Abstract
Following anterior cruciate ligament reconstruction, individuals experience inadequate functioning of the quadriceps and decreased muscular strength. Decreased function delays return to physical activity and increases potential for re-injury. While several squat variations exist, a new variation has emerged in rehabilitation. The purpose of this study was to compare muscle activation of the Vastus Lateralis (VL), Vastus Medialis (VM), Rectus Femoris (RF), Gluteus Maximus (GM), and anterior posterior center of pressure (AP displacement) alterations during a single leg squat variation (SLS variation) versus a traditional split squat using electromyography (EMG) in healthy active females. Seventeen females performed one set of both squat variations on a force plate while muscle activation was measured. Paired t-tests were used to compare dependent variable (DV) means between squat variations. Results indicated SLS variation yielded lower peak and mean quadriceps activation compared to traditional split squat, (p < 0.05). However, peak and mean GM muscle activity was greater in the SLS variation compared to the traditional split squat, (p < 0.01). Lastly, AP displacement was greater during the SLS variation, (p < 0.001). All three quadricep muscles had greater peak and mean EMG suggesting the traditional split squat be used for quadricep activation in rehabilitation/training settings, while the SLS variation should be prescribed for greater GM muscle activation. Understanding muscle activation patterns amongst squat variations can be practically applied by therapists, coaches and trainers to aid in reducing risks of arthrokinetic dysfunction via synergistic dominance, faster return to physical activity and normal functions of daily activity.
Keywords: electromyography, rehabilitation, ground reactive forces, resistance training, wireless goniometer
INTRODUCTION
Previous research estimates roughly 250,000 physically active young adults sustain anterior cruciate ligament (ACL) injuries annually (16,18). In 2000, over half of the ACL injuries lead to anterior cruciate ligament reconstruction (ACLR) (24). Today, the incident and reconstruction rates are rising, perhaps due to year-round sports starting at a younger age, increased clinician awareness of signs and symptoms, increased female athletic participation and improved diagnostic technology (4). Aside from restoring range of motion, the goal of ACLR rehabilitation is strengthening leg musculature while avoiding excessive loading of the reconstructed ACL (6). Developing optimal rehabilitation methods for post knee operations is a constant focus in the field of sports medicine and physical therapy. A traditional double-legged squat is a validated exercise that is widely used in post-operative ACL recovery (12). The squat requires use of the back, hip, and thigh muscles making it a compound movement (13). However, even with traditional squat techniques used, many post-operative patients are not maximizing recovery within the recommended time frame (3,5,29). One of the most prevalent issues after ACLR is proper functioning of the quadriceps (22). Decreased function causes a delay in the return to physical activity and increases potential for re-injury (21). Designing an optimal exercise regimen is crucial in order to regain quadriceps strength.
Electromyography (EMG) measures electrical currents generated within the muscle during contraction—representing neuromuscular activity. EMG allows researchers and clinicians to determine how a specific movement recruits muscle to contract (27). Numerous studies have analyzed muscle activity of the skeletal muscles during exercise (25,7). For example, Monajati et al. (2018) found a traditional split squat will elicit higher quadriceps muscle activation, specifically in the Vastus Medialis (VM) and Vastus Lateralis (VL), compared to a double leg squat performed with both legs on the ground, likely due to shifting from two points of contact and distribution to one. A single leg squat has also shown to elicit levels of quadriceps activation that are high enough for strength building, which is advantageous for rebuilding quadriceps muscle symmetry between two legs after knee surgery like ACLR (7).
While the traditional single leg squat is commonly prescribed, other variations exists such as a single leg forward leaning squat (SLS variation). To our knowledge, no studies have been conducted to observe muscle activation comparisons between two separate single-leg squat variations creating a void in existing literature. Furthermore, most studies examined male participants creating an additional void. This could be beneficial information for therapists and trainers during ACLR rehabilitation.
