Abstract
Purpose of review:
Limited physical activity (PA) and obesity are two primary risk factors for cardiovascular disease (CVD). Within a socio-ecological framework, neighborhood social environment may play a key role in influencing PA and obesity. However, the mechanisms underlying this relationship remain ambiguous. Our goals in this review are: (1) to summarize findings from the recent studies on neighborhood social environment in relation to PA and obesity as CVD risk factors, and (2) to briefly describe several innovative approaches to assessing neighborhood social environment.
Recent findings:
Almost all recent studies assessed neighborhood social environment around residential areas. There were consistent associations between neighborhood social environment and PA and obesity, with some exceptions (indicating null associations or paradoxical associations). However, a focus on residential social environment may limit results because these studies did not account for any exposures occurring away from individuals’ homes. Additionally, the majority of studies utilized a cross-sectional design, which limits our ability to make inferences regarding the causality of the association between social environment and PA or obesity as CV risk factors.
Summary:
The majority of the studies on neighborhood social environment characterized factors around residential areas and assessed participant activity via self-reported surveys. Future research should leverage tools to account for the spatial mismatch between environmental exposures and outcomes by using global positioning systems, ecological momentary assessments, virtual neighborhood audits, and simulation modeling. These approaches can overcome major limitations by tracking individuals’ daily activity and real-time perceptions of neighborhood social environments linked to CVD events.
Keywords: Physical activity, obesity, social environment, health disparities, neighborhood socioeconomic position, cardiovascular disease risk
Introduction
Insufficient levels of physical activity (PA) and widespread obesity are two important drivers behind the persistently high levels of cardiovascular disease (CVD) in the U.S. population [1, 2]. In 2015-2016, nearly 40% of U.S. adults suffered from obesity (i.e., body mass index [BMI] ≥ 30.0 kg/m2 [weight (kg)/height (m2)]. Non-Hispanic black and Hispanic populations were disproportionately more likely to be obese as compared to other racial/ethnic groups (Non-Hispanic black - 46.8%, Hispanic - 47.0%, Non-Hispanic Asian - 12.7%, Non-Hispanic white - 37.9%) [3]. Individuals with obesity had high rates of physical inactivity [4], a known risk factor for obesity [5], which is also independently associated with CVD [6]. Insufficient PA remains a widespread problem among U.S. populations, including among those with a normal weight, as demonstrated by one study using accelerometer-measured data from the 2005-2006 National Health and Nutrition Examination Survey (NHANES) [7]. This study showed that less than 10% of American adults were achieving the recommended 150 minutes/week of at least moderate PA [7].
In an effort to encourage increased PA participation, the National Physical Activity Plan [8] and Community Preventive Services Task Force [9] have each endorsed a variety of national- and community-level efforts to increase the accessibility of safe environments conducive to PA. To facilitate significant increases in PA participation, however, it is first essential to understand the multitude of factors that influence PA participation among U.S. adults. An improved understanding of these factors can then inform allocation of limited public health resources and the development of interventions designed to improve cardiovascular health in at-risk communities. For example, the finding that higher levels of neighborhood deprivation are associated with lower PA levels [10] and increased weight gain over time [11•], could serve as the basis for implementing community-level PA interventions which specifically target residents in high-deprivation neighborhoods. To this end, recent research has increasingly conceptualized PA within the context of the socio-ecological framework [12]. The socio-ecological framework is a model that considers each individual’s health behavior to be influenced by a wide variety of interrelated institutional-, environmental-, and community-level factors [13], and therefore emphasizes the use of environmental and public policy approaches to facilitate health behavior change [12].
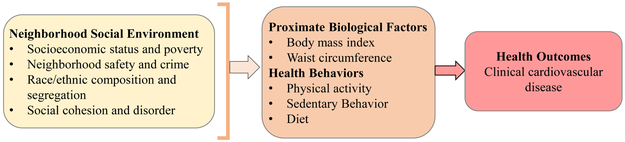
Within this framework, the role of neighborhood social environment as a determinant of PA and obesity has attracted particular attention [14]. Neighborhood social environment refers to the relationships and social processes existing between individuals in a certain neighborhood [15]. It encompasses a wide variety of community-level features which have been shown to influence PA and obesity, such as neighborhood socioeconomic status (SES) [16], racial/ethnic segregation [17, 18], neighborhood crime and safety [16, 19], social cohesion (i.e. trust among neighbors) [20], and social disorder (i.e. vandalism within a community) [14]. Selected summary definitions for these neighborhood social environment factors are provided in Table 1 and the conceptual model connecting these factors to CVD risk is presented in Figure 1.
Table 1.
Summary of neighborhood social environment domains, domain definitions, representative variables, and example studies demonstrating associations with PA and obesity
| Neighborhood Social Environment Domain |
Domain Definition | Representative Variable |
Example Studies (year) |
|---|---|---|---|
| Association with PA | |||
| Socioeconomic status | Based on U.S. Census tract or block group level data, including median home value and median household income | Neighborhood SES | James et al. (2015) [28] |
| Poverty | Based on U.S. Census poverty line | Neighborhood poverty | James et al. (2015) [28]; Derose et al. (2018) [34] |
| Poverty-Income Ratio adjusted for household size, neighborhood areas, and eligibility for government assistance | Poverty-income ratio | Kakinami et al. (2018) [33•] | |
| Segregation | Racial segregation, defined as neighborhoods that were predominantly composed of African Americans, based on percent of non-Hispanic African American residents living in a census tract | Segregation | Armstrong-Brown et al. (2015) [39•] |
| Race and ethnic composition | Simpson Index, defined as the probability that two randomly selected people from the Census tract would be of different races/ethnicities | Neighborhood racial/ethnic diversity | Derose et al. (2015) [41] |
| Perceived safety | Perceived safety measure; for example, using the following survey items: 1) “feeling safe walking in their neighborhood day or night,” and 2) “violence being a problem in their neighborhood,” with respondents responding with a number from 1 (lowest safety) to 5 (highest safety) | Perceived safety | Kerr et al. (2015) [50•]; Perez et al. (2017) [49]; Tamayo et al. (2016) [48] |
| Perceived crime | Perceived crime measure based on resident reports of violent crime within the neighborhood during the previous six months. Respondents were asked how often there had been "a fight which a weapon was used, gang fights, sexual assault or rape, and a robbery/ mugging in their neighborhood". Response options include: agreed, strongly agreed, neither agreed nor disagreed, disagreed, or strongly disagreed. | Tamayo et al. (2016) [48] | |
| Neighborhood crime | Neighborhood crime rates based on objective data from law enforcement agencies | Police-reported crime | Richardson et al. (2017) [57] |
| Social cohesion | Subjective ratings of social cohesion based on feelings of close-knit community among neighbors, taking care of homes and neighbors' children, and getting along with neighbors | Neighborhood social cohesion | Andersen et al. (2015) [59•]; Yuma-Guerrero et al. (2017) [61]; Mooney et al. (2017) [60] |
| Social disorder | Neighborhood disorder was based on visual street audit, which quantified levels of litter, graffiti, abandoned buildings; Kriging (Gaussian process regression) was then employed to create a disorder measure in ArcGIS | Neighborhood disorder | Mooney et al. (2017) [60] |
| Association with obesity | |||
| Socioeconomic status | A composite measure, using factor analysis, based on population size, % of households receiving government assistance, % of households headed by females with children, % of residents with high school degrees, levels of employment, and levels of poverty | Concentrated disadvantage | Kimbro et al. (2017) [26] |
