Abstract
An os acromiale occurs when any of the primary ossification centres of the acromion fail to fuse with the basi-acromion. It is present in approximately 8% of individuals, and whilst the majority of these individuals are unaffected it can cause significant pain and disability. It can impact seemingly unrelated surgical intervention in the region such as subacromial decompression and reverse shoulder arthroplasty. A painful os acromiale can be both a diagnostic challenge, and difficult to manage. There remain a wide variety of surgical practices with variable outcomes achieved. We present an evidence-based discussion of the surgical techniques described to date in the literature, alongside a comprehensive review of the incidence and pathophysiology of os acromiale.
This review was written after a comprehensive analysis of the literature to date relating to os acromiale. Particular focus was given to material examining surgical management techniques, and the condition’s incidence across different population groups.
Open reduction and internal fixation using cannulated screws, or tension band wiring have superior outcomes in the literature in the treatment of symptomatic os acromiale. There may be a biomechanical advantage of combining the two techniques. Preservation of large anterior deltoid attachment is necessary, with consideration being given to the local blood supply. There is likely no additional benefit from iliac crest vs local bone grafting. Research in this area remains of a low evidence level with small samples sizes. Appropriately powered clinical research of a higher-level evidence methodology is needed in order to differentiate further in the choice of surgical intervention.
Cite this article: EFORT Open Rev 2019;4:525-532. DOI: 10.1302/2058-5241.4.180100
Keywords: acromion, meso-aromion, meta-acromion, os acromiale, preacromion, shoulder pain, shoulder stiffness
Origins and pathoanatomy
When any of the primary ossification centres of the acromion fail to fuse to the basi-acromion the resulting non-union is termed an os acromiale.1 An early mention of this type of os in the literature comes from British anatomist John Gregory Smith in 1834. Cadaveric specimens with presumed injury to the shoulder joint were examined at the Hunterian Theatre of Anatomy in London, UK. The os acromiale is described in the published dissection notes as a ‘fracture of the humeral extremity of the clavicle, which extended into its articulation with the clavicle’.2 Later that century, the Austrian anatomist Wenzel Gurber coined the term os acromiale, and described a distinct synovial joint. At the time, Gurber was under the stewardship of Nikolay Pirogov at the famous Medical Military Academy in St Petersburg, Russia. Pirogov had recently returned from the Crimean War and is considered the founder of military field surgery.3,4 By the century’s end, Irishman Alexander Macalister at the University of Cambridge, UK, had completed a full definition of this condition.5,6
Understanding the developmental anatomy of the scapula remains important to surgeons confronted with affected patients. The scapula has at least nine ossification centres – three of these ossification centres form the adult acromion. The pre-acromion, meso-acromion, and meta-acromion. By 15 years to 18 years of age these have usually fused.1 Macalister’s work probably defines this process best, and he felt that there were likely many more nuclei preceding these.6 These principle nuclei allow the acromion to be divided into four anatomical regions (see Fig. 1). The pre-acromion, meso-acromion, meta-acromion, and basi-acromion, with a failure of any to fuse to the basi-acromial region resulting in an os acromiale.
Fig. 1.
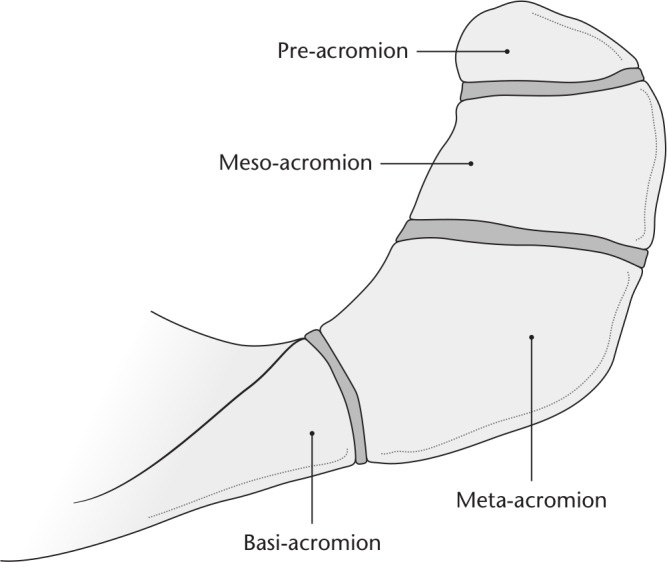
Acromial physes, and the resultant anatomical regions relevant to os acromiale. Illustration provided by Antbits Ltd.
