Abstract
Background
Accurate knowledge of the intervertebral center of rotation (COR) and its corresponding range of motion (ROM) can help understand development of cervical pathology and guide surgical treatment.
Methods
Ten asymptomatic subjects were imaged using MRI and dual fluoroscopic imaging techniques during dynamic extension-flexion-extension (EFE) and axial left-right-left (LRL) rotation. The intervertebral segment CORs and ROMs were measured from C34 to C67, as the correlations between two variables were analyzed as well.
Results
During the EFE motion, the CORs were located at 32.4 ± 20.6%, -2.4 ± 11.7%, 21.8 ± 12.5% and 32.3 ± 25.5% posteriorly, and the corresponding ROMs were 13.8 ± 4.3°, 15.1 ± 5.1°, 14.4 ± 7.0° and 9.2 ± 4.3° from C34 to C67. The ROM of C67 was significantly smaller than other segments. The ROMs were not shown to significantly correlate to COR locations (r = −0.243, p = 0.132). During the LRL rotation cycle, the average CORs were at 85.6 ± 18.2%, 32.3 ± 25.3%, 15.7 ± 12.3% and 82.4 ± 31.3% posteriorly, and the corresponding ROMs were 3.5 ± 1.7°, 6.9 ± 3.8°, 9.6 ± 4.1° and 2.6 ± 2.5° from C34 to C67. The ROMs of C34 and C67 was significantly smaller than those of C45 and C56. A more posterior COR was associated with a less ROM during the neck rotation (r = −0.583, p < 0.001). The ROMs during EFE were significantly larger than those during LRL in each intervertebral level.
Conclusion
The CORs and ROMs of the subaxial cervical intervertebral segments were segment level- and neck motion-dependent during the in-vivo neck motions.
The translational potential of this article
Our study indicates that the subaxial cervical intervertebral CORs and ROMs were segment level- and neck motion-dependent. This may help to improve the artificial disc design as well as surgical technique by which the neck functional motion is restored following the cervical arthroplasty.
Keywords: Center of rotation, Cervical spine, Intervertebral segments, In-vivo spine kinematics, Range of motion, Total disc replacement
Introduction
The subaxial cervical spine is the most mobile region of the cervical spine, allowing positioning of the head in a multitude of positions for various activities of daily living. As the discs degenerate, the relationship between alteration in kinematics, resting alignment and symptom development is not clear. Surgical treatment of disc degeneration not responding to conservative measures with anterior cervical discectomy with fusion has been the gold standard although concern remains regarding development of adjacent segment disease [1]. Although total disc replacement (TDR) and other motion-preserving technologies are becoming popular alternatives that are capable of restoring the cervical spine motion [2], [3], [4], [5], recent follow-up studies indicated that symptomatic adjacent segment degeneration is not eliminated and reoperation rates of approximately 9% were reported at 24 months after surgery [6], [7], [8]. The complications after TDR surgery are thought to be caused by inadequate restoration of the in vivo intervertebral kinematics of the affected segments [9], [10], [11]. Simply understanding ranges of motion (ROMs) does not capture the quality of normal cervical motion, nor does it allow appreciation for the change in the quality of motion associated with disease development and restoration of quality motion through surgical treatment.
Previous studies of cervical spine kinematics have mostly focused on the intervertebral ROMs [12], [13], [14], [15], [16], [17], [18], [19]. However, there is no consensus on the “needed” ROM to provide a physiological load-sharing function to the adjacent segment [20]. In addition to the ROM studies, the quality of cervical vertebral kinematics (e.g., center of rotation [COR]) is another important variable that affects the spinal function. CORs of the intervertebral segments have been investigated using cadaveric specimens and finite element analyses under simulated loading conditions or using static 2D radiographs at selected postures of living individuals [21], [22], [23], [24], [25], [26]. Penning [22] reported the first normative data on sagittal plane CORs, showing that the lower segments have CORs located closer to the corresponding intervertebral centres. Amevo et al. [23] showed that the CORs were positioned posteriorly against the endplate centre. In addition, studying CORs by only investigating the extreme ends of motion is likely to be subject to measurement error. Recently, biplane radiographic technique was used to investigate the instantaneous CORs of individual cervical vertebra during dynamic flexion-extension of the neck [27] and showed that the COR locations of C23 to C67 segments moved anteriorly with neck flexion [28].
For clinical problems such as the artificial disc dislocation and unavoidable adjacent segment disease (ASD), it is difficult to explain appropriately based on the relative motion of adjacent vertebrae. In artificial disc replacement, the geometry of the articulating surfaces is one of the most important design features for its functioning, stability, wear characteristics and longevity [29]. Therefore, knowledge on the relative motion of upper and lower endplates between the index disc space should be critical for the artificial disc development. No data have been reported on the relationship between the intervertebral segmental CORs and the corresponding ROMs of the cervical spine during various functional activities of the neck. This knowledge is vital to optimize the surgical treatments of cervical spine diseases [30].
The primary goal of the present study was to describe the intervertebral segment COR locations and the corresponding ROMs of the subaxial cervical spine of asymptomatic patients during two dynamic functional neck motions: 1) from maximal extension to maximal flexion and then back to maximal extension motion and 2) axial rotation from maximal left to maximal right positions and then back to maximal left position. Specifically, we determined the relationship between the COR locations and ROMs of the cervical intervertebral segments. We hypothesize that the locations of the CORs and the ROMs are correlated during EFE and LRL motions in asymptomatic healthy cervical spines.
