Abstract
Introduction
Nursing home residents typically have greater needs for medical care than community-dwelling elderly. However, restricted cognitive abilities and limited mobility may impede their access to general practitioners and medical specialists. The provision of medical care in nursing homes may therefore be inappropriate in some areas of medical care. The purpose of this mixed-methods study is to systematically assess, evaluate and explain met and unmet medical care needs in German nursing homes and to develop solutions where medical care is found to be inappropriate.
Methods and analysis
First, statutory health insurance claims data are analysed to identify differences in the utilisation of medical care between nursing home residents and community-dwelling elderly with and without need for long-term care. Second, the health status and medical care of 500 nursing home residents are assessed and evaluated to quantify met and unmet medical care needs. Third, qualitative expert interviews and case conferences and, fourth, quantitative analyses of linked data are used to provide structural, case-specific and generalisable explanations of inappropriate medical care among nursing home residents. Fifth, a modified Delphi study is employed to develop pilot projects aiming to improve medical care in nursing homes.
Ethics and dissemination
This study was approved by the Ethics Committee of the University of Bremen on 23 November 2017. Research findings are disseminated through presentations at national and international conferences and publications in peer-reviewed scientific journals.
Trial registration number
DRKS00012383.
Keywords: medical care, nursing homes, needs assessment, administrative claims, health services research
Strengths and limitations of this study.
Based on longitudinal statutory health insurance claims data, cross-sectional data collected in nursing homes, expert interviews and case conferences the provision of medical care is analysed for the first time in relation to individual medical care needs among nursing home residents in Germany.
The mixed-methods design allows a comprehensive assessment, evaluation and explanation of met and unmet medical care needs in nursing homes.
Participatory approaches involving general practitioners, medical specialists, nursing home staff, statutory health insurance employees, nursing home residents and relatives are used to increase the acceptance and effectiveness of pilot projects to be developed to improve medical care where it is found to be inappropriate.
Differences in the willingness to participate among nursing homes and nursing home residents may result in a selective study population.
Focusing on nursing homes located in the federal state of Bremen and members of one local statutory health insurance fund may limit the generalisability of the study results.
Introduction
Nursing home residents may not receive appropriate medical care since restricted cognitive abilities and limited mobility may impede their access to general practitioners (GPs) and medical specialists.1–3 Moreover, nursing home residents typically suffer from multimorbidity, frailty, cognitive impairments and polypharmacy, resulting in diverse medical care needs that compound the challenge of providing appropriate medical care.4–7
Empirical studies support this view, indicating inappropriate medical care provision in nursing homes for the treatment of visual and hearing impairments,8–10 oral healthcare,1 2 11 12 pain treatment13 and drug prescriptions.2 14–17 Atramont et al, furthermore, found nursing home admission to be negatively associated with some forms of outpatient care18 and positively associated with psychotropic and antibacterial drug use.19
There is, however, hardly any empirical evidence on explanations of inappropriate medical care provision in nursing homes. In this regard, a health technology assessment report concluded that there is not sufficient data available to allow recommendations to be drawn on how medical care provision in German nursing homes can be improved.2
Given this lack of evidence, the proposed research project aims to systematically assess, evaluate and explain met and unmet medical care needs in German nursing homes and to develop solutions where medical care is found to be inappropriate. The specific aims are: (1) to identify differences in the utilisation of medical care between (a) nursing home residents, (b) community-dwelling elderly in need for long-term care and (c) community-dwelling elderly without need for long-term care; (2) to quantify met and unmet medical care needs of nursing home residents; (3) to provide structural and case-specific explanations of inappropriate medical care provision in nursing homes; (4) to provide explanations of inappropriate medical care provision that are generalisable to the total population of nursing home residents; and (5) to develop pilot projects aiming to improve medical care provision in nursing homes.