Population prevalence
Both anatomical and radiological studies examining the frequency of os acromiale exist in the literature (see Table 1).5–13 Early anatomical studies from Gruber, and Macalister suggest an incidence ranging from 3% to 15%.5,6 In the modern literature, Sammarco suggests an incidence of 8% from the examination of 1198 scapulas from the Hamann–Todd osteological collection in Cleveland, USA.9 The collection remains the largest documented collection of modern human skeleton remains worldwide.
Table 1.
A summary of studies in the literature examining the incidence of os acromiale across different populations
| Author | Year | Type | No. of cases | Methodology | Frequency of os acromiale (%) | Frequency of bilaterality (%) |
|---|---|---|---|---|---|---|
| Gruber5 | 1863 | Anatomical | 100 | Cadaveric dissection | 3.0 | Not reported |
| Macalister6 | 1893 | Anatomical | 100 | Examination of museum specimens | 15.0 | Not reported |
| Edelson et al7 | 1993 | Anatomical | 270 | Specimens from three archaeological sites | 8.2 | Not reported |
| Nicholson et al8 | 1996 | Anatomical | 420 | Examination of museum specimens | 8.0 | 41 |
| Sammarco9 | 2000 | Anatomical | 1198 | Examination of museum specimens | 8.0 | 33 |
| Liberson10 | 1937 | Radiological | 1800 | Sagittal plane radiographs (a modified axillary view for some cases) | 2.7 | 62 |
| Grasso11 | 1992 | Radiological | 398 | Anteroposterior and axillary radiographs and CT | 9.5 | Not reported |
| Burbank12 | 2007 | Radiological | 93 | Anteroposterior, scapular Y and axillary radiographs | 6.5 | Not reported |
| Rovesta et al13 | 2017 | Radiological | 1042 | MRI imaging of shoulder region | 3.4 | Not reported |
Radiologically, Burbank et al identified an incidence of 6.5% using axillary radiographs from 93 patients presenting to an upper limb clinic with shoulder pain.12 The most recent evidence using MRI imaging in a cohort of 1042 patients suggests a lower frequency of 3.4%.13 Examination of Table 1 suggests a spread of frequency from 2.7–15.0% with generally higher frequencies seen in anatomical studies. Of note, Sammarco reports a significant demographic variance. Os acromiale was seen in 13.2% of Afro-Caribbean specimens, vs 5.8% of Caucasian specimens, and 8.5% of male specimens, vs 4.9% of female specimens.9 The strong influence of demographic factors is likely to contribute to this observed variance. Taking the evidence in its totality, clinicians in European and North American healthcare settings can expect an os acromiale to be present in up to 8% of their patients, noting that it is likely to be more common than this in certain ethnic groupings.
Pathophysiology
Most diagnoses of os acromiale are made incidentally on axillary view radiographs of the shoulder.10,12,14 The unfused segment is most commonly the meso-acromion. This represents what is often termed a meso-type os acromiale. Any primary shoulder pain is usually unrelated to the unfused os. If the os acromiale is driving symptoms then there are two principle causes for this: motion at the non-union site, or an impingement-type syndrome resulting from flexion of the os fragment during deltoid contraction and arm elevation.15 Pain from an os acromiale by this mechanism has been reported on in a variety of sports, in particular among throwing athletes and swimmers.16–18 Previously stable non-unions can become unstable following an episode of blunt trauma to the region, such as might occur following direct impact to the shoulder region when tacking another player during a game of American football.19
Diagnosis
Patients often present with non-specific symptoms. These can include shoulder pain localized to the anterolateral acromion, a difficulty in performing overhead activities, night-time pain, and weakness. All can be associated with other conditions, such as those seen with impingement syndrome.20 Examination findings can be similarly general with localized acromial tenderness, reduced range of motion, and positive impingement signs.20,21 As a result it is important to exclude other causes before embarking on a management programme focused solely on os acromiale as the primary symptom generator.
Particular attention should be paid in the history to any precipitating episode of blunt trauma to the shoulder region.22 Gross motion of an unstable os fragment is also occasionally detectable on examination.23 Routine radiographs should include anteroposterior, and axillary views of the affected shoulder. The presence of an os acromiale is best appreciated on the axillary view. Once an os acromiale has been identified, and other causes of the patient’s symptoms excluded, further other imaging modalities may be useful. The presence of bone oedema on T2 fat-suppressed magnetic resonance axial images can add weight to the os acromiale being the cause of symptoms. A T2 fat-suppressed image showing a meso-type os acromiale is shown in Fig. 2. These should be considered alongside traditional T1, and T2 image series. Short T1 inversion recovery (STIR) sequences can also be used. If the diagnosis remains unclear, a technetium bone scan, and the injection of local anaesthetic into the non-union site with both repeat clinical examination and completion of a pain diary for a defined period, can be useful.
