Abstract
Background
The Healthy Eating Index (HEI), a diet quality index that measures alignment with the Dietary Guidelines for Americans, was updated with the 2015–2020 Dietary Guidelines for Americans.
Objective and design
To evaluate the psychometric properties of the HEI-2015, eight questions were examined: five relevant to construct validity, two related to reliability, and one to assess criterion validity.
Data sources
Three data sources were used: exemplary menus (n=4), National Health and Nutrition Examination Survey 2011–2012 (N=7,935), and the National Institutes of Health-AARP (formally known as the American Association of Retired Persons) Diet and Health Study (N=422,928).
Statistical analyses
Exemplary menus: Scores were calculated using the population ratio method. National Health and Nutrition Examination Survey 2011–2012: Means and standard errors were estimated using the Markov Chain Monte Carlo approach. Analyses were stratified to compare groups (with t tests and analysis of variance). Principal components analysis examined the number of dimensions. Pearson correlations were estimated between components, energy, and Cronbach’s coefficient alpha. National Institutes of Health-AARP Diet and Health Study: Adjusted Cox proportional hazards models were used to examine scores and mortality outcomes.
Results
For construct validity, the HEI-2015 yielded high scores for exemplary menus as four menus received high scores (87.8 to 100). The mean score for National Health and Nutrition Examination Survey was 56.6, and the first to 99th percentile were 32.6 to 81.2, respectively, supporting sufficient variation. Among smokers, the mean score was significantly lower than among nonsmokers (53.3 and 59.7, respectively) (P<0.01), demonstrating differentiation between groups. The correlation between diet quality and diet quantity was low (all <0.25) supporting these elements being independent. The components demonstrated multidimensionality when examined with a scree plot (at least four dimensions). For reliability, most of the intercorrelations among the components were low to moderate (0.01 to 0.49) with a few exceptions, and the standardized Cronbach’s alpha was .67. For criterion validity, the highest vs the lowest quintile of HEI-2015 scores were associated with a 13% to 23% decreased risk of all-cause, cancer, and cardiovascular disease mortality.
Conclusions
The results demonstrated evidence supportive of construct validity, reliability, and criterion validity. The HEI-2015 can be used to examine diet quality relative to the 2015–2020 Dietary Guidelines for Americans.
Keywords: Healthy Eating Index, Evaluation, Diet quality, Diet indexes, Dietary patterns
THE HEALTHY EATING INDEX (HEI) IS A DIET QUALITY index that measures alignment with the Dietary Guidelines for Americans (DGA).1 As such, it can be used to assess the conformance of any group of foods to the key diet quality recommendations set forth in the DGA. In the past, the HEI has been used to assess diet quality for a variety of research purposes, including epidemiology, population surveillance, and evaluations of food environments, food assistance programs, and nutrition interventions.2–5
With the release of the 2015–2020 DGA, the HEI has been updated to reflect current federal dietary advice through a collaboration between researchers at the National Cancer Institute (NCI) and the US Department of Agriculture (USDA) Center for Nutrition Policy and Promotion (CNPP). The HEI-2015 includes 13 dietary components (Table 1). Nine adequacy components (those recommended for inclusion in a healthy diet) include Total Fruits, Whole Fruits, Total Vegetables, Greens and Beans, Whole Grains, Dairy, Total Protein Foods, Seafood and Plant Proteins, and Fatty Acids. Four moderation components (those that should be consumed sparingly) include Refined Grains, Sodium, Added Sugars, and Saturated Fats. Added Sugars is a newly distinct component in the HEI-2015, added to address new quantitative recommendations to limit added sugars in the diet. With the inclusion of Added Sugars as a distinct component, Empty Calories (a component in the 2010 index)6 was removed and Saturated Fats was reintroduced (from the 2005 index).7 Other details on the changes in the HEI-2015 compared with previous versions have been described elsewhere.8
Table 1.
Healthy Eating Index-2015 components, point values, and standards for scoring
| Component | Maximum points | Standard for maximum score | Standard for minimum score of zero |
|---|---|---|---|
| Adequacy | |||
| Total Fruits | 5 | ≥0.8 c equivalents/1,000 kcal | No fruit |
| Whole Fruits | 5 | ≥0.4 c equivalents/1,000 kcal | No whole fruit |
| Total Vegetables | 5 | ≥1.1 c equivalents/1,000 kcal | No vegetables |
| Greens and Beans | 5 | ≥0.2 c equivalents/1,000 kcal | No dark green vegetables or beans and peas |
| Whole Grains | 10 | ≥1.5 oz equivalents/1,000 kcal | No whole grains |
| Dairy | 10 | ≥1.3 c equivalents/1,000 kcal | No dairy |
| Total Protein Foods | 5 | ≥2.5 oz equivalents/1,000 kcal | No protein foods |
| Seafood and Plant Proteins | 5 | ≥0.8 c equivalents/1,000 kcal | No seafood or plant proteins |
| Fatty Acids | 10 | (PUFAsa+MUFAsb)/SFAsc ≥2.5 | (PUFAs+MUFAs)/SFAs ≤1.2 |
| Moderation | |||
| Refined Grains | 10 | ≤1.8 oz equivalents/1,000 kcal | ≥4.3 oz equivalents/1,000 kcal |
| Sodium | 10 | ≤1.1 g/1,000 kcal | ≥ 2.0 g/1,000 kcal |
| Added Sugars | 10 | ≤6.5% of energy | ≥26% of energy |
| Saturated Fats | 10 | ≤8% of energy | ≥16% of energy |
PUFAs=polyunsaturated fatty acids.
MUFAs=monounsaturated fatty acids.
SFAs=saturated fatty acids.
This article presents the evaluation of the index’s validity and reliability. As done previously, content validity, or how completely the HEI-2015 captures the dimensions of a healthy diet, is explored and reported in the update article.8
METHODS
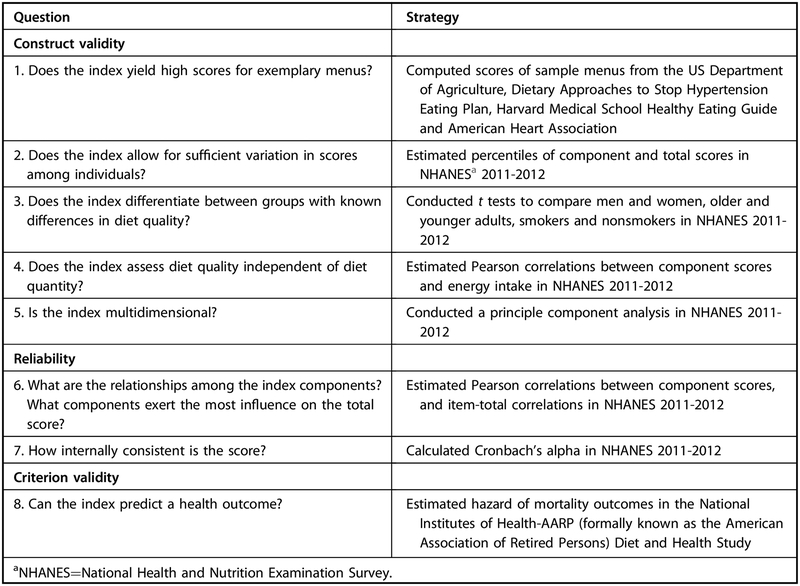
The HEI-2015 was evaluated by assessing its psychometric properties (strategies shown in Figure 1). These included five questions relevant to construct validity, two related to reliability (internal consistency), and one to assess criterion validity.