Materials and methods
Patient selection
Ten asymptomatic patients (6 males and 4 females; age: 40.3 ± 10.9 years; body mass index: 24.6 ± 3.2 kg/m2) were recruited for the study of in vivo cervical spine kinematics with the approval of the institutional review board. Patients with chronic neck pain or other spinal disorders that affect neck functional motion were excluded. Written consent was obtained from all patients before participation in the study. The CORs and ROMs of intervertebral segments (C34, C45, C56 and C67) of each patient were investigated.
Three-dimensional vertebral models
Each patient was scanned in a supine, relaxed position using a 3-T MRI scanner (MAGNETOM Trio; Siemens, Erlangen, Germany) with a spine coil and a proton density–weighted sequence. Three-dimensional (3D) models of the vertebrae from C3 to C7 were constructed using the magnetic resonance images [31] using a solid modelling software (3D slicer, MIT Artificial Intelligence Lab and Brigham and Women's Hospital, Boston, MA) [32].
Invivo cervical spine kinematics
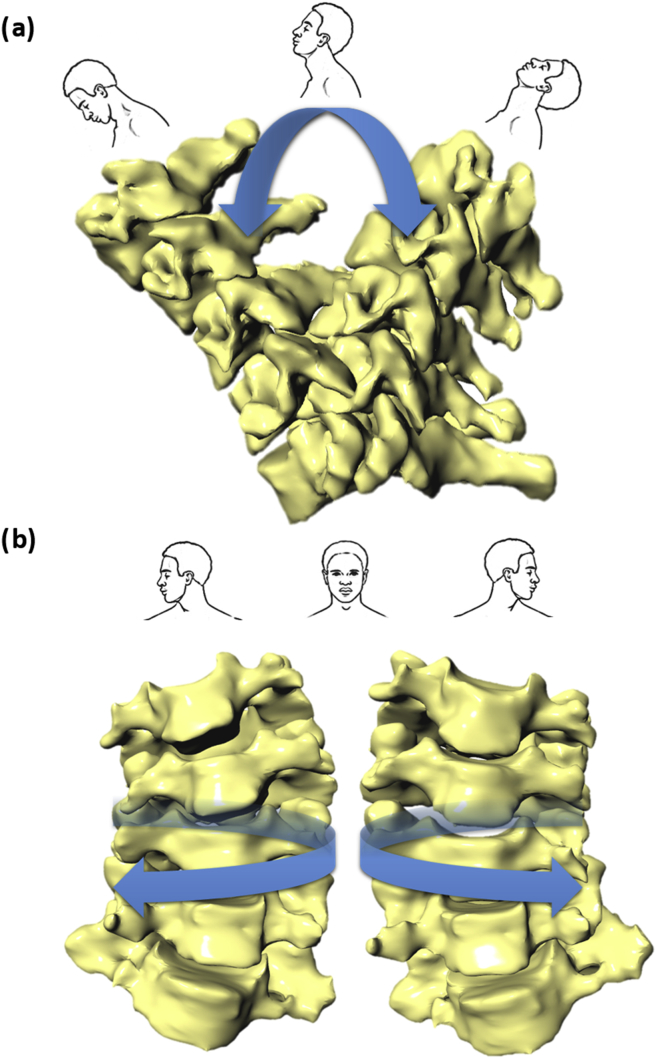
The dual fluoroscopic imaging system (DFIS) was used to capture the cervical spine motion [33], [34]. The DFIS consists of two fluoroscopes (BV Pulsera; Phillips, Bothell, WA, USA) with their imaging intensifiers positioned perpendicular to each other. During the experiment, the patient sat and moved the neck within the field of view of the two fluoroscopes. The neck was imaged while the patient was performing two functional neck motions: 1) extension-flexion-extension (EFE) motion (from maximal extension position to maximal flexion and then extend to maximal extension position) and 2) left-right-left (LRL) rotation (axial rotation from maximal left position to maximal right position and then twisting back to maximal left position) (Figure 1). The images were captured with a frame rate of 30 Hz and an 8-ms pulse. Each patient was exposed to ∼0.08-mSv radiation dosage in this study.
Figure 1.
(A) The 3D cervical vertebral models and invivo cervical spine motion showing extension-flexion-extension (EFE) motion; (B) the 3D cervical vertebral models and in-vivo cervical spine motion showing axial left-right-left (LRL) rotation.
The pairs of fluoroscopic images captured during the neck motion were input into a solid modelling software (Rhinoceros; Robert McNeel & Associates, Seattle, WA, USA) and positioned as virtual imaging intensifiers for construction of a virtual DFIS that reproduces the actual DFIS setup [33], [34], [35]. The 3D magnetic resonance–based vertebral models were introduced into the virtual DFIS environment and viewed from two virtual cameras that represent the two X-ray sources of the actual DFIS. Each vertebral model could be translated and rotated independently in six degrees of freedom until their projections on the virtual imaging intensifiers matched the corresponding images captured during the experiment to reproduce the actual in vivo vertebral locations. The C1 and C2 vertebrae were not studied as their images were obscured by the skull and mandible. This technique has been validated by the roentgen stereophotogrammetric analysis technique as the gold standard to have a submillimeter accuracy in measurement of dynamic cervical motion [34].
