review 2011;58(2):203‐10. [DOI] [PubMed] [Google Scholar]
Lökk 2000 {published data only}
- Lökk J, Arnetz B. Impact of management change and an intervention program on health care personnel. Psychotherapy and Psychosomatics 2000;69(2):79‐85. [DOI] [PubMed] [Google Scholar]
- Lökk J, Arnetz B. Psychophysiological concomitants of organizational change in health care personnel: effects of a controlled intervention study. Psychotherapy and Psychosomatics 1997;66(2):74‐7. [DOI] [PubMed] [Google Scholar]
Lucas 2012 {published data only}
- Lucas B, Trick W, Evans A, Weinstein R, Varkey A, Smith J, et al. Emotional exhaustion, life stress, and perceived control among medicine ward attending physicians: A randomized trial of 2‐versus 4‐week ward rotations. Journal of Hospital Medicine 2011;6(4):S43‐4. [Google Scholar]
- Lucas BP, Trick WE, Evans AT, Mba B, Smith J, Das K, et al. Effects of 2‐ vs 4‐week attending physician inpatient rotations on unplanned patient revisits, evaluations by trainees, and attending physician burnout: a randomized trial. JAMA 2012;308(21):2199‐207. [DOI] [PubMed] [Google Scholar]
Mackenzie 2006 {published data only}
- Mackenzie CS, Poulin PA, Seidman‐Carlson R. A brief mindfulness‐based stress reduction intervention for nurses and nurse aides. Applied Nursing Research 2006;19(2):105‐9. [DOI] [PubMed] [Google Scholar]
Martins 2011 {published data only}
- Martins AE, Davenport MC, Valle MD, Lalla S, Dominguez P, Ormando L, et al. Impact of a brief intervention on the burnout levels of pediatric residents. Jornal de Pediatria 2011;87(6):493‐8. [DOI] [PubMed] [Google Scholar]
McElligott 2003 {published data only}
- McElligott D, Holz MB, Carollo L, Somerville S, Baggett M, Kuzniewski S, et al. A pilot feasibility study of the effects of touch therapy on nurses. Journal of the New York State Nurses Association 2003;34(1):16‐24. [PubMed] [Google Scholar]
Melchior 1996 {published data only}
- Melchior ME, Philipsen H, Abu‐Saad HH, Halfens RJ, Berg AA, Gassman P. The effectiveness of primary nursing on burnout among psychiatric nurses in long‐stay settings. Journal of Advanced Nursing 1996;24(4):694‐702. [DOI] [PubMed] [Google Scholar]
Moody 2013 {published data only}
- Moody K, Kramer D, Santizo RO, Magro L, Wyshogrod D, Ambrosio J, et al. Helping the helpers: mindfulness training for burnout in pediatric oncology‐‐a pilot program. Journal of Pediatric Oncology Nursing 2013;30(5):275‐84. [DOI] [PubMed] [Google Scholar]
Moyle 2013 {published data only}
- Moyle W, Cooke M, O'Dwyer ST, Murfield J, Johnston A, Sung B. The effect of foot massage on long‐term care staff working with older people with dementia: a pilot, parallel group, randomized controlled trial. BMC Nursing 2013;12:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Norvell 1987 {published data only}
- Norvell N, Belles D, Brody S, Freund A. Worksite stress management for medical care personnel: results from a pilot program. Journal for Specialists in Group Work 1987;57:118‐26. [Google Scholar]
Oman 2006 {published data only}
- Oman D, Hedberg J, Thoresen CE. Passage meditation reduces perceived stress in health professionals: A randomized, controlled trial. Journal of Consulting and Clinical Psychology 2006;74(4):714‐9. [DOI] [PubMed] [Google Scholar]
Palumbo 2012 {published data only}
- Palumbo MV, Wu G, Shaner‐McRae H, Rambur B, McIntosh B. Tai Chi for older nurses: A workplace wellness pilot study. Applied Nursing Research 2012;25(1):54‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peterson 2008 {published data only}
- Peterson U, Bergstrom G, Samuelsson M, Asberg M, Nygren A. Reflecting peer‐support groups in the prevention of stress and burnout: randomized controlled trial. Journal of Advanced Nursing 2008;63(5):506‐16. [DOI] [PubMed] [Google Scholar]
Proctor 1998 {published data only}
- Proctor R, Stratton‐Powell H, Tarrier N, Burns A. The impact of training and support on stress among care staff in nursing and residential homes for the elderly. Journal of Mental Health 1998;7(1):59‐71. [Google Scholar]
Razavi 1993 {published data only (unpublished sought but not used)}
- Razavi D, Delvaux N, Marchal S, Bredart A, Farvacques C, Paesmans M. The effects of a 24‐h psychological training program on attitudes, communication skills and occupational stress in oncology: a randomised study. European Journal of Cancer 1993;29A(13):1858‐63. [DOI] [PubMed] [Google Scholar]
Redhead 2011 {published data only}
- Redhead K, Bradshaw T, Braynion P, Doyle M. An evaluation of the outcomes of psychosocial intervention training for qualified and unqualified nursing staff working in a low‐secure mental health unit. Journal of Psychiatric and Mental Health Nursing 2011;18(1):59‐66. [DOI] [PubMed] [Google Scholar]
Reynolds 1993 {published data only}
- Reynolds S, Taylor E, Shapiro D. Session impact and outcome in stress management‐training. Journal of Community & Applied Social Psychology 1993;3(4):325‐37. [Google Scholar]
Romig 2012 {published data only}
