Abstract
Total knee arthroplasty (TKA) has evolved into a successful, cost-effective treatment for end-stage knee arthrosis.
The patellofemoral articulation in TKA has largely been ignored during its development despite being an important determinant of outcome.
New technologies still need further development to incorporate the patella in TKA surgical planning and operative technique.
Alternative approaches to alignment in TKA will have a secondary impact on patellofemoral mechanics and possibly future implant designs.
Technologies that assist with precise implant positioning may alter our understanding and overall practice of TKA.
Cite this article: EFORT Open Rev 2019;4:503-512. DOI: 10.1302/2058-5241.4.180094
Keywords: evolution, patellofemoral prosthesis design, total knee arthroplasty
Introduction
Total knee arthroplasty (TKA) is generally described as a successful, cost-effective treatment for patients with end-stage arthritis of the knee,1–3 and it certainly is for 80% of patients.4,5 Since the innovations of the early 1970s, considerable advances have been made in terms of component design, peri-operative care, alignment strategies, surgical approaches, and, more recently, the use of advanced technologies such as computer navigation and robotic-assisted surgery to improve patient outcomes.6–11 The patellofemoral part of TKA, however, has a history of neglect despite the patellofemoral articulation being an important aspect of TKA that has a profound impact on outcome and may be a composite indicator for the overall success of the procedure.12 During this review, we will outline the evolution of design of the patellofemoral part of TKA and highlight the areas in much need of further research.
Early innovations
Early attempts at anatomical knee arthroplasty focussed on the tibiofemoral articulation and were used to treat severe axial deformities as a result of rheumatoid arthritis and tuberculosis.13 The patellofemoral joint (PFJ), however, was largely ignored. Innovations such as the Freeman-Swanson Total Condylar Prosthesis (1970) and the Kodama-Yamamoto prosthesis (1970), paved the way for future designs, yet the original versions made no allowance for the patella.14,15 Patellectomy was frequently performed either at the primary procedure, or subsequently for patellofemoral pain and instability.13,16
Parallel to the development of the total knee replacement was the evolution of isolated PFJ arthroplasty, which had humble beginnings with the use of a Vitallium prosthesis secured with a single transfixing screw to resurface the patella alone, as described by McKeever in 1955,17 reportedly showing good functional results, and offering an alternative to patellectomy in isolated patellofemoral arthrosis.18,19
Early TKA pioneers soon revisited their designs when extensor mechanism dysfunction and anterior knee pain became evident. For example, in 1973 the total condylar prosthesis was redesigned to include a proximal flange that could accommodate a resurfaced patella;20 Groeneveld reported on the use of an all polyethylene (PE) patellar resurfacing with the Münster-TKA;21 and Hanslik reported on the use of a modification of the McKeever patellar resurfacing prosthesis with the Young hinged knee in 1973.22 From 1975, authors such as Aglietti, Insall and Mathews were investigating the biomechanics of the patellofemoral joint and highlighted the importance of design considerations that could accommodate the high-contact stress witnessed in experimental models of patellar prostheses.23,24
Patellar resurfacing became an integral part of TKA, and authors were reporting promising results, albeit with potential risks such as patellar fracture, implant loosening, component wear and instability. Many of these issues are unresolved, and the orthopaedic community remains divided in terms of whether, when and how to resurface the patella during TKA.16 With accumulating clinical experience and improved understanding of the biomechanical nature of the PFJ, five key areas have emerged as having a profound impact on the patellofemoral articulation in TKA, including (i) the shape of the femoral and patellar components, (ii) the position and alignment of the components, (iii) bone preparation, (iv) the materials used, and (v) the impact of tibiofemoral stability on the patellofemoral articulation.
Shape of the components
Advances in imaging modalities, the development of validated finite element analyses, and well-designed cadaver studies have improved our understanding of the kinematics of the patellofemoral articulation. A deepened trochlear groove with a lateral wall build-up appears to improve patellar tracking, tilt and contact profiles.25,26 Valgus trochlear alignment of 7° reduces lateral shear forces at low flexion angles in comparison with neutral trochlear alignment, but this difference lessens at flexion angles close to 90° due to the concurrent distal translation of the patella relative to the trochlea in deep flexion.27
The kinematics in unresurfaced versus resurfaced patellae are affected by trochlear shape. A trochlea with a V-shaped axial profile has been shown to generate less contact stress in unresurfaced patellae, whereas with resurfaced patellae, a curved femoral component that accommodates a dome-shaped patellar prosthesis demonstrates favourable contact forces,28 highlighting the importance of appropriate implant choice to match the surgical strategy.
Buechel, Pappas and Makris studied five patellar resurfacing designs in TKA in 1991, and highlighted that the lack of stringent regulation for design alteration in TKA prostheses permitted manufacturers to release inadequately tested prostheses that led to early failures, again suggesting the relative lack of attention to the patellofemoral articulation in design.29
Whiteside’s group studied the contact stress in unresurfaced patellae using five different TKA designs in 2000 and demonstrated that the trochlear design plays an important role in the level of stress in the PFJ. They also correlated high-contact stresses with poorly conforming designs that had high rates of anterior knee pain, such as the Insall-Burnstein and Miller-Galante designs.30
In 2014, Dejour’s group highlighted the plethora of trochlear designs in available TKA implants when they studied the profiles of 14 commonly used implants, demonstrating considerable variation in proximal extension, width, sulcus angle and depth of the trochlea, and the resemblance that many designs have to dysplastic trochlea.31 For example, 13/14 designs had a sulcus angle > 143° in the Brattström view (30° flexion), and 8/14 had a lateral facet < 5 mm high at 30–45°. Although manufacturers have made improvements in more recent generations of TKA implants, the trochlear part in newer designs remains 3–6° shallower than normal native knee anatomy.11 They also demonstrated similar concerns regarding patellofemoral arthroplasty designs.32 Recently, Werth et al demonstrated the greater tendency for older implant designs with lateral trochlear heights > 5 mm to require secondary patellar resurfacing due to patellofemoral pain following TKA and highlighted that the optimal design characteristics of the patellofemoral joint should take into consideration an anatomically shaped, asymmetric, non-dysplastic trochlear groove with appropriate medial and lateral facet height.33
Bonnin et al analysed the shape of 114 arthritic knees using pre-operative CT scans prior to primary TKA and, after comparing this to the corresponding morphometry of 12 TKA models, demonstrated that most femoral components appeared to be excessively rectangular at the level of the distal femoral resection.34 Intra-operative compensations for this may alter the chosen size or rotation of the component, which may in turn impact on the patellofemoral mechanics.
