Abstract
Background
With the improvements of modern surgical techniques and hip prosthesis, the causes for dislocation after total hip arthroplasty (THA) have changed. The aim of this retrospective analysis was to identify new plain radiography findings to predict dislocation after THA.
Methods
Five thousand five hundred thirteen consecutive primary THAs performed between January 2000 and December 2014 were reviewed through a nested case–control study design. Among them, 38 patients with 39 hip dislocations (dislocation group) were selected and matched to 78 hips in 78 patients without dislocation (control group). The factors that might influence the prosthetic stability were identified by univariate analyses, and a multivariate logistic regression analysis was performed to determine the odds ratio of each factor.
Results
The difference of the cup position was not statistically significant. The newly identified risk factors were the following: preoperative hip adduction deformity combined with limb lengthening of 2 cm postoperatively; a knee valgus combined with pelvic obliquity deformity and bilateral pathological hips.
Conclusions
Patients with soft tissue imbalance, across joint deformity around hips and bilateral pathological hips seem more predisposed to suffer from dislocation after THA. Appropriate surgical intervention strategies along with meticulously postoperative management may help preventing dislocation after THA.
The translational potential of this article
A better understanding of the probable causes of dislocation after THA proposed a new clinical application of plain radiography. This radiography-related clinical research may reveal the novel mechanism of dislocation after THA and new preventive measures.
Keywords: Case–control study, Dislocation, Total hip arthroplasty, Risk factors
Abbreviations: AD, Adduction deformity; ASA, American Society of Anesthesiologists; BMI, Body mass index; BP, Bilateral pathological hips; KV, Valgus deformity of the knee; MLL, Mild limb lengthening; OR, Odds ratios; PO, Pelvic obliquity; THA, Total hip arthroplasty
Background
With the improvement of the surgical techniques and prosthesis design, the rate of dislocation after total hip arthroplasty (THA) has decreased to 0.05–3.9%, according to the recent reports [1], [2], [3]. Nevertheless, postoperative dislocation is still the most common early complication after THA and one of the most common causes of early revision of primary THA [4]. Moreover, this complication directly increases the patients' medical costs and may result in loss of trust between the patients and their surgeons.
The postoperative instability is caused by implant-, surgical- and patient-related factors. The main causes of dislocation after THA include the following: (1) malpositioning or loosening of the stem or acetabular component; (2) contact between the prosthesis neck and articular component subject to joint position; (3) contact between the bony femur and bony pelvis; (4) post-traumatic THA; (5) hyperlaxity of the joint due to insufficient muscle strength or a lack of tissue tension; (6) neuromuscular disorders and (7) osteonecrosis of the femoral head [5], [6], [7]. Two recommendations such as improving the accuracy of implant settlement [8], [9] and choosing a large-diameter femoral head were made to reduce the dislocation rate. Nevertheless, it is apparent that the problem of instability after THA remains unsolved [10]. Most studies have focussed mainly on the component malposition and soft tissue laxity [11], which can increase the rate of dislocation individually or synergistically. The authors of this study assumed that there were some unknown factors involved, especially individual factors found in plain radiography, which could predispose the patients to dislocation after THA.
Therefore, the aim of the present retrospective analysis was to find new risk factors of dislocation after THA. The results could help identifying patients who are at higher risk of dislocation after THA and in need of a closer management.
Methods
Study design and patients
A total of 5513 consecutive primary THAs were performed between January 2000 and December 2014. The mean age at the time of the operation in the entire cohort of patients was 59 years (range, 21–91 years). There were 3321 females (3802 hips) and 1329 males (1711 hips). All patients were followed up for at least 2 years.
The inclusion criteria were the following: (1) primary THA; (2) follow-up for ≥2 years and (3) postoperative dislocation (at least once). The exclusion criteria were the following: (1) catastrophic wear of polyethylene; (2) abductor muscle loss or (3) nonunion of the greater trochanter.