- Romig MC, Latif A, Gill RS, Pronovost PJ, Sapirstein A. Perceived benefit of a telemedicine consultative service in a highly staffed intensive care unit. Journal of Critical Care 2012;27(4):426.e9‐16. [DOI] [PubMed] [Google Scholar]
Rowe 2006 {published data only}
- Rowe MM. Four‐year longitudinal study of behavioral changes in coping with stress. American Journal of Health Behavior 2006;30(6):602‐12. [DOI] [PubMed] [Google Scholar]
- Rowe MM. Teaching health‐care providers coping: results of a two‐year study. Journal of Behavioral Medicine 1999;22(5):511‐27. [DOI] [PubMed] [Google Scholar]
Saganha 2012 {published data only}
- Saganha JP, Doenitz C, Greten T, Efferth T, Greten HJ. Qigong therapy for physiotherapists suffering from burnout: A preliminary study. Journal of Chinese Integrative Medicine 2012;10(11):1233‐9. [DOI] [PubMed] [Google Scholar]
Salles 2013 {published data only}
- Salles A, Nandagopal K, Walton G. Belonging: A simple, brief intervention decreases burnout. Journal of the American College of Surgeons 2013;217(3):S116. [Google Scholar]
Schrijnemaekers 2003 {published data only}
- Schrijnemaekers VJ, Rossum E, Candel MJ, Frederiks CM, Derix MM, Sielhorst H, et al. Effects of emotion‐oriented care on work‐related outcomes of professional caregivers in homes for elderly persons. Journals of Gerontology Series B‐Psychological Sciences & Social Sciences 2003;58(1):S50‐7. [DOI] [PubMed] [Google Scholar]
Shapiro 2005 {published data only}
- Shapiro SL, Astin JA, Bishop SR, Cordova M. Mindfulness‐based stress reduction for health care professionals: results from a randomized trial. International Journal of Stress Management 2005;12(2):164‐76. [Google Scholar]
Sood 2011 {published data only}
- Sood A, Prasad K, Schroeder D, Varkey P. Stress management and resilience training among department of medicine faculty: A pilot randomized clinical trial. Journal of General Internal Medicine 2011;26(8):858‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stanton 1988 {published data only}
- Stanton HE. Relaxation, deepening, and ego‐enhancement: a stress reduction "package". Australian Psychologist 1988;23:315‐22. [Google Scholar]
Tsai 1993 {published data only}
- Tsai SL, Crockett MS. Effects of relaxation training, combining imagery, and meditation on the stress level of Chinese nurses working in modern hospitals in Taiwan. Issues in Mental Health Nursing 1993;14(1):51‐66. [DOI] [PubMed] [Google Scholar]
Uchiyama 2013 {published data only}
- Uchiyama A, Odagiri Y, Ohya Y, Takamiya T, Inoue S, Shimomitsu T. Effect on mental health of a participatory intervention to improve psychosocial work environment: a cluster randomized controlled trial among nurses. Journal of Occupational Health 2013;55(3):173‐83. [DOI] [PubMed] [Google Scholar]
Von Baeyer 1983 {published data only}
- Baeyer C, Krause L. Effectiveness of stress management training for nurses working in a burn treatment unit. International Journal of Psychiatry in Medicine 1983;13(2):113‐26. [DOI] [PubMed] [Google Scholar]
West 1984 {published data only}
- West DJ Jr, Horan JJ, Games PA. Component analysis of occupational stress inoculation applied to registered nurses in an acute care hospital setting. Journal of Counseling Psychology 1984;31(2):209‐18. [Google Scholar]
Yamagishi 2008 {published data only}
- Yamagishi M, Kobayashi T, Nakamura Y. Effects of web‐based career identity training for stress management among Japanese nurses: a randomized control trial. Journal of Occupational Health 2008;50(2):191‐3. [DOI] [PubMed] [Google Scholar]
Yazdani 2010 {published data only}
- Yazdani M, Rezaei S, Pahlavanzadeh S. The effectiveness of stress management training program on depression, anxiety and stress of the nursing students. Iranian Journal of Nursing and Midwifery Research 2010;15(4):208‐15. [PMC free article] [PubMed] [Google Scholar]
Yung 2004 {published data only}
- Yung PM, Fung MY, Chan TM, Lau BW. Relaxation training methods for nurse managers in Hong Kong: a controlled study. International Journal of Mental Health Nursing 2004;13(4):255‐61. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Andersen 2010 {published data only}
- Andersen I, Borritz M, Christensen KB, Diderichsen F. Changing job‐related burnout after intervention‐‐a quasi‐experimental study in six human service organizations. Journal of Occupational and Environmental Medicine 2010;52(3):318‐23. [DOI] [PubMed] [Google Scholar]
Baldelli 2004 {published data only}
- Baldelli MV, Fabbo A, Costopulos C, Carbone G, Gatti R, Zucchl P. Is it possible to reduce job burnout of the health care staff working with demented patients?. Archives of Gerontology and Geriatrics. Supplement 2004;Suppl(9):51‐6. [DOI] [PubMed] [Google Scholar]
Bay 2010 {published data only}
- Bay PS, Ivy SS, Terry CL. The effect of spiritual retreat on nurses' spirituality: a randomized controlled study. Holistic Nursing Practice 2010;24(3):125‐33. [DOI] [PubMed] [Google Scholar]
Beddoe 2004 {published data only}
- Beddoe AE, Murphy SO. Does mindfulness decrease stress and foster empathy among nursing students?. The Journal of Nursing Education 2004;43(7):305‐12. [DOI] [PubMed] [Google Scholar]