| Neighborhood deprivation index (NDI; higher NDI = greater deprivation) | Neighborhood deprivation index | Powell-Wiley et al. (2014) [11•]; | |
| Multiple versions employed - one used 21 Census level measures on education, income, poverty, racial and ethnic composition, employment status, housing conditions, residential stability analyzed by principal components analysis | Stoddard (2013) [35] | ||
| Another used 8 Census-level variables including percentages of men in neighborhood working in business, living in house with many people, poverty, education, and unemployment | |||
| Poverty | Percent of population in poverty or below the poverty line, based on U.S. Census data | Neighborhood poverty | Do and Zheng (2017) [27]; Kwarteng et al. (2016) [29]; Kwarteng et al. (2017) [30]; Sheehan et al. (2017) [31]; Lippert et al. (2017) [32] |
| Segregation | Black Isolation Index- a metric evaluating the degree to which blacks inhabit the same spaces as other blacks by accounting for the number of black residents in proportion to the total population; Index ranges from 0 to 1, where 0 means that blacks are completely integrated and 1 means that blacks are completely isolated from whites | Black Isolation Index | Bower et al. (2015) [44•] |
| Racial segregation - neighborhoods were defined as "racially segregated" if they were predominantly composed of African Americans (i.e. a census tract contained > 50% African Americans) | Neighborhood segregation | Cozier et al. (2014) [40]; Lim and Harris (2015) [43] | |
| Neighborhood safety | Based on one item, "how often participants felt safe in their neighborhood" Response options include: all, most, some, or none of the time | Neighborhood safety | Wong et al. (2018) [52]; Tamayo et al. (2016) [48] |
| Neighborhood crime | Neighborhood crime rate, based on crime data from law enforcement agencies. Crime types were categorized as assault/battery, criminal offenses (robbery, sexual assault, weapons), incivilities (drugs, prostitution, vandalism), and homicides | Police-reported crime | Powell-Wiley et al. (2017) [53•]; Jones et al. (2015) [54]; Richardson et al. (2017) [56]; Mathis et al. (2017) [58]; Tung et al. (2018) [55] |
| Perceived crime | Perceived crime measure based on levels of violent crime in the neighborhood during the past six months Respondents were asked how often there had been "a fight in which a weapon was used, a gang fight, a sexual assault or rape, and/or a robbery/mugging" in their neighborhood | Tamayo et al. (2016) [48] | |
| Social cohesion | Social cohesion, based on three questions regarding willingness to help among neighbors, trustworthiness, and willingness to take care of children in the neighborhood | Social cohesion | Wong et al. (2018) [52•]; Yu (2017)[63] |
| Social disorder | Counts of physical disorder using 311 complaint reports, regarding graffiti, abandoned vehicles, and abandoned buildings, in a census block group where respondents reside. Each type of physical disorder was quantified as counts of each disorder per 100 persons in the block group | Physical disorder | Mayne et al. (2015) [62] |
Figure 1.
Hypothesized conceptual model of associations between neighborhood social environment factors, physical activity and obesity, and cardiovascular disease
Literature reviews exploring neighborhood determinants of CVD risk factors, such as PA and obesity, have thus far focused primarily on the role of the built environment (i.e. human-made physical characteristics including street connectivity, proximity to parks, land use, and playground access) [21-25]. Despite growing recognition that neighborhood social environment also exerts significant influence on cardiovascular health outcomes, prior reviews have not comprehensively evaluated its relationship to CVD risk factors, including PA and obesity [14, 16-19]. Therefore, the goal of this review is to summarize the findings from recent studies examining associations between the neighborhood social environment and PA and obesity (Figure 1; Table 1), followed by recommendations for future research (Table 2). This is not a systematic review, and thus does not purport to provide an exhaustive summary of all available literature pertaining to this topic.
Table 2.
Summary of neighborhood environment domains, domain definitions, representative variables, and example studies for emerging methods for measuring neighborhood social environment
| Neighborhood Environment Domain |
Definition | Variable | Studies (year) |
|---|---|---|---|
| Neighborhood social environment | Perceived residential neighborhood environment around participants' homes (i.e., home-centric, static) Measures were based on survey questions |
Perceived residential exposures | Brownson et al. (2009) [78]; Yang et al. (2011) [83]; Powell-Wiley et al. (2017) [84••] |
| Objective neighborhood environment around participants' homes (i.e., home-centric, static); measures were created using GIS technology | Objective residential exposures | Powell-Wiley et al. (2017) [84••] | |
| Activity Space | GPS-defined activity space, based on participants' daily movements during the study period, as documented by a GPS unit Measures were trips, monitoring points, and daily movements, with respect to environmental exposures |
GPS-defined activity space for specific environment exposures | Tamura et al. (2018) [69••]; Tamura et al. (2018) [71]; Chaix et al. (2016) [70••]; Zenk et al. (2011) [72] |
| Real-time perceived social environment | Real-time perceived environment was often measured through ecological momentary assessment (EMA) Measures were generally created based on survey items administered throughout the study period, about 1-7 times throughout the day | Real-time momentary variables on PA and diet | Dunton et al. (2016) [74]; Dunton et al. (2014) [75]; Zenk et al. (2017) [76]; |
| Neighborhood Audit | Objective neighborhood audits using Google Street View to assess neighborhood features, including quality and condition of streets, sidewalks, graffiti on walls and buildings, abandoned buildings and cars, and access to transportation | Objective neighborhood features | Adu-Brimpong et al. (2017) [81]; Ben-Joseph et al. (2013) [80]; Kelly et al. (2013) [79]; Mayne et al. (2018) [62] |
The Role of Neighborhood Social Environment Factors in PA and Obesity
Socioeconomic position and poverty
Socioeconomic position (SEP) or socioeconomic status (SES) and poverty are important neighborhood environmental exposures which are known to impact CVD risk factors, including PA levels and obesity. SES has been expressed using various metrics; some researchers have defined it as concentrated socio-economic disadvantage (based on population size, households with public assistance, household with children headed by females, poverty rate, education attainment, unemployment rate) [26] whereas others have looked only at poverty, which is defined as an income beneath the U.S. federal poverty line [27-32], and poverty-to-income ratio [33•].
Some recent studies examined neighborhood poverty by evaluating neighborhoods located in low-income areas in Los Angeles, California [34, 33•]. For instance, a study by Derose and colleagues demonstrated that women who reside in high-poverty neighborhoods utilize parks less than men (−0.28 times/week; p<0.001) [34]. Kakinami and colleagues found that individuals living in households with the lowest poverty-income ratios engaged in 17-30 fewer minutes of moderate of and 20-25 fewer minutes of vigorous leisure time PA (LTPA) per week [33•].
Several recent studies used neighborhood deprivation indices, a set of measures for neighborhood SES which incorporate numerous neighborhood features based on U.S. Census data; one such deprivation index was developed by Diez Roux and colleagues [10]. These studies demonstrated relationships between neighborhood SES and CVD risk [35, 11•]. For example, one recent longitudinal study by Powell-Wiley and colleagues used data from the Dallas Heart Study to assess a neighborhood deprivation index (NDI; created based on U.S. Census variables from six domains [education, income/poverty, occupation, racial composition, housing conditions, and residential stability] using principal component analysis to select six major census block group-level variables, such as %unemployment, % the population below the federal poverty line, etc.), where a greater NDI value was associated with lower neighborhood SES [11•]. The authors examined the relationship between NDI and weight change over seven years and demonstrated that respondents living in the highest NDI tertile gained significantly 6.0 kilograms more weight over time than those living in the lowest NDI tertile [11•]. While these individual-level changes may appear relatively small, they can be significant on the population level.