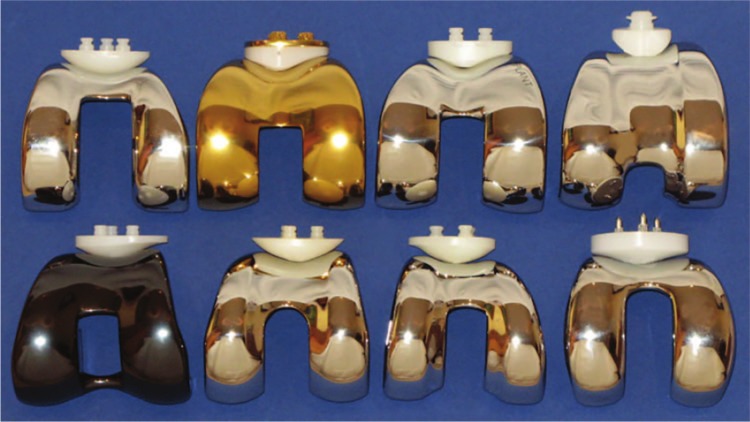
The patellar component design can be categorized broadly as anatomical, dome-shaped, or cylindrical, with some variations within these categories (Fig. 1 and Fig. 2). The first reported patellar resurfacing by Groeneveld et al made use of an anatomical design with the Münster condylar-type TKA.21 The anatomical prostheses, which are highly conforming, have shown the most impressive in vitro contact stress properties but are unforgiving – malposition of the femoral or patellar components can result in instability, increased wear, increased shear stress at the prosthesis–bone interface, and anterior knee pain. Mobile bearing anatomical components (e.g. Buechel-Pappas, Endotec, Orlando, USA) aim to accommodate this, and showed promising results, but have faced complications associated with metal backing and inter-prosthesis dislocation.29,35,36 Dome-shaped patellar components (e.g. AGC, Biomet, Warsaw, USA) can be forgiving in the appropriately conforming femoral component.13 However, they have a propensity for increased contact stress and subsequent wear in higher degrees of flexion within a deepening femoral sulcus,13 and are at a disadvantage for wear, since bearings perform best when softer materials are concave rather than convex.37 The modified dome or Gaussian shape with a convex centre and concave rim (resembling a ‘sombrero’ in cross-section) reduces contact stress in deep flexion,38 and the offset dome (e.g. Triathlon, Stryker, Kalamazoo, USA) allows medialization of the patellar component to improve tracking. The dome, or a variation thereof, remains the most frequently utilized design for the patellar component. Cylindrical designs have also shown reduced contact stress but faced concerns about fracture from a large central peg, over constraint, and the use of an inlay technique.13
Fig. 1.
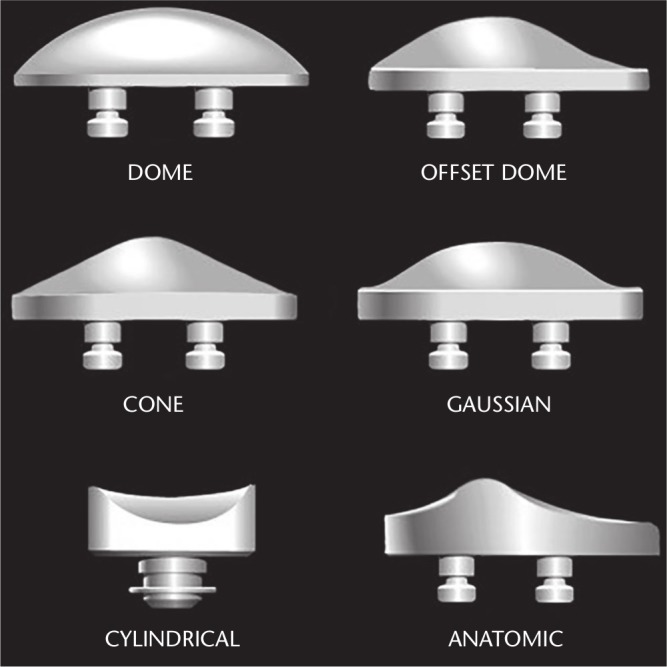
Predominant design configurations for patellar components, namely dome-shaped, anatomical and cylindrical, or a variation of these.
Reproduced with permission from: Schindler OS. Patellar resurfacing in total knee arthroplasty. In: Scott WN, ed. Insall and Scott, surgery of the knee. Sixth ed. Elsevier, Churchill Livingstone, Philadelphia, 2018:1585–1629.
Fig. 2.
Examples of femoral components with their respective patellar implants.
Top row, from left to right: AGC® (dome-shaped patella), Biomet, Warsaw, USA; Buechel-Pappas (uncemented anatomical rotating platform patella), Endotec, Orlando, USA; LCS® (anatomical fixed bearing patella), DePuy, Warsaw, USA; Medial rotating knee® (cylindrical patella), Finsbury, England.
Bottom row, from left to right: Journey® (offset dome patella), Smith and Nephew, Andover, USA; PFC-Sigma® (modified dome patella), DePuy; Triathlon® (offset dome patella), Stryker, Kalamazoo, USA; Bio-Pro® Townley Total Knee Original (uncemented metal-backed dome patella), Biopro®, Port Huron, USA.
Reproduced with permission from Schindler OS. The controversy of patellar resurfacing in total knee arthroplasty: Ibisne in medio tutissimus? Knee Surg Sports Traumatol Arthrosc 2012;20:1227–1244.
Preparation of the patella
The McKeever prosthesis, and subsequently Hanslik’s PE modification, were applied in an ‘overlay’ fashion after reshaping the patella sufficiently to fit the retropatellar surface within the prosthesis, which was then transfixed with a single screw. Since these early attempts, two strategies for patellar resurfacing have emerged, namely, the onlay technique where the patella is placed onto the cut retropatellar surface, and the inlay technique where the patella is placed within a reamed cavity thereby preserving the surrounding bone. In order to achieve favourable patellar tracking and reduce the risk of patellar fracture, the objective for the onlay technique is to obtain a uniformly thick patellar remnant of no less than 12 mm while restoring the native height of the patella with adequate medialization of the highest point of the prosthesis. Comparative studies are small in number and cohort sizes, with no clear benefit being attributed to either technique,39,40 yet the onlay technique is the most frequently utilized and arguably more versatile than the inlay technique.