Definition of the CORs and ROMs of the cervical intervertebral segments
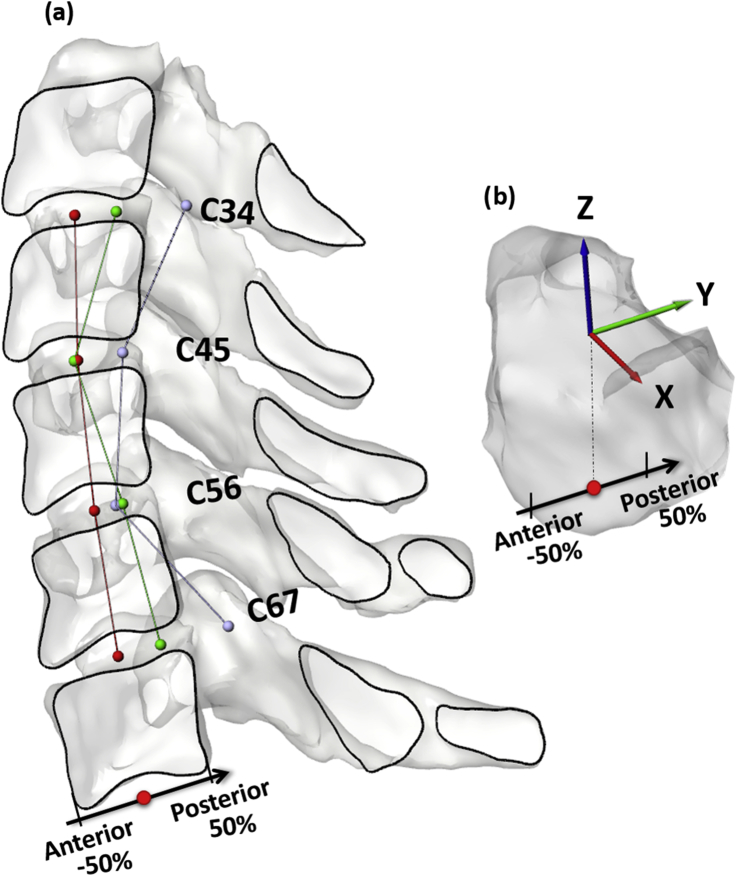
The relative coordinate systems of the two endplate surfaces of each intervertebral segment (C34, C45, C56 and C67) (Figure 2-a) were used to calculate the intervertebral segment kinematics [34]. The x-axis was defined towards left, and the y-axis was posteriorly directed to spinous process as x-y plane was parallel to the endplate surface. The geometric centre of each endplate was chosen as the origin of the corresponding coordinate system. The z-axis was defined in the cephalic direction as perpendicular to the x-y plane. For each intervertebral segment, the coordinate system of the upper endplate surface of the inferior vertebra was used as a reference for calculation of the relative motion of the lower endplate of the superior vertebra (Figure 2-b). The static standing neutral posture was used as a reference for calculation of the intervertebral segment motion.
Figure 2.
(A) The average intervertebral segment COR locations are calculated using the endplate coordinate systems. The red spheres represent the geometric centres of the intervertebral segments, the green spheres represent the average CORs during the flexion-extension motion and the purple spheres represent the average CORs during the left-right rotation of each intervertebral segment; (B) the coordinate system of an endplate. The upper endplate surface of the inferior vertebra was used as a reference for calculation of the relative motion of the lower endplate of the superior vertebra at each intervertebral segment.
To define the intervertebral segment CORs, the anterior-posterior (AP) axis of the lower endplate of the superior vertebra was projected onto the primary motion plane of the reference coordinate system of the upper endplate of inferior vertebra. The intersection of the projections of the axes of two consecutive motions was represented as the COR of the intervertebral segment [35], [36], [37]. The COR location was measured as the distance to the geometric centre of the intervertebral segment. The COR was defined positive when posterior and negative when anterior to the intersegment centre. In this study, the COR was normalized to the AP dimension of the intervertebral disc [38] (Figure 2-b).
For the EFE neck motion, the CORs and ROMs were measured during the motion from full extension to flexion position, and the CORs and ROMs were also measured as the patients moved from the full flexion position to the full extension position. The averages of the CORs and ROMs of each intervertebral segment during the motion cycle were defined as the COR and ROM of the segment. The COR and ROM were similarly calculated for each intersegment during the LRL neck motion.
Statistics
To test the differences in COR locations and the ROMs of the 4 intervertebral segments during the EFE motion and LRL rotation, two-way repeated-measures analysis of variance and the Newman–Keuls post hoc test were performed. To test the difference in COR and ROM between motions, paired t test was performed for each segment. A Pearson's correlation between COR locations and the corresponding ROMs were analyzed statistically. The significance was defined when p < 0.05 for all tests.
Results
Intervertebral disc dimensions
The disc dimensions of C34 to C67 levels were similar in the AP direction (Table 1). In the medial-lateral direction, the C67 was significantly longer than other segments (p < 0.001). In the proximal-distal direction, the C67 was lower, but not significantly different compared with the other segments.
Table 1.