Figure 1.
Strategies used to evaluate the validity of Healthy Eating Index-2015 (HEI-2015).
Data Sources
To examine these questions, three data sources were used.
Exemplary Menus.
The exemplary menus, which provide benchmarks representative of high-quality diets, were created by nutrition experts at a variety of organizations. Specifically, these included the 7-day 2,000-kcal sample menu from the USDA Food Patterns9 (available by contacting US Department of Agriculture’s Center for Nutrition Policy and Promotion, 3101 Park Center Dr, Suite 1034; Alexandria, VA 22302); 7-day 2,000-kcal sample menu for the National Heart, Lung, and Blood Institute’s Dietary Approaches to Stop Hypertension (DASH) diet10; two sets of 7-day 1,600-kcal and 2,000-kcal sample menus from the Harvard Medical School’s Healthy Eating Guide11; and two 1-day 1,200-kcal and 2,000-kcal sample menus from the 2005 American Heart Association (AHA) No-Fad Diet.12
Nationally Representative Dietary Data.
Data from the 2011–2012 cycle of the What We Eat in America National Health and Nutrition Examination Survey (NHANES),13 conducted by the Centers for Disease Control and Prevention National Center for Health Statistics, were used to enable examination of HEI scores for the US population and of population subgroups. Each cycle of the survey is approved by the National Center for Health Statistics Research Ethics Review Board.
The total sample for 2011–2012 included 9,338 people. Children younger than age 2 years (n=601) and participants without at least one reliable dietary recall (n=939) were excluded. Some of the excluded participants fell into both categories (n=137), and thus the analytic sample included 7,935 participants. Of these, 7,100 completed 2 interviewer-administered 24-hour dietary recalls and 835 completed 1 recall. Analyses with adults aged 20 years and older included 4,797 participants (of these, 4,305 completed 2 recalls and 492 completed 1 recall). Nutrient data from the NHANES survey are derived from the USDA Agricultural Research Service’s Food and Nutrient Database for Dietary Studies (FNDDS) and the Food Patterns Equivalents Database 2011–2012 (FPED 2011–2012). NHANES 2011–2012 data do not include information about salt added at the table, although the dietary database includes assumptions for salt added during cooking.14
Prospective Cohort Data.
Data from the National Institutes of Health-AARP (formally known as the American Association of Retired Persons) (NIH-AARP) Diet and Health Study, a prospective cohort study designed to investigate diet and cancer, were used to examine the relationship between HEI-2015 scores and mortality outcomes as an indicator of predictive validity. AARP members who were between ages 50 and 71 years and who were residents of six states (California, Florida, Louisiana, New Jersey, North Carolina, and Pennsylvania) or two metropolitan areas (Atlanta, GA, and Detroit, MI) were contacted during 1995–1996 to participate; the response rate was 17.6%.15 Of 566,398 satisfactorily completed questionnaires, exclusions were made for questionnaires completed by proxy (n 15,760), respondents with previous cancer (n=55,614) or heart disease (n=68,271), and individuals with extreme energy (kcal) intake (>2 interquartile ranges above the 75th percentile or below the 25th percentile on the logarithmic scale [n=3,825]). The final analytic cohort included 422,928 people. Study participants were followed from enrollment in 1995–1996 through December 2011. Addresses were updated periodically by matching the cohort database to the National Change of Address maintained by the US Postal Service and other address change update services, and by direct communication with participants.16 Vital status was determined by annual linkage of the cohort to the Social Security Administration Death Master File on deaths in the United States, follow-up searches of the National Death Index for participants who correspond to the Social Security Administration Death Master File, cancer registry linkage, and responses to questionnaires and other mailings. The Surveillance Epidemiology and End Results (SEER) coding system was used to investigate cause-specific mortality, including cardiovascular disease (CVD) and cancer mortality.17 The NIH-AARP Diet and Health Study was approved by the Special Studies Institutional Review Board of the NCI.
At baseline, study participants completed the AARP 124-item food frequency questionnaire (AARP-FFQ) to assess dietary intake during the past year.18 The MyPyramid Equivalents Database was merged with the AARP food frequency questionnaire data to derive guidance-based food group equivalents and generate nutrient and energy estimates using the USDA Survey Nutrient Database associated with the Continuing Survey for Food Intake by Individuals 1994–199619 and the Nutrition Data System for Research database (University of Minnesota Nutrition Coordinating Center, 2004).
Statistical Methods
All analyses were performed using SAS software, version 9.4,20 and a two-sided alpha level of .05 was used to indicate statistical significance unless otherwise noted.
Construct Validity
To evaluate construct validity, or how well the score operationalizes a healthy diet as defined by the DGA, the HEI-2015 was examined to determine its ability to yield high scores for exemplary menus, to show variation in the distribution of scores across the US population, to yield a detectable difference in scores in groups of people with different quality diets (also referred to as concurrent criterion validity and known groups validity), to assess diet quality independent of diet quantity, and to capture multiple dimensions of diet. Further details are given below.
Scoring Exemplary Menus.
Updated HEI-2015 component scores and total scores were calculated for the exemplary menus. For this calculation, the population ratio method21 was employed because advice from the DGA is designed to be met over time and this method best encompasses that intent for menu evaluation.
Estimating Distributions of Nationally Representative Dietary Data for the US Population and Subgroups.
The Markov Chain Monte Carlo (MCMC) approach was used to estimate distributions (mean and percentiles) of HEI-2015 and HEI-2010 component and total scores for the US population. The MCMC method, which was first applied to estimate distributions of scores for the HEI-2005, has been described in detail elsewhere.22 Briefly, it is an extension of the NCI method,23,24 and uses a multipart, nonlinear mixed model with correlated random effects to estimate distributions of usual intake, accounting for episodic consumption of some components, covariates, nuisance effects (eg, weekend/weekday or interview sequence), skewness, correlation, and random measurement error.22 The NCI method enabled estimation of distributions of usual intake of both episodically and non-episodically consumed dietary components but were limited to the analysis of only one or two dietary components at a time.25–28 To address this limitation for the use in applications such as the HEI, Zhang and colleagues22 developed an approach that uses MCMC computational methods to simultaneously model multiple food groups and nutrients.
Because the dietary variables are modeled simultaneously in the MCMC method, no dietary constituent (eg, whole fruits) can be contained within another group (eg, total fruits). Therefore, several HEI components were decoupled so they could be included in the MCMC model, resulting in 15 discrete variables for HEI-2015. For example, fruit was modeled as whole fruits and fruit juice. For this analysis with HEI-2015, six of these discrete variables were defined as episodically consumed because more than 10% of recalls had zero intake: whole fruits; fruit juice; dark green vegetables; whole grains; seafood and plant proteins, excluding legumes; and legumes. Nine were classified as nonepisodically consumed: vegetables, excluding dark green vegetables and legumes; refined grains; dairy; meat, poultry, and egg proteins; sodium; monounsaturated fatty acids and poly-unsaturated fatty acids; saturated fats; added sugars; and energy intake. Although energy is a constituent that is included in all components, it does not need to be decoupled for HEI-2015 (for HEI-2010 energy was decoupled as empty calories and nonempty calories). The need to decouple occurs when variables are on the same scale, the variables are included within another, and/or are collinear.
