Abstract
A patient in his mid-40s presented with acute basilar artery thrombosis 7 hours postsymptom onset. Initial attempts to perform mechanical thrombectomy (MT) via the femoral and radial arterial approaches were unsuccessful as the left vertebral artery (VA) was occluded at its origin and the right VA terminated in the posterior inferior cerebellar artery territory, without contribution to the basilar system. MT was thus performed following ultrasound-guided direct arterial puncture of the left VA in its V3 segment, with antegrade advancement of a 4 French radial access sheath. First pass thrombolyisis in cerebral infarction (TICI) 3 recanalisation achieved with a 6 mm Solitaire stent retriever and concurrent aspiration on the 4 French sheath. Vertebral closure achieved with manual compression.
Keywords: interventional radiology, stroke
Background
Mechanical thrombectomy (MT) is an established treatment option in the management of acute ischaemic stroke, however cases with difficult access can cause significant delays to revascularisation of the target vessel.
Several novel access methods have been described in the literature, including vertebral artery (VA) puncture with retrograde recanalisation of the VA origin prior to thrombectomy. We present the first described case in which access to the posterior circulation was achieved following ultrasound (US)-guided puncture of the V3 segment of the left VA with subsequent antegrade basilar thrombectomy performed directly from the vertebral access site.
Case presentation
Patient presented following an ambulance stand-by call to the emergency department at 17:10, following symptom onset at 10:00. On examination there was right-sided weakness, right third nerve palsy, right internuclear ophthalmoplegia and dysarthria. Initial National Institutes of Health Stroke Scale (NIHSS) was 10.
Investigations
Patient had a non-contrast CT brain at 17:18 which demonstrated a hyperdense basilar artery, in keeping with acute basilar artery thrombosis (figure 1A).
Figure 1.
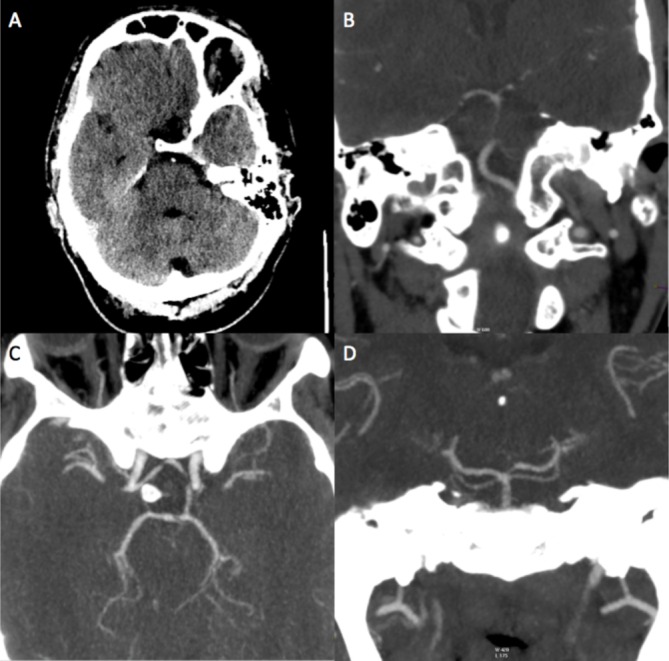
Non-contrast CT demonstrates a hyperdense basilar artery in keeping with acute thrombosis (A). Enhanced CT angiogram confirms basilar artery occlusion as well as posterior inferior cerebellar artery termination of the right vertebral artery (B). Posterior circulation was partly supplied via a patent left posterior communicating artery (C); however, the P1 segment of the left posterior cerebral artery was congenitally hypoplastic (D) meaning it was not a feasible route for thrombectomy.
CT angiography confirmed occlusive thrombus within the basilar artery, with a congenitally hypoplastic right VA not contributing to the basilar system (figure 1B).
There was some contribution to the posterior circulation via a patent left posterior communicating artery (figure 1C); however, the P1 segment of the left posterior cerebral artery (PCA) was hypoplastic and therefore not feasible as a route for thrombectomy (figure 1D).
Treatment
Patient did not receive intravenous thrombolysis due to the delayed presentation, and proceeded to MT.