Therefore, the purpose of this study was to compare muscle activation of the VL, VM, Rectus Femoris (RF), and Gluteus Maximus (GM) between the SLS variation and the traditional split squat in healthy, college-aged females. Due to hormonal, anatomical, environmental and neuromuscular factors, the number of female ACL tears are greater compared to the number seen in males, making them the preferred subjects (8). A secondary variable examined was anterior/posterior (AP) displacement of center of pressure (COP) changes via force plate between the traditional split squat and SLS variation. Hip degree angle differences were also recorded. It was hypothesized that an exaggerated forward shift of the center of gravity in the SLS variation would result in positive AP displacement values and increased muscle activity of the VL, VM, RF while decreasing muscle activation of the GM. This study aims to provide evidence-based recommendations that may lead to novel clinical procedures and efficient, timely rehabilitation.
METHODS
Participants
A power analysis performed by G*POWER 3.1.9.2 (Universitat Kiel, Germany) indicated 17 participants were needed with a power of 0.80, an effect size of 0.65, and an α= 0.05. Seventeen females (n = 17) participated in this study (19.70±1.49 years, 168.68±7.62 cm, 60.43±7.71 kg). Participants had no previous injury to their dominant leg in the last six months. Exclusion criteria included previous ACL reconstruction on their dominant leg. Participants stated to have participated in recreational, physical activity three times a week for 30 minutes (20). A Pre-Activity Readiness Questionnaire (PAR-Q) was completed by all participants to guard against any adverse events during exercise and to screen for any prior health conditions that would exclude them from participation. All subjects provided written, informed consent prior to participation. Ethics approval for the study was approved from a University Institutional Review Board.
Protocol
All participants attended two training sessions. During the first session, participants were informed of the benefits/risks and completed all required paperwork. Participants were familiarized with squat variations, proper movements, and the protocol for data collection. Anthropometric measurements, including sex, height, weight, age, and dominant leg was assessed.
During session two, muscle activity was measured for the VM, VL, RF, and GM of the dominant leg via Electromyography (Delsys Inc, Trigno™ EMG Wireless System, SP-W02A-242 Boston, MA USA). Leg dominance was determined by which leg the participants would preferentially use to kick a ball (11). In preparation for electrode placement, the surface of the skin was rid of any hair and cleaned with isopropyl alcohol wipes. Electrodes (Delsys Inc, Boston, MA USA) were placed according to the SENIAM project guidelines) (18). A Delsys goniometer and goniometer adapter were placed vertically at the hip joint, with the goniometer situated so that its mid-length point was centered at the greater trochanter, the proximal component situated on the lateral pelvis, and the distal component situated on the lateral thigh (30). This measurement was observed to ensure consistent hip angle was achieved for all participants. Participants were instructed to partake in a standard warm-up: five minutes on a treadmill at a self-selected pace (31).
Following completion of the warm-up, participants then performed maximum voluntary isometric contractions (MVICs) for the GM, VL, VM and RF. To obtain MVICs for the quadriceps muscles, the participant was seated on an examination table with the knee at approximately 110 degrees of knee flexion. The participant was then asked to extend their leg with maximal force for three seconds pressing into an immovable object. A two-minute rest period was given between trials. The MVIC for the GM required the participant to lie in a prone position on a table, with the participant’s knee flexed to 90 degrees. An immovable apparatus placed downward pressure on the popliteal region of the leg and the sole of the shoe. Instruction was given to contract the GM pressing the foot vertically for three seconds against the immovable apparatus (14).