To examine scores for Americans aged 2 years and older, the NHANES 2011–2012 sample was stratified into three groups (children aged 2 to 11 years, males aged 12 years and older, females aged 12 years and older), and covariates were included for sex (for children aged 2 to 11 years only), recall day (first or second recall), day of the week (weekend or weekday), age (2 to 5, 6 to 11, 12 to 19, 20 to 39, 40 to 49, 50 to 59, 60 to 80 years), and race/ethnicity (non-Hispanic white, non-Hispanic black, Asian, Hispanic). To compare scores between groups for adults aged 20 years and older, additional analyses were stratified by sex, age (20 to 39, 40 to 49, 50 to 59, ≥60 years), and smoking status (current smokers vs nonsmokers for adults aged 20 years or older). The MCMC method used both recalls and accounted for correlation of the two recalls within an individual. The approach predicted usual intakes for each dietary constituent for a population of pseudo-individuals based on the parameters estimated from the multivariate model. Next, the variables were combined to create the dietary constituents, ratios were created (for each component and energy), and then the ratios were scored. Finally, means and percentiles were computed for the population of pseudo-individuals (100 per person=793,500), and the step was replicated 16 times using balanced repeated replication to obtain standard errors. Means, percentiles, and standard errors of component and total scores were estimated for the US population and for subgroups. To compare scores between groups, two-group t tests (sex and smoking) and one-way analysis of variance (age) were used. All analyses were appropriately weighted to account for the complex survey structure of NHANES.29
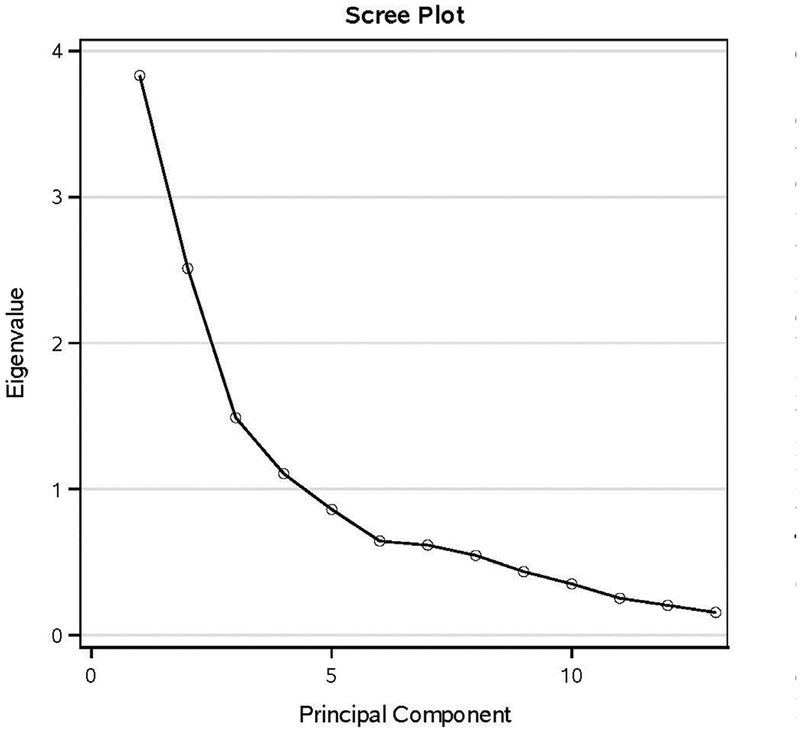
Multidimensionality.
Principal components analysis was used to examine the number of dimensions that emerged from the data, based on the correlations among the components. To determine whether there was one or more than one factor that accounted for the systematic variation observed in the data, the general patterns of the scree plot were examined. In addition, rules for identifying the number of factors, such as eigenvalue >1, were examined.
Reliability (Internal Consistency)
To evaluate reliability in terms of internal consistency (testeretest and interrater reliability were not evaluated), the HEI-2015 was examined to determine the relationships among the components and the degree to which each component influenced the total score, and to assess the internal consistency of the score. The NHANES 2011–2012 data were used to estimate Pearson correlations between items, item-total correlations (correlations between components and the total HEI-2015 score, minus the specified component), and Cronbach’s coefficient alpha.
Criterion Validity
To evaluate criterion validity, the HEI-2015 was examined to determine how well it predicted mortality outcomes.
Prediction of Mortality in the Prospective Cohort Data.
To analyze associations between HEI-2015 scores and mortality outcomes among the NIH-AARP sample, Cox proportional hazards models30 were used with person-years as the underlying time metric to model the hazard of all-cause mortality for men and women separately by HEI quintile. Covariates included age (years), race (white, black, other), education (less than high school, high school, some college, college graduate), body mass index (calculated as kg/m2) (18.5 to <25, 25 to <30, 30 to <35, 35 to <40, ≥40), smoking (never smoker, former smoker of ≤1 pack/day, former smoker of >1 pack/day, current smoker of ≤1 pack/day, current smoker of >1 pack/day), vigorous physical activity (≥20 daily minutes reported rarely or never, 1 to 3 times/month, 1 to 2 times/week, 3 to 4 times/week, ≥5 times/week), energy intake (kcal per day), marital status (married, widowed, divorced, separated, never married), diabetes (yes, no), alcohol use (grams per day), and menopausal hormone therapy (only among women: yes, no). Cancer and CVD mortality were also modeled as separate outcomes using the same covariates. Missing values were included in the model as indicator variables as were valid categories.
RESULTS
Construct Validity
1. Does the Index Yield High Scores for Exemplary Menus?
The four sets of menus scored using the HEI-2015 received total scores ranging from 87.8 to 100 (Table 2). The Dietary Approaches to Stop Hypertension diet received a perfect score. The USDA menus achieved a near-perfect score, with maximum points for all but the Added Sugars component. The Harvard menu received maximum points for all components, except Dairy and Sodium. The AHA menu did not achieve maximum scores for several components, including Greens and Beans, Dairy, Seafood and Plant Proteins, Sodium, and Added Sugars.
Table 2.
Healthy Eating Index-2015 component and total scores for exemplary menus
| Component | Maximum score | USDAa | DASHb | HARVARDc | AHAd |
|---|---|---|---|---|---|
| Total Fruits | 5 | 5 | 5 | 5 | 5 |
| Whole Fruits | 5 | 5 | 5 | 5 | 5 |
| Total Vegetables | 5 | 5 | 5 | 5 | 5 |
| Greens and Beans | 5 | 5 | 5 | 5 | 1.8e |
| Whole Grains | 10 | 10 | 10 | 10 | 10 |
| Dairy | 10 | 10 | 10 | 0.9 | 8.7 |
| Total Protein Foods | 5 | 5 | 5 | 5 | 5 |
| Seafood and Plant Proteins | 5 | 5 | 5 | 5 | 4.8 |
| Fatty Acids | 10 | 10 | 10 | 10 | 10 |
| Refined Grains | 10 | 10 | 10 | 10 | 10 |
| Sodium | 10 | 10 | 10 | 6.9 | 8.3 |
| Saturated Fat | 10 | 10 | 10 | 10 | 10 |
| Added Sugars | 10 | 9.1 | 10 | 10 | 8.4 |
| Total score | 100 | 99.1 | 100 | 87.8 | 92 |
USDA=US Department of Agriculture/USDA Food Patterns. Based on one 7-day 2,000 kcal/day sample menu.9
DASH=Dietary Approaches to Stop Hypertension. Based on one 7-day 2,000 kcal/day sample menu.10
HARVARD=Harvard/Willet. Based on two 7-day 1,600 kcal/day and 2,000 kcal/day sample menus.11
AHA=American Heart Association. Based on two 1-day 1,200 kcal/day and 2,000 kcal/day sample menus.12
Three sets of 14-day 1,200 kcal/day, 1,600 kcal/day, and 2,000 kcal/day sample menus in the most current and updated edition earned a score of 5.0.12
2. Does the Index Allow for Sufficient Variation in Scores among Individuals?
The mean total HEI-2015 score from the MCMC analysis based on NHANES 2011–2012 was 56.6, ranging from 32.6 to 81.2 in the first to the 99th percentiles, respectively (Table 3). Across almost all component scores, the first percentile scores were low, frequently in the 0 to 1 range, whereas the 99th percentile component scores were high, with all components except Sodium reaching maximum scores. At the fifth percentile for each component, component scores were in the 0 to 1 range except for Dairy, Total Protein Foods, and Saturated Fats. At the 95th percentile, most HEI-2015 component scores, with the exception of Whole Grains, Fatty Acids, Sodium, and Saturated Fats, were at maximum values. Values were consistent with the HEI-2010, values for which are also detailed in Table 3 (mean=56.1). The correlation between the HEI-2010 and HEI-2015 total scores was 0.96 (data not shown).