Methods and analysis
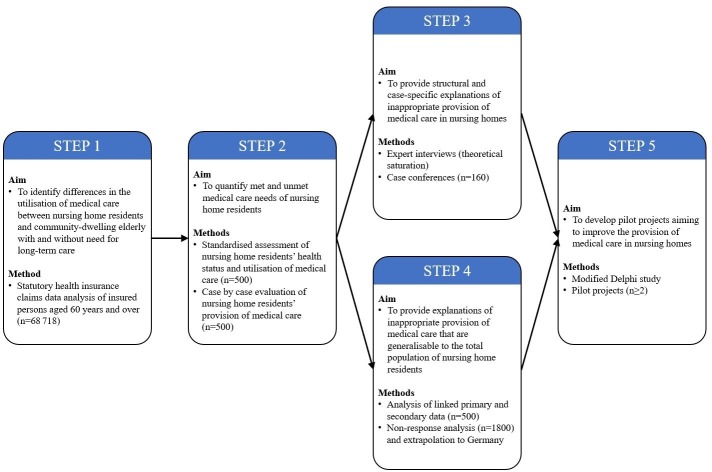
This mixed-methods study is running from 1 April 2017 to 31 March 2020. It is structured into five steps (figure 1). In step 1, statutory health insurance (SHI) claims data are analysed in order to identify differences in the utilisation of medical care between nursing home residents and community-dwelling elderly with and without the need for long-term care. Such differences in the utilisation of medical care may indicate, but not prove, inappropriate medical care provision in nursing homes. Thus, in step 2, nursing home residents’ health status and utilisation of medical care are assessed and evaluated to quantify met and unmet medical care needs with respect to vision, hearing, oral health and Parkinson’s disease. In steps 3 and 4, qualitative expert interviews and case conferences as well as quantitative methods are used to provide structural, case-specific and generalisable explanations of inappropriate medical care in nursing homes. In step 5, a modified Delphi study is used to generate ideas on how to improve the provision of medical care in nursing homes. Consequently, at least two pilot projects are developed and implemented in one nursing home to test for practicability. In the following sections, each step is described in detail.
Figure 1.
Conceptual framework of the mixed-methods study.
Step 1: analysis of SHI claims data
SHI claims data from AOK Bremen/Bremerhaven, a local SHI fund, are analysed to identify differences in the utilisation of medical care that indicate inappropriate medical care provision in German nursing homes. The available data comprise information on sex, age, in/outpatient care as well as on long-term care use of 245 000 insured persons (ie, 34.7% of the total population in the federal state of Bremen). The data represent 51.8% of the population of community-dwelling individuals with need for long-term care and 54.9% of the population of nursing home residents in Bremen. All diagnoses are coded according to the German Modification of the International Classification of Diseases, 10th Revision (ICD-10-GM) and can be differentiated according to GPs and medical specialties in the outpatient setting. In Germany, the Federal Joint Committee defines which services are reimbursed by the SHI ensuring that all SHI insured persons are treated according to the current standard of care.20 SHI claims data comprise all diagnoses coded by physicians for reimbursement purposes of services with clear benefits. Services with unclear benefits, which have to be paid out of pocket, are not included.
From the 245 000 insured persons, a subsample of 68 718 insured persons aged 60 years and over is drawn. Insured persons with missing or invalid information on demographic characteristics (n=124) are not considered. For this subsample, the morbidity status of each insured person is defined by 31 disease categories related to at least one of 13 examined medical specialties (table 1).
Table 1.
Disease categories and related medical specialties used to define the individual morbidity status of insured persons examined in step 1
| No. | Disease categories | ICD-10-GM 2015 codes | Related medical specialties* |
| 01 | Hypertensive diseases | I10-I15 | Internal medicine, cardiology |
| 02 | Ischaemic heart diseases | I20-I52 | Internal medicine, cardiology |
| 03 | Metabolic disorders | E70-E90 | Internal medicine |
| 04 | Arthropathies | M00-M25 | Internal medicine, orthopaedics |
| 05 | Diabetes mellitus | E10-E14 | Internal medicine |
| 06 | Dorsopathies | M40-M54 | Orthopaedics |
| 07 | Disorders of thyroid gland | E00-E07 | Internal medicine |
| 08 | Vascular diseases | I70-I89 | Internal medicine, cardiology |
| 09 | Organic, including symptomatic, mental disorders; other degenerative diseases of the nervous system | F00-F09; G30-G32 | Neurology/psychiatry |
| 10 | Diseases of oesophagus, stomach and duodenum; hernia; other diseases of intestines | K20-K31; K40-K46; K55-K64 | Internal medicine |
| 11 | Chronic lower respiratory diseases | J40-J47 | Internal medicine, pulmonology |
| 12 | Mood (affective) disorders | F30-F39 | Neurology/psychiatry |
| 13 | Cerebrovascular diseases | I60-I69 | Internal medicine, neurology/psychiatry |
| 14 | Neurotic, stress-related and somatoform disorders | F40-F48 | Neurology/psychiatry |
| 15 | Other diseases of urinary system; symptoms and signs involving the urinary system | N30-N39; R30-R39 | Gynaecology, urology |
| 16 | Diseases of the eye and adnexa | H00-H59 | Ophthalmology |
| 17 | Renal failure | N17-N19 | Internal medicine, nephrology |
| 18 | Osteopathies and chondropathies | M80-M94 | Orthopaedics |
| 19 | Diseases of the ear and mastoid process | H60-H95 | Otorhinolaryngology |
