Abstract
Head and Neck Cancer (HNC) is the sixth most common type of cancer across the globe, with more than 300,000 deaths each year, globally. However, there are currently no standardised molecular markers that assist in determining HNC prognosis. The literature for this systematic review and meta-analysis were sourced from multiple bibliographic databases. This review followed PRISMA guidelines. The Hazard Ratio (HR) was selected as the effect size metric to independently assess overall survival (OS), disease-free survival (DFS), and prognosis. Subgroup analysis was performed for individual highly represented miRNA. A total of 6843 patients across 50 studies were included in the systematic review and 34 studies were included in the meta-analysis. Studies across 12 countries were assessed, with China representing 36.7% of all included studies. The analysis of the survival endpoints of OS and DFS were conducted separately, with the overall pooled effect size (HR) for each being 1.825 (95% CI 1.527–2.181; p < 0.05) and 2.596 (95% CI 1.917–3.515; p < 0.05), respectively. Subgroup analysis was conducted for impact of miR-21, 200b, 155, 18a, 34c-5p, 125b, 20a and 375 on OS, and miR-21 and 34a on DFS. The pooled results were found to be statistically significant for both OS and DFS. The meta-analysis indicated that miRNA alterations can account for an 82.5% decrease in OS probability and a 159.6% decrease in DFS probability. These results indicate that miRNAs have potential clinical value as prognostic biomarkers in HNC, with miR-21, 125b, 34c-5p and 18a, in particular, showing great potential as prognostic molecular markers. Further large scale cohort studies focusing on these miRNAs are recommended to verify the clinical utility of these markers individually and/or in combination.
Keywords: microRNAs, head and neck cancer, prognosis, systematic review, meta-analysis
1. Introduction
Head and Neck Cancer (HNC) is the sixth leading cancer by incidence worldwide, with an annual incidence rate of more than 550,000 cases and around 300,000 deaths each year [1]. It has shown to be strongly associated with environmental and lifestyle risk factors including tobacco use, alcohol consumption, human papilloma virus or Ebstein-Barr virus infection, poor oral and dental hygiene, malnutrition, gastroesophageal or laryngopharyngeal reflux disease, and occupational exposure to chemicals and fumes [2]. Treatment for early HNC primarily involves multi-modality therapy with a combination of surgery and radiation [3]. Patients with advanced disease stages have been shown to frequently develop recurrences or distant metastases, resulting in five-year overall survival (OS) rates of less than 60% with poor long-term prognosis [4]. Patients with loco-regional relapse or metastatic disease usually cannot be cured, with only limited benefits arising from palliative chemotherapy [5]. In this regard, there is an urgent need for the identification of biomarkers for accurate prognosis, in order to inform and direct patient treatment. MicroRNAs (miRNAs) have been proposed as quantitative prognostic markers in HNC [6]. MicroRNAs are small non-coding RNAs (~22 nucleotides) transcribed from DNA into RNA hairpins. MicroRNAs post-transcriptionally regulate gene expression by binding to the 3′-UTR of target mRNAs, resulting in target mRNA degradation or inhibition of their translation [7,8]. Other recent studies have also suggested that the secondary structure of the 5′ untranslated region (5′ UTR) of messenger RNA (mRNA) is important for microRNA (miRNA)-mediated gene regulation in humans [9]. MiRNAs are first transcribed as primary transcripts (pri-miRNA) with a cap and poly-A tail by RNA polymerase II or RNA polymerase III, with a typical pri-miRNA being composed of a double stranded stem of ’33 base pairs, a terminal ‘hairpin’ loop and two flanking unstructured single-stranded segments. MiRNAs are first transcribed as primary transcripts (pri-miRNA) with a cap and poly-A tail by RNA polymerase II or RNA polymerase III, with a typical pri-miRNA being composed of a double stranded stem of ’33 base pairs, a terminal ‘hairpin’ loop and two flanking unstructured single-stranded segments. The Pri-miRNA is then processed to a short 70 nucleotide stem-loop structure known as