Fig. 2.
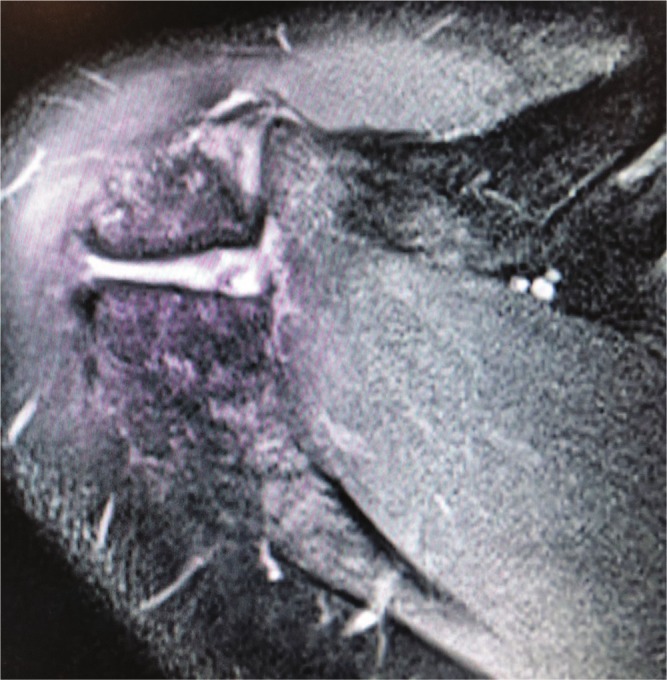
T2 weighted MRI showing a meso-type os acromiale.
Axial cut of fat-suppressed T2-weighted MRI of a rugby player with associated bone marrow oedema – newly symptomatic from a meso-type os acromiale following an episode of trauma during play.
Medicolegal considerations
The other important cause of a symptomatic unstable os acromiale is iatrogenic. Its presence or not should be identified prior to embarking on any intervention in the shoulder – but it takes on great relevance in reverse shoulder arthroplasty, and any procedure involving subacromial decompression.24,25 Removal of bone on the under surface of the acromion (such as during a decompression) in the presence of an unfused fragment, can result in destabilization, leading to pain, and disability. Excessive acromial tilting and os fragmentation has been noted when reverse shoulder arthroplasty is performed in the presence of an os – although its clinical significance remains unclear.24–27 Preoperative fixation has been used successfully in patients undergoing anatomic shoulder arthroplasty, although its potential value in patients undergoing reverse remains uncertain.28
The presence of an os acromiale is an important cause of failed arthroscopic subacromial decompression (ASAD).29,30 Once its presence is known this must be recorded in the clinical notes, and the patient adequately counselled as to the risks of the decompression. Alternatively, a more conservative resection can be undertaken, or other management strategies pursued.
Management
Once the diagnosis of a symptomatic os acromiale has been made, patients should be given a trial of conservative treatment. A thought process similar to that employed when treating subacromial impingement is used with treatment tailored towards the needs of the individual patient. Generally, this would include activity modification, rest, and local application of cold or heat, in conjunction with systemic non-steroidal anti-inflammatory medication. A course of steroid injections into the subacromial space can be used to augment this, with no more than three to four injections given in total. Physiotherapy is commenced at the onset, which can be increased as symptoms allow. This should follow an impingement protocol – starting with gentle exercises focused on range of movement, then progressing to those focused on muscle strengthening.31
A conservative based approach should be persisted with over a 6-to-12-month period, except in those individuals with concurrent large cuff tears in which early surgical intervention may be appropriate. A wide variety of surgical techniques have been described to date in the literature for those patients who fail to improve with conservative treatment. The principle papers are summarized in Table 2, and represent over 35 years of evidence on the subject. Fragment excision, acromionectomy, open reduction and internal fixation (ORIF), and isolated ASAD are all proposed amongst other techniques. The majority of the evidence explores the treatment of meso-type os acromiale.32
Table 2.