Table 3.
Estimated means in percentiles (p) of Healthy Eating Index-2015 (HEI-2015)a and Healthy Eating Index-2010 (HEI-2010) component and total scores, based on the National Health and Nutrition Examination Survey 2011–2012 (N=7,935)b
| Index | Score | p1 | p5 | p10 | p25 | p50 | p75 | p90 | p95 | p99 |
|---|---|---|---|---|---|---|---|---|---|---|
| mean±standard error | ||||||||||
| HEI-2015 component/total | ||||||||||
| Total Fruits | 2.9±0.07 | 0.1 ±0.04 | 0.4±0.08 | 0.6±0.10 | 1.4±0.12 | 2.8±0.12 | 4.7±0.18 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 |
| Whole Fruits | 3.1±0.10 | 0.0±0.02 | 0.2±0.08 | 0.5±0.12 | 1.5±0.19 | 3.5±0.19 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 |
| Total Vegetables | 3.1 ±0.03 | 1.0±0.11 | 1.4±0.09 | 1.6±0.07 | 2.2±0.04 | 3.0±0.03 | 4.1 ±0.08 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 |
| Greens and Beans | 2.5±0.09 | 0.2±0.06 | 0.5±0.08 | 0.7±0.09 | 1.2±0.09 | 2.1 ±0.11 | 3.7±0.21 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 |
| Whole Grains | 3.0±0.10 | 0.1 ±0.04 | 0.4±0.06 | 0.7±0.07 | 1.4±0.09 | 2.5±0.10 | 4.0±0.14 | 5.8±0.29 | 7.1 ±0.42 | 10.0±0.43 |
| Dairy | 6.5±0.08 | 1.4±0.10 | 2.4±0.11 | 3.0±0.11 | 4.4±0.11 | 6.5±0.11 | 9.0±0.13 | 10.0±0.00 | 10.0±0.00 | 10.0±0.00 |
| Total Protein Foods | 4.6±0.04 | 2.3±0.19 | 3.0±0.15 | 3.5±0.13 | 4.3±0.09 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 |
| Seafood and Plant Proteins | 3.6±0.09 | 0.6±0.10 | 1.1 ±0.13 | 1.5±0.14 | 2.4±0.16 | 4.0±0.18 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 |
| Fatty Acids | 4.6±0.10 | 0.0±0.13 | 1.1 ±0.15 | 1.7±0.13 | 2.9±0.11 | 4.4±0.11 | 6.2±0.13 | 8.0±0.18 | 9.2±0.22 | 10.0±0.00 |
| Refined Grains | 5.9±0.08 | 0.0±0.00 | 1.4±0.21 | 2.6±0.15 | 4.3±0.10 | 6.0±0.09 | 7.8±0.12 | 9.3±0.18 | 10.0±0.02 | 10.0±0.00 |
| Sodium | 4.3±0.06 | 0.0±0.00 | 0.0±0.00 | 0.7±0.12 | 2.6±0.08 | 4.5±0.07 | 6.1 ±0.09 | 7.4±0.14 | 8.2±0.16 | 9.5±0.22 |
| Added Sugars | 6.3±0.09 | 0.0±0.00 | 1.2±0.31 | 2.6±0.25 | 4.6±0.15 | 6.5±0.08 | 8.3±0.08 | 9.7±0.11 | 10.0±0.00 | 10.0±0.00 |
| Saturated Fats | 6.1 ±0.15 | 0.7±0.38 | 2.4±0.30 | 3.3±0.25 | 4.7±0.18 | 6.2±0.14 | 7.7±0.12 | 9.0±0.13 | 9.7±0.14 | 10.0±0.00 |
| Total score | 56.6±0.53 | 32.6±0.59 | 39.1 ±0.55 | 42.8±0.56 | 49.1 ±0.57 | 56.4±0.56 | 63.9±0.62 | 70.9±0.68 | 74.8±0.70 | 81.2±0.74 |
| HEI-2010 component/total | ||||||||||
| Total Fruits | 2.9±0.06 | 0.1 ±0.03 | 0.4±0.06 | 0.7±0.06 | 1.4±0.07 | 2.8±0.09 | 4.7±0.18 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 |
| Whole Fruits | 3.2±0.09 | 0.0±0.02 | 0.2±0.06 | 0.5±0.09 | 1.5±0.15 | 3.6±0.18 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 |
| Total Vegetables | 3.1 ±0.03 | 0.9±0.10 | 1.3±0.08 | 1.5±0.06 | 2.1 ±0.04 | 2.9±0.04 | 4.0±0.09 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 |
| Greens and Beans | 2.1 ±0.07 | 0.0±0.01 | 0.1 ±0.04 | 0.2±0.05 | 0.7±0.05 | 1.7±0.06 | 3.3±0.17 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 |
| Whole Grains | 2.9±0.10 | 0.1 ±0.03 | 0.4±0.05 | 0.7±0.06 | 1.5±0.07 | 2.6±0.10 | 4.0±0.16 | 5.6±0.30 | 6.9±0.44 | 9.7±0.47 |
| Dairy | 6.5±0.08 | 1.4±0.09 | 2.4±0.10 | 3.1 ±0.10 | 4.5±0.11 | 6.4±0.11 | 8.9±0.12 | 10.0±0.00 | 10.0±0.00 | 10.0±0.00 |
| Total Protein Foods | 4.6±0.04 | 2.4±0.20 | 3.0±0.15 | 3.5±0.12 | 4.3±0.11 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 |
| Seafood and Plant Proteins | 3.2±0.11 | 0.2±0.06 | 0.7±0.09 | 1.0±0.11 | 1.9±0.15 | 3.3±0.19 | 5.0±0.02 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 |
| Fatty Acids | 4.7±0.10 | 0.2±0.19 | 1.2±0.16 | 1.8±0.14 | 2.9±0.11 | 4.4±0.11 | 6.2±0.13 | 7.9±0.17 | 9.1 ±0.22 | 10.0±0.00 |
| Refined Grains | 5.9±0.08 | 0.0±0.00 | 1.4±0.24 | 2.5±0.17 | 4.3±0.11 | 6.0±0.08 | 7.8±0.12 | 9.3±0.18 | 10.0±0.02 | 10.0±0.00 |
| Sodium | 4.4±0.06 | 0.0±0.00 | 0.0±0.00 | 0.8±0.12 | 2.7±0.08 | 4.5±0.07 | 6.1 ±0.09 | 7.4±0.12 | 8.2±0.15 | 9.5±0.18 |
| Empty Calories | 12.6±0.16 | 2.8±0.53 | 5.9±0.42 | 7.4±0.36 | 9.9±0.25 | 12.6±0.17 | 15.5±0.19 | 18.2±0.25 | 19.8±0.27 | 20.0±0.00 |
| Total score | 56.1 ±0.50 | 30.7±0.61 | 37.4±0.45 | 41.3±0.43 | 48.0±0.49 | 55.8±0.55 | 63.9±0.69 | 71.5±0.85 | 75.7±0.89 | 82.6±0.88 |
HEI-2015 component and total scores calculated using the index as detailed by Krebs-Smith and colleagues.8
Percentiles are estimated separately for each component in each row (numbers will not sum within columns).