pre-miRNA by a protein complex known as the Microprocessor complex. After the pre-miRNA is generated in the nucleus, it is exported to the cytoplasm by the action of RanGTPase. In the cytoplasm, an RNAse III endonuclease cleaves pre-miRNA into short miRNA duplexes. After cleavage, the miRNA duplec is unwound by an RNA helicase and the mature miRNA strand binds to an Argonaute (Ago) protein into an RNP complex. The mature miRNA binds to the target mRNA and typically in the 3’-untranslated region (3’-UTR), interfering with the translation of the mRNA, thereby, regulating gene expression in cancer by inhibiting translation or by targeting the mRNA for degradation or deadenylation or by upregulating the translation of oncogenes [10,11]. Therefore, MicroRNAs are involved in a variety of biological functions including playing a role in the majority of known hallmarks of cancer, while playing a major role in cancers by functioning as upregulators of oncogenes, or even as tumour suppressors [7]. Furthermore, studies have suggested that due to this, miRNAs have a prognostic value in several human cancers [6,12]. miRNAs can function as both tumour-suppressors as well as oncogenes. Therefore, miRNAs may be capable of offering a sensitive method for HNC detection, monitoring and prognosis. Previous studies have shown that miRNA deregulation occurs in HNC patients. However concrete miRNA prognostic markers capable of informing clinical decision making, have not yet been identified [13]. Therefore, an objective, systematic review on studies about miRNA and HNC was performed, in order to elucidate the significance of specific miRNA in HNC prognosis. Additionally, a comprehensive meta-analysis was performed to investigate the significance of miRNA in determining patient prognosis, with subsequent subgroup analysis further exploring the prognostic significance of frequently expressed miRNAs.
2. Methods
2.1. Search Strategy and Study Selection
The following systematic review and meta-analysis were conducted based on the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) guidelines [14]. The search strategy was designed to be comprehensive and exhaustive with a prime focus on minimising bias and maximising sensitivity. The EMBASE, PubMed, Web of Science and Science Direct bibliographic databases were used to search for relevant published literature in the field of miRNA as prognostic markers in HNC. Predefined ‘search strings’ (as shown in Supplementary Table S1) were generated using a few core ‘keywords’, which included;
miRNA
Head and Neck Cancer
Prognosis
Survival
Overall Survival
Disease-Free Survival
miRNA expression
upregulation
downregulation
deregulation/dysregulation
Biomarkers
Treatment
Surgical resection
Radiotherapy
Chemotherapy
Clinical study
Oral cancer
Head and Neck Squamous Cell Carcinoma (HNSCC)
These ‘search strings’ were subsequently used for searching literature databases for relevant studies published until September 2018. The search was conducted individually by two reviewers (C.K. and R.J.), in order to ameliorate any possible selection bias. Initial screening of articles and studies was based on the pertinence of the title and abstract of each publication to the systematic review and meta-analysis. The screening was conducted simultaneously alongside the initial search, at the discretion of the two reviewers (C.K. and R.J.). To further bolster the results of the search strategy, the reference lists of included publications (initial post-screening), were also screened for pertinent studies. Any disagreements arising during initial screening were solved with the inclusion of the third reviewer.
2.2. Inclusion and Exclusion Criteria
After initial search and screening, the full-texts of selected studies were then subjected to further rigorous screening based on a set of predefined inclusion and exclusion criteria. This secondary screening process was also conducted by two reviewers in tandem (C.K. and R.J.), based on the following criteria:
Inclusion criteria
The studies discuss miRNA expression in HNC patients.
The studies investigate the association between miRNA expression and patient survival in HNC.
The studies explicitly presented the resulting survival data in terms of hazard ratios (HRs) and 95% confidence intervals (CIs).