Bormann 2006 {published data only}
- Bormann JE, Oman D, Kemppainen JK, Becker S, Gershwin M, Kelly A. Mantram repetition for stress management in veterans and employees: a critical incident study. Journal of Advanced Nursing 2006;53(5):502‐12. [DOI] [PubMed] [Google Scholar]
Bost 2006 {published data only}
- Bost N. The effectiveness of a 15 minute weekly massage in reducing physical and psychological stress in nurses. Australian Journal of Advanced Nursing 2006;23(4):28‐33. [PubMed] [Google Scholar]
Bourbonnais 2006a {published data only}
- Bourbonnais R, Brisson C, Vinet A, Vézina M, Abdous B, Gaudet M. Effectiveness of a participative intervention on psychosocial work factors to prevent mental health problems in a hospital setting. Occupational and Environmental Medicine 2006;63(5):335‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bourbonnais 2006b {published data only}
- Bourbonnais R, Brisson C, Vinet A, Vézina M, Lower A. Development and implementation of a participative intervention to improve the psychosocial work environment and mental health in an acute care hospital. Occupational and Environmental Medicine 2006;63(5):326‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brinkborg 2011 {published data only}
- Brinkborg H, Michanek J, Hesser H, Berglund G. Acceptance and commitment therapy for the treatment of stress among social workers: A randomized controlled trial. Behaviour Research and Therapy 2011;49(6‐7):389‐98. [DOI] [PubMed] [Google Scholar]
Bruneau 2004 {published data only}
- Bruneau BM, Ellison GT. Palliative care stress in a UK community hospital: evaluation of a stress‐reduction programme. International Journal of Palliative Nursing 2004;10(6):296‐304. [DOI] [PubMed] [Google Scholar]
Cámara Conde 2009 {published data only}
- Cámara Conde N, Carretero Román J, Sánchez Alfonso J, Reina Alonso CN. Effectiveness of a nurse cognitive behavioral intervention to reduce stress in health professionals in emergency extra hospital devices of SUMMA 112 [Spanish]. Nure Investigación 2010; Vol. 7, issue 45:1‐29.
Cohen 2005 {published data only}
- Cohen M, Gagin R. Can skill‐development training alleviate burnout in hospital social workers?. Social Work in Health Care 2005;40(4):83‐97. [DOI] [PubMed] [Google Scholar]
Cooke 2007 {published data only}
- Cooke M, Holzhauser K, Jones M, Davis C, Finucane J. The effect of aromatherapy massage with music on the stress and anxiety levels of emergency nurses: comparison between summer and winter. Journal of Clinical Nursing 2007;16(9):1695‐703. [DOI] [PubMed] [Google Scholar]
Cuneo 2011 {published data only}
- Cuneo CL, Curtis Cooper M‐R, Drew CS, Naoum‐Heffernan C, Sherman T, Walz K, et al. The effect of Reiki on work‐related stress of the registered nurse. Journal of Holistic Nursing 2011;29(1):33‐43. [DOI] [PubMed] [Google Scholar]
Cutshall 2011 {published data only}
- Cutshall SM, Wentworth LJ, Wahner‐Roedler DL, Vincent A, Schmidt JE, Loehrer LL, et al. Evaluation of a biofeedback‐assisted meditation program as a stress management tool for hospital nurses: a pilot study. Explore‐the Journal of Science and Healing 2011;7(2):110‐2. [DOI] [PubMed] [Google Scholar]
Davis 2005 {published data only}
- Davis C, Cooke M, Holzhauser K, Jones M, Finucane J. The effect of aromatherapy massage with music on the stress and anxiety levels of emergency nurses. Australasian Emergency Nursing Journal. 2005;8(1‐2):43‐50. [DOI] [PubMed] [Google Scholar]
Diaz‐Rodriguez 2011a {published data only}
- Diaz‐Rodriguez L, Arroyo‐Morales M, Cantarero‐Villanueva I, Fernandez‐Lao C, Polley M, Fernandez‐de‐las‐Penas C. The application of reiki in nurses diagnosed with burnout syndrome has beneficial effects on concentration of salivary IgA and blood pressure. Revista Latino‐Americana de Enfermagem 2011;19(5):1132‐8. [DOI] [PubMed] [Google Scholar]
Diaz‐Rodriguez 2011b {published data only}
- Diaz‐Rodriguez L, Arroyo‐Morales M, Fernandez‐de‐las‐Penas C, Garcia‐Lafuente F, Garcia‐Royo C, Tomas‐Rojas I. Immediate effects of reiki on heart rate variability, cortisol levels, and body temperature in health care professionals with burnout. Biological Research for Nursing 2011;13(4):376‐82. [DOI] [PubMed] [Google Scholar]
Drain 1991 {published data only}
- Drain CB, Dirks KR, Jenkins OC, Campbell JK, Finstuen K, Johnson GR. Comparison of two instructional methods on the levels of physiologic and psychologic stress as measured by blood cortisol and the State‐Trait Anxiety Inventory. Nurse Anesthesia 1991;2(4):172‐83. [PubMed] [Google Scholar]
Dunn 2007 {published data only}
- Dunn PM, Arnetz BB, Christensen JF, Homer L. Meeting the imperative to improve physician well‐being: assessment of an innovative program. Journal of General Internal Medicine 2007;22(11):1544‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Edmonds 2012 {published data only}
- Edmonds C, Lockwood GM, Bezjak A, Nyhof‐Young J. Alleviating emotional exhaustion in oncology nurses: an evaluation of Wellspring's "Care for the Professional Caregiver Program". Journal of Cancer Education 2012;27(1):27‐36. [DOI] [PubMed] [Google Scholar]