Intervertebral disc dimensions (mm) measured at the static neutral position of the patients.
| Disc level | Intervertebral disc dimensions |
||
|---|---|---|---|
| AP | ML | SI | |
| C34 | 17.3 ± 1.9 | 16.4 ± 1.5 | 4.1 ± 0.9 |
| C45 | 17.7 ± 1.6 | 16.6 ± 1.5 | 4.2 ± 0.9 |
| C56 | 17.8 ± 1.8 | 17.7 ± 1.5 | 4.2 ± 0.8 |
| C67 | 18.2 ± 1.9 | 21.0 ± 2.3a | 3.7 ± 0.5 |
AP = anterior-posterior; ML = medial-lateral; SI = superior-inferior.
Represents the statistically significant difference between C67 and other levels.
Intervertebral segmental CORs and ROMs
EFE motion
The average CORs were located at 32.4 ± 20.6%, −2.4 ± 11.7%, 21.8 ± 12.5% and 32.3 ± 25.5% posterior to the centre of the vertebral body for C34, C45, C56 and C67 segments, respectively (Table 2) (Figure 2-a). The COR of C45 was significantly more anterior to its intervertebral centre than the other intervertebral segments (p < 0.001). The ROMs of the 4 intervertebral segments were 13.8 ± 4.3°, 15.1 ± 5.1°, 14.4 ± 7.0° and 9.2 ± 4.3° (Table 2). The ROM of C67 was significantly less than the other 3 segments.
Table 2.
The average intervertebral segment COR locations (%) and angular ROMs (°) of the cervical spine during the EFE motion and LRL rotation.
|
COR |
C34a |
C45a |
C56 |
C67a |
| EFE motion (a, d, e) | 32.4 ± 20.6 | −2.4 ± 11.7 | 21.8 ± 12.5 | 32.3 ± 25.5 |
|
LRL rotation (a, b, d, e, f) |
85.6 ± 18.2 |
32.3 ± 25.3 |
15.7 ± 12.3 |
82.4 ± 31.3 |
|
ROM |
C34a |
C45a |
C56a |
C67a |
| EFE motion (c, e, f) | 13.8 ± 4.3 | 15.1 ± 5.1 | 14.4 ± 7.0 | 9.2 ± 4.3 |
| LRL rotation (b, f) | 3.5 ± 1.7 | 6.9 ± 3.8 | 9.6 ± 4.1 | 2.6 ± 2.5 |
EFE = extension-flexion-extension; LRL = left-right-left; ROM = range of motion.
Significant differences between different intervertebral segments when p < 0.05: a for C34 vs. C45, b for C34 vs. C56, c for C34 vs. C67, d for C45 vs. C56, e for C45 vs. C67 and f for C56 vs. C67.
Represents the statistically significant difference between EFE motion and LRL rotation.
LRL rotation
The average CORs were located at 85.6 ± 18.2%, 32.3 ± 25.3%, 15.7 ± 12.3% and 82.4 ± 31.3% posterior to the centre of the vertebral body for C34, C45, C56 and C67 segments, respectively (Table 2) (Figure 2-a). The average COR locations of the C34 and C67 were not significantly different from each other (p = 0.568), and both were out of the posterior edges of their discs. The COR of C56 was significantly closer to its intervertebral centre than other segments (p < 0.003). The ROMs of the 4 intervertebral segments were 3.5 ± 1.7°, 6.9 ± 3.8°, 9.6 ± 4.1° and 2.6 ± 2.5° (Table 2). The ROM of C56 was significantly larger than other segments (p < 0.008) except the C45 (p = 0.173).
Comparison of EFE motion and LRL rotation
The CORs of C34, C45 and C67 were more posteriorly positioned during the LRL rotation than during the EFE motion (p < 0.05) (Table 2). The positions of the CORs of C56 were not significantly different during the two neck motions (p > 0.05). The ROMs of each intervertebral segment during the EFE motion were significantly larger than during the LRL rotation (p < 0.05) (Table 2).
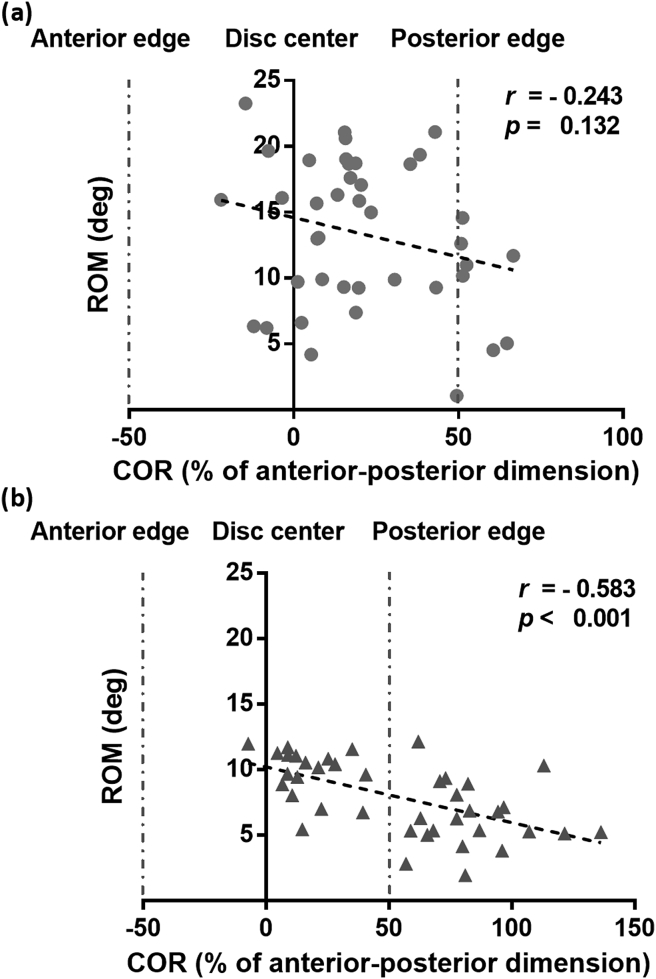
Correlation of COR locations and corresponding ROMs during EFE and LRL neck motions
Generally, a closer COR to the disc centre corresponds to a larger ROM (Figure 3). There was no significant correlation (r = −0.243, p = 0.132) between the posterior COR positions and the corresponding ROMs of all intervertebral segments of C34 to C67 during the EFE neck motion (Figure 3-a). During the LRL neck rotation, there was a negative correlation (r = −0.583, p < 0.001) between these two variables (Figure 3-b).
