Abstract
With advances in the treatment of femoral shaft nonunion after intramedullary nailing, the optimal option remains controversial. This study aimed to quantitatively investigate outcomes in a comparison of exchange nailing and augmentative plating for femoral shaft nonunion after intramedullary nailing.
The EMBASE, PubMed, Cochrane library and Clinical databases were systematically searched dating from their inception to March 2018. All retrospective controlled and prospective trials evaluating exchange nailing and augmentative plating for the treatment of femoral shaft nonunion after intramedullary nailing were identified. Two investigators extracted all related data independently and we used the review manager software to perform the meta-analysis.
Three studies with a total of 232 patients were eligible for data extraction in our study. The meta-analysis indicated that the augmentative plating group had a lower nonunion rate, shorter time to union, less intra-operative blood loss, and shorter operative time than the exchange nailing group. While for the infection rate, there was no significant difference between augmentative plating and exchange nailing group.
The available evidence has shown that augmentative plating is superior to exchange nailing for femoral shaft nonunion after intramedullary nailing.
Cite this article: EFORT Open Rev 2019;4:513-518. DOI: 10.1302/2058-5241.4.180054
Keywords: femoral shaft nonunion, intramedullary nailing, meta-analysis, treatment
Introduction
Intramedullary nailing (IMN) has been a standard for treating acute adult femur shaft fracture for decades. It is known that the nonunion or delayed union rate after IM nailing for acute femoral shaft fractures is less than 2%.1,2 However, a cohort study showed that the nonunion or delayed union might be more general than expected. Pihlajamäk et al even reported that the nonunion rate reached 12.5%.3 The femoral shaft nonunion or delayed union after intramedullary nailing not only results in considerable morbidity but also increases social and financial burdens.
According to the diagnostic criteria made by the United States Food and Drug Administration (FDA), a nonunion is when a fracture fails to union over a period of nine or more months or fails to prove any radiographic clues of healing response in an osseous environment within the previous three months of the follow-up.
There are several treatment selections for femoral shaft nonunion or delayed union including exchanging a larger size nailing, augmentative plating with the nailing in situ, dynamization, bone grafting alone, and use of a compression plate after nail removal.3–7 The variety of methods advocated for nonunion or delayed union inferred the lack of a gold standard. Among these methods, exchange for a larger IMN has been put forward as a perfect option for aseptic femoral shaft nonunion or delayed union after IMN fails with bony union rates from 72% to as high as 100%.3,8,9 However, Weresh et al reported the failure rate is even as high as 47%.10 On the other hand, Birjandinejad et al described the high success rates of 100% in femur shaft nonunion after augmentation plating.11 The optimal option for the treatment of femoral shaft nonunion or delayed union after nailing remains controversial.
Several studies have compared exchange nailing and augmentative plating for femur shaft nonunion after nailing.12–14 On the other hand, both treatments have different advantages and disadvantages. Hence, it is necessary to assess the efficiency of different treatments between exchange nailing and augmentative plating based on the available evidence. We considered that this meta-analysis would provide the best proof to advise current clinical practice as well as future research efforts.
Methods
This meta-analysis was conducted in agreement with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement.15 The protocol was registered on PROSPERO (Registration No: CRD42018093125).
Search strategy
We searched the EMBASE, PubMed, Cochrane library and Clinical databases before March 2018, using the keywords “exchange”, “plating”, “nailing”, “femoral”, “nonunion or delayed union”, and “shaft” to identify published articles evaluating the efficacy between exchange nailing and augmentative plating in the treatment of femoral shaft nonunion or delayed union after IM nailing. No language restriction was applied. We also searched the reference lists of articles retrieved from the electronic search for related articles.
Inclusion criteria
We selected trails with the following inclusion criteria: (1) trials enrolling adults over the age of 18 years with nonunion or delayed union after IMN in femoral shaft fracture; (2) both exchange nailing (EN) and augmentative plating (AP) were adopted; and (3) both randomized and non-randomized studies were included. Exclusion criteria were: (1) patients with open fractures at their first injury; (2) pathological fractures; (3) suspected underlying infection; and (4) trials with animal studies or biomechanical studies.
Risk of bias assessments
Two investigators (Luo and Su) independently assessed the methodological quality of the included studies according to the Cochrane handbook for systematic reviews of interventions 5.3.16 Any disagreement was resolved by consensus. If no agreement was achieved, a third investigator (Xue) was the adjudicator. Cohort studies that were used in functional outcome analysis were assessed for risk of bias by the Newcastle-Ottawa Quality Assessment Scale (NOS), which was adopted by the Cochrane library databases. A total NOS score was 9, if the NOS score was higher than 6 that considered to high quality.