Inaccurate resection with any technique is not uncommon, even amongst experienced surgeons, and leaving the patella too thick, too thin, or asymmetrical in the coronal or sagittal plane has been linked to patellar maltracking, abnormal kinematics, increased risk of fracture, loosening, patellofemoral impingement and anterior knee pain.41–44 Patellar cutting guides may assist in providing a uniform resection, but in reality, currently available systems are highly dependent on correct application, and do not appear to be more accurate than freehand technique in experienced hands.45 Furthermore, the depth of the patellar resection cannot be considered in isolation, and an appreciation of the corresponding femoral resection is required.46
Technological aids such as computer-assisted surgery and robotics have not formally incorporated the preparation of the patella into the surgical technique. However, Belvedere et al were able to use a secondary navigation system to monitor patellar kinematics intra-operatively to evaluate the quality of the patellar resection and component position,47 and Fu et al have demonstrated the feasibility and accuracy with the use of a computer-assisted patellar resection in experimental models.48
Component position
Patellofemoral kinematics are inextricably linked to tibiofemoral kinematics – one cannot be altered without a significant impact on the other.49–51 Femoral and tibial component rotation, translation and flexion, patellar translation and posterior condylar offset are key considerations. Despite advances in design, patellar kinematics in TKA differ considerably from those seen in the native knee.50,51
In the early 1990s, Whiteside’s group compared cadaver patellar tracking and knee stability to that of TKA using the Ortholoc II prosthesis.51 External rotation of 5° provided better stability and patellar tracking than neutral or internal rotation. It was postulated that the external rotation compensates for the orthogonal proximal tibia cut, which is approximately 3° from the native proximal tibial varus joint line.51 However, external rotation may create excessive asymmetry in the posterior condyles, with detrimental effects on the tibiofemoral stability and lateral overhang.52 A more recent finite element analysis has demonstrated that femoral component internal rotation can increase the patellofemoral contact forces two-fold in comparison with femoral component external rotation, especially in conditions of deep knee flexion.53
Anglin et al studied 11 different positions of femoral, tibial and patellar components and described the impact that these had on patellar tracking, using the NexGen TKA in cadaver models. They confirmed that femoral component external rotation can improve patellar tracking, but is limited by the impact on tibiofemoral mechanics; tibial component rotation has a small impact on patellar tracking; patellar resection angle influences tilt and shift, and requires more attention than previously thought; and patellar medialization improves patellar shift, but excessive medialization (beyond 2.5 mm) can increase patellar tilt.42 They noted the significant contribution that soft tissues play in patellar kinematics, especially at 90° of flexion. Patellar medialization is also supported in other studies.25,27
Increasing posterior condylar offset by more than 2 mm and decreasing the tibial slope both increase the patellar contact forces and should be avoided.54 Maximal coverage of the patella by the patellar component has been associated with improved patellofemoral load distribution.55 Increasing PE thickness and the patellofemoral offset have been shown to reduce knee range of motion exponentially in cadaver models,56,57 and increase the lateral patellar tilt.58
The overall alignment strategy may also have a significant impact on the patellofemoral articulation, and optimal limb alignment has long been regarded as an important factor determining outcome and longevity in TKA.59 However, what constitutes optimal alignment is still a matter of debate.60,61 Classically, two alignment strategies were described: (1) anatomical alignment, which aims to achieve a neutral hip–knee–ankle angle with the anatomical joint line orientation of 2–3° from the horizontal to bring the joint line parallel to the floor during single leg stance;62 and (2) mechanical alignment, which aims to restore a neutral mechanical axis with orthogonal femoral and tibial resections and subsequent soft tissue balancing, in order to distribute load evenly through the implant bone interface. The latter has become the gold standard.63 More recently, an alternative alignment strategy has been studied, namely kinematic or functional alignment, which is based on a three-dimensional appreciation of the single axis of rotation of the knee.8–10 In this approach, the objective is to position the implants so as to restore the pre-arthritic knee anatomy, permitting motion more akin to native knee motion. In the coronal plane, the native distal femoral valgus and proximal tibia varus are respected to create a joint line orientation angle approximately 3° from the horizontal.9,10 In the sagittal plane, the native tibial slope is maintained, since cruciate-retaining implants are usually utilized, and in the axial plane the distal femoral rotation remains neutral, rather than externally rotated as desired with mechanical alignment.10 While some institutions have reported promising short and mid-terms results, clinical and biomechanical studies remain divided regarding which is the optimal strategy to employ.60,64–71 Furthermore, alternative alignment strategies will have a secondary impact on the patellofemoral mechanics and possibly the evolution of implant designs, and will require further evaluation.
Materials
Modern TKA with patellar resurfacing most frequently involves a cobalt-chromium femoral component with a PE patellar component.72 However, numerous materials have been tried with varying success. McKeever’s patellar prothesis, designed to articulate with the native trochlea, was fashioned from Vitallium, which is an inert alloy composed predominantly of cobalt and chromium with good resistance to corrosion and well documented use in orthopaedics from the early 1940s.73 Hanslik utilized a high-density PE variant of McKeever’s design to resurface the patella with the Young hinged knee from 1969 in 46 patients and described good function and pain relief in the majority of cases.22 Gunston and MacKenzie designed a stainless steel patellar button that articulated with a PE track in the trochlea with the polycentric knee system and described promising results in 1976, but cautioned about potential complications of additional prosthetic components.74 Groeneveld described the use of an anatomical three-peg PE patellar prosthesis with the Münster TKA in 1973, and soon thereafter other innovators described the use of PE patellar components with condylar-type TKA prostheses.16,21 Metal-backed patellar designs were introduced in the 1980s since they were shown to improve load transfer and allow for biological fixation in tibial and acetabular components. But decreasing the relative thickness of the PE to accommodate for the metal back, increasing the patellofemoral offset and imperfections in patellar alignment, contributed to complications such as PE fatigue failure, patellar fracture and implant dissociation.36,75 Carbon-fibre-reinforced PE showed inferior wear and fatigue fracture characteristics.76
Improvements in the manufacturing process for PE, including heat annealing, appropriate doses of gamma radiation, vitamin-E enrichment, and avoiding a prolonged shelf life have improved strength and wear properties.13,77,78 However, the biomechanical stresses in TKA cannot be compared with those seen in total hip arthroplasty, where the focus of research has been for these new developments in PE processing, and the long-term mechanical properties remain to be delineated in TKA.79
Oxinium has been used successfully in TKA,80,81 but has not demonstrated superiority to cobalt-chromium implants.82,83 Ceramics have faced challenges with regard to fixation at the implant bone interface, but have also shown good survivorship at 10 and 15 years in TKA.84–86 Polyetheretherketone (PEEK) is currently being investigated as an alternative material in TKA and has shown promising results in vitro.87
Effect of tibiofemoral stability
There is a paucity of literature demonstrating the impact that tibiofemoral stability has on the PFJ, and the impact this has on TKA. Femoral rollback, a characteristic of native knee kinematics, is achieved by an intact posterior cruciate ligament (PCL) or cam-and-post mechanism and permits greater degrees of knee flexion. It effectively lengthens the patellar moment arm, which increases the efficacy of the extensor mechanism but also increases the contact forces in the PFJ, which can be detrimental to the joint.88 Increasing the patellofemoral offset will exacerbate this. In cadaver models, removal of the anterior cruciate ligament (ACL) appears to create substantial lateral patellar tilt and lateral patellar translation, which is restored with ACL reconstruction.89 Similarly, PCL deficiency appears to alter patellar flexion, lateral translation, rotation and tilt, which are restored, in part, by PCL reconstruction.88,90
Patellar resurfacing or not
After initially ignoring the patellofemoral joint during TKA, then making patellar resurfacing a routine part of the procedure within the same decade,91 when the potential complications of patellar resurfacing became apparent, three main approaches emerged – those who never resurface, those who routinely resurface, and those who selectively resurface the patella. Even today, there is much controversy in this debate,92 with clinical, economical and medicolegal considerations influencing the chosen approach.