Figure 3.
(A) The correlations between the COR locations (%) and corresponding ROMs (°) during the EFE motion of the neck; (B) the correlations between the COR locations (%) and corresponding ROMs (○) during the LRL rotation of the neck. The “0” on the COR axis represents the location of disc centre. The −50% represents the anterior edge of disc, whereas the +50% represents the posterior edge of disc. EFE = extension-flexion-extension; LRL = left-right-left; ROM = range of motion.
Discussion
This study found that the CORs of C45 and C56 are closer to the intervertebral centres than those of C34 and C67 during the EFE motion and LRL rotation of the neck. The CORs are more posteriorly positioned during the LRL rotation than during the EFE motion at all segments except the C56 level. The ROM of each intervertebral segment is larger during the EFE motion than during the LRL rotation. Generally, a closer position of the COR to the intervertebral centre corresponds to a larger ROM. These data were consistent with our hypothesis that the locations of the CORs are segment specific and neck motion dependent in asymptomatic healthy cervical spines.
Previous studies have investigated the CORs of the cervical vertebral columns primarily during the flexion-extension motion of the neck [22], [23], [24], [25], [26], [27], [28]. The CORs were generally shown to be close but posterior to the endplate centres via measurement of plain radiographs captured at static flexion and extension postures [22], [23]. In a recent study of the instantaneous CORs of the cervical vertebrae during dynamic neck flexion-extension motion, the mean locations of the CORs measured from the inferior vertebral body centres were found to change increasingly posteriorly from C34 to C67 during the flexion-extension of the neck [28]. In general, our data were consistent with the data reported in literature on neck flexion-extension. However, our data showed that the mean intervertebral segmental COR of the C45 was slightly anterior to the disc centre (−2.4%) during the flexion-extension of the neck. It is difficult to make a direct comparison between various studies of cervical spine because different studies used different experimental setups and measured the intervertebral motion using different methods. No data have been reported on the cervical intervertebral segment rotation during neck axial rotation.
The data found in this study may have interesting clinical implications. Most contemporary TDRs were designed using the ball–socket joint concept that has designed articulation path of the device [39], [40], [41]. This mechanical design concept may not be compatible to the large range of COR location variations as shown at different intervertebral segments and during different neck motions. For example, Duggal et al. [42] found that a TDR at C56 could result in significant increases in global spinal ROM compared with preoperative evaluations in a patient follow-up study. Skeppholm et al. [43] investigated the intervertebral ROM using an in vivo computed tomography study and reported that the treated intervertebral ROM of the C56 was similar to that of the C45 but statistically larger than that of the C67. This could be explained by the fact that the CORs of C56 were located close to the intervertebral centre. Our data and the findings of Dvorak et al. [44] also showed that the C56 and C45 were the more mobile than other levels in the subaxial cervical spine.
However, our data also indicated that the COR locations of the C34 and C67 were more posterior than C45 and C56 during rotations of the neck. In general, a more posteriorly positioned COR corresponded to a smaller ROM. Therefore, to achieve a large ROM, the TDR may need to be positioned close to the intervertebral segment centre. Current TDRs may not be suitable for treatment of C34 and C67 as it is difficult to achieve the posterior CORs of the two segments using these devices. No study has compared the clinical outcome of cervical TDRs when applied to different segments. Future improvement of motion preservation treatments for cervical diseases may need to consider the variations of motion characteristics of different intervertebral segments during different neck motions.
There are several limitations to this study. First, C12 and C23 were not included in the analysis because of the obstruction of their images by the mandibular and occipital bones in certain postures along the neck motion path. Second, only 10 asymptomatic patients were investigated with age ranged from 30 to 59 years. Future studies should include more patients with a wider range of age to investigate the effects of age on cervical spine biomechanics. Finally, we investigated the intervertebral segment CORs of the cervical spine during two functional neck motions. In future, the cervical spine should also be investigated during dynamic walking, the most common loading condition experienced during daily life.
Conclusion
This study investigated the intervertebral segmental CORs and ROMs of the subaxial cervical spine during two neck functional motions. The locations of the CORs during the dynamic EFE motion and axial LRL rotation were shown to be segment level specific and neck motion dependent. The intervertebral segmental CORs of C45 and C56 were located closer to the geometric centres than those of C34 and C67. The ROMs were larger during the EFE motion than during the LRL rotation at each intervertebral level. A more posteriorly positioned COR was corresponding to a smaller ROM during the LRL rotation. The data obtained in this study could provide insights into the improvement of motion preservation prosthesis design and surgical implantation techniques that is aimed to restore normal neck function and prevent adjacent segment degeneration after the cervical spine surgery.