Of the 5513 patients, 48 patients (49 hips) had postoperative dislocation (femoral head detachment from its liner postoperatively [12]), for a total dislocation rate of 0.89%. Among them, three hips with catastrophic wear of polyethylene liner, four hips with abductor muscle loss and three nonunion of the greater trochanter were excluded. Finally, 38 patients (39 hips; dislocation group) were identified for this retrospective analysis. According to the method of nested case–control study [13], diagnosis of disease-, age- and sex-matched patients (78 hips; 1:2 matched ratio) with no dislocation after THA were selected as the control group. The age difference between the patients with and without dislocation is less than 10 years. The admission time of every patient from the control group was within 1 month from the day of hospitalization of patients with dislocation after THA. In our cases, none of the patients in the dislocation group had body mass index (BMI) >30 or the American Society of Anesthesiologist (ASA) classification score ≥3. The femoral head size was the same between the dislocated and the control cases. This study was approved by the ethical committee.
Data collection
Our preoperative anteroposterior radiography of hip was obtained, with the patient lying flat on the table in their natural position. The postoperative film was obtained in the same way on the 2nd day after surgery. The cup position was measured on this plain X-ray film. The anteversion angle was obtained from trigonometric functions of the length of the short ellipse axis and long ellipse axis, according to the Widmer algorithm [14]. Lewinnek et al. [9] proposed a radiographic safe range for the position of the cup as cup abduction angle of 40 ± 10° and anteversion angle of 15 ± 10. Accordingly, the patients after THA were divided as patients with safe and unsafe hips.
The following parameters were examined for their possible association with dislocation after THA:
-
1.
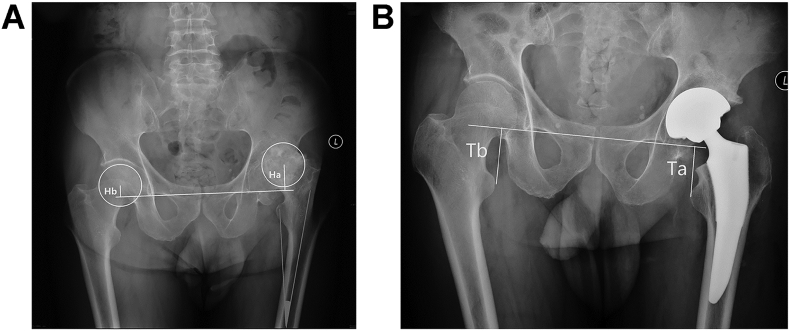
Preoperative hip adduction deformity (AD): An angle between the femoral shaft axis and median line of the body of ≥10° was defined as AD (Fig. 1A) [15]. AD was not only measured by the supine position film but also confirmed by the physical examination of patients with hip adduction movement ≤0° or fixed adduction contracture.
-
2.
Mild limb lengthening (MLL): The limb lengthening referred to the sum of preoperative limb shortening and postoperative limb lengthening (Fig. 1B) [16]. In this study, MLL was defined as lengthening by 2 cm.
-
3.
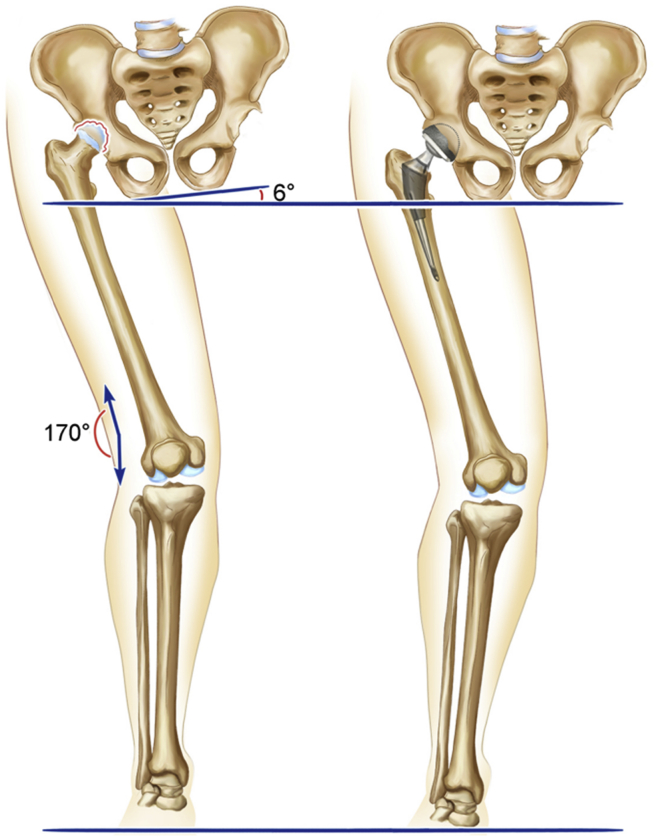
Valgus deformity of the knee (KV): The KV was defined as a preoperative femoral-tibial angle of ≤170°, leaving to valgus knee (Fig. 2) [17].