Proponents of resurfacing suggest it reduces post-operative anterior knee pain, avoids revision and secondary resurfacing, avoids cartilage–metal articulation which causes cartilage wear, and improves patient outcomes.13,93–95 Opponents of resurfacing argue for maintaining patellar bone stock, reducing operative time, maintaining physiological patellofemoral kinematics, and avoiding complications associated with resurfacing.96–98 Complications such as maltracking and anterior knee pain are usually a result of errors in technique, or design, or both, and simply resurfacing the patella secondarily does not always resolve the symptomatic unresurfaced patella.12
Applying strict criteria (patients < 65 years old, without advanced patella cartilage loss or inflammatory arthropathy, central patellar tracking and the appropriately designed prosthesis) to selective patellar resurfacing has produced high survival rates at 10 years.99 However, it has been highlighted that manufacturers provide femoral components that have varying degrees of ‘patella-friendly’ trochlear designs,99 and care should be taken when selecting the appropriate implant.
Zangger and Detsky determined the mean probability of complications associated with patellar resurfacing versus non-resurfacing, and used a Bayesian model to demonstrate that even with the help of a computer-based decision model and available data, there is no difference in overall risk between resurfacing or not resurfacing, and either approach can have arithmetically similar advantages and disadvantages.100 This may indicate that we have a long way to go before we fully understand the patellofemoral articulation.
Meta-analyses have failed to demonstrate a clear benefit from patellar resurfacing versus non-resurfacing in TKA in terms of pain, functional outcome scores, patient satisfaction, and complication rates.101 The risk of re-operation has repeatedly been shown to be higher in patients undergoing patellar resurfacing,102–105 yet when only evaluating high-quality randomized controlled trials, He et al demonstrated equivalent results.104 Interestingly, no high-quality meta-analyses have reported superior outcomes for non-patellar resurfacing.101 Concerns with selection bias, relatively small sample sizes, heterogeneity in terms of outcome metrics and numerous confounding variables that influence the outcome after TKA (as discussed above), encumber our ability to evaluate the question of whether or not to resurface the patella.101 If we are to obtain the answer to this question, it will require well-designed studies with adequate control of confounding variables that are able to identify potential individual characteristics predictive of good outcomes rather than pooling heterogenous data.
Generation ‘R’
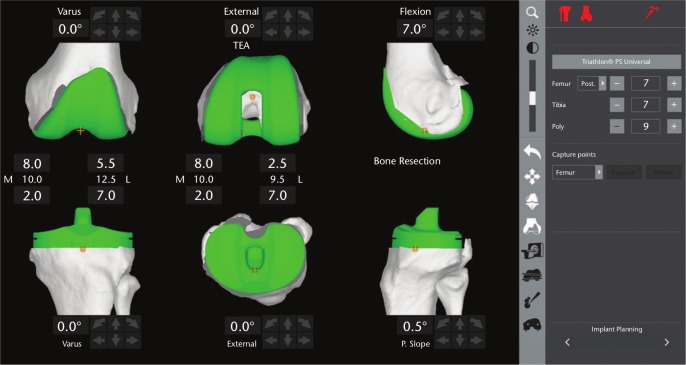
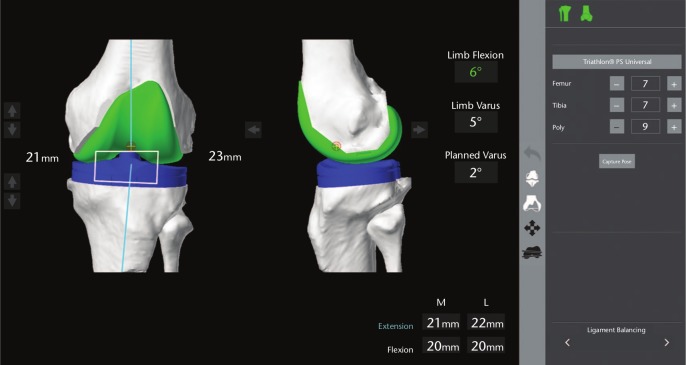
Fast-track to 2019, and we have at our disposal advanced technologies such as computer navigation and robotic-assisted surgery, which allow us to plan and achieve the desired component position, limb alignment and soft tissue balance with increasing accuracy for the tibial and femoral components.106,107 Yet we still ignore the PFJ to a large extent with key determinants of patellar tracking not included in the operative planning or execution – the patella is not visible on the pre-operative plan (Fig. 3), which precludes an evaluation of the depth of resection and component position, and the final intra-operative preparation to accommodate femoral and tibial component translation is performed manually, as is the rotation of the tibial component and the patellar resection. Tibiofemoral range of motion and coronal balance are evaluated with the navigation system intra-operatively, but patellar tracking and soft tissue balance are not (Fig. 4).
Fig. 3.
Screen capture of pre-operative plan for a robotic-assisted total knee arthroplasty.
Fig. 4.
Intra-operative screen capture of a robotic-assisted total knee arthroplasty during assessment of soft tissue balance prior to performing distal femoral and proximal tibial resections.
Technologies that allow us to place implants in the exact position in which we want them may influence our surgical goals in TKA, and we will need to utilize them efficiently in order to understand the optimal solution for our individual patients.108,109 They may also assist in controlling some of the confounding variables that make outcomes in patellar resurfacing versus non-resurfacing difficult to compare.
Summary and recommendations
We have seen considerable design and technological advancements in TKA since the ground-breaking work of the early 1970s. The patellofemoral articulation, however, has a history of being ignored. Future research efforts and technological advances will need to incorporate the patellofemoral articulation in the design, operative planning and surgical technique of TKA in order to improve our surgical accuracy, collection of data, and our understanding of this aspect of TKA, which may be a composite indicator of the overall success of the procedure.