Data extraction
Two investigators (Luo and Su) independently extracted all related data from selected studies. Disagreements were resolved by consensus. The data extracted included lead author, publication year, participant characteristics, surgical interventions, patient-based outcomes, and implants. The total sample size was 119 for augmentative plating and 113 for exchange nailing. For exchange nailing, all studies exchanged larger nailing. As for the plating, one study adopted the DCP (dynamic compression plate) and the locking plate, and the other two studies did not mention the plate type. The union rate and the time to union were the primary outcome measurements. Intra-operative blood loss, the mean operation time, and complication rate were regarded as the secondary outcomes.
Statistical analysis
We used the Review Manager (RevMan version 5.3, Copenhagen, Denmark, The Nordic Cochrane Centre) software to perform the meta-analysis. For continuous data, we measured means and standard deviations for weighted mean differences (WMD) with 95% confidence interval (CI). For discontinuous variables, we assessed the odds ratio (OR) and 95% CI. Heterogeneity between studies was quantified using the I2 statistic and chi-square test. When the I2 > 50% or chi-square test showed P < 0.05, representing between-study inconsistency, the random-effects model was used; otherwise, the fixed-effects model was used. There was a significant difference when P < 0.05.
Results
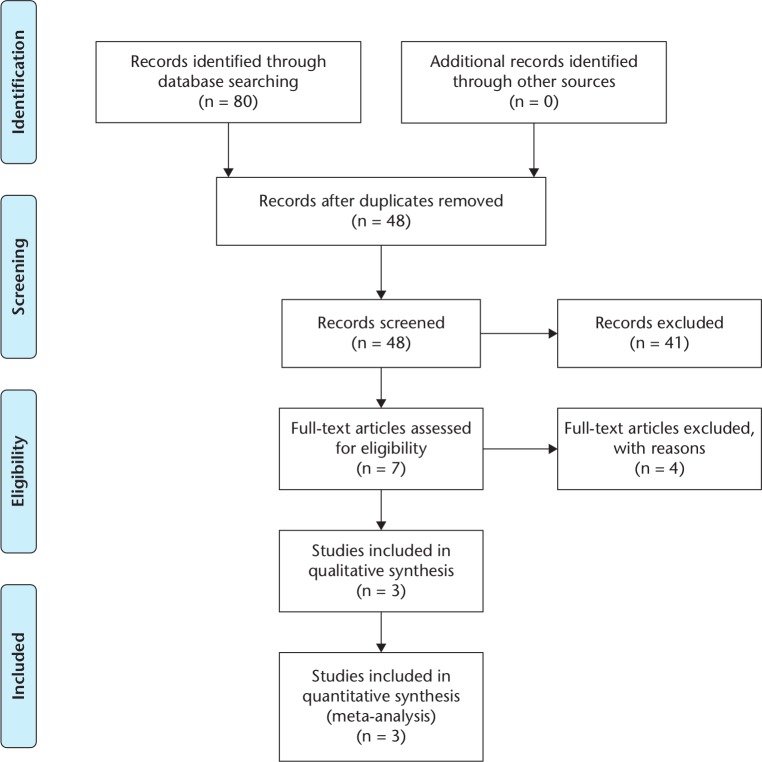
In all, our electronic data search retrieved 80 references. Two studies were not included in the overall meta-analysis because an identical patient cohort occurred within another selected cohort.17,18 One study was excluded because they did not investigate exchange nailing.19 One study was not included because they only used exchange nailing and an augment plate.20 The other excluded records include three tibia nonunions, three reviews, nine fractures and 26 studies without available survival information. Finally, there were three eligible studies eventually that met our eligibility criteria (Fig. 1). All three studies are retrospective trials registering a total of 232 patients eligible for meta-analysis.12–14 Details of the included studies are shown in Table 1. All three studies were evaluated by NOS score and were of high technical quality (Table 2).
Fig. 1.
Flow diagram for search and selection of included studies.
Table 1.
Characteristics of included studies.
Table 2.
Newcastle Ottawa scale ratings.
