Several validated outcome measures exist for the assessment of postoperative linear scars, but all are subjective in nature.1 These measures suffer from inter- and intra-rater discrepancies depending on observer expertise or inherent biases.2 As a result, several instruments have been developed to help clinicians measure scar parameters objectively. Planimetry is a validated objective method for assessing wound surface area, but can be cumbersome to perform or require expensive proprietary computer software.3 We have devised an elegant improvement upon the traditional planimetry method called trace-to-tape. We tested its feasibility and reliability, and performed an initial validation by comparing it to the Patient and Observer Scar Assessment Scale (POSAS)4 and manual planimetry.5
This study was approved by the institutional review board of University of California, Davis. 20 patients were recruited from the University of California, Davis dermatology clinic. Patients were included if they were greater than 18 years and had a linear postoperative scar greater than 1 month old. Additional patient characteristics are available upon direct application to the corresponding author.
Each scar was evaluated by two unblinded independent observers. Scars were traced with a water-based gel pen applied directly to the skin. While still wet, the gel residue was lifted from the skin with clear packaging tape and transferred onto a sheet of paper, so that an unbroken outline of each scar was preserved on paper to be scanned into the computer. Gel residue was fully removed from the skin with alcohol pads and tracings were redrawn for a total of three measurements per observer. Using the open-source software ImageJ,6 scars were calibrated by length and surface area was measured. Mean scar width was calculated by dividing scar surface area by scar length. Manual planimetry was performed by tracing each scar three times over transparent film comprised of 0.5 cm2 box grids. The area inside the scar border was calculated by counting the number of square boxes inside each tracing. Boxes ≥50% within the tracing were counted as one full box, while those <50% were disregarded.5 Lastly, scars were assessed according to established POSAS guidelines.4
Intra-rater reliabilities for scar surface area derived via the trace-to-tape and manual planimetry methods were estimated with the intraclass correlation (ICC) with blocking by rater7 using the average surface area for each subject and rater and for each measurement time individually. For POSAS scores, inter-rater reliability was estimated as the ICC with fixed raters. Confidence intervals were estimated from 5,000 bootstrap samples. The correlations between average scar width and POSAS scores were estimated with Spearman’s rank correlation.
Trace-to-tape and manual planimetry yielded similar inter-rater (0.97 [95% CI: 0.87–0.99] versus 0.97 [95% CI: 0.66–0.99], respectively) and intra-rater reliabilities (0.95 [95% CI: 0.85–0.97] versus 0.94 [95% CI: 0.62–0.97], respectively), but the confidence limits for trace-to-tape were considerably smaller. Both trace-to-tape and manual planimetry had higher inter-rater reliabilities than POSAS surface area scores (0.65 [95% CI: 0.46–0.81]) and POSAS overall opinion scores (0.59 [95% CI: 0.12–0.81]). Averaging three measurements for either method yielded higher reliabilities and narrower confidence limits than using only a single measurement. Scar width significantly positively correlated with both POSAS surface area and overall opinion scores (Fig. 1).
Figure 1.
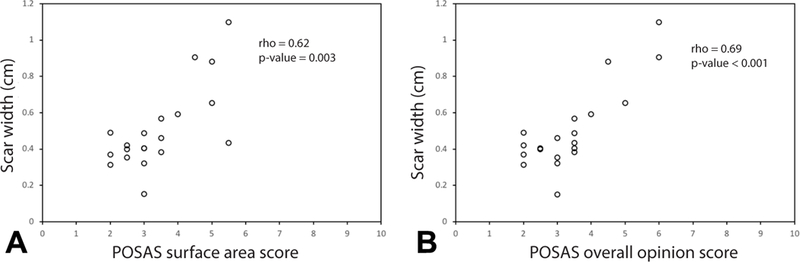
Relationship between scar width as determined with the trace-to-tape method and (a) POSAS surface area score and (b) POSAS overall opinion score. n = 20 patients.
Both manual planimetry and trace-to-tape outperformed POSAS in inter-rater and intra-rater reliability, addressing the inherent pitfalls found in subjective assessment tools. We also found that scar width accurately reflected the overall opinion of scars. Scar width has been used to assess overall appearance, but width varies markedly along the length of the scar.8 However, our method does not rely on an isolated measurement to determine scar width.
While manual planimetry on graph paper was found to be reliable and valid, accuracy depended on where scars were drawn in relation to each grid. Planimetry was also more cumbersome to perform on curved surfaces such as the face. On the other hand, tracing around scars directly on the skin was easier to perform. Water-based gel pens also transferred ink easily from the skin to tape as long as the ink was wet and the tape was applied firmly to the skin.
Our pilot study is currently limited by its small sample size and its inability to address the patient perspective. The tracing methodology itself is not new, but we have introduced a technical improvement that is both simple and fast to perform in a consistent fashion. Therefore, we do not propose that our method completely replace current outcome measures, but supplement them as an inexpensive and accurate instrument to evaluate postoperative scars.
Acknowledgments
Funding sources: Supported by National Center for Advancing Translational Sciences, National Institutes of Health (grant #UL1 TR001860).
Footnotes
Conflicts of interest: None disclosed.
References
- 1.Nguyen TA, Feldstein SI, Shumaker PR, Krakowski AC. A review of scar assessment scales. Seminars in cutaneous medicine and surgery. 2015;34(1):28–36. [DOI] [PubMed] [Google Scholar]
- 2.Fearmonti R, Bond J, Erdmann D, Levinson H. A review of scar scales and scar measuring devices. Eplasty. 2010;10:e43. [PMC free article] [PubMed] [Google Scholar]
- 3.Verhaegen PD, van der Wal MB, Middelkoop E, van Zuijlen PP. Objective scar assessment tools: a clinimetric appraisal. Plastic and reconstructive surgery. 2011;127(4):1561–1570. [DOI] [PubMed] [Google Scholar]
- 4.Draaijers LJ, Tempelman FR, Botman YA, et al. The patient and observer scar assessment scale: a reliable and feasible tool for scar evaluation. Plastic and reconstructive surgery. 2004;113(7):1960–1965; discussion 1966–1967. [DOI] [PubMed] [Google Scholar]
- 5.Bohannon RW, Pfaller BA. Documentation of wound surface area from tracings of wound perimeters. Clinical report on three techniques. Phys Ther. 1983;63(10):1622–1624. [DOI] [PubMed] [Google Scholar]
- 6.Schneider CA, Rasband WS, Eliceiri KW. NIH Image to ImageJ: 25 years of image analysis. Nat Methods. 2012;9(7):671–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gwet KL. Computing inter-rater reliability and its variance in the presence of high agreement. Br J Math Stat Psychol. 2008;61(Pt 1):29–48. [DOI] [PubMed] [Google Scholar]
- 8.Wray RC. Force required for wound closure and scar appearance. Plastic and reconstructive surgery. 1983;72(3):380–382. [DOI] [PubMed] [Google Scholar]


