Abstract
Objective. To evaluate the impact of a large-scale interprofessional forum on pharmacy students’ attitudes toward interprofessional collaborative practice.
Methods. Pharmacy students were asked to complete the Interprofessional Attitudes Scale (IPAS) prior to and after completing a three-hour interprofessional forum. Scores for the total IPAS and each of the subscales were computed using the mean of students’ responses to the items for each.
Results. Of the 133 pharmacy students who participated in the forum, there were valid pre- and post-intervention matched IPAS data for 124 (93.2%). In general, prior to the forum, students reported positive attitudes toward interprofessional collaborative practice as demonstrated by mean scores greater than 4.0 (agree) on the total IPAS scale and on all of the IPAS subscales except the Interprofessional Biases subscale). There was a significant increase from pre- to post-intervention scores on all the subscales except Patient-Centeredness. Based on the Cohen d measure of effect size, the greatest changes were in the Teamwork, Roles and Responsibilities and Community-Centeredness subscales, followed by the Interprofessional Biases subscale and Diversity and Ethics subscale.
Conclusion. Prior to participating in an interprofessional student forum, pharmacy students generally had positive attitudes toward interprofessional collaborative practice. After participating in the forum, these attitudes become even more positive. Interprofessional education interventions, such as the forum, play an important role in shaping student’s attitudes toward interprofessional collaboration.
Keywords: interprofessional, patient care team, opioid analgesics, pharmacy students
INTRODUCTION
In practice, health care professionals are increasingly required to work collaboratively as part of an interprofessional health care team with the goal of optimizing health care delivery, increasing patient satisfaction, and improving patient outcomes. As such, interprofessional education (IPE) has become a focus for programs training future health care professionals. Interprofessional education interventions have resulted in positive outcomes in chronic disease state management, culture and patient satisfaction, and teamwork, and reductions in clinical errors.1 Additionally, early implementation of IPE is important and may prevent the development of negative interprofessional attitudes.2
Within pharmacy education there is increased emphasis on developing and assessing IPE experiences to prepare pharmacy students to be collaborators on interprofessional health care teams. The Center for the Advancement of Pharmacy Education (CAPE)3 outcomes and the Accreditation Council for Pharmacy Education (ACPE)4 standards both have an increased focus on IPE, and ACPE requires documentation of student assessment outcomes. While many IPE activities have been described, large gaps remain in the literature relating to their evaluation, the effect of the context in which they are delivered, and the experience of the participants.5 These gaps likely exist because of the challenges encountered when implementing IPE. The Interprofessional Education Collaborative (IPEC) highlights some of these challenges, which include institutional challenges (eg, lack of leadership and resources), practical issues when scheduling students across professions, and faculty development in IPE.6
In fall 2016, the Office of Interprofessional Education at the University at Buffalo hosted its first large-scale interprofessional forum designed to bring 740 students from nine health professions education programs at the university together for an IPE experience. The primary objective of this study was to assess the impact of the forum on pharmacy students’ attitudes toward interprofessional collaborative practice using a validated assessment instrument. Herein we discuss our overall approach to delivering and assessing the forum and the changes in pharmacy students’ attitudes toward interprofessional collaborative practice as a result of participation in the forum. The structure of the forum and the assessment process may be useful to other institutions developing and evaluating IPE.
METHODS
At the University at Buffalo, the Office of Interprofessional Education (http://www.buffalo.edu/ipe) was established in 2013 to develop and implement high-impact interprofessional educational experiences integrated into the existing curricula to promote achievement of the IPEC core competencies. The Office of Interprofessional Education is endorsed and supported by the University at Buffalo School of Medicine and Biomedical Sciences, School of Dental Medicine, School of Nursing, School of Pharmacy and Pharmaceutical Sciences, School of Public Health and Health Professions, School of Social Work, School of Law, and School of Management.
In fall 2016, the forum, “Confronting Opioid Dependence: An Interprofessional Approach,” was delivered. The overall goal of the forum was to create an experience for students to learn about, with, and from each other regarding professional roles and responsibilities and concepts of teamwork and team-based practice in the context of a major public health emergency. The objectives for the forum were that upon completion, students could describe the rise of opioid addiction; explain the reason why prevention and treatment of this problem must be addressed with an interprofessional team approach; describe their unique professional role and responsibilities as well as those of other providers within an interprofessional team; and, create a multifaceted prevention and treatment plan for opioid addiction with their interprofessional team members based on the case reviewed.