| 20 | Mononeuropathies; polyneuropathies and other disorders of the peripheral nervous system | G56-G64 | Internal medicine, neurology/psychiatry |
| 21 | Diseases of male genital organs | N40-N51 | Urology |
| 22 | Melanoma and other malignant neoplasms of skin; dermatitis, eczema | C43-C44; L20-L30 | Dermatology, surgery |
| 23 | Noninflammatory disorders of female genital tract | N80-N98 | Gynaecology |
| 24 | Other disorders of the skin and subcutaneous tissue | L80-L99 | Dermatology |
| 25 | Extrapyramidal and movement disorders | G20-G26 | Internal medicine, neurology/psychiatry |
| 26 | Mental and behavioural disorders due to psychoactive substance use | F10-F19 | Neurology/psychiatry |
| 27 | Cerebral palsy and other paralytic syndromes | G80-G83 | Internal medicine, neurology/psychiatry |
| 28 | Malnutrition; obesity and other hyperalimentation | E40-E46; E65-E68 | Internal medicine |
| 29 | Schizophrenia, schizotypal and delusional disorders; disorders of adult personality and behaviour | F20-F29; F60-F69 | Neurology/psychiatry |
| 30 | Functional impairments | U50-U52 | Internal medicine, Orthopaedics |
| 31 | Injuries | S00-S99; T08-T14 | Orthopaedics, surgery |
*Due to the availability of data, dentistry had to be analysed separately and is therefore not presented.
Descriptive analyses are conducted in two steps. First, the prevalence of each single disease category in 2015 is determined among the groups of nursing home residents, community-dwelling elderly in need for long-term care and community-dwelling elderly without need for long-term care. Second, for the 45 combinations of disease categories and related medical specialties, the proportion of prevalent cases with an outpatient visit in the related medical specialty in 2015 is calculated among the three groups (ie, nursing home residents as well as community-dwelling elderly with and without need for long-term care). Lower proportions of prevalent cases with an outpatient visit in the related medical specialty may indicate, but not prove, unmet medical care needs.
Poisson regression analyses are conducted to investigate the intensity of medical care for the 45 combinations of disease categories and related medical specialties separately. In cases of overdispersion, negative binomial regression and in cases of excess zeros, zero-inflated Poisson regression or zero-inflated negative binomial regression analyses are conducted. Each regression model includes only those insured persons who are diagnosed in the examined disease category and have valid information on all variables included in the model. The dependent variable is the number of outpatient visits in the related medical specialty in 2015. Independent variables are age (in 5-year groups), sex and dummy variables as a combination of the obtained level of care (no long-term care dependency, level 1, level 2, level 3 of long-term care dependency) and the care setting (community, nursing home). To take account of differences in morbidity and mortality that likely impact the number of outpatient visits, the remaining 30 disease categories and death are included as control variables. Multicollinearity between variables is evaluated on the basis of the variance inflation factor.
Step 2: assessment of nursing home residents
The standardised assessment focuses on vision, hearing, oral health and Parkinson’s disease. It consists of two parts: first, the individual health status and medical care provision of 500 nursing home residents are assessed. Second, the provision of medical care is evaluated for each resident to determine met and unmet medical care needs.
Residents are eligible for assessment if (1) they are in need for long-term care, (2) are aged 60 years and over, (3) have been residing in a nursing home located in the federal state of Bremen for at least 12 months and (4) are a member of the AOK Bremen/Bremerhaven. The total number of eligible nursing home residents is approximately 1800. The recruitment strategy comprises two stages: at stage 1, the total number of nursing homes located in the federal state of Bremen is approached for participation by the research team (ie, no sampling strategy is applied). At stage 2, all eligible residents (or their legal guardians) are invited for participation and approached for informed consent by the nursing homes agreeing to participate (ie, also no sampling strategy is applied). We expect that not all nursing homes and not all nursing home residents agree to participate and assume to reach 25%–30% of the approximately 1800 eligible nursing home residents, resulting in a study population of 500 nursing home residents. In case of reaching considerably less than 500 participants, the recruitment strategy may be extended to the federal state of Lower Saxony.