Elo 2000 {published data only}
- Elo A‐L, Lehtomäki K, Nuutinen I, Hulkkonen A. Työterveyshenkilöstön stressin ja työuupumuksen ehkäisy : evaluoitu interventio. Työ Ja Ihminen 2000;14(2):395‐407. [Google Scholar]
Freedy 1994 {published data only}
- Freedy JR, Hobfoll SE. Stress inoculation for reduction of burnout: a conservation of resources approach. Anxiety, Stress, and Coping 1994;6:311‐25. [Google Scholar]
Galantino 2005 {published data only}
- Galantino ML, Baime M, Maguire M, Szapary PO, Farrar JT. Short Communication: Association of psychological and physiological measures of stress in health‐care professionals during an 8‐week mindfulness meditation program: mindfulness in practice. Stress and Health 2005;21(4):255‐61. [Google Scholar]
Gorter 2001 {published data only}
- Gorter RC, Eijkman MAJ, Hoogstraten J. A career counseling program for dentists: Effects on burnout. Patient Education and Counseling 2001;43(1):23‐30. [DOI] [PubMed] [Google Scholar]
Holt 2006 {published data only}
- Holt J, Mar C. Reducing occupational psychological distress: a randomized controlled trial of a mailed intervention. Health Education Research. 2006;21(4):501‐7. [DOI] [PubMed] [Google Scholar]
Isaksson Rø 2008 {published data only}
- Isaksson Rø KE, Gude T, Tyssen R, Aasland OG. Counselling for burnout in Norwegian doctors: One year cohort study. BMJ 2008;337(7679):a2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Isaksson Rø 2010 {published data only}
- Isaksson Rø KE, Gude T, Tyssen R, Aasland OG. A self‐referral preventive intervention for burnout among Norwegian nurses: One‐year follow‐up study. Patient Education and Counseling 2010;78(2):191‐7. [DOI] [PubMed] [Google Scholar]
Italia 2008 {published data only}
- Italia S, Favara‐Scacco C, Cataldo A, Russo G. Evaluation and art therapy treatment of the burnout syndrome in oncology units. Psycho‐Oncology 2008;17(7):676‐80. [DOI] [PubMed] [Google Scholar]
Johansson 1991 {published data only}
- Johansson N. Effectiveness of a stress management program in reducing anxiety and depression in nursing students. Journal of American College Health 1991;40(3):125‐9. [DOI] [PubMed] [Google Scholar]
Ju 2006 {published data only}
- Ju ZM, Shi K, Wan Q. Effect of organizational intervention on job burnout of the Plateau nurses in Tibet. [Chinese]. Chinese Journal of Clinical Psychology 2006;14(6):654. [Google Scholar]
Kendall 2005 {published data only}
- Kendall J, Waddington C, Kendall C. The daily moment: a stress reduction program for cancer center staff. Journal of Oncology Management 2005;14(3):68‐71. [PubMed] [Google Scholar]
Keyes 1988 {published data only}
- Keyes JB, Dean SF. Stress inoculation training for direct contact staff working with mentally retarded persons. Behavioral Residential Treatment 1988;3:315‐23. [Google Scholar]
Koivu 2012 {published data only}
- Koivu A, Saarinen PI, Hyrkas K. Does clinical supervision promote medical‐surgical nurses' well‐being at work? A quasi‐experimental 4‐year follow‐up study. Journal of Nursing Management 2012;20(3):401‐13. [DOI] [PubMed] [Google Scholar]
Kushnir 1994 {published data only}
- Kushnir T, Malkinson R, Ribak J. Teaching stress management skills to occupational and environmental health physicians and practitioners. A graduate‐level practicum. Journal of Occupational Medicine 1994;36(12):1335‐40. [DOI] [PubMed] [Google Scholar]
Kushnir 1998 {published data only}
- Kushnir T, Malkinson R, Ribak J. Rational thinking and stress management in health workers: a psychoeducational program. International Journal of Stress Management 1998;5(3):169‐78. [Google Scholar]
Lai 2012 {published data only}
- Lai HL, Liao KW, Huang C Y, Chen PW, Peng TC. Effects of music on immunity and physiological responses in healthcare workers: a randomized controlled trial. Stress Health 2013;29(2):91‐8. [DOI] [PubMed] [Google Scholar]
Lewis 1990 {published data only}
- Lewis DJ, McLin PA. Stress management: a program designed to facilitate coping. Journal of Continuing Education in Nursing 1990;21(5):212‐5. [DOI] [PubMed] [Google Scholar]
McCue 1991 {published data only}
- McCue JD, Sachs CL. A stress management workshop improves resident's coping skills. Archives of Internal Medicine 1991;151(11):2273‐7. [PubMed] [Google Scholar]
Michie 1992 {published data only}
- Michie S. Evaluation of a staff stress management service. Health Manpower Management 1992;18(1):15‐7. [DOI] [PubMed] [Google Scholar]
Michie 1994 {published data only}
- Michie S, Sandhu S. Stress management for clinical medical students. Medical Education 1994;28(6):528‐33. [DOI] [PubMed] [Google Scholar]
Moeini 2011 {published data only}
- Moeini B, Hazavehei SMM, Hosseini Z, Aghamolaei T, Moghimbeigi A. The impact of cognitive‐behavioral stress management training program on job stress in Hospital nurses: Applying PRECEDE model. Journal of Research in Health Sciences 2011;11(2):114‐20. [PubMed] [Google Scholar]
Murphy 1983 {published data only}
- Murphy LR. A comparison of relaxation methods for reducing stress in nursing personnel. Human Factors 1983;25(4):431‐40. [DOI] [PubMed] [Google Scholar]