-
4.
Pelvic obliquity (PO): An preoperative angle between the iliac crest line and horizontal line ≥6° was defined as PO (Fig. 2) [18].
-
5.
Bilateral pathological hips (BP): In this study, BP was defined as patients who underwent bilateral THAs within 1 year or patients who underwent THA with the need of THA on the other side because of the same pathological reason [19].
Figure 1.
(A) Adduction deformity was defined as the angle between the femoral shaft axis and median line of the body ≥10°. (B) Limb lengthening = h1 + h2, where h1 = difference between the distance from the femoral head center to the teardrop line preoperatively (Ha-Hb) and h2 = difference between the distance from lesser trochanter to the teardrop line postoperatively (Ta-Tb). Mild limb lengthening was defined as 2 cm.
Figure 2.
Knee valgus deformity (KV) was defined as femoral tibial angle of ≤170°. The angle between the iliac crest line and horizontal line of ≥6° was defined as pelvic obliquity (PO). The dislocation caused by “across joint deformity” around the hip was the combined deformity of KV and PO.
Statistical analysis
Statistical analysis was performed using SPSS 11.0 (SPSS Inc., Chicago, IL, USA). Two-sided P-values<0.05 were considered statically significant. Continuous data were tested for normality using the Kolmogorov–Smirnov test. Normally distributed data were presented as mean ± standard deviation and analysed using the Student t test. Non-normally distributed data were presented as median (range) and analysed using the nonparametric Mann–Whitney U test. Categorical variables were presented as frequencies and analysed using the Fisher's exact test. A multivariate logistic regression analysis was performed, and the odds ratios (ORs) were used to estimate the risk factors for dislocation.
Results
Characteristics of the results
Among the patients with dislocation, three underwent open reduction, nine received revision THA and 27 underwent closed reduction. One patient developed recurrent dislocation after revision and had to wear a waist-hip-ankle brace.
Table 1 presents the characteristics of the patients. In the dislocation group, there were 14 males and 25 females, and the mean age of patients was 56.7 years (range, 20–79 years). The follow-up period was 2–11 years (average, 5.6 years). The BMI was between 21.4 and 28.2 (mean, 22.3 ± 3.5), and the mean ASA classification score was 2.1 ± 0.6. None of the patients from the dislocation group suffered from alcoholism or neuromuscular disorders. All the THAs were performed in the lateral position following the posterolateral approach by high-volume surgeons. They performed posterolateral approach and posterior soft tissue repair in the same method.
Table 1.
Characteristics of the patients.
| Previous factors | Dislocated, N = 48 | Control, N = 78 | P |
|---|---|---|---|
| Gender (female/male) | 25/14 | 48/30 | 0.79 |
| Age, years (range) | 56.7 (20–79) | 57.9 (23–79) | 0.67 |
| Body mass index, kg/m2 (range) | 22.3 (21.4–28.2) | 22.5 (21.5–28.0) | 0.57 |
| Side (right/left) | 20/19 | 41/37 | 0.90 |
| ASA score | 2.1 ± 0.6 | 2.0 ± 0.6 | 0.65 |
ASA = American Society of Anesthesiologists.
Factors for dislocation after THA
In the present study, there were no significant differences in cup abduction (P = 0.87) and anteversion (P = 0.44) between the two groups. Ten hips (25.6%) and nine hips (11.5%) from the dislocation group and control group were deemed unsafe (P = 0.05), respectively.
The results of the univariate analyses indicated that preoperative AD, MLL, KV and PO did not affect the risk of dislocation separately, but when combining factors, AD + MLL (P < 0.01) and KV + PO (P = 0.03, by Fisher's exact test) were significantly different between the two groups. It was found that the BP ratio was significantly different between the two groups (P = 0.02) (Table 2).