The standardised assessment is carried out by trained study nurses and includes: (1) examinations of residents, (2) self-assessments by residents, (3) proxy-assessments by residents’ care nurses and (4) reviews of nursing records (table 2). The examination of residents comprises the application of a visual test,21 a whispered voice test22 and the Oral Health Assessment Tool (OHAT).23 During the self-assessments, nursing home residents are asked, inter alia, to rate their vision, hearing and oral health as well as whether they use a visual aid, a hearing device or dentures. Further questions relate to their general health status. The residents’ self-assessments are complemented by the proxy-assessments in which the residents’ care nurses are asked the same or comparable questions. Information regarding the utilisation of medical care (eg, contacts to general and specialised care), sociodemographic data and nursing home characteristics are obtained from the residents’ care nurses and nursing records.
Table 2.
Instruments used to assess cross-sectional data in step 2
| Category | Instrument | Source* | |||
| E | S | P | R | ||
| Area of medical care | |||||
| Vision | Visual test21 | X | |||
| Questionnaire for individual rating of vision and use of visual aids | X | X | |||
| Review of nursing records in terms of vision-related diagnoses (eg, age-related macular degeneration, cataract) and relevant comorbidities (eg, diabetes mellitus) | X | ||||
| Hearing | Whispered voice test22 | X | |||
| Questionnaire for individual rating of hearing and use of hearing devices | X | X | |||
| Review of nursing records in terms of hearing-related diagnoses (eg, presbycusis) | X | ||||
| Oral health | OHAT23 | X | |||
| OHIP24 | X | ||||
| Questionnaire for individual rating of dental problems as well as availability and use of dentures | X | X | |||
| Review of nursing records in terms of oral health-related diagnoses (eg, gingivitis) | X | ||||
| Parkinson’s disease | Review of nursing records in terms of diagnosis of Parkinson’s disease, prescribed medications and contacts to medical specialists (eg, neurologists) and/or therapists (eg, physiotherapists) | X | |||
| General health status | |||||
| Health-related quality of life | SF-1225 | X | X | ||
| Depression | GDS26 27 | X | |||
| CSDD28 | X | ||||
| Functional and cognitive status | Mini-Mental State Examination29 | X | |||
| Extended Barthel-Index30 | X | ||||
| Nutrition | MNA-SF31–34 | X | |||
| Vital signs | Review of nursing records in terms of vital signs and falls | X | |||
| Level of care | Review of nursing records in terms of level of care | X | |||
| Additional data | |||||
| Utilisation of medical care | Questionnaire for and review of nursing records in terms of diagnoses, prescriptions of medication and aids, contacts to and organisation of general and specialised care, hospitalisation, contacts to duty doctors and emergency calls | X | X | ||
| Sociodemographic data | Questionnaire for and review of nursing records in terms of age, sex, education, marital status, migrant status and relatives | X | X | ||
| Nursing home characteristics | Questionnaire† for size, number of employees and residents, location-related information | X | |||
*E, examinations of residents; S, self-assessed by residents; P, proxy assessed by residents’ care nurses; R, reviewed in nursing records.
†This questionnaire is completed by administrative employees of the respective nursing home.
CSDD, Cornell Scale for Depression in Dementia; GDS, Geriatric Depression Scale; MNA-SF, Mini-Nutritional Assessment Short Form; OHAT, Oral Health Assessment Tool; OHIP, Oral Health Impact Profile; SF-12, Short-Form Health Survey.
In addition, health-related aspects (eg, quality of life and depression) are assessed as well as structural factors relating to the participating nursing homes (eg, numbers of employees and residents) that may act as explanatory variables of medical care.
The assessed data are summarised in individual case reports. These case reports comprise information on age, sex, level of care, date of nursing home admission, in- and outpatient medical care, diagnoses, medication, aids, vital signs, falls, the result of the visual test and self-reported use of visual aids, the result of the whispered voice test and self-reported use of hearing devices, all data of the OHAT, the self/proxy-assessed oral health, the proxy-assessed availability and use of dentures as well as the result of the Oral Health Impact Profile.24 Moreover, the case reports include the results of the instruments applied for assessing the health-related quality of life,25 depression,26–28 functional and cognitive status,29 30 nutrition31–34 as well as all comments made by the trained study nurses during the assessment. Based on the case reports (in printed form), a geriatrician and a GP jointly determine case by case whether or not medical care needs in the areas of vision, hearing, oral health and Parkinson’s disease are met, that is, whether or not the provision of medical care is appropriate. In cases of uncertainties or discrepancies, geriatricians and GPs may access all assessed data (in digital form) and decide to consult a medical specialist of the corresponding field (i.e. an ophthalmologist, an ear, nose and throat specialist, a dentist or a neurologist) who independently determines whether or not medical care needs in the respective area are met. Based on these data, the prevalence of met and unmet medical care needs is quantified for each area. The process of evaluating met and unmet medical care needs is based on standardised guidelines and is tested and adjusted before final application. All physicians are trained on how to evaluate met and unmet medical care needs. Intercoder reliability is assessed for a subsample of 50 nursing home residents.