Newsome 2010 {published data only}
- Newsome S. Effects of a mindfulness course on helping professionals in training: Examining levels of perceived stress, mindfulness, and self‐compassion. Dissertation Abstracts International Section A: Humanities and Social Sciences 2010;71(1‐A):97. [Google Scholar]
Newton 2006 {published data only}
- Newton JT, Allen CD, Coates J, Turner A, Prior J. How to reduce the stress of general dental practice: The need for research into the effectiveness of multifaceted interventions. British Dental Journal 2006;200(8):437‐40. [DOI] [PubMed] [Google Scholar]
Nhiwatiwa 2003 {published data only}
- Nhiwatiwa FG. The effects of single session education in reducing symptoms of distress following patient assault in nurses working in medium secure settings. Journal of Psychiatric & Mental Health Nursing 2003;10(5):561‐8. [DOI] [PubMed] [Google Scholar]
Nooryan 2011 {published data only}
- Nooryan K, Gasparyan K, Sharif F, Zoladl M. The effect of teaching emotional intelligence (EI) items on job related stress in physicians and nurses working in ICU wards in hospitals, Yerevan, Armenia. International Journal of Collaborative Research on Internal Medicine and Public Health 2011;3(10):704‐13. [Google Scholar]
Nooryan 2012 {published data only}
- Nooryan K, Gasparyan K, Sharif F, Zoladl M. Controlling anxiety in physicians and nurses working in intensive care units using emotional intelligence items as an anxiety management tool in Iran. International Journal of General Medicine 2012;5:5‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Orly 2011 {published data only}
- Orly S, Rivka B, Rivka E, Dorit SE. Are cognitive‐behavioral interventions effective in reducing occupational stress among nurses?. Applied Nursing Research 2012;25(3):152‐7. [DOI] [PubMed] [Google Scholar]
Ortega Ruiz 2008 {published data only}
- Ortega Ruiz C, Lopez Rios F, Gomez Martin S. Psychological intervention for professional burnout in the Palliative Care Unit at Gregorio Maranon University Hospital. Medicina Paliativa 2008;15(2):93‐7. [Google Scholar]
Panda 2010 {published data only}
- Panda M, Cunningham CJL. Addressing and preventing stress, fatigue and burnout in health care providers. Journal of General Internal Medicine 2010;25:S437‐8. [Google Scholar]
Pemberton 2008 {published data only}
- Pemberton E, Turpin PG. The effect of essential oils on work‐related stress in intensive care unit nurses. Holistic Nursing Practice 2008;22(2):97‐102. [DOI] [PubMed] [Google Scholar]
Petterson 1998 {published data only}
- Petterson IL, Arnetz BB. Psychosocial stressors and well‐being in health care workers. The impact of an intervention program. Social Science and Medicine 1998;47(11):1763‐72. [DOI] [PubMed] [Google Scholar]
Petterson 2006 {published data only}
- Petterson IL, Donnersvard HA, Lagerstrom M, Toomingas A. Evaluation of an intervention programme based on empowerment for eldercare nursing staff. Work and Stress 2006;20(4):353‐69. [Google Scholar]
Pipe 2009 {published data only}
- Pipe TB, Bortz JJ, Dueck A, Pendergast D, Buchda V, Summers J. Nurse leader mindfulness meditation program for stress management: a randomized controlled trial. Journal of Nursing Administration 2009;39(3):130‐7. [DOI] [PubMed] [Google Scholar]
Poulin 2008 {published data only}
- Poulin PA, Mackenzie CS, Soloway G, Karayolas E. Mindfulness training as an evidenced‐based approach to reducing stress and promoting well‐being among human services professionals. International Journal of Health Promotion and Education 2008;46(2):72‐80. [Google Scholar]
Prasad 2011 {published data only}
- Prasad K, Wahner‐Roedler DL, Cha SS, Sood A. Effect of a single‐session meditation training to reduce stress and improve quality of life among health care professionals: a "dose‐ranging" feasibility study. Alternative Therapies in Health and Medicine 2011;17(3):46‐9. [PubMed] [Google Scholar]
Ridge 2011 {published data only}
- Ridge M, Wells J, Denny M, Cunningham J, Chalder T. Developing a web‐based stress management intervention for occupational support workers. Journal of Mental Health 2011;20(2):185‐97. [DOI] [PubMed] [Google Scholar]
Russler 1991 {published data only}
- Russler MF. Multidimensional stress management in nursing education. Journal of Nursing Education 1991;30(8):341‐6. [DOI] [PubMed] [Google Scholar]
Saadat 2012 {published data only}
- Saadat H, Snow DL, Ottenheimer S, Dai F, Kain ZN. Wellness program for anesthesiology residents: a randomized, controlled trial. Acta Anaesthesiologica Scandinavica 2012;56(9):1130‐8. [DOI] [PubMed] [Google Scholar]
Salyers 2011 {published data only}
- Salyers MP, Hudson C, Morse G, Rollins AL, Monroe‐DeVita M, Wilson C, et al. BREATHE: a pilot study of a one‐day retreat to reduce burnout among mental health professionals. Psychiatric Services 2011;62(2):214‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sarid 2010 {published data only}
- Sarid O, Berger R, Segal‐Engelchin D. The impact of cognitive behavioral interventions on SOC, perceived stress and mood states of nurses. Procedia‐Social and Behavioral Sciences 2010;2(2):928‐32. [Google Scholar]