Table 2.
Univariate analysis of factors possibly associated with dislocation after THA.
| Factors | Dislocated, N = 39 | Control, N = 78 | P |
|---|---|---|---|
| Abduction angle(°) | 42.4 (28–66) | 41.8 (25–56) | 0.87 |
| Anteversion angle(°) | 13.9 (0–29) | 15.5 (2–32) | 0.44 |
| Unsafe (Lewinnek [9] safe zone) | 10 (25.6%) | 9 (11.5%) | 0.05 |
| Adduction deformity (AD) | 33 (84.6%) | 57 (73.1%) | 0.16 |
| Mild limb lengthening (MLL) | 21 (53.8%) | 34 (43.6%) | 0.30 |
| AD + MLL | 20 (51.3%) | 17 (21.8%) | <0.01 |
| Knee valgus deformity (KV) | 7 (17.9%) | 7 (9.0%) | 0.27 |
| Pelvic obliquity (PO) | 8 (20.5%) | 15 (19.2%) | 0.87 |
| KV + PO | 6 (15.4%) | 2 (2.6%) | 0.03 |
| Bilateral pathological hips (BP) | 19 (48.7%) | 21 (26.9%) | 0.02 |
THA = total hip arthroplasty.
The multivariate logistic regression analysis indicated that BP and two combined factors including KV + PO and AD + MLL were significantly different between the two groups (Table 3). The corresponding ORs were 2.69, 6.42 and 3.65 for BP (P = 0.03), KV + PO (P = 0.04), and AD + MLL (P = 0.001), respectively.
Table 3.
Multivariate logistic regression analysis of factors associated with dislocation after THA.
| Factors | Regression coefficient | Odds ratio | P | 95% confidence interval |
|---|---|---|---|---|
| AD + MLL | 1.30 | 3.65 | <0.01 | 1.53–8.72 |
| KV + PO | 1.86 | 6.42 | 0.04 | 1.14–36.21 |
| BP | 0.99 | 2.69 | 0.03 | 1.13–6.38 |
THA = total hip arthroplasty; AD = adduction deformity; BP = bilateral pathological hips; KV = knee valgus deformity; MLL = mild limb lengthening; PO = pelvic obliquity
Discussion
The postoperative instability is caused by implant-, surgical- and patient-related factors. Surgeons tried to prevent dislocation after THA by implanting the prosthesis more accurately and using a bigger head [20]. Nevertheless, modern surgical techniques and hip prosthesis could not eliminate dislocation after THA. This study aimed to identify new risk factors of dislocation after THA, which we did not considerate enough. The results showed that the difference of the cup position was not statistically significant. The newly identified risk factors were the following: preoperative hip AD combined with limb lengthening of 2 cm postoperatively; knee valgus combined with PO deformity and bilateral pathological hips. Appropriate surgical intervention strategies along with meticulously postoperative management may help preventing dislocation after THA.
Previous studies explored inherent factors including etiological factors, age, gender, BMI >30, ASA classification score ≥3 [21], surgical volume [22] and neuromuscular disorders [23]. In the present study, diagnosis of disease-, sex- and age -matched patients without dislocation after THA were selected as the control group. No patients with neurologic disease and alcoholism were found. None of the patients in the dislocation group had BMI >30 or ASA classification score ≥3. Those surgeries were performed by high-volume surgeons in the same approach and posterior soft tissue repair. After that, the authors believed that the interference from other risk factors mentioned previously has been removed.
The total dislocation rate (0.89%) reported in this study was actually lower than that in the published literature [24]. The Dorr dislocation Type I [25], called “postural dislocation”, was rare. The authors assume that some new risk factors, which may not be identified yet, can lead to the instability of hip prosthesis in these relatively “safe patients”.
In the present study, a nested case–control design was used, which was first reported by, an American epidemiologist, Mantel [26] in 1973. This method is a combination of cohort and case–control research. The advantages of the nested case–control design are data collection before diagnosis, small selection bias and small information bias. The patients included in the dislocation and control groups were selected from the same cohort and were with good comparability. It is known that the OR is approximately equal to the relative risk when the complication rate is low [26].