Author contributions statement
Each of the coauthors has involved in the design of the study, data analyses, interpretation of data and writing of the manuscript. All authors have read and approved the final submitted manuscript.
Ethical review committee statement
This research was approved by the Partners Human Research Committee (Protocol Number: 2012P002508/MGH).
Conflicts of interest statement
There is no conflict of interest to declare.
Acknowledgements
This study has been supported by the National Institutes of Health (R21AR057989), K2M Group Holdings, Inc., National Natural Science Foundation of China (No. 81873774), Shanghai Rising-Star Program (No. 18QA1403800) and Guizhou provincial people's hospital doctor's fund (GZSYBS[2017]12).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jot.2018.12.002.
Contributor Information
Liming Cheng, Email: chlm.d@163.com.
Guoan Li, Email: gli1@partners.org.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.Garringer S.M., Sasso R.C. Safety of anterior cervical discectomy and fusion performed as outpatient surgery. J Spinal Disord Tech. 2010;23(7):439–443. doi: 10.1097/BSD.0b013e3181bd0419. [DOI] [PubMed] [Google Scholar]
- 2.Radcliff K., Coric D., Albert T. Five-year clinical results of cervical total disc replacement compared with anterior discectomy and fusion for treatment of 2-level symptomatic degenerative disc disease: a prospective, randomized, controlled, multicenter investigational device exemption clinical trial. J Neurosurg Spine. 2016;25(2):213–224. doi: 10.3171/2015.12.SPINE15824. [DOI] [PubMed] [Google Scholar]
- 3.Delamarter R.B., Zigler J. Five-year reoperation rates, cervical total disc replacement versus fusion, results of a prospective randomized clinical trial. Spine (Phila Pa 1976) 2013;38(9):711–717. doi: 10.1097/BRS.0b013e3182797592. [DOI] [PubMed] [Google Scholar]
- 4.Robertson J.T., Papadopoulos S.M., Traynelis V.C. Assessment of adjacent-segment disease in patients treated with cervical fusion or arthroplasty: a prospective 2-year study. J Neurosurg Spine. 2005;3(6):417–423. doi: 10.3171/spi.2005.3.6.0417. [DOI] [PubMed] [Google Scholar]
- 5.Zigler J.E., Delamarter R., Murrey D., Spivak J., Janssen M. ProDisc-C and anterior cervical discectomy and fusion as surgical treatment for single-level cervical symptomatic degenerative disc disease: five-year results of a Food and Drug Administration study. Spine (Phila Pa 1976) 2013;38(3):203–209. doi: 10.1097/BRS.0b013e318278eb38. [DOI] [PubMed] [Google Scholar]
- 6.Ren C., Song Y., Xue Y., Yang X. Mid- to long-term outcomes after cervical disc arthroplasty compared with anterior discectomy and fusion: a systematic review and meta-analysis of randomized controlled trials. Eur Spine J. 2014;23(5):1115–1123. doi: 10.1007/s00586-014-3220-3. [DOI] [PubMed] [Google Scholar]
- 7.Verma K., Gandhi S.D., Maltenfort M., Albert T.J., Hilibrand A.S., Vaccaro A.R. Rate of adjacent segment disease in cervical disc arthroplasty versus single-level fusion: meta-analysis of prospective studies. Spine (Phila Pa 1976) 2013;38(26):2253–2257. doi: 10.1097/BRS.0000000000000052. [DOI] [PubMed] [Google Scholar]
- 8.Blumenthal S.L., Ohnmeiss D.D., Guyer R.D., Zigler J.E. Reoperations in cervical total disc replacement compared with anterior cervical fusion: results compiled from multiple prospective food and drug administration investigational device exemption trials conducted at a single site. Spine (Phila Pa 1976) 2013;38(14):1177–1182. doi: 10.1097/BRS.0b013e31828ce774. [DOI] [PubMed] [Google Scholar]
- 9.Anderst W.J., Donaldson W.F., 3rd, Lee J.Y., Kang J.D. Three-dimensional intervertebral kinematics in the healthy young adult cervical spine during dynamic functional loading. J Biomech. 2015;48(7):1286–1293. doi: 10.1016/j.jbiomech.2015.02.049. [DOI] [PubMed] [Google Scholar]
- 10.Heidecke V., Burkert W., Brucke M., Rainov N.G. Intervertebral disc replacement for cervical degenerative disease--clinical results and functional outcome at two years in patients implanted with the Bryan cervical disc prosthesis. Acta Neurochir (Wien) 2008;150(5):453–459. doi: 10.1007/s00701-008-1552-7. discussion 59. [DOI] [PubMed] [Google Scholar]
- 11.Kim S.W., Shin J.H., Arbatin J.J., Park M.S., Chung Y.K., McAfee P.C. Effects of a cervical disc prosthesis on maintaining sagittal alignment of the functional spinal unit and overall sagittal balance of the cervical spine. Eur Spine J. 2008;17(1):20–29. doi: 10.1007/s00586-007-0459-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miyazaki M., Hymanson H.J., Morishita Y., He W., Zhang H., Wu G. Kinematic analysis of the relationship between sagittal alignment and disc degeneration in the cervical spine. Spine (Phila Pa 1976) 2008;33(23):E870–E876. doi: 10.1097/BRS.0b013e3181839733. [DOI] [PubMed] [Google Scholar]