The studies assessed patient survival based on the endpoints of OS, disease-free survival (DFS), or both.
The studies provided sufficient data to extract the HR and 95% CI, in case the studies do not explicitly state these values.
Exclusion criteria
Conference abstracts, reviews and correspondence.
Studies that only reported results from in-vitro, in-silico or animal studies.
Studies that were conducted as part of theses, or incomplete studies.
Studies will very small sample sizes, or case studies.
No limits were placed on the patients’ demographic or the clinicopathological characteristics, for the selection of studies for conducting the systematic review and meta-analysis.
2.3. Data Extraction
Extraction of data from selected studies was preceded by the preparation of a standardised data extraction form using Microsoft Excel. The data extraction was carried out individually, with all collated data bring combined into one single database at the end of the extraction process, with duplicated data being simultaneously removed. All tables, charts and figures from selected studies were compiled into a separate database for ease of analysis. The following data items were extracted from the studies:
Name of the first author
Year of publication
Country
Number of participants
Study population
Assay methods
Tumour stage
Tumour anatomic location
Clinicopathological characteristics (age, gender, risk factors and metastasis)
Significantly expressed miRNAs
Upregulated, downregulated and dysregulated miRNAs
HR with 95% CI of OS and DFS.
2.4. Quality Assessment
The quality of included studies was based on a quality assessment tool developed by the National Heart, Lung and Blood Institute (NHLBI) (USA) for Observational and Cross-sectional studies [15]. This tool was applied to the full texts of all included studies. The NHLBI quality assessment tool uses a set of 14 criteria according to which each study is subjectively rated as ‘good’, ‘fair’, or ‘poor’ based on the opinion of two reviewers. As per the guidelines accompanying the assessment tool, the quality assessment was carried out independently by the reviewers. A ‘high’ quality rating via this tool corresponds to a low risk of bias in the study being assessed, while a ‘low’ quality rating is indicative of a high risk of bias.
2.5. Meta-Analysis and Assessment of Heterogeneity
The meta-analysis was conducted using the aid of the Comprehensive Meta-Analysis software [16]. The HR and 95% CI values for OS and DFS extracted from each study were pooled together in the form of a Forest Plot. As HR is the effect size metric chosen for the study, the pooled HR and 95% CI are indicative of the probability of survival for given miRNA expression, thereby indicating the prognostic value of said miRNA. The random-effects model of the meta-analysis was chosen to pool the HR values, due to the inherent heterogeneity that arises from the differences between the study parameters of each study [17]. In the case of studies not presenting the HR and 95% CI values for OS and DFS, the respective values were estimated using the Kaplan-Meier curves for miRNA expression, which were presented in said studies. Additionally, for the assessment and comparison of miRNA concerning each other, each assessment of a discrete patient group within the larger patient group of a single study will be included in the meta-analysis as a unique cohort. Subgroup analysis was carried out based on the survival endpoint of each study (OS or DFS), the change in the miRNA expression (upregulated/downregulated), and the specific miRNA that was represented in at least two separate studies.
The assessment of between-study heterogeneity was based on the Higgins I2 statistic, Cochran’s Q and the Tau2 value [18,19,20]. The I2 statistic was the primary method of assessing heterogeneity, owing to its high power of detection (a lower I2 value indicates a lower amount of heterogeneity). However, as I2 may generate biased results in a small meta-analysis, the Cochran’s Q Test and Tau2 value were also assessed in order to generate a higher degree redundancy in the assessment of heterogeneity between studies [21]. Here, the Tau2 value refers to the variance of effect size parameters across the population of studies and reflects the variance of true effect sizes.
2.6. Publication Bias
Publication bias is inherent to studies such as systematic reviews and meta-analyses as they consist of previously published studies and literature [22,23,24,25,26,27]. This bias is an extension of the publication process wherein it is more likely that extensive studies and positive results are published, while smaller studies and negative results are unfavoured and often are not published as part of the peer-reviewed literature [23,24,28,29,30,31]. Therefore, publication bias cannot be wholly eradicated from any systematic review and meta-analysis study [32,33]. To ameliorate this issue, assessment of publication bias was conducted to assess the degree of impact publication bias has upon this study’s results [30,34,35,36].