3. Does the Index Differentiate between Groups with Known Differences in Diet Quality?
Women (mean total HEI-2015 score=59.7) had significantly higher HEI-2015 total scores than men (mean total HEI-2015 score=57.2), with significantly higher component scores for Total Fruits, Whole Fruits, Total Vegetables, and Whole Grains (Table 4). Similarly, the means across the age groups were significantly different, with the oldest age groups having a mean score of 62.8 and the youngest age group having a mean score of 55.0, driven by higher scores for eight components, including Total Fruits, Whole Fruits, Total Vegetables, Whole Grains, Seafood and Plant Proteins, Fatty Acids, Refined Grains, and Added Sugars. Finally, the mean total score for nonsmokers (mean total HEI-2015 score=59.7) was significantly higher than the mean total score for current smokers (mean total HEI-2015 score=53.3). Nonsmokers had significantly higher scores for Total Fruits, Whole Fruits, Total Vegetables, Greens and Beans, Whole Grains, Sodium, and Added Sugars compared with smokers.
Table 4.
Estimated mean±standard error of Healthy Eating Index-2015a component and total scores, grouped by sex, age group, and smoking status, based on the National Health and Nutrition Examination Survey 2011–2012
| Component | Men (n = 2,391) | Women (n = 2,406) | Age 20–39 y (n=1,714) | Age ≥60 y (n= 1,501) | Current smokers (n = 983) | Nonsmokers (n = 3,814) |
|---|---|---|---|---|---|---|
| mean±standard error | ||||||
| Total Fruits | 2.3±0.1 | 2.9±0.1b | 2.3±0.1 | 3.2±0.1c | 1.7±0.1 | 2.8±0.1d |
| Whole Fruits | 2.6±0.2 | 3.3±0.1b | 2.5±0.1 | 3.7±0.1c | 1.8±0.2 | 3.2±0.1d |
| Total Vegetables | 3.4±0.1 | 3.8±0.1b | 3.2±0.1 | 3.9±0.1c | 3.0±0.1 | 3.7±0.1d |
| Greens and Beans | 2.7±0.1 | 3.2±0.1 | 2.7±0.2 | 3.0±0.2 | 2.0±0.2 | 3.2±0.1d |
| Whole Grains | 2.9±0.1 | 3.4±0.2b | 2.5±0.1 | 4.1 ±0.2c | 2.2±0.3 | 3.4±0.2d |
| Dairy | 5.4±0.1 | 5.9±0.1 | 5.8±0.1 | 5.8±0.1 | 5.0±0.3 | 5.8±0.1 |
| Total Protein Foods | 4.9±0.0 | 4.8±0.1 | 4.8±0.0 | 4.9±0.0 | 4.8±0.1 | 4.8±0.0 |
| Seafood and Plant Proteins | 4.0±0.1 | 4.0±0.1 | 3.8±0.1 | 4.3±0.1c | 3.6±0.2 | 4.2±0.1 |
| Fatty Acids | 5.3±0.2 | 5.2±0.2 | 4.9±0.2 | 5.7±0.2c | 5.0±0.2 | 5.4±0.1 |
| Refined Grains | 6.5±0.2 | 6.4±0.1 | 5.8±0.2 | 7.1 ±0.2c | 6.8±0.2 | 6.3±0.1 |
| Sodium | 3.9±0.1 | 4.0±0.1 | 4.0±0.1 | 3.9±0.2 | 5.0±0.3 | 3.7±0.1d |
| Added Sugars | 6.7±0.1 | 6.5±0.2 | 6.2±0.1 | 7.0±0.2c | 5.6±0.2 | 6.9±0.1d |
| Saturated Fats | 6.5±0.2 | 6.4±0.2 | 6.5±0.2 | 6.5±0.2 | 6.7±0.4 | 6.4±0.1 |
| Total score | 57.2±0.6 | 59.7±0.6b | 55.0±0.7 | 62.8±1.1c | 53.3±0.9 | 59.7±0.7d |
Healthy Eating Index-2015 component and total scores calculated using the index detailed by Krebs-Smith and colleagues.8
Significantly different from men (P<0.01).
Significantly different from age 20–39 y (P<0.01).
Significantly different from smokers (P<0.01).
4. Does the Index Assess Diet Quality Independent of Diet Quantity?
Correlations between each HEI-2015 component and energy were all low (below 0.25) (Table 5). The highest absolute correlations were between energy and Total Fruits (−0.23) and Whole Fruits (−0.21). The correlation between energy and the total score was also low (−0.06) and not statistically significantly different from zero.
Table 5.
Estimated correlations of Healthy Eating Index-2015 (HEI-2015)a component and total scoresb and energy intake, based on the National Health and Nutrition Examination Survey 2011–2012 (N=7,935)
| Component | Total Fruits | Whole Fruits | Total Vegetables | Greens and Beans | Whole Grains | Dairy | Total Protein Foods | Seafood and Plant Proteins | Fatty Acids | Refined Grains | Sodium | Added Sugars | Saturated Fats | Total scoreb |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Whole Fruits | 0.83** | |||||||||||||
| Total Vegetables | 0.16** | 0.23** | ||||||||||||
| Greens and Beans | 0.17** | 0.23** | 0.74** | |||||||||||
| Whole Grains | 0.29** | 0.37** | 0.31** | 0.32** | ||||||||||
| Dairy | 0.20** | 0.21** | −0.35** | −0.22** | 0.18** | |||||||||
| Total Protein Foods | −0.20** | −0.16** | 0.35** | 0.31** | −0.06 | −0.36** | ||||||||
| Seafood and Plant Proteins | 0.11 | 0.21 | 0.49** | 0.59** | 0.33** | −0.19** | 0.38** | |||||||
| Fatty Acids | −0.08 | −0.05 | 0.42** | 0.34** | 0.14 | −0.55** | 0.30** | 0.38** | ||||||
| Refined Grains | 0.14** | 0.13 | 0.27** | 0.22** | 0.21** | −0.06 | 0.11** | 0.29** | 0.11** | |||||
| Sodium | 0.17** | 0.11 | −0.43** | −0.32** | −0.07 | 0.19** | −0.43** | −0.15 | −0.21** | 0.20** | ||||
| Added Sugars | 0.25** | 0.27** | 0.43** | 0.41** | 0.30** | 0.02 | 0.23** | 0.34** | 0.16** | 0.16 | −0.27** | |||
| Saturated Fats | 0.07 | 0.05 | 0.28** | 0.22** | 0.16** | −0.36** | 0.03 | 0.12 | 0.61** | 0.05 | 0.01 | 0.02 | ||
| Total score | 0.39** | 0.46** | 0.56** | 0.58** | 0.47** | −0.21** | 0.09 | 0.56** | 0.29** | 0.34** | −0.20** | 0.43** | 0.23** | |
| Energy | −0.23** | −0.21** | −0.07 | 0.03 | −0.15** | −0.12** | 0.14** | 0.16** | 0.06 | 0.12 | 0.10 | −0.07 | −0.04 | −0.06 |
HEI-2015 component and total scores calculated using the index detailed by Krebs-Smith and colleagues.8
HEI-2015 total score minus specified component.