A summary of studies in the literature examining different surgical treatment strategies for symptomatic os acromiale
| Author | Year | Journal | Treatment | Open/arthroscopic | Study type | Study participant no. (N) | Conclusion |
|---|---|---|---|---|---|---|---|
| Neer and Marberry35 | 1981 | JBJS | Radical acromionectomy | Open | Retrospective case series (> 80% acromion removed) | 30 | Poor results due to deltoid failure |
| Mudge et al33 | 1984 | JBJS | Os fragment excision (+/- rotator cuff repair) | Open | Single surgeon case series | 6 | Excision of small os fragments alleviated symptoms in 4/6 patients |
| Armengol et al34 | 1994 | JSES | Os fragment excision | Open | Single surgeon case series | 40 | No improvements in symptoms |
| Warner et al23 | 1998 | JBJS | ORIF using 3.5 mm cannulated screws + TBW and iliac crest bone grafting | Open | Prospective single centre case series | 14 | In favour of ORIF with cannulated screws, TBW, and iliac crest graft |
| Hertel et al37 | 1998 | JSES | Comparison of two surgical approaches. ORIF using TBW. Anterior deltoid off and transacromial | Open | Prospective single centre case series | 15 | Radiological union (axillary view). 3/7 deltoid off vs 7/8 transacromial. Higher constant scores when union achieved |
| Ryu et al38 | 1999 | Orthopaedics | ORIF using 3.5 mm cannulated screws | Open | Single surgeon case series | 4 | Improvement in UCLA from 19 to 35 |
| Satterlee42 | 1999 | JSES | Dorsal wedge osteotomy of non-union + ORIF using 4.5 mm Herbert screws and suture TBW | Open | Single surgeon case series | 6 | 6/6 excellent JSES PRO scores postoperatively |
| Wright et al46 | 2000 | Arthroscopy | Extended arthroscopic subacromial decompression | Arthroscopic | Single surgeon case series | 12 | UCLA score from 17–31 at 12 months |
| Boehm et al48 | 2003 | BJJ | Comparison of outcomes in open fragment excision, ORIF, and ASD | Open/ arthroscopic | Retrospective case series comparing fragment excision, ORIF, and ASD | 31 | No difference between different treatment |
| Peckett et al39 | 2004 | JSES | ORIF using a variety of methods; k-wires, TBW, and 3.5 mm cannulated screws in patients who failed to have relief from ASD. Local bone grafting. | Open | Prospective single centre case series | 26 | 25/26 radiological union at four months. 24/26 satisfied |
| Neyton et al30 | 2014 | JSES | Acromial and deltoid reconstruction ORIF + iliac crest bone graft after failed subacromial decompression for meso-type os acromiale | Open | Single surgeon case series | 2 | 2/2 radiographic union at 6/12. Improvement in symptoms and shoulder function |
| Spiegl et al40 | 2015 | JSES | Comparison of biomechanical properties of ORIF using 3.5 mm cannulated screws alone vs 3.5 mm cannulated screws and TBW | N/A | Lab-based biomechanical prospective study in cadavers | 28 | Strongest fixation (higher load to failure) with 3.5 mm cannulated screws inserted in AP direction supplemented with TBW |
| Lebus et al41 | 2017 | Arthrosc Tech | Description of surgical technique based on biomechanical work by Spiegl et al | Arthroscopic | Detailed description of technique with video material | 1 | Operative demonstration of technique from biomechanical work |
| Atinga et al28 | 2018 | JSES | Comparison of different TBW techniques, and iliac crest vs local bone grafting | Open | Single surgeon case series | 32 | No difference between TBW techniques or bone graft harvest site. 100% union at three months postoperatively |
Notes. ORIF, open reduction and internal fixation; TBW, tension band wiring; UCLA, University of California Los Angeles; JSES PRO, Journal of Shoulder & Elbow Surgery patient reported outcome; ASD, arthroscopic subacromial decompression.
Historically, Mudge et al33 had good results with fragment excision and deltoid reconstruction onto the remaining acromion in a single surgeon series of six patients with concurrent rotator cuff tears. Repair of the rotator cuff was also performed. However, ten years later Armengol et al,34 in a much larger single surgeon series of 41 patients, had no satisfactory results with this technique.
Both Mudge et al and Armengol et al’s work cautions against large fragment excision, and this is further supported in work by Charles Neer in New York, USA. His principle concern was defunctioning of the deltoid lever arm. He reported very poor results with a series of 30 patients referred to himself and Marberry following radical acromionectomy (< 80% of the acromion removed); of these, 27 (90%) had persistent pain and were unable to lift the affected limb above 90 degrees.35 It has been suggested that a failure to adequately reconstruct the deltoid is a reason for poor results with acromial resection.36
Various methods of ORIF exist in the literature and avoid some of the complications associated with fragment excision. These include tension band wiring (TBW), sutures, and cannulated screws with and without augmentation with bone graft. Warner et al23 in Pittsburgh, USA were among the first to publish single surgeon series data on the use of TBW constructs supplemented by iliac crest bone graft with poor results – 4/5 patients had symptomatic non-union. Results were improved significantly, however, when the construct was further augmented by 4.0 mm cannulated screws – 6/7 with improvement in symptoms and union. Good results have been achieved with TBW in isolation by Hertel et al.37 Their work emphasized the importance of the surgical approach utilized. A high non-union rate was seen when an anterior ‘deltoid off’ approach was used, as opposed to a transacromial approach – thereby preserving the terminal branches of the thoracoacromial artery and potentially improving the physiological environment for healing. More recently, Neyton et al in France have also used TBW as a construct method with good results.30
Evidence also exists in support of the use of cannulated screws as an isolated construct. Ryu et al38 performed ORIF using 3.5 mm cannulated screws placed from anterior to posterior and supplemented by local bone graft obtained from the humeral head. Four out of four patients achieved union, and symptomatic benefit.