- 13.Dmitriev A.E., Cunningham B.W., Hu N., Sell G., Vigna F., McAfee P.C. Adjacent level intradiscal pressure and segmental kinematics following a cervical total disc arthroplasty: an in vitro human cadaveric model. Spine (Phila Pa 1976) 2005;30(10):1165–1172. doi: 10.1097/01.brs.0000162441.23824.95. [DOI] [PubMed] [Google Scholar]
- 14.Schwab J.S., Diangelo D.J., Foley K.T. Motion compensation associated with single-level cervical fusion: where does the lost motion go? Spine (Phila Pa 1976) 2006;31(21):2439–2448. doi: 10.1097/01.brs.0000239125.54761.23. [DOI] [PubMed] [Google Scholar]
- 15.Brodke D.S., Klimo P., Jr., Bachus K.N., Braun J.T., Dailey A.T. Anterior cervical fixation: analysis of load-sharing and stability with use of static and dynamic plates. J Bone Jt Surg Am. 2006;88(7):1566–1573. doi: 10.2106/JBJS.E.00305. [DOI] [PubMed] [Google Scholar]
- 16.Davies M.A., Bryant S.C., Larsen S.P., Murrey D.B., Nussman D.S., Laxer E.B. Comparison of cervical disk implants and cervical disk fusion treatments in human cadaveric models. J Biomech Eng. 2006;128(4):481–486. doi: 10.1115/1.2205373. [DOI] [PubMed] [Google Scholar]
- 17.Anderst W.J., Baillargeon E., Donaldson W.F., 3rd, Lee J.Y., Kang J.D. Validation of a noninvasive technique to precisely measure in vivo three-dimensional cervical spine movement. Spine (Phila Pa 1976) 2011;36(6):E393–E400. doi: 10.1097/BRS.0b013e31820b7e2f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anderst W.J. Bootstrap prediction bands for cervical spine intervertebral kinematics during in vivo three-dimensional head movements. J Biomech. 2015;48(7):1270–1276. doi: 10.1016/j.jbiomech.2015.02.054. [DOI] [PubMed] [Google Scholar]
- 19.Morishita Y., Hida S., Miyazaki M., Hong S.W., Zou J., Wei F. The effects of the degenerative changes in the functional spinal unit on the kinematics of the cervical spine. Spine (Phila Pa 1976) 2008;33(6):E178–E182. doi: 10.1097/BRS.0b013e318166f059. [DOI] [PubMed] [Google Scholar]
- 20.Mehren C., Heider F., Sauer D., Kothe R., Korge A., Hitzl W. Clinical and radiological outcome of a new total cervical disc replacement design. Spine (Phila Pa 1976) 2018 doi: 10.1097/BRS.0000000000002799. [DOI] [PubMed] [Google Scholar]
- 21.Mo Z., Zhao Y., Du C., Sun Y., Zhang M., Fan Y. Does location of rotation center in artificial disc affect cervical biomechanics? Spine (Phila Pa 1976) 2015;40(8):E469–E475. doi: 10.1097/BRS.0000000000000818. [DOI] [PubMed] [Google Scholar]
- 22.Penning L. Differences in anatomy, motion, development and aging of the upper and lower cervical disk segments. Clin Biomech (Bristol, Avon) 1988;3(1):37–47. doi: 10.1016/0268-0033(88)90124-6. [DOI] [PubMed] [Google Scholar]
- 23.Amevo B., Worth D., Bogduk N. Instantaneous axes of rotation of the typical cervical motion segments: a study in normal volunteers. Clin Biomech (Bristol, Avon) 1991;6(2):111–117. doi: 10.1016/0268-0033(91)90008-E. [DOI] [PubMed] [Google Scholar]
- 24.Bogduk N., Mercer S. Biomechanics of the cervical spine. I: normal kinematics. Clin Biomech (Bristol, Avon) 2000;15(9):633–648. doi: 10.1016/s0268-0033(00)00034-6. [DOI] [PubMed] [Google Scholar]
- 25.Liu B., Liu Z., VanHoof T., Kalala J., Zeng Z., Lin X. Kinematic study of the relation between the instantaneous center of rotation and degenerative changes in the cervical intervertebral disc. Eur Spine J. 2014;23(11):2307–2313. doi: 10.1007/s00586-014-3431-7. [DOI] [PubMed] [Google Scholar]
- 26.Liu S., Lafage R., Smith J.S., Protopsaltis T.S., Lafage V.C., Challier V. Impact of dynamic alignment, motion, and center of rotation on myelopathy grade and regional disability in cervical spondylotic myelopathy. J Neurosurg Spine. 2015;23(6):690–700. doi: 10.3171/2015.2.SPINE14414. [DOI] [PubMed] [Google Scholar]
- 27.Baillargeon E., Anderst W.J. Sensitivity, reliability and accuracy of the instant center of rotation calculation in the cervical spine during in vivo dynamic flexion-extension. J Biomech. 2013;46(4):670–676. doi: 10.1016/j.jbiomech.2012.11.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anderst W., Baillargeon E., Donaldson W., Lee J., Kang J. Motion path of the instant center of rotation in the cervical spine during in vivo dynamic flexion-extension: implications for artificial disc design and evaluation of motion quality after arthrodesis. Spine (Phila Pa 1976) 2013;38(10):E594–E601. doi: 10.1097/BRS.0b013e31828ca5c7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Staudt M.D., Das K., Duggal N. Does design matter? Cervical disc replacements under review. Neurosurg Rev. 2018;41(2):399–407. doi: 10.1007/s10143-016-0765-0. [DOI] [PubMed] [Google Scholar]
