Abstract
Objective:
Although mental health conditions are widely considered to be risk factors for suicide, there is limited data available on suicide mortality for specific mental health conditions within the general US population. This study aims to fill this gap.
Method:
This study used a case-control study design. Patients in the case group were those who died by suicide between 2000 and 2013 from eight health care systems in the Mental Health Research Network. Each patient who died by suicide was matched with 100 general population patients. A total of 2674 individuals who died by suicide and 267,400 matched patients were included.
Results:
Approximately 50% of patients in the case group had recorded mental health conditions in the year prior to death, compared to 13% for patients in the control group. Risk of suicide mortality was highest among individuals with schizophrenia spectrum disorder after adjusting for age and sociodemographic characteristics (adjusted odds ratio [AOR]=15.0) followed by bipolar disorders (AOR=13.2), depressive disorders (AOR=7.2), anxiety disorders (AOR=5.8), and ADHD (AOR=2.4). The risk of suicide death among those with a diagnosed bipolar disorder condition was higher in women than men.
Conclusions:
Nearly half of those who died by suicide had at least one diagnosed mental health condition in the year before death, and most mental health conditions were associated with an increased risk of suicide. Our findings suggest the importance of suicide screening and providing an approach to improve awareness of mental health conditions, as well as going beyond those with mental health conditions.
Keywords: Suicide, mental health, diagnosis, prevention, healthcare
INTRODUCTION
Suicide is a major public health issue in the United States. More than 40,000 Americans die by suicide each year. In the past two decades, suicide rates increased more than 20%. This increase included men and women across all ages (1–3).
Mental health conditions are widely considered to be risk factors for suicide. Most studies that have investigated this association have focused on suicidal ideation or suicide attempts as outcomes (4, 5); few studies have examined risk of suicide mortality as the main outcome (6–12). The research gap is particularly evident within the U.S. general population. In a U.S. veteran population, anxiety disorder, bipolar disorder, depression, and schizophrenia spectrum disorder were found to be associated with a two to three-fold increased risk of suicide death (8). In Sweden and Denmark, the suicide mortality rate was increased in patients with bipolar disorder (13, 14), while schizophrenia was found to be associated with an elevated risk of suicide mortality in a national clinical survey in England (15). In addition, Brown and colleagues found that mood disorder, major depressive disorder, and bipolar disorder were associated with a 3- to 10-fold increased risk of suicide mortality (16). However, most of these studies were either conducted in other countries or within the U.S. veteran population, and there is limited data from the general U.S. population relating individual mental health diagnoses to risk of suicide death.
This study aims to fill this gap by using healthcare data to study suicide mortality in the general U.S. population. The data used in this study allow a comprehensive look at the relationship between mental health diagnoses and suicide mortality. All diagnoses from all health care settings in a large and diverse population were recorded. We also assess whether risk of suicide death differs by sex, given that there are wide variations in rates of suicide death, mental health conditions, and healthcare utilization between men and women.
METHODS
Data Source
The Mental Health Research Network (MHRN), a consortium of 13 healthcare systems across the U.S., collectively provides healthcare services to more than 15 million demographically and geographically diverse individuals each year (see www.mhresearchnetwork.org for more details). All MHRN sites have organized their electronic medical record (EMR) and insurance claims data into locally-stored federated data systems called the Virtual Data Warehouse (VDW). Affiliated health plans provide a diverse range of health insurance for individuals, including commercial, private, Medicaid, and Medicare plans. The same data definitions and variables are included across sites to facilitate multi-site research. These data include comprehensive capture of encounters, procedures, diagnoses, providers, cancer/tumor, pharmacy, vital signs, laboratory values, demographics, and insurance enrollment across large multi-specialty health care delivery systems.
In this study, data were collected from the following 8 healthcare systems: Harvard Pilgrim Health Care (Massachusetts), HealthPartners (Minnesota), Henry Ford Health System (Michigan), and Kaiser Permanente systems in Colorado, Georgia, Hawaii, Oregon, and Washington. Suicide mortality data was identified from official state mortality records using International Classification of Diseases – 10th version, Clinical Modification (ICD-10 CM) codes from X60 to X84 and Y87.0. Healthcare utilization in the year before the index date was obtained from all healthcare settings including inpatient, outpatient specialty, emergency, and primary care. A detailed data description has been published previously (17). Institutional Review Boards at each health system approved the use of de-identified data for this research.
Study Sample & Study Design
This study used a case-control design. A total of 2,674 individuals who died by suicide between 2000 and 2013 and were health plan members at one of the eight participating health systems were considered as those in the case group. Patients in the case and control groups were continuously enrolled in the healthcare system’s health plan for at least 10 months during the year before the index date. Each patient who died by suicide was matched with 100 general population patients as a control; patients in the control group were randomly selected among health plan members enrolled in the same healthcare system, and during the same time period as patients in the case group. Thus, all patients in the case and control groups were matched by site and enrollment period. A total of 267,400 patients who did not die by suicide were included in the study as the control group. The date of death was considered to be the index date for individuals who died by suicide, and the same date was selected as the index date for matched patients in the control group. Patients in the control group survived within the year before the index date.