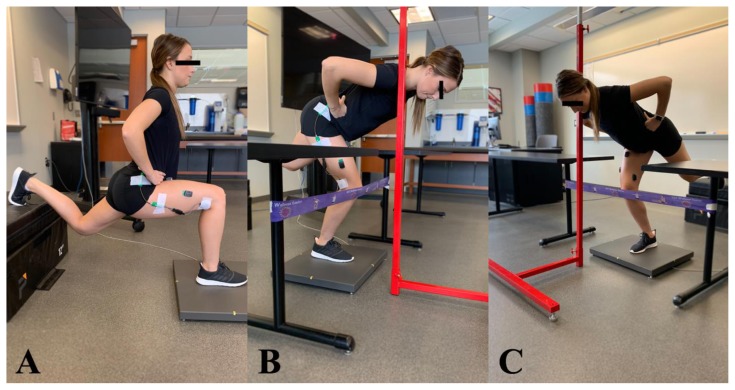
Following completion of the MVIC’s, each participant performed 7 single-leg squats under two separate counterbalanced conditions (23). These counterbalanced groups were chosen at random. A resistance band was fixed at knee level for the participants to tap during each squat to ensure their knee remained directly over their toes, and consistent movements among participants. In the traditional split squat, the rear leg was elevated to guarantee that the descent phase allowed for 90° knee flexion of the front leg. The height was tailored to each participant (see Figure 1, A). During the SLS variation, a vertical bar was set up in front of the participant. The distance each participant stood from the vertical bar was adjusted to ensure the participants hip flexion was within the range of 90° and 110° of flexion as they tapped their shoulder on the bar (see Figure 1, B & C). The eccentric phase of the movement was from the starting position to instructed knee and hip flexion (see Figure 1, A & B). The concentric phase was from the deepest portion of squat to full knee and hip extension. A metronome was set at the rate of 60 beats per minute to control for uniform squat cadences among all participants (26). Instruction was given to descend until their shoulder touched the bar for two beats of the metronome, ascended for two beats towards standing and paused in the starting position for two beats (26). A five-minute rest followed each set of seven repetitions. Participants performed all squats on a force plate (Bertec Corp, Columbus OH) in order to collect AP displacement.
Figure 1.
Experimental set up of participant performing traditional split squat (A) and SLS variation (B & C) at points of maximum knee flexion
For both squats, EMG signals were band-pass filtered with a cut-off frequency of 20–450 Hz respectively. Furthermore, signals were full-wave rectified and smoothed using a root-mean-square (RMS) filter along a 250 ms moving window (31). The average peak and mean muscle activity of repetitions 3, 4, and 5 of both squat protocols were normalized to the peak amplitude during the MVIC for the respective muscles for each participant. Both the eccentric and concentric phases were analyzed for all repetitions.
Statistical Analysis
For all statistical analysis, an alpha level was set at 0.05, beta level at 0.2, and power at 0.8. Eight separate paired-sample t-tests were used to compared peak and mean muscle activity for all four muscles between both squat variations (traditional split squat vs. SLS variation). One additional t-test was completed to assess AP displacement between the traditional split and the SLS variation. All analyses were ran via SPSS (V.25) (Chicago, IL, USA). One participant’s data for VM peak and mean muscle activity was removed prior to data analysis due to being greater than ±2 standard deviations away from the mean.
RESULTS
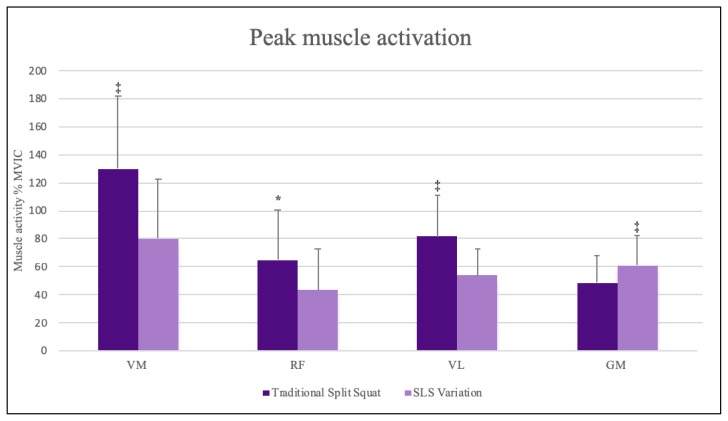
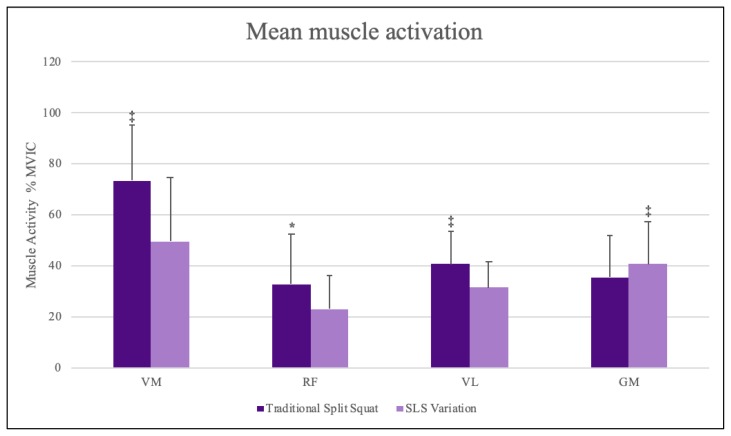
All eight paired samples t-test examining muscle activity between the two squat variations were statistically significant. The traditional split squat demonstrated greater peak and mean muscle activation vs. the SLS variation for all three examined quadriceps muscles: VL peak EMG % MVIC t(16)= −4.418, p < 0.001, d = 1.071, VL mean EMG % MVIC t (16)= −3.343, p = 0.004, d = 0.811, VM peak EMG % of MVIC t(15)= −7.464, p < 0.001, d = 1.866, VM mean EMG % of MVIC t(15)= −4.458, p < 0.001, d = 1.115, RF peak EMG % of MVIC t(16)= −2.143, p = 0.048, d = 0.520, RF mean EMG % of MVIC t(16)= −2.188, p = 0.044, d = 0.531 (Figures 2 and 3).