Schaufeli 1995 {published data only}
- Schaufeli WB. The evaluation of a burnout workshop for community nurses. Journal of Health and Human Services Administration 1995;18(1):11‐30. [PubMed] [Google Scholar]
Shanafelt 2014 {published data only}
- Shanafelt TD, Kaups KL, Nelson H, Satele DV, Sloan JA, Oreskovich MR, et al. An interactive individualized intervention to promote behavioral change to increase personal well‐being in US surgeons. Annals of Surgery 2014;259(1):82‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sharif 2004 {published data only}
- Sharif F, Armitage P. The effect of psychological and educational counselling in reducing anxiety in nursing students. Journal of Psychiatric and Mental Health Nursing 2004;11(4):386‐92. [DOI] [PubMed] [Google Scholar]
Sharif 2013 {published data only}
- Sharif F, Rezaie S, Keshavarzi S, Mansoori P, Ghadakpoor S. Teaching emotional intelligence to intensive care unit nurses and their general health: a randomized clinical trial. International Journal of Occupational and Environmental Medicine 2013;4(3):141‐8. [PubMed] [Google Scholar]
Tang 2010 {published data only}
- Tang R, Tegeler C, Larrimore D, Cowgill S, Kemper KJ. Improving the well‐being of nursing leaders through healing touch training. Journal of Alternative and Complementary Medicine 2010;16(8):837‐41. [DOI] [PubMed] [Google Scholar]
Taylor 2001 {published data only}
- Taylor B, Lo R. The effects of Healing Touch on the coping ability, self esteem and general health of undergraduate nursing students. Complementary Therapies in Nursing & Midwifery 2001;7(1):34‐42. [DOI] [PubMed] [Google Scholar]
Te Brake 2001 {published data only}
- Brake HT, Gorter R, Hoogstraten J, Eijkman M. Burnout intervention among Dutch dentists: long‐term effects. European Journal of Oral Sciences 2001;109(6):380‐7. [DOI] [PubMed] [Google Scholar]
Van Dierendonck 1998 {published data only}
- Dierendonck D, Schaufeli W, Buunk BP. The evaluation of an individual burnout intervention program: the role of inequity and social support. Journal of Applied Psychology 1998;83(3):392‐407. [Google Scholar]
Villani 2011 {published data only}
- Villani D, Grassi A, Cognetta C, Toniolo D, Cipresso P, Riva G. Self‐help stress management training through mobile phones: An experience with oncology nurses. Psychological Services 2013;10(3):215‐22. [DOI] [PubMed] [Google Scholar]
Villani 2012 {published data only}
- Villani D, Grassi A, Cognetta C, Cipresso P, Toniolo D, Riva G. The effects of a mobile stress management protocol on nurses working with cancer patients: a preliminary controlled study. Studies in Health Technology and Informatics 2012;173:524‐8. [PubMed] [Google Scholar]
Wassel 1993 {published data only}
- Wassel ML. A stress management incentive program for nursing staff during Operation Desert Storm. American Association of Occupational Health Nurses Journal 1993;41(8):393‐5. [PubMed] [Google Scholar]
Wetzel 2011 {published data only}
- Wetzel CM, George A, Hanna GB, Athanasiou T, Black SA, Kneebone RL, et al. Stress management training for surgeons‐a randomized, controlled, intervention study. Annals of Surgery 2011;253(3):488‐94. [DOI] [PubMed] [Google Scholar]
Winefield 1998 {published data only}
- Winefield H, Farmer E, Denson L. Work stress management for women general practitioners: An evaluation. Psychology, Health and Medicine 1998;3(2):163‐70. [Google Scholar]
Yamagishi 2007 {published data only}
- Yamagishi M, Kobayashi T, Kobayashi T, Nagami M, Shimazu A, Kageyama T. Effect of web‐based assertion training for stress management of Japanese nurses. Journal of Nursing Management 2007;15(6):603‐7. [DOI] [PubMed] [Google Scholar]
Yong 2011 {published data only}
- Yong J, Kim J, Park J, Seo I, Swinton J. Effects of a spirituality training program on the spiritual and psychosocial well‐being of hospital middle manager nurses in Korea. Journal of Continuing Education in Nursing 2011;42(6):280‐8. [DOI] [PubMed] [Google Scholar]
Young 2001 {published data only}
- Young LE, Bruce A, Turner L, Linden W. Evaluation of mindfulness‐based stress reduction intervention. Canadian Nurse 2001;97(6):23‐6. [PubMed] [Google Scholar]
Zimber 2001 {published data only}
- Zimber A, Rudolf A, Teufel S. A training program to reduce distress among geriatric caregivers [Arbeitsbelastungen in der Altenpflege reduzieren: Ein Trainingsprogramm für Mitarbeiter und Leitugskräfte]. Zeitschrift fur Gerontologie und Geriatrie 2001;34(5):401‐7. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Khaghanizadeh 2008 {published data only}
- Khaghanizadeh M, Vafadar Z, Salari M, Ebadi A. Effects of suggestions' system on decreasing job burn out among the staff. Journal of Psychology 2008;12(46):213‐26. [Google Scholar]
Ruehl 2013 {published data only}
- Ruehl BD. The psychological and physical heatlh effects of written emotional expression in pediatric hematology/oncology, intensive care, and neonatal intensive care nursing staff. Alliant International University 2013:Psy.D.: 319 p.
