Abstract
Electrical injuries are a common occurrence and can be minor or even fatal depending on the voltage to which an individual has been exposed to. Electrical current causes tissue damage by producing heat due to local tissue resistance. Serious electrocution may manifest with cutaneous burns, visceral injuries, organ perforation, and cardiac and respiratory effects. Pneumothorax as a complication of electrical injury is a very rare entity. We report one such case of electrical burn injury with right-sided pneumothorax as an immediate complication.
Keywords: pneumothorax, trauma
Background
Electrical injury needs emergency care for immediate complications including cardiac arrhythmias and respiratory arrest, skin burns, and damage to the internal organs and soft tissues. Pneumothorax must be considered in the differential diagnosis of respiratory distress in patients with electrical injuries to the limbs or trunk. An electrical injury presenting with pneumothorax is a rare occurrence, and the physician needs to be watchful as the development of pneumothorax may be delayed.
Case presentation
A 29-year-old man was referred to our hospital with a history of right-sided chest pain, breathlessness and dry cough following a prolonged electrical shock (220–240 V alternating current (AC), lasting 4–5 min) about 3 days earlier, with injury to the right hand and the right foot. Electrical shock resulted from handling an electrical plug without any protective gloves or footwear. He had been given initial treatment by his primary care doctor for the burn injury on his right hand. Clinical examination showed superficial burn wounds on the palmar aspect of the right hand and the right foot. He had no visible external injuries on the head, trunk or legs. He had a regular pulse rate of 112 per minute, blood pressure of 100/66 mm Hg, respiratory rate of 36 per minute and peripheral capillary oxygen saturation (SpO2) of 92% on ambient air. His chest was symmetrical, and there were no cutaneous burns on the chest wall. There was decreased chest expansion on the right side with hyper-resonant note on percussion and vesicular breath sounds reduced in intensity. The left lung was normal on examination, and the rest of the systemic examination was normal.
Investigations
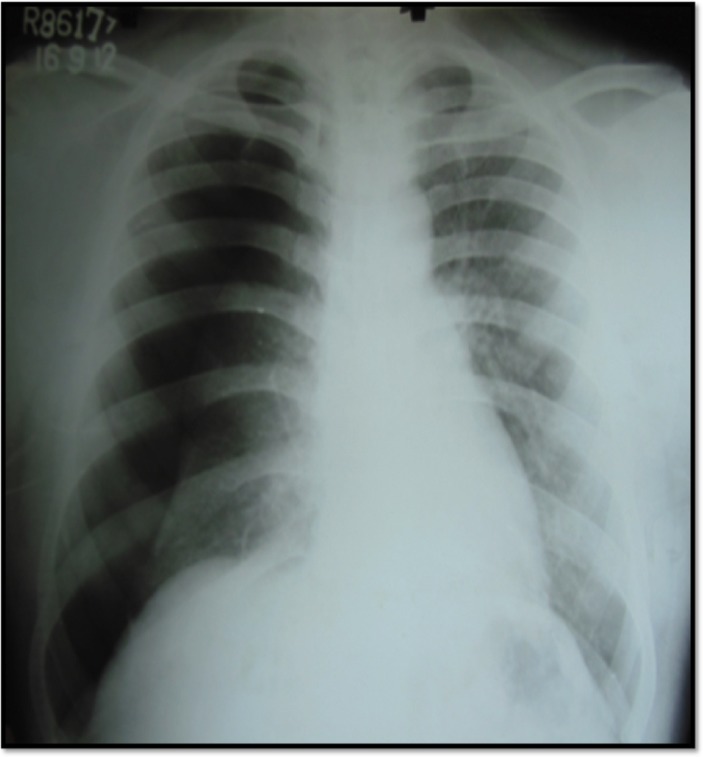
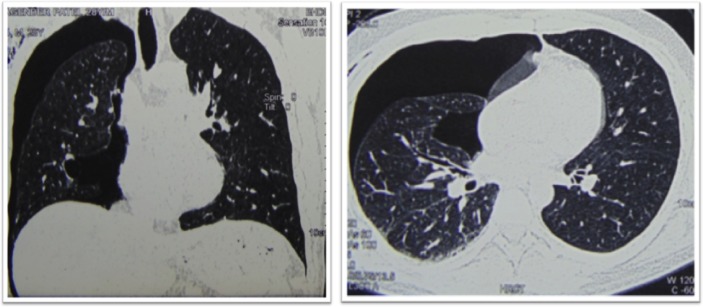
Routine haematological and biochemical parameters, including transaminases and creatinine, were normal. Electrocardiograph showed sinus tachycardia. Chest X-ray confirmed right-sided pneumothorax (estimated volume of 45%) with no bony fractures (figure 1). High Resolution Contrast Computed Tomography (HRCT) of the chest (figure 2) had large pneumothorax with collapsed right lung and mediastinal shift to the left, and there was no evidence of lung contusion or bullae seen on the left lung.
Figure 1.
Chest radiograph showing large, right-sided pneumothorax seen with the passive collapse of the lung and contralateral shift of the mediastinum.
Figure 2.
CT showing large pneumothorax on the right side with collapsed lung and shift of the mediastinum to the left.
Treatment
A 28-French intercostal drain was inserted into the right pleural space under local anaesthesia, and a gush of air was noted in the underwater seal bag. The patient improved promptly. Postprocedure, his pulse was 86 per minute, his blood pressure was 140/86 mm Hg, and his respiratory rate was 24 per minute, with an SpO2 of 95% on ambient air. Postintercostal tube drainage, there was persistent air leak in the underwater seal drainage bag for 3 weeks. The course in the hospital was complicated by the development of fever and purulent pleural fluid suggestive of empyema thoracis, which was managed with intravenous antibiotics (ceftriaxone injection 1 g intravenously 12th hourly and clindamycin injection 600 mg intravenously 12th hourly for 4 weeks). Blood culture was sterile, and pleural fluid Gram stain and culture were negative. Intercostal drain was removed after 4 weeks once his empyema had resolved completely and there was no purulent fluid drainage for 2 days.
Outcome and follow-up
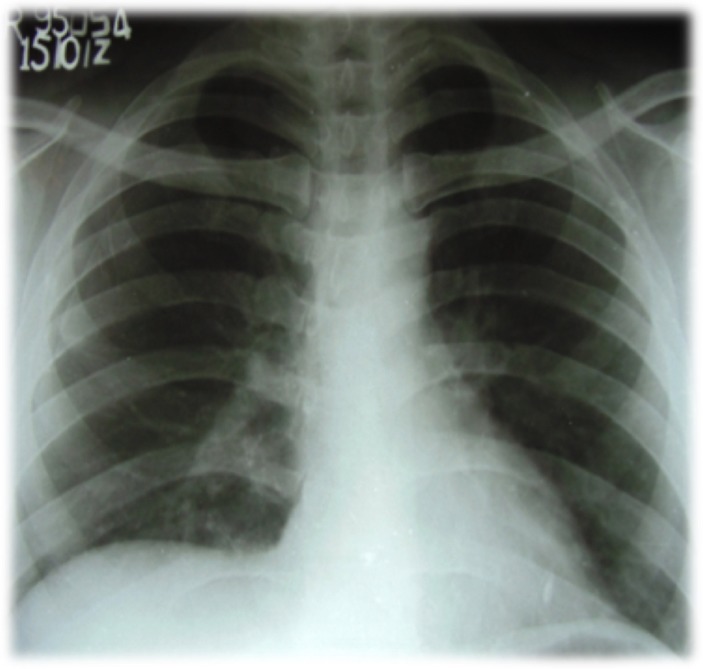
The patient was asymptomatic with complete resolution of pneumothorax (figure 3) without pleural thickening and with normal spirometry on follow-up at 5 months. The patient has been counselled about safe handling of electrical circuits.
Figure 3.
Chest X-ray (Postero Anterior View) showing significant resolution of pneumothorax.
Discussion
Electrical injuries are a common occurrence and can be very trivial or fatal depending on the voltage an individual has been exposed to. The voltage necessary for electrocution depends on the current through the body and the duration of the current. Electrical current causes tissue damage by producing heat due to local tissue resistance.1 2
Electrical current causes damage by altering cell resting membrane potential and by converting electrical energy into thermal energy, resulting in massive tissue destruction and coagulative necrosis. Secondary damage due to falls and violent muscle contractions is also documented.3
The severity of electrical injury to an individual depends on various aspects of the electrical current, referred to as Kouwenhoven’s factors. 4 These include the following: type of current, amount of current, current path, voltage, resistance and duration of exposure.
Type of current: Depending on the flow of electrical charge, current is divided into alternating and direct current. The tendency of an electrical shock to prevent the patient from letting go of the source is due to a tetanic muscle contraction which is sustained over time. This tendency is more in direct current as compared with AC. Human tissue is most sensitive to frequencies between 40 and 150 Hz. The frequency of household AC is about 50 Hz, which can lead to serious electrical injury.
Amount of current: The human body can perceive current more than 1 mA. Depending on the amount of current, the effects can range from mild tingling sensation to cardiac arrest. Muscular tetany leading to difficulty in releasing the grip from the source can be evident at a current of 7–9 mA, whereas a current of 20–50 mA and 50–100 mA can lead to respiratory distress and ventricular fibrillation, respectively. A current over 2 A can result in cardiac asystole.
Current path: The injury to the body due to current is dependent on the path the electrical current has traversed. The hand is the most common point of entry, followed by the head. The foot is the most common ground point. Current that travels between the arms or between the arm and the foot is likely to traverse through the heart and the lungs and may cause arrhythmias and respiratory distress, with immediate mortality of up to 60%. In cautery, an electrosurgical procedure composed of active electrodes and neutral electrodes (monopolar system), electrical current moves from the active electrode, traverses the tissue and exits through the neutral electrode. The heat caused due to resistance in the tissue is responsible for the cauterisation effect. As it is the basic nature of current that it follows a path of least resistance, the entry and exit of the cautery system offer the least resistance to the current flow, thus preventing damage to other tissues. Generator → Active electrode → Patient’s tissue →-> Neutral electrode. Defibrillators used in resuscitation have two electrodes placed at the apex of the heart and over the right upper chest, respectively, providing an inlet and outlet to the current as it passes through the heart tissue.
Voltage: Tissue damage is directly proportional to voltage. Less than 50 V is not likely to cause injury. Household voltage is between 220 and 240 V, and this can effectively cause small entry and exit wounds. More than 1000 V can lead to significant tissue damage.
Resistance: The current travels through the body taking the path of least resistance.5 The greater the resistance, the greater the damage. Often due to less resistance of the skin, skin burns are minimal; however, due to the greater resistance of internal structures, significant injury occurs to organs. Thus, the absence of external burns does not predict the absence of electrical injury, and the severity of external burns does not predict the severity of electrical injury, as sometimes patients present with visceral damage and organ perforation.
Duration of exposure: Duration of exposure is directly proportional to the severity of electrical injury.
Systemic effects of electrical injury
Tissue damage due to electrical current is primarily the result of local heat produced due to tissue resistance. Damage to the viscera may present in late stages, with organ perforations presenting immediately or after several days of electrical injury. The various organ systems which can be affected are as discussed below.
Electrical skin burns
There can be mild first-degree burns or significant third-degree burns depending on various factors mentioned above. The hallmark of these burns is a depressed and charred central area with surrounding oedema. There may be several entry and exit wounds. Certain characteristic burns due to electrical injury are the ‘Arc Burns’ and ‘Kissing Burns’. Arc burns are produced by the passage of a current of electricity from the source to the ground and may be associated with extensive skin damage. During an electrical shock, sustained muscle contraction leads to flexion of the joint, which causes the current to flow through the contiguous skin. This type of burns around the flexor creases is known as the kissing burn.3
Cardiac effects
Depending on the amount of current and the path traversed, cardiac effects can range from arrhythmias to sudden cardiac death. Usually the cause of death is ventricular fibrillation. Cardiac biomarkers (creatine kinase MB, troponin T and troponin I) will be elevated in most patients with electrocution injury and cannot be relied on to establish myocardial damage.6
Nervous system
Electrical injury can have effects on the nervous system, ranging from confusion, seizures and respiratory arrest. Ischaemic stroke and coma due to electrical injury have also been reported.
Complex regional pain syndrome and peripheral nerve injury are delayed presentations attributable to electrical injury.
Renal system
Electrical injury can lead to myoglobinuria due to muscle damage. Other effects include dehydration and direct damage to the renal vessels. These can potentially lead to acute tubular necrosis causing acute renal failure. Transient renal abnormalities such as oliguria, albuminuria, haemoglobinuria and renal casts may also occur.7
Musculoskeletal effects
Muscle injury leads to myoglobinuria. Muscle rupture and bone fractures are reported secondary to tetanic muscle contraction. Secondary injuries arise from being thrown back from the source.8
Abdominal organs
Organ perforation may occur due to damage to the visceral walls after a significant electrical injury.7
Miscellaneous
Cataract formation is well documented after significant electrical injury, and this occurs days to years later.1
Respiratory effects
Electrical burns may cause many respiratory complications, such as rib fractures, pulmonary contusions, unilateral or bilateral hydrothorax, haemothorax, or pneumothorax. Pneumothorax as an immediate complication of electrical burn injury is a rare entity and indicates severe injury with pulmonary contusion; more often, it develops 2 days after electrical injury.1 2 Pneumothorax is usually ipsilateral to the site of the electrical injury as the chest wall and the lung come into the arc of the current, and potential differences between different parts of the body create the shear stress. The probability of pneumothorax must be considered in high-voltage electrical injuries with ports of entry on the trunk.
In our case the pneumothorax due to electrical injury resulted from the damage to the lung tissue as it would come into the arc of electrical current flow. Pus in the chest can be a result of secondary infection in the pleural cavity after the pneumothorax. The exact reason why electrical injury affected the lungs and not other organs can be ascribed to the Kouwenhoven’s factors. As in our case the patient developed pneumothorax after 3 days of electrical injury. Such patients need to be observed for 48–72 hours for delayed pneumothorax.
Learning points.
Pneumothorax must be considered in the differential diagnosis of respiratory distress in patients with electrical injuries to the limbs or trunk.
Evidence of pneumothorax after electrical injury can be delayed by 1–3 days.
Pneumothorax is usually ipsilateral to the site of the injury.
Footnotes
Contributors: AH was involved in making the diagnosis and management of the patient. He has provided guidance in writing the manuscript. MST was involved in compiling data for the manuscript and in data collection. SS was involved in managing the patient and in data collection. PNG was involved in the treatment of the patient and compiling data for the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Ceber M, Ozturk C, Baghaki S, et al. Pneumothorax due to electrical burn injury. Emerg Med J 2007;24:371–2. 10.1136/emj.2006.042978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Khan AH, Siddiqui RJ. Pneumothorax due to electrical burn. Indian J Chest Dis Allied Sci 1998;40:291–3. [PubMed] [Google Scholar]
- 3. Rai J, Jeschke MG, Barrow RE, et al. Electrical injuries: a 30-year review. J Trauma 1999;46:933–6. 10.1097/00005373-199905000-00026 [DOI] [PubMed] [Google Scholar]
- 4. Hettiaratchy S, Dziewulski P. ABC of burns: pathophysiology and types of burns. BMJ 2004;328:1427–9. 10.1136/bmj.328.7453.1427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ferreiro I, Meléndez J, Regalado J, et al. Factors influencing the sequelae of high tension electrical injuries. Burns 1998;24:649–53. 10.1016/S0305-4179(98)00082-5 [DOI] [PubMed] [Google Scholar]
- 6. Sandhir RK, Tiwari IN, Goel A. Management of electrical injuries of the abdomen. Burns 1992;18:253–5. 10.1016/0305-4179(92)90082-6 [DOI] [PubMed] [Google Scholar]
- 7. Huan-Jui Y, Chih-Yang L, Huei-Yu L, et al. Acute ischemic stroke in low-voltage electrical injury: a case report. Surg Neurol Int 2010;1:83–3. 10.4103/2152-7806.74093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fatovich DM. Delayed lethal arrhythmia after an electrical injury. Emerg Med J 2007;24:743 10.1136/emj.2007.050245 [DOI] [PMC free article] [PubMed] [Google Scholar]