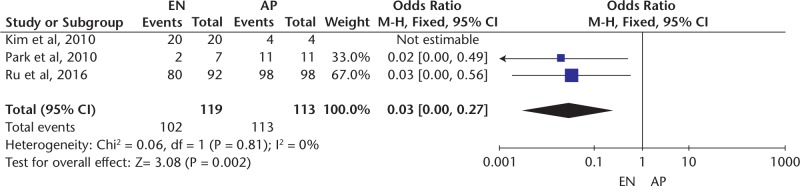
Union rate
The union rate was documented in three studies.12–14 The available data demonstrated that the augmentative plating group had a lower nonunion rate than the EN group. There was a significant difference between the two surgical methods regarding the union rate for the treatment of femoral shaft nonunion after IM nailing (OR, 0.03; 95% CI, 0 to 0.27, P = 0.002; I2 = 0%, Fig. 2).
Fig. 2.
Forest plot of comparison: EN versus AP, outcome: union rate.
Note. EN, exchange nailing; AP, augmentative plating; M-H, Mantel-Haenszel.
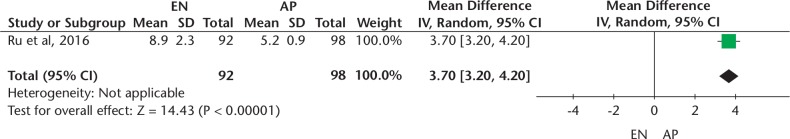
The time to union
Three studies provided the average time to union.12–14 However, two of them did not report the complete data of standard deviation or 95% CI.12,13 There was a significant difference between the AP group and EN group regarding the time to union (OR, 3.70; 95% CI, 3.20 to 4.20, P < 0.00001; heterogeneity: not applicable, Fig. 3). This difference indicated that the time to union in the AP group was significantly shorter than that observed in the EN group.
Fig. 3.
Forest plot of comparison: EN versus AP, outcome: the time to union.
Note. EN, exchange nailing; AP, augmentative plating; IV, Inverse Variance.
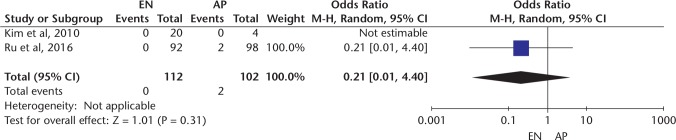
Infection
Two studies reported data on the infection rate.12,14 No significant difference was found between EN and AP (OR, 0.21; 95% CI, 0.01 to 4.40, P = 0.31; heterogeneity: not applicable, Fig. 4).
Fig. 4.
Forest plot of comparison: EN versus AP, outcome: infection.
Note. EN, exchange nailing; AP, augmentative plating; M-H, Mantel-Haenszel.
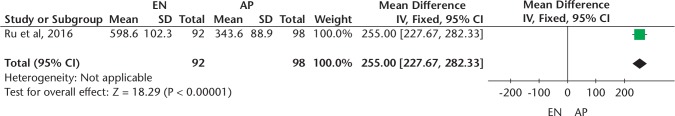
Intra-operative blood loss
The intra-operative blood loss was documented in one study.14 The forest plot showed that the AP group had a less intra-operative blood loss than the EN group (MD = 255.00; 95% Cl 227.67 to 282.33, P < 0.00001, heterogeneity: not applicable, Fig. 5)
Fig. 5.
Forest plot of comparison: EN versus AP, outcome: intra-operative blood loss.
Note. EN, exchange nailing; AP, augmentative plating; IV, Inverse Variance.
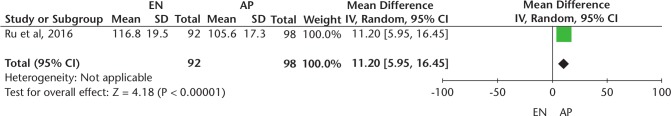
Operative time
The operation time was calculated for only one study.14 There was a significant difference in the operative time between EN and AP (MD = 11.20; 95% Cl 5.95 to 16.45, P < 0.0001, heterogeneity: not applicable, Fig. 6). The data showed that the AP group had a shorter operative time than the EN group.
Fig. 6.
Forest plot of comparison: EN versus AP, outcome: operative time.
Note. EN, exchange nailing; AP, augmentative plating; IV, Inverse Variance.
Publication bias
Considering the small sample size (< 10) in our meta-analysis, funnel plot analysis was not applicable for the determination of publication bias.
Discussion
The purpose of this meta-analysis was to evaluate the relative merits of exchange nailing versus augmentative plating in the treatment of femoral shaft nonunion after IM nailing. This analysis indicated that AP group had a lower nonunion rate and decreased the time to union than EN group. However, there was no significant difference in infection rate between EN and AP.