Table 1 presents the activities that made up the forum. To prepare for the forum, students were asked to view material regarding opioid addiction. Additionally, students were asked to complete two online modules entitled, “What Is Interprofessional Collaboration and Why Is It Important?” and “Roles and Responsibilities.” These modules were developed internally and are components of a six-part module series entitled Foundations of Interprofessional Collaborative Practice Online Module Series. This series provides students an easily accessible method to develop foundational knowledge essential for subsequent in-person interprofessional experiences. The modules are based on the IPEC Core Competencies for Interprofessional Collaborative Practice and principles of cultural engagement.6
Table 1.
Student Activities Held and Learning Objectives for a Three-Hour Interprofessional Forum on Opioid Dependence
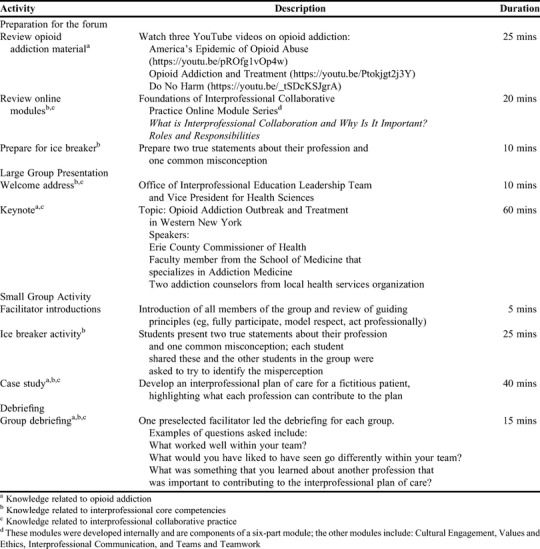
The forum occurred on one day during the fall 2016 semester. Students were assigned to attend one of three identical three-hour sessions. For the first 45 minutes, students (∼250 students per session) gathered for a large group activity in one large lecture hall where they listened to a welcome address from the Office of Interprofessional Education Leadership Team, remarks from the Vice President for Health Sciences (∼10 minutes), and a keynote address (∼1 hour). After the large group activity, students participated in a small group activity (∼35 groups per session) where they broke into small, interprofessional teams of six to seven students (with no team having more than two students from a single profession) and met in different classrooms. During the small group activity, each student team completed an ice breaker activity and a case discussion. The small group activities were guided by faculty facilitators (∼35 facilitators per session) from the various professional programs that were involved. Facilitators assisted student groups by guiding their discussion of the interprofessional plan of care and conducting a short debriefing (15 minute) at the end of the small group activities. Each professional program was required to provide coverage of one faculty facilitator for every seven students of that program participating in the forum (eg, the school of pharmacy was required to cover 19 facilitator spots throughout the entire forum to cover the 133 pharmacy student who participated). The same faculty facilitator was allowed to facilitate multiple sessions throughout the day.
Each program attempted to send cohorts of students with similar experience (eg, students with some professional awareness and clinical experience) based on year in their respective program. There were 740 students from nine programs: dental medicine (n=102), medicine (n=140), nursing (n=121), pharmacy (n=133), occupational therapy (n=61), physical therapy (n=44), social work (n=125), law (n=3), and management (n=11). The forum was required for students in the dental medicine, medicine, nursing, pharmacy, occupational therapy, physical therapy, and social work cohorts, but optional for law and management students
The University at Buffalo Institutional Review Board reviewed this study and determined it to be exempt. Third-year pharmacy students were required to participate in the forum. All third-year pharmacy students were asked to complete the Interprofessional Attitudes Scale (IPAS)7 prior to the forum (pre-intervention) and after completing the forum (post-intervention). The IPAS is a scale designed to assess attitudes that relate to the 2011 Core Competencies for Interprofessional Collaborative Practice. The IPAS tool was chosen because it was developed with input from health professional students, including pharmacy students. The IPAS is best used to assess students’ readiness to engage in interprofessional activities and should be used early in the IPE implementation process, which was consistent with the objectives of the forum.8 The tool consists of 27 items that use a five-point Likert-scale rating system on which 1=strongly disagree, 2=disagree, 3=undecided, 4=agree, and 5=strongly agree. The IPAS has five subscales: Teamwork, Roles and Responsibilities; Patient-Centeredness; Interprofessional Biases; Diversity and Ethics; and Community-Centeredness.