Measurements
Diagnostic codes were extracted from the VDW for the year prior to the index date for all study individuals. Five types of mental health conditions were defined by International Classification of Diseases – 9th version, Clinical Modification (ICD-9 CM) codes, including: Anxiety Disorders (ICD-9 CM codes: 300.0, 300.2, 300.3, 309.20, 309.21, 309.24, 309.81), Attention Deficit/Hyperactivity Disorder (ADHD) (ICD-9 CM code: 314), Bipolar Disorder (ICD-9 CM codes: 296.0, 296.1, 296.4, 296.5, 296.6, 296.7, 296.80, 296.81, 296.89), Depressive Disorders (ICD-9 CM codes: 296.2, 296.3, 296.82, 298.0, 300.4, 301.12, 309.0, 309.1, 309.28, 311), and Schizophrenia Spectrum Disorders (ICD-9 CM code: 295). These diagnoses were chosen because they represent the most prevalent mental health diagnoses among the general US population (8, 13–16); other mental health diagnoses are seldom diagnosed. The findings for substance use disorders were too comprehensive to include in this paper. Therefore, we wanted to dedicate a separate paper to those findings and allow the focus of this manuscript to be on the five conditions presented.
Insurance type was captured from the VDW with the classifications of commercial, Medicaid, Medicare, private pay, and other. Neighborhood income and education were calculated by using geocoded address and U.S. Census Bureau block data. Individuals were considered to be of low income if they resided in a census block where >20% of residents had an income below the U.S. poverty level. Individuals were considered to have a high education level if they resided in a census block where ≥25% of residents were college graduates.
Statistical Analysis
Conditional logistic regression was used to investigate the relationship between mental health conditions and suicide mortality. Each diagnosis was coded as a dichotomous variable (yes/no) to indicate the diagnosed condition in the year prior to index date. The sociodemographic-adjusted model was adjusted for age, insurance type, and sociodemographic characteristics. The fully-adjusted model was adjusted for sociodemographic characteristics and all diagnosed mental health conditions. In patients with multiple diagnoses, each diagnosed mental health condition was flagged in the model simultaneously to determine the contribution of each predicted factor while controlling for the others. All models were conditional on site and index year.
Among individuals who died by suicide, time was coded from the index date backward to the date of each diagnosed mental health condition in the reverse-survival analyses. For individuals with multiple diagnosed mental health conditions contributing to the time-to-event information to multiple Kaplan–Meier survival curves, the time between the diagnoses is competitive. The event used in this analysis was the last clinical visit which the relevant diagnosis was coded. Time was measured from the index date backward to the event for each recorded mental health condition. All individuals in this analysis had continuously enrolled in the healthcare system’s health plan for at least 10 months prior to the index date. Kaplan–Meier curves were used to capture the probability of the last clinical encounter where the relevant diagnosis was recorded before suicide death and are displayed backward with time.
The effect of mental health diagnoses on suicide mortality in the population was examined by calculating the population attributable fraction (PAF). The prevalence of each mental health condition was obtained from MHRN data.
All analyses were performed by using SAS 9.4 (SAS Institute, Inc., Cary, NC), and R-Studio 1.0.136 (RStudio, Inc.).
RESULTS
Individuals who died by suicide were more likely to be male (n=2,072, 77.5%) and to have had at least one diagnosed mental health condition in the year before suicide (Table 1). Overall, 51.3% (n=1,371) of individuals who died by suicide had at least one of the listed diagnosed mental health condition in the year before the index date as compared with 13% (n=34,049) of patients in the control group. Individuals who died by suicide had, on average, more healthcare visits for diagnosed mental health conditions prior to the index date when compared with patients in the control group (5.2 vs. 0.6 visits, respectively). Mean values of time intervals between last visit with diagnosed mental health condition and suicide death among those who died by suicide were also shown in the table 1. The shortest interval was found among those with a diagnosed schizophrenia spectrum disorder (45.4 days) and the longest was among those with ADHD (87.0 days).
TABLE 1.
Demographic characteristics and mental healthcare utilization among patients died by suicide during 2000–2013 and matched patients in the control group.