Initial angiography demonstrated occlusion of the left VA origin, with distal recanalisation via anastomoses from collateral branches of the ascending cervical artery (figure 2A). These anastomoses were not of a suitable calibre to allow any useful navigation, and intra-arterial thrombolysis was not felt safe due to the delayed presentation (with associated risk of haemorrhagic transformation). Multiple attempts were made to access the left VA without success, both from right groin and left radial artery access (figure 2B,C). It was then decided the only possible access to the basilar artery would be through a direct VA puncture, and so the patient was placed under a general anaesthetic. Pre-intubation Glasgow Coma Scale (GCS) was 13.
Figure 2.
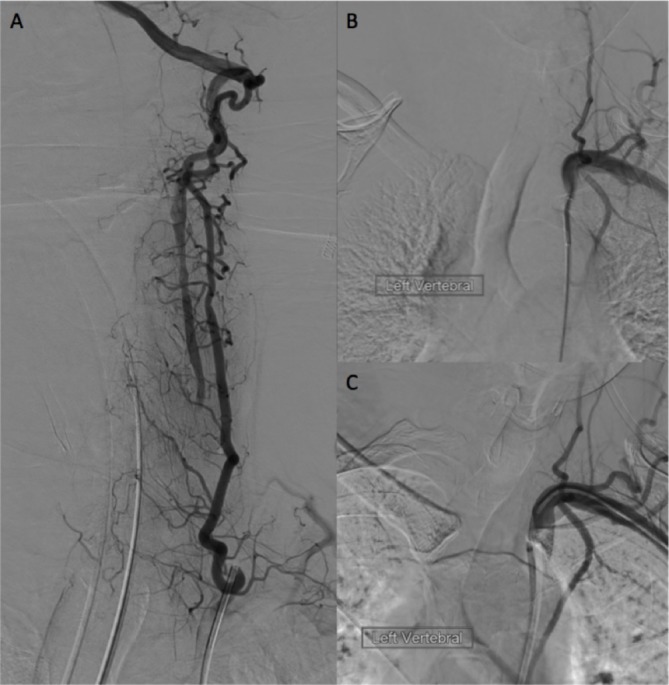
Digital subtraction angiography following injection of the left thyrocervical trunk (A) reveals distal filling of the left vertebral artery (VA) via collaterals. Despite attempts from the groin (B) and radial access sheath (C) the occluded left VA origin could not be accessed.
Using an US probe placed just below the left mastoid process, the left VA was accessed in its V3 segment with a micropuncture needle, proximal to the main collateral feeding branch (figure 3A). Through this a microwire was advanced into the basilar artery and a 4 French radial access sheath was advanced into the V3 segment (figure 3B).
Figure 3.
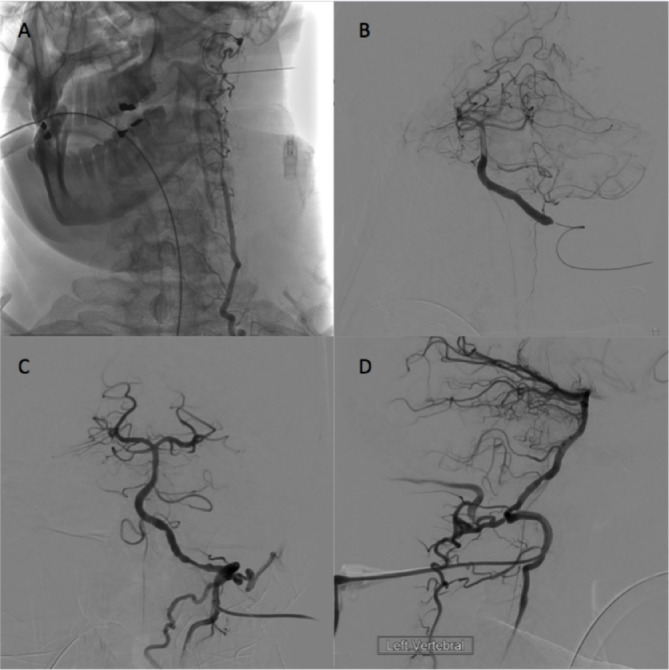
Unsubtracted digital angiography of the left thyrocervical trunk following ultrasound-guided puncture of the V3 segment of the left vertebral artery (VA) (A). Initial anteroposterior (AP) run from the VA access sheath demonstrating basilar artery thrombosis (B). AP and lateral views (C and D) following a single pass of a 6 mm Solitaire stent demonstrating thrombolyisis in cerebral infarction (TICI) 3 recanalisation of the basilar system.
An Excelsior XT-27 microcatheter (Stryker Neurovascular) and Traxcess microwire (Microvention) were advanced directly through the sheath into the P1 segment of the right PCA. A 6 mm Solitaire stent (Medtronic) was deployed across the basilar thrombus and retrieved with concurrent aspiration applied to the 4 French sheath. Following a single pass of the stent, thrombolyisis in cerebral infarction (TICI) 3 recanalisation of the basilar territory was achieved (figure 3C,D).
Our intention was to close the vertebral access site with point occlusion of the arteriotomy site using an Amplatzer plug (St Jude Medical); however on withdrawing the sheath so that it was proximal to the large collateral feeding vessel, it fell out of the VA. Haemostasis was therefore achieved following several minutes of manual compression without complication.
Outcome and follow-up
Patient was transferred to the high dependency unit for extubation and close monitoring of blood pressure. Anticoagulation with 40 mg two times per day of subcutaneous enoxaparin was given, which was changed to oral aspirin at day 1. Following postprocedural extubation GCS improved back to 15. NIHSS at day 1 had also improved to 4 (from 10).
MRI at day 1 revealed areas of infarction involving the inferior left cerebellar hemisphere, left hemipons and medial right occipital lobe without haemorrhagic transformation (figure 4A–C). MR angiography revealed persistent occlusion of the left VA origin, with distal refilling of this vessel via collaterals (figure 4D). Basilar artery was also partially supplied via the left posterior communicating artery.
Figure 4.
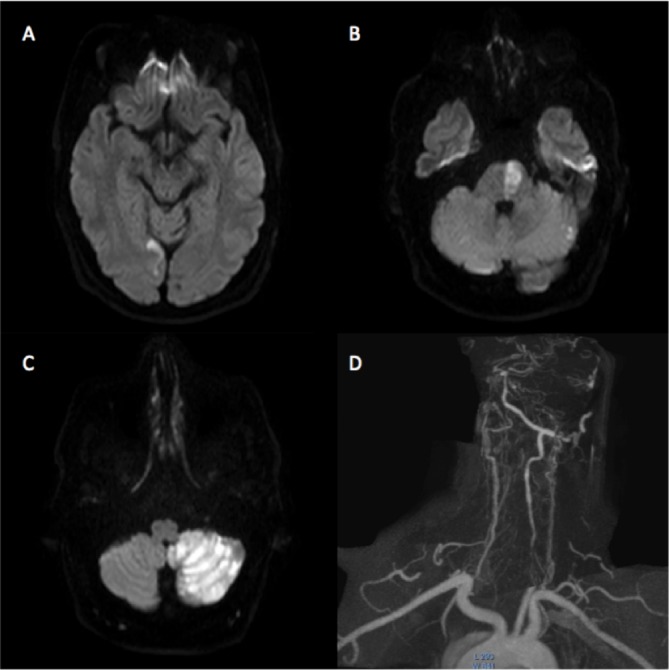
Diffusion weighted MRI sequences performed at day 1 postprocedure demonstrate areas of infarction with the medial right occipital lobe (A), left hemipons (B) and left cerebellar hemisphere (C). MR angiography confirms persistent occlusion of the left vertebral artery origin, however there is distal filling via collaterals (D).
Patient was transferred to a regional hospital on day 8 for ongoing rehabilitation. Persistent symptoms at time of transfer included right foot drop, right upper limb ataxia and intermittent episodes of diplopia.
Discussion
Stroke is the leading cause of disability in developed countries, with posterior circulation strokes accounting for approximately 20% of cases. Although there have been many advances in the treatment of acute ischaemic stroke, basilar artery occlusion remains associated with death or disability rates approaching 70%.1
Successful treatment of acute ischaemic stroke is incumbent on rapid recanalisation of the occluded vascular territory, whether this is achieved via intravenous thrombolysis, intra-arterial thrombolysis or MT.