Peckett et al39 used a variety of methods of ORIF in case series of 26 patients based in three separate centres in Australia, USA, and the UK. Success was achieved using either k-wires or 3.5 mm cannulated screws, which were then supplemented by TBW. It was felt that 3.5 mm screws should be used in preference to k-wires in patients whose bone stock allowed this method of fixation.
Fixation methods have also been compared in laboratory settings. The biomechanical properties of 4.0 mm cannulated screws alone, vs when the screws are augmented by a TBW construct have been compared at The Steadman Philippon Research Institute in Vail, USA.40 The researchers simulated meso-type os acromiale in 12 matched pairs of cadaveric acromia. A high-strength suture tape was inserted into the acromion 1 cm form the anterior tip in order to test the two fixation construct types. The mean load to failure was 336 N when the screws were augmented with TBW vs 242 N when used in isolation – 39% higher. This fixation method was then described in a case report using a transacromial approach by the group with good results.41
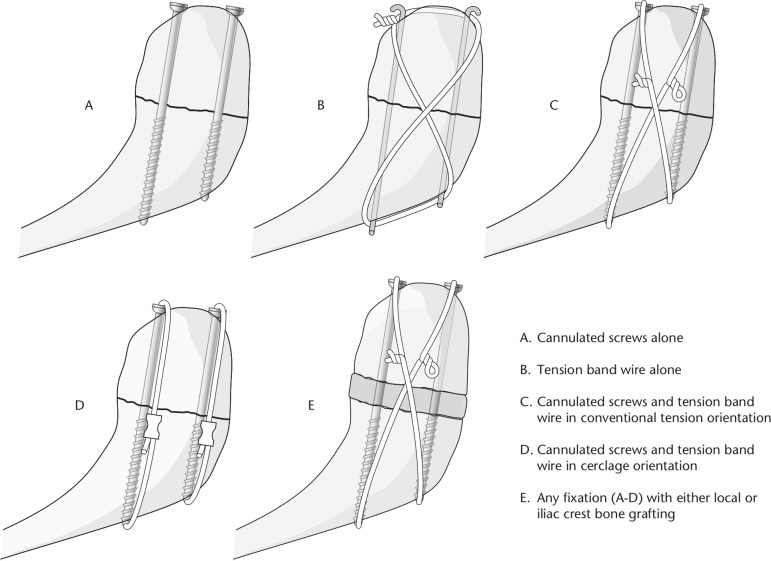
Most recently outcomes have been compared between iliac crest vs local bone grafting when using a similar fixation technique of cannulated screws augmented with TBW. The TBW was constructed using either a conventional tension orientation, or in a modified cerclage orientation. Local bone graft was obtained from the non-union site during preparation. All 32 patients in both groups were fused clinically and radiologically at three months postoperatively, with no difference in complication rates between the two groups. This suggests no benefit from iliac crest over local bone graft.28 In addition, there appears to be no significance in the orientation of the TBW construct. An overview of fixation methods is shown in Fig. 3.
Fig. 3.
Illustrations showing the principle surgical techniques for managing symptomatic os acromiale. Illustration provided by Antbits Ltd.
Other techniques focus on relieving subacromial impingement, either by fragment movement or decompression. Satterlee et al describe a technique whereby a dorsal wedge osteotomy is used to tilt the anterior os fragment upward, thereby increasing subacromial space and relieving any impingement.42
ASAD is a well-established technique for the treatment of subacromial impingement in patients who have failed a conservative treatment programme.43,44 However, some concerns exist regarding its efficacy, and there is limited evidence for its use as a treatment option in patients with symptomatic unstable os acromiale.45,46 Potential benefits, however, include the avoidance hardware, and a smaller surgical footprint associated with other management options. Ortiguera et al14 have previously described an arthroscopic technique and routine for meso-type os acromiale, citing evidence from Hutchinson and Veenstra’s work ten years previously.47 There remains a low volume of modern contemporary evidence in support of this as a primary treatment methodology, and given the concerns surrounding conversion of a stable os towards instability, the use of ASAD in these patients should be considered very carefully, if not avoided altogether.