The analyses were conducted using IBM SPSS (Armonk, NY).10 Scores were computed for the total IPAS and each of the subscales using the total mean of the responses to the items that comprised the scale. Use of the mean of the item responses, as opposed to the summated score, made the scores easier to interpret as they can be interpreted the same as the Likert scale. The reliability of the obtained scale scores was estimated using Cronbach alpha. Cronbach alpha reliabilities of 0.70 or above are considered generally acceptable for instruments with low stakes.9 In addition, each item was examined by estimating the reliability of the scale score if the item was removed from the scale.
The means and standard deviation (SD) of the pre-intervention, post-intervention, and difference scores were presented for the total IPAS scale and each of the subscales. To examine differences between pre- and post-intervention, paired sample t tests were conducted; p values <.05 were considered significant. In addition, the Cohen d effect size, which indicates the number of standard deviations by which the pre- and post-intervention scores differ was computed for each comparison. Cohen d values less than 0.2 were considered very small (meaningless); greater than 0.2 and up to 0.5 were considered small but meaningful; greater than 0.5 and up to 0.8 were considered medium; and greater than 0.8 were considered large.11
RESULTS
Of the 136 third-year pharmacy students enrolled, 133 participated. Of the 133 pharmacy students who participated in the forum, there were valid pre- and posttest matched IPAS data for 124 students (93.2% of pharmacy student attendees).
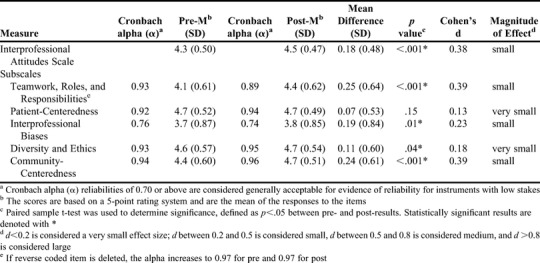
The results pertaining to the IPAS scale and each of the subscales are presented in Table 2. The Cronbach alpha for all of the subscales and for the IPAS scale were above 0.70, indicating acceptable reliability. In general, prior to attending the forum, students reported positive attitudes toward interprofessional collaborative practice as demonstrated by mean scores greater than 4.0 (agree) for the total IPAS scale and all of the IPAS subscales except the Interprofessional Biases subscale. There was a significant increase from pre- to post-intervention scores on all of the subscales except Patient-Centeredness. Based on the Cohen d measure of effect size, the greatest changes were in the Teamwork, Roles and Responsibilities and the Community-Centeredness subscales, followed by changes in the Interprofessional Biases subscale and the Diversity and Ethics subscale. Of note, there was one item on the Teamwork, Roles and Responsibilities subscale (“It is not necessary for health sciences students to learn together”) that was reverse coded per the instrument developers. If this item were removed from the scale, the Cronbach alpha would have increased for both the pre- and post-intervention scores.
Table 2.
Analysis of Pharmacy Students’ Attitudes Toward Interprofessional Collaboration Before and After Participation in a Three-Hour Interprofessional Forum on Opioid Dependence
DISCUSSION
Within pharmacy education, there is an increased emphasis on developing high-quality IPE interventions and using well aligned, reliable measurement instruments to evaluate the impact of the intervention at a designated level (reaction, perceptions and attitudes, knowledge and skills, behavioral change, organizational practice, benefits to patients/clients).8 Our study examined the impact of a large-scale interprofessional forum on pharmacy students’ attitudes toward collaborative practice using a measurement tool (IPAS) that aligns with the IPEC core competencies and that included pharmacy students in the validity and reliability testing of the instrument. The results demonstrate that the forum increased pharmacy students’ attitudes toward interprofessional collaborative health care practice, which corroborates and extends previously published reports of the impact of IPE learning experiences on pharmacy students’ attitudes.2,12 Overall, the IPAS scores indicated that pharmacy students initially had positive attitudes toward interprofessional collaborative practice and these attitudes became even more positive following their participation in the IPE program. The interpretation of the measure of effect size categorizes this effect as small (d=0.38). More recent studies of effect sizes in educational research have noted that a small effect size is practically meaningful for an educational intervention, and that the mean Cohen d effect size across different types of interventions was 0.28 and the median effect size was 0.18.13 Thus, the effect size of 0.38 on the IPAS scale is significant, especially given that the intervention took place over a couple of hours.