| Suicide Deaths (n=2,674) | Controls (n=267,400) | |||
|---|---|---|---|---|
| n | % | n | % | |
| Age (year) | ||||
| 0–17 | 104 | 3.89 | 59,264 | 22.16 |
| 18–39 | 641 | 23.97 | 69,187 | 25.87 |
| 40–64 | 1,349 | 50.45 | 104,804 | 39.19 |
| 65+ | 580 | 21.69 | 34,145 | 12.77 |
| Sex | ||||
| Female | 602 | 22.51 | 140,418 | 52.51 |
| Male | 2,072 | 77.49 | 126,980 | 47.49 |
| Insurance type | ||||
| Commercial | 1,855 | 69.66 | 214,650 | 80.68 |
| Medicaid | 49 | 1.84 | 6,990 | 2.63 |
| Medicare | 636 | 23.88 | 34,137 | 12.83 |
| Other | 6 | 0.23 | 257 | 0.1 |
| Private Payment | 117 | 4.39 | 10,019 | 3.77 |
| Neighborhood poverty levela | ||||
| Higher than low income | 2,105 | 89.84 | 211,613 | 90.25 |
| Low income | 238 | 10.16 | 22,852 | 9.75 |
| Neighborhood educationb | ||||
| <25% college graduate | 1,626 | 61.73 | 166,638 | 63.23 |
| ≥25% college graduate | 1,008 | 38.27 | 96,908 | 36.77 |
| Mental health conditionc | ||||
| Anxiety Disorder | 673 | 25.17 | 13,760 | 5.15 |
| ADHD | 67 | 2.51 | 4,282 | 1.6 |
| Bipolar Disorder | 213 | 7.97 | 1,717 | 0.64 |
| Depressive Disorders | 1,126 | 42.11 | 22,213 | 8.31 |
| Schizophrenia Spectrum | 61 | 2.28 | 329 | 0.12 |
| Any Mental Health Condition | 1,371 | 51.27 | 34,049 | 12.73 |
| Mean | SD | Mean | SD | |
| Number of visits with recorded conditionc,d | ||||
| Anxiety Disorder | 1.3 | 4.53 | 0.18 | 1.46 |
| ADHD | 0.1 | 0.94 | 0.06 | 0.76 |
| Bipolar Disorder | 0.68 | 3.74 | 0.04 | 0.8 |
| Depressive Disorders | 2.9 | 7.13 | 0.34 | 2.14 |
| Schizophrenia Spectrum | 0.22 | 2.47 | 0.01 | 0.66 |
| Any Mental Health Condition | 5.2 | 11.72 | 0.62 | 3.42 |
| Days between the last visit and suicide death | ||||
| Anxiety Disorder | 64.92 | 89.52 | - | - |
| ADHD | 87.03 | 112.57 | - | - |
| Bipolar Disorder | 53.53 | 74.29 | - | - |
| Depressive Disorders | 67.4 | 90.39 | - | - |
| Schizophrenia Spectrum | 45.44 | 71.51 | - | - |
| Any Mental Health Condition | 65.5 | 89.17 | - | - |
Abbreviations: ADHD, attention-deficit hyperactivity disorder
Proportion of individuals living in Census blocks where >20% have incomes below the U.S. poverty level
Education is defined as the proportion of individuals living in Census blocks where ≥25% are college graduates
Each individual might have more than one visit within the year before index date
Number of healthcare visits by types of mental health diagnoses within the year before index date
Overall, having mental health diagnoses in the preceding year was associated with a higher risk of death by suicide (Table 2). After adjusting for sociodemographic characteristics, individuals with diagnosed mental health conditions in the year prior to the index date were 6.8 times more likely to die by suicide (adjusted odds ratio [AOR] = 6.84, 95% confidence interval [CI] = 6.29–7.44). Diagnoses of schizophrenia spectrum disorder or bipolar disorder were associated with the highest relative odds of suicide mortality. Those with a diagnosed schizophrenia spectrum disorder in the year prior to index date were 15 times more likely to die by suicide (AOR=15, 95% CI = 11.04–20.38), followed by bipolar disorder (AOR=13.17, 95% CI = 11.19–15.51). Elevated risks were also observed for depressive disorders (AOR=7.20, 95% CI = 6.61–7.84), anxiety disorder (AOR=5.84, 95% CI = 5.29–6.44), and ADHD (AOR=2.37, 95% CI = 1.79–3.15). After adjusting for all listed mental health diagnoses, suicide risk remained highest among individuals with diagnoses of bipolar disorder (AOR=5.14), depressive disorders (AOR=4.98), and schizophrenia spectrum disorders (AOR=4.88). The estimated effect of ADHD on suicide mortality was no longer significant after adjusting for other mental health diagnoses.
TABLE 2.