While some studies were longitudinal in nature [35, 11•], the majority relied on a cross-sectional design and thus acknowledged that their study designs precluded them from inferring causality from the results. Another shortcoming of these studies is that NDI is a limited measure which does not account for important factors outside of U.S. Census-based measures that may affect individuals’ weight status, such as the food environment (i.e. the higher density of supermarkets in predominantly white neighborhoods vs. black neighborhoods) [27]. Further work on neighborhood deprivation should consider utilizing analyses that include measures of neighborhood segregation [27]. An additional limitation of these studies is their failure to control for self-selection of neighborhood environment, which can bias results (i.e. result in inaccurate estimation of the true associations between neighborhood SES and CVD outcomes) [28]. For example, there may be certain instances in which populations of higher-income individuals will choose to inhabit lower-income neighborhoods. These individuals may selectively position themselves in proximity to parks and green space, have increased access to PA resources, and have a greater propensity to engage in PA compared to other residents of the neighborhood. This can skew the relationship between neighborhood-level SES and PA levels [28]. One approach to account for self-selection of neighborhoods is to use Heckman’s Correction Factor (HCF), a technique which originated in the field of econometrics and is used to correct for selection bias based on non-randomly selected samples (e.g., HCF can account for factors that may determine individuals’ self-selection into a specific socioeconomic-level neighborhood, including race, home ownership, marital status, family size, or employment status) [36]. Lastly, many of the existing studies used differing measures to assess socioeconomic inequality, neighborhood poverty, and neighborhood deprivation. For example, we encountered many different variants of the NDI, each of which was composed of a different combination of neighborhood factors. The use of many disparate measures in this area of research makes it challenging to compare the findings of different studies. Recent work recommends use of the NDI developed by Diez Roux et al for uniformity in measuring neighborhood SES across obesity-related studies [37].
Racial and ethnic composition or segregation
Racial and ethnic composition and neighborhood segregation are thought to influence CVD risk [38]. Most studies related to this topic focus on the racial and ethnic composition of neighborhoods (with census tract or block group serving as a proxy for residential neighborhood) [39•-43]. Inconsistent with what researchers typically hypothesize, one study found that African Americans residing in highly segregated neighborhoods (compared to areas with predominantly European Americans) had a 21% greater odds of meeting PA guidelines (i.e., 150 minutes of moderate-to-vigorous PA/week; p<0.01) [39•]. Another study by Derose and colleagues found that the neighborhood racial-ethnic diversity (accounting for neighborhood mixture of racial and ethnicity at census tract level) was not related to PA [41].
A few studies sought instead to measure neighborhood segregation, and thus employed other metrics, such as a black isolation index [44•], spatial analysis of racial clustering [45] or measures of racial-ethnic heterogeneity [46]. One study by Bower and colleagues used the black isolation index, which measures the degree to which black individuals reside in the same areas as other black individuals, adjusting for the percentage of blacks in the overall population. The index ranges from 0 (completely uniform mixing of white and black individuals) to 10 (complete isolation of black individuals) [44•]. The authors found that a one-point increase in the index was associated with a 6% greater likelihood of obesity among black women (p<0.05) [44•].
A recent longitudinal study by Pool and colleagues assessed neighborhood segregation via the Getis-Ord Gi*, a measure of spatial clustering which can show the racial composition of census tracts and how a given tract differs from its surrounding areas [45]. The authors demonstrated that black women residing in highly-segregated neighborhoods were 30% more likely to develop obesity during the follow-up period than black women living in low-segregation neighborhoods (hazard ratio=1.3, 95 % confidence interval=1.0-1.7) [45]. Another study by Xu and Wang derived each area’s racial/ethnic heterogeneity (based on six different definitions of race and ethnicity) by , where Pi is the fraction of the total population in a certain county [46]. This heterogeneity index ranges from 0 (homogenous, with only one racial or ethnic group living in a county) to 1 (complete heterogeneity) [46]. The authors found that counties with high levels of racial/ethnic heterogeneity (approaching 1) had 11% lower odds of obesity (p<0.05), controlling for socio-demographic variables (e.g., age, income) and county-level variables (e.g., street connectivity) [46].
These studies have a number of important limitations. Given that the majority of them are cross-sectional, more longitudinal studies are needed to explore the effects of exposure to neighborhood segregation over time. In addition, outcome measures such as PA levels and BMI were based mostly on self-report, which could impact the strength or directionality of these results via social desirability bias [47]. Furthermore, most of this research focused on segregation between black, Hispanic, and white populations. More research is needed to better understand the impact of residential segregation on additional racial/ethnic groups, such as Asian populations and diverse Latinx populations of different national origins.
Neighborhood crime and safety
Levels of crime within a neighborhood represent an important environmental determinant of PA, obesity, and CV health. Existing work exploring relationships between neighborhood safety and crime and CV risk factors can be broadly divided into two categories: (1) research that assessed subjective perceptions of neighborhood safety and crime levels based on survey data, and (2) research that objectively assessed neighborhood crime using geographic information systems (GIS) technology in conjunction with data obtained from law enforcement agencies.
A number of recent studies explored the relationship between self-reported perceptions of neighborhood safety and crime and PA [48-50•]. For example, a recent longitudinal study assessed perceived neighborhood safety via survey items and the authors found no relationships between perceptions of neighborhood safety and the frequency with which individuals engaged in walking for both transportation and recreational purposes over time [50•]. While other studies broadly assessed perceptions of neighborhood safety, some studies focused specifically on determining the level of perceived neighborhood crime [48, 51]. For instance, one study found no significant association between neighborhood safety concerns or violent crime with PA [48].
Recent studies also explored the relationship between self-reported perceptions of neighborhood safety and obesity [52•] or adiposity [48, 53•]. For example, a recent longitudinal study assessed both individual- and neighborhood-level safety in relation to change in adiposity over time [53•]. For the purposes of this study, neighborhood-level safety was described using summary measures that aggregated the perceptions of multiple neighborhood residents [53•]. The authors demonstrated that individual-level safety was positively related to BMI at baseline (mean difference per standard deviation=0.57, p<0.05). In contrast, increases in both individual- and neighborhood-level safety were associated with decreases in BMI over a 10-year follow-up, with BMI decreasing 0.11 kg/m2 with increasing individual-level safety and 0.16 kg/m2 with increasing neighborhood-level safety (p<0.05) [53•]. Interestingly, change in BMI among women appeared to be more impacted by individual-level safety changes, while BMI change among men were more related to neighborhood-level safety change, suggesting sex-specific effects of neighborhood social environment.
Several studies assessed the relationship between neighborhood crime and obesity using objective crime data, which were drawn from a number of different sources including state and local law enforcement agencies [54-56, 53•, 57] and the Federal Bureau of Investigation (FBI) [58]. For instance, one longitudinal study examined associations between crime rate and obesity among young adults over time [54]. The authors used data from the FBI’s Uniform Crime Reports to assess the crime rate per 100,000 residents occurring within each individual’s county of residence. They demonstrated that a one-unit increase (i.e. 100,000 crime reports/county) was related to 6% greater odds of developing obesity over time in the sample of adults (p<0.05) [54]. Another recent longitudinal study used data from the Chicago Police Department to determine levels of crime within one mile of each participant’s address. Ultimately, this study did not find any association between police-reported crime and adiposity among adults in Chicago [53•].
Studies focused on subjective measures of safety and crime and those that have used objective crime data to examine the relationship between PA and obesity have yet to account for two important dimensions of the relationship between crime, safety, and CVD risk. First, they have not explored real-time perceptions of safety. Assessing perceptions of neighborhood safety in real time could be helpful in mitigating recall bias and providing more precise data regarding perceptions of safety. Second, these studies failed to account for other locations outside of residential neighborhoods in which participants may spend substantial portions of their time. In addition, more longitudinal studies are needed to better elucidate the complex link between neighborhood safety, crime and CVD risk factors like PA and obesity.
Social cohesion and disorder
There has recently been increased attention focused on social cohesion and disorder in relation to PA and obesity [14]. Both social cohesion (defined as trust among neighbors and willingness to help one another within the community) and disorder (defined as incivilities in a community such as graffiti, vacant lots, litter, etc.) remain understudied with respect to their relationship with CVD risk. However, both have been demonstrated to associate with PA [59•-61] and weight status [62, 63, 52•].