The postoperative management of patients varies considerably in the literature and is dictated in some part by the treatment employed. There is no clear evidence in support of one particular methodology. Regimens described after ORIF include a period of spica cast, or up to eight weeks shoulder rest on a 60° abduction pillow. However, good results have also been achieved with sling immobilization in isolation, with passive range of motion (ROM) allowed from day one, and full unrestricted ROM from 12 weeks.41
Conclusions
Symptomatic unstable os acromiale can be both a challenging condition to diagnose and to treat when conservative methods fail. An os acromiale may be present in as many as one in ten patients. Given this, and the commonality of shoulder pain, and other non-specific sequelae, in practice it seems likely that an unstable os may well be an underdiagnosed symptom generator. It becomes increasingly relevant as a differential diagnosis in contact athletes, and those who partake in sports with a significant overhead component.
It is of paramount importance to identify those patients who have an os acromiale, as its presence can be a key determiner in the suitability and outcome of seemingly unrelated surgical interventions in the shoulder region. This can have devastating consequences with medicolegal repercussions. It is best evaluated for using axillary view radiographs. It remains unclear whether concurrent os fixation can alter the outcome in procedures of risk such as reverse shoulder arthroplasty.
Conservative treatment should nearly always form the mainstay of initial treatment and be persisted with for up to 12 months. Only when this fails should surgical intervention be considered in appropriately selected and counselled patients.
Evidence is limited, and surgical intervention techniques vary considerably. However, we can glean that it is largely in favour of ORIF over other methodologies. Preservation of large anterior deltoid attachment is necessary, with consideration to the local blood supply. There is likely no additional benefit from iliac crest vs local bone grafting. Whatever fixation method is chosen, bony union is the primary focus, with improved functional outcome, and reduced pain when this is successful. Consideration must be given as to the biological footprint of the hardware being utilized, with a view taken on the likely need for later removal. A meticulous surgical technique will as always ensure the best results possible are achieved whatever method chosen by the surgeon. Overall, the choice of implant type should be dictated by surgeon familiarity and patient factors, representing a tailored approach.
In the postoperative period, patients should usually be allowed free passive ROM as dictated by comfort, with a restriction on contact activity, and heaving loading of the limb for up to 12 weeks, or until radiological union is seen. Physiotherapy should be initiated at an early point to assist in rehabilitation and avoid complications of excessive stiffness.
Further biomechanical studies, and appropriately powered clinical research representing a higher-level evidence methodology, are needed in order to differentiate further in the choice of surgical intervention in this area. There remains a compelling need for this. However, adherence to certain key principles can ensure that this condition is safely, and adequately, managed in the interim.
Footnotes
ICMJE Conflict of interest statement: TMG reports consultancy to Evolutis and a patent planned, pending or issued for a shoulder apparatus system.
PR and SAH declare no conflict of interest relevant to this work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Folliasson A. Un cas d’os acromial. Rev Orthop 1933;20:533–538. [Google Scholar]
- 2. Smith JG. The classic: pathological appearances of seven cases of injury of the shoulder-joint: with remarks. Clin Orthop Relat Res 2010;468:1471–1475. (Originally published 1834). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hendriks IF, Bovill JG, Boer F, Houwaart ES, Hogendoorn PC. Nikolay Ivanovich Pirogov: a surgeon’s contribution to military and civilian anaesthesia. Anaesthesia 2015;70:219–227. [DOI] [PubMed] [Google Scholar]