The Egger’s graphical test for assessment of bias was used to construct a funnel plot (a scatter plot constructed using the standard error [y-axis] and log (HR) [x-axis]), of all included studies. The symmetry of the study distribution on the plot, across the regression line, is inversely correlated with the magnitude of publication bias in the meta-analysis [37].
The Orwin’s Fail-Safe N test was used to determine the presence of missing studies that may skew the regression line in the funnel plot, with Duval and Tweedie’s Trim and Fill method being used for imputation of the missing studies [38,39]. These methods were used in conjunction to adjust the Funnel Plot to better represent the likely publication bias.
Additionally, the Begg and Mazumdar’s Rank Correlation test was used to correlate the ranks of effect sizes and the ranks of their variances, with a positive value indicating a higher test accuracy [40].
3. Results
3.1. Study Selection and Data Extraction
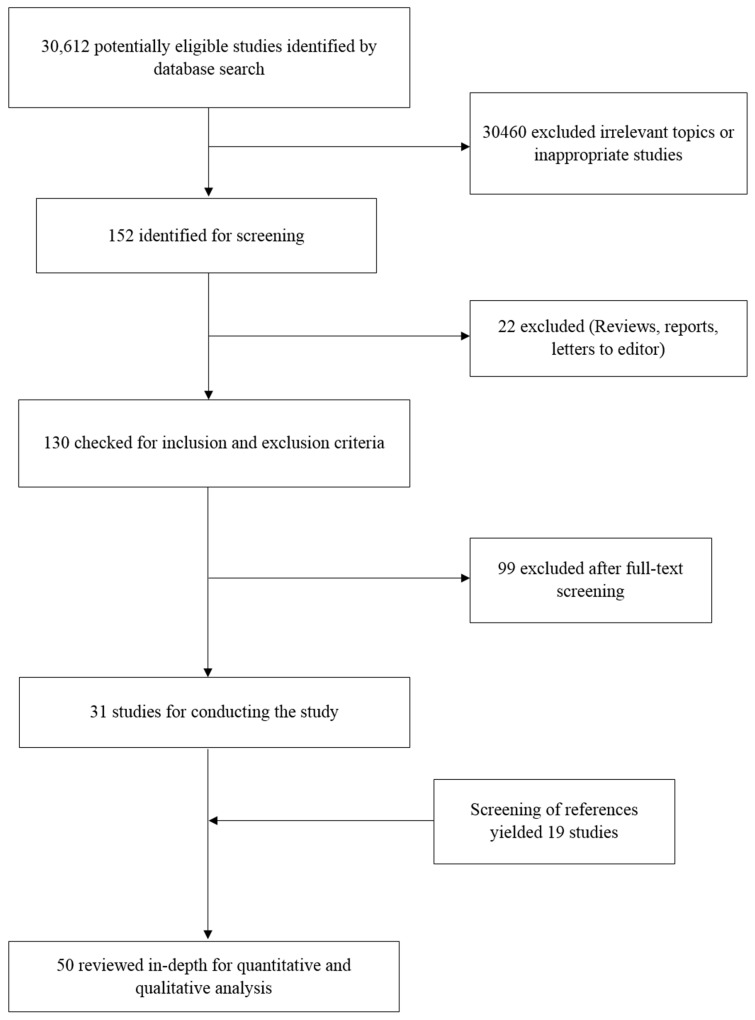
After following the search strategy, the number of search results of all databases combined totalled to 30,612 potential studies. Out of these studies, a majority were screened out by the reviewers, as they were not relevant to the study being conducted or were focused on tangential topics of research. After this initial screening, 152 studies were selected for further processing. Eliminating duplicates in the search results led to further 22 studies being eliminated, leaving 130 studies for secondary screening based on the inclusion and exclusion criteria. The full texts of the 130 studies were obtained and screened, leading to 99 studies being eliminated and leaving a final total of 31 studies for conducting the study. Screening of the reference lists of these 31 studies revealed 19 more studies that satisfied the requirements for being included in this systematic review and meta-analysis. A final total of 50 studies were included for the systematic review part of the study. However, as not all 50 studies presented sufficient statistical data for conducting of a meta-analysis, studies that did not present HR and 95% CI values, and did not have data from which these values could be extracted, were eliminated from the meta-analysis. Therefore, 16 studies were eliminated, and a total of 34 studies were included in the meta-analysis. The entire process was monitored by the third reviewer at all stages. Figure 1 depicts the entire study selection process in the form of a flowchart.