Several recent studies have examined associations between social cohesion and both PA and obesity [52•, 63, 59-61]. Higher levels of social cohesion were associated with increased leisure-time PA in low SES neighborhoods [64]. Yuma-Guerrero and colleagues demonstrated that social cohesion mediated the association between neighborhood SES (β=−0.18 between SES and social cohesion, p<0.05) and PA (β=0.10 between social cohesion and PA; p<0.05), in a fully-adjusted model, including age, race/ethnicity, marital status, number of children in the home, depression, and obesity [61]. Additional studies employed survey items to measure social cohesion via assessment of whether individuals felt that their neighborhood was close-knit or whether community members shared the same values. These studies had mixed results, with one demonstrating that individuals in neighborhoods with higher levels of social cohesion had lower BMIs (β=−0.17 [95% C.I. =−0.22, −0.12] for Whites; β=−0.10 [95% C.I.=−0.20, −0.00] for Hispanics) [52•] and another showing no association [63].
Social disorder and neighborhood physical disorder are also thought to influence CVD risk factors. Recent work has generally used survey items to assess disorder in neighborhoods (e.g. via questions regarding items on conditions of homes, streets, litter, and graffiti, etc.). For example, a recent longitudinal study found a negative relationship between neighborhood disorder and scores on the Physical Activity Scale for the Elderly (PASE, mean difference=−2.0 units in PASE score [95% C.I.=−3.6, −0.3]) at baseline, but no association between disorder and PASE score after 2 years of follow up [60]. In contrast, a cross-sectional study examining the association between physical disorder (based on 311 complaint reports) and BMI indicated no association between them [62].
One limitation of recent work exploring social cohesion and disorder is that many of the survey items used to measure cohesion and disorder may not be specific enough to be correlated to PA outcomes. In addition, many of these studies only assessed single cities, which reduced the generalizability of the study findings to different areas of the U.S. [62, 60]. In future studies, researchers should attempt to develop more validated survey instruments to measure cohesion and disorder and should perform research across multiple U.S. cities to further clarify the role of social cohesion and disorder in CVD risk.
Future Directions
Spatially dynamic definition of neighborhood environment
Much of the current neighborhood social environment research has focused specifically on the locations of individuals’ homes, examining the relationship between home location and self-reported PA and adiposity. The standard procedure has been to obtain each individual’s home address and geocode the address (i.e., plot the address on a map using GIS technology). While this is useful for approximating the geographic area in which an individual may be more likely to spend time, a potential weakness of this method is the fact that people frequently visit many different locations, and often follow different patterns of movement based on the time of day and day of the week. A definition of neighborhood which relies upon home address alone fails to account for spatial mismatch between the exposure and the outcome and is a key limitation of neighborhood research that has been recognized by a growing body of literature [65, 66]. Thus, measures of social environment factors in relation to PA and obesity should consider accounting for the fact that individuals’ daily movements are spatially dynamic, rather than static (home-centric) [67].
To overcome this, recent studies have sought to employ dynamic measures of neighborhood environment. For example, previous work has used GPS technology to assign each study participant a GPS-defined activity space composed of all the areas he or she visited over a defined time period [68]. Two recent studies using GPS coordinates linked to accelerometer data tracked PA that occurred in a wide variety of spaces not restricted to residential areas [69••, 70••]. Two additional studies quantified the density of fast-food restaurants via GPS-defined food environments (i.e., quantifying food environment based upon an individual’s movements in space) [71, 72]. More work is needed to develop the social environment measures around GPS-defined activity space. Both home-centric and spatially dynamic approaches to defining neighborhood environment are valuable and provide useful insights. Further research is also needed to compare influences of social environment factors between residential and GPS activity space environments to better understand how each is associated with PA and obesity.
Neighborhood social environment through ecological momentary assessment
To complement the objectively-measured data obtained through GPS units and GIS technology, there is significant benefit to incorporating subjective self-reported data. These data can be obtained through mobile devices, such as smartphone applications [73]. Ecological momentary assessment (EMA) has become increasingly popular and has been applied in behavioral studies related to PA [74-76]. This allows researchers to repeatedly measure psychosocial factors (e.g. mood, emotion), behaviors (e.g. PA), and perceived neighborhood environmental contexts (e.g. poverty, safety, crime, social disorder) in real time.
EMA is particularly useful in addressing recall bias related to the retrospective nature of survey-based assessments [77]. Measures of social environment factors, like perceived safety or social disorder, can be time-stamped, which permits researchers to link them temporally to objectively assessed data through GPS and accelerometer data measuring PA. Such an approach has been employed previously to measure within-person variability in mood and PA [76], and relationships between neighborhood social characteristics, PA and sedentary behavior [76].
Detailed measures of neighborhood social environment through audit tools
To assess objectively neighborhood social environment, systematic observational methods (i.e., audits) can be used in neighborhood research [78]. Assessing neighborhood social environment through audit tools (i.e., evaluating the quality and presence/absence of specific environmental features at a certain street segment such as presence and condition of sidewalks, litters, graffiti on a wall) [78] requires trained observers and can be time-consuming. Despite this, researchers have still employed this technique to comprehensively evaluate neighborhood quality [79-81, 62]. Recently, some studies have begun to conduct such audits digitally using tools such as Google Street View. Mayne and colleagues used Google Street View audits to assign physical disorder scores to census blocks in four Chicago neighborhoods and subsequently examined associations of physical disorder scores with PA, BMI, and obesity [62]. They found that neighborhood physical disorder was positively associated with obesity (odds ratio=1.43 [95% C.I.=1.01, 2.02]) [62]. Adu-Brimpong et al. used Google Street View to audit measures of physical disorder in Washington, D.C. using the Active Neighborhood Checklist [81]. The authors audited five major neighborhood features: 1) land use, 2) access to public transportation, 3) street characteristics, 4) neighborhood quality, and 5) sidewalk quality and walking and biking locations. They found a strong correlation between their scores based on neighborhood features and a validated neighborhood walkability measure called the Walk Score. Web-based audit tools, like Google Street View, may not fully substitute for direct observation through on-site audit. However, they offer an efficient and cost-effective alternative to direct observation audits for quantifying neighborhood social environment characteristics.
Simulation modeling in evaluating relationships between neighborhood social environment and PA and obesity
Variability in PA and obesity due to neighborhood social environment exposure is expected to be dynamic, meaning that individuals and their environments are inter-related and are part of a complex system. However, a key limitation of traditional statistical modeling approaches is that these models are unable to account for feedback loops in the inter-relationships of individuals with their neighborhood social environment [82]. Only a few studies have applied agent-based models (ABMs), a type of simulation modeling, to assess the dynamic interactions between neighborhood social environment and CVD risk factors such as PA [83-85] and obesity [84••].
For example, Yang and colleagues developed a spatial ABM to simulate individuals’ walking behavior within a neighborhood [83]. Each individual in the model was assigned a set of characteristics, such as age, walking capability, SES, attitude toward walking, and residential location [83]. The authors demonstrated that each individual’s attitude toward walking over time was determined by his/her social network [83]. Powell-Wiley et al. developed an ABM to simulate the impact of crime on LTPA and obesity among African American women in Washington, D. C. neighborhoods [84••]. The modeling demonstrated that crime reductions resulting in greater access to LTPA facilities could lead more African American women to participate in LTPA, which would reduce obesity prevalence [84••]. These innovative modeling approaches can account for the dynamic nature of neighborhood characteristics, could offer new insights into the effects of adverse neighborhood social environment on PA or obesity, and potentially aid in developing improved intervention targets for CVD risk reduction.