There are several treatment selections for femoral shaft nonunion or delayed union such as exchange for a larger size nailing, adding an augmentative plating, dynamization, or bone grafting alone. Concerning stability, several studies suggested that the nonunion is caused by instability.21,22 The benefits of EN likely root in using a larger size nailing that improves mechanical stability, especially in the endosteal surface of the femoral isthmus. Although exchange for a larger diameter nailing is typically considered the gold standard compared with other open techniques,5 some reports question the role of EN. Weresh et al and Banaszkiewicz et al have reported unsatisfactory results after exchange nailing, and the nonunion rate is reported to be as high as 47% and 58% respectively.10,23 Nowadays, a number of femoral nonunions treated with an augmentative plating with the nail in situ have been reported. Chen et al reported a 100% union rate for 50 aseptic femoral shaft nonunions by using an augmentative plating.24 In 16 cases of femoral nonunion, Vaishya et al reported union in all cases within 6.25 months after plating with the nail in situ without significant complication or implant failure.25 It seems that plate augmentation is an active, safe and reliable method for the treatment of femoral shaft nonunion after IMN. Several studies have compared the efficiency between exchange nailing and augmentative plating for femur shaft nonunion or delayed union after nailing.12–14 However, there is still debate about the nonunion rate, the time to union, as well as complications. To our knowledge, there is still no meta-analysis to compare the efficiency of these two surgical treatments. This meta-analysis showed that there was a significant difference in the nonunion rate and the time to union between EN and AP.
Our meta-analysis had several limitations. First, there were insufficient studies to permit the evaluation of the therapeutic effects. Although several studies reported the union time, two of them did not report the complete data of standard deviation or 95% CIs. Second, the studies included in our meta-analysis are all retrospective, therefore the level of the evidence is lower than that that provided by randomized controlled trials. Third, this study has a small sample size, and only 232 patients were included. Forth, two studies12,13 have not mentioned the complications such as intra-operative blood loss and the union time. Besides, the majority of included studies are short of detailed information such as patient treatment, and potential bias is not fully protected against even though we used a methodology assessment on the treatment. Studies may have different features compared to the baseline characteristics of the patients, including the duration of follow-up, the adjustments for other co-factors and the adjuvant treatment they might have received. Thus, our results need to be proved by further prospective studies.
Conclusion
In the present meta-analysis, augmentative plating is superior to exchange nailing for femoral shaft nonunion after IMN. Current evidence has indicated that AP had a lower nonunion rate, shorter time to union, less intra-operative blood loss, and shorter operative time than EN. The two approaches are similar in terms of infection. Still, this conclusion must be carefully considered, for the evidence used potentially underpowered samples and presented some methodological limitations. Thus, our viewpoints require well-conducted, adequately powered multicenter randomized controlled trials to confirm.
Footnotes
ICMJE Conflict of interest statement: The author declares no conflict of interest relevant to this work.
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Winquist RA, Hansen ST, Jr, Clawson DK. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Joint Surg Am 1984;66:529–539. [PubMed] [Google Scholar]
- 2. Brumback RJ, Uwagie-Ero S, Lakatos RP, Poka A, Bathon GH, Burgess AR. Intramedullary nailing of femoral shaft fractures. Part II: fracture-healing with static interlocking fixation. J Bone Joint Surg Am 1988;70:1453–1462. [PubMed] [Google Scholar]
- 3. Pihlajamäki HK, Salminen ST, Böstman OM. The treatment of nonunions following intramedullary nailing of femoral shaft fractures. J Orthop Trauma 2002;16:394–402. [DOI] [PubMed] [Google Scholar]