References to ongoing studies
Gomez‐Gascon 2013 {published data only}
- Gomez‐Gascon T, Martin‐Fernandez J, Galvez‐Herrer M, Tapias‐Merino E, Beamud‐Lagos M, Mingote‐Adan JC. Effectiveness of an intervention for prevention and treatment of burnout in primary health care professionals. BMC Family Practice 2013;14(1):173. [DOI] [PMC free article] [PubMed] [Google Scholar]
Niks 2013 {published data only}
- Niks IMW, Jonge J, Gevers JMP, Houtman ILD. Design of the DISCovery project: tailored work‐oriented interventions to improve employee health, well‐being, and performance‐related outcomes in hospital care. BMC Health Services Research 2013; Vol. 13. [DOI] [PMC free article] [PubMed]
Spoor 2010 {published data only}
- Spoor E, Jonge J, Hamers JP. Design of the DIRECT‐project: interventions to increase job resources and recovery opportunities to improve job‐related health, well‐being, and performance outcomes in nursing homes. BMC Public Health 2010;10:293. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Awa 2010
- Awa WL, Plaumann M, Walter U. Burnout prevention: a review of intervention programs. Patient Education and Counseling 2010;78(2):184‐90. [DOI] [PubMed] [Google Scholar]
Beck 1961
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry 1961;4:561‐71. [DOI] [PubMed] [Google Scholar]
Benoliel 1990
- Benoliel JQ, McCorkle R, Georgiadou F, Denton T, Spitzer A. Measurement of stress in clinical nursing. Cancer Nursing 1990;13(4):221‐28. [DOI] [PubMed] [Google Scholar]
Bhui 2012
- Bhui KS, Dinos S, Stansfeld SA, White PD. A synthesis of the evidence for managing stress at work: a review of the reviews reporting on anxiety, depression, and absenteeism. Journal of Environmental and Public Health 2012 Feb 14 [epub ahead of print];2012:515874. [DOI] [PMC free article] [PubMed] [Google Scholar]
Campbell 2001
- Campbell MK, Mollison J, Grimshaw JM. Cluster trials in implementation research: estimation of intra‐cluster correlation and sample size. Statistics in Medicine 2001;20(3):391‐9. [DOI] [PubMed] [Google Scholar]
Chiesa 2009
- Chiesa A, Serretti A. Mindfulness‐based stress reduction for stress management in healthy people: a review and meta‐analysis. Journal of Alternative and Complementary Medicine 2009;15(5):593‐600. [DOI] [PubMed] [Google Scholar]
Cohen 1983
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior 1983;24(4):385‐96. [PubMed] [Google Scholar]
Cooper 1988
- Cooper CL, Sloane SJ, Williams S. The Occupational Stress Indicator. Windsor, Berkshire: NFER‐Nelson, 1988. [Google Scholar]
Cooper 2001
- Cooper CL, Dewe P, O'Driscoll MP. Organizational Stress. London: SAGE, 2001. [Google Scholar]
Deckard 1994
- Deckard G, Meterko M, Field D. Physician burnout: an examination of personal, professional, and organizational relationships. Medical Care 1994;32(7):745‐54. [DOI] [PubMed] [Google Scholar]
DeFrank 1987
- DeFrank RS, Cooper CL. Worksite stress management interventions: their effectiveness and conceptualisation. Journal of Managerial Psychology 1987;2(1):4‐10. [Google Scholar]
Derogatis 1976
- Derogatis L, Rickels K, Rock A. The SCL‐90 and MMPI: A step in the validation of a new self‐report scale. British Journal of Psychiatry 1976;128:280‐9. [DOI] [PubMed] [Google Scholar]
Derogatis 1983
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychological Medicine 1983;13(3):595‐605. [PubMed] [Google Scholar]
EPOC 2013
- Cochrane Effective Practice and Organisation of Care Group. Interrupted time series (ITS) analyses. epoc.cochrane.org/sites/epoc.cochrane.org/files/uploads/21%20Interrupted%20time%20series%20analyses%202013%2008%2012.pdf (accessed 9 July 2014):1‐5.
Eurofound 2012
- Eurofound. Fifth European Working Conditions Survey. www.eurofound.europa.eu/publications/htmlfiles/ef1182.htm. Luxembourg, (accessed 7 July 2014):na.
Firth‐Cozens 1999
- Firth‐Cozens J, Payne R. Stress in Health Professionals. Chichester: Wiley, 1999. [Google Scholar]
Galbraith 2011
- Galbraith N, Brown K. Assessing intervention effectiveness for reducing stress in student nurses: quantitative systematic review. Journal of Advanced Nursing 2011;67(4):709‐21. [DOI] [PubMed] [Google Scholar]
Gilbody 2006
- Gilbody S, Cahill J, Barkham M, Richards D, Bee P, Glanville J. Can we improve the morale of staff working in psychiatric units? A systematic review. Journal of Mental Health 2006;15(1):7‐17. [Google Scholar]
Goldberg 1991
- Goldberg D, Williams P. A User's Guide to the General Health Questionnaire. London: NFER–Nelson, 1991. [Google Scholar]
Gray‐Toft 1981
- Gray‐Toft P, Anderson JG. The Nursing Stress Scale: Development of an instrument. Journal of Psychopathology and Behavioral Assessment 1981;3(1):11‐23. [Google Scholar]
Günthner 2010
- Günthner A, Batra A. Prevention of burnout by stress management (in German). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2012;55(2):183‐9. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. The Cochrane Collaboration.
HSE 2013
- Health and Safety Executive. Stress and Psychological Disorders in Great Britain 2013. www.hse.gov.uk/statistics/causdis/stress/stress.pdf (accessed 7 July 2014):na.
