Abstract
Acute appendicitis is the most common cause of the acute abdomen syndrome and can be treated either surgically or conservatively with antibiotics. This case demonstrates the first time use of mechanics based MRI by tomoelastography with generation of quantitative maps of tissue stiffness (shear wave speed in m/s) and tissue fluidity (shear modulus loss angle, in rad) in a case of uncomplicated acute appendicitis with antibiotic treatment at (i) baseline, (ii) the end of treatment (EOT) and (iii) the 10 day follow-up after EOT. Baseline maps of stiffness and fluidity revealed to the naked eye the extent of intestinal inflammation by markedly increased values of stiffness and fluidity (2.56±0.12 m/s, 1.37±0.24 rad) compared with normal values, indicating the immediate response to antibiotic treatment at EOT (1.47±0.28 m/s, 0.80±0.11 rad) and persistent normalisation at follow-up (1.54±0.22 m/s, 0.92±0.22 rad). Tomoelastography is a non-invasive, quantitative imaging method for mechanics based characterisation and follow-up of acute appendicitis.
Keywords: radiology, infection (gastroenterology), drugs: gastrointestinal system, drug therapy related to surgery
Background
Acute appendicitis is the most common cause of acute abdomen.1 Its clinical presentation varies, from a simple or uncomplicated form with local inflammation of the appendix to complicated appendicitis with extensive inflammation leading to gangrene or abscess formation or even causing perforation.2 Open or laparoscopic appendectomy used to be the standard therapy for appendicitis. Recently, various randomised controlled trials3–8 and meta-analyses9–14 have confirmed that antibiotic administration is an effective and safe primary treatment option for early uncomplicated appendicitis. Ultrasound (US) and CT are the primary imaging modalities to diagnose acute appendicitis.15–17 However, quantification is only based on size measurements and qualitative description of morphological changes. Tomoelastography has been recently introduced as an elastography method based on MRI and provides quantitative mechanical parameters of biological soft tissues.18 19
We report a case of first time use of tomoelastography for the diagnosis of uncomplicated appendicitis and monitoring of non-operative antibiotic treatment. The case demonstrates that tomoelastography provides useful quantitative imaging markers for the detection and assessment of the extent of local intestinal inflammation.
Case presentation
A 34-year-old man with no family history of abdominal diseases or cancer presented to a physician, subspecialised in gastroenterology, with acute pain in the lower right abdomen and slight fever (37.7°C). Symptoms began 2 days earlier with undefined and dull pain in the upper abdomen and subsequent migration into the lower right abdomen. The character of the pain changed to stabbing pain within 1 day of symptom onset. Examination revealed local tenderness and slight hyperthermia in the right lower abdominal quadrant and overall paleness. There was no nausea, vomiting or diarrhoea. The patient was normotensive with a blood pressure of 120/80 mm Hg and a heart rate of 60 bpm. The Alvarado score, a clinical scoring system combining history, physical examination and laboratory tests20 with good diagnostic accuracy in men,21 was 6, suggesting uncomplicated appendicitis.
Investigations
Blood tests showed an increased C reactive protein level of 102 mg/L (reference range <5 mg/L) and an elevated leucocyte count of 10.9/nl (reference range 3.7–10.1/nl). Other standard chemical laboratory results were normal.
Standard US imaging (mylabXvision50, 3.5-MHz transducer) revealed focal, oedematous wall thickening of the appendix with surrounding fluid accumulation. The maximum appendix diameter was 7.6 mm, which is unspecific regarding the underlying pathology (figure 1). Due to the inherent limitations of US, such as restricted field of view, limited penetration depth and degradation by bowel gas artefacts, a further quantitative analysis of morphological features or elastographic examinations was not possible.
Figure 1.
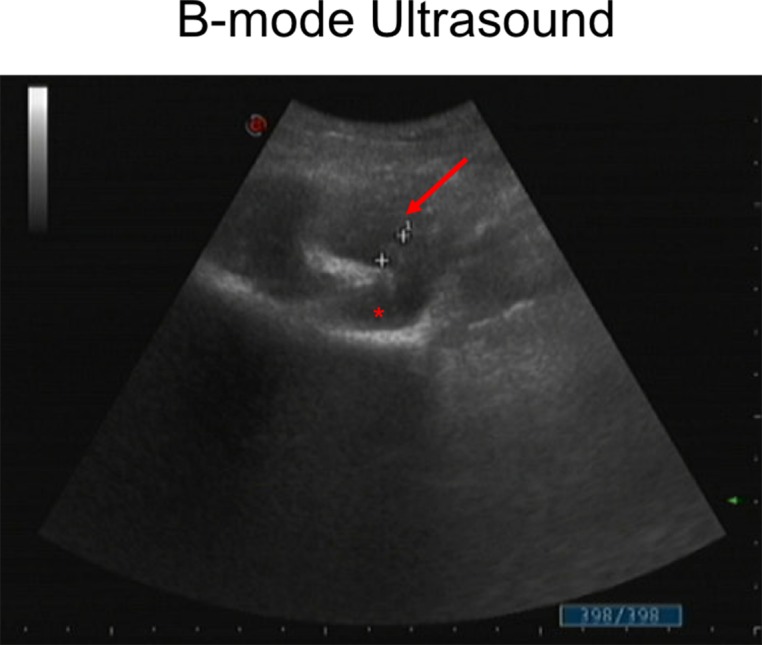
B mode ultrasound images of acute appendicitis (arrow) demonstrating focal, oedematous wall thickening with a maximum appendix diameter of 7.6 mm (white crosses) and surrounding fluid accumulation (asterisk).
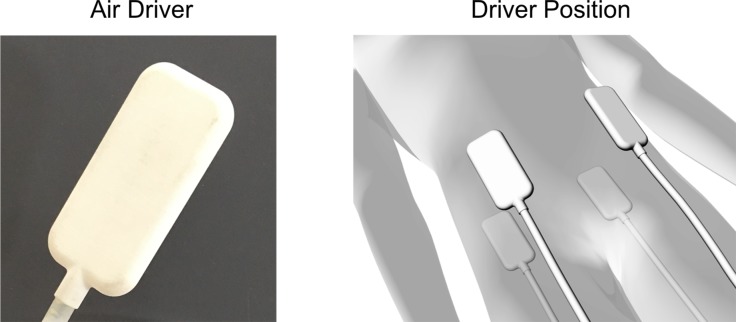
Following this diagnosis and unspecific US findings, the patient underwent an MRI examination. After standard T1 and T2 weighted MRI acquisition for anatomical correlation, we used multifrequency MRI elastography with tomoelastography postprocessing.19 The latter was performed at three time points: (i) baseline, (ii) end of treatment (EOT) and (iii) follow-up 10 days after EOT. We used four mechanical stimulation frequencies of 40, 50, 60 and 70 Hz induced by a custom made pressurised air driver, which was gently wrapped around the abdomen of the patient (see figure 2). Single shot, spin echo, echo planar imaging was performed in coronal and axial orientation at 1.5 T (Sonata, Siemens). Tomoelastography provides full field of view maps of shear wave speed (SWS in m/s) as a surrogate of stiffness as well as the loss angle of the complex shear modulus (φ in rad). φ is related to the solid–fluid behaviour of the tissue and potentially important in any disease associated with water accumulation or oedema. Since larger values (φ >0.78) are considered to be dominated by fluid tissue properties, φ is also referred to as ’fluidity'. The total acquisition time of the tomoelastography scan was 4 min with the patient breathing normally.
Figure 2.
Left: Example of a custom made pressurised air driver. Right: Driver position around the lower abdomen, two anterior (white) and two posterior (grey).
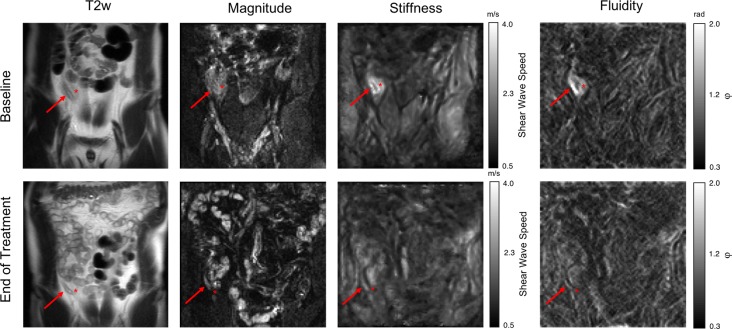
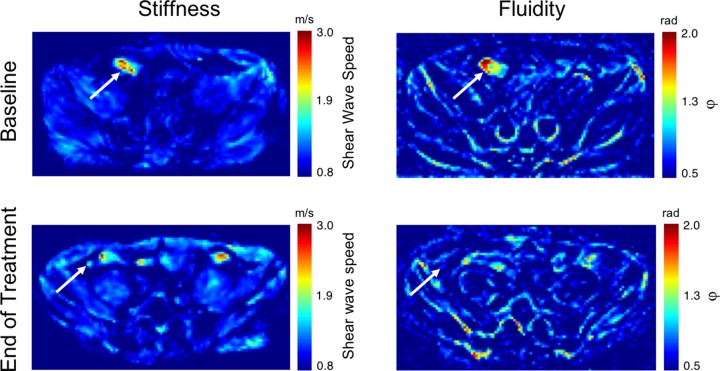
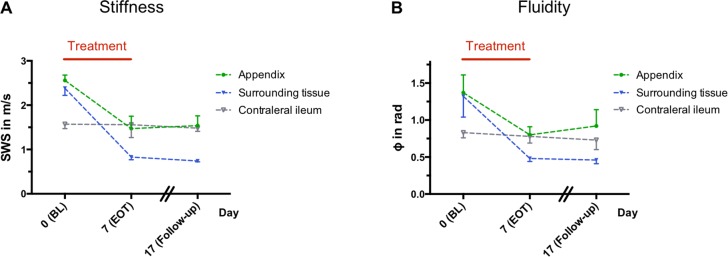
At baseline (before treatment), SWS and φ were increased in the appendix (2.56±0.12 m/s, 1.37±0.24 rad) and the surrounding tissue (2.38±0.16 m/s, 1.32±0.28 rad). The increase in SWS and φ is apparent to the naked eye when looking at the tomoelastography maps presented in figures 3 and 4. Intriguingly, a wider inflammatory area of the appendix and surrounding soft tissue with elevated stiffness and fluidity and relatively sharp boundaries is visible in these maps. The large area of elevated stiffness and fluidity indicates widespread inflammation and related oedema associated with acute appendicitis. A three-dimensional stiffness map reconstruction of the inflammation (red area) is provided in video 1. Normal contralateral intestine (ileum) was used as reference tissue. In this unaffected region, the tissue was softer and less fluid (SWS 1.57 ± 0.10 m/s, φ=0.83 ± 0.07 rad). Stiffness and fluidity values are summarised in figure 5. No signs of perforation were detected by US or MRI.
Figure 3.
Coronal T2 weighted (T2w), magnitude, stiffness and fluidity images of the appendix (arrow) in grey scale at baseline (top row) and at the end of antibiotic treatment (bottom row). At baseline, the inflammatory appendix (arrow) and the surrounding tissue (asterisk) were significantly stiffer and more fluid than after antibiotic treatment. Inflammatory areas in stiffness and fluidity maps are demarcated with higher contrast from surrounding healthy soft tissue compared with T2w images, allowing a clear identification of the extent of inflammatory involvement. Grey scale for stiffness: bright=stiff, dark=soft; grey scale for fluidity: bright=high fluidity, dark=low fluidity.
Figure 4.
Axial view of coloured stiffness and fluidity maps at baseline (top row) and at the end of antibiotic treatment (bottom row). Acute appendicitis (arrow) is characterised by high stiffness and fluidity. Colour bar for stiffness: red=stiff, blue=soft; colour bar for fluidity: red=high fluidity, blue=low fluidity.
Video 1.
Three-dimensional view of acute appendicitis at baseline (before treatment), fusion of three-dimensional T1 weighted and three-dimensional stiffness map reconstruction. Green=caecum with appendix, red=inflammation (stiff area based on stiffness map), yellow=iliopsoas muscle.
Figure 5.
Development of stiffness (A) and fluidity (B) over time in a patient with acute appendicitis. At baseline (BL), shear wave speed (SWS) (A) and shear modulus loss angle (φ) (B) of the acutely inflamed appendix (green line) and the inflamed surrounding soft tissue (blue line) were significantly higher than in the contralateral ileum (healthy, grey line). At the end of antibiotic treatment (EOT), SWS (A) and φ (B) of the appendix decreased to those of the healthy ileum and remained stable at follow-up (10 days after EOT). Healthy surrounding soft tissue has a lower SWS (A) and φ (B) than healthy appendix and ileum. Red bar=treatment period.
Treatment
Because the clinical presentation suggested a simple and uncomplicated appendicitis, the patient was treated with oral antibiotics (daily dose of 800 mg metronidazole and 1000 mg clarithromycin) for 1 week.
Outcome and follow-up
C reactive protein was normalised at EOT (4 mg/L; reference range <5 mg/L). The patient first reported subjective symptom relief 5 days after starting antibiotics. At EOT, the patient reported subjective well being (Alvarado score of 0) apart from a slight pulling sensation in the lower right abdomen (region of appendix). Pulling ceased 10 days after EOT, and the patient was considered cured.
Consistent with the patient’s clinical presentation and laboratory results, tomoelastography showed a significant reduction of stiffness and fluidity in the appendix (SWS and φ, 1.47±0.28 m/s, 0.80±0.11 rad, respectively) and the surrounding soft tissue (SWS and φ, 0.83±0.06 m/s,0.78±0.09 rad, respectively at EOT) (see figures 3 and 4). Follow-up 10 days after EOT showed persistent normalisation of these parameters for both the appendix (SWS and φ, 1.54±0.22 m/s, 0.92±0.22 rad, respectively) and the surrounding soft tissue (SWS and φ, 0.74±0.02, 0.46±0.05 rad, respectively). Stiffness and fluidity values over the entire course of disease are illustrated in figure 5. Wall oedema seen in tomoelastography maps decreased to a diameter of 5.8 mm at EOT and remained stable over 10 days after EOT (5.9 mm).
Discussion
This case demonstrates the clinical value of MRI based tomoelastography for the diagnostic characterisation of acute appendicitis and monitoring the treatment response. To the best of our knowledge, this is the first report of MRI elastography of the intestine in a patient. Our tomoelastography technique sufficiently resolved small intestinal structures, including the appendix, while conventional MR elastography often suffers from single frequency wave interferences and cannot resolve viscoelasticity details on the scale of single pixels. One other study investigated acute appendicitis using US elastography and showed a similar increase in stiffness within the appendix (25.0 kPa converted to 2.89 m/s SWS) versus the surrounding tissue (10.4 kPa converted to 1.86 m/s).22 However, this method is often limited by B mode artefacts due to bowel gas or a retrocoecal appendix.
Surgery is recommended as firstline treatment of acute appendicitis by current guidelines and is considered the gold standard despite its invasiveness.15 23 Nevertheless, conservative treatment based on antibiotics is increasingly being used and regarded as a valid alternative in uncomplicated cases.3–8 15 23 Therefore, it is likely that there will be an increasing demand for quantitative imaging methods sensitive to inflammation in the intestinal region.2 24
The initial diagnosis and monitoring of patients with appendicitis are still challenging due to the highly variable clinical and/or laboratory presentation.24 Being widely available at low cost, US is considered the firstline imaging modality.16 However, US is operator dependent and fails in ruling out appendicitis in patients with low grade inflammation and normal B mode appearance.25 The diagnostic accuracy of CT and MRI is comparable and superior to US but both modalities lack specificity in distinguishing uncomplicated and complicated appendicitis while CT is also limited by the use of ionising radiation and MRI by the fact that a Gd based contrast agent is required to detect inflammation.8 Furthermore, most imaging examinations are non-quantitative, limiting their diagnostic value in follow-up examinations and treatment monitoring.17 26 27 Intestinal tomoelastography addresses this diagnostic challenge by offering a new mechanics based contrast, allowing quantitative identification of the extent of inflammation on the basis of increased tissue stiffness and fluidity. Moreover, it does not involve exposure to radiation or contrast agents and might therefore be of diagnostic value for clinical detection and characterisation of inflammatory lesions in undecided cases, pregnant women and children. Furthermore, tomoelastography could also be used for monitoring the response to antibiotic treatment as patients not responding to antibiotics face the risk of developing severe complications, such as perforation and peritonitis.
Patient ’s perspective.
The disease started with diffuse stomach pain lasting for about 1–4 hours. First, I attributed it to eating spicy food. Later that evening, the pain relocated to the lower right abdomen. The pain remained stable over the next 2 days, and I measured a slightly elevated temperature of 37.7°, so that I decided to go to the gastroenterologic doctor’s office. A clinical and abdominal ultrasound examination and blood collection were performed by the doctor. Due to the outpatient setting it took 3 days before I was informed about the blood results. The doctor diagnosed an acute appendicitis based on the clinical examination and the US findings.
The doctor explained the diagnosis to me and informed me in detail about the treatment options, including possible side effects. I had the choice between surgery and treatment with antibiotics. I opted to decline surgery and considered the antibiotics a better alternative. I never had an operation before and I feared such an invasive procedure.
On the same evening, I felt uncertain regarding my decision and began to think that an operation might be better after all. I was aware that failure of antibiotic treatment could lead to the complication of a perforation and I was afraid that an inflammation could increase and get worse. I had to choose between a planned surgery or a possible emergency surgery if antibiotic treatment failed.
Tomoelastography confirmed the diagnosis of uncomplicated appendicitis. The external vibration needed for creating the waves was well tolerable and adapted to my subjective feeling. It felt like a cell phone vibration, but it was better tolerable than walking. The radiologist showed the elastograms to me. My anatomical orientation was very poor, but I could follow the radiologist, and the very bright inflammatory spot was clearly visible to me without any deeper knowledge. After tomoelastography, I felt reassured and decided to stick to the antibiotic therapy. On the following day, the inflammation was still apparent but it did not get worse. So I continued with the antibiotics.
After 7 days on antibiotics, I was uncertain about the next steps after the end of treatment. A second blood test was performed at the end of treatment. These results were normal. Furthermore, another tomoelastography was performed after treatment, and the radiologist reassured me that everything looked normal again. The stiffness values of the appendix were similar to those elsewhere in the intestine. Both results confirmed the success of antibiotic treatment, and I felt much reassured and comfortable although a slight pulling sensation was still apparent in the lower right abdomen. After 10 days, the feeling of pulling disappeared, and I had no further physical restrictions.
Now that I had my first experience with a serious disease I am very happy that I had a good alternative treatment option and was spared surgery. I believe that everything in our body has its function and should be preserved as long as possible. In my case imaging with display of changes I could see gave me the confidence I needed to understand that antibiotic treatment was successful.
Learning points.
Acute appendicitis is characterised by higher stiffness and fluidity.
Tomoelastography is a promising non-invasive and quantitative method for identification of acute appendicitis and confirmation of an uncomplicated stage.
Tomoelastography provides quantitative values allowing follow-up for monitoring the response to antibiotic treatment.