Conclusions
Neighborhood social environment has increasingly been recognized as an important determinant of CVD risk. The reviewed studies covered a wide range of neighborhood social environment factors, including SES and poverty, racial and ethnic composition and segregation, neighborhood crime and safety, and social cohesion and disorder. Work across these four domains demonstrated that neighborhood social environment was linked to PA and obesity. The majority of these studies relied on neighborhood social environment exposures around participants’ residences, so future work should strive to account for exposures away from individuals’ homes. Additionally, future studies should consider employing EMA to quantify participants’ real-time perceptions of their experiences within the social environment and neighborhood auditing via Google Street View to facilitate objective assessment of neighborhood exposures. Furthermore, the use of newer approaches (GPS, accelerometers, EMA, audits, and simulation modeling) to complement existing objective or survey-based measures of neighborhood social environment may provide a more robust understanding of the complex and dynamic linkages between neighborhood social environment and CVD risk in the U.S.
Acknowledgement
The views of the present review study are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute (NHLBI), the National Institute on Minority Health and Health Disparities, the National Institutes of Health (NIH), or the U.S. Department of Health and Human Services. Funding for the Social Determinants of Obesity and Cardiovascular Risk Laboratory is provided through the Division of Intramural Research (DIR) of the NHLBI of the NIH, and through the Intramural Research Program of the National Institute on Minority Health and Health Disparities of the NIH.
This research was made possible through the NIH Medical Research Scholars Program, a public-private partnership supported jointly by the NIH and generous contributions to the Foundation for the NIH from the Doris Duke Charitable Foundation, Genentech, the American Association for Dental Research, the Colgate-Palmolive Company, Elsevier, alumni of student research programs, and other individual supporters via contributions to the Foundation for the National Institutes of Health.
Abbreviations:
- ABM
agent-based mode
- BMI
body mass index
- CVD
cardiovascular disease
- EMA
ecological momentary assessment
- FBI
Federal Bureau of Investigation
- GIS
geographic information system
- GPS
global positioning system
- LTPA
leisure-time physical activity
- MVPA
moderate-to-vigorous physical activity
- NDI
neighborhood deprivation index
- NHANES
National Health and Nutrition Examination Survey
- PA
physical activity
- SEP
socio-economic position
- SES
socio-economic status
Footnotes
Conflict of Interest
All the authors (Tamura, Langerman, Ceasar, Andrews, Agrawal, Powell-Wiley) declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Contributor Information
Kosuke Tamura, Social Determinants of Obesity and Cardiovascular Risk Laboratory, Cardiovascular Branch, Division of Intramural Research, National Heart, Lung, and Blood Institute, National Institutes of Health, Bldg 10-CRC, 5-5330, 10 Center Drive, Bethesda, MD 20892, USA.
Steven D. Langerman, Social Determinants of Obesity and Cardiovascular Risk Laboratory, Cardiovascular Branch, Division of Intramural Research, National Heart, Lung, and Blood Institute, National Institutes of Health, Bldg 10-CRC, 5-5330, 10 Center Drive, Bethesda, MD 20892, USA.
Joniqua N. Ceasar, Social Determinants of Obesity and Cardiovascular Risk Laboratory, Cardiovascular Branch, Division of Intramural Research, National Heart, Lung, and Blood Institute, National Institutes of Health, Bldg 10-CRC, 5-5330, 10 Center Drive, Bethesda, MD 20892, USA.
Marcus R. Andrews, Social Determinants of Obesity and Cardiovascular Risk Laboratory, Cardiovascular Branch, Division of Intramural Research, National Heart, Lung, and Blood Institute, National Institutes of Health, Bldg 10-CRC, 5-5330, 10 Center Drive, Bethesda, MD 20892, USA.
Malhaar Agrawal, Social Determinants of Obesity and Cardiovascular Risk Laboratory, Cardiovascular Branch, Division of Intramural Research, National Heart, Lung, and Blood Institute, National Institutes of Health, Bldg 10-CRC, 5-5330, 10 Center Drive, Bethesda, MD 20892, USA.
Tiffany M. Powell-Wiley, Social Determinants of Obesity and Cardiovascular Risk Laboratory, Cardiovascular Branch, Division of Intramural Research, National Heart, Lung, and Blood Institute, National Institutes of Health, Bldg 10-CRC, 5-5330, 10 Center Drive, Bethesda, MD 20892, USA; and Intramural Research Program, National Institute on Minority Health and Health Disparities, National Institutes of Health, Bethesda, MD 20892.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance•• Of major importance
- 1.Sidney S, Quesenberry CP Jr., Jaffe MG, Sorel M, Nguyen-Huynh MN, Kushi LH et al. Recent Trends in Cardiovascular Mortality in the United States and Public Health Goals. JAMA Cardiol. 2016;1(5):594–9. doi: 10.1001/jamacardio.2016.1326. [DOI] [PubMed] [Google Scholar]
- 2.Mensah GA, Wei GS, Sorlie PD, Fine LJ, Rosenberg Y, Kaufmann PG et al. Decline in Cardiovascular Mortality: Possible Causes and Implications. Circ Res. 2017;120(2):366–80. doi: 10.1161/CIRCRESAHA.116.309115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of Obesity Among Adults and Youth: United States, 2015-2016. NCHS Data Brief. 2017(288):1–8. [PubMed] [Google Scholar]
- 4.An R, Xiang X, Yang Y, Yan H. Mapping the Prevalence of Physical Inactivity in U.S. States, 1984-2015. PLoS One. 2016;11(12):e0168175. doi: 10.1371/journal.pone.0168175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pietilainen KH, Kaprio J, Borg P, Plasqui G, Yki-Jarvinen H, Kujala UM et al. Physical inactivity and obesity: a vicious circle. Obesity (Silver Spring). 2008;16(2):409–14. doi: 10.1038/oby.2007.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spencer RM, Heidecker B, Ganz P. Behavioral Cardiovascular Risk Factors- Effect of Physical Activity and Cardiorespiratory Fitness on Cardiovascular Outcomes. Circ J. 2016;80(1):34–43. doi: 10.1253/circj.CJ-15-1159. [DOI] [PubMed] [Google Scholar]
- 7.Tucker JM, Welk GJ, Beyler NK. Physical activity in U.S.: adults compliance with the Physical Activity Guidelines for Americans. Am J Prev Med. 2011;40(4):454–61. doi: 10.1016/j.amepre.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 8.Kraus WE, Bittner V, Appel L, Blair SN, Church T, Despres JP et al. The National Physical Activity Plan: a call to action from the American Heart Association: a science advisory from the American Heart Association. Circulation. 2015;131(21):1932–40. doi: 10.1161/CIR.0000000000000203. [DOI] [PubMed] [Google Scholar]
- 9.Community Preventive Services Task Force. Physical Activity: Built Environment Approaches Combining Transportation System Interventions with Land Use and Environmental Design. CDC; 2016. https://www.thecommunityguide.org/ Accessed 6/20 2018. [Google Scholar]
- 10.Boone-Heinonen J, Roux AVD, Kiefe CI, Lewis CE, Guilkey DK, Gordon-Larsen P. Neighborhood socioeconomic status predictors of physical activity through young to middle adulthood: The CARDIA study. Social Science & Medicine. 2011;72(5):641–9. doi: 10.1016/j.socscimed.2010.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. •.Powell-Wiley TM, Ayers C, Agyemang P, Leonard T, Berrigan D, Ballard-Barbash R et al. Neighborhood-level socioeconomic deprivation predicts weight gain in a multi-ethnic population: longitudinal data from the Dallas Heart Study. Prev Med. 2014;66:22–7. doi: 10.1016/j.ypmed.2014.05.011.This study demonstrated that individuals residing in the highest-deprivation neighborhoods gained 6.0 kg compared to those living in the lowest ones, suggesting that individuals living in deprived neighborhoods for a longer period of time experienced an increase in their weight.