Step 3: expert interviews and case conferences
Semi-structured expert interviews and case conferences are used to identify structural and case-specific explanations of inappropriate medical care provision in nursing homes. Expert interviews are conducted with nursing home staff, physicians, people in need for long-term care and informal caregivers who provide informed consent. The number of interviews is determined by the principal of theoretical saturation. All interviews are recorded on tape, transcribed and analysed using content analysis.35 The results provide a framework for the subsequent case conferences, which are conducted for a selected subsample of nursing home residents assessed in step 2.
The case conferences are held with the consenting nurses and, where necessary, the consenting physicians and other health professionals involved in the provision of nursing and medical care of the respective resident. Twenty residents with appropriate medical care and twenty residents with inappropriate medical care are randomly selected for each field of medical care (ie, vision, hearing, oral health and Parkinson’s disease). The case conferences are based on a summarised presentation of the health status and medical care provision of the respective resident. Using problem-centred group interviews,36 the conference members then discuss, case by case, factors that foster or inhibit the provision of needs-based medical care.
Step 4: analysis of linked data, non-response analysis and extrapolation
In step 4, primary data of the 500 nursing home residents assessed in step 2 and SHI claims data covering the years 2014–2018 are linked at the individual level. The linked data are analysed to identify generalisable factors that impact the provision of medical care.
First, retrospective and prospective regression analyses are conducted. Retrospective analyses are used to identify factors in the utilisation of medical care that impact the quantified met and unmet medical care needs of nursing home residents. Prospective analyses are used to investigate the impact of the standardised assessment conducted in step 2 on the utilisation of medical care.
Next, a non-response analysis is conducted. SHI claims data of 500 responders and 1300 non-responders are analysed to identify systematic differences between responders and non-responders. χ2 tests are used to identify differences in the distribution of age groups, sex, morbidity and long-term care levels. Differences in the mean duration of stays in long-term care and nursing homes are identified using t-tests for normally distributed variables and Wilcoxon-Mann-Whitney tests for non-normal distributions.
Third, prevalence of met and unmet medical care needs determined in step 2 is extrapolated. Controlling for systematic differences between responders and non-responders identified in the non-response analysis, prevalence of met and unmet medical care needs in the areas of vision, hearing, oral health and Parkinson’s disease is projected to all nursing home residents insured by the AOK Bremen/Bremerhaven. Using official statistics, systematic differences in the distribution of age groups, sex and long-term care levels between nursing home residents insured by the AOK Bremen/Bremerhaven and the total population of nursing home residents in the federal state of Bremen are identified. Taking into account identified differences, the prevalence of met and unmet medical care needs is then projected to all nursing home residents of Bremen. Finally, the prevalence is projected to all nursing home residents of Germany controlling for identifiable differences in the distribution of age groups, sex and long-term care levels between nursing home residents in Bremen and Germany.
Step 5: modified Delphi study and pilot projects
Based on the factors identified that may explain inappropriate medical care in steps 3 and 4, a modified Delphi study is then carried out. The technique is used with stakeholders from the fields of nursing and medical care and comprises three rounds. The first round is based on face-to-face focus group discussions, while the second and third rounds each consist of a semi-structured online survey. Each survey takes about 20 min to complete and is online for up to 2 weeks.
In the first round, a convenience sample of at least two homogeneous and two heterogeneous focus groups of four to six participating stakeholders (ie, nursing home staff, GPs, medical specialist, SHI employees, nursing home residents and relatives) generates ideas on how medical care provision to nursing home residents can be improved. The focus groups are led by two experienced project researchers, who feed the results of steps 3 and 4 into the discussions. All focus group discussions are recorded, summarised and discussed within the research team. Based on the results, the project researchers draft at least two potential pilot projects.
In the second round, the experts of the first round are given descriptions of the potential pilot projects. They rate and comment on the proposed pilot projects with respect to their feasibility and effectiveness for improving medical care of nursing home residents. These ratings are narratively and visually summarised.