Risk of suicide death among individuals with mental health conditions
| Univariate Modela | ||||||
|---|---|---|---|---|---|---|
| ALL | Male | Female | ||||
| (Reference: None) | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Anxiety Disorder | 6.39 | 5.84–7.00 | 8.04 | 7.21–8.97 | 7.79 | 6.56–9.25 |
| ADHD | 1.58 | 1.24–2.02 | 1.16 | 0.88–1.54 | 2.32 | 1.41–3.83 |
| Bipolar Disorder | 13.48 | 11.62–15.64 | 12.94 | 10.57–15.84 | 22.93 | 18.22–28.87 |
| Depressive Disorders | 8.29 | 7.66–8.97 | 11.06 | 10.08–12.14 | 11.09 | 9.4–13.08 |
| Schizophrenia Spectrum | 18.96 | 14.39–24.99 | 15.12 | 10.67–21.43 | 29.43 | 18.49–46.86 |
| Any Mental Health Condition* | 6.39 | 5.84–7.00 | 8.04 | 7.21–8.97 | 7.79 | 6.56–9.25 |
| Sociodemographic-Adjusted Modelb | ||||||
| ALL | Male | Female | ||||
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Anxiety Disorder | 5.84 | 5.29–6.44 | 7.55 | 6.71–8.50 | 7.15 | 5.93–8.62 |
| ADHD | 2.37 | 1.79–3.15 | 1.92 | 1.38–2.67 | 3.14 | 1.80–5.50 |
| Bipolar Disorder | 13.17 | 11.19–15.51 | 12.60 | 10.07–15.78 | 22.87 | 17.79–29.40 |
| Depressive Disorders | 7.20 | 6.61–7.84 | 9.50 | 8.59–10.52 | 10.09 | 8.43–12.08 |
| Schizophrenia Spectrum | 15.00 | 11.04–20.38 | 13.18 | 8.95–19.41 | 23.07 | 13.73–38.74 |
| Any Mental Health Condition* | 6.84 | 6.29–7.44 | 8.27 | 7.51–9.12 | 10.60 | 8.79–12.78 |
| Fully-Adjusted Modelc | ||||||
| ALL | Male | Female | ||||
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Anxiety Disorder | 2.36 | 2.11–2.64 | 2.83 | 2.46–3.25 | 2.40 | 1.94–2.97 |
| ADHD | 0.88 | 0.66–1.18 | 0.67 | 0.48–0.95 | 0.86 | 0.48–1.53 |
| Bipolar Disorder | 5.14 | 4.29–6.16 | 4.09 | 3.16–5.29 | 8.92 | 6.75–11.78 |
| Depressive Disorders | 4.98 | 4.52–5.48 | 6.43 | 5.73–7.22 | 6.45 | 5.29–7.87 |
| Schizophrenia Spectrum | 4.88 | 3.42–6.95 | 4.66 | 2.95–7.38 | 5.23 | 2.83–9.66 |
| Any Mental Health Condition* | --- | --- | --- | |||
Abbreviations: ADHD, attention-deficit hyperactivity disorder
Any of the listed mental health conditions
Unadjusted model
Adjusted for age, insurance type, poverty level, and education level
Fully-adjusted model included age, insurance type, poverty level, education level, and all listed mental health conditions
After adjusting for sociodemographic characteristics and stratifying by sex, women with diagnosed mental health conditions in the preceding year had a higher relative odds of death by suicide when compared with men (AOR=10.60 vs. AOR=8.27, respectively). In addition, women with diagnosed mental health conditions of bipolar disorder, depressive disorders, and schizophrenia spectrum disorders were more likely to die by suicide than men. The relative likelihood of dying by suicide among women with a diagnosed bipolar disorder (AOR=22.87, 95% CI = 17.79–29.40) was significantly higher than the relative likelihood in men (AOR=12.60, 95% CI = 10.07–15.78). Overall, the effect of mental health diagnoses on suicide mortality was higher in women than in men.
We performed additional analyses to investigate how substance use disorders (SUD) might impact the results that were presented in Table 2. After adjusting for SUD in the sociodemographic-adjusted model and fully-adjusted model separately, the adjusted odds ratios were attenuated. For example, individuals with any of the listed diagnosed mental health conditions in the year prior to the index date were 5 times more likely to die by suicide after adjusting for SUD and sociodemographic characteristics. More details are provided in Supplement Table 1 and Table 2.