The effect sizes on the subscales allowed us to examine what areas demonstrated the most change. The largest change in students’ attitudes as measured by the effect size was seen in the Teamwork, Roles, and Responsibilities scale (d=0.39) and the Community-Centeredness scale (d=0.39). Items in the Teamwork, Roles, and Responsibilities subscale reflect content covered in the learning objectives of the IPE program, which prioritizes learning the roles and responsibilities of other health care professionals and the importance of interprofessional teamwork to enhance patient health care outcomes. The Community-Centeredness subscale measures positive attitude toward community-based public health initiatives, the role of administrators and legislators, and the importance of advocating for patient and community health programs. The content of the IPE program aligned with the items in this subscale. Students were asked not only to discuss the management of the fictitious patient in the case study, but also to discuss strategies for prevention and changes to the health care system that might improve the patient’s situation. In addition, social work, law, and management professional students were involved in the small group patient case discussions. Exposure to the perspectives of these professional students regarding the management of the patient may have contributed to the pharmacy students’ positive attitudes.
The IPAS instrument was selected because it has demonstrated good factor structure and internal consistency7 and aligns with the IPEC Core Competencies for Interprofessional Collaborative Practice.6 However, the IPAS developers note some cautions when using the instrument.7 The developers suggest that the IPAS could be used for pre- and post-intervention assessment, though validation for using it for this purpose is needed. The IPAS developers also noted that the students that they administered the instrument to had few formal IPE experiences prior to completing the instrument, yet responses showed favorable attitudes toward interprofessionalism, suggesting that there may be a “ceiling effect” that could make it difficult to detect changes. Our study demonstrates that there may have been a ceiling effect. Our student sample had few formal IPE experiences, yet like the student sample used when the instrument was developed, the students had very positive attitudes toward interprofessionalism. The pre-intervention means of all but one of the subscales (Interprofessional Biases) were above 4.0. The students’ strongly positive attitudes toward interprofessionalism and patient-centered care exhibited by our students prior to the IPE program are consistent with our school’s values. The IPAS developers suggest the possibility of using a 100-point slider scale for each item to avoid a ceiling effect; however, this has not been validated. Developing measures sensitive enough to detect change over time is often challenging and has been discussed in previous education research.14,15 Our research suggests that creating instruments for IPE that can measure change over time is important, especially as more programs implement multiple IPE activities in their curriculum.
The strengths of this study include the large sample size, the very high response and participation rates, and the use of an instrument to measure student attitudes that has strong psychometric properties. This study used a well-designed assessment strategy to evaluate a high quality, large-scale, IPE program and thus contributes to the literature on effective IPE interventions. In addition, the study used a validated measure of attitudes toward IPE and therefore provides information on the validity and reliability of the tool and additional contexts for its potential use.7
The forum included students from a broad range of professional programs, which provided opportunities for pharmacy students to interact with many different types of professional students. Other students who participated in the IPE forum were of similar experience to ours within their professional program, which is an important consideration when designing an IPE activity.5,16,17 Several barriers that are common to organizing an IPE event, particularly one of this size, were overcome. To accommodate different class schedules across programs, three different sessions were offered throughout the day. This allowed us to maximize student attendance while still accommodating program-specific conflicts. We chose a topic (opioid dependence) that has relevance at the local, state, and national level, and therefore student interest and buy-in was evident. The event was held on a day of the week when there were the most vacant classrooms available within the school of pharmacy building. Finally, we provided pre-forum training to faculty members by distributing a video to them created by the Office of Interprofessional Education on how to be an effective IPE group facilitator, along with the same materials that students would receive.
This study is not without limitations. This study was conducted with one cohort of pharmacy students at one institution; therefore, it is not known whether pharmacy students at different phases of their education or at different educational institutions would respond similarly. The professions represented in the small groups varied. Given the range of class sizes, not every profession was represented in every small group, and in many cases, there were two students from one profession in each group. Despite these limitations in profession representation in the small groups, pharmacy students reported increased positive attitudes following the IPE program, which is consistent with the World Health Organization’s belief that interprofessional education occurs when two or more health care students learn about, from, and with each other.18 To facilitate conversations about the roles of health professions not represented in a group, the group faculty facilitators were provided with an informational guide describing the contributions of unrepresented professions. This information could be shared with the students during the case discussion.
While we observed a change in pharmacy students’ attitudes after this single event, we cannot say whether these changes will be sustained. As this program was one of the first large-scale IPE events on campus, the intent was that it would provide students with foundational knowledge about the principles of IPE and interprofessional collaborative practice on which further IPE events can be built. Further research should be aimed at implementing and assessing higher-level activities (eg, simulation, experiential education IPE activities) that can determine whether these changes in attitudes affect students’ behaviors and ultimately health outcomes.