In the third round, the same experts re-rate the projects based on the summarised ratings from the previous round. The re-ratings are summarised using the same method as in the second round. Taking the results of this last round into account, the concept of the pilot projects is revised. This is expected to result in a more consensual decision. At least two pilot projects are implemented simultaneously in one nursing home to test for practicability. To minimise the risk of contamination effects, the pilot projects are implemented in different areas of the nursing home. A systematic evaluation of the pilot projects is planned in a follow-up study.
Patient and public involvement
Nursing home residents and the public were not involved in the development of the research questions and outcome measures as well as in the design of and the recruitment to the study. Nursing home residents are involved in the standardised assessments of vision, hearing, oral health, health-related quality of life, depression as well as functional and cognitive status (self-assessments). Furthermore, nursing home residents and relatives are involved in the expert interviews, the modified Delphi study and the development of pilot projects. The results of the standardised assessment are summarised and disseminated to the participating nursing homes (ie, the results are not directly disseminated to the participating residents). The results of the expert interviews, the modified Delphi study and the development of pilot projects are disseminated to the participating nursing home residents and relatives.
Discussion
This mixed-methods study broadens the limited evidence on the needs-based provision of medical care in nursing homes. It systematically assesses, evaluates and explains met and unmet medical care needs in nursing homes and takes first steps towards improvement.
Up to now, several studies have described differences in the utilisation of medical care between nursing home residents and community-dwelling elderly with and without need for long-term care.2 37–39 None of these, however, has evaluated whether such differences reflect unmet medical care needs at the individual level. Neither have differences in the utilisation of medical care been explained by prevailing structures that may be changed.
This mixed-methods study addresses this evidence gap: based on longitudinal SHI claims data, cross-sectional data collected in nursing homes as well as transcripts of expert interviews and case conferences, differences in the utilisation of medical care are identified, met and unmet medical care needs are quantified, explanations of inappropriate provision of medical care are provided and pilot projects are developed aiming to improve the provision of medical care where it is found to be inappropriate. Participatory approaches involve GPs, medical specialists, nursing home staff, SHI employees, nursing home residents and relatives. This is expected to result in strong acceptance and effective pilot projects which will be systematically evaluated in a follow-up study.
There are, however, some limitations to consider. First, in this study, all nursing homes in the federal state of Bremen are invited to participate and to recruit nursing home residents for study participation. Differences in the willingness to participate among nursing homes and nursing home residents may result in a selective study population. The claims-based non-response analysis, however, permits the identification of structural differences between participants and non-participants. Second, the study focuses on nursing homes located in the federal state of Bremen and members of one local SHI fund. Therefore, the generalisability of research findings may be limited.
In conclusion, the findings from this study enhance our knowledge of met and unmet medical care needs in nursing homes. The pilot projects provide a first step towards a sustainable improvement of medical care in German nursing homes. Therefore, it is expected that the findings are highly relevant for many stakeholders from the fields of nursing and medical care.
Supplementary Material
Acknowledgments
We are grateful to the AOK Bremen/Bremerhaven for the provision of longitudinal statutory health insurance (SHI) claims data as well as to the Bremer Heimstiftung, the Bundesverband privater Anbieter sozialer Dienste e.V., the LandesArbeitsGemeinschaft der Freien Wohlfahrtspflege Bremen e.V. and the Hausärzteverband Bremen for their cooperation. Furthermore, we are grateful to the participating nursing homes, nursing home residents, physicians, relatives, study nurses, student assistants and SHI employees as well as to Vicki May for proofreading this protocol.
Footnotes
Contributors: JC, TK, ASchw, GS, KW-O, AG and HR designed the study. MS, TK, CT, ASchw and HR specified the analysis of longitudinal statutory health insurance claims data. MS, FH, DG, ASchm, SK, GS, KW-O, AG and HR specified the collection of cross-sectional primary data. JC, MS, FH, DG, ASchm, CT, ASchw and SK wrote the first draft of the protocol which was critically revised by TK, GS, KW-O, AG and HR. All authors approved the final version of the protocol.
Funding: This work was supported by the Innovation Committee at the Federal Joint Committee (grant number 01VSF16039).