P<0.01.
5. Is the Index Multidimensional?
The principal component analysis yielded a scree plot (Figure 2) that illustrated no one single linear combination of the HEI-2015 components accounted for a significant proportion of the covariation in dietary patterns. There was evidence for four to six dimensions as four factors had an eigenvalue >1, and the line in the scree plot appeared to plateau around six factors.
Figure 2.
Scree plot from principal components analysis of Healthy Eating Index-2015. Source of intake data was National Health and Nutrition Examination Survey 2011–2012.
Reliability (Internal Consistency)
6. What Are the Relationships among the Index Components? What Components Exert the Most Influence on the Total Score?
There were higher correlations between Total Fruits and Whole Fruits (0.83) and between Greens and Beans and Total Vegetables (0.74) than between unrelated components. Overall, the intercorrelations among the scores for the remaining components were low to moderate, ranging between 0.01 and 0.49 (Table 5). Exceptions were evident in cases in which correlations would be expected to be high, such as between associated components like Saturated Fats and Fatty Acids. Between the total score and the component scores, the item-total correlations ranged from −0.21 (Dairy) to 0.58 (Greens and Beans). Five components have moderate correlations with the HEI-2015 total score (range, 0.46 to 0.58): Whole Fruits, Total Vegetables, Greens and Beans, Whole Grains, and Seafood and Plant Proteins.
7. How Internally Consistent Is the Score?
The standardized Cronbach’s alpha for the NHANES sample was .67. By examining the degree of association among components within the index, this statistic captures any systematic variation underlying the HEI components.
Criterion Validity
8. Can the Index Predict a Health Outcome?
During 15 years of follow-up among the NIH-AARP prospective cohort, 84,774 deaths were documented, including 27,962 cancer deaths and 23,438 CVD deaths. Table 6 shows that men and women in quintile 5 (highest diet quality) compared with quintile 1 (lowest) had a 13% to 23% decreased risk of all-cause, cancer, and CVD mortality. Specifically, the adjusted hazard ratios (HRs) and 95% CIs for men and women, respectively, for all-cause mortality were HR: 0.80, 95% CI: 0.78 to 0.82 and HR: 0.77, 95% CI: 0.74 to 0.80; for cancer mortality were HR: 0.78, 95% CI: 0.74 to 0.82 and HR: 0.80, 95% CI: 0.75 to 0.86; and for CVD mortality were HR: 0.87, 95% CI: 0.83 to 0.92 and HR: 0.79, 95% CI: 0.73 to 0.85.
Table 6.
Multivariate hazard ratios (HRs) and 95% CIs for mortality according to quintile (Q) of the Healthy Eating Index-2015 (HEI-2015) among men (n=241,214) and women (n=181,714) in the National Institutes of Health-AARP (formerly known as the American Association of Retired Persons) Diet and Health Studya
| Population | n | Multivariate HR (95% CI) All-cause mortality | Multivariate HR (95% CI) Cancer mortality | Multivariate HR (95% CI) CVDb mortality |
|---|---|---|---|---|
| Men (n=241,214) | Any deaths (n=53,826) | Cancer deaths (n=17,754) | CVD deaths (n=15,446) | |
| HEI-2015 (points) | ||||
| Q1 (21.5–58.3) | 48,242 | 1.00 | 1.00 | 1.00 |
| Q2 (58.3–64.7) | 48,243 | 0.96 (0.93–0.98) | 0.96 (0.92–1.00) | 1.00 (0.95–1.05) |
| Q3 (64.7–69.8) | 48,243 | 0.90 (0.87–0.92) | 0.89 (0.85–0.93) | 0.95 (0.90–1.00) |
| Q4 (69.8–75.1) | 48,243 | 0.85 (0.82–0.87) | 0.80 (0.76–0.84) | 0.90 (0.85–0.94) |
| Q5 (75.1–96.1) | 48,243 | 0.80 (0.78–0.82) | 0.78 (0.74–0.82) | 0.87 (0.83–0.92) |
| Women (n=181,714) | Any deaths (n=30,948) | Cancer deaths (n=10,208) | CVD deaths (n=7,992) | |
| HEI-2015 (points) | ||||
| Q1 (26.5–61.0) | 36,342 | 1.00 | 1.00 | 1.00 |
| Q2 (61.0–67.3) | 36,343 | 0.91 (0.88–0.94) | 0.90 (0.85–0.96) | 0.92 (0.86–0.99) |
| Q3 (67.3–72.0) | 36,343 | 0.88 (0.85–0.91) | 0.90 (0.85–0.96) | 0.89 (0.83–0.95) |
| Q4 (72.0–76.8) | 36,343 | 0.83 (0.80–0.86) | 0.84 (0.79–0.89) | 0.82 (0.76–0.88) |
| Q5 (76.8–95.8) | 36,343 | 0.77 (0.74–0.80) | 0.80 (0.75–0.86) | 0.79 (0.73–0.85) |
Adjusted for age, race/ethnicity, education, marital status, physical activity, smoking, energy, body mass index, diabetes, alcohol, and hormone replacement therapy (women only). Ranges appear to overlap; however, this is due to rounding and quintiles are discrete categories.
CVD=cardiovascular disease.
DISCUSSION
As expected based on previous analyses with similarly structured versions of the HEI, analysis of the HEI-2015 demonstrates that it captures variation in diet quality and does so in a manner reflecting the multidimensional nature of healthy diets. Specifically, this evaluation provided evidence that the updated index captures constructs of interest; that is, it 1) gives high scores to known high-quality menus, 2) demonstrates variation in scores across the US population, 3) differentiates diet quality among groups of people with known differences in diet, 4) assesses diet quality independent of diet quantity, and 5) captures the multidimensionality of diet quality. Furthermore, the HEI-2015 6) captures distinct dietary components, 7) demonstrates a reasonable level of internal consistency for a multidimensional measure, and 8) is associated with a reduced risk of mortality, indicating criterion validity.
Four sets of exemplary menus had high HEI-2015 total scores indicating construct validity. Although not all menus received optimal scores for all components, these scores reflect high-quality diets, and, in the case of the Harvard Healthy Eating Guide, reflect the interpretation of the science as intended with their menus; for example, recommendations to limit dairy products.11 Menus, which were kept consistent with previous HEI evaluations, did not always receive perfect scores on some components because these older menus may not reflect recent refinement regarding guidance for added sugars. Indeed, there was significant variation in added sugars intake across days on the USDA (0.4% to 14.8%) and AHA menus (7% to 14%). In addition, although menus often maintain sodium values below a defined goal such as 2,300 mg or 2.3 g, most menus designed at levels <2,150 kcal, such as those from AHA (1,200 kcal) and Harvard (1,600 kcal), will exceed the density-based scoring standard for sodium ([2.3 g/2,150 kcal] × 1,000 or 1.1 g/1,000 kcal). Further, analyzing a limited number of menus reflecting a short period of time (for example, the 2-day AHA menus) may lead to lower scores compared with analyses reflecting a longer period of time. This is because components such as Greens and Beans and Seafood and Plant Proteins may receive lower scores due to being episodically consumed foods. When analyses were conducted using a larger number of menu days drawn from a subsequent publication of the AHA menu, scores improved for the Greens and Beans and Seafood and Plant Proteins components.12
Construct validity was supported by the analyses of NHANES data, which showed that HEI scores reflected variability across the diets of the US population and between groups known to have differences in dietary quality. There was a large range of scores observed, indicating the ability to detect meaningful differences across the population, as well as distinguishing between groups (women and men, older and younger adults, and smokers and nonsmokers), in both total and component scores. However, because some components have more or less variability than others, further research may be useful to elucidate what truly reflects meaningful (or statistically significant) differences in scores across individuals within a population or between population subgroups. This may have implications for the weighting of components as well as scoring standards for moderation and adequacy components. Additional research is also needed to explore the ability of an index like the HEI to detect differences between populations or cultures that might have significant variation in common foods consumed or overall eating patterns.
Calculating HEI-2010 and HEI-2015 scores using NHANES 2011–2012 data allowed for comparison between versions of the index based on the same sample (Table 3). The mean total score using HEI-2015 (mean total HEI-2015 score=56.6) was quite similar to the mean total score using HEI-2010 (mean total HEI-2015 score=56.1) and the scores were highly correlated. Mean component scores were also similar between index versions, with small but expected changes in components in cases in which the scoring standards have changed (as with the legume allocation in Total Protein Foods, Seafood and Plant Proteins, Total Vegetables, and Greens and Beans). Overall the distribution of the total HEI-2015 was slightly narrower from the first to the 99th percentiles (32.6 to 81.2) compared with the distribution of the total HEI-2010 in these percentiles (30.7 to 82.6). This narrowing occurred because of the combined effects from the two main changes to the HEI-2015: a slight increase in the scores by giving credit to legumes as sources of both vegetables and protein and a slight narrowing in the scores by including discrete standards for added sugars and saturated fats rather than a single component (Empty Calories in HEI-2010). In addition, because the HEI-2015 allocates legumes to all four components where it is relevant (Total Vegetables, Greens and Beans, Total Protein Foods, and Seafood and Plant Proteins), it will be more straightforward to detect and interpret any differences over time in these component scores.
Construct validity was also illustrated by the low correlations between component scores and energy. These low correlations indicate that the HEI-2015 can assess diet quality independent of quantity. This is an essential feature of the HEI because if the score was dependent on quantity of foods eaten, higher scores may be due to eating greater quantities of food rather than higher quality of foods eaten.
The principal components analysis showed no evidence for a single, systematic underlying relationship among all the components of the HEI-2015. That is, no one single linear combination of the 13 components explained the variation in the data. This finding was expected because diet quality comprises a broad array of differing and, to some extent, independent aspects.
In addition, the HEI-2015 total score approached the standard of .70 for reliability, as assessed by internal consistency (Cronbach’s alpha). This suggests that the HEI captures an underlying construct of overall diet quality. However, it is important to note that characteristics of the index and the sample affect the size of the reliability coefficient.31 In particular, the coefficient is affected by whether the construct is unidimensional or multidimensional, the heterogeneity of the sample, and the homogeneity among items.31 Although reliability coefficients are useful for measuring to what degree items are interrelated, when an index is multidimensional, captures the full diet, and is evaluated on the entire US population, it is expected that the reliability coefficient would be lower compared with that for a tool that captures one dimension on a homogenous population. The coefficient had been expected to be rather low because diet quality is known to be a complex and multidimensional construct and because individuals do not consistently meet, or fail to meet, all the dietary standards used to assess diet quality. Although internal consistency is not a necessary characteristic of the HEI, it has implications in terms of how much confidence can be placed in the total score.
Variation in the total score is reflective of the variation in the components that have higher correlations with the total score. The components having the lowest correlations with the total score may not be adding much information about the variation in the total score, but rather, they provide important independent information. The approach used in the HEI-2015 aligns with federal guidance, and includes all aspects of the diet equally.8
The HEI-2015 has demonstrated predictive validity with mortality (in the range of 13% to 23% lower risk associated with high diet quality) among older US men and women. These findings align with previous studies examining the predictive criterion validity of prior versions of the HEI, as well as those with other diet quality indexes.32–34
Like any measure of a construct such as diet quality, the HEI has limitations. Measurement error is an important consideration relevant to all self-reported behavioral variables. The simple models used to examine predictive validity do not address measurement error; however, efforts are underway to do so for future analyses.35 Other potential issues exist related to HEI scoring. For example, there are multiple ways to arrive at the same total score (a score of 60 can be attained through very different profiles of component scores). Because of this, examining component scores, as well as total scores, is encouraged. There is greater confidence regarding total scores at the higher and lower ends of the range of scores because they represent more homogenous diets across individuals. In addition, unlike the range of intakes for nutrients or food groups, HEI component and total scores are truncated, and so may not capture some important information. For example, a high score for Total Protein Foods does not capture potentially excessive intakes, which could be further explored.
CONCLUSIONS
These analyses demonstrate evidence supportive of construct validity, reliability, and criterion validity for the HEI-2015, as has been shown in earlier work with the HEI-200536 and HEI-2010.37 The HEI-2015 can be used for questions examining diet quality relative to the 2015–2020 DGA. However, limitations in the HEI as well as those inherent to dietary intake data more broadly should be considered in any application of the index. Details about how nutrition and dietetics practitioners can use the HEI have been described in an applications article.35 As the applications of the HEI continue to expand, additional efforts related to validation can be explored, supporting its robust use to enhance our understanding of diet quality among the population.
RESEARCH SNAPSHOT.
Research Question: Does the Healthy Eating Index-2015 (HEI-2015) exhibit construct validity, reliability, and criterion validity?
Key Findings: This evaluation found that HEI-2015 demonstrated construct validity by yielding high scores on exemplary menus, and using National Health and Nutrition Examination Survey data, the index showed variation in scores in the population, differentiated between groups such as smokers and nonsmokers, assessed diet quality independent of quantity, and captured multidimensionality. The HEI-2015 displayed reliability with low to moderate correlations among distinct components and internal consistency. Finally, the index demonstrated criterion validity because the HEI-2015 was associated with a statistically significant reduced risk of mortality in the National Institutes of Health-AARP (formally known as the American Association of Retired Persons) Diet and Health Study.
ACKNOWLEDGEMENTS
The authors thank Kevin W. Dodd, PhD, National Cancer Institute, for providing statistical guidance.
FUNDING/SUPPORT
S. I. Kirkpatrick is supported in part by a Canadian Cancer Society Research Institute Capacity Development Award (grant no. 702855). J. A. Tooze is supported in part by NCI Cancer Center Support Grant (grant no. P30 CA012097), Comprehensive Cancer Center of Wake Forest Baptist Medical Center. Other authors have no other funding disclosures.
Footnotes
STATEMENT OF POTENTIAL CONFLICT OF INTEREST
No potential conflict of interest was reported by the authors.
References
- 1.Nutrition and Your Health: 2015–2020 Dietary Guidelines for Americans. 8th edition Washington, DC: US Government Printing Office; 2015. Home and Garden Bulletin No. 232. [Google Scholar]
- 2.Jahns L, Scheett AJ, Johnson LK, et al. Diet quality of items advertised in supermarket sales circulars compared to diets of the US population, as Assessed by the Healthy Eating Index-2010. J Acad Nutr Diet. 2016;116(1):115–122. [DOI] [PubMed] [Google Scholar]
- 3.Wilson MM, Reedy J, Krebs-Smith SM. American diet quality: Where it is, where it is heading, and what it could be. J Acad Nutr Diet. 2016;116(2):302–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nanney MS, Grannon KY, Cureton C, et al. Application of the Healthy Eating Index-2010 to the Hunger Relief System. Public Health Nutr. 2016;19(16):2906–2914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park SY, Boushey CJ, Wilkens LR, Haiman CA, Le Marchand L. High-quality diets associate with reduced risk of colorectal cancer: analyses of diet quality indexes in the Multiethnic Cohort. Gastroenterology. 2017;153(2):386–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guenther PM, Casavale KO, Reedy J, et al. Update of the Healthy Eating Index: HEI-2010. J Acad Nutr Diet. 2013;113(4):569–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guenther PM, Reedy J, Krebs-Smith SM. Development of the Healthy Eating Index-2005. J Am Diet Assoc. 2008;108(11):1896–1901. [DOI] [PubMed] [Google Scholar]
- 8.Krebs-Smith SM, Pannucci TE, Subar AF, et al. Update of the Healthy Eating Index-2015. J Acad Nutr Diet. 2018;118(9):1591–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sample menus for a 2000 calorie food pattern. Alexandria, VA: US Department of Agriculture, Center for Nutrition Policy and Promotion; 2011. [Google Scholar]
- 10.National Heart Lung and Blood Institute. Your guide to lowering your blood pressure with DASH. 2006. http://www.nhlbi.nih.gov/health/public/heart/hbp/dash/new_dash.pdf. Accessed August 1, 2017.
- 11.Willet WC. Eat, Drink and Be Healthy The Harvard Medical School Guide to Healthy Eating. New York, NY: Simon and Schuster; 2001. [Google Scholar]
- 12.American Heart Association. American Heart Association No-Fad Diet: A Personal Plan for Healthy Weight Loss. New York, NY: Crown Publishers; 2011. [Google Scholar]
- 13.Centers for Disease Control and Prevention. NHANES 2011–2012 dietary data. https://wwwn.cdc.gov/nchs/nhanes/Search/DataPage.aspx?Component=Dietary&CycleBeginYear=2011. Accessed August 18, 2017.
- 14.Sebastian RS, Enns CW, Steinfeldt LC, Goldman JD, Moshfegh AJ. Discontinuation of data processing step: Salt adjustment on designated foods likely to be prepared at home. 2012; https://www.ars.usda.gov/ARSUserFiles/80400530/pdf/0910/discontinuation%20of%20data%20processig%20step-salt%20adjustment.pdf. Accessed September 14, 2017.
- 15.Schatzkin A, Subar AF, Thompson FE, et al. Design and serendipity in establishing a large cohort with wide dietary intake distributions: The National Institutes of Health-American Association of Retired Persons Diet and Health Study. Am J Epidemiol. 2001;154(12):1119–1125. [DOI] [PubMed] [Google Scholar]
- 16.Michaud D, Midthune D, Hermansen S, et al. Comparison of cancer registry case ascertainment with SEER estimates and self-reported in a subset of the NIH-AARP Diet and Health Study. J Registry Manage. 2005;32:70–75. [Google Scholar]
- 17.National Cancer Institute. SEER cause of death record 1969þ. http://seer.cancer.gov/codrecode/1969+_d04162012/index.html. Accessed September 12, 2017.
- 18.Thompson FE, Kipnis V, Midthune D, et al. Performance of a food-frequency questionnaire in the US NIH-AARP (National Institutes of Health-American Association of Retired Persons) Diet and Health Study. Public Health Nutr. 2008;11(2):183–195. [DOI] [PubMed] [Google Scholar]
- 19.Subar AF, Midthune D, Kulldorff M, et al. Evaluation of alternative approaches to assign nutrient values to food groups in food frequency questionnaires. Am J Epidemiol. 2000;152(3):279–286. [DOI] [PubMed] [Google Scholar]
- 20.SAS [computer program]. Version 9.4. Cary, NC: SAS Institute Inc; 2016. [Google Scholar]
- 21.National Cancer Institute. Healthy Eating Index: Overview of the methods & calculations. https://epi.grants.cancer.gov/hei/hei-methods-and-calculations.html. Accessed September 14, 2017.
- 22.Zhang S, Midthune D, Guenther PM, et al. A new multivatiate measurement error model with zero-inflated dietary data, and its application to dietary assessment. Ann Appl Stat. 2011;5(2b):1456–1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tooze JA, Kipnis V, Buckman DW, et al. A mixed-effects model approach for estimating the distribution of usual intake of nutrients: the NCI method. Stat Med. 2010;29(27):2857–2868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tooze JA, Midthune D, Dodd KW, et al. A new statistical method for estimating the usual intake of episodically consumed foods with application to their distribution. J Am Diet Assoc. 2006;106(10):1575–1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Freedman LS, Guenther PM, Dodd KW, Krebs-Smith SM, Midthune D. The population distribution of ratios of usual intakes of dietary components that are consumed every day can be estimated from repeated 24-hour recalls. J Nutr. 2010;140(1):111–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Freedman LS, Guenther PM, Krebs-Smith SM, Dodd KW, Midthune D. A population’s distribution of Healthy Eating Index-2005 component scores can be estimated when more than one 24-hour recall is available. J Nutr. 2010;140(8):1529–1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kipnis V, Midthune D, Buckman DW, et al. Modeling data with excess zeros and measurement error: Application to evaluating relationships between episodically consumed foods and health outcomes. Biometrics. 2009;65(4):1003–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.National Cancer Institute. Measurement error webinar series. https://epi.grants.cancer.gov/events/measurement-error/. Accessed August 2017.
- 29.Centers for Disease Control and Prevention. NHANES Dietary Web tutorial: Dietary data survey orientation. https://www.cdc.gov/nchs/tutorials/dietary/SurveyOrientation/intro.htm. Accessed January 25, 2018.
- 30.Cox DR. Regression models and life tables. J R Stat Soc Ser Z. 1972;B34:187–220. [Google Scholar]
- 31.Goodwin LD, Goodwin WL. Research design and methodology section. Measurement myths and misconceptions. School Psychol Q. 1999;14(4):408–427. [Google Scholar]
- 32.George SM, Ballard-Barbash R, Manson JE, et al. Comparing indices of diet quality with chronic disease mortality risk in postmenopausal women in the Women’s Health Initiative Observational Study: Evidence to inform national dietary guidance. Am J Epidemiol. 2014;180(6):616–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harmon BE, Boushey CJ, Shvetsov YB, et al. Associations of key dietquality indexes with mortality in the Multiethnic Cohort: the Dietary Patterns Methods Project. Am J Clin Nutr. 2015;101(3):587–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reedy J, Krebs-Smith SM, Miller PE, et al. Higher diet quality is associated with decreased risk of all-cause, cardiovascular disease, and cancer mortality among older adults. J Nutr. 2014;144(6):881–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kirkpatrick SI, Reedy J, Krebs-Smith SM, et al. Applications of the Healthy Eating Index (HEI) for surveillance, epidemiology and intervention research: Considerations and caveats. J Acad Nutr Diet. 2018;118(9):1603–1621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guenther PM, Reedy J, Krebs-Smith SM, Reeve BB. Evaluation of the Healthy Eating Index-2005. J Am Diet Assoc. 2008;108(11): 1854–1864. [DOI] [PubMed] [Google Scholar]
- 37.Guenther PM, Kirkpatrick SI, Reedy J, et al. The Healthy Eating Index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J Nutr. 2014;144(3):399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]