- 30.Galbusera F., Anasetti F., Bellini C.M., Costa F., Fornari M. The influence of the axial, antero-posterior and lateral positions of the center of rotation of a ball-and-socket disc prosthesis on the cervical spine biomechanics. Clin Biomech (Bristol, Avon) 2010;25(5):397–401. doi: 10.1016/j.clinbiomech.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 31.Li G., DeFrate L.E., Park S.E., Gill T.J., Rubash H.E. In vivo articular cartilage contact kinematics of the knee: an investigation using dual-orthogonal fluoroscopy and magnetic resonance image-based computer models. Am J Sports Med. 2005;33(1):102–107. doi: 10.1177/0363546504265577. [DOI] [PubMed] [Google Scholar]
- 32.Fedorov A., Beichel R., Kalpathy-Cramer J., Finet J., Fillion-Robin J.C., Pujol S. 3D slicer as an image computing platform for the quantitative imaging network. Magn Reson Imaging. 2012;30(9):1323–1341. doi: 10.1016/j.mri.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mao H., Driscoll S.J., Li J.S., Li G., Wood K.B., Cha T.D. Dimensional changes of the neuroforamina in subaxial cervical spine during in vivo dynamic flexion-extension. Spine J. 2016;16(4):540–546. doi: 10.1016/j.spinee.2015.11.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yu Y., Mao H., Li J.S., Tsai T.Y., Cheng L., Wood K.B. Ranges of cervical intervertebral disc deformation during an in vivo dynamic flexion-extension of the neck. J Biomech Eng. 2017;139(6) doi: 10.1115/1.4036311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu Z., Tsai T.Y., Wang S., Wu M., Zhong W., Li J.S. Sagittal plane rotation center of lower lumbar spine during a dynamic weight-lifting activity. J Biomech. 2016;49(3):371–375. doi: 10.1016/j.jbiomech.2015.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dennis D.A., Mahfouz M.R., Komistek R.D., Hoff W. In vivo determination of normal and anterior cruciate ligament-deficient knee kinematics. J Biomech. 2005;38(2):241–253. doi: 10.1016/j.jbiomech.2004.02.042. [DOI] [PubMed] [Google Scholar]
- 37.Moro-oka T.A., Hamai S., Miura H., Shimoto T., Higaki H., Fregly B.J. Dynamic activity dependence of in vivo normal knee kinematics. J Orthop Res. 2008;26(4):428–434. doi: 10.1002/jor.20488. [DOI] [PubMed] [Google Scholar]
- 38.Xia Q., Wang S., Kozanek M., Passias P., Wood K., Li G. In-vivo motion characteristics of lumbar vertebrae in sagittal and transverse planes. J Biomech. 2010;43(10):1905–1909. doi: 10.1016/j.jbiomech.2010.03.023. [DOI] [PubMed] [Google Scholar]
- 39.Obernauer J., Landscheidt J., Hartmann S., Schubert G.A., Thome C., Lumenta C. Cervical arthroplasty with ROTAIO(R) cervical disc prosthesis: first clinical and radiographic outcome analysis in a multicenter prospective trial. BMC Muscoskelet Disord. 2016;17:11. doi: 10.1186/s12891-016-0880-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Heller J.G., Sasso R.C., Papadopoulos S.M., Anderson P.A., Fessler R.G., Hacker R.J. Comparison of BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion: clinical and radiographic results of a randomized, controlled, clinical trial. Spine (Phila Pa 1976) 2009;34(2):101–107. doi: 10.1097/BRS.0b013e31818ee263. [DOI] [PubMed] [Google Scholar]
- 41.Li J., Liang L., Ye X.F., Qi M., Chen H.J., Yuan W. Cervical arthroplasty with Discover prosthesis: clinical outcomes and analysis of factors that may influence postoperative range of motion. Eur Spine J. 2013;22(10):2303–2309. doi: 10.1007/s00586-013-2897-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Duggal N., Pickett G.E., Mitsis D.K., Keller J.L. Early clinical and biomechanical results following cervical arthroplasty. Neurosurg Focus. 2004;17(3):E9. doi: 10.3171/foc.2004.17.3.9. [DOI] [PubMed] [Google Scholar]
- 43.Skeppholm M., Svedmark P., Noz M.E., Maguire G.Q., Jr., Olivecrona H., Olerud C. Evaluation of mobility and stability in the Discover artificial disc: an in vivo motion study using high-accuracy 3D CT data. J Neurosurg Spine. 2015;23(3):383–389. doi: 10.3171/2014.12.SPINE14813. [DOI] [PubMed] [Google Scholar]
- 44.Dvorak J., Panjabi M.M., Novotny J.E., Antinnes J.A. In vivo flexion/extension of the normal cervical spine. J Orthop Res. 1991;9(6):828–834. doi: 10.1002/jor.1100090608. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.