Jacobson 1996
- Jacobson BH, Aldana SG, Goetzel RZ, Vardell KD, Adams TB, Piedras RJ. The relationship between perceived stress and self‐reported illness‐related absenteeism. American Journal of Health Promotion 1996;11(1):54‐61. [DOI] [PubMed] [Google Scholar]
Jones 2000b
- Jones MC, Johnston DW. Reducing distress in first level and student nurses: a review of the applied stress management literature. Journal of Advanced Nursing 2000;32(1):66‐74. [DOI] [PubMed] [Google Scholar]
Karasek 1992
- Karasek R. Stress prevention through work reorganization: a summary of 19 international case studies. Conditions of Work Digest 1992;11:23‐42. [Google Scholar]
Karasek 1998
- Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. Journal of Occupational Health Psychology 1998;3(4):322‐55. [DOI] [PubMed] [Google Scholar]
Lamontagne 2007
- Lamontagne AD, Keegel T, Louie AM, Ostry A, Landsbergis PA. A systematic review of the job‐stress intervention evaluation literature, 1990‐2005. International Journal of Occupational and Environmental Health 2007;13(3):268‐80. [PUBMED: 17915541] [DOI] [PubMed] [Google Scholar]
Malgorzata 2010
- Małgorzata W, Merecz D, Drabek M. Stress prevention programs‐‐strategies, techniques, effectiveness. Part II. Organizational activities to prevent stress at work. Medycyna Pracy 2010;61(2):191‐204. [PubMed] [Google Scholar]
Maslach 1982
- Maslach C. Burnout: the Cost of Caring. New York, NY: Prentice‐Hall, 1982. [Google Scholar]
Maslach 1996
- Maslach C, Jackson SE, Leiter SP. Maslach Burnout Inventory Manual. 3rd Edition. Palo Alto, CA: Consulting Psychologists Press, 1996. [Google Scholar]
McNeely 2005
- McNeely E. The consequences of job stress for nurses' health: time for a check‐up. Nursing Outlook 2005;53(6):291‐9. [DOI] [PubMed] [Google Scholar]
Michie 2003
- Michie S, Williams S. Reducing work related psychological ill health and sickness absence: a systematic literature review. Occupational and Environmental Medicine 2003;60(1):3‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mimura 2003
- Mimura C, Griffiths P. The effectiveness of current approaches to workplace stress management in the nursing profession: an evidence based literature review. Occupational and Environmental Medicine 2003;60(1):10‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Murphy 1995
- Murphy S. Stress management in work settings: a critical review of the health effects. American Journal of Health Promotion 1995;11(2):112‐35. [DOI] [PubMed] [Google Scholar]
Paris 2010
- Paris M Jr, Hoge MA. Burnout in the mental health workforce: A review. Journal of Behavioral Health Services & Research 2010;37(4):519‐28. [DOI] [PubMed] [Google Scholar]
Payne 1987
- Payne RL, Firth‐Cozens J. Stress in Health Professionals. Chichester: Wiley, 1987. [Google Scholar]
Petrie 2006
- Petrie A, Sabin C. Medical Statistics at a Glance. Malden (MA), USA: Blackwell Publishing Ltd, 2006. [Google Scholar]
Pulido‐Martos 2012
- Pulido‐Martos M, Augusto‐Landa J, Lopez‐Zafra E. Sources of stress in nursing students: A systematic review of quantitative studies. International Nursing Review 2012;59(1):15‐25. [Google Scholar]
Raiger 2005
- Raiger J. Applying a cultural lens to the concept of burnout. Journal of Transcultural Nursing 2005;16(1):71‐6. [DOI] [PubMed] [Google Scholar]
Ramirez 1996
- Ramirez AJ, Graham J, Richards MA, Cull A, Gregory WM. Mental health of hospital consultants: the effects of stress and satisfaction at work. Lancet 1996;347(9003):724‐8. [DOI] [PubMed] [Google Scholar]
Richardson 2008
- Richardson KM, Rothstein HR. Effects of occupational stress management intervention programs: a meta‐analysis. Journal of Occupational Health Psychology 2008;13(1):69‐93. [DOI] [PubMed] [Google Scholar]
Rohland 2004
- Rohland BM, Kruse GR, Rohrer JE. Validation of a single‐item measure of burnout against the Maslach Burnout Inventory among physicians. Stress and Health 2004;20:75‐79. [Google Scholar]
Rowe 1999
- Rowe MM. Teaching health‐care providers coping: results of a two‐year study. Journal of Behavioral Medicine 1999;22(5):511‐27. [DOI] [PubMed] [Google Scholar]
Schaufeli 2003
- Schaufeli WB, Buunk BP. Burnout: An overview of 25 years of research and theorizing. In: Schabracq MJ, Winnubst JAM, Cooper CL editor(s). The Handbook of Work and Health Psychology. 2nd Edition. Chichester: Wiley, 2003:383‐424. [Google Scholar]
Siegrist 2004
- Siegrist J, Starke D, Chandola T, Godin I, Marmot M, Niedhammer I, et al. The measurement of effort‐reward imbalance at work: European comparisons. Social Science and Medicine 2004;58(8):1483‐99. [DOI] [PubMed] [Google Scholar]
Spielberger 1970
- Spielberger CD, Gorsuch RL, Lushene RE. Manual for the State‐Trait Anxiety Inventory (Self‐Evaluation Questionnaire). Palo Alto, CA: Mind Garden, 1970. [Google Scholar]
Van der Hek 1997
- Hek H, Plomp HN. Occupational stress management programmes: a practical overview of published effect studies. Occupational Medicine [London] 1997;47(3):133‐41. [DOI] [PubMed] [Google Scholar]
Van der Klink 2001
- Klink JJ, Blonk RW, Schene AH, Dijk FJ. The benefits of interventions for work‐related stress. American Journal of Public Health 2001;91(2):270‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
van Wyk 2010
- Wyk BE, Pillay‐Van Wyk V. Preventive staff‐support interventions for health workers. Cochrane Database of Systematic Reviews 2010, Issue 3. [DOI: 10.1002/14651858.CD003541] [DOI] [PubMed] [Google Scholar]
Weinberg 2000
- Weinberg A, Creed F. Stress and psychiatric disorder in healthcare professionals and hospital staff. Lancet 2000;355(9203):533‐7. [DOI] [PubMed] [Google Scholar]
Williamson 1994
- Williamson AM. Managing stress in the workplace .2. the scientific basis (knowledge‐base) for the guide. International Journal of Industrial Ergonomics 1994;14(1‐2):171‐96. [Google Scholar]
References to other published versions of this review
Marine 2006
Serra 2000
- Serra C. Occupational health programmes for psychological stress in health care professionals. Cochrane Database of Systematic Reviews 2001, Issue 1,. [DOI: 10.1002/14651858.CD002892] [DOI] [Google Scholar]