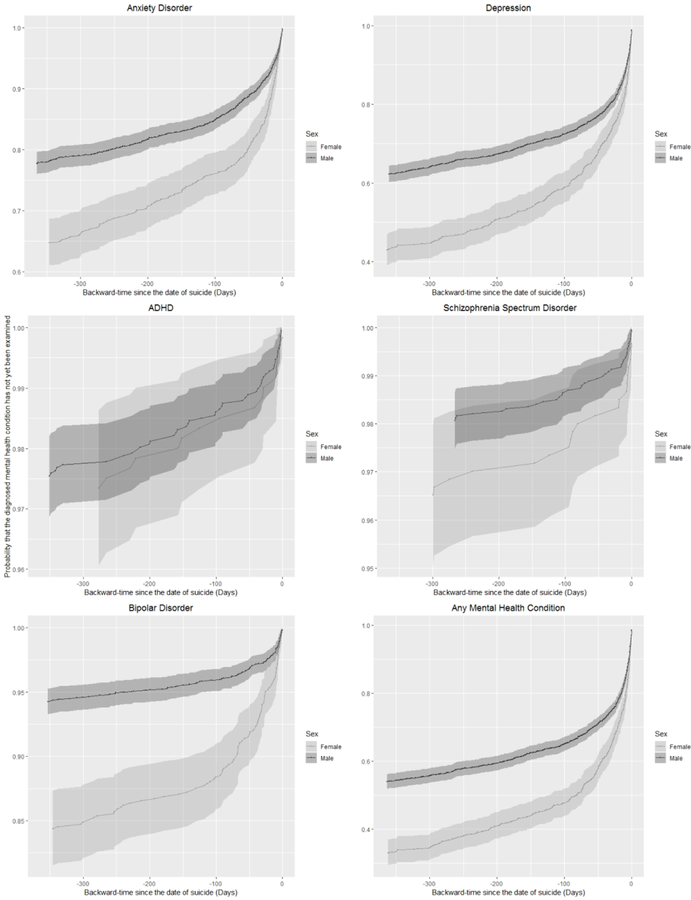
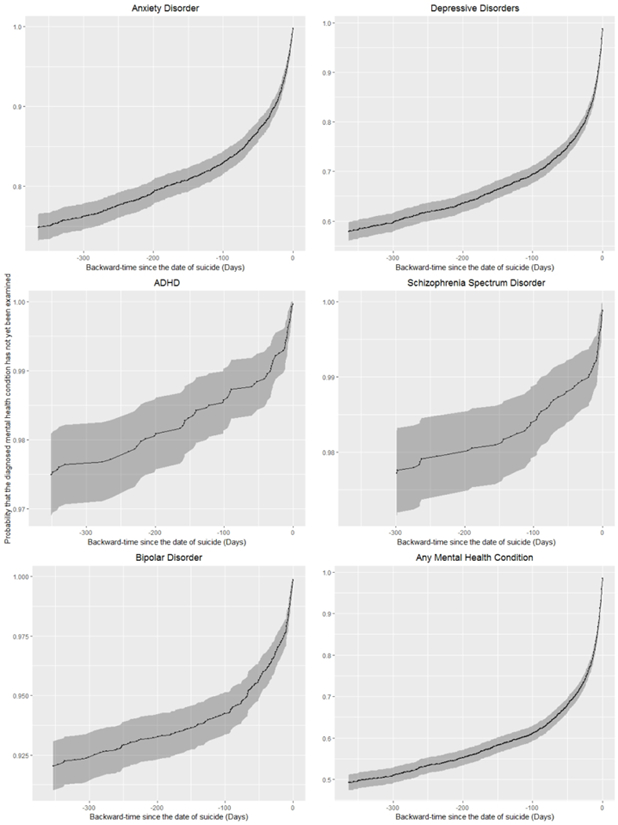
Kaplan-Meier survival curves with inverse time were used to estimate the probability of diagnosed mental health conditions before suicide death (Figure 1). Nearly 40% of individuals who died by suicide had at least one clinical visit with a recorded mental health condition within 3 months before suicide death. This gradually increased to approximately 50% up to within a year before suicide death. More than 40% of individuals had a recorded depressive disorder in the year before suicide death, followed by anxiety disorders (15%), bipolar disorder (7.5%), ADHD (2.5%), and had schizophrenia spectrum disorders (2.1%). Among those with diagnosed mental health condition(s) in the year before suicide, the most recent one often occurred within the 3 months before index date. Nearly 50% of women who died by suicide had at least one clinical visit with a recorded mental health condition within the 3 months before suicide death compared to 35% of males (Figure 2). In addition, within one year before suicide, more than 65% of women who died by suicide had at least one recorded mental health condition compared to 35% of men.
FIGURE 1.
Kaplan–Meier survival curves were used to depict the estimated probability of diagnosed mental health conditions in a year before suicide, plotted with 95% confidence interval bands in inverse survival curve with relation to elapsed time (in days), calculating backward from the time of suicide death to the last clinical visit which the relevant diagnosis was coded.
FIGURE 2.
Kaplan–Meier survival curves were used to the estimated probability of diagnosed mental health conditions in a year before suicide, plotted with 95% confidence interval bands in inverse survival curve with relation to elapsed time (in days), calculating backward from the time of suicide death to the last clinical visit which the relevant diagnosis was coded, stratified by sex.
To reflect the importance of both relative odds and prevalence, we evaluated the PAF of suicide mortality associated with diagnosed mental health conditions in the year before suicide death. An estimated 27% of suicide deaths were attributable to depressive disorders, 22% anxiety disorder, 8% to bipolar disorder, 2 % to schizophrenia spectrum disorders, and 1% to ADHD (Figure 3).
FIGURE 3.
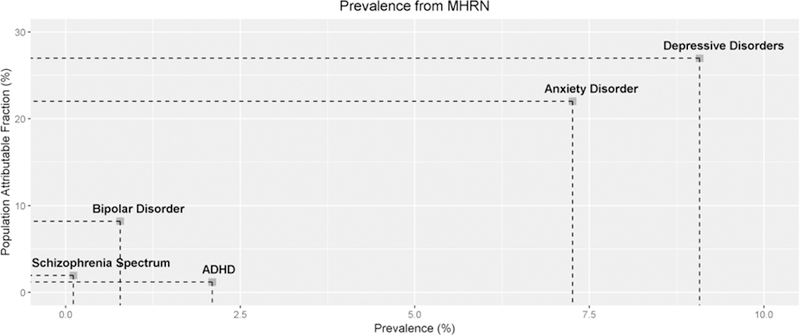
Population attributable fraction (PAF) for the proportion of suicide deaths attributable to mental health conditions. The prevalence of each mental health condition was obtained from Mental Health Research Network (MHRN).
