Abbreviations
- eConsult
electronic consultation
- PCMH‐N
patient‐centered medical home‐neighbors
- PCP
primary care provider
- RVU
relative work unit
The burden of chronic liver disease in the United States is likely underestimated.1 Studies have demonstrated increasing complications of hepatitis C cirrhosis, increasing prevalence of nonalcoholic fatty liver disease, and the rising incidence of liver cancer.2, 3, 4 Nonalcoholic fatty liver disease has an estimated prevalence of approximately 20%‐35% in the United States and is expected to increase commensurate with the current obesity epidemic.5, 6 Hepatocellular carcinoma is expected to surpass breast, colorectal, and prostate cancers to become the third leading cause of cancer‐related death by 2030.7 Despite this increasing burden of disease, there remains a shortage of specialists to care for these patients. In fact, the American Association of Medical Colleges has predicted a shortage of more than 40,000 specialty physicians by 2020 and more than 65,000 by the year 2025.8, 9 With just over 1,000 fully trained hepatologists practicing in the United States, an increasingly growing coverage gap will emerge without clear solutions.
It is widely acknowledged that access to specialty care is a common problem in the United States' health care system with demand for specialists far surpassing supply in most tertiary care referral centers.10 There has been an observed trend upward in the number of ambulatory clinic visits and the percentage of those visits that result in a referral to a specialty provider.11 In fact, referral rates have more than doubled in the past decade, leading to more than a 3.5‐fold increase in referral‐generating visits for all Medicare patients.12 Furthermore, a survey of safety‐net hospitals in the United States revealed an average wait time of between 6 and 12 months for an initial visit with a specialist.13 Ultimately, traditional workflow for ambulatory referrals to specialists has led to higher costs and more fragmented care, as communication breakdowns occur commonly in the outpatient referral process.14
Electronic consultations (eConsults) offer one potential solution to improving access to specialty care for patients with liver disease. eConsults are defined as “an asynchronous, directed communication over a secure electronic medium that involves sharing of patient‐specific information and seeks clarification or guidance regarding clinical care.”15 eConsults allow for quick, direct, and documented communication between specialists and primary care physicians (PCPs) and may obviate the need for face‐to‐face visits in clinic (Fig. 1). As such, they have immense potential in providing cost‐effective and efficient care to patients while expediting coordination with a specialist for commonly encountered clinical questions in the primary care setting.16
Figure 1.
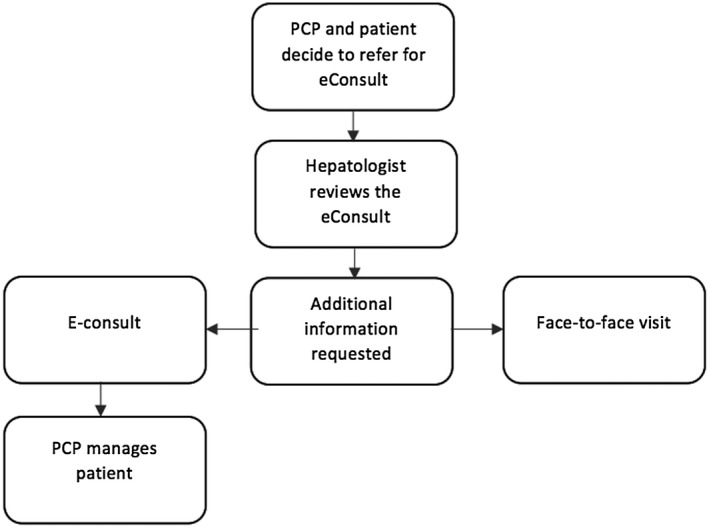
Basic steps of an eConsult. The diagram depicts the general steps involved in placing an eConsult, although not all steps occur for every eConsult placed. PCPs place an eConsult through the electronic health record. It is then reviewed by a specialist who may deem it too complex for eConsult, request additional information, or close the eConsult by making management recommendations to the PCP.