The increasing push towards alternative alignment strategies will also cause secondary changes in patellofemoral mechanics, and possibly in the designs of knee arthroplasty. Moreover, the available technologies that now allow us to place implants exactly where we want them, may also improve exactly what we do.
Footnotes
Conflict of interest statement: FSH reports board membership of The Bone and Joint Journal; consultancy, payment for lectures including service on speakers’ bureaus for Smith & Nephew; royalties paid by Smith & Nephew, Corin and MattOrtho; payment for development of educational presentations for Smith & Nephew, all outside the submitted work.
MAR declares no conflict of interest relevant to this work.
Funding statement
The author or one or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article. In addition, benefits have been or will be directed to a research fund, foundation, educational institution, or other non-profit organization with which one or more of the authors are associated.
References
- 1. Khan M, Osman K, Green G, Haddad FS. The epidemiology of failure in total knee arthroplasty: avoiding your next revision. Bone Joint J 2016;98-B:105–112. [DOI] [PubMed] [Google Scholar]
- 2. Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty: a qualitative and systematic review of the literature. J Bone Joint Surg Am 2004;86-A:963–974. [DOI] [PubMed] [Google Scholar]
- 3. Jenkins PJ, Clement ND, Hamilton DF, Gaston P, Patton JT, Howie CR. Predicting the cost-effectiveness of total hip and knee replacement: a health economic analysis. Bone Joint J 2013;95-B:115–121. [DOI] [PubMed] [Google Scholar]
- 4. Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 2010;468:57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hawker G, Wright J, Coyte P, et al. Health-related quality of life after knee replacement. J Bone Joint Surg Am 1998;80:163–173. [DOI] [PubMed] [Google Scholar]
- 6. El Bitar YF, Illingworth KD, Scaife SL, Horberg JV, Saleh KJ. Hospital length of stay following primary total knee arthroplasty: data from the nationwide inpatient sample database. J Arthroplasty 2015;30:1710–1715. [DOI] [PubMed] [Google Scholar]
- 7. Kayani B, Konan S, Tahmassebi J, Pietrzak JRT, Haddad FS. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty. Bone Joint J 2018;100-B:930–937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hollister AM, Jatana S, Singh AK, Sullivan WW, Lupichuk AG. The axes of rotation of the knee. Clin Orthop Relat Res 1993;290:259–268. [PubMed] [Google Scholar]
- 9. Eckhoff DG, Bach JM, Spitzer VM, et al. Three-dimensional mechanics, kinematics, and morphology of the knee viewed in virtual reality. J Bone Joint Surg Am 2005;87:71–80. [DOI] [PubMed] [Google Scholar]
- 10. Howell SM, Kuznik K, Hull ML, Siston RA. Results of an initial experience with custom-fit positioning total knee arthroplasty in a series of 48 patients. Orthopedics 2008;31:857–863. [DOI] [PubMed] [Google Scholar]
- 11. Saffarini M, Demey G, Nover L, Dejour D. Evolution of trochlear compartment geometry in total knee arthroplasty. Ann Transl Med 2016;4:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Barrack RL, Burak C. Patella in total knee arthroplasty. Clin Orthop Relat Res 2001;389:62–73. [DOI] [PubMed] [Google Scholar]
- 13. Schindler OS. The controversy of patellar resurfacing in total knee arthroplasty: ibisne in medio tutissimus? Knee Surg Sports Traumatol Arthrosc 2012;20:1227–1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Swanson SA, Freeman MA. A new prosthesis for the total replacement of the knee. Acta Orthop Belg 1972;38:55–62. [PubMed] [Google Scholar]
- 15. Kodama T, Yamamoto S. Total knee prosthesis without hinge, total knee replacement. Institute of Mechanical Engineering, London Google Scholar. 1975. [Google Scholar]
- 16. Robinson RP. The early innovators of today’s resurfacing condylar knees. J Arthroplasty 2005;20:2–26. [DOI] [PubMed] [Google Scholar]
- 17. McKeever DC. Patellar prosthesis. J Bone Joint Surg Am 1955;37-A:1074–1084. [PubMed] [Google Scholar]
- 18. De Palma AF, Sawyer B, Hoffman JD. Reconsideration of lesions affecting the patellofemoral joint. South Med J 1963;56:182–186. [DOI] [PubMed] [Google Scholar]
- 19. Harrington KD. Long-term results for the McKeever patellar resurfacing prosthesis used as a salvage procedure for severe chondromalacia patellae. Clin Orthop Relat Res 1992;279:201–213. [PubMed] [Google Scholar]
- 20. Freeman MA, Todd RC, Bamert P, Day WH. ICLH arthroplasty of the knee: 1968–1977. J Bone Joint Surg Br 1978;60-B:339–344. [DOI] [PubMed] [Google Scholar]
- 21. Groeneveld HB. Combined femoro-tibial-patellar endoprosthesis of the kneejoint preserving the ligaments. Acta Orthop Belg 1973;39:210–215. [PubMed] [Google Scholar]
- 22. Hanslik L. First experience on knee joint replacement using the Young hinged prosthesis combined with a modification on the McKeever patella prosthesis. Clin Orthop Relat Res 1973;94:115–121. [DOI] [PubMed] [Google Scholar]
- 23. Aglietti P, Insall JN, Walker PS, Trent P. A new patella prosthesis: design and application. Clin Orthop Relat Res 1975;107:175–187. [PubMed] [Google Scholar]
- 24. Matthews LS, Sonstegard DA, Henke JA. Load bearing characteristics of the patello-femoral joint. Acta Orthop Scand 1977;48:511–516. [DOI] [PubMed] [Google Scholar]
- 25. Yoshii I, Whiteside LA, Anouchi YS. The effect of patellar button placement and femoral component design on patellar tracking in total knee arthroplasty. Clin Orthop Relat Res 1992;275:211–219. [PubMed] [Google Scholar]
- 26. Leichtle UG, Lange B, Herzog Y, et al. Influence of different patellofemoral design variations based on Genesis II total knee endoprosthesis on patellofemoral pressure and kinematics. Appl Bionics Biomech 2017;2017:5492383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. D’Lima DD, Chen PC, Kester MA, Colwell CW., Jr Impact of patellofemoral design on patellofemoral forces and polyethylene stresses. J Bone Joint Surg Am 2003;85-A:85–93. [DOI] [PubMed] [Google Scholar]