DISCUSSION
The present study found that nearly 50% of people who died by suicide had at least one diagnosed mental health condition in the year before suicide death. Nearly all mental health conditions were associated with an increased risk of suicide mortality, and this risk was highest among those with bipolar disorder, depressive disorders, and schizophrenia spectrum disorders. In addition, among individuals who died by suicide, a greater proportion of women (65%) had recorded mental health diagnoses in the year before suicide when compared with men (35%). Moreover, with respect to the PAF within healthcare systems (i.e., MHRN), approximately 27% of suicide deaths were attributable to depressive disorders.
The findings of this study are similar to previous studies in other populations. Bipolar disorder, depression, and schizophrenia spectrum disorder are three of the most common diagnosed mental health conditions associated with suicide death. Among veterans, bipolar disorder, depression, and schizophrenia spectrum disorder were found to be associated with increased risk of suicide death as well (8). Suicide risk among individuals with any of the listed diagnosed mental health conditions was slightly lower in a veteran population than our study sample. This could be explained by a higher proportion of men than women in veteran populations and that men are less likely to have diagnosed mental health conditions. An English study found a similar result that more than 40% of individuals who died from suicide had a diagnosis of depression or bipolar disorders within 12 months before death and more than 20% had a diagnosed schizophrenia spectrum disorder (7, 18). A meta-analysis also showed that the risk for suicide among patients with bipolar disorder was 20 to 30 times greater than that of the general population (19).
Previous studies have found that, compared to those without anxiety, patients with anxiety were more likely to have suicidal ideation, attempted suicides, or completed suicides in general populations and in veterans (4, 8, 27, 28). Our findings are consistent with these. However, due to the flagged bundled disorders in the dataset, we were not able to tease trauma and other anxiety disorders apart.
Few studies have examined male-female differences of suicide risk among individuals with mental health diagnoses (8, 13, 20–24). Previous studies found that suicide risk was higher among those with bipolar disorder and schizophrenia spectrum disorder, especially for women (20, 24). These findings are in line with those of the current study. In a Swedish population, the standardized mortality ratio (SMR) for suicide was especially high among individuals with bipolar disorder. SMRs for suicide were 8 times higher in men and 10 times higher in women with bipolar disorder as compared to all natural causes of death (13). Sex differences could be explained by the evidence that depression, bipolar and schizophrenia spectrum disorders are more common in women than men. In addition, women are more likely to seek mental health treatment (25, 26), thus making them more likely to have a recorded mental health conditions. This finding is important for men, given that they have a much greater overall risk of suicide, but are much less likely to have a diagnosed mental health condition. This suggests that outreach and universal suicide prevention approaches may be needed, especially for men not being diagnosed with any of the listed mental health conditions within the health system (26).
The association between ADHD and suicide was higher among women than men after adjustment for the effect of age and other socioeconomic factors. Although ADHD is more common in men than women (29), women with ADHD were found to have a much higher risk for self-harm and suicide attempts than men (30). However, the association between diagnosed ADHD and suicide mortality was no longer significant after adjusting for other mental health conditions, suggesting that the risk of suicide mortality is greater among other mental health conditions than ADHD when they co-exist.
Healthcare utilization within one month or one year before suicide has been examined in other studies (31–33). In this study, we examined the estimated probability of clinical visits with a recorded mental health conditions month-by-month from the preceding 1 month to 12 months prior to suicide. These findings will contribute a more detailed timeframe for suicide deaths. Approximately 45% of those who died by suicide had at least one recorded mental health condition within 3 months prior to suicide, a finding similar to previous studies (32, 34, 35). This suggests that there are opportunities to intervene with patients within the healthcare environment prior to suicide, which supports the need for effective identification, assessment, and treatment. The national Zero Suicide initiative provides recommendations for structured processes to accomplish these care pathways (36).
These analyses provide estimates of population-level relative risk as well as number of individuals at risk in the population. Both are important issues to consider when assessing the relationship between mental health conditions and risk of suicide. For example, individual patients with bipolar or schizophrenia spectrum disorders are at highest relative risk of suicide death, but also represent smaller numbers of individuals. Alternatively, the largest number of individuals who died by suicide were individuals with depressive and anxiety disorders, and these individuals may be the focus of larger health system wide suicide prevention approaches. Conditions with greater relative risk, but lower numbers, may be assessed and treated with higher intensity interventions. Conditions occurring among more people, but which have lower relative risk estimates, may be the focus of larger system-wide efforts, including lower intensity screening and intervention approaches.