Figure 2.
Peak muscle activation for select lower limb muscles during two squat variations * p <0.05, ‡ p <0.001
Figure 3.
Mean muscle activation for select lower limb muscles during two squat variations * p <0.05, ‡ p <0. 001
However, the SLS variation generated greater peak and mean muscle activation of the GM than the traditional split squat; GM peak EMG % MVIC t(16)=3.611, p = 0.002, d = 0.876, GM mean EMG % MVIC t(16)= 2.641, p = 0.018, d = 0.641 (Figures 2 and 3). Lastly, the SLS variation rendered greater positive AP displacement compared to the traditional split squat t(8)= 12.927, p < 0.001, d = 4.309 (see Table 1).
Table 1.
AP displacement of COP. Positive values relate to anterior displacement, while negative values relate to posterior.
| Mean (mm) | Standard Deviation (mm) | |
|---|---|---|
| SLS Variation* | 0.01776 | 0.01638 |
| Traditional split squat* | −0.04122 | 0.01895 |
indicates p < 0.001.
DISCUSSION
The purpose of this study was to compare muscle activation of the VL, VM, RF and GM during the SLS variation versus the traditional split squat in college-aged females. Secondly, AP displacement of COP was measured between the traditional split squat and SLS variation. It was hypothesized that the SLS variation would increase muscle activity of the quadriceps (RF, VL, and VM) while decreasing the GM muscle activation. Contrary to the hypothesis, in reference to muscle activation, the results of this study indicate that the SLS variation recruits more motor units of the GM, and therefore more muscle activation compared to the traditional split squat. Additionally, the muscle activation of the three examined quadriceps muscles proved to be greater in the traditional split squat rather than the SLS variation; this finding is also contradictory to the hypothesis about muscle activation. In accordance with the hypothesis regarding AP displacement, the SLS variation produced positive AP displacement values.
Korak et al. analyzed muscle activity of five lower-body muscles during the back-squat, front-squat and deadlift; the authors found the front-squat exercise elicited greater GM muscle activity in comparison to the deadlift, likely due to an increase in hip flexion i.e. depth achieved. Shifting one’s center of mass forward creates a larger lever arm in the sagittal plane, thus requiring more internal torque be produced by the hip extensors (i.e. the GM) to overcome the external torque (19). Similarly, in the current study, the SLS variation intentionally shifted participants’ center of gravity forward and therefore eccentrically and concentrically contracting the GM greater compared to the traditional split squat. The increase in muscle activity was likely due to intentional creation of a longer external moment arm from the axis of rotation i.e. the hip. As stated previously, such alterations require more internal torque to overcome the external forces, which can explain the increased muscle activation of the GM. Table 2 indicates the SLS variation had a statistically positive mean AP displacement further validating a forward shift in center of mass. This further confirms the need for greater GM activation from the increased torque required.