After univariate analysis, either AD (P = 0.28) or MML (P = 0.30) showed no significant difference between the two groups. Then, AD and MLL were combined as one factor. The authors assumed that adduction muscle was tightened after THA with MLL, which might force the femur in the adduction position. Abductor tension also increases after MLL (specifically 2 cm, neither 1 cm nor more than 3 cm); however, this might be less than adductor tension in patients with preoperative AD. On the other hand, the injured gluteus muscle (gluteus maximus) might lead to decreased abduction torque postoperatively. In this way, the hip joint tended to remain in the adducted position to relax the whole envelope, which led to hip instability, which was shown in Fig. 3. The newly found factor impacted the prosthesis stability (P < 0.01). The authors believe that AD + MLL would result in “soft tissue imbalance” around the hip joint, which is different from soft tissue laxity (Dorr dislocation Type II). The authors suggested that the AD should be corrected by percutaneous adductor release or limited adductor tenotomy in THA with MLL of 2 cm.
Figure 3.
Dislocation caused by “soft tissue imbalance” around hip. The combination of preoperative AD and postoperative limb lengthening (2 cm) resulted in severe imbalance around the hip joint on the coronal plane. AD = adduction deformity.
Some surgeons try to achieve a stable hip at the cost of slightly increasing the leg length, believing that lengthening extremity can increase hip stability. MLL is defined as the sum of preoperative limb shortening and postoperative limb lengthening but not the final limb discrepancy. After analysis, limb lengthening by 1 cm did not show significant differences, but if leg lengthening reached ≥3 cm, dislocation was rare in both groups. Only the MLL of 2 cm showed significant difference (P < 0.01). Benedetti et al. [27] found that the hip function remained very poor if limb lengthening was ≥2 cm. The authors also agree that leg length discrepancy >1 cm after THA should be avoided.
KV and PO are common deformities, especially in patients with hip dysplasia [28], [29]. In univariate analyses of KV and PO, no significant difference was found between the two groups, but the combination of PO and KV showed a significant difference (P = 0.02). The authors consider that the cause of dislocation was “across joint deformity” around the hip. This result indicated that surgeons should correct the KV deformity before or after THA; meanwhile, they must adequately evaluate PO deformity restoration after THA.
Previous reports have not identified that dislocation is more likely to develop after THA in patients with bilateral pathological hips compared with patients with unilateral disease. The present study supported this assumption (P < 0.05), but the underlying mechanism is still uncertain. The authors speculate that it might be associated with poor function of the contralateral hips and self-protect ability deficiency.
The present study had some limitations. First, a relatively small number of patients were included in this analysis. Second, both acetabular cups and femoral stems should be considered while studying hip dislocation, but the authors had to ignore the effects of femoral stem rotation [30] on hip dislocation because of the limited radiological data. We did not compare the difference between the supine and standing position of hip radiography. Third, the Lewinnek et al. [9] method was used to determine the safe zone, but this method is controversial [31]. Nevertheless, the authors had to work with a definition that could be fitted to the available data. Finally, this research was a retrospective study, and the authors did not evaluate the effects of different intervention on risk factors of hip dislocation. These theoretical assumptions should be proven in future clinical studies.
Conclusions
Dislocation after THA is still a major challenge for surgeons. It is caused by a synergetic effect of multiple factors. The patients with preoperative AD and postoperative MLL are at higher risk for dislocation. The combined KV and PO deformity is another influencing risk factor for hip dislocation. In patients with bilateral pathological hips, dislocation is prone to develop after THA. Awareness of these plain radiography findings to predict dislocation can help surgeons identifying high-risk patients and thereby planning appropriate intervention strategies.
Funding
Not applicable.
Availability of data and materials
All data related to this case report are contained within the manuscript.
Ethical approval and consent to participate
The study was approved by the ethical committees, and all participants provided written informed consent.
Consent for publication
Not applicable.
Conflict of interest
The authors declare that they have no competing interests.
Contributor Information
Qing Liu, Email: liuqing77@sohu.com.
Xiaoguang Cheng, Email: xiao65@263.net.
Dong Yan, Email: bmuyandong@126.com.