- 4. Hendriks IF, Bovill JG, van Luijt PA, Hogendoorn PC. Nikolay Ivanovich Pirogov (1810–1881): a pioneering Russian surgeon and medical scientist. J Med Biogr 2018;26:10–22. [DOI] [PubMed] [Google Scholar]
- 5. Gruber W. Über die Arten der Acromialknochen und accidentellen Acromialgelenke. Archiv Anatomie, Physiol Wiss Medicin 1863:373–387. [Google Scholar]
- 6. Macalister A. Notes on acromion. J Anat Physiol 1893;27:1–51. [PMC free article] [PubMed] [Google Scholar]
- 7. Edelson JG, Zuckerman J, Hershkovitz I. Os acromiale: anatomy and surgical implications. J Bone Joint Surg Br 1993;75:551–555. [DOI] [PubMed] [Google Scholar]
- 8. Nicholson GP, Goodman DA, Flatow EL, Bigliani LU. The acromion: morphologic condition and age-related changes. A study of 420 scapulas. J Shoulder Elbow Surg 1996;5:1–11. [DOI] [PubMed] [Google Scholar]
- 9. Sammarco VJ. Os acromiale: frequency, anatomy, and clinical implications. J Bone Joint Surg Am 2000;82:394–400. [DOI] [PubMed] [Google Scholar]
- 10. Liberson F. Os acromiale: a contested anomaly. J Bone Joint Surg 1937;19:683–689. [Google Scholar]
- 11. Grasso A. [The incidence and role of the os acromiale in the acromiohumeral impingement syndrome]. Radiol Med 1992;84:567–570. [PubMed] [Google Scholar]
- 12. Burbank KM, Lemos MJ, Bell G, Lemos DW. Incidence of os acromiale in patients with shoulder pain. Am J Orthop (Belle Mead NJ) 2007;36:153–155. [PubMed] [Google Scholar]
- 13. Rovesta C, Marongiu MC, Corradini A, Torricelli P, Ligabue G. Os acromiale: frequency and a review of 726 shoulder MRI. Musculoskelet Surg 2017;101:201–205. [DOI] [PubMed] [Google Scholar]
- 14. Ortiguera CJ, Buss DD. Surgical management of the symptomatic os acromiale. J Shoulder Elbow Surg 2002;11:521–528. [DOI] [PubMed] [Google Scholar]
- 15. Kurtz CA, Humble BJ, Rodosky MW, Sekiya JK. Symptomatic os acromiale. J Am Acad Orthop Surg 2006;14:12–19. [DOI] [PubMed] [Google Scholar]
- 16. Bedi A, Rodeo SA. Os acromiale as a cause for shoulder pain in a competitive swimmer: a case report. Sports Health 2009;1:121–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Frizziero A, Benedetti MG, Creta D, Moio A, Galletti S, Maffulli N. Painful os acromiale: conservative management in a young swimmer athlete. J Sports Sci Med 2012;11:352–356. [PMC free article] [PubMed] [Google Scholar]
- 18. Demetracopoulos CA, Kapadia NS, Herickhoff PK, Cosgarea AJ, McFarland EG. Surgical stabilization of os acromiale in a fast-pitch softball pitcher. Am J Sports Med 2006;34:1855–1859. [DOI] [PubMed] [Google Scholar]
- 19. Anwar I, Amiras D, Khanna M, Walker M. Physes around the shoulder girdle: normal development and injury patterns. Clin Radiol 2016;71:702–709. [DOI] [PubMed] [Google Scholar]
- 20. Neer CS., II Impingement lesions. Clin Orthop Relat Res 1983;173:70–77. [PubMed] [Google Scholar]
- 21. Spangehl MJ, Hawkins RH, McCormack RG, Loomer RL. Arthroscopic versus open acromioplasty: a prospective, randomized, blinded study. J Shoulder Elbow Surg 2002;11:101–107. [DOI] [PubMed] [Google Scholar]
- 22. Sassmannshausen G, Wilson TC, Mair SD. Operative stabilization of an unstable os acromiale in an adolescent football player. Orthopedics 2003;26:509–511. [DOI] [PubMed] [Google Scholar]
- 23. Warner JJ, Beim GM, Higgins L. The treatment of symptomatic os acromiale. J Bone Joint Surg Am 1998;80:1320–1326. [DOI] [PubMed] [Google Scholar]
- 24. Mottier F, Wall B, Nove-Josserand L, Galoisy Guibal L, Walch G. Prothèse d’épaule inversée en présence de mésoacromion ou d’acromion fracturé. Rev Chir Orthop Repar Appar Mot 2007;93:133–141. [DOI] [PubMed] [Google Scholar]
- 25. Aibinder WR, Schoch BS, Cofield RH, Sperling JW, Sánchez-Sotelo J. Reverse shoulder arthroplasty in patients with os acromiale. J Shoulder Elbow Surg 2017;26:1598–1602. [DOI] [PubMed] [Google Scholar]
- 26. Walch G, Mottier F, Wall B, Boileau P, Molé D, Favard L. Acromial insufficiency in reverse shoulder arthroplasties. J Shoulder Elbow Surg 2009;18:495–502. [DOI] [PubMed] [Google Scholar]