Differences in squat depth, specifically from knee flexion, during the traditional split squat can also account for the increases quadricep activity compared to the SLS variation. Greater knee flexion will lengthen the quadricep muscles creating an increase in muscle activation. Gorsuch et al. (15) measured muscle activity via EMG during partial and parallel squats in 20 Division I collegiate cross-country runners. Participants performed 6 repetitions using their 10-repetition max load. Their findings indicated RF activity was significantly higher during a parallel squat rather than in a partial squat, likely attributing their results of greater ROM at the knee joint. Although the parallel squat is a weight bearing exercise, it required participants to achieve 90° knee flexion of the front leg just as the traditional split squat does, resulting in greater elongation of the quadriceps. Previous literature has further indicated a muscle lengthened to a greater degree will elicit an increase in motor unit activation (9). Therefore, the increase in muscle activity during the traditional split squat of the VM, VL, and RF was likely attributed to an increase in muscle length change from greater knee flexion compared to the SLS variation (9,15,19).
Diminished quadriceps function following ACLR increases the risk in patients of encountering synergistic dominance, which can increase the likelihood of arthrokinetic dysfunction. Synergistic dominance is defined as a neuromuscular phenomenon in which a weak prime mover is over-powered by a helper, synergist muscle (i.e. hamstrings take over GM hip extension); arthrokinetic disfunction is defined as a biomechanical and neuromuscular dysfunction resulting in altered joint motions which can lead to increased risk of injury (10). However, this occurrence is not exclusive to ACLR patients. It is often observed in cases of strong hamstrings dominating weak glutes; researchers suggest specialized exercises to increase musculature of weakened muscles (10). Though our hypothesis failed, our findings may be prescribed if a training goal is to target the GM or the quadriceps muscles. Current findings indicate the SLS variation squat to be more beneficial when compared to the traditional split squat since the SLS variation will cause greater activation of the GM, which can lead to a decrease risk of synergistic dominance and its detrimental effects. However, if training the quadriceps is the goal, the traditional split squat should be prescribed. It may be practical for future researchers to examine the difference in muscle activity of the hamstrings, hip abductors, and lumbar spine muscles during the traditional split squat and SLS variation variations. Furthermore, future research should focus on how the traditional split squat and SLS variation affect the post-ACLR population over a longer chronic period regarding rebuilding quadricep muscle strength.
A limitation of this study could be the participants themselves. Participants were trained in single leg squatting, therefore it may be assumed that trained squatters will shift their weight towards their heels, as they would for a regular squat. The purpose of the SLS variation was to shift weight forward and thus more precise instruction to shift weight into the ball of the foot could have greater impacted the values of AP displacement; this type of instruction would be provided in a clinical setting. Another limitation to our study the lack of control for foot size as a larger foot increases the participants’ base of support.
In conclusion, for young recreationally active females, the traditional split squat will recruit greater muscle activation in the VL, VM, RF, while the SLS variation squat created greater muscle activation of the GM. If the goal of a specific training is to strengthen the quadriceps, this study indicates the traditional split squat is the ideal variation of the two squats to do so. These findings can be useful for therapists, trainers, and coaches to improve ACLR recovery, and decrease synergistic dominance which can lead to arthrokinetic dysfunction.