Patients and Methods
This retrospective study of eConsults to hepatology specialists was completed at a single tertiary care academic medical center in the United States from March 1, 2015, to May 1, 2018. The eConsults workflow at our institution operates through an “opt‐in” model in which PCPs may choose to refer patients to hepatology through an eConsult or traditional ambulatory referral. eConsult questions were identified as pertaining to either luminal gastroenterology or hepatology and referred for answers depending on the subject of the clinical query. eConsults made within the medical center's health system were cataloged and deemed appropriate for inclusion in the study if they were initiated by a PCP to a hepatologist. eConsults to hepatology were excluded if patients were already established in the hepatology clinic. eConsults referred to hepatology by another specialty provider were excluded, as grant funding for the pilot of this program limited its use to PCPs and midlevel providers in primary care clinics. Referring providers received 0.5 relative work units (RVUs) for each eConsult placed. A total of 187 eConsults to hepatology were identified during the study period, and seven eConsults were excluded.
We then analyzed the trend of the total number of eConsults placed to hepatology within the time period of the study. Using retrospective chart review, each eConsult was individually evaluated to identify the most common reasons for eConsult, time to eConsult response, and rate of conversion to an initial visit with a hepatologist. Time to eConsult response was identified by the total turnaround time between the placement of the eConsult to hepatology and the PCP receiving a response, as tracked in the institution's electronic health record. The average time it took for hepatology to answer each consult was identified based on a standardized template and International Classification of Disease‐10 code associated with each eConsult. Furthermore, indirect costs saved through avoided traditional referrals and travel costs were evaluated by examining the distance each individual patient would have traveled round‐trip to be seen as an initial visit in clinic.
Results
A total of 187 eConsults were placed to hepatology during the study period through a standardized eConsult template jointly created by a team of PCPs and hepatologists. The average response time was 22 hours (± 28 hours) compared with an average wait time of 68 days (± 55 days) for an initial visit in clinic (Fig. 2). Hepatologists spent less than 20 minutes answering 81% of eConsults and less than 10 minutes answering 40% of eConsults. The most common eConsults were related to management of abnormal liver enzymes (47%), abnormal imaging of the liver (27%), viral hepatitis (22%), and drug‐induced liver injury (4%). Only 44 of 187 eConsults led to an initial visit with a hepatologist. PCPs were able to use the recommendations by the specialist in 96.9% of patients, but 3.1% of patients were lost to PCP follow‐up. The most common recommendations made by the consultant included further laboratory testing and/or further imaging studies. For the 44 patients who were ultimately seen in a hepatology clinic, 87% had received the complete work‐up recommended by the specialist before their initial visit. Most eConsults, 143 of 187 (76%), were resolved and obviated the need for face‐to‐face referrals. Interestingly, 100% of the patients who were seen as initial visits had abnormal imaging findings that required follow‐up imaging, liver biopsy, or even presentation at multidisciplinary case conferences. There were no instances in which patients who were initially referred for eConsult were later seen in a hepatology clinic unless this recommendation was made in the initial eConsult itself. The total round‐trip mileage (home to clinic visit) saved was 10,599 miles.
Figure 2.
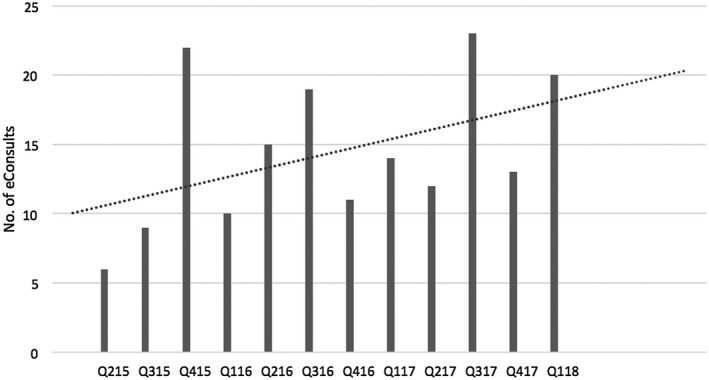
Trend of total eConsults to hepatology. The diagram illustrates the total number of eConsults placed to hepatology by quarter from 2015 to 2018. The overall trend in eConsult frequency has continued to rise since the program's inception, as shown.