Figure 1.
Flow chart describing search strategy.
3.2. Study Characteristics
The 50 studies included in this systematic review and meta-analysis study were found to originate from 12 countries around the world, including Brazil (n = 3), Canada (n = 2), China (n = 18), Chile (n = 1), Czech Republic (n = 1), Denmark (n = 1), Germany (n = 2), Italy (n = 3), Japan (n = 5), Taiwan (n = 6), UK (n = 2) and USA (n = 5), while one study did not specify the region in which it was conducted. A total of 6834 patients across the 50 studies were included in this study. Out of all 50 studies, 39 studies were found to involve a higher percentage of men compared to women, with only 1 study reporting having women as the majority of its participants, while the remaining ten studies did not divulge any information regarding the gender ratios of their participants. The miRNA expression in patients was detected using qRT-PCR in 44 studies and immunohistochemistry in 3 studies, with the rest of the studies using other different techniques. In-situ hybridisation (ISH) was also used by three studies, in conjunction with qRT-PCR as the primary method of miRNA quantification. Patients included in 14 of the studies were also found to indulge, or were formerly indulging in smoking, with the studies showing that smokers formed the majority of the at-risk group of these studies, with only three studies describing risk factors besides smoking. The rest of the 33 studies did not provide any information regarding risk factors in the given patient groups. The study and patient characteristics of all 50 studies are described in Table 1.
Table 1.
The study and patient characteristics of all 50 studies.
| Article | Year | miR | Sample Size | Anatomic Location | Assay Method | Study Population | Gender | Stage | Metastasis | Risk Factors | Age |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Carvalho et al. [41] | 2015 | miR-203 miR-205 | 127 | Tongue 58.3% Floor of mouth 31.3% Alveolar ridge 8.3% Lower gum 2.1% | qRT-PCR | Brazil | Male (79.2%) | T2 (62.5%) | Metastases + ve (52.083%) Metastases − ve (47.916%) | Smoking (47.9%) | 43–84 |
| Hou et.al. [42] | 2015 | miR-223 miR-99a miR-21 | 16 | Head and Neck | qRT-PCR | Japan | Male (93.75%) | T2 (18.75%) T3 (12.5%) T4 (68.75%) | NA | NA | 48–80 |
| Maia et al. [43] | 2015 | miR-296-5p | 34 | Supraglottic 20.6% Glottic 79.4% | qRT-PCR | Brazil | Male (88.2%) | T1 (47.1%) T2 (52.9%) | NA | Tobacco (91.2%) | ≤60 years (47%) >60 years (53%) |
| Hudcova et al. [44] | 2016 | miR-29c miR-200b miR-375 | 42 | Head and Neck | qRT-PCR | Czech Republic | Male (100%) | T1 + T2 (45%) T3 + T4 (55%) | Metastases + ve (11.42%) Metastases − ve (88.57%) | NA | NA |
| Wang et al. [45] | 2015 | miR-451 | 50 | Head and Neck | qRT-PCR | