Description
An 84-year-old man was admitted to our Department of Internal Medicine for exertional dyspnea.
His medical history showed he had been diagnosed with hypertensive cardiomyopathy with heart failure a few years before admission and a permanent pacemaker had also been implanted after a syncope.
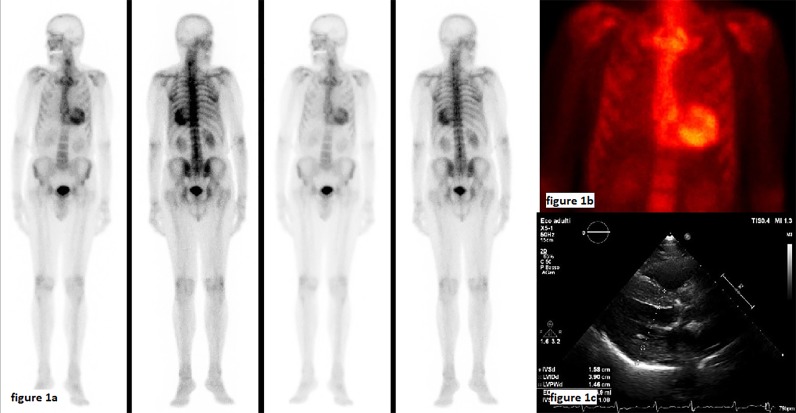
During physical examination his general condition was discrete. The patient was alert, cooperative and eupneic at rest. His blood pressure was 115/60 mm Hg, pulse rate was 68 beats/min, and respiratory rate was 12 breaths/min. Oxygen saturation was 95% in room air. Cardiac tones were attenuated without murmurs, and basal crackles were present in both lungs. Laboratory tests showed raised troponin (0.056 ng/mL, vn <0.015) and NTproBNP (2627 pg/mL; vn <450) levels. ECG showed sinus rhythm, 1st degree A-V block and left ventricle hypertrophy. Chest X-ray was not significant. Echocardiography showed severe left ventricular concentric hypertrophy with sparkling myocardium, mildly reduced ejection fraction with severe diastolic dysfunction (restrictive pattern), biatrial dilatation and severe aortic stenosis (AVA 0.6 cm2, 0.38 cm2/m2) with a low transvalvular gradient due to the reduced stroke volume secondary to left ventricle hypertrophy (paradoxical ’low-flow low-gradient'). Dobutamine stress echocardiography was not performed. On the basis of clinical and echocardiographic data, cardiac amyloidosis was suspected. Urinalysis, serum/urine immunofixation and bone scintigraphy were performed. The absence of proteinuria and monoclonal component excluded AL amyloidosis. 99mTc-hydroxymethylene-diphosphonate (HMDP) bone scintigraphy showed intense myocardial hyper-fixation of the radiotracer (figure 1A–C). These findings confirmed the clinical suspicion of transthyretin cardiac amyloidosis (ATTR). The patient underwent transcatheter aortic valve replacement (TAVR) without complications.
Figure 1.
(A) 99mTc-hydroxymethylene-diphosphonate bone scintigraphy showing intense myocardial hyper-fixation of the radiotracer consistent with transthyretin cardiac amyloidosis. (B) Particular of the cardiac hyper-fixation at bone scintigraphy. (C) Parasternal long-axis echocardiographic view.
Cardiac amyloidosis, particularly ATTR, represents an increasing cause of heart failure.1 Moreover, retrospective studies have shown a high prevalence of ATTR among patients affected by aortic stenosis undergoing to TAVR.2 Diagnosis of ATTR was difficult until few years ago, because it required endomyocardial biopsies. At present, cardiac MRI represents a useful diagnostic technique to confirm the suspicion of cardiac amyloidosis.3 Recently, bone scintigraphy has been proposed in addition to cardiac MRI— as a novel and sensitive test for the non-biopsy diagnosis of ATTR,4 being able to differentiate ATTR from light chain (AL) amyloidosis.
Our patient showed several features of ATTR: heart failure with diastolic dysfunction, thick and sparkling ventricular wall, low QRS voltages, first degree atrio-ventricular block, previous pacemaker implant and ’low-flow low-gradient' aortic stenosis treated by TAVR.
At present, ATTR represents an under-recognised cause of heart failure. Affected patients are generally older with poor ventricular function and prognosis. Physicians, particularly the internist, should be aware of clinical characteristics of this diagnosis in order to recognise patients at risk. 99mTc-HMDP bone scintigraphy is cost-effective for identifying this ‘bony heart’ and performing a correct diagnosis,5 highly impacting the prognosis of these patients, even considering newly available drugs.
Learning points.
Cardiac amyloidosis represents an increasing and under-recognised cause of heart failure, with an increasing prevalence among elderly patients.
Suggestive symptoms can be represented by diastolic heart failure, thick and sparkling ventricular wall, low QRS voltages, first degree AVB and aortic stenosis, particularly if ‘low-flow low-gradient’.
Bone scintigraphy with 99mTc-HMDP is helpful for a non-invasive diagnosis of cardiac amyloidosis.
Acknowledgments
The authors thank Ms Caterina Mirijello for the revision of English language.
Footnotes
Contributors: AM, SC, MMD and SDC designed, wrote and reviewed the manuscript. AM and SC managed the patient during hospitalisation.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Grogan M, Scott CG, Kyle RA, et al. Natural history of wild-type transthyretin cardiac amyloidosis and risk stratification using a novel staging system. J Am Coll Cardiol 2016;68:1014–20. 10.1016/j.jacc.2016.06.033 [DOI] [PubMed] [Google Scholar]
- 2. Castaño A, Narotsky DL, Hamid N, et al. Unveiling transthyretin cardiac amyloidosis and its predictors among elderly patients with severe aortic stenosis undergoing transcatheter aortic valve replacement. Eur Heart J 2017;38:2879–87. 10.1093/eurheartj/ehx350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Agha AM, Parwani P, Guha A, et al. Role of cardiovascular imaging for the diagnosis and prognosis of cardiac amyloidosis. Open Heart 2018;5:e000881 10.1136/openhrt-2018-000881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gillmore JD, Maurer MS, Falk RH, et al. Nonbiopsy diagnosis of cardiac transthyretin amyloidosis. Circulation 2016;133:2404–12. 10.1161/CIRCULATIONAHA.116.021612 [DOI] [PubMed] [Google Scholar]
- 5. Ruiz-Negrón N, Nativi-Nicolau J, Maurer MS, et al. Cost-effectiveness of technetium pyrophosphate scintigraphy versus heart biopsy for the diagnosis of transthyretin amyloidosis. Amyloid 2019;26(sup1):71–2. 10.1080/13506129.2019.1583192 [DOI] [PubMed] [Google Scholar]