The data presented in this study is a more accurate representation of who would have an actual diagnosis in the clinic. However, these findings must be viewed in the context of several limitations. First, uninsured individuals were not included in the study population. Therefore, our findings may not be generalizable to this group, such as for calculating attributable suicide deaths. Second, the severity of mental illness was not available in the clinical data collected for this study. Data on the severity of illness could provide more context for these findings. Third, patients who did not survive within the entire year before index date were excluded from the control group. This exclusion criteria might influence differences between the case and control groups. For example, we may have excluded those with mental disorders and died by drug overdose a year before the index date from control group. Finally, all recorded mental health diagnoses were coded by health care providers. Therefore, some conditions may have been undetected or not coded in clinical records because some individuals may not have presented with symptoms during a clinic visit, or presented with symptoms but not met enough criteria for a full diagnosis.
In summary, approximately half of those individuals who died by suicide had at least one diagnosed mental health condition in the year before index date, and most were associated with increased risk of suicide. Our findings suggest the importance of suicide screening and providing approaches to improve the awareness of mental health conditions, as well as going beyond those with mental health conditions to address the risk of suicide more directly (37).
Supplementary Material
HIGHLIGHTS.
Using healthcare data from a large and diverse participant population, we found that nearly all mental health diagnoses were associated with increased risk of suicide.
Suicide mortality risk was associated with different mental health diagnoses for men and women.
The findings may help healthcare professionals identify at-risk individuals for suicide and implement efficient prevention strategies for both men and women.
Acknowledgments:
This project was supported by grants R01MH103529 and U19MH092201 from the National Institute of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Disclosures
Dr. Williams reports serving on an advisory committee for GSK. Dr. Simon reports receipt of royalties from UpToDate. The other authors report no financial relationships with commercial interests.
Previous presentation:
The results of this study were presented at the Health Care Systems Research Network Annual Meeting; April 12, 2018; Minneapolis, Minnesota.
REFERENCES
- 1.Curtin SC, Warner M, Hedegaard H: Increase in Suicide in the United States, 1999–2014. NCHS Data Brief:1–8, 2016. [PubMed] [Google Scholar]
- 2.Gibbons RD, Hur K, Mann JJ: Suicide Rates and the Declining Psychiatric Hospital Bed Capacity in the United States. JAMA Psychiatry 74:849–850, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention: National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS) [online];
- 4.DeVylder JE, Lukens EP, Link BG, et al. : Suicidal ideation and suicide attempts among adults with psychotic experiences: data from the Collaborative Psychiatric Epidemiology Surveys. JAMA Psychiatry 72:219–225, 2015 [DOI] [PubMed] [Google Scholar]
- 5.Nock MK, Hwang I, Sampson NA, et al. : Mental disorders, comorbidity and suicidal behavior: results from the National Comorbidity Survey Replication. Mol Psychiatry 15:868–876, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ahmedani BK, Perron B, Ilgen M, et al. : Suicide thoughts and attempts and psychiatric treatment utilization: informing prevention strategies. Psychiatr Serv 63:186–189, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Appleby L, Shaw J, Amos T, et al. : Suicide within 12 months of contact with mental health services: national clinical survey. BMJ 318:1235–1239, 1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ilgen MA, Bohnert AS, Ignacio RV, et al. : Psychiatric diagnoses and risk of suicide in veterans. Arch Gen Psychiatry 67:1152–1158, 2010 [DOI] [PubMed] [Google Scholar]
- 9.Lewandowski-Romps L, Schroeder HM, Berglund PA, et al. : Medical-encounter mental health diagnoses, non-fatal injury and polypharmacy indicators of risk for accident death in the US Army enlisted soldiers, 2004–2009. Prev Med, 2017 [DOI] [PMC free article] [PubMed]
- 10.Nock MK, Ursano RJ, Heeringa SG, et al. : Mental Disorders, Comorbidity, and Pre-enlistment Suicidal Behavior Among New Soldiers in the U.S. Army: Results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Suicide Life Threat Behav, 2015 [DOI] [PMC free article] [PubMed]
- 11.Fontanella CA, Warner LA, Hiance-Steelesmith DL, et al. : Service Use in the Month and Year Prior to Suicide Among Adults Enrolled in Ohio Medicaid. Psychiatr Serv 68:674–680, 2017 [DOI] [PubMed] [Google Scholar]