Yixin Zhou, Email: 6qq@sina.com.
References
- 1.Lombardi A.V., Jr., Skeels M.D., Berend K.R., Adams J.B., Franchi O.J. Do large heads enhance stability and restore native anatomy in primary total hip arthroplasty? Clinsignifthop Relat Res. 2011;469:1547–1553. doi: 10.1007/s11999-010-1605-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Soohoo N.F., Farng E., Lieberman J.R., Chambers L., Zingmond D.S. Factors that predict short-term complication rates after total hip arthroplasty. Clin Orthop Relat Res. 2010;468:2363–2371. doi: 10.1007/s11999-010-1354-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stroh D.A., Issa K., Johnson A.J., Delanois R.E., Mont M.A. Reduced dislocation rates and excellent functional outcomes with large-diameter femoral heads. J Arthroplasty. 2013;28:1415–1420. doi: 10.1016/j.arth.2012.11.017. [DOI] [PubMed] [Google Scholar]
- 4.Salassa T., Hoeffel D., Mehle S., Tatman P., Gioe T.J. Efficacy of revision surgery for the dislocating total hip arthroplasty: report from a large community registry. Clin Orthop Relat Res. 2014;472:962–967. doi: 10.1007/s11999-013-3344-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dargel J., Oppermann J., Bruggemann G.P., Eysel P. Dislocation following total hip replacement. Dtsch Arztebl Int. 2014;111:884–890. doi: 10.3238/arztebl.2014.0884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zahar A., Rastogi A., Kendoff D. Dislocation after total hip arthroplasty. Curr Rev Musculoskelet Med. 2013;6:350–356. doi: 10.1007/s12178-013-9187-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brooks P.J. Dislocation following total hip replacement: causes and cures. Bone Joint Lett J. 2013;95-B:67–69. doi: 10.1302/0301-620X.95B11.32645. [DOI] [PubMed] [Google Scholar]
- 8.Jaramaz B., DiGioia A.M., 3rd, Blackwell M., Nikou C. Computer assisted measurement of cup placement in total hip replacement. Clin Orthop Relat Res. 1998;354:70–81. doi: 10.1097/00003086-199809000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Lewinnek G.E., Lewis J.L., Tarr R., Compere C.L., Zimmerman J.R. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 10.Noble P.C. Biomechanics of dislocation after total hip replacement. Curr Opin Orthop. 2001;12:79–84. [Google Scholar]
- 11.Dorr L.D., Wolf A.W., Chandler R., Conaty J.P. Classification and treatment of dislocations of total hip arthroplasty. Clin Orthop Relat Res. 1983;173:151–158. [PubMed] [Google Scholar]
- 12.Barrack R.L., Burke D.W., Cook S.D., Skinner H.B., Harris W.H. Complications related to modularity of total hip components. J Bone Joint Surg Br. 1993;75:688–692. doi: 10.1302/0301-620X.75B5.8376421. [DOI] [PubMed] [Google Scholar]
- 13.Lagnaoui R., Begaud B., Moore N., Chaslerie A., Fourrier A., Letenneur L. Benzodiazepine use and risk of dementia: a nested case-control study. J Clin Epidemiol. 2002;55:314–318. doi: 10.1016/s0895-4356(01)00453-x. [DOI] [PubMed] [Google Scholar]
- 14.Widmer K.H. A simplified method to determine acetabular cup anteversion from plain radiographs. J Arthroplasty. 2004;19:387–390. doi: 10.1016/j.arth.2003.10.016. [DOI] [PubMed] [Google Scholar]
- 15.Krenzel B.A., Berend M.E., Malinzak R.A., Faris P.M., Keating E.M., Meding J.B. High preoperative range of motion is a significant risk factor for dislocation in primary total hip arthroplasty. J Arthroplasty. 2010;25:31–35. doi: 10.1016/j.arth.2010.04.007. [DOI] [PubMed] [Google Scholar]
- 16.Al-Amiry B., Mahmood S., Krupic F., Sayed-Noor A. Leg lengthening and femoral-offset reduction after total hip arthroplasty: where is the problem - stem or cup positioning? Acta Radiol. 2017;58:1125–1131. doi: 10.1177/0284185116684676. [DOI] [PubMed] [Google Scholar]