REFERENCES
- 1.Allen CC, Dean KA, Jung AP, Petrella JK. Upper body muscular activation during variations of push-ups in healthy men. Int J Exerc Sci. 2013;6(4):278–288. [Google Scholar]
- 2.Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48:1543–1552. doi: 10.1136/bjsports-2013-093398. [DOI] [PubMed] [Google Scholar]
- 3.Ardern CL, Webster KE, Taylor NF, Feller JA. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. Am J Sports Med. 2011;39(3):538–543. doi: 10.1177/0363546510384798. [DOI] [PubMed] [Google Scholar]
- 4.Beck N, Lawrence J, Nordin D, DeFor T, Tompkins M. ACL tears in school-aged children and adolescents over 20 years. Pediatrics. 2017;139(3) doi: 10.1542/peds.2016-1877. [DOI] [PubMed] [Google Scholar]
- 5.Begalle RL, Distefano LJ, Blackburn T, Padua DA. Quadriceps and hamstrings coactivation during common therapeutic exercises. J Athl Train. 2012;47:396–405. doi: 10.4085/1062-6050-47.4.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beynnon BD, Fleming BC, Johnson RJ, Nichols CE, Renstrom PA, Pope MH. Anterior cruciate ligament strain behavior during rehabilitation exercises in vivo. Am J Sports Med. 1995;23(1):24–34. doi: 10.1177/036354659502300105. [DOI] [PubMed] [Google Scholar]
- 7.Beutler A, Cooper L, Kirkendall D, Garrett W. Electromyographic analysis of single leg, closed chain exercises: implications for knee rehabilitation. Med Sci Sports Exerc. 1998;30(Supplement):26. [PMC free article] [PubMed] [Google Scholar]
- 8.Boden BP, Griffin LY, Garrett WE. Etiology and Prevention of Noncontact ACL Injury. Phys Sportsmed. 2000;28(4):53–60. doi: 10.3810/psm.2000.04.841. [DOI] [PubMed] [Google Scholar]
- 9.Caterisano A, Moss RE, Pellinger TK, Woodruff K, Lewis VC, Booth W, Khadra T. The effect of back squat depth on the EMG activity of 4 superficial hip and thigh muscles. J Strength Cond Res. 2002;16(3):428–432. [PubMed] [Google Scholar]
- 10.Clark MA, Sutton BG, Lucett SC. NASM Essentials of Personal Fitness Training (Revised) Jones & Bartlett Publishing; 2014. [Google Scholar]
- 11.Demers E, Pendenza J, Radevich V, Preuss R. The effect of stance width and anthropometrics on joint range of motion in the lower extremities during a back squat. Int J of Ex Sci. 2018;11(1):764–775. [PMC free article] [PubMed] [Google Scholar]
- 12.Di Stasi S, Myer G, Hewett T. Neuromuscular training to target deficits associated with second anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2013;43(11):777–792. A1–11. doi: 10.2519/jospt.2013.4693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Escamilla RF. Knee biomechanics of the dynamic squat exercise. Med Sci Sports Exerc. 2001;33(1):127–141. doi: 10.1097/00005768-200101000-00020. [DOI] [PubMed] [Google Scholar]
- 14.Garden FH, Bodenheimer C. In: Handbook of manual muscle testing. Cutter NC, Kevorkian GC, editors. New York, NY: McGraw-Hill; 1999. pp. 121–154. [Google Scholar]
- 15.Gorsuch J, Long J, Miller K, Primeau K, Rutledge S, Sossong A, Durocher JJ. The effect of squat depth on multiarticular muscle activation in collegiate cross-country runners. J Strength Cond Res. 2013;27(9):2619–2625. doi: 10.1519/JSC.0b013e31828055d5. [DOI] [PubMed] [Google Scholar]
- 16.Griffen LY, Albohm MJ, Arendt EA, Bahr R, Beynnon BD, DeMaio M, Dick RW, Engebretsen L, Garrett WE, Hannafin JA, Hewett TE. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005. Am J Sports Med. 2006;34(9):1512–1532. doi: 10.1177/0363546506286866. [DOI] [PubMed] [Google Scholar]