- 12.Walby FA, Myhre MO, Kildahl AT: Contact With Mental Health Services Prior to Suicide: A Systematic Review and Meta-Analysis. Psychiatr Serv 69:751–759, 2018 [DOI] [PubMed] [Google Scholar]
- 13.Osby U, Brandt L, Correia N, et al. : Excess mortality in bipolar and unipolar disorder in Sweden. Arch Gen Psychiatry 58:844–850, 2001 [DOI] [PubMed] [Google Scholar]
- 14.Hoyer EH, Mortensen PB, Olesen AV: Mortality and causes of death in a total national sample of patients with affective disorders admitted for the first time between 1973 and 1993. Br J Psychiatry 176:76–82, 2000 [DOI] [PubMed] [Google Scholar]
- 15.Hunt IM, Kapur N, Windfuhr K, et al. : Suicide in schizophrenia: findings from a national clinical survey. J Psychiatr Pract 12:139–147, 2006 [DOI] [PubMed] [Google Scholar]
- 16.Brown GK, Beck AT, Steer RA, et al. : Risk factors for suicide in psychiatric outpatients: a 20-year prospective study. J Consult Clin Psychol 68:371–377, 2000 [PubMed] [Google Scholar]
- 17.Ahmedani BK, Peterson EL, Hu Y, et al. : Major Physical Health Conditions and Risk of Suicide. Am J Prev Med, 2017 [DOI] [PMC free article] [PubMed]
- 18.Osborn D, Levy G, Nazareth I, et al. : Suicide and severe mental illnesses. Cohort study within the UK general practice research database. Schizophr Res 99:134–138, 2008 [DOI] [PubMed] [Google Scholar]
- 19.Pompili M, Gonda X, Serafini G, et al. : Epidemiology of suicide in bipolar disorders: a systematic review of the literature. Bipolar Disord 15:457–490, 2013 [DOI] [PubMed] [Google Scholar]
- 20.Qin P: The impact of psychiatric illness on suicide: differences by diagnosis of disorders and by sex and age of subjects. J Psychiatr Res 45:1445–1452, 2011 [DOI] [PubMed] [Google Scholar]
- 21.Chang CM, Liao SC, Chiang HC, et al. : Gender differences in healthcare service utilisation 1 year before suicide: national record linkage study. Br J Psychiatry 195:459–460, 2009 [DOI] [PubMed] [Google Scholar]
- 22.Cho J, Kang DR, Moon KT, et al. : Age and gender differences in medical care utilization prior to suicide. J Affect Disord 146:181–188, 2013 [DOI] [PubMed] [Google Scholar]
- 23.Qin P, Agerbo E, Westergard-Nielsen N, et al. : Gender differences in risk factors for suicide in Denmark. Br J Psychiatry 177:546–550, 2000 [DOI] [PubMed] [Google Scholar]
- 24.Palmer BA, Pankratz VS, Bostwick JM: The lifetime risk of suicide in schizophrenia: a reexamination. Arch Gen Psychiatry 62:247–253, 2005 [DOI] [PubMed] [Google Scholar]
- 25.Andrade LH, Alonso J, Mneimneh Z, et al. : Barriers to mental health treatment: results from the WHO World Mental Health surveys. Psychol Med 44:1303–1317, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moller-Leimkuhler AM: The gender gap in suicide and premature death or: why are men so vulnerable? Eur Arch Psychiatry Clin Neurosci 253:1–8, 2003 [DOI] [PubMed] [Google Scholar]
- 27.Kanwar A, Malik S, Prokop LJ, et al. : The association between anxiety disorders and suicidal behaviors: a systematic review and meta-analysis. Depress Anxiety 30:917–929, 2013 [DOI] [PubMed] [Google Scholar]
- 28.Sareen J, Cox BJ, Afifi TO, et al. : Anxiety disorders and risk for suicidal ideation and suicide attempts: a population-based longitudinal study of adults. Arch Gen Psychiatry 62:1249–1257, 2005 [DOI] [PubMed] [Google Scholar]
- 29.Cantwell DP: Attention deficit disorder: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry 35:978–987, 1996 [DOI] [PubMed] [Google Scholar]
- 30.Swanson EN, Owens EB, Hinshaw SP: Pathways to self-harmful behaviors in young women with and without ADHD: a longitudinal examination of mediating factors. J Child Psychol Psychiatry 55:505–515, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Luoma JB, Martin CE, Pearson JL: Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry 159:909–916, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vasiliadis HM, Ngamini-Ngui A, Lesage A: Factors associated with suicide in the month following contact with different types of health services in Quebec. Psychiatr Serv 66:121–126, 2015 [DOI] [PubMed] [Google Scholar]
- 33.Ahmedani BK, Simon GE, Stewart C, et al. : Health care contacts in the year before suicide death. J Gen Intern Med 29:870–877, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pearson A, Saini P, Da Cruz D, et al. : Primary care contact prior to suicide in individuals with mental illness. Br J Gen Pract 59:825–832, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Meehan J, Kapur N, Hunt IM, et al. : Suicide in mental health in-patients and within 3 months of discharge. National clinical survey. Br J Psychiatry 188:129–134, 2006 [DOI] [PubMed] [Google Scholar]
- 36.Ahmedani BK, Vannoy S: National pathways for suicide prevention and health services research. Am J Prev Med 47:S222–228, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hogan MF: To Prevent Suicide, Address It Directly. Psychiatr Serv 69:737, 2018 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.