Discussion
eConsults are an efficient and cost‐effective tool that simultaneously fulfills the aims of both patients and providers. Supply and demand mismatch for patients with liver disease is expected to worsen as the incidence of liver disease increases. Traditional ambulatory referrals by PCPs to hepatologists are often missing crucial information that enables specialists to fully address a clinical question. This lack of communication often leads to the dissatisfaction of referring providers with the quality of the specialists' feedback.14
In an effort to more effectively coordinate care for patients with complex medical needs, the practice care model of the “patient‐centered medical home” began in the late 2000s. The goal of the medical home was to improve access and communication, better utilize electronic health records, augment care management and coordination with other providers, and empower patients to share in medical decision making.17 In 2010, the American College of Physicians recognized the trend toward specialty referrals and introduced the concept of the patient‐centered medical home‐neighbors (PCMH‐N) to better integrate care for patients between PCPs (“home”) and specialists (“neighbor”).18 The PCMH‐N enhances interactions between PCPs and specialists, and promotes preconsultation exchanges to either clarify the need for or expedite referrals. Additionally, the PCMH‐N advocates for co‐management of disease between providers and expands the role of the specialist to focus on ongoing education of PCPs.19
In 2011, the Department of Health and Human Services issued new guidelines under the Affordable Care Act that created Accountable Care Organizations (ACOs) to further incentivize communication between providers.20 The goal of ACOs is to improve care provided to patients while reducing the overall cost of their services.21 eConsults represent a nontraditional care delivery model, akin to preconsultation exchanges, that improves access to specialty care.
Preconsultation exchanges in hepatology have been identified as particularly helpful to PCPs, as hepatology referrals are usually more cognitive in nature than they are procedural.20 Past studies have noted that despite their potential, 40% of preconsultation exchanges in hepatology lack appropriate information needed for specialists to make adequate recommendations.21 The use of standardized eConsults is beneficial to patients in multiple ways. There are significant cost savings associated with avoided face‐to‐face visits, which include travel costs as well as lost productivity and wages. These cost savings are even more notable to patients traveling long distances to be seen at tertiary care centers with large catchment areas. Furthermore, eConsults improve patient satisfaction by decreasing the overall wait times for in‐person visits.22 eConsults also improve the quality of care by making specialty input more timely. Patients who were referred to hepatology in our study through eConsult received specific and relevant feedback from a hepatologist in an average of 22 hours compared with a wait time of 68 days to be seen for an in‐person visit. A survey of PCPs at the University of Virginia Health System, who referred patients for eConsult, indicated that 91% were highly satisfied with the eConsult response; patients who were referred quoted the “practicality and ease of eConsults” as their primary benefit.23 Perhaps even more compelling is that patients who had never been referred for eConsult indicated a preference for future eConsults compared with traditional outpatient referrals.24
The opportunity cost savings for the health system is also promising. The use of eConsult as an alternative to traditional referrals to a hepatologist averted an in‐person initial visit in 143 of 187 patients included in this study. The proportion of eConsults that were addressed without the need for an initial visit is termed the clinic avoidance rate and was noted to be 76% in our study.25 It is estimated that the costs saved in provider charges average $124 when comparing the reimbursement of an eConsult to that of a level 4 office visit.22
Although eConsult programs cut costs and provide a standardized workflow to the “curbside consult,” creating buy‐in for their implementation requires the support of both PCPs and specialists. PCPs gain more access to specialty input and receive RVU credit for each completed eConsult. There is concern that PCPs may be overburdened by increased task‐shifting to the primary care setting, although we believe this most commonly occurs in practice settings, such as the Los Angeles County Department of Health, where eConsults are mandatory and traditional referrals are not available to PCPs.26, 27 Hepatologists, on the other hand, benefit from a more centralized consult system and receive recognition of their work by time‐based RVUs for each eConsult completed. eConsults answered in less than 10 minutes are reimbursed approximately $57 dollars (0.5 RVUs) and those that take between 11 and 20 minutes to answer are reimbursed approximately $114 (1 RVU). eConsults also enable specialists to make management recommendations earlier in the clinical courses of patients and thereby eliminate marginal referrals to ultimately increase the clinical complexity of their initial visits.