- 17.Guo S.J., Zhou Y.X., Yang D.J., Yang X.C. Lower-limb valgus deformity associated with developmental hip dysplasia. Chin Med J (Engl) 2012;125:3956–3960. [PubMed] [Google Scholar]
- 18.Carrole M., Roberts B.S.N.M.S. How does pelvic rotation or tilt affect radiographic measurement of acetabular component inclination angle during THA? J Orthop. 2015;12:222–227. doi: 10.1016/j.jor.2015.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parvizi J., Tarity T.D., Sheikh E., Sharkey P.F., Hozack W.J., Rothman R.H. Bilateral total hip arthroplasty: one-stage versus two-stage procedures. Clin Orthop Relat Res. 2006;453:137–141. doi: 10.1097/01.blo.0000246529.14135.2b. [DOI] [PubMed] [Google Scholar]
- 20.Wera G.D., Ting N.T., Moric M., Paprosky W.G., Sporer S.M., Della Valle C.J. Classification and management of the unstable total hip arthroplasty. J Arthroplasty. 2012;27:710–715. doi: 10.1016/j.arth.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 21.Khatod M., Barber T., Paxton E., Namba R., Fithian D. An analysis of the risk of hip dislocation with a contemporary total joint registry. Clin Orthop Relat Res. 2006;447:19–23. doi: 10.1097/01.blo.0000218752.22613.78. [DOI] [PubMed] [Google Scholar]
- 22.Meek R.M., Allan D.B., McPhillips G., Kerr L., Howie C.R. Epidemiology of dislocation after total hip arthroplasty. Clin Orthop Relat Res. 2006;447:9–18. doi: 10.1097/01.blo.0000218754.12311.4a. [DOI] [PubMed] [Google Scholar]
- 23.Coventry M.B. Late dislocations in patients with Charnley total hip arthroplasty. J Bone Joint Surg Am. 1985;67:832–841. [PubMed] [Google Scholar]
- 24.Phillips C.B., Barrett J.A., Losina E., Mahomed N.N., Lingard E.A., Guadagnoli E. Incidence rates of dislocation, pulmonary embolism, and deep infection during the first six months after elective total hip replacement. J Bone Joint Surg Am. 2003;85-A:20–26. doi: 10.2106/00004623-200301000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Dorr L.D., Wan Z. Causes of and treatment protocol for instability of total hip replacement. Clin Orthop Relat Res. 1998;355:144–151. doi: 10.1097/00003086-199810000-00015. [DOI] [PubMed] [Google Scholar]
- 26.Mantel N. Synthetic retrospective studies and related topics. Biometrics. 1973;29:479–486. [PubMed] [Google Scholar]
- 27.Benedetti M.G., Catani F., Benedetti E., Berti L., Di Gioia A., Giannini S. To what extent does leg length discrepancy impair motor activity in patients after total hip arthroplasty? Int Orthop. 2010;34:1115–1121. doi: 10.1007/s00264-009-0855-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weinstein S.L. Natural history of congenital hip dislocation (CDH) and hip dysplasia. Clin Orthop Relat Res. 1987;225:62–76. [PubMed] [Google Scholar]
- 29.Zhou X., Wang Q., Zhang X., Chen Y., Shen H., Jiang Y. Effect of pelvic obliquity on the orientation of the acetabular component in total hip arthroplasty. J Arthroplasty. 2012;27:299–304. doi: 10.1016/j.arth.2011.09.022. [DOI] [PubMed] [Google Scholar]
- 30.Biedermann R., Tonin A., Krismer M., Rachbauer F., Eibl G., Stockl B. Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation of the acetabular component. J Bone Joint Surg Br. 2005;87:762–769. doi: 10.1302/0301-620X.87B6.14745. [DOI] [PubMed] [Google Scholar]
- 31.Esposito C.I., Gladnick B.P., Lee Y.Y., Lyman S., Wright T.M., Mayman D.J. Cup position alone does not predict risk of dislocation after hip arthroplasty. J Arthroplasty. 2015;30:109–113. doi: 10.1016/j.arth.2014.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data related to this case report are contained within the manuscript.