Cut-offs are needed for therapeutic decision making and could be generated for different stages of appendicitis in the future.
Acknowledgments
The authors would like to acknowledge Dr Lutz Liebich-Bartholain for providing ultrasound images and permission for publication, Dr Zully Maritza Ritter and Dr Jürgen Braun for their technical support, and the patient for his continued engagement and support.
Footnotes
Contributors: SRMG and IS: conception, design, and analysis and interpretation of the data. SRMG: drafting the article. SRMG, BH and IS: revising the manuscript critically for important intellectual content and final approval of the version published.
Funding: This study was funded by Bundesministerium für Bildung und Forschung (grant No: LiSyM 031L0057) and Deutsche Forschungsgemeinschaft (grant No: BIOQIC GRK 2260, SFB 1340).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Buckius MT, McGrath B, Monk J, et al. Changing epidemiology of acute appendicitis in the United States: study period 1993-2008. J Surg Res 2012;175:185–90. 10.1016/j.jss.2011.07.017 [DOI] [PubMed] [Google Scholar]
- 2. Becker P, Fichtner-Feigl S, Schilling D. Clinical management of appendicitis. Visc Med 2018;34:453–8. 10.1159/000494883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Eriksson S, Granström L. Randomized controlled trial of appendicectomy versus antibiotic therapy for acute appendicitis. Br J Surg 1995;82:166–9. 10.1002/bjs.1800820207 [DOI] [PubMed] [Google Scholar]
- 4. Hansson J, Körner U, Khorram-Manesh A, et al. Randomized clinical trial of antibiotic therapy versus appendicectomy as primary treatment of acute appendicitis in unselected patients. Br J Surg 2009;96:473–81. 10.1002/bjs.6482 [DOI] [PubMed] [Google Scholar]
- 5. Salminen P, Paajanen H, Rautio T, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. JAMA 2015;313:2340–8. 10.1001/jama.2015.6154 [DOI] [PubMed] [Google Scholar]
- 6. Styrud J, Eriksson S, Nilsson I, et al. Appendectomy versus antibiotic treatment in acute appendicitis. a prospective multicenter randomized controlled trial. World J Surg 2006;30:1033–7. 10.1007/s00268-005-0304-6 [DOI] [PubMed] [Google Scholar]
- 7. Talan DA, Saltzman DJ, Mower WR, et al. Antibiotics-first versus surgery for appendicitis: a US pilot randomized controlled trial allowing outpatient antibiotic management. Ann Emerg Med 2017;70:1–11. 10.1016/j.annemergmed.2016.08.446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Vons C, Barry C, Maitre S, et al. Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet 2011;377:1573–9. 10.1016/S0140-6736(11)60410-8 [DOI] [PubMed] [Google Scholar]
- 9. Findlay JM, Kafsi JE, Hammer C, et al. Nonoperative management of appendicitis in adults: a systematic review and meta-analysis of randomized controlled trials. J Am Coll Surg 2016;223:814–24. 10.1016/j.jamcollsurg.2016.09.005 [DOI] [PubMed] [Google Scholar]
- 10. Harnoss JC, Zelienka I, Probst P, et al. Antibiotics versus surgical therapy for uncomplicated appendicitis: systematic review and meta-analysis of controlled trials (PROSPERO 2015: CRD42015016882). Ann Surg 2017;265:889–900. 10.1097/SLA.0000000000002039 [DOI] [PubMed] [Google Scholar]
- 11. Poprom N, Numthavaj P, Wilasrusmee C, et al. The efficacy of antibiotic treatment versus surgical treatment of uncomplicated acute appendicitis: Systematic review and network meta-analysis of randomized controlled trial. Am J Surg 2019;218:192–200. 10.1016/j.amjsurg.2018.10.009 [DOI] [PubMed] [Google Scholar]