Moniz was the first to describe direct VA puncture in the 1920s,2 with subsequent refinement in techniques over the subsequent decades before falling out of favour following the advent of non-invasive CT imaging and improved catheter angiography techniques.3–5
However, with the expansion of endovascular treatment options, alternative access methods may be required in certain cases when conventional access proves especially difficult. Several case reports have been published regarding direct VA puncture, both in the emergent treatment of acute ischaemic stroke and more electively in the management of posterior circulation aneurysms, demonstrating both the feasibility and safety of this technique in experienced hands.6–8
Our case is the first to describe direct US-guided VA puncture with subsequent basilar thrombectomy performed in an antegrade fashion from the VA access sheath. We feel that while this approach may be less eloquent, it can save time by skipping the need for recanalisation of the occluded VA origin prior to removal of the occlusive thrombus; this may be particularly useful in patients such as ours where the VA occlusion appears to be chronic and there is good collateral supply distally.
Subsequent reopening of the VA origin could then be attempted following thrombectomy, much as in the management of tandem carotid/middle cerebral artery (MCA) occlusions, or if there is good collateral supply the patient may be placed on oral anti-platelet medication as in this case.
Given the significant morbidity and mortality associated with basilar artery occlusion, aggressive approaches such as this should be considered particularly if other treatment options are not possible.9
Learning points.
Stroke is the leading cause of disability in developed countries, with basilar artery occlusion associated with death or disability rates approaching 70%.
Successful treatment of acute ischaemic stroke is incumbent on rapid recanalisation of the occluded vascular territory—time is brain!
Given the significant morbidity and mortality associated with basilar artery occlusion, more aggressive approaches such as ours may be considered in experienced hands should other treatment options prove unsuccessful.
Footnotes
Contributors: STO’R involved in the case presented, wrote up the case report and produced the figures attached as well as the discussion. IR and GS involved in the case presented and proof read the report. JMI involved in the case presented, contacted patient for consent to publish and proof read the report.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. van der Hoeven EJRJ, Schonewille WJ, Vos J, et al. The Basilar Artery International Cooperation Study (BASICS): study protocol for a randomised controlled trial. Trials 2013;14:200 10.1186/1745-6215-14-200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Artico M, Spoletini M, Fumagalli L, et al. Egas Moniz: 90 years (1927-2017) from cerebral angiography. Front Neuroanat 2017;11:81 10.3389/fnana.2017.00081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lindgren E. Percutaneous angiography of the vertebral artery. Acta Radiol 1950;33:389–404. 10.3109/00016925009133899 [DOI] [PubMed] [Google Scholar]
- 4. Mones R. Vertebral Arteriography: an evaluation of methods. Radiology 1961;76:230–6.13771994 [Google Scholar]
- 5. Scatliff JH, Mishkin MM, Hyde I. Vertebral arteriography: an evaluation of methods. Radiology 1965;85:14–22. 10.1148/85.1.14 [DOI] [PubMed] [Google Scholar]
- 6. Dorfer C, Standhardt H, Gruber A, et al. Direct percutaneous puncture approach versus surgical cutdown technique for intracranial neuroendovascular procedures: technical aspects. World Neurosurg 2012;77:192–200. 10.1016/j.wneu.2010.11.007 [DOI] [PubMed] [Google Scholar]
- 7. Desai JA, Almekhlafi MA, Hill MD, et al. Ultrasound guided V3 segment vertebral artery direct percutaneous puncture for basilar artery mechanical thrombectomy in acute stroke: a technical report. J Neurointerv Surg 2014;6:e18 10.1136/neurintsurg-2012-010601.rep [DOI] [PubMed] [Google Scholar]
- 8. Dobrocky T, Beck J, Gralla J, et al. Stent-assisted coiling of a ruptured vertebrobasilar junction aneurysm via direct vertebral artery puncture. BMJ Case Rep 2017;2017:neurintsurg-2017-013099 10.1136/bcr-2017-013099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Morales A, Parry PV, Jadhav A, et al. A novel route of revascularization in basilar artery occlusion and review of the literature. J Neurointerv Surg 2016;8:e25 10.1136/neurintsurg-2015-011723.rep [DOI] [PubMed] [Google Scholar]