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Iliffe S, Davies SL, Gordon AL, et al. Provision of NHS generalist and specialist services to care homes in England: review of surveys. Prim Health Care Res Dev 2016;17:122–37. 10.1017/S1463423615000250 [DOI] [PubMed] [Google Scholar]
- 2. Balzer K, Butz S, Bentzel J, et al. Medical specialist attendance in nursing homes. GMS Health Technol Assess 2013;9:Doc02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Burns E, Nair S. New horizons in care home medicine. Age Ageing 2014;43:2–7. 10.1093/ageing/aft186 [DOI] [PubMed] [Google Scholar]
- 4. Briggs R, Holmerová I, Martin FC, et al. Towards standards of medical care for physicians in nursing homes. Eur Geriatr Med 2015;6:401–3. 10.1016/j.eurger.2015.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gordon AL, Franklin M, Bradshaw L, et al. Health status of UK care home residents: a cohort study. Age Ageing 2014;43:97–103. 10.1093/ageing/aft077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Björk S, Juthberg C, Lindkvist M, et al. Exploring the prevalence and variance of cognitive impairment, pain, neuropsychiatric symptoms and ADL dependency among persons living in nursing homes; a cross-sectional study. BMC Geriatr 2016;16:154 10.1186/s12877-016-0328-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tolson D, Rolland Y, Andrieu S, et al. International association of gerontology and geriatrics: a global agenda for clinical research and quality of care in nursing homes. J Am Med Dir Assoc 2011;12:184–9. 10.1016/j.jamda.2010.12.013 [DOI] [PubMed] [Google Scholar]
- 8. Thibault L, Kergoat H. Eye care services for older institutionalised individuals affected by cognitive and visual deficits: a systematic review. Ophthalmic Physiol Opt 2016;36:566–83. 10.1111/opo.12311 [DOI] [PubMed] [Google Scholar]
- 9. Yamada Y, Vlachova M, Richter T, et al. Prevalence and correlates of hearing and visual impairments in European nursing homes: results from the shelter study. J Am Med Dir Assoc 2014;15:738–43. 10.1016/j.jamda.2014.05.012 [DOI] [PubMed] [Google Scholar]
- 10. Cohen-Mansfield J, Infeld DL. Hearing AIDS for nursing home residents: current policy and future needs. Health Policy 2006;79:49–56. 10.1016/j.healthpol.2005.11.016 [DOI] [PubMed] [Google Scholar]
- 11. Zenthoefer A, Cabrera T, Hassel A, et al. Increasing dependency of older people in nursing homes is associated with need for dental treatments. Neuropsychiatr Dis Treat 2014;10:2285–90. 10.2147/NDT.S71184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Müller F, Naharro M, Carlsson GE. What are the prevalence and incidence of tooth loss in the adult and elderly population in Europe? Clin Oral Impl Res 2007;18(Suppl 3):2–14. 10.1111/j.1600-0501.2007.01459.x [DOI] [PubMed] [Google Scholar]
- 13. Lukas A, Mayer B, Onder G, et al. [Pain therapy in German long-term care facilities in a European comparison. Results of the SHELTER study]. Schmerz 2015;29:411–21. [DOI] [PubMed] [Google Scholar]
- 14. Storms H, Marquet K, Aertgeerts B, et al. Prevalence of inappropriate medication use in residential long-term care facilities for the elderly: a systematic review. Eur J Gen Pract 2017;23:69–77. 10.1080/13814788.2017.1288211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dörks M, Allers K, Schmiemann G, et al. Inappropriate medication in non-hospitalized patients with renal insufficiency: a systematic review. J Am Geriatr Soc 2017;65:853–62. 10.1111/jgs.14809 [DOI] [PubMed] [Google Scholar]
- 16. Morin L, Laroche M-L, Texier G, et al. Prevalence of potentially inappropriate medication use in older adults living in nursing homes: a systematic review. J Am Med Dir Assoc 2016;17:862.e1–9. 10.1016/j.jamda.2016.06.011 [DOI] [PubMed] [Google Scholar]
- 17. Johnell K. Inappropriate drug use in people with cognitive impairment and dementia: a systematic review. Curr Clin Pharmacol 2015;10:178–84. 10.2174/1574884710666150609154741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Atramont A, Bourdel-Marchasson I, Bonnet-Zamponi D, et al. Impact of nursing home admission on health care use and disease status elderly dependent people one year before and one year after skilled nursing home admission based on 2012–2013 SNIIRAM data. BMC Health Serv Res 2017;17:667 10.1186/s12913-017-2620-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Atramont A, Bonnet-Zamponi D, Bourdel-Marchasson I, et al. Health status and drug use 1 year before and 1 year after skilled nursing home admission during the first quarter of 2013 in France: a study based on the French National Health Insurance Information System. Eur J Clin Pharmacol 2018;74:109–18. 10.1007/s00228-017-2343-y [DOI] [PubMed] [Google Scholar]
- 20. Gemeinsamer Bundesausschuss The federal joint Committee. Available: https://www.g-ba.de/downloads/17-98-2804/2018-12-04_G-BA_Flyer_Der_Gemeinsame_Bundesausschuss_EN_bf.pdf [Accessed 22 Apr 2019].