Since the implementation of the hepatology eConsult program, there has been significant growth in the number of eConsults placed, and the clinic capacity ratio, or supply–demand mismatch between providers and patients, has decreased. The number of initial visits per clinician grew 9% during the study period, with an average number of initial visits per clinician of 687 in 2017 and 723 in 2018. Although impossible to determine a direct correlation, one could reason that up‐front specialist support through the eConsult program made a positive impact on patients and led to an increased show rate.
Furthermore, the eConsult program has been well‐received by providers at our institution, as it empowers PCPs and allows for ongoing education through the routine discourse of the eConsult exchange.20 Interestingly, when identifying the most common reason for eConsult, we noted that the percentage of eConsults for management of abnormal liver enzymes had decreased by 15% in the past 10 months. Survey data indicate that this is directly attributable to the educational points made by hepatologists during previous eConsults and has served to improve the disease‐specific familiarity for PCPs with management of patients with liver disease.24
In conclusion, as health care moves away from traditional fee‐for‐service to value‐based reimbursement, it is necessary to build a care delivery infrastructure that supports efficient, less expensive, and more accessible care. As the burden and clinical complexity of liver disease increases, the clinic capacity gap of hepatologists is expected to widen. eConsults offer one potential solution to that growing coverage gap and represent the revival of close, collaborative care between specialists and PCPs. Further work should expand the role of eConsults across health systems to design new and innovative workflow and improve access to hepatology care.
Supported by the Centers for Medicare and Medicaid Services (Grant/Award Number: 1C1CMS331324‐01‐00).
Potential conflict of interest: Nothing to report.
See Editorial on Page 1171.
References
- 1. Scaglione S, Kliethermes S, Cao G, Shoham D, Durazo R, Luke A, et al. The epidemiology of cirrhosis in the United States: a population‐based study. J Clin Gastroenterol 2015;49:690‐696. [DOI] [PubMed] [Google Scholar]
- 2. Davis GL, Alter MJ, El–Serag H, Poynard T, Jennings LW. Aging of hepatitis C virus (HCV)‐infected persons in the United States: a multiple cohort model of HCV prevalence and disease progression. Gastroenterology 2010;138(2):513‐521, e1‐e6. [DOI] [PubMed] [Google Scholar]
- 3. Charlton MR, Burns JM, Pedersen RA, Watt KD, Heimbach JK, Dierkhising RA. Frequency and outcomes of liver transplantation for nonalcoholic steatohepatitis in the United States. Gastroenterology 2011;141:1249‐1253. [DOI] [PubMed] [Google Scholar]
- 4. Asrani SK, Kouznetsova M, Ogola G, Taylor T, Masica A, Pope B, et al. Increasing healthcare burden of chronic liver disease compared to other chronic diseases, 2004–2013. Gastroenterology 2018;155:719‐729.e4. [DOI] [PubMed] [Google Scholar]
- 5. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311:806‐814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Estes C, Razavi H, Loomba R, Younossi Z, Sanyal AJ. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology 2018;67:123‐133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res 2014;74:2913‐2921. [DOI] [PubMed] [Google Scholar]
- 8. Grover A. Now you have healthcare coverage—but who will treat you? https://www.aamc.org/advocacy/secondopinion/296560/070312.htm. Accessed June 20, 2018. [Google Scholar]