- 27. Familiari F, Huri G, Gonzalez-Zapata A, McFarland EG. Scapula fracture and os acromiale after reverse total shoulder arthroplasty. Orthopedics 2014;37:434, 492–495. [DOI] [PubMed] [Google Scholar]
- 28. Atinga M, Gregor R, Selvaraj KM, Hong TF. Os acromiale open reduction and internal fixation: a review of iliac crest autogenous bone grafting and local bone grafting. J Shoulder Elbow Surg 2018;27:1030–1036. [DOI] [PubMed] [Google Scholar]
- 29. Dopirak R, Ryu RK. Management of the failed arthroscopic subacromial decompression: causation and treatment. Sports Med Arthrosc Rev 2010;18:207–212. [DOI] [PubMed] [Google Scholar]
- 30. Neyton L, Noël E, Walch G, Pons-Villanueva J. Acromion reconstruction after failed subacromial decompression in shoulders with os acromiale (meso-acromion): the tongue-and-groove assembly. J Shoulder Elbow Surg 2014;23:e261–e265. [DOI] [PubMed] [Google Scholar]
- 31. Fukuda H. The management of partial-thickness tears of the rotator cuff. J Bone Joint Surg Br 2003;85:3–11. [DOI] [PubMed] [Google Scholar]
- 32. Harris JD, Griesser MJ, Jones GL. Systematic review of the surgical treatment for symptomatic os acromiale. Int J Shoulder Surg 2011;5:9–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mudge MK, Wood VE, Frykman GK. Rotator cuff tears associated with os acromiale. J Bone Joint Surg Am 1984;66:427–429. [PubMed] [Google Scholar]
- 34. Armengol J, Brittis D, Pollock R, Flatow E, Self E, Bigliani L. The association of an unfused acromial epiphysis with tears of the rotator cuff: a review of 42 cases. J Shoulder Elbow Surg 1994;3:S14. [Google Scholar]
- 35. Neer CS, II, Marberry TA. On the disadvantages of radical acromionectomy. J Bone Joint Surg Am 1981;63:416–419. [PubMed] [Google Scholar]
- 36. Bosley RC. Total acromionectomy: a twenty-year review. J Bone Joint Surg Am 1991;73:961–968. [PubMed] [Google Scholar]
- 37. Hertel R, Windisch W, Schuster A, Ballmer FT. Transacromial approach to obtain fusion of unstable os acromiale. J Shoulder Elbow Surg 1998;7:606–609. [DOI] [PubMed] [Google Scholar]
- 38. Ryu RK, Fan RS, Dunbar WH V. The treatment of symptomatic os acromiale. Orthopedics 1999;22:325–328. [DOI] [PubMed] [Google Scholar]
- 39. Peckett WR, Gunther SB, Harper GD, Hughes JS, Sonnabend DH. Internal fixation of symptomatic os acromiale: a series of twenty-six cases. J Shoulder Elbow Surg 2004;13:381–385. [DOI] [PubMed] [Google Scholar]
- 40. Spiegl UJ, Smith SD, Todd JN, Wijdicks CA, Millett PJ. Biomechanical evaluation of internal fixation techniques for unstable meso-type os acromiale. J Shoulder Elbow Surg 2015;24:520–526. [DOI] [PubMed] [Google Scholar]
- 41. Lebus GF, Fritz EM, Hussain ZB, Pogorzelski J, Millett PJ. Operative treatment of symptomatic meso-type os acromiale. Arthrosc Tech 2017;6:e1093–e1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Satterlee CC. Successful osteosynthesis of an unstable mesoacromion in 6 shoulders: a new technique. J Shoulder Elbow Surg 1999;8:125–129. [DOI] [PubMed] [Google Scholar]
- 43. Ellman H. Arthroscopic subacromial decompression: analysis of one- to three-year results. Arthroscopy 1987;3:173–181. [DOI] [PubMed] [Google Scholar]
- 44. Ellman H, Kay SP. Arthroscopic subacromial decompression for chronic impingement. Two- to five-year results. J Bone Joint Surg Br 1991;73:395–398. [DOI] [PubMed] [Google Scholar]
- 45. Beard DJ, Rees JL, Cook JA, et al. ; CSAW Study Group. Arthroscopic subacromial decompression for subacromial shoulder pain (CSAW): a multicentre, pragmatic, parallel group, placebo-controlled, three-group, randomised surgical trial. Lancet 2018;391(10118):329–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wright RW, Heller MA, Quick DC, Buss DD. Arthroscopic decompression for impingement syndrome secondary to an unstable os acromiale. Arthroscopy 2000;16:595–599. [DOI] [PubMed] [Google Scholar]
- 47. Hutchinson MR, Veenstra MA. Arthroscopic decompression of shoulder impingement secondary to os acromiale. Arthroscopy 1993;9:28–32. [DOI] [PubMed] [Google Scholar]
- 48. Boehm TD, Matzer M, Brazda D, et al. Os acromiale associated with tear of the rotator cuff treated operatively. Review of 33 patients. J Bone Joint Surg Br 2003;85:545–549. [DOI] [PubMed] [Google Scholar]