- 12. Rollins KE, Varadhan KK, Neal KR, et al. Antibiotics versus appendicectomy for the treatment of uncomplicated acute appendicitis: an updated meta-analysis of randomised controlled trials. World J Surg 2016;40:2305–18. 10.1007/s00268-016-3561-7 [DOI] [PubMed] [Google Scholar]
- 13. Sallinen V, Akl EA, You JJ, et al. Meta-analysis of antibiotics versus appendicectomy for non-perforated acute appendicitis. Br J Surg 2016;103:656–67. 10.1002/bjs.10147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Varadhan KK, Neal KR, Lobo DN. Safety and efficacy of antibiotics compared with appendicectomy for treatment of uncomplicated acute appendicitis: meta-analysis of randomised controlled trials. BMJ 2012;344:e2156 10.1136/bmj.e2156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Di Saverio S, Birindelli A, Kelly MD, et al. WSES Jerusalem guidelines for diagnosis and treatment of acute appendicitis. World J Emerg Surg 2016;11:34 10.1186/s13017-016-0090-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dirks K, Calabrese E, Dietrich CF, et al. EFSUMB position paper: recommendations for gastrointestinal ultrasound (GIUS) in acute appendicitis and diverticulitis. Ultraschall Med 2019;40:163–75. 10.1055/a-0824-6952 [DOI] [PubMed] [Google Scholar]
- 17. Kim K, Kim YH, Kim SY, et al. Low-dose abdominal CT for evaluating suspected appendicitis. N Engl J Med 2012;366:1596–605. 10.1056/NEJMoa1110734 [DOI] [PubMed] [Google Scholar]
- 18. Dittmann F, Tzschätzsch H, Hirsch S, et al. Tomoelastography of the abdomen: tissue mechanical properties of the liver, spleen, kidney, and pancreas from single MR elastography scans at different hydration states. Magn Reson Med 2017;78:976–83. 10.1002/mrm.26484 [DOI] [PubMed] [Google Scholar]
- 19. Tzschätzsch H, Guo J, Dittmann F, et al. Tomoelastography by multifrequency wave number recovery from time-harmonic propagating shear waves. Med Image Anal 2016;30:1–10. 10.1016/j.media.2016.01.001 [DOI] [PubMed] [Google Scholar]
- 20. Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med 1986;15:557–64. 10.1016/S0196-0644(86)80993-3 [DOI] [PubMed] [Google Scholar]
- 21. Ohle R, O’Reilly F, O’Brien KK, et al. The Alvarado score for predicting acute appendicitis: a systematic review. BMC Med 2011;9:139 10.1186/1741-7015-9-139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cha SW, Kim IY, Kim YW. Quantitative measurement of elasticity of the appendix using shear wave elastography in patients with suspected acute appendicitis. PLoS One 2014;9:e101292 10.1371/journal.pone.0101292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Baird DLH, Simillis C, Kontovounisios C, et al. Acute appendicitis. BMJ 2017;357:j1703 10.1136/bmj.j1703 [DOI] [PubMed] [Google Scholar]
- 24. Gorter RR, Eker HH, Gorter-Stam MA, et al. Diagnosis and management of acute appendicitis. EAES consensus development conference 2015. Surg Endosc 2016;30:4668–90. 10.1007/s00464-016-5245-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shogilev DJ, Duus N, Odom SR, et al. Diagnosing appendicitis: evidence-based review of the diagnostic approach in 2014. West J Emerg Med 2014;15:859–71. 10.5811/westjem.2014.9.21568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hoffmann M, Anthuber M. [Rational diagnostics of acute appendicitis]. Chirurg 2019;90:173–7. 10.1007/s00104-018-0755-6 [DOI] [PubMed] [Google Scholar]
- 27. Repplinger MD, Levy JF, Peethumnongsin E, et al. Systematic review and meta-analysis of the accuracy of MRI to diagnose appendicitis in the general population. J Magn Reson Imaging 2016;43:1346–54. 10.1002/jmri.25115 [DOI] [PMC free article] [PubMed] [Google Scholar]