- 28. Huang CH, Hsu LI, Chang TK, et al. Stress distribution of the patellofemoral joint in the anatomic V-shape and curved dome-shape femoral component: a comparison of resurfaced and unresurfaced patellae. Knee Surg Sports Traumatol Arthrosc 2017;25:263–271. [DOI] [PubMed] [Google Scholar]
- 29. Buechel FF, Pappas MJ, Makris G. Evaluation of contact stress in metal-backed patellar replacements: a predictor of survivorship. Clin Orthop Relat Res 1991;273:190–197. [PubMed] [Google Scholar]
- 30. Matsuda S, Ishinishi T, Whiteside LA. Contact stresses with an unresurfaced patella in total knee arthroplasty: the effect of femoral component design. Orthopedics 2000;23:213–218. [DOI] [PubMed] [Google Scholar]
- 31. Dejour D, Ntagiopoulos PG, Saffarini M. Evidence of trochlear dysplasia in femoral component designs. Knee Surg Sports Traumatol Arthrosc 2014;22:2599–2607. [DOI] [PubMed] [Google Scholar]
- 32. Saffarini M, Ntagiopoulos PG, Demey G, Le Negaret B, Dejour DH. Evidence of trochlear dysplasia in patellofemoral arthroplasty designs. Knee Surg Sports Traumatol Arthrosc 2014;22:2574–2581. [DOI] [PubMed] [Google Scholar]
- 33. Werth L, Saffarini M, Amsler F, Abdelkafy A, Hirschmann MT. The need for secondary resurfacing is affected by trochlear height in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2017;25:3818–3823. [DOI] [PubMed] [Google Scholar]
- 34. Bonnin MP, Saffarini M, Bossard N, Dantony E, Victor J. Morphometric analysis of the distal femur in total knee arthroplasty and native knees. Bone Joint J 2016;98-B:49–57. [DOI] [PubMed] [Google Scholar]
- 35. Bayley JC, Scott RD. Further observations on metal-backed patellar component failure. Clin Orthop Relat Res 1988;236:82–87. [PubMed] [Google Scholar]
- 36. Lombardi AV, Jr, Engh GA, Volz RG, Albrigo JL, Brainard BJ. Fracture/dissociation of the polyethylene in metal-backed patellar components in total knee arthroplasty. J Bone Joint Surg Am 1988;70:675–679. [PubMed] [Google Scholar]
- 37. Revell PA, Weightman B, Freeman MA, Roberts BV. The production and biology of polyethylene wear debris. Arch Orthop Trauma Surg 1978;91:167–181. [DOI] [PubMed] [Google Scholar]
- 38. Hsu HP, Walker PS. Wear and deformation of patellar components in total knee arthroplasty. Clin Orthop Relat Res 1989;246:260–265. [PubMed] [Google Scholar]
- 39. Rand JA, Gustilo B. Comparison of inset and resurfacing patellar prostheses in total knee arthroplasty. Acta Orthop Belg 1996;62:154–163. [PubMed] [Google Scholar]
- 40. Ezzet KA, Hershey AL, D’Lima DD, Irby SE, Kaufman KR, Colwell CW., Jr Patellar tracking in total knee arthroplasty: inset versus onset design. J Arthroplasty 2001;16:838–843. [DOI] [PubMed] [Google Scholar]
- 41. Pagnano MW, Trousdale RT. Asymmetric patella resurfacing in total knee arthroplasty. Am J Knee Surg 2000;13:228–233. [PubMed] [Google Scholar]
- 42. Anglin C, Brimacombe JM, Hodgson AJ, et al. Determinants of patellar tracking in total knee arthroplasty. Clin Biomech (Bristol, Avon) 2008;23:900–910. [DOI] [PubMed] [Google Scholar]
- 43. Bengs BC, Scott RD. The effect of patellar thickness on intraoperative knee flexion and patellar tracking in total knee arthroplasty. J Arthroplasty 2006;21:650–655. [DOI] [PubMed] [Google Scholar]
- 44. Oishi CS, Kaufman KR, Irby SE, Colwell CW., Jr Effects of patellar thickness on compression and shear forces in total knee arthroplasty. Clin Orthop Relat Res 1996;331:283–290. [DOI] [PubMed] [Google Scholar]
- 45. Camp CL, Martin JR, Krych AJ, Taunton MJ, Spencer-Gardner L, Trousdale RT. Resection technique does affect resection symmetry and thickness of the patella during total knee arthroplasty: a prospective randomized trial. J Arthroplasty 2015;30:2110–2115. [DOI] [PubMed] [Google Scholar]
- 46. Valoroso M, Saffarini M, La Barbera G, et al. Correction of patellofemoral malalignment with patellofemoral arthroplasty. J Arthroplasty 2017;32:3598–3602. [DOI] [PubMed] [Google Scholar]
- 47. Belvedere C, Ensini A, Leardini A, et al. Tibio-femoral and patello-femoral joint kinematics during navigated total knee arthroplasty with patellar resurfacing. Knee Surg Sports Traumatol Arthrosc 2014;22:1719–1727. [DOI] [PubMed] [Google Scholar]
- 48. Fu CK, Wai J, Lee E, et al. Computer-assisted patellar resection system: development and insights. J Orthop Res 2012;30:535–540. [DOI] [PubMed] [Google Scholar]
- 49. Varadarajan KM, Freiberg AA, Gill TJ, Rubash HE, Li G. Relationship between three-dimensional geometry of the trochlear groove and in vivo patellar tracking during weight-bearing knee flexion. J Biomech Eng 2010;132:061008. [DOI] [PubMed] [Google Scholar]
- 50. Merican AM, Ghosh KM, Iranpour F, Deehan DJ, Amis AA. The effect of femoral component rotation on the kinematics of the tibiofemoral and patellofemoral joints after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2011;19:1479–1487. [DOI] [PubMed] [Google Scholar]
- 51. Anouchi YS, Whiteside LA, Kaiser AD, Milliano MT. The effects of axial rotational alignment of the femoral component on knee stability and patellar tracking in total knee arthroplasty demonstrated on autopsy specimens. Clin Orthop Relat Res 1993;287:170–177. [PubMed] [Google Scholar]
- 52. Bonnin MP, Saffarini M, Nover L, van der Maas J, Haeberle C, Hannink G, et al. External rotation of the femoral component increases asymmetry of the posterior condyles. Bone Joint J 2017;99-B:894–903. [DOI] [PubMed] [Google Scholar]
- 53. Kang KT, Koh YG, Son J, et al. Measuring the effect of femoral malrotation on knee joint biomechanics for total knee arthroplasty using computational simulation. Bone Joint Res 2016;5:552–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Kang KT, Koh YG, Son J, Kwon OR, Lee JS, Kwon SK. A computational simulation study to determine the biomechanical influence of posterior condylar offset and tibial slope in cruciate retaining total knee arthroplasty. Bone Joint Res 2018;7:69–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Lee TQ, Budoff JE, Glaser FE. Patellar component positioning in total knee arthroplasty. Clin Orthop Relat Res 1999;366:274–281. [DOI] [PubMed] [Google Scholar]
