Abstract
Background
The American Cancer Society discourages the dual use of electronic cigarettes (ECs) and cigarettes because such use has not resulted in reduced exposures to the harmful effects of smoking. American Indian (AI) people have the highest prevalence of smoking and of EC use in the United States, but very little is known about dual EC and cigarette use in AI communities.
Methods
In 2016, 375 adult AI in Oklahoma who smoked cigarettes completed a survey about EC use (vaping). We describe vaping patterns, nicotine dependence, and reasons for EC use among the subset of 44 (12%) current dual EC users. To differentiate habitual EC users from occasional or merely curious users, we defined dual use as using ECs on some days or every day in the past 30 days.
Results
About one-third of dual users vaped ten or more times daily. About two-thirds used a tank product. Eleven percent used ECs without nicotine and another 9% were unsure of the nicotine content. A minority (40%) enjoyed vaping more than smoking, and most (76%) would smoke first on days they did both. Thirty-one percent vaped within 5 min of waking and another 24% within 30 min. Although the two-item heaviness of use index did not differ significantly between smoking and vaping, the ten-item Penn State Dependence Index (PSDI) suggested greater dependence on smoking than vaping (11.02 vs. 6.42, respectively; p < .0001). The most common reasons for vaping were to reduce smoking (79%), enjoyment of flavors (78%), and ability to vape where smoking is not allowed (73%). Perceptions of less harm to others (69%) or to self were the next most common (65%). Fewer than half used ECs to reduce stress, for affordability, or because others used them.
Conclusions
Nearly 20% of dual users used ECs either without nicotine or without knowing if the product contained nicotine. The PSDI indicated greater dependence on smoking than vaping. Reasons for vaping were nearly equal between smoking reduction and enjoying flavors. Understanding patterns of dual use will inform future efforts to address nicotine dependence for AI communities with high prevalence of smoking.
Keywords: Electronic cigarettes, Smoking, American Indian, Adult, Tobacco use
Introduction
The prevalence of smoking in the U.S. is decreasing [1] and the prevalence of electronic cigarette (EC) use increasing [2]. Many individuals use ECs, or vape, in effort to reduce or quit smoking [3–5]. While complete substitution of ECs for cigarettes has been associated with smoking cessation [6, 7], concomitant or “dual” use of ECs and cigarettes has not [8], and dual use is now the most common form of EC use [9]. Further, dual use has not been shown to reduce exposure to the harmful products of combustible cigarettes, including carcinogens [10–18]. The American Cancer Society, as a result, strongly discourages the dual use of EC and cigarettes [19]. Additionally, recent evidence suggests that frequent vaping itself carries increased risk of cardiovascular disease [20, 21], and newer generation EC devices can achieve nicotine levels comparable or exceeding those of conventional cigarettes [22], increasing the potential for adverse effects from nicotine.
The American Indian (AI) population in general has a very high smoking prevalence, particularly in the Plains states [23–26]. AI people also have the highest prevalence of EC use of any single-race group in the U.S. [27, 28]. However, use of EC by AI who smoke has been reported only rarely [29, 30], and the patterns and preferences of EC use among AI dual users, never. We now describe patterns, EC dependence, and preferences by focusing on the dual user subset, defined as people who smoked cigarettes and used ECs on some days or every day of the past 30 days. This common definition [31] minimizes the inclusion of people who merely experimented with ECs once or twice, and allows focus on persons with more habitual EC use.
Methods
The “Vaping among Smokers: A Cherokee Nation Cohort Study” was designed to provide estimates of the prevalence and patterns of EC use among adult AI smokers and has been described in detail elsewhere [30]. Briefly, in 2016 we recruited 375 adult AI men and women, who smoke, at a large Cherokee Nation Health Services outpatient facility in northeastern Oklahoma to participate in the study. Eligibility for services includes proof of AI or Alaska Native (AN) descent, such as a Certificate of Degree of Indian Blood (CDIB), from a federally recognized AI or Alaska Native tribe or community. Eligibility to participate in the cohort included being age 18 years or older, smoking at least 100 cigarettes in one’s lifetime, smoking in the past 30 days, and answering “yes” to both “Are you American Indian?” and “Do you have a CDIB card?”
Participants completed a survey including patterns of smoking and EC use. The current cross-sectional descriptive analysis is limited to the subset of dual users as defined below.
Measures
All participants reported whether they ever used ECs, and if so, whether they used any in the past 30 days [30]. Among these, dual users were defined as using EC on some days or every day within the past 30 days. This definition of dual use reduces the chance of including persons whose vaping was limited to curiosity or brief experimentation [31].
Vaping measures
Dual users reported how many times per day they used an EC (categorized as: less than 5, 5–9, 10–14, 15–19, 20–29, or 30 or more), which type of product most often used (cigalike, tank, mods, other), whether their e-liquid contained nicotine (yes, no, don’t know/not sure) and the nicotine content of their usual EC product (0 mg, 1–12 mg, 13–17 mg, 18+ mg, don’t know/not sure). Dual users also reported whether they enjoyed vaping more than smoking, and whether they use EC vs a cigarette first on days they use both.
Vaping dependence and smoking dependence were separately assessed using the Heaviness of Vaping Index [32], Heaviness of Smoking Index [33] and the Penn State Dependence Index (PSDI) for vaping or smoking [32] as adapted slightly for this study (Appendix). The Heaviness of Vaping and Heaviness of Smoking indices are two-item measures of nicotine dependence for EC users and smokers, respectively. The PSDI for vaping and PSDI for smoking are 10-item indices to measure dependence on vaping or smoking, respectively. Cases with any missing component of the index were excluded from the scoring to reduce bias towards low dependence [32].
Participants indicated one or more reasons for using ECs, including to reduce cigarette smoking, liking the flavors, using when smoking is not allowed, less harmful to self than smoking, less harmful to others than smoking, reducing stress, better affordability, and/or other people important to them use ECs, or other (write in).
Analysis
Categorical data are represented by count (percent). Continuous data are represented using the mean (SD). Dependence scales were assessed for normality using the Shapiro-Wilk test and visual confirmation via quantile-quantile plots, then compared between vaping and smoking using paired t-tests with complete case analysis. The Shapiro-Wilk test is a commonly-applied method to assess normality assumptions underlying parametric statistical procedures [34, 35]. All analyses were performed using SAS software v9.4 and R v3.5.1.
Results
Of the 375 enrolled participants, 44 (12%) were dual users, defined as using ECs on some or all of the past 30 days.
Table 1 shows that among dual users, about one-third vaped 10 or more times a day, and less than one-half vaped fewer than 5 times per day. “Cigalikes” were the least frequently used product and tank systems were the most frequently used product. While 80% indicated that their e-liquid contained nicotine, 11% used e-liquid without nicotine, and 9% were unsure or did not know if their e-liquid contained nicotine. The most frequently reported nicotine content was 12 mg or less, but 14% did not know the nicotine concentration. More than half did not find vaping more enjoyable than smoking and most reported smoking before vaping on days they did both.
Table 1.
Vaping patterns and preferences, American Indian EC dual users (N = 44)
| Frequency | |
|---|---|
| Frequency of EC use per day | |
| Less than 5 times per day | 46% |
| 5–9 times per day | 20% |
| 10 or more times per day | 34% |
| Type of EC product used most often | |
| Cigalike | 12% |
| Tank | 68% |
| Mods | 18% |
| Other | 2% |
| E-liquid contains nicotine | |
| Yes | 80% |
| No | 11% |
| Don’t know/Not sure | 9% |
| Usual E-liquid nicotine content | |
| 0 mg | 7% |
| 1–12 mg | 39% |
| 13–17 mg | 18% |
| 18 or more mg | 23% |
| Don’t know/Not sure | 14% |
| Enjoy vaping more than smoking | |
| Yes | 40% |
| No | 60% |
| On vaping days, which is used first | |
| Cigarette | 76% |
| EC | 24% |
EC Electronic Cigarette
Vaping and smoking dependence item measures and scales are shown in Table 2. Although 76% reported smoking before vaping as noted above, vaping or smoking within the first 5 min of waking was not infrequent for either habit (31% and 24%, respectively), and cumulatively, the frequency of vaping or smoking within 30 min of waking was the same (55%). Individual measures show more dependence on smoking than vaping. Heaviness of vaping index and heaviness of smoking index did not differ significantly among the dual users (p = 0.22), but the mean PSDI dependence score for vaping was significantly lower than that for smoking (6.4 +/− 4.8 vs 11.0 +/− 5.0, respectively; p < .0001). Results were unchanged when median values of the PSDI were compared via the Wilcoxon signed-rank test (6 vs 11, p < .0001).
Table 2.
Vaping dependence and smoking dependence measures among adult AI dual EC and cigarette users (N = 44)
| Vaping Dependence Measures | % | Smoking Dependence Measures | % | |||
|---|---|---|---|---|---|---|
| Minutes after waking use first EC | Minutes after waking use first cigarette | |||||
| 5 or less | 31% | 5 or less | 24% | |||
| 6–30 | 24% | 6–30 | 31% | |||
| 31–120 | 24% | 31–120 | 38% | |||
| 121+ | 21% | 121+ | 7% | |||
| Nights per week wake to use EC | Nights per week wake to smoke | |||||
| Never/less than weekly | 73% | Never/less than weekly | 54% | |||
| 1 to 2 | 12% | 1 to 2 | 23% | |||
| 3 or more | 15% | 3 or more | 23% | |||
| Continue using EC because hard to quit | Continue to smoke because hard to quit | |||||
| Yes | 44% | Yes | 80% | |||
| No | 56% | No | 20% | |||
| Ever have strong cravings to use EC | Ever have strong cravings to smoke | |||||
| Yes | 33% | Yes | 84% | |||
| No | 67% | No | 16% | |||
| How strong were urges to vape, past week | How strong were urges to smoke in past week | |||||
| None | 44% | None | 0% | |||
| Slight | 34% | Slight | 18% | |||
| Moderate | 10% | Moderate | 25% | |||
| Very/extremely strong | 22% | Very/extremely strong | 57% | |||
| Hard to keep from using EC | Hard to keep from smoking | |||||
| Yes | 36% | Yes | 58% | |||
| No | 64% | No | 42% | |||
| WHEN HAVE NOT USED [EC; tobacco] for a while OR when you tried to stop [vaping; smoking] … | ||||||
| Irritable because can’t use EC | Irritable because can’t smoke | |||||
| Yes | 32% | Yes | 73% | |||
| No | 68% | No | 27% | |||
| Nervous because can’t vape | Nervous because can’t smoke | |||||
| Yes | 32% | Yes | 66% | |||
| No | 68% | No | 34% | |||
| Composite Dependence Scores | p-value* | |||||
| Heaviness of Vaping Index [32] | Mean (SD) | 2.07 (1.76) | Heaviness of Smoking Index [33] | Mean (SD) | 2.36 (1.66) | .2155 |
| PSDI-EC [32] | Mean (SD) | 6.42 (4.84) | PSDI-smoking [32] | Mean (SD) | 11.02 (5.00) | <.0001 |
EC Electronic Cigarette
PSDI Penn State Dependence Index
Missing = 10 for Heaviness of Vaping Index, 12 for PSDI-EC, 2 for Heaviness of Smoking Index, and 3 for PSDI-smoking
*Paired t-test on the differences between the vaping dependence scores and smoking dependence scores
Reasons for vaping are shown in Fig. 1. The top three most commonly endorsed reasons for vaping were to cut down on smoking, liking EC flavors, and being able to vape in places wherein smoking is not allowed. Perceiving less harm to others or to oneself compared with smoking were the next most frequent responses. Less than one-half endorsed using EC to reduce stress, reduce cost, or because other persons important to them used EC. Other reasons (write in) for EC use were endorsed by only two (4.5%) participants.
Fig. 1.
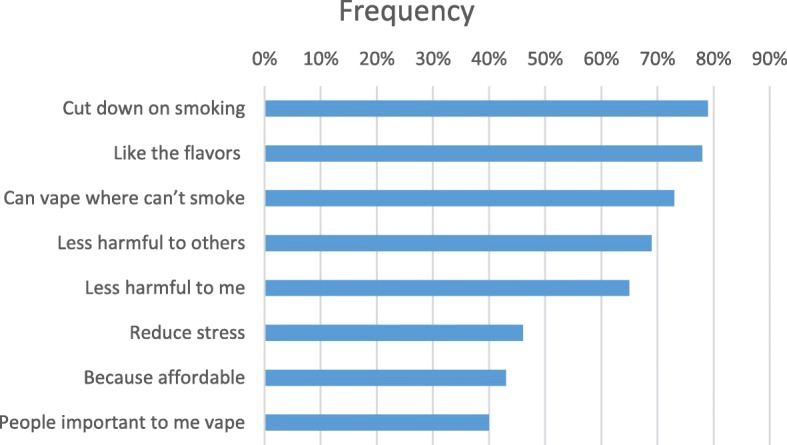
Reasons for vaping among American Indian dual EC and cigarette users
Discussion
In this cohort of adult AI persons who smoke, the prevalence of dual use, defined as using EC on some or all of the past 30 days, was 12%. This definition of dual use is similar to other longitudinal studies [7, 36] and helps to exclude recent experimenters or infrequent users [31]. Other studies vary widely in estimates of prevalence of dual use by smokers. In a 2014 study, nearly 52% of a cohort of smokers used ECs either daily or more than just a few days [7]. However, in a 2013 study, prevalence of EC use more than 50 times during lifetime was only 3.8% among smokers [37] and among current smokers in the Current Population Survey in 2014, regular EC use among smokers was 3.6% [38]. Definitions of dual use may vary enough to limit our ability to directly compare prevalence estimates between different cohorts, and the rapid rise in EC use also limits comparison with older studies. Standardized definitions of dual use will be useful in future studies.
Vaping patterns
Vaping 10 or more times per day was reported by one-third of the dual users. Very few studies report on the frequency of vaping by dual users, and often use different measures [39]. Given the continued debate regarding utility of EC in smoking cessation [40] and evidence of no clear benefit of dual EC and cigarette use [17], frequency of vaping needs more exploration by this group of smokers. Again, standardization of measures of vaping frequency will help in comparing future studies.
First generation (cigalike) ECs were the least often used products and the second-generation “tank” products the most often used. Second- and third-generation products allow users to customize their product, unlike the first generation cigalikes [41], in ways that likely improve the nicotine delivery [22, 42].
Nicotine content of vaping products among dual users
While the majority of participants used ECs that contained nicotine, nearly 20% either did not or were unsure if they did. In another study, of 399 adult EC users who were current smokers in 2015, 337 (80.7%) used EC containing nicotine, with 19% not [43]. While many smokers who also use ECs do so to reduce smoking, several EC users did not know the nicotine content of their EC product, or even if the product contained nicotine. If ECs are to replace, rather than supplement combustible cigarettes, nicotine content may be an important factor.
Measures of EC dependence
Measures of EC dependence were relatively low compared to measures of cigarette dependence among these dual users, similar to findings in other studies [32, 39, 44, 45]. In our study, all participants were current smokers at baseline, so EC dependence among these dual users are not directly comparable to studies of exclusive EC uses. In addition, a relatively higher proportion of dual EC users had missing data for the vaping dependence scales, but the effect of this potential bias is unclear. Smoking dependence questions preceded vaping dependence questions in our survey and the similarity in questions and format may have confused participants. Whether ECs had reduced these respondents’ dependence on cigarettes could not be assessed in this study.
Reasons for vaping
Flavoring was the most often endorsed reason for vaping. The impact of flavoring has never been reported for AI who smoke and use ECs. The role of flavoring in use of EC products is of increasing interest. A recent study found that flavors influenced nicotine exposure through flavor liking, but also contributed to heart rate acceleration, and nicotine titration [46]. In the US, sales of flavored EC products have greatly increased, including in Oklahoma [47]. In one study, adult smokers’ interest in flavored EC was modest, but among the smokers who also use ECs, EC use was most affected by flavor [48]. In contrast, flavoring was only infrequently (14.7%) cited as a reason for EC use by current smokers in a national survey [5].
Other than using EC to stop smoking, the convenience of vaping in places where smoking was not allowed was another leading reason for vaping. More than half cited their perception of EC being less harmful to others, and stress, affordability, or others’ vaping were among the least common. Reasons for dual use of EC among smokers usually include desire to quit smoking [49, 50], and perceptions of less harm than cigarettes [49, 51], but other factors are less frequently assessed.
Limitations
A small, convenience and clinic-based sample limits our study. In addition, patterns of tobacco use vary across AI communities in the US, and findings from this study may not reflect use in other regions. Nonetheless, this pilot study took place in a region with high prevalence of tobacco use and provides a unique snapshot of AI dual users and their vaping habits. Larger, population based studies will greatly help to elucidate regional differences in the effects of ECs upon the smoking habits of AI people. As EC technology continues to evolve rapidly, the types of EC products used in 2016 may not reflect currently used EC products. Follow up studies are needed to assess changes in use over time.
Acknowledgements
The authors acknowledge Ms. Gloria Tallbull, research staff at the University of Oklahoma, and the staff at Cherokee Nation Health Services for their assistance in carrying out this project.
Abbreviations
- AI
American Indian
- AN
Alaska Native
- CDIB
Certificate of Degree of American Indian or Alaska Native Blood
- EC
electronic cigarette
- US
United States
Appendix
The Penn State Electronic Cigarette Dependence Index [32] as adapted for this study.
How many times per day do you usually use your electronic cigarette? (Scoring: 0–4 times/day = 0, 5–9 = 1, 10–14 = 2, 15–19 = 3, 20–29 = 4, 30+ = 5),
How soon after you wake up do you first use your e-cig or vape? (Scoring: 0–5 min = 5, 6–15 = 4, 16–30 = 3, 31–60 = 2, 61–120 = 1, 121+ = 0),
Do you sometimes awaken at night to vape or use your e-cig? (Yes = 1, No = 0),
How many nights per week do you typically wake up to vape or use your e-cig? I never wake up at night to vape, less than one night per week, 1 night per week, 2 nights per week, 3 nights per week, 4 or more nights per week. (Scoring 0–1 nights = 0, 2–3 nights = 1, 4+ nights = 2)
Do you vape or use an e-cig now because it is really hard to quit? (Yes = 1, No = 0)
Do you ever have strong cravings to use an e-cig or vape? (Yes = 1, No = 0)
Over the past week, how strong have the urges to vape or use an e-cig been? None, slight, moderate, strong, very strong, extremely strong. (Scoring: None/slight = 0, Moderate/Strong = 1, Very Strong/Extremely strong = 2)
Is it hard to keep from using an e-cig or vaping in places where you are not supposed to, such as restaurants, hospital/clinics, or other public areas? (Yes = 1, No = 0)
When you haven’t used an e-cig or vaped for a while or when you tried to stop … Did you feel more irritable because you couldn’t vape or use an e-cig? (Yes = 1, No = 0)
When you haven’t used an e-cig or vaped for a while or when you tried to stop … Did you feel nervous, restless, or anxious because you couldn’t vape or use an e-cig? (Yes = 1, No = 0)
Authors’ contributions
DAR co-designed the study, contributed to analysis and interpretation of the data, drafted and revised the manuscript. AC co-designed the study and was a major contributor to the writing of the manuscript. JD and KD conducted the majority of analyses, were major contributors to the interpretation of the data, and contributed to the writing of the manuscript. MH collected the data and contributed to the design of the study. PS acquired funding support and contributed to the writing of the manuscript. TW contributed to the design of the study, interpretation of the data, and writing of the manuscript. MD was a major contributor to the design of the study, interpretation of the data, and writing of the manuscript. All authors read and approved the final manuscript.
Funding
Grants from the National Cancer Institute of the National Institutes of Health (P20CA202921 to University of Oklahoma, and 5P20CA202923 to Cherokee Nation) supported this study. The funding body had no role in the design of the study and collection, analysis, interpretation of data, or writing the manuscript. Content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health or of Cherokee Nation.
Availability of data and materials
The data that support the findings are available from Cherokee Nation, but restrictions apply to the availability of these data. These data were used under agreement for the current study, and are not publicly available. Data are, however, available from the authors but only with explicit permission of Cherokee Nation.
Ethics approval and consent to participate
The Cherokee Nation Institutional Review Board and the University of Oklahoma Health Sciences Center Institutional Review Board (IRB case number 5970) approved this study. All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Dorothy A. Rhoades, Phone: 405-271-4778, Email: Dorothy-Rhoades@ouhsc.edu
Ashley L. Comiford, Email: ashley-comiford@cherokee.org
Justin D. Dvorak, Email: Justin-Dvorak@ouhsc.edu
Kai Ding, Email: Kai-Ding@ouhsc.edu.
Michelle Hopkins, Email: Michelle-Hopkins@ouhsc.edu.
Paul Spicer, Email: paul.spicer@ou.edu.
Theodore L. Wagener, Email: theodore-wagener@ouhsc.edu
Mark P. Doescher, Email: Mark-Doescher@ouhsc.edu
References
- 1.Jamal Ahmed, King Brian A., Neff Linda J., Whitmill Jennifer, Babb Stephen D., Graffunder Corinne M. Current Cigarette Smoking Among Adults — United States, 2005–2015. MMWR. Morbidity and Mortality Weekly Report. 2016;65(44):1205–1211. doi: 10.15585/mmwr.mm6544a2. [DOI] [PubMed] [Google Scholar]
- 2.King B. A., Patel R., Nguyen K. H., Dube S. R. Trends in Awareness and Use of Electronic Cigarettes Among US Adults, 2010-2013. Nicotine & Tobacco Research. 2014;17(2):219–227. doi: 10.1093/ntr/ntu191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McMillen Robert C., Gottlieb Mark A., Shaefer Regina M. Whitmore, Winickoff Jonathan P., Klein Jonathan D. Trends in Electronic Cigarette Use Among U.S. Adults: Use is Increasing in Both Smokers and Nonsmokers. Nicotine & Tobacco Research. 2014;17(10):1195–1202. doi: 10.1093/ntr/ntu213. [DOI] [PubMed] [Google Scholar]
- 4.Patel Deesha, Davis Kevin C., Cox Shanna, Bradfield Brian, King Brian A., Shafer Paul, Caraballo Ralph, Bunnell Rebecca. Reasons for current E -cigarette use among U.S. adults. Preventive Medicine. 2016;93:14–20. doi: 10.1016/j.ypmed.2016.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rutten Lila J. Finney, Blake Kelly D., Agunwamba Amenah A., Grana Rachel A., Wilson Patrick M., Ebbert Jon O., Okamoto Janet, Leischow Scott J. Use of E-Cigarettes Among Current Smokers: Associations Among Reasons for Use, Quit Intentions, and Current Tobacco Use. Nicotine & Tobacco Research. 2015;17(10):1228–1234. doi: 10.1093/ntr/ntv003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhu SH, Zhuang YL, Wong S, Cummins SE, Tedeschi GJ. E-cigarette use and associated changes in population smoking cessation: evidence from US current population surveys. BMJ. 2017;358:j3262. doi: 10.1136/bmj.j3262. PubMed PMID: 28747333; PMCID: PMC5526046. [DOI] [PMC free article] [PubMed]
- 7.Biener L., Hargraves J. L. A Longitudinal Study of Electronic Cigarette Use Among a Population-Based Sample of Adult Smokers: Association With Smoking Cessation and Motivation to Quit. Nicotine & Tobacco Research. 2014;17(2):127–133. doi: 10.1093/ntr/ntu200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weaver Scott R., Huang Jidong, Pechacek Terry F., Heath John Wesley, Ashley David L., Eriksen Michael P. Are electronic nicotine delivery systems helping cigarette smokers quit? Evidence from a prospective cohort study of U.S. adult smokers, 2015–2016. PLOS ONE. 2018;13(7):e0198047. doi: 10.1371/journal.pone.0198047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mirbolouk Mohammadhassan, Charkhchi Paniz, Kianoush Sina, Uddin S.M. Iftekhar, Orimoloye Olusola A., Jaber Rana, Bhatnagar Aruni, Benjamin Emelia J., Hall Michael E., DeFilippis Andrew P., Maziak Wasim, Nasir Khurram, Blaha Michael J. Prevalence and Distribution of E-Cigarette Use Among U.S. Adults: Behavioral Risk Factor Surveillance System, 2016. Annals of Internal Medicine. 2018;169(7):429. doi: 10.7326/M17-3440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pasquereau Anne, Guignard Romain, Andler Raphaël, Nguyen-Thanh Viêt. Electronic cigarettes, quit attempts and smoking cessation: a 6-month follow-up. Addiction. 2017;112(9):1620–1628. doi: 10.1111/add.13869. [DOI] [PubMed] [Google Scholar]
- 11.Al-Delaimy Wael K., Myers Mark G., Leas Eric C., Strong David R., Hofstetter C. Richard. E-Cigarette Use in the Past and Quitting Behavior in the Future: A Population-Based Study. American Journal of Public Health. 2015;105(6):1213–1219. doi: 10.2105/AJPH.2014.302482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grana Rachel A., Popova Lucy, Ling Pamela M. A Longitudinal Analysis of Electronic Cigarette Use and Smoking Cessation. JAMA Internal Medicine. 2014;174(5):812. doi: 10.1001/jamainternmed.2014.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kalkhoran Sara, Glantz Stanton A. E-cigarettes and smoking cessation in real-world and clinical settings: a systematic review and meta-analysis. The Lancet Respiratory Medicine. 2016;4(2):116–128. doi: 10.1016/S2213-2600(15)00521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manzoli Lamberto, Flacco Maria Elena, Fiore Maria, La Vecchia Carlo, Marzuillo Carolina, Gualano Maria Rosaria, Liguori Giorgio, Cicolini Giancarlo, Capasso Lorenzo, D'Amario Claudio, Boccia Stefania, Siliquini Roberta, Ricciardi Walter, Villari Paolo. Electronic Cigarettes Efficacy and Safety at 12 Months: Cohort Study. PLOS ONE. 2015;10(6):e0129443. doi: 10.1371/journal.pone.0129443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brose Leonie S., Hitchman Sara C., Brown Jamie, West Robert, McNeill Ann. Is the use of electronic cigarettes while smoking associated with smoking cessation attempts, cessation and reduced cigarette consumption? A survey with a 1-year follow-up. Addiction. 2015;110(7):1160–1168. doi: 10.1111/add.12917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berg Carla J., Barr Dana Boyd, Stratton Erin, Escoffery Cam, Kegler Michelle. Attitudes toward E-Cigarettes, Reasons for Initiating E-Cigarette Use, and Changes in Smoking Behavior after Initiation: A Pilot Longitudinal Study of Regular Cigarette Smokers. Open Journal of Preventive Medicine. 2014;04(10):789–800. doi: 10.4236/ojpm.2014.410089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shahab Lion, Goniewicz Maciej L., Blount Benjamin C., Brown Jamie, McNeill Ann, Alwis K. Udeni, Feng June, Wang Lanqing, West Robert. Nicotine, Carcinogen, and Toxin Exposure in Long-Term E-Cigarette and Nicotine Replacement Therapy Users. Annals of Internal Medicine. 2017;166(6):390. doi: 10.7326/M16-1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fagan Pebbles, Pokhrel Pallav, Herzog Thaddeus A, Moolchan Eric T, Cassel Kevin D, Franke Adrian A, Li Xingnan, Pagano Ian, Trinidad Dennis R, Sakuma Kari-lyn K, Sterling Kymberle, Jorgensen Dorothy, Lynch Tania, Kawamoto Crissy, Guy Mignonne C, Lagua Ian, Hanes Sarah, Alexander Linda A, Clanton Mark S, Graham-Tutt Camonia, Eissenberg Thomas. Sugar and Aldehyde Content in Flavored Electronic Cigarette Liquids. Nicotine & Tobacco Research. 2017;20(8):985–992. doi: 10.1093/ntr/ntx234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American Cancer Society. American Cancer Society Position Statement on Electronic Cigarettes. 2018. https://www.cancer.org/healthy/stay-away-from-tobacco/e-cigarette-position-statement.html. Accessed 3 July 2018.
- 20.Alzahrani Talal, Pena Ivan, Temesgen Nardos, Glantz Stanton A. Association Between Electronic Cigarette Use and Myocardial Infarction. American Journal of Preventive Medicine. 2018;55(4):455–461. doi: 10.1016/j.amepre.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olfert I. Mark, DeVallance Evan, Hoskinson Hannah, Branyan Kayla W., Clayton Stuart, Pitzer Christopher R., Sullivan D. Patrick, Breit Matthew J., Wu Zhongxin, Klinkhachorn Powsiri, Mandler W. Kyle, Erdreich Brett H., Ducatman Barbara S., Bryner Randall W., Dasgupta Piyali, Chantler Paul D. Chronic exposure to electronic cigarettes results in impaired cardiovascular function in mice. Journal of Applied Physiology. 2018;124(3):573–582. doi: 10.1152/japplphysiol.00713.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wagener Theodore L, Floyd Evan L, Stepanov Irina, Driskill Leslie M, Frank Summer G, Meier Ellen, Leavens Eleanor L, Tackett Alayna P, Molina Neil, Queimado Lurdes. Have combustible cigarettes met their match? The nicotine delivery profiles and harmful constituent exposures of second-generation and third-generation electronic cigarette users. Tobacco Control. 2016;26(e1):e23–e28. doi: 10.1136/tobaccocontrol-2016-053041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garrett BE, Dube SR, Winder C, Caraballo RS, et al. Cigarette smoking - United States, 2006-2008 and 2009-2010. MMWR Suppl 2013;62(3):81–84. PubMed PMID: 24264495. [PubMed]
- 24.Martell Brandi N., Garrett Bridgette E., Caraballo Ralph S. Disparities in Adult Cigarette Smoking — United States, 2002–2005 and 2010–2013. MMWR. Morbidity and Mortality Weekly Report. 2016;65(30):753–758. doi: 10.15585/mmwr.mm6530a1. [DOI] [PubMed] [Google Scholar]
- 25.Cobb Nathaniel, Espey David, King Jessica. Health Behaviors and Risk Factors Among American Indians and Alaska Natives, 2000–2010. American Journal of Public Health. 2014;104(S3):S481–S489. doi: 10.2105/AJPH.2014.301879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eichner June E., Cravatt Kymberly, Beebe Laura A., Blevins Kathleen S., Stoddart Martha L., Bursac Zoran, Yeh Fawn, Lee Elisa T., Moore William E. Tobacco Use among American Indians in Oklahoma: An Epidemiologic View. Public Health Reports. 2005;120(2):192–199. doi: 10.1177/003335490512000214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kasza Karin A., Ambrose Bridget K., Conway Kevin P., Borek Nicolette, Taylor Kristie, Goniewicz Maciej L., Cummings K. Michael, Sharma Eva, Pearson Jennifer L., Green Victoria R., Kaufman Annette R., Bansal-Travers Maansi, Travers Mark J., Kwan Jonathan, Tworek Cindy, Cheng Yu-Ching, Yang Ling, Pharris-Ciurej Nikolas, van Bemmel Dana M., Backinger Cathy L., Compton Wilson M., Hyland Andrew J. Tobacco-Product Use by Adults and Youths in the United States in 2013 and 2014. New England Journal of Medicine. 2017;376(4):342–353. doi: 10.1056/NEJMsa1607538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schoenborn CA, Gindi RM. Electronic cigarette use among adults: United States, 2014. NCHS Data Brief 2015(217):1–8. Epub 2015/11/12. PubMed PMID: 26555932. [PubMed]
- 29.Carroll Dana Mowls, Wagener Theodore L, Thompson David M, Stephens Lancer D, Peck Jennifer D, Campbell Janis E, Beebe Laura A. Electronic nicotine delivery system use behaviour and loss of autonomy among American Indians: results from an observational study. BMJ Open. 2017;7(12):e018469. doi: 10.1136/bmjopen-2017-018469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Comiford Ashley L., Rhoades Dorothy A., Spicer Paul, Ding Kai, Dvorak Justin D., Driskill Leslie, Wagener Theodore L., Doescher Mark P. E-cigarettes and Tobacco Exposure Biomarkers among American Indian Smokers. American Journal of Health Behavior. 2018;42(6):101–109. doi: 10.5993/AJHB.42.6.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Amato Michael S, Boyle Raymond G, Levy David. How to define e-cigarette prevalence? Finding clues in the use frequency distribution. Tobacco Control. 2015;25(e1):e24–e29. doi: 10.1136/tobaccocontrol-2015-052236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Foulds J., Veldheer S., Yingst J., Hrabovsky S., Wilson S. J., Nichols T. T., Eissenberg T. Development of a Questionnaire for Assessing Dependence on Electronic Cigarettes Among a Large Sample of Ex-Smoking E-cigarette Users. Nicotine & Tobacco Research. 2014;17(2):186–192. doi: 10.1093/ntr/ntu204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.HEATHERTON TODD F., KOZLOWSKI LYNN T., FRECKER RICHARD C., RICKERT WILLIAM, ROBINSON JACK. Measuring the Heaviness of Smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Addiction. 1989;84(7):791–800. doi: 10.1111/j.1360-0443.1989.tb03059.x. [DOI] [PubMed] [Google Scholar]
- 34.Flamini G, Romano G, Curigliano G, et al. 4-Aminobiphenyl-DNA adducts in laryngeal tissue and smoking habits: an immunohistochemical study. Carcinogenesis. 1998;19(2):353–357. doi: https://doi.org/10.1093/carcin/19.2.353. [DOI] [PubMed]
- 35.Shearston J, Lee L, Eazor J, et al. Effects of exposure to direct and secondhand hookah and e-cigarette aerosols on ambient air quality and cardiopulmonary health in adults and children: protocol for a panel study. BMJ Open. 2019;9:e029490. doi: 10.1136/bmjopen-2019-029490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Buu Anne, Hu Yi-Han, Piper Megan E., Lin Hsien-Chang. The association between e-cigarette use characteristics and combustible cigarette consumption and dependence symptoms: Results from a national longitudinal study. Addictive Behaviors. 2018;84:69–74. doi: 10.1016/j.addbeh.2018.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Giovenco Daniel P., Lewis M. Jane, Delnevo Cristine D. Factors Associated with E-cigarette Use. American Journal of Preventive Medicine. 2014;47(4):476–480. doi: 10.1016/j.amepre.2014.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Levy DT, Yuan Z, Li Y. The prevalence and characteristics of e-cigarette users in the U.S. Int J Environ Res Public Health. 2017;14(10). doi: 10.3390/ijerph14101200. PubMed PMID: 29019917; PMCID: PMC5664701. [DOI] [PMC free article] [PubMed]
- 39.Morean Meghan, Krishnan-Sarin Suchitra, O'Malley Stephanie S. Comparing cigarette and e-cigarette dependence and predicting frequency of smoking and e-cigarette use in dual-users of cigarettes and e-cigarettes. Addictive Behaviors. 2018;87:92–96. doi: 10.1016/j.addbeh.2018.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Glasser Allison M., Collins Lauren, Pearson Jennifer L., Abudayyeh Haneen, Niaura Raymond S., Abrams David B., Villanti Andrea C. Overview of Electronic Nicotine Delivery Systems: A Systematic Review. American Journal of Preventive Medicine. 2017;52(2):e33–e66. doi: 10.1016/j.amepre.2016.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bhatnagar Aruni, Whitsel Laurie P., Ribisl Kurt M., Bullen Chris, Chaloupka Frank, Piano Mariann R., Robertson Rose Marie, McAuley Timothy, Goff David, Benowitz Neal. Electronic Cigarettes. Circulation. 2014;130(16):1418–1436. doi: 10.1161/CIR.0000000000000107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lechner William V., Meier Ellen, Wiener Josh L., Grant DeMond M., Gilmore Jenna, Judah Matt R., Mills Adam C., Wagener Theodore L. The comparative efficacy of first- versus second-generation electronic cigarettes in reducing symptoms of nicotine withdrawal. Addiction. 2015;110(5):862–867. doi: 10.1111/add.12870. [DOI] [PubMed] [Google Scholar]
- 43.Weaver Scott R., Kemp Catherine B., Heath J. Wesley, Pechacek Terry F., Eriksen Michael P. Use of Nicotine in Electronic Nicotine and Non-Nicotine Delivery Systems by US Adults, 2015. Public Health Reports. 2017;132(5):545–548. doi: 10.1177/0033354917723597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Farsalinos KE, Romagna G, Tsiapras D, Kyrzopoulos S, Voudris V. Evaluating nicotine levels selection and patterns of electronic cigarette use in a group of "vapers" who had achieved complete substitution of smoking. Subst Abuse. 2013;7:139–146. doi: 10.4137/SART.S12756. PubMed PMID: 24049448; PMCID: PMC3772898. [DOI] [PMC free article] [PubMed]
- 45.Etter Jean-François, Eissenberg Thomas. Dependence levels in users of electronic cigarettes, nicotine gums and tobacco cigarettes. Drug and Alcohol Dependence. 2015;147:68–75. doi: 10.1016/j.drugalcdep.2014.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.St.Helen Gideon, Dempsey Delia A., Havel Christopher M., Jacob Peyton, Benowitz Neal L. Impact of e-liquid flavors on nicotine intake and pharmacology of e-cigarettes. Drug and Alcohol Dependence. 2017;178:391–398. doi: 10.1016/j.drugalcdep.2017.05.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kuiper NM, Loomis BR, Falvey KT, et al. Trends in unit sales of flavored and menthol electronic cigarettes in the United States, 2012–2016. Prev Chronic Dis. 2018;15:E105. doi: 10.5888/pcd15.170576. PubMed PMID: 30148426; PMCID: PMC6110400. [DOI] [PMC free article] [PubMed]
- 48.Shiffman Saul, Sembower Mark A, Pillitteri Janine L, Gerlach Karen K, Gitchell Joseph G. The Impact of Flavor Descriptors on Nonsmoking Teens’ and Adult Smokers’ Interest in Electronic Cigarettes. Nicotine & Tobacco Research. 2015;17(10):1255–1262. doi: 10.1093/ntr/ntu333. [DOI] [PubMed] [Google Scholar]
- 49.Pearson Jennifer L., Richardson Amanda, Niaura Raymond S., Vallone Donna M., Abrams David B. e-Cigarette Awareness, Use, and Harm Perceptions in US Adults. American Journal of Public Health. 2012;102(9):1758–1766. doi: 10.2105/AJPH.2011.300526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pulvers Kim, Hayes Rashelle B., Scheuermann Taneisha S., Romero Devan R., Emami Ashley S., Resnicow Ken, Olendzki Effie, Person Sharina D., Ahluwalia Jasjit S. Tobacco Use, Quitting Behavior, and Health Characteristics Among Current Electronic Cigarette Users in a National Tri-Ethnic Adult Stable Smoker Sample. Nicotine & Tobacco Research. 2014;17(9):1085–1095. doi: 10.1093/ntr/ntu241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pericot-Valverde Irene, Gaalema Diann E., Priest Jeff S., Higgins Stephen T. E-cigarette awareness, perceived harmfulness, and ever use among U.S. adults. Preventive Medicine. 2017;104:92–99. doi: 10.1016/j.ypmed.2017.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings are available from Cherokee Nation, but restrictions apply to the availability of these data. These data were used under agreement for the current study, and are not publicly available. Data are, however, available from the authors but only with explicit permission of Cherokee Nation.