- 17.Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes: a prospective study. Am J Sports Med. 1999;27(6):699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 18.Hermens HJ, Freriks B, Merletti R, Stegeman D, Blok J, Rau G, Hägg G. European recommendations for surface electromyography. Roessingh Res Dev. 1999;8(2):13–54. [Google Scholar]
- 19.Korak J, Paquette M, Fuller D, Caputo J, Coons J. Muscle Activation Patterns of Lower-Body Musculature Among 3 Traditional Lower-Body Exercises in Trained Women. J Strength Cond Res. 2018;32(10):2770–2775. doi: 10.1519/JSC.0000000000002513. [DOI] [PubMed] [Google Scholar]
- 20.Kuenze CM, Hertel J, Hart JM. Quadriceps muscle function after exercise in men and women with a history of anterior cruciate ligament reconstruction. J Athl Train. 2014;49(6):740–6. doi: 10.4085/1062-6050-49.3.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kvist J. Rehabilitation following anterior cruciate ligament injury. Sports Med. 2004;34(4):269–280. doi: 10.2165/00007256-200434040-00006. [DOI] [PubMed] [Google Scholar]
- 22.LoPresti C, Kirkendall DT, Street GM, Dudley AW. Quadriceps insufficiency following repair of the anterior cruciate ligament. J Orthop Sports Phys Ther. 1988;9(7):245–24. doi: 10.2519/jospt.1988.9.7.245. [DOI] [PubMed] [Google Scholar]
- 23.Macrum E, Bell DR, Boling M, Lewek M, Padua D. Effect of limiting ankle-dorsiflexion range of motion on lower extremity kinematics and muscle-activation patterns during a squat. J of Sport Rehab. 2012;21(2):144–150. doi: 10.1123/jsr.21.2.144. [DOI] [PubMed] [Google Scholar]
- 24.Mall N, Chalmers P, Moric M, Tanaka M, Cole B, Bach B, Paletta G. Incidence and Trends of Anterior Cruciate Ligament Reconstruction in the United States. Am J Sports Med. 2014;42(10):2363–2370. doi: 10.1177/0363546514542796. [DOI] [PubMed] [Google Scholar]
- 25.Monajati A, Larumbe-Zabala E, Goss-Sampson M, Naclerio F. Surface electromyography analysis of three squat exercises. J Hum Kinet. 2018 doi: 10.2478/hukin-2018-0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Panagiotopoulos E, Strzelczyk P, Herrmann M, Scuderi G. Cadaveric study on static medial patellar stabilizers: the dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2005;14:7–12. doi: 10.1007/s00167-005-0631-z. [DOI] [PubMed] [Google Scholar]
- 27.Raez MB, Hussain MS, Mohd-Yasin F. Techniques of EMG signal analysis: detection, processing, classification and applications. Biol Proced Online. 2006;8:11–35. doi: 10.1251/bpo115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Welling W, Benjaminse A, Seil R, Lemmink K, Zaffagnini S, Gokeler A. Low rates of patients meeting return to sport criteria 9 months after anterior cruciate ligament reconstruction: a prospective longitudinal study. Knee Surg Sports Traumatol Arthrosc. 2018:1–9. doi: 10.1007/s00167-018-4916-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Willcox EL, Burden AM. The influence of varying hip angle and pelvis position on muscle recruitment patterns of the hip abductor muscles during the clam exercise. J Orthop Sports Phys Ther. 2013;43(5):325–331. doi: 10.2519/jospt.2013.4004. [DOI] [PubMed] [Google Scholar]
- 30.White A, Klemetson C, Farmer B, Katsavelis, Bagwell J, Grindstaff T. Comparison of clinical fatigue protocols to decrease single-leg forward hop performance in healthy individuals. Int J Sports Phys Ther. 2018;13(2):143–151. [PMC free article] [PubMed] [Google Scholar]
- 31.Yavuz H, Erdağ D, Amca A, Aritan S. Kinematic and EMG activities during front and back squat variations in maximum loads. J of Sports Sciences. 2015;33(10):1058–1066. doi: 10.1080/02640414.2014.984240. [DOI] [PubMed] [Google Scholar]