- 56. Abolghasemian M, Samiezadeh S, Sternheim A, Bougherara H, Barnes CL, Backstein DJ. Effect of patellar thickness on knee flexion in total knee arthroplasty: a biomechanical and experimental study. J Arthroplasty 2014;29:80–84. [DOI] [PubMed] [Google Scholar]
- 57. Hsu HC, Luo ZP, Rand JA, An KN. Influence of patellar thickness on patellar tracking and patellofemoral contact characteristics after total knee arthroplasty. J Arthroplasty 1996;11:69–80. [DOI] [PubMed] [Google Scholar]
- 58. Matz J, Howard JL, Morden DJ, MacDonald SJ, Teeter MG, Lanting BA. Do changes in patellofemoral joint offset lead to adverse outcomes in total knee arthroplasty with patellar resurfacing? A radiographic review. J Arthroplasty 2017;32:783–787.e1. [DOI] [PubMed] [Google Scholar]
- 59. Lotke PA, Ecker ML. Influence of positioning of prosthesis in total knee replacement. J Bone Joint Surg Am 1977;59:77–79. [PubMed] [Google Scholar]
- 60. Abdel MP, Oussedik S, Parratte S, Lustig S, Haddad FS. Coronal alignment in total knee replacement: historical review, contemporary analysis, and future direction. Bone Joint J 2014;96-B:857-62. [DOI] [PubMed] [Google Scholar]
- 61. Cherian JJ, Kapadia BH, Banerjee S, Jauregui JJ, Issa K, Mont MA. Mechanical, anatomical, and kinematic axis in TKA: concepts and practical applications. Curr Rev Musculoskelet Med 2014;7:89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Hungerford DS, Krackow KA. Total joint arthroplasty of the knee. Clin Orthop Relat Res 1985;192:23–33. [PubMed] [Google Scholar]
- 63. Insall JN, Binazzi R, Soudry M, Mestriner LA. Total knee arthroplasty. Clin Orthop Relat Res 1985;192:13–22. [PubMed] [Google Scholar]
- 64. Mooney LT, Smith A, Sloan K, Clark GW. The effect of the native kinematics of the knee on the outcome following total knee arthroplasty. Bone Joint J 2016;98-B:1471–1478. [DOI] [PubMed] [Google Scholar]
- 65. Nakamura S, Tian Y, Tanaka Y, et al. The effects of kinematically aligned total knee arthroplasty on stress at the medial tibia: a case study for varus knee. Bone Joint Res 2017;6:43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Waterson HB, Clement ND, Eyres KS, Mandalia VI, Toms AD. The early outcome of kinematic versus mechanical alignment in total knee arthroplasty: a prospective randomised control trial. Bone Joint J 2016;98-B:1360–1368. [DOI] [PubMed] [Google Scholar]
- 67. Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am 2010;92:2143–2149. [DOI] [PubMed] [Google Scholar]
- 68. Suh DS, Kang KT, Son J, Kwon OR, Baek C, Koh YG. Computational study on the effect of malalignment of the tibial component on the biomechanics of total knee arthroplasty: a finite element analysis. Bone Joint Res 2017;6:623–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Matsumoto T, Takayama K, Ishida K, Hayashi S, Hashimoto S, Kuroda R. Radiological and clinical comparison of kinematically versus mechanically aligned total knee arthroplasty. Bone Joint J 2017;99-B:640–646. [DOI] [PubMed] [Google Scholar]
- 70. Kutzner I, Bender A, Dymke J, Duda G, von Roth P, Bergmann G. Mediolateral force distribution at the knee joint shifts across activities and is driven by tibiofemoral alignment. Bone Joint J 2017;99-B:779–787. [DOI] [PubMed] [Google Scholar]
- 71. Shelton TJ, Nedopil AJ, Howell SM, Hull ML. Do varus or valgus outliers have higher forces in the medial or lateral compartments than those which are in-range after a kinematically aligned total knee arthroplasty? Limb and joint line alignment after kinematically aligned total knee arthroplasty. Bone Joint J 2017;99-B:1319–1328. [DOI] [PubMed] [Google Scholar]
- 72. Vertullo CJ, Lewis PL, Peng Y, Graves SE, de Steiger RN. The effect of alternative bearing surfaces on the risk of revision due to infection in minimally stabilized total knee replacement: an analysis of 326,603 prostheses from the Australian Orthopaedic Association National Joint Replacement Registry. J Bone Joint Surg Am 2018;100:115–123. [DOI] [PubMed] [Google Scholar]
- 73. Venable CS, Stuck WG. Clinical uses of vitallium. Ann Surg 1943;117:772–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Gunston FH, MacKenzie RI. Complications of polycentric knee arthroplasty. Clin Orthop Relat Res 1976;120:11–17. [PubMed] [Google Scholar]
- 75. Stulberg SD, Stulberg BN, Hamati Y, Tsao A. Failure mechanisms of metal-backed patellar components. Clin Orthop Relat Res 1988;236:88–105. [PubMed] [Google Scholar]
- 76. Connelly GM, Rimnac CM, Wright TM, Hertzberg RW, Manson JA. Fatigue crack propagation behavior of ultrahigh molecular weight polyethylene. J Orthop Res 1984;2:119–125. [DOI] [PubMed] [Google Scholar]
- 77. Collier MB, Engh CA, Jr, McAuley JP, Engh GA. Factors associated with the loss of thickness of polyethylene tibial bearings after knee arthroplasty. J Bone Joint Surg Am 2007;89:1306–1314. [DOI] [PubMed] [Google Scholar]
- 78. Collier JP, Sperling DK, Currier JH, Sutula LC, Saum KA, Mayor MB. Impact of gamma sterilization on clinical performance of polyethylene in the knee. J Arthroplasty 1996;11:377–389. [DOI] [PubMed] [Google Scholar]
- 79. Brown TS, Van Citters DW, Berry DJ, Abdel MP. The use of highly crosslinked polyethylene in total knee arthroplasty. Bone Joint J 2017;99-B:996–1002. [DOI] [PubMed] [Google Scholar]
- 80. Matassi F, Paoli T, Civinini R, Carulli C, Innocenti M. Oxidized zirconium versus cobalt-chromium against the native patella in total knee arthroplasty: patellofemoral outcomes. Knee 2017;24:1160–1165. [DOI] [PubMed] [Google Scholar]
- 81. Ahmed I, Salmon LJ, Waller A, Watanabe H, Roe JP, Pinczewski LA. Total knee arthroplasty with an oxidised zirconium femoral component: ten-year survivorship analysis. Bone Joint J 2016;98-B:58–64. [DOI] [PubMed] [Google Scholar]
- 82. Vertullo CJ, Lewis PL, Graves S, Kelly L, Lorimer M, Myers P. Twelve-year outcomes of an oxinium total knee replacement compared with the same cobalt-chromium design: an analysis of 17,577 prostheses from the Australian Orthopaedic Association National Joint Replacement Registry. J Bone Joint Surg Am 2017;99:275–283. [DOI] [PubMed] [Google Scholar]
- 83. Essner A, Herrera L, Hughes P, Kester M. The influence of material and design on total knee replacement wear. J Knee Surg 2011;24:9–17. [DOI] [PubMed] [Google Scholar]
- 84. Solarino G, Piconi C, De Santis V, Piazzolla A, Moretti B. Ceramic total knee arthroplasty: ready to go? Joints 2017;5:224–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Nakamura S, Minoda Y, Nakagawa S, et al. Clinical results of alumina medial pivot total knee arthroplasty at a minimum follow-up of 10 years. Knee 2017;24:434–438. [DOI] [PubMed] [Google Scholar]
- 86. Nakamura S, Ito H, Nakamura K, Kuriyama S, Furu M, Matsuda S. Long-term durability of ceramic tri-condylar knee implants: a minimum 15-year follow-up. J Arthroplasty 2017;32:1874–1879. [DOI] [PubMed] [Google Scholar]
- 87. de Ruiter L, Janssen D, Briscoe A, Verdonschot N. The mechanical response of a polyetheretherketone femoral knee implant under a deep squatting loading condition. Proc Inst Mech Eng H 2017;231:1204–1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Gill TJ, Van de, Velde SK, Wing DW, Oh LS, Hosseini A, Li G. Tibiofemoral and patellofemoral kinematics after reconstruction of an isolated posterior cruciate ligament injury: in vivo analysis during lunge. Am J Sports Med 2009;37:2377–2385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Hsieh YF, Draganich LF, Ho SH, Reider B. The effects of removal and reconstruction of the anterior cruciate ligament on patellofemoral kinematics. Am J Sports Med 1998;26:201–209. [DOI] [PubMed] [Google Scholar]
- 90. von Eisenhart-Rothe R, Lenze U, Hinterwimmer S, et al. Tibiofemoral and patellofemoral joint 3D-kinematics in patients with posterior cruciate ligament deficiency compared to healthy volunteers. BMC Musculoskelet Disord 2012;13:231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Levai JP, McLeod HC, Freeman MA. Why not resurface the patella? J Bone Joint Surg Br 1983;65:448–451. [DOI] [PubMed] [Google Scholar]
- 92. Abdel MP, Parratte S, Budhiparama NC. The patella in total knee arthroplasty: to resurface or not is the question. Curr Rev Musculoskelet Med 2014;7:117–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Forster H, Fisher J. The influence of continuous sliding and subsequent surface wear on the friction of articular cartilage. Proc Inst Mech Eng H 1999;213:329–345. [DOI] [PubMed] [Google Scholar]
- 94. Scott WN, Kim H. Resurfacing the patella offers lower complication and revision rates. Orthopedics 2001;24:24. [DOI] [PubMed] [Google Scholar]
- 95. Ranawat CS. The patellofemoral joint in total condylar knee arthroplasty: pros and cons based on five- to ten-year follow-up observations. Clin Orthop Relat Res 1986;205:93–99. [PubMed] [Google Scholar]
- 96. Keblish PA, Varma AK, Greenwald AS. Patellar resurfacing or retention in total knee arthroplasty: a prospective study of patients with bilateral replacements. J Bone Joint Surg Br 1994;76:930–937. [PubMed] [Google Scholar]
- 97. Feller JA, Bartlett RJ, Lang DM. Patellar resurfacing versus retention in total knee arthroplasty. J Bone Joint Surg Br 1996;78:226–228. [PubMed] [Google Scholar]
- 98. Meneghini RM. Should the patella be resurfaced in primary total knee arthroplasty? An evidence-based analysis. J Arthroplasty 2008;23:11–14. [DOI] [PubMed] [Google Scholar]
- 99. Kim BS, Reitman RD, Schai PA, Scott RD. Selective patellar nonresurfacing in total knee arthroplasty: 10 year results. Clin Orthop Relat Res 1999;367:81–88. [PubMed] [Google Scholar]
- 100. Zangger P, Detsky A. Computer-assisted decision analysis in orthopedics: resurfacing the patella in total knee arthroplasty as an example. J Arthroplasty 2000;15:283–288. [DOI] [PubMed] [Google Scholar]
- 101. Grassi A, Compagnoni R, Ferrua P, et al. Patellar resurfacing versus patellar retention in primary total knee arthroplasty: a systematic review of overlapping meta-analyses. Knee Surg Sports Traumatol Arthrosc 2018;26:3206–3218. [DOI] [PubMed] [Google Scholar]
- 102. Pilling RW, Moulder E, Allgar V, Messner J, Sun Z, Mohsen A. Patellar resurfacing in primary total knee replacement: a meta-analysis. J Bone Joint Surg Am 2012;94:2270–2278. [DOI] [PubMed] [Google Scholar]
- 103. Chen K, Li G, Fu D, Yuan C, Zhang Q, Cai Z. Patellar resurfacing versus nonresurfacing in total knee arthroplasty: a meta-analysis of randomised controlled trials. Int Orthop 2013;37:1075–1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. He J-Y, Jiang L-S, Dai L-Y. Is patellar resurfacing superior than nonresurfacing in total knee arthroplasty? A meta-analysis of randomized trials. Knee 2011;18:137–144. [DOI] [PubMed] [Google Scholar]
- 105. Fu Y, Wang G, Fu Q. Patellar resurfacing in total knee arthroplasty for osteoarthritis: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 2011;19:1460–1466. [DOI] [PubMed] [Google Scholar]
- 106. Blyth MJG, Anthony I, Rowe P, Banger MS, MacLean A, Jones B. Robotic arm-assisted versus conventional unicompartmental knee arthroplasty: exploratory secondary analysis of a randomised controlled trial. Bone Joint Res 2017;6:631–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Clement ND, Deehan DJ. Knee biomechanics: will we ever know the truth? Bone Joint Res 2018;7:325–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Roussot MA, Haddad FS. The evolution and role of patellofemoral joint arthroplasty: the road less travelled, but not forgotten. Bone Joint Res 2019;7:636–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Haddad FS. Evolving techniques: the need for better technology. Bone Joint J 2017;99-B:145–146. [DOI] [PubMed] [Google Scholar]