- 12.Sallis JF, Cervero RB, Ascher W, Henderson KA, Kraft MK, Kerr J. An ecological approach to creating active living communities. Annu Rev Public Health. 2006;27:297–322. doi: 10.1146/annurev.publhealth.27.021405.102100. [DOI] [PubMed] [Google Scholar]
- 13.Sallis J, Owen N. Ecological models of health behavior In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: theory, research, and practice. 5 ed.: Jossey-Bass; 2015. [Google Scholar]
- 14.Diez Roux AV, Mujahid MS, Hirsch JA, Moore K, Moore LV. The Impact of Neighborhoods on CV Risk. Glob Heart. 2016;11(3):353–63. doi: 10.1016/j.gheart.2016.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carroll-Scott A, Gilstad-Hayden K, Rosenthal L, Peters SM, McCaslin C, Joyce R et al. Disentangling neighborhood contextual associations with child body mass index, diet, and physical activity: the role of built, socioeconomic, and social environments. Soc Sci Med. 2013;95:106–14. doi: 10.1016/j.socscimed.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barnett DW, Barnett A, Nathan A, Van Cauwenberg J, Cerin E, Council on E et al. Built environmental correlates of older adults' total physical activity and walking: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2017;14(1):103. doi: 10.1186/s12966-017-0558-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Corral I, Landrine H, Hao Y, Zhao LH, Mellerson JL, Cooper DL. Residential segregation, health behavior and overweight/obesity among a national sample of African American adults. Journal of Health Psychology. 2012;17(3):371–8. doi: 10.1177/1359105311417191. [DOI] [PubMed] [Google Scholar]
- 18.Kershaw KN, Pender AE. Racial/Ethnic Residential Segregation, Obesity, and Diabetes Mellitus. Curr Diab Rep. 2016;16(11):108. doi: 10.1007/s11892-016-0800-0. [DOI] [PubMed] [Google Scholar]
- 19.Won J, Lee C, Forjuoh SN, Ory MG. Neighborhood safety factors associated with older adults’ health-related outcomes: A systematic literature review. Soc Sci Med. 2016;165:177–86. doi: 10.1016/j.socscimed.2016.07.024. [DOI] [PubMed] [Google Scholar]
- 20.Yi SS, Trinh-Shevrin C, Yen IH, Kwon SC. Racial/Ethnic Differences in Associations Between Neighborhood Social Cohesion and Meeting Physical Activity Guidelines, United States, 2013-2014. Preventing Chronic Disease. 2016;13. doi:ARTN E16510.5888/pcd13.160261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Karmeniemi M, Lankila T, Ikaheimo T, Koivumaa-Honkanen H, Korpelainen R. The Built Environment as a Determinant of Physical Activity: A Systematic Review of Longitudinal Studies and Natural Experiments. Annals of Behavioral Medicine. 2018;52(3):239–51. doi: 10.1093/abm/kax043. [DOI] [PubMed] [Google Scholar]
- 22.Smith M, Hosking J, Woodward A, Witten K, MacMillan A, Field A et al. Systematic literature review of built environment effects on physical activity and active transport - an update and new findings on health equity. Int J Behav Nutr Phys Act. 2017;14(1):158. doi: 10.1186/s12966-017-0613-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Masoumi HE. Associations of built environment and children’s physical activity: a narrative review. Rev Environ Health. 2017;32(4):315–31. doi: 10.1515/reveh-2016-0046. [DOI] [PubMed] [Google Scholar]
- 24.Feng J, Glass TA, Curriero FC, Stewart WF, Schwartz BS. The built environment and obesity: a systematic review of the epidemiologic evidence. Health Place. 2010;16(2):175–90. doi:S1353-8292(09)00098-7 [pii] 10.1016/j.healthplace.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 25.Sallis JF, Floyd MF, Rodriguez DA, Saelens BE. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation. 2012;125(5):729–37. doi:125/5/729[pii] 10.1161/CIRCULATIONAHA.110.969022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kimbro RT, Sharp G, Denney JT. Home and away: Area socioeconomic disadvantage and obesity risk. Health & Place. 2017;44:94–102. doi: 10.1016/j.healthplace.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 27.Do DP, Zheng C. A marginal structural modeling strategy investigating short and long-term exposure to neighborhood poverty on BMI among U.S. black and white adults. Health Place. 2017;46:201–9. doi: 10.1016/j.healthplace.2017.05.010. [DOI] [PubMed] [Google Scholar]
- 28.James P, Hart JE, Arcaya MC, Feskanich D, Laden F, Subramanian SV. Neighborhood Self-Selection: The Role of Pre-Move Health Factors on the Built and Socioeconomic Environment. Int J Environ Res Public Health. 2015;12(10):12489–504. doi: 10.3390/ijerph121012489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kwarteng JL, Schulz AJ, Mentz GB, Israel BA, Shanks TR, Perkins DW. Neighbourhood Poverty, Perceived Discrimination and Central Adiposity in the USA: Independent Associations in a Repeated Measures Analysis. J Biosoc Sci. 2016;48(6):709–22. doi: 10.1017/S0021932016000225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kwarteng JL, Schulz AJ, Mentz GB, Israel BA, Perkins DW. Independent Effects of Neighborhood Poverty and Psychosocial Stress on Obesity Over Time. Journal of Urban Health-Bulletin of the New York Academy of Medicine. 2017;94(6):791–802. doi: 10.1007/s11524-017-0193-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sheehan CM, Cantu PA, Powers DA, Margerison-Zilko CE, Cubbin C. Long-term neighborhood poverty trajectories and obesity in a sample of california mothers. Health Place. 2017;46:49–57. doi: 10.1016/j.healthplace.2017.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lippert AM, Evans CR, Razak F, Subramanian SV. Associations of Continuity and Change in Early Neighborhood Poverty With Adult Cardiometabolic Biomarkers in the United States: Results From the National Longitudinal Study of Adolescent to Adult Health, 1995-2008. Am J Epidemiol. 2017;185(9):765–76. doi: 10.1093/aje/kww206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. •.Kakinami L, Wissa R, Khan R, Paradis G, Barnett TA, Gauvin L. The association between income and leisure-time physical activity is moderated by utilitarian lifestyles: A nationally representative US population (NHANES 1999-2014). Preventive Medicine. 2018;113:147–52. doi: 10.1016/j.ypmed.2018.05.013.This study indicated that individuals having the lowest poverty-income ratio had fewer minutes of moderate, vigorous, and moderate-vigorous PA than those with the highest poverty-income ratio. This study also found that individuals w/ the lowest poverty-income ratio were 31-55% less likely to meet national PA recommendations.
- 34.Derose KP, Han B, Williamson S, Cohen DA. Gender Disparities in Park Use and Physical Activity among Residents of High-Poverty Neighborhoods in Los Angeles. Women Health Iss. 2018;28(1):6–13. doi: 10.1016/j.whi.2017.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stoddard PJ, Laraia BA, Warton EM, Moffet HH, Adler NE, Schillinger D et al. Neighborhood Deprivation and Change in BMI Among Adults With Type 2 Diabetes. Diabetes Care. 2013;36(5):1200–8. doi: 10.2337/dc11-1866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Powell-Wiley TM, Cooper-McCann R, Ayers C, Berrigan D, Lian M, McClurkin M et al. Change in Neighborhood Socioeconomic Status and Weight Gain:Dallas Heart Study. Am J Prev Med. 2015;49(1):72–9. doi: 10.1016/j.amepre.2015.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Saelens BE, Arteaga SS, Berrigan D, Ballard RM, Gorin AA, Powell-Wiley TM et al. Accumulating Data to Optimally Predict Obesity Treatment (ADOPT) Core Measures: Environmental Domain. Obesity (Silver Spring). 2018;26 Suppl 2:S35–S44. doi: 10.1002/oby.22159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kershaw KN, Albrecht SS. Racial/ethnic residential segregation and cardiovascular disease risk. Curr Cardiovasc Risk Rep. 2015;9(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. •.Armstrong-Brown J, Eng E, Hammond WP, Zimmer C, Bowling JM. Redefining Racial Residential Segregation and its Association With Physical Activity Among African Americans 50 years and Older: A Mixed Methods Approach. Journal of Aging and Physical Activity. 2015;23(2):237–46. doi: 10.1123/japa.2013-0069.This study demonstrated that racial residential segregation was positively associated with minutes of PA and odds of meeting PA guidelines.
- 40.Cozier YC, Yu J, Coogan PF, Bethea TN, Rosenberg L, Palmer JR. Racism, Segregation, and Risk of Obesity in the Black Womens Health Study. American Journal of Epidemiology. 2014;179(7):875–83. doi: 10.1093/aje/kwu004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Derose KP, Han B, Williamson S, Cohen DA. Racial-Ethnic Variation in Park Use and Physical Activity in the City of Los Angeles. Journal of Urban Health-Bulletin of the New York Academy of Medicine. 2015;92(6):1011–23. doi: 10.1007/s11524-015-9994-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Le-Scherban F, Albrecht SS, Osypuk TL, Sanchez BN, Roux AVD. Neighborhood Ethnic Composition, Spatial Assimilation, and Change in Body Mass Index Over Time Among Hispanic and Chinese Immigrants: Multi-Ethnic Study of Atherosclerosis. American Journal of Public Health. 2014;104(11):2138–46. doi: 10.2105/Ajph.2014.302154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lim S, Harris TG. Neighborhood Contributions to Racial and Ethnic Disparities in Obesity Among New York City Adults. American Journal of Public Health. 2015;105(1):159–65. doi: 10.2105/Ajph.2013.301782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. •.Bower KM, Thorpe RJ, Yenokyan G, McGinty EEE, Dubay L, Gaskin DJ. Racial Residential Segregation and Disparities in Obesity among Women. Journal of Urban Health-Bulletin of the New York Academy of Medicine. 2015;92(5):843–52. doi: 10.1007/s11524-015-9974-z.The authors showed that, within each Metropolitan Statistical Area, living in a neighborhood with a higher Black Isolation Index was associated with higher odds of obesity, especially among Black women.
- 45.Pool LR, Carnethon MR, Goff DC, Gordon-Larsen P, Robinson WR, Kershaw KN. Longitudinal Associations of Neighborhood-level Racial Residential Segregation with Obesity Among Blacks. Epidemiology. 2018;29(2):207–14. doi: 10.1097/Ede.0000000000000792. [DOI] [PubMed] [Google Scholar]
- 46.Xu Y, Wang F. Built environment and obesity by urbanicity in the U.S. Health Place. 2015;34:19–29. doi: 10.1016/j.healthplace.2015.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Adams SA, Matthews CE, Ebbeling CB, Moore CG, Cunningham JE, Fulton J et al. The effect of social desirability and social approval on self-reports of physical activity. Am J Epidemiol. 2005;161(4):389–98. doi: 10.1093/aje/kwi054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tamayo A, Karter AJ, Mujahid MS, Warton EM, Moffet HH, Adler N et al. Associations of perceived neighborhood safety and crime with cardiometabolic risk factors among a population with type 2 diabetes. Health Place. 2016;39:116–21. doi: 10.1016/j.healthplace.2016.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Perez LG, Slymen DJ, Sallis JF, Ayala GX, Elder JP, Arredondo EM. Interactions between individual and perceived environmental factors on Latinas’ physical activity. J Public Health-Uk. 2017;39(2):E10–E8. doi: 10.1093/pubmed/fdw061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. •.Kerr Z, Evenson KR, Moore K, Block R, Diez Roux AV. Changes in walking associated with perceived neighborhood safety and police-recorded crime: The multi-ethnic study of atherosclerosis. Prev Med. 2015;73:88–93. doi: 10.1016/j.ypmed.2015.01.017.The authors found that there were no relationships between changes in perceived safety and changes in walking for transportation or recreation. In contrast, individuals living in neighborhoods with increases in murder rates based on police-records had decreases in transportation walking.
- 51.Adlakha D, Hipp AJ, Marx C, Yang L, Tabak R, Dodson EA et al. Home and workplace built environment supports for physical activity. Am J Prev Med. 2015;48(1):104–7. doi: 10.1016/j.amepre.2014.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. •.Wong MS, Chan KS, Jones-Smith JC, Colantuoni E, Thorpe RJ Jr., Bleich SN. The neighborhood environment and obesity: Understanding variation by race/ethnicity. Prev Med. 2018;111:371–7. doi: 10.1016/j.ypmed.2017.11.029.The authors found that neighborhood social cohesion was negatively associated with BMI among Whites and Hispanics, as well as obesity among Whites. No associations between them were found for African Americans and Asians.
- 53. •.Powell-Wiley TM, Moore K, Allen N, Block R, Evenson KR, Mujahid M et al. Associations of Neighborhood Crime and Safety and With Changes in Body Mass Index and Waist Circumference: The Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2017;186(3):280–8. doi: 10.1093/aje/kwx082.This study indicated that individual- and neighborhood-level safety over time were related to lower BMI over 10 years. In contrast, they found that objectively-assessed neighborhood crime based on police records was not associated with adiposity.
- 54.Jones A Residential instability and obesity over time: the role of the social and built environment. Health Place. 2015;32:74–82. doi: 10.1016/j.healthplace.2015.01.001. [DOI] [PubMed] [Google Scholar]
- 55.Tung EL, Wroblewski KE, Boyd K, Makelarski JA, Peek ME, Lindau ST. Police-Recorded Crime and Disparities in Obesity and Blood Pressure Status in Chicago. J Am Heart Assoc. 2018;7(7). doi: 10.1161/JAHA.117.008030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Richardson AS, Troxel WM, Ghosh-Dastidar M, Hunter GP, Beckman R, Colabianchi N et al. Pathways through which higher neighborhood crime is longitudinally associated with greater body mass index. Int J Behav Nutr Phy. 2017;14. doi:ARTN 155 10.1186/s12966-017-0611-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Richardson AS, Troxel WM, Ghosh-Dastidar MB, Beckman R, Hunter GP, DeSantis AS et al. One size doesn’t fit all: cross-sectional associations between neighborhood walkability, crime and physical activity depends on age and sex of residents. Bmc Public Health. 2017;17. doi:ARTN9710.1186/s12889-016-3959-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mathis AL, Rooks RN, Tawk RH, Kruger DJ. Neighborhood Influences and BMI in Urban Older Adults. J Appl Gerontol. 2017;36(6):692–708. doi: 10.1177/0733464815584670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. •.Andersen L, Gustat J, Becker AB. The Relationship Between the Social Environment and Lifestyle-Related Physical Activity in a Low-Income African American Inner-City Southern Neighborhood. Journal of Community Health. 2015;40(5):967–74. doi: 10.1007/s10900-015-0019-z.This study showed that social cohesion mediated the association between neighborhood safety and mother’s PA, suggesting that future PA interventions could incorporate social cohesion, which in turn may increase mother’s PA level in the community perceived as unsafe.
- 60.Mooney SJ, Joshi S, Cerda M, Kennedy GJ, Beard JR, Rundle AG. Neighborhood Disorder and Physical Activity among Older Adults: A Longitudinal Study. Journal of Urban Health-Bulletin of the New York Academy of Medicine. 2017;94(1):30–42. doi: 10.1007/s11524-016-0125-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yuma-Guerrero PJ, Cubbin C, von Sternberg K. Neighborhood Social Cohesion as a Mediator of Neighborhood Conditions on Mothers’ Engagement in Physical Activity: Results From the Geographic Research on Wellbeing Study. Health Education & Behavior. 2017;44(6):845–56. doi: 10.1177/1090198116687537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mayne SL, Jose A, Mo A, Vo L, Rachapalli S, Ali H et al. Neighborhood Disorder and Obesity-Related Outcomes among Women in Chicago. Int J Environ Res Public Health. 2018;15(7). doi: 10.3390/ijerph15071395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yu CY. Racial/Ethnic and Income Differences in Obesity Among Older Adults: The Role of Leisure-time Physical Activity and Neighborhood Social Cohesion. Journal of Physical Activity & Health. 2017;14(3):169–75. doi: 10.1123/jpah.2016-0370. [DOI] [PubMed] [Google Scholar]
- 64.Sawyer ADM, Jones R, Ucci M, Smith L, Kearns A, Fisher A. Cross-sectional interactions between quality of the physical and social environment and self-reported physical activity in adults living in income-deprived communities. Plos One. 2017;12(12). doi:ARTN e0188962 10.1371/journal.pone.0188962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Leal C, Chaix B. The influence of geographic life environments on cardiometabolic risk factors: a systematic review, a methodological assessment and a research agenda. Obes Rev. 2011;12(3):217–30. doi: 10.1111/j.1467-789X.2010.00726.x. [DOI] [PubMed] [Google Scholar]
- 66.Chaix B Mobile Sensing in Environmental Health and Neighborhood Research. Annu Rev Public Health. 2018;39:367–84. doi: 10.1146/annurev-publhealth-040617-013731. [DOI] [PubMed] [Google Scholar]
- 67.Drewnowski A, Aggarwal A, Tang W, Hurvitz PM, Scully J, Stewart O et al. Obesity, diet quality, physical activity, and the built environment: the need for behavioral pathways. BMC Public Health. 2016;16(1):1153. doi: 10.1186/s12889-016-3798-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zenk SN, Matthews SA, Kraft AN, Jones KK. How many days of global positioning system (GPS) monitoring do you need to measure activity space environments in health research? Health & Place. 2018;51:52–60. doi: 10.1016/j.healthplace.2018.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. ••.Tamura K, Wilson JS, Puett RC, Klenosky DB, Harper WA, Troped PJ. Accelerometer and GPS Analysis of Trail Use and Associations With Physical Activity. Journal of Physical Activity & Health. 2018;15(7):523–30. doi: 10.1123/jpah.2016-0667.The authors demonstrated that concurrent use of accelerometers and GPS data has indicated that more trail use days were related to higher moderate physical activity.
- 70. ••.Chaix B, Kestens Y, Duncan DT, Brondeel R, Meline J, El Aarbaoui T et al. A GPS-Based Methodology to Analyze Environment-Health Associations at the Trip Level: Case-Crossover Analyses of Built Environments and Walking. Am J Epidemiol. 2016;184(8):570–8. doi: 10.1093/aje/kww071.The authors used GPS and web-based surveys to better understand physical activity throughout the day, which allows researchers to investigate life-segment assessments of environment exposures in relation to walking.
- 71.Tamura K, Elbel B, Athens JK, Rummo PE, Chaix B, Regan SD et al. Assessments of residential and global positioning system activity space for food environments, body mass index and blood pressure among low-income housing residents in New York City. Geospat Health. 2018;13(2):298–307. doi: 10.4081/gh.2018.712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zenk SN, Schulz AJ, Matthews SA, Odoms-Young A, Wilbur J, Wegrzyn L et al. Activity space environment and dietary and physical activity behaviors: a pilot study. Health Place. 2011;17(5):1150–61. doi: 10.1016/j.healthplace.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Burke LE, Shiffman S, Music E, Styn MA, Kriska A, Smailagic A et al. Ecological Momentary Assessment in Behavioral Research: Addressing Technological and Human Participant Challenges. J Med Internet Res. 2017;19(3):e77. doi: 10.2196/jmir.7138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dunton GF, Dzubur E, Intille S. Feasibility and Performance Test of a Real-Time Sensor-Informed Context-Sensitive Ecological Momentary Assessment to Capture Physical Activity. Journal of Medical Internet Research. 2016;18(6). doi:ARTN e106 10.2196/jmir.5398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Dunton GF, Dzubur E, Kawabata K, Bo B, Intille S. Development of a Smartphone Application to Measure Physical Activity Using Sensor-Driven Context-Sensitive Ecological Momentary Assessment. Annals of Behavioral Medicine. 2014;47:S52–S52. [Google Scholar]
- 76.Zenk SN, Horoi I, Jones KK, Finnegan L, Corte C, Riley B et al. Environmental and personal correlates of physical activity and sedentary behavior in African American women: An ecological momentary assessment study. Women Health. 2017;57(4):446–62. doi: 10.1080/03630242.2016.1170093. [DOI] [PubMed] [Google Scholar]
- 77.Jones M, Taylor A, Liao Y, Intille SS, Dunton GF. Real-Time Subjective Assessment of Psychological Stress: Associations with Objectively-Measured Physical Activity Levels. Psychol Sport Exerc. 2017;31:79–87. doi: 10.1016/j.psychsport.2017.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Brownson RC, Hoehner CM, Day K, Forsyth A, Sallis JF. Measuring the built environment for physical activity: state of the science. Am J Prev Med. 2009;36(4 Suppl):S99–123 e12. doi:S0749-3797(09)00013-0 [pii] 10.1016/j.amepre.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kelly CM, Wilson JS, Baker EA, Miller DK, Schootman M. Using Google Street View to Audit the Built Environment: Inter-rater Reliability Results. Annals of Behavioral Medicine. 2013;45:S108–S12. doi: 10.1007/s12160-012-9419-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ben-Joseph E, Lee JS, Cromley EK, Laden F, Troped PJ. Virtual and actual: Relative accuracy of on-site and web-based instruments in auditing the environment for physical activity. Health & Place. 2013;19:138–50. doi: 10.1016/j.healthplace.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Adu-Brimpong J, Coffey N, Ayers C, Berrigan D, Yingling LR, Thomas S et al. Optimizing Scoring and Sampling Methods for Assessing Built Neighborhood Environment Quality in Residential Areas. Int J Env Res Pub He. 2017;14(3). doi:ARTN 273 10.3390/ijerph14030273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Maglio PP, Mabry PL. Agent-based models and systems science approaches to public health. Am J Prev Med. 2011;40(3):392–4. doi: 10.1016/j.amepre.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yang Y, Diez Roux AV, Auchincloss AH, Rodriguez DA, Brown DG. A spatial agent-based model for the simulation of adults’ daily walking within a city. Am J Prev Med. 2011;40(3):353–61. doi: 10.1016/j.amepre.2010.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. ••.Powell-Wiley TM, Wong MS, Adu-Brimpong J, Brown ST, Hertenstein DL, Zenkov E et al. Simulating the Impact of Crime on African American Women’s Physical Activity and Obesity. Obesity (Silver Spring). 2017;25(12):2149–55. doi: 10.1002/oby.22040.This study demonstrated that neighborhood crime could play a role as a barrier for leisure-time physical activity, suggesting that crime reduction with multilevel intervention strategies and programs could lower obesity prevalence, which in turn contributes to promote physical activity.
- 85.Zhu W, Nedovic-Budic Z, Olshansky RB, Marti J, Gao Y, Park Y et al. Agent-based modeling of physical activity behavior and environmental correlations: an introduction and illustration. J Phys Act Health. 2013;10(3):309–22. [DOI] [PubMed] [Google Scholar]