CONCLUSION
The pharmacy students had positive attitudes toward interprofessional collaborative practice even before participating in the IPE intervention. Students’ attitudes about IPE were more positive following participation in the forum, during which students had the opportunity to learn about other professions, patient management, prevention, and health system with colleagues from other health and non-health professions programs.
REFERENCES
- 1.Reeves S, Perrier L, Goldman J, Freeth D, Zwarenstein M. Interprofessional education: effects on professional practice and healthcare outcomes (update) Cochrane Database Syst Rev. 2013;3:CD002213. doi: 10.1002/14651858.CD002213.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hood K, Cant R, Baulch J, et al. Prior experience of interprofessional learning enhances undergraduate nursing and healthcare students' professional identity and attitudes to teamwork. Nurse Educ Pract. 2014;14:117–122. doi: 10.1016/j.nepr.2013.07.013. [DOI] [PubMed] [Google Scholar]
- 3.Medina MS, Plaza CM, Stowe CD, et al. Center for the Advancement of Pharmacy Education 2013 educational outcomes. Am J Pharm Educ. 2013;77:162. doi: 10.5688/ajpe778162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Accreditation Standards and Key Elements for the Professional Program in Pharmacy Learning to the Doctor of Pharmacy Degree, Accreditation Council for Pharmacy Education. https://www.acpe-accredit.org/pdf/Standards2016FINAL.pdf. Accessed September 1, 2017.
- 5.Olson R, Bialocerkowski A. Interprofessional education in allied health: a systematic review. Med Educ. 2014;48:236–246. doi: 10.1111/medu.12290. [DOI] [PubMed] [Google Scholar]
- 6. Core Competencies for Interprofessional Collaborative Practice: 2016 Update, Interprofessional Education Collaborative. IPEC. Core Competencies. https://nebula.wsimg.com/3ee8a4b5b5f7ab794c742b14601d5f23?AccessKeyId=DC06780E69ED19E2B3A5&disposition=0&alloworigin=1. Accessed September 1, 2017.
- 7.Norris J, Carpenter JG, Eaton J, et al. The development and validation of the interprofessional attitudes scale: assessing the interprofessional attitudes of students in the health professions. Acad Med. 2015;90:1394–1400. doi: 10.1097/ACM.0000000000000764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shrader S, Farland MZ, Danielson J, Sicat B, Umland EM.A systematic review of assessment tools measuring interprofessional education outcomes relevant to pharmacy education Am J Pharm Educ 2017816):Article 119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nunnaly JC. Psychometric Theory. 2nd ed. New York, NY: McGraw Hill; 1978. [Google Scholar]
- 10.2015. SPSS Statistic for Windows [computer program]. Version 23. Armonk, NY: IBM Corporation.
- 11.Cohen J. 2nd ed. New York, NY: Academic Press; 1988. Statistical Power Analysis for the Behavioural Sciences. [Google Scholar]
- 12.Terreri LA, Homish GG, Wahler RG, Brody PM, Ohtake PJ. Impact of interprofessional falls risk assessment program on student perceptions of other healthcare professionals. J Interprof Educ Pract. 2017;9:82–85. [Google Scholar]
- 13. Translating the Statistical Representation of the Effects of Education Interventions Into More Readily Interpretable Forms, National Center for Special Education Research. https://ies.ed.gov/ncser/pubs/20133000/pdf/20133000.pdf. Accessed September 1, 2017.
- 14.Maerten-Rivera J, Huggins-Manley AC, Adamson K, et al. Development and validation of a measure of elementary teachers’ science content knowledge in two multiyear teacher professional development intervention projects. J Res Sci Teaching. 2015;52:371–396. [Google Scholar]
- 15.Desimone LM. Improving impact studies of teachers’ professional development: toward better conceptualizations and measures. Educ Res. 2009;38:181–199. [Google Scholar]
- 16.Poirier TI, Wilhelm M. Interprofessional education: fad or imperative. Am J Pharm Educ. 2013;77:68. doi: 10.5688/ajpe77468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jorm C, Nisbet G, Roberts C, Gordon C, Gentilcore S, Chen TF. Using complexity theory to develop a student-directed interprofessional learning activity for 1220 healthcare students. BMC Med Educ. 2016;16:199. doi: 10.1186/s12909-016-0717-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Framework for Action on Interprofessional Education and Collaborative Practice. World Health Organization. http://www.who.int/hrh/resources/framework_action/en/. Accessed September 1, 2017.