- 21. Bailey IL, Lovie JE. New design principles for visual acuity letter charts. Am J Optom Physiol Opt 1976;53:740–5. 10.1097/00006324-197611000-00006 [DOI] [PubMed] [Google Scholar]
- 22. Macphee GJA, Crowther JA, McAlpine CH. A simple screening test for hearing impairment in elderly patients. Age Ageing 1988;17:347–51. 10.1093/ageing/17.5.347 [DOI] [PubMed] [Google Scholar]
- 23. Chalmers JM, King PL, Spencer AJ, et al. The oral health assessment tool — validity and reliability. Aust Dent J 2005;50:191–9. 10.1111/j.1834-7819.2005.tb00360.x [DOI] [PubMed] [Google Scholar]
- 24. John MT, Miglioretti DL, LeResche L, et al. German short forms of the oral health impact profile. Community Dent Oral Epidemiol 2006;34:277–88. 10.1111/j.1600-0528.2006.00279.x [DOI] [PubMed] [Google Scholar]
- 25. Morfeld M, Kirchberger I, Bullinger M. SF-36. Fragebogen zum Gesundheitszustand: Deutsche Version des Short Form - 36 Health Survey. Göttingen: Hogrefe, 2011. [Google Scholar]
- 26. Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 1982;17:37–49. 10.1016/0022-3956(82)90033-4 [DOI] [PubMed] [Google Scholar]
- 27. Allgaier AK, Kramer D, Mergl R, et al. [Validity of the geriatric depression scale in nursing home residents: comparison of GDS-15, GDS-8, and GDS-4]. Psychiatrische Praxis 2011;38:280–6. [DOI] [PubMed] [Google Scholar]
- 28. Alexopoulos GS, Abrams RC, Young RC, et al. Cornell scale for depression in dementia. Biol Psychiatry 1988;23:271–84. 10.1016/0006-3223(88)90038-8 [DOI] [PubMed] [Google Scholar]
- 29. Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–98. [DOI] [PubMed] [Google Scholar]
- 30. Prosiegel M, Böttger S, Schenk T, et al. Der Erweiterte Barthel-Index (EBI) - eine neue Skala zur Erfassung von Fähigkeitsstörungen bei neurologischen Patienten. Neurol Rehabil 1996;2:7–13. [Google Scholar]
- 31. Rubenstein LZ, Harker JO, Salva A, et al. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J Gerontol A Biol Sci Med Sci 2001;56:M366–72. 10.1093/gerona/56.6.M366 [DOI] [PubMed] [Google Scholar]
- 32. Vellas B, Villars H, Abellan G, et al. Overview of the MNA-Its history and challenges. J Nutr Health Aging 2006;10:456–63. discussion 463-5. [PubMed] [Google Scholar]
- 33. Guigoz Y. The mini nutritional assessment (MNA) review of the literature-What does it tell us? J Nutr Health Aging 2006;10:466–85. discussion 485-7. [PubMed] [Google Scholar]
- 34. Kaiser MJ, Bauer JM, Ramsch C, et al. Validation of the mini nutritional assessment short-form (MNA®-SF): a practical tool for identification of nutritional status. J Nutr Health Aging 2009;13:782–8. 10.1007/s12603-009-0214-7 [DOI] [PubMed] [Google Scholar]
- 35. Kohlbacher F. The use of qualitative content analysis in case study research. Forum: Qual Soc Res 2006. [Google Scholar]
- 36. Witzel A. The problem-centered interview. Forum: Qual Soc Res 2000. [Google Scholar]
- 37. Kleina T, Horn A, Suhr R, et al. [Current status of medical care for nursing home residents in Germany - results of an empirical study]. Gesundheitswesen 2017;79:382–7. [DOI] [PubMed] [Google Scholar]
- 38. Schmiemann G, Herget-Rosenthal S, Hoffmann F. [Medical services for nursing home residents: results of the study on inappropriate medication in patients with renal insufficiency in nursing homes]. Z Gerontol Geriatr 2016;49:727–33. [DOI] [PubMed] [Google Scholar]
- 39. Pittrow D, Krappweis J, Rentsch A, et al. Pattern of prescriptions issued by nursing home-based physicians versus office-based physicians for frail elderly patients in German nursing homes. Pharmacoepidemiol Drug Saf 2003;12:595–9. 10.1002/pds.860 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.