- 4. Abdel-Aa AM, Farouk OA, Elsayed A, Said HG. The use of a locked plate in the treatment of ununited femoral shaft fractures. J Trauma 2004;57:832–836. [DOI] [PubMed] [Google Scholar]
- 5. Brinker MR, O’Connor DP. Exchange nailing of ununited fractures. J Bone Joint Surg Am 2007;89:177–188. [DOI] [PubMed] [Google Scholar]
- 6. Richardson JB, Gardner TN, Hardy JR, Jr, Evans M, Kuiper JH, Kenwright J. Dynamisation of tibial fractures. J Bone Joint Surg Br 1995;77:412–416. [PubMed] [Google Scholar]
- 7. Ueng SW, Chao EK, Lee SS, Shih CH. Augmentative plate fixation for the management of femoral nonunion after intramedullary nailing. J Trauma 1997;43:640–644. [DOI] [PubMed] [Google Scholar]
- 8. Wu CC, Chen WJ. Exchange nailing for aseptic nonunion of the femoral shaft. Int Orthop 2002;26:80–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Furlong AJ, Giannoudis PV, DeBoer P, Matthews SJ, MacDonald DA, Smith RM. Exchange nailing for femoral shaft aseptic non-union. Injury 1999;30:245–249. [DOI] [PubMed] [Google Scholar]
- 10. Weresh MJ, Hakanson R, Stover MD, Sims SH, Kellam JF, Bosse MJ. Failure of exchange reamed intramedullary nails for ununited femoral shaft fractures. J Orthop Trauma 2000;14:335–338. [DOI] [PubMed] [Google Scholar]
- 11. Birjandinejad A, Ebrahimzadeh MH, Ahmadzadeh-Chabock H. Augmentation plate fixation for the treatment of femoral and tibial nonunion after intramedullary nailing. Orthopedics 2009;32:409–412. [DOI] [PubMed] [Google Scholar]
- 12. Kim JR, Chung WC, Shin SJ, Seo KB. The management of aseptic nonunion of femoral shaft fractures after interlocking intramedullary nailing. Eur J Orthop Surg Traumatol 2011;21:171–177. [Google Scholar]
- 13. Park J, Kim SG, Yoon HK, Yang KH. The treatment of nonisthmal femoral shaft nonunions with im nail exchange versus augmentation plating. J Orthop Trauma 2010;24:89–94. [DOI] [PubMed] [Google Scholar]
- 14. Ru J, Xu H, Kang W, Chang H, Niu Y, Zhao J. Augmentative compression plating versus exchanging reamed nailing for nonunion of femoral shaft fracture after intramedullary nailing: a retrospective cohort study. Acta Orthop Belg 2016;82:249–257. [PubMed] [Google Scholar]
- 15. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009;6:e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wang AJ, Zong SL, Su LX, Liang WD, Cao X, Zheng Q, et al. Meta-analysis of postoperative complications in distal femoral fractures: Retrograde intramedullary nailing versus plating. Int J Clin Exp Med 2016;9(10):18900–18911. [Google Scholar]
- 17. Ru I, Cang H, Hu C, Hu Y. [Comparison of two surgical methods for aseptic nonunions of femoral shaft orthopaedic surgery]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2013;27:25–29. [PubMed] [Google Scholar]
- 18. Ru JY, Niu YF, Cong Y, Kang WB, Cang HB, Zhao JN. Exchanging reamed nailing versus augmentative compression plating with autogenous bone grafting for aseptic femoral shaft nonunion: a retrospective cohort study. Acta Orthop Traumatol Turc 2015;49:668–675. [DOI] [PubMed] [Google Scholar]
- 19. Jiang L, Pan Z, Zheng Q. Augmentation plating in hypertrophic non-union after nail fixation of femoral shaft fracture compared with exchange plating. Chin Med J (Engl) 2014;127:2900–2905. [PubMed] [Google Scholar]
- 20. Wang Z, Liu C, Liu C, Zhou Q, Liu J. Effectiveness of exchange nailing and augmentation plating for femoral shaft nonunion after nailing. Int Orthop 2014;38:2343–2347. [DOI] [PubMed] [Google Scholar]
- 21. Boyd HB, Lipinski S, Wiley JH. Observation on nonunion of the shafts of the long bones, with a statistical analysis of 842 patients. J Bone Joint Surg Am 1961;43:159–168. [Google Scholar]
- 22. Brumback RJ. The rationales of interlocking nailing of the femur, tibia, and humerus. Clin Orthop Relat Res 1996;324:292–320. [DOI] [PubMed] [Google Scholar]
- 23. Banaszkiewicz PA, Sabboubeh A, McLeod I, Maffulli N. Femoral exchange nailing for aseptic non-union: not the end to all problems. Injury 2003;34:349–356. [DOI] [PubMed] [Google Scholar]
- 24. Chen CM, Su YP, Hung SH, Lin CL, Chiu FY. Dynamic compression plate and cancellous bone graft for aseptic nonunion after intramedullary nailing of femoral fracture. Orthopedics 2010;33:393. [DOI] [PubMed] [Google Scholar]
- 25. Vaishya R, Agarwal AK, Gupta N, Vijay V. Plate augmentation with retention of intramedullary nail is effective for resistant femoral shaft non-union. J Orthop 2016;13:242–245. [DOI] [PMC free article] [PubMed] [Google Scholar]