- 9. De Haleouga, Marzio DL, Herrine SK. Training the next generation of hepatologist: what will they need to know? Clinical Liver Disease 2015;5:129‐130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gleason N, Prasad PA, Ackerman S, Ho C, Monacelli J, Wang M, et al. Adoption and impact of an eConsult system in a fee‐for‐service setting. Healthcare 2017;5:40‐45. [DOI] [PubMed] [Google Scholar]
- 11. Barnett JC, Vornovitsky MS. Health insurance coverage in the United States: 2015. Washington, DC: US Government Printing Office; 2016:60‐257. [Google Scholar]
- 12. Mayorga CA. Econsults: an approach to improve access to specialty care. September 2017. Internal Medicine Grand Rounds at University of Texas Southwestern Medical Center, Dallas, TX. [Google Scholar]
- 13. Felt‐Lisk S, McHugh M, Howell E. Monitoring local safety‐net providers: do they have adequate capacity? Health Aff 2002;21:277‐283. [DOI] [PubMed] [Google Scholar]
- 14. Gandhi TK, Sittig DF, Franklin M, Sussman AJ, Fairchild DG, Bates DW. Communication breakdown in the outpatient referral process. JGIM 2000;15:626‐631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Liddy C, Drosinis P, Deri Armstrong C, McKellips F, Afkham A, Keely E. What are the cost savings associated with providing access to specialist care through the Champlain BASE eConsult service? A costing evaluation. BMJ Open 2016;6:e01920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Vimalanadnda V, Gupte G, Seraj SM, Orlander J, Berlowitz D, Fincke BG, et al. Electronic‐consultations (e‐consults) to improve access to specialty care: a systematic review and narrative synthesis. J Telemed Telecare 2015;21:323‐330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fisher ES. Building a medical neighborhood for the medical home. NEJM 2008;359:1202‐1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Laine C. Welcome to the patient‐centered medical neighborhood. Ann Int Med 2011;154:60. [DOI] [PubMed] [Google Scholar]
- 19. Yee HF. The patient‐centered medical home neighbor: a subspecialty physician's view. Ann Int Med 2011;154:63‐64. [DOI] [PubMed] [Google Scholar]
- 20. Sewll JL, Guy J, Kwon A, Chen AH, Yee HF Jr. Preconsultation exchange for ambulatory hepatology consultation. Am J Med 2013;126:523‐528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Keely E, Canning S, Soloojee N, Afkham A, Liddy C. Improving access to gastroenterologist using eConsultation: a way to potentially shorten wait times. J Can Association Gastroenterology 2018;1:124‐128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff 2008;27:759‐769. [DOI] [PubMed] [Google Scholar]
- 23. Wasfy JH, Rao SK, Kalwani N, Chittle MD, Richardson CA, Gallen KM, et al. Longer‐term impact of cardiology e‐consults. Am Heart J 2016;173:86‐93. [DOI] [PubMed] [Google Scholar]
- 24. Mehotra A, Forrest CB, Lin CY. Dropping the baton: specialty referrals in the United States. Milbank Q 2011;89:39‐68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dowdell L, Babbott S, Chen J, Kubiak N. Implementing eConsult and eCounseling: promise, pitfalls, and progress. Denver, CO: Workshop at SGIM; 2018. [Google Scholar]
- 26. Liddy C, Drosinis P, Keely E. Electronic consultation systems: worldwide prevalence and their impact on patient care—a systematic review. Fam Pract 2016;33:274‐285. [DOI] [PubMed] [Google Scholar]
- 27. Lee MS, Ray KN, Mehrotra A, Giboney P, Yee HF, Barnett ML. Primary care practitioners' perceptions of electronic consult systems: a qualitative analysis. JAMA Intern Med 2018;178:782‐789. [DOI] [PMC free article] [PubMed] [Google Scholar]


