Abstract
Background
Electronic nicotine delivery systems, including electronic cigarettes (e-cigarettes) are gaining popularity. The objectives of this study were to assess the knowledge and beliefs about e-cigarettes among physicians in Poland.
Material/Methods
A questionnaire-based survey was conducted among physicians attending mandatory courses delivered at the School of Public Health, Centre of Postgraduate Medical Education (Warsaw, Poland). The questionnaire included 24 questions concerning beliefs and attitudes about e-cigarettes.
Results
Data were obtained from 412 physicians (64.3% females; aged 31.9±5.7 years) with a response rate of 82.4%. Among participants, 99.8% were aware of e-cigarettes. The main sources of information about e-cigarettes were: news stories (67.2%) or points of sale of e-cigarettes (67.6%). Approximately half of respondents (50.2%) declared moderate knowledge about e-cigarettes, and over three-quarters (78.1%) declared willingness to learn more about e-cigarettes. The majority (96.5%) of participants agreed with the statement that e-cigarette use is harmful to the user’s health, and most (80.5%) agreed that exhaled e-cigarette aerosol is harmful to bystanders. The statement that e-cigarettes could be “gateway” to conventional smoking was supported by 87% of participants. Only 11.5% of physicians agreed that e-cigarettes should be recommended as a smoking cessation method.
Conclusions
Physicians in Poland perceive e-cigarettes as harmful and addictive. Physicians’ knowledge about e-cigarettes is mostly based on non-scientific sources, which points out the urgent need to develop national smoking cessation guidelines regulating the issue of e-cigarettes based on scientific evidence.
MeSH Keywords: Behavior, Addictive; Nicotine; Smoking
Background
Over the past 40 years, a marked decline in daily smoking prevalence in Poland has been observed [1,2]. It is estimated that between 1976 and 2014, smoking prevalence has declined from 73% to 28% among males and from 30% to 19% among females [1]. According to the data from the Chief Sanitary Inspectorate, in 2017, one-quarter of Poles aged ≥15 years old smoked cigarettes regularly [3]. While the prevalence of tobacco use among Poles is monitored [1–3], electronic nicotine delivery systems, including electronic cigarettes (e-cigarettes) are gaining popularity [4–6].
Electronic cigarettes are battery-operated devices with a heating mechanism that heats the dedicated inhalation solution, producing an aerosol (called vapor) which is inhaled into the lungs [7]. There are multiple models of e-cigarette devices and a variety of flavor variants of the inhalation solution (called e-liquids) [8]. Chemical analysis of e-cigarette vapor and cigarette smoke revealed that e-cigarette use emits fewer numbers and lower levels of toxicants compared to cigarette smoking [9–11]. However, there is growing evidence from human-based studies showing potential harmful effects of e-cigarette use [12–15]. Due to the ambiguity of evidence on the impact of e-cigarettes on health, and the lack of long-term prospective cohort studies on e-cigarettes, there is a wide debate whether e-cigarettes can be used as a harm reduction tool [9,16–18]. According to the US National Academies of Sciences, Engineering, and Medicine (NASEM) report, e-cigarettes may pose a lower risk for health compared to cigarette smoking, but also can encourage young individuals who start with e-cigarettes to switch to combustible cigarettes (“gateway effect”) [9]. The NASEM committee of experts concluded that more research is needed to assess the potential impact of e-cigarette use on public health at the individual and the population levels [9].
Controversy around whether e-cigarettes will reduce or induce harm has resulted in e-cigarette regulation that varies between countries, ranging from lack of regulation to completely ban on e-cigarette sale or use [19]. In Poland, e-cigarettes are classified as tobacco related products and regulated by the amendment of the National Tobacco Control Act (Journal of Laws, Item 1331, 2016), which has been in force since September 2016 [20]. Regulation sets rules on sale and advertising as well as packaging and labelling of e-cigarettes [20]. Sale or distribution of e-cigarettes to minors under 18 years, cross-border distance sales, and sale via vending machines or self-service systems are prohibited. There is also a ban on e-cigarette use in public places, including hospitals and public transportation [20]. The amendment also introduced a ban on advertising, promotion, and sponsorship related to e-cigarettes. The same rules apply to e-cigarettes with and without nicotine [20].
Healthcare professionals have a prominent role to play in addressing the tobacco epidemic [21–23]. Evidence shows that brief interventions to smokers by healthcare professionals can increase rates of smoking cessation [22,23]. To facilitate the treatment of a smoking patient, in many countries national guidelines for smoking cessation were developed [2,24–26]. The Polish smoking cessation guidelines recommend healthcare professionals (especially primary care physicians) systematically identify smokers and provide a minimum intervention on smoking cessation based on the “Five As” (ask, advise, assess, assist, arrange) [26]. The growing interest of patients in e-cigarettes has led some countries to update their smoking cessation guidelines to information regarding e-cigarettes [27,28]. In the United Kingdom, the National Institute for Health and Care Excellence published guidelines for healthcare professionals on how to discuss abut e-cigarettes with the patients [27].
According to data from a cross-sectional survey of 27 901 EU citizens in 2017, 15% of Europeans aged 15 years or older declared at least one-time use of e-cigarettes and 2% were regular e-cigarette users [29]. In Poland, the prevalence of e-cigarette use among adults decreased from 3% in 2013 to 2% in 2017 [3]. The highest prevalence was observed among adolescents [6,30]. Between 2010 and 2016, in a group of students aged 15–19 years old, the proportion of regular exclusive e-cigarette users increased from 2% in 2010–2011 to 11% in 2015–2016 [31]. Among e-cigarettes users, the dominant group are dual users who regularly use other nicotine containing products as well as e-cigarettes [5,30,31]. It is estimated that every fourth teenager in Poland is a dual user [30].
The growing popularity of e-cigarettes makes more and more people ask their doctor for advice on e-cigarettes [28]. Currently there is a lack of national guidelines regarding e-cigarettes in Poland. Due to the lack of recommendations developed by national scientific committees, guidance to patients depends on the individual decision of physicians and is shaped by physicians’ perceptions of e-cigarettes. As healthcare professionals hold diverse views about the efficacy and safety of electronic nicotine delivery systems [32], it is important to know how e-cigarettes are perceived by physicians. Therefore, the objectives of this study were to assess the knowledge and beliefs about e-cigarettes among physicians in Poland.
Material and Methods
Participants
A questionnaire-based survey was conducted between September and December 2018. Within Poland, each physician must attend a public health training course within 5–6 years of beginning their profession. The participation in the course is compulsory for each of 25 000 physician undergoing specialty in Poland. The participants in the courses are selected randomly and represented different regions and healthcare institutions from all over Poland. We approached physicians attending the training courses held during September, October, and November 2018 (8 different courses). All 500 physicians attending these specialist training courses delivered at the School of Public Health, Centre of Postgraduate Medical Education (Warsaw, Poland) during this period were eligible to take the survey.
Study questionnaire
The research tool was a self-administered questionnaire developed for the purpose of this study. The questionnaire was developed in Polish. In preparation of the questionnaire, we analyzed the previously published studies on the perceptions of e-cigarettes among healthcare professionals [28,33,34].
The questionnaire included 24 questions concerning beliefs and attitudes about e-cigarettes. Additional questions also addressed background information including age, sex, level of training, specialty, years of professional experience, practice type, and practice location.
E-cigarette awareness was assessed by the question “Are you aware of electronic cigarettes (commonly called e-cigarettes)?” (“Yes”/“No”). An additional question regarding the source of knowledge about e-cigarettes was addressed to all participants who declared being aware of e-cigarettes. To measure physicians’ perceptions of e-cigarettes, a survey containing 22 questions regarding e-cigarettes was distributed to the attendees of the specialist training courses (Table 1). Questions regarding individual beliefs and attitudes about e-cigarettes were divided into 3 blocks: 1) health effects of e-cigarettes use, 2) addictive potential of e-cigarettes use, and 3) regulations concerning e-cigarettes. All 22 questions (Table 1) were meant to assess attitudes and beliefs with 4-point response scale: 1=“totally disagree”, 2=“rather disagree”, 3=“rather agree” and 4=“totally agree”.
Table 1.
Beliefs and attitudes about e-cigarettes among physicians who were aware of e-cigarettes (n=411).
| Totally disagree % (95% CI) | Rather disagree % (95% CI) | Rather agree % (95% CI) | Totally agree % (95% CI) | |
|---|---|---|---|---|
| Health effects of e-cigarette use | ||||
| E-cigarettes use is harmful for health of the user | 0.7 (0.3–2.1) | 2.7 (1.5–4.8) | 38.1 (33.6–42.9) | 58.4 (53.6–63.1) |
| E-cigarette aerosol is harmful for people in the vicinity of the users | 1.7 (0.8–3.5) | 17.9 (14.5–21.9) | 50.3 (45.4–55.1) | 30.2 (25.9–34.8) |
| E-cigarettes are less harmful than conventional cigarettes | 13.7 (10.7–17.4) | 27.2 (23.1–31.7) | 47.3 (42.5–52.2) | 11.8 (9.0–15.3) |
| E-cigarettes are carcinogenic | 0.7 (0.3–2.1) | 13.2 (10.3–16.8) | 50.6 (45.8–55.4) | 35.5 (31.0–40.2) |
| The risk of cancer is lower for the e-cigarettes than for the conventional cigarettes | 8.7 (6.4–11.9) | 27.7 (23.6–32.2) | 53.6 (48.8–58.4) | 10.0 (7.4–13.2) |
| E-cigarette use increases the risk of cardiovascular diseases, including myocardial infarction and stroke | 1.0 (0.4–2.5) | 9.3 (6.9–12.5) | 53.4 (48.6–58.2) | 36.3 (31.8–41.1) |
| The risk of cardiovascular diseases is lower for the e-cigarettes than for the conventional cigarettes | 11.2 (8.5–14.6) | 32.1 (27.8–36.8) | 50.1 (45.3–54.9) | 6.6 (4.6–9.4) |
| E-cigarette use increases the risk of chronic lung diseases, including COPD | 1.0 (0.4–2.5) | 13.8 (10.8–17.5) | 50.5 (45.7–55.3) | 34.7 (30.3–39.4) |
| The risk of chronic lung diseases is lower for the e-cigarettes than for the conventional cigarettes | 10.5 (7.9–13.8) | 32.6 (28.3–37.3) | 49.4 (44.6–54.2) | 7.5 (5.4–10.5) |
| Addictive potential of e-cigarettes use | ||||
| E-cigarettes could be a „gateway” to conventional cigarettes use in the future | 1.9 (1.0–3.8) | 10.7 (8.1–14.1) | 45.7 (41.0–50.6) | 41.6 (36.9–46.4) |
| You can become addicted to the e-cigarette | 1.0 (0.4–2.5) | 1.9 (1.0–3.8) | 30.4 (26.2–35.0) | 66.7 (62.0–71.1) |
| E-cigarettes are less addictive than conventional cigarettes | 32.9 (28.5–37.6) | 46.9 (42.1–51.8) | 18.2 (14.7–22.2) | 2.0 (1.0–3.8) |
| E-cigarettes should be recommended as a smoking cessation tool | 43.3 (38.6–48.1) | 43.3 (38.6–48.1) | 11.5 (8.8–15.0) | 1.9 (1.0–3.8) |
| Smokers who do not want to quit smoking, should be offered and encouraged to use e-cigarettes | 30.8 (26.5–35.4) | 35.2 (30.7–40.0) | 30.8 (26.5–35.4) | 3.2 (1.9–5.4) |
| Smokers who failed to quit with conventional smoking cessation should be offered and encouraged to use e-cigarettes | 24.3 (20.4–28.6) | 32.0 (27.7–36.7) | 39.8 (35.2–44.6) | 3.9 (2.4–6.2) |
| I recommend the e-cigarettes to my patients smoking conventional cigarettes | 48.5 (43.7–53.4) | 38.2 (33.7–43.0) | 11.8 (9.0–15.3) | 1.5 (0.7–3.2) |
| Discussing e-cigarettes with patients may encourage them to use e-cigarettes | 15.6 (12.4–19.4) | 35.6 (31.1–40.4) | 43.9 (39.2–48.7) | 4.9 (3.2–7.4) |
| Regulation of e-cigarettes | ||||
| E-cigarette promotion and advertising should be banned | 4.2 (2.6–6.6) | 11.5 (8.8–15.0) | 29.4 (25.2–34.0) | 54.9 (50.1–59.7) |
| E-cigarettes should be prohibited to minors (under 18 years) | 2.2 (1.2–4.1) | 0.7 (0.3–2.1) | 10.5 (7.9–13.8) | 86.6 (82.9–89.6) |
| E-cigarettes use in public places should be banned | 3.6 (2.2–5.9) | 7.5 (5.4–10.5) | 22.8 (19.0–27.1) | 66.0 (61.3–70.4) |
| E-cigarettes use should be banned indoors | 3.4 (2.0–5.6) | 4.9 (3.2–7.4) | 19.4 (15.9–23.5) | 72.3 (67.8–76.4) |
| E-cigarettes should be regulated in the same way as tobacco products | 4.1 (2.6–6.5) | 7.3 (5.2–10.2) | 18.7 (15.2–22.7) | 69.9 (65.3–74.1) |
Repeatability of the prepared questionnaire was assessed by conducting it twice in an interval of 5 days among 14 physicians. Questionnaires as well as the form of distribution in both samples were identical. Kappa coefficients for the critical questions ranged from 0.88 to 0.96 so as these values were greater than 0.80 all questions were included in the final questionnaire.
A paper-based questionnaire was delivered to each of the 500 participants by a member of the research team. Participation in the study was voluntary and anonymous. Informed verbal consent was obtained from all individual participants involved in the study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Statistical analysis
For assessment of repeatability, Fleiss’ kappa coefficients were calculated using SAS (SAS Institute Inc., Cary, NC, USA). The data was analyzed with Statistica 12 Software (TIBCO Software Inc., Palo Alto, CA, USA). Normality of distributions of continuous variables was assessed by the Shapiro-Wilk test. The distribution of categorical variables was shown by frequencies and proportions along with 95% confidence intervals. The chi-square test was used to compare categorical variables. Statistical inference was based on the criterion P<0.05.
Depending on the level of professional development, participants were allocated to either a specialist-in-training group (specialty ongoing) or a specialist group (specialty completed). Based on self-declared field of medical practice, participants were assigned to a surgical or a non-surgical specialty.
Results
Data were obtained from 412 physicians (64.3% females), with a response rate of 82.4%. The average age of the respondents was 31.9±5.7 years, with no age differences between males and females (P>0.05). The vast majority of participants were physicians-in-training (85.7%). Physicians from 52 different specialties (out of 77 available specializations) took part in the survey. A total of 72.8% of all participants were trained in non-surgical specialties, mostly in internal medicine (116 participants) or pediatrics (86 participants). The predominant group of participants (89.1%) declared hospital as a place of primary employment. Over half of the physicians practiced in cities with more than 500 000 residents. Detailed participant characteristics are presented in Table 2.
Table 2.
Participant characteristics (n=412).
| n (%) | |
|---|---|
| Age (years), mean±SD, (min–max) | 31.9±5.7 (26–64) |
| Sex | |
| Male | 147 (35.7) |
| Female | 265 (64.3) |
| Medical education level | |
| In-training (during specialization) | 353 (85.7) |
| Specialist | 59 (14.3) |
| Specialty (n=390) | |
| Surgical | 106 (27.2) |
| Non-Surgical | 284 (72.8) |
| Years of professional experience, mean±SD, (min–max) | 5.8±5.2 (1–35) |
| Place of primary employment (practice type) | |
| Hospital | 367 (89.1) |
| Ambulatory | 45 (10.9) |
| Practice location | |
| Rural | 9 (2.2) |
| City up to 200 000 residents | 120 (29.1) |
| City from 200 000 to 500,000 residents | 66 (16.0) |
| City above 500 000 residents | 217 (52.7) |
SD – standard deviation.
Knowledge about e-cigarettes
Among participants who were aware of e-cigarettes, the main sources of information about e-cigarettes were news stories (67.2%) or points of sale of e-cigarettes (67.6%). Over half of respondents (55.7%) indicated having learnt about e-cigarettes from family members or friends and only 20.9% of physicians gained knowledge about e-cigarettes from scientific articles or professional medical press (Figure 1).
Figure 1.
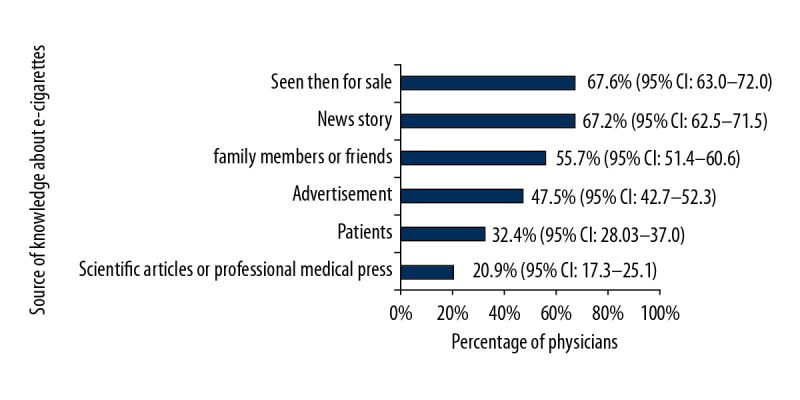
Source of physician knowledge about e-cigarettes.
Approximately 50.2% of respondents declared moderate knowledge about e-cigarettes and 24.3% of respondents rated their knowledge as poor (Table 3). Willingness to learn more about e-cigarettes was declared by the majority of participants (78.1%) as presented in Table 3. Females declared their willingness to learn more often than males (82.6% versus 70.1%; P=0.003). There were no significant differences in the perception of self-reported knowledge (P>0.05) about e-cigarettes between physicians trained in the surgical or non-surgical specialties. Nevertheless, physicians trained in non-surgical specialties declared willingness to learn more about e-cigarettes more often (83.2%), compared to those trained in surgical specialties (67.9%; P=0.003). Specialists more often declared a good or very good level of knowledge about e-cigarettes (33.9%) compared to physicians-in-training (21.3%; P=0.01).
Table 3.
Physicians’ awareness and knowledge about e-cigarettes (n=412).
| % (95% CI) | |
|---|---|
| Awareness of e-cigarettes | |
| Yes | 99.8 (98.6–100.0) |
| No | 0.2 (0.0–1.4) |
| Self-reported knowledge about e-cigarettes | |
| Nothing at all | 1.9 (1.0–3.8) |
| A little | 24.3 (20.4–28.6) |
| A moderate | 50.8 (45.9–55.5) |
| Somewhat strong | 21.1 (17.5–25.3) |
| Strong | 1.9 (1.0–3.8) |
| Willingness to learn more about e-cigarettes | |
| Strongly disagree | 3.2 (1.9–5.3) |
| Somewhat disagree | 18.7 (15.2–22.7) |
| Somewhat agree | 49.5 (44.7–54.3) |
| Strongly agree | 28.6 (24.5–33.2) |
CI – confidence interval.
Health effects of e-cigarettes
The vast majority of participants (96.5%) agreed (“rather agree” or “totally agree”) with the statement that e-cigarette use is harmful to the user’s health and 80.5% agreed that exhaled e-cigarette aerosol is harmful to bystanders (Table 1). Among participants, 40.9% disagreed (“rather disagree” or “totally disagree”) that e-cigarettes are less harmful than conventional cigarettes. Overall, according to the respondents, e-cigarettes are carcinogenic (86.1%), increase the risk of cardiovascular diseases (89.7%), and increase the risk of chronic lung diseases (85.2%). However, over one-third of physicians (36.4%) agreed with the statement that the risk of cancer is lower for the use of e-cigarettes compared to smoking conventional cigarettes and almost half of participants agreed that e-cigarette use, compared to cigarette smoking, is associated with a lower risk of cardiovascular or chronic lung diseases (Table 1).
Males more often agreed with the statement that, in contrast to conventional smoking, e-cigarette use is associated with lower risk of cancer (59.3% versus 71.5%; P=0.01), cardiovascular diseases (51.2% versus 66.7%; P=0.03), and chronic lung diseases (51.1% versus 67.3%; P=0.01). Specialists compared to physicians-in-training more often disagreed with the statement that e-cigarettes are less harmful than conventional cigarettes (66.6% versus 36.7%; P=0.0001). Participants who declared a hospital as a place of primary employment, compared to those who practice in ambulatory care, more often agreed with the statement that e-cigarettes are carcinogenic (86.6% versus 82.1%;P=0.02) and increase the risk of chronic lung diseases (86.7% versus 73.4%; P=0.02).
Addictive potential of e-cigarettes
Almost all of the respondents (97.1%) agreed with the statement that you can become addicted to e-cigarettes, and the majority (79.8%) disagreed that e-cigarettes are less addictive than conventional smoking (Table 1). The statement that e-cigarettes could be a “gateway” to conventional smoking was supported by 87% of participants. Among participants, 13.4% agreed that e-cigarettes should be recommended as a smoking cessation method, and 34% agreed that smokers who do not want to quit smoking should be encouraged to switch to e-cigarettes (Table 1).
Respondents who practice mainly in a hospital responded more often than their colleagues in the ambulatory care that they disagreed with the statement that e-cigarettes should be recommended as a smoking cessation tool (88.7% versus 68.9%; P=0.001). Among physicians, there were no statistically significant differences in the perceptions of health effects and addictive potential of e-cigarettes depending on the physicians’ specialty or practice location (P>0.05).
Legal regulations for e-cigarettes
As high as 84.3% of the participants agreed that the promotion and advertising of e-cigarettes should be banned. Most respondents also agreed that e-cigarette use should be prohibited for minors (97.1%), in public places (88.8%), and indoors (91.7%) (Table 1). There were no differences (P>0.05) in perceptions of legal provisions regarding e-cigarettes depending on the sex, level of training, specialty, practice type and practice location.
Discussion
To the authors’ best knowledge this is one of the biggest studies aiming to assess knowledge and beliefs concerning e-cigarette use among physicians representing various medical specialties, and the only one conducted among physicians in Poland. In our study almost all respondents (99.8%) were aware of e-cigarettes, which is a higher prevalence of awareness compared to those reported in the general population in Europe and US [35,36]. Such a high awareness of e-cigarettes may be due to the fact that this issue was widely discussed in the mass media, especially because the first e-cigarette regulation was introduced in 2016 by the amendment of the National Tobacco Control Act [20]. According to this document, e-cigarettes are considered equivalent to conventional tobacco cigarettes and this statement caused a great deal of discussion in the media.
We have observed that only 21% of physicians get information about e-cigarettes from scientific articles. Most participants learned about e-cigarettes from non-scientific sources such as news stories or storefronts. Information obtained from such sources are not scientifically verified and might be biased. This poses a threat that education and guidance about e-cigarettes delivered by physicians is not based on evidence. Similar results were observed among healthcare providers’ in the US where the most frequently reported source of knowledge about e-cigarettes were patients (62%) or news stories (39%) [34]. A study conducted with members of The British Thoracic Oncology Group revealed that 81% of clinicians reported being asked about e-cigarettes by patients [37]. Similarly, approximately 70% of primary-care physicians, pulmonologists, and surgeons in the US were asked about e-cigarettes by their patients [38]. Despite such a high interest in e-cigarettes among patients, many studies show that healthcare professionals feel uncomfortable discussing e-cigarettes [34,38–40]. Among lung-cancer specialists in South Korea, 83% reported being uncomfortable when discussing e-cigarettes with their patients [39]. In the US, more than half of pediatricians and primary-care physicians reported that they are not confident about their level of knowledge about e-cigarettes and ability to answer questions about e-cigarettes [34,38,41]. Healthcare professionals in the UK were hesitant before advising and potentially prescribing e-cigarettes [40]. General practitioners and nurses in the UK suggested that they need more evidence on e-cigarettes to feel comfortable in advising and potentially offering e-cigarettes to their patients [40]. In our study, only a quarter of participants declared a high level of knowledge about e-cigarettes, and three-quarters of physicians expressed their willingness to learn more about e-cigarettes. The aforementioned data indicate an urgent need to provide all healthcare providers with unbiased, evidence-based knowledge about e-cigarettes and their impact on health.
There is no scientific consensus about whether e-cigarette use can be used as a harm reduction tool. According to the experts of US National Academies of Sciences, Engineering, and Medicine (NASEM), e-cigarettes may pose less risk for health than combustible tobacco cigarettes and might also increase smoking cessation rates among adult tobacco smokers [9]. A different statement is presented by the European Respiratory Society Tobacco Control Committee (ERS TCC) [18]. The ERS committee stated that tobacco harm reduction strategies are based upon incorrect assumptions and undocumented claims about safety and effectiveness of alternative nicotine delivery products (including e-cigarettes) for smoking cessation [18]. In the opinion of the ERS, e-cigarettes should not be used as a population-based strategy in tobacco control [18].
In our study, according to the majority of respondents, e-cigarettes were considered as harmful both for user and bystanders. This is consistent with previously published data on beliefs about e-cigarettes among healthcare professionals from other countries [33,34,42,43]. In our study, over 80% of participants agreed that e-cigarette use increases the risk of cancer, cardiovascular, and chronic lung diseases. However, the health risks of e-cigarette use were perceived as lower than those of conventional cigarettes. More in depth consideration of the harmfulness of e-cigarettes among physicians who practice in the hospital may be a result of the fact that they encounter patients with more severe clinical cases compared to physicians working in the ambulatory care.
A group particularly exposed to the harmful effects of nicotine are adolescents whose developing brains are particularly sensitive to the impact of nicotine, including their addictive potential [44,45]. In our study, physicians almost unanimously agreed that e-cigarettes are addictive and their use by adolescents can lead to conventional cigarette use in the future (“the gateway effect”). Similar results were obtained in studies performed among physicians in the US, UK, and Belgium [33,34,40]. Three-quarters of US physicians believed that e-cigarettes could be a “gateway” to combustible tobacco products use [34]. A qualitative interview study revealed that physicians and nurses in the UK are aware of the safety of e-cigarettes and implications of their use on future nicotine dependence [40]. The vast majority (83%) of healthcare professionals in Belgium declared that e-cigarettes will cause renormalization of smoking and can lead to uptake of conventional cigarettes [33]. Despite the differences in approach to the harm reduction strategy presented in the statement prepared by the NASEM and the ERS, both organizations point to the possibility of a “gateway effect” and risk for transition from e-cigarette to combustible tobacco products among youth who started nicotine use with e-cigarettes [9,18].
E-cigarettes are promoted as a smoking cessation method [46]. Currently available evidence on the effectiveness of e-cigarettes in quitting smoking is debatable and further research is needed [47,48]. In this study, the largest variation in answers was found in the case of questions about the potential role of e-cigarettes as a tool in smoking cessation, especially among people who do not want to or failed to quit. The issue of recommending e-cigarettes to smokers and encouraging smokers to switch to e-cigarettes raises concerns among physicians globally [28,33,34,37–42]. Generally, physicians do not recommend e-cigarettes for smoking cessation due to the lack of evidence on their effectiveness and uncertainty regarding short-term and long-term safety [43]. The proportion of physicians who recommend e-cigarettes to the patients vary from 3.7% in the UK [37], 12% in South Korea [39], 33% in Greece [49], and up to 37.9% in the US [2]. In our study, 13.3% of physicians declared that they would recommend e-cigarettes to smoking patients, wherein only 1.5% of participants totally agreed with this statement. In the US, resident-physicians are less likely to recommend e-cigarettes to patients than practicing physicians [43]. In our study, specialists compared to physicians-in-training more often declared concerns about harmfulness of e-cigarettes, however, the frequency of recommendation of e-cigarettes to the patients was comparable (P>0.05) in both groups. Further studies are needed to assess the effect of e-cigarette use for smoking cessation and to achieve a scientific consensus on the role of e-cigarettes in quitting smoking.
This is one of the largest studies assessing perceptions of e-cigarettes among physicians. Our study has an important implication for public health, especially in view of shaping the policies on tobacco control. Results of our study support the call for further training and support of healthcare professionals regarding e-cigarette use, so that they may provide their patients with evidence-based information regarding e-cigarettes [32]. The group that should be particularly aware of e-cigarettes and their potential benefits and risks to health are primary care physicians responsible for providing smoking cessation intervention among smokers. In addition, our study can be a basis for further research, especially among individual groups of specialists, including general practitioners, oncologists, pulmonologists and psychiatrists.
This study has several limitations. First, it was narrowed down to a selected group of physicians attending a course at the School of Public Health, the Centre of Postgraduate Medical Education in Warsaw, Poland. However, participation in the course is compulsory for each of 25 000 physician undergoing specialty training in Poland and the group participating in the study represented different regions and healthcare institutions from all over Poland. Second, questions regarding perceptions of e-cigarettes were based on a 4-point scale. The interpretation of participants’ answers on these items may be problematic. Nevertheless, during the preparation of the questionnaire we tried to narrow down and refine the questions in detail. In addition, the results of the pilot study, where the questionnaire was validated, made it possible to develop a final precise research tool. Third, our findings should be interpreted with caution as they reflect general physicians’ attitudes and beliefs towards e-cigarettes, rather than the precise risk estimates.
Conclusions
Physicians in Poland perceive e-cigarettes as harmful and addictive, whereas the health risk of e-cigarettes use is perceived as lower than those of conventional cigarettes. Beliefs about the role of e-cigarette as a smoking cessation tool are diverse. Physicians’ knowledge about e-cigarettes is mostly based on non-scientific sources. Our study points out the urgent need to develop national smoking cessation guidelines regulating the use of e-cigarettes.
Footnotes
Source of support: Departmental sources
References
- 1.Zatoński WA, Zatoński M, Janik-Koncewicz K, Połtyn-Zaradna K, Wijatkowska K, Marciniak A. Hundred years of cigarette smoking in Poland: Three phases of the tobacco epidemic. J Health Inequal. 2017;3(2):118–22. [Google Scholar]
- 2.Jassem J, Przewoźniak K, Zatoński W. Tobacco control in Poland-successes and challenges. Transl Lung Cancer Res. 2014;3(5):280–85. doi: 10.3978/j.issn.2218-6751.2014.09.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kantar Public for Chief Sanitary Inspectorate. [cited 2019 Feb 16]. Available from: URL: https://gis.gov.pl/wp-content/uploads/2018/04/Postawy-Polak%C3%B3w-do-palenia-tytoniu-Raport-2017.pdf [in Polish]
- 4.Jankowski M, Brożek G, Lawson J, et al. E-smoking: Emerging public health problem? Int J Occup Med Environ Health. 2017;30(3):329–44. doi: 10.13075/ijomeh.1896.01046. [DOI] [PubMed] [Google Scholar]
- 5.Farsalinos KE, Poulas K, Voudris V, Le Houezec J. Electronic cigarette use in the European Union: Analysis of a representative sample of 27 460 Europeans from 28 countries. Addiction. 2016;111(11):2032–40. doi: 10.1111/add.13506. [DOI] [PubMed] [Google Scholar]
- 6.Goniewicz ML, Gawron M, Nadolska J, et al. Rise in electronic cigarette use among adolescents in Poland. J Adolesc Health. 2014;55(5):713–15. doi: 10.1016/j.jadohealth.2014.07.015. [DOI] [PubMed] [Google Scholar]
- 7.Caponnetto P, Campagna D, Papale G, et al. The emerging phenomenon of electronic cigarettes. Expert Rev Respir Med. 2012;6(1):63–74. doi: 10.1586/ers.11.92. [DOI] [PubMed] [Google Scholar]
- 8.Zhu SH, Sun JY, Bonnevie E, et al. Four hundred and sixty brands of e-cigarettes and counting: implications for product regulation. Tob Control. 2014;23(3):iii3–9. doi: 10.1136/tobaccocontrol-2014-051670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Academies of Science. Public Health Consequences of E-Cigarettes. [cited 2019 Jun 30]. Available from: URL: http://nationalacademies.org/hmd/Reports/2018/public-health-consequences-of-e-cigarettes.aspx. [PubMed]
- 10.Goniewicz ML, Smith DM, Edwards KC, et al. Comparison of nicotine and toxicant exposure in users of electronic cigarettes and combustible cigarettes. JAMA Netw Open. 2018;1(8):e185937. doi: 10.1001/jamanetworkopen.2018.5937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Margham J, McAdam K, Forster M, et al. Chemical composition of aerosol from an e-cigarette: A quantitative comparison with cigarette smoke. Chem Res Toxicol. 2016;29(10):1662–78. doi: 10.1021/acs.chemrestox.6b00188. [DOI] [PubMed] [Google Scholar]
- 12.Alzahrani T, Pena I, Temesgen N, Glantz SA. Association between electronic cigarette use and myocardial infarction. Am J Prev Med. 2018;55(4):455–61. doi: 10.1016/j.amepre.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Qasim H, Karim ZA, Silva-Espinoza JC, et al. Short-term e-cigarette exposure increases the risk of thrombogenesis and enhances platelet function in mice. J Am Heart Assoc. 2018;7(15):e009264. doi: 10.1161/JAHA.118.009264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glynos C, Bibli SI, Katsaounou P, et al. Comparison of the effects of e-cigarette vapor with cigarette smoke on lung function and inflammation in mice. Am J Physiol Lung Cell Mol Physiol. 2018;315(5):L662–72. doi: 10.1152/ajplung.00389.2017. [DOI] [PubMed] [Google Scholar]
- 15.Brożek GM, Jankowski M, Zejda JE. Acute respiratory responses to the use of e-cigarette: An intervention study. Sci Rep. 2019;9(1):6844. doi: 10.1038/s41598-019-43324-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Franck C, Filion KB, Kimmelman J, et al. Ethical considerations of e-cigarette use for tobacco harm reduction. Respir Res. 2016;17(1):53. doi: 10.1186/s12931-016-0370-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fairchild AL, Bayer R, Lee JS. The e-cigarette debate: What counts as evidence? Am J Public Health. 2019;109(7):1000–6. doi: 10.2105/AJPH.2019.305107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.European Respiratory Society. ERS Tobacco Control Committee. ERS Position Paper on Tobacco Harm Reduction. [cited 2019 Jun 30]. Available from: URL: https://ers.app.box.com/v/ERSTCC-Harm-Reduction-Position.
- 19.Kennedy RD, Awopegba A, De León E, Cohen JE. Global approaches to regulating electronic cigarettes. Tob Control. 2017;26(4):440–45. doi: 10.1136/tobaccocontrol-2016-053179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parliament of the Republic of Poland. Act from 22 July 2016 on amending the Act on Protection of Health against the Consequences of the Use of Tobacco and Tobacco Products in Poland. Journal of Laws from 24 August 2016 (item 1331) [cited 2019 Feb 16]. Available from: URL: http://prawo.sejm.gov.pl/isap.nsf/DocDetails.xsp?id=WDU20160001331 [in Polish]
- 21.World Health Organization. The role of health professionals in tobacco control. [cited 2019 Jun 30]. Available from: URL: https://www.who.int/tobacco/resources/publications/wntd/2005/bookletfinal_20april.pdf.
- 22.Pinget C, Martin E, Wasserfallen JB, et al. Cost-effectiveness analysis of a European primary care physician training in smoking cessation counseling. Eur J Cardiovasc Prev Rehabil. 2007;14(3):451–55. doi: 10.1097/HJR.0b013e32804955a0. [DOI] [PubMed] [Google Scholar]
- 23.Carson KV, Verbiest ME, Crone MR, et al. Training health professionals in smoking cessation. Cochrane Database Syst Rev. 2012;(5):CD000214. doi: 10.1002/14651858.CD000214.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Verbiest M, Brakema E, van der Kleij R, et al. National guidelines for smoking cessation in primary care: A literature review and evidence analysis. NPJ Prim Care Respir Med. 2017;27(1):2. doi: 10.1038/s41533-016-0004-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McRobbie H, Bullen C, Glover M, et al. New Zealand smoking cessation guidelines. N Z Med J. 2008;121(1276):57–70. [PubMed] [Google Scholar]
- 26.Jankowski P, Kawecka-Jaszcz K, Kopeć G, et al. Polish forum for prevention guidelines on smoking: Update 2017. Kardiol Pol. 2017;75(4):409–11. doi: 10.5603/KP.2017.0066. [DOI] [PubMed] [Google Scholar]
- 27.National Institute for Health and Clinical Excellence. Stop smoking interventions and services. [cited 2019 Jun 30]. Available from: URL: https://www.nice.org.uk/guidance/ng92/chapter/Recommendations#advice-on-ecigarettes.
- 28.Kandra KL, Ranney LM, Lee JGL, Goldstein AO. Physicians’ attitudes and use of e-cigarettes as cessation devices, North Carolina 2013. PLoS One. 2014;9:e103462. doi: 10.1371/journal.pone.0103462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.European Commission. Special Eurobarometer 458. Attitudes of Europeans towards tobacco and electronic cigarettes. [cited 2019 Feb 16]. Available from: URL: https://data.europa.eu/euodp/en/data/dataset/S2146_87_1_458_ENG.
- 30.Smith DM, Gawron M, Balwicki L, et al. Exclusive versus dual use of tobacco and electronic cigarettes among adolescents in Poland 2010–2016. Addict Behav. 2019;90:341–48. doi: 10.1016/j.addbeh.2018.11.035. [DOI] [PubMed] [Google Scholar]
- 31.Brożek GM, Jankowski M, Lawson JA, et al. The prevalence of cigarette and e-cigarette smoking among students in central and eastern Europe – results of the YUPESS study. Int J Environ Res Public Health. 2019;16:2297. doi: 10.3390/ijerph16132297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Erku DA, Gartner CE, Morphett K, Steadman KJ. Beliefs and self-reported practices of healthcare professionals regarding electronic nicotine delivery systems (ENDS): A mixed-methods systematic review and synthesis. Nicotine Tob Res. 2019 doi: 10.1093/ntr/ntz046. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 33.Van Gucht D, Baeyens F. Health professionals in Flanders perceive the potential health risks of vaping as lower than those of smoking but do not recommend using e-cigarettes to their smoking patients. Harm Reduct J. 2016;13(1):22. doi: 10.1186/s12954-016-0111-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pepper JK, McRee AL, Gilkey MB. Healthcare providers’ beliefs and attitudes about electronic cigarettes and preventive counseling for adolescent patients. J Adolesc Health. 2014;54(6):678–83. doi: 10.1016/j.jadohealth.2013.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xu Y, Guo Y, Liu K, et al. E-cigarette awareness, use, and harm perception among adults: A meta-analysis of observational studies. PLoS One. 2016;11(11):e0165938. doi: 10.1371/journal.pone.0165938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vardavas CI, Filippidis FT, Agaku IT. Determinants and prevalence of e-cigarette use throughout the European Union: A secondary analysis of 26 566 youth and adults from 27 Countries. Tob Control. 2015;24(5):442–48. doi: 10.1136/tobaccocontrol-2013-051394. [DOI] [PubMed] [Google Scholar]
- 37.Sherratt FC, Newson L, Field JK. Electronic cigarettes: A survey of perceived patient use and attitudes among members of the British thoracic oncology group. Respir Res. 2016;17(1):55. doi: 10.1186/s12931-016-0367-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nickels AS, Warner DO, Jenkins SM, et al. Beliefs, practices, and self-efficacy of us physicians regarding smoking cessation and electronic cigarettes: A national survey. Nicotine Tob Res. 2017;19(2):197–207. doi: 10.1093/ntr/ntw194. [DOI] [PubMed] [Google Scholar]
- 39.Shin DW, Kim YI, Kim SJ, et al. Lung cancer specialist physicians’ attitudes towards e-cigarettes: A nationwide survey. PLoS One. 2017;12(2):e0172568. doi: 10.1371/journal.pone.0172568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stepney M, Aveyard P, Begh R. GPs’ and nurses’ perceptions of electronic cigarettes in England: A qualitative interview study. Br J Gen Pract. 2019;69(678):e8–e14. doi: 10.3399/bjgp18X699821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gorzkowski JA, Whitmore RM, Kaseeska KR, et al. Pediatrician knowledge, attitudes, and practice related to electronic cigarettes. J Adolesc Health. 2016;59(1):81–86. doi: 10.1016/j.jadohealth.2016.03.036. [DOI] [PubMed] [Google Scholar]
- 42.Kanchustambham V, Saladi S, Rodrigues J, et al. The knowledge, concerns and healthcare practices among physicians regarding electronic cigarettes. J Community Hosp Intern Med Perspect. 2017;7(3):144–50. doi: 10.1080/20009666.2017.1343076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ofei-Dodoo S, Kellerman R, Nilsen K, et al. Family physicians’ perceptions of electronic cigarettes in tobacco use counseling. J Am Board Fam Med. 2017;30(4):448–59. doi: 10.3122/jabfm.2017.04.170084. [DOI] [PubMed] [Google Scholar]
- 44.Benowitz NL. Nicotine addiction. N Engl J Med. 2010;362(24):2295–303. doi: 10.1056/NEJMra0809890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yuan M, Cross SJ, Loughlin SE, Leslie FM. Nicotine and the adolescent brain. J Physiol. 2015;593(16):3397–412. doi: 10.1113/JP270492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.de Andrade M, Hastings G, Angus K. Promotion of electronic cigarettes: Tobacco marketing reinvented? BMJ. 2013;347:f7473. doi: 10.1136/bmj.f7473. [DOI] [PubMed] [Google Scholar]
- 47.Kalkhoran S, Glantz SA. E-cigarettes and smoking cessation in real-world and clinical settings: A systematic review and meta-analysis. Lancet Respir Med. 2016;4(2):116–28. doi: 10.1016/S2213-2600(15)00521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ghosh S, Drummond MB. Electronic cigarettes as smoking cessation tool: Are we there? Curr Opin Pulm Med. 2017;23(2):111–16. doi: 10.1097/MCP.0000000000000348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Moysidou A, Farsalinos KE, Voudris V, et al. Knowledge and perceptions about nicotine, nicotine replacement therapies and electronic cigarettes among healthcare professionals in Greece. Int J Environ Res Public Health. 2016;13(5):E514. doi: 10.3390/ijerph13050514. [DOI] [PMC free article] [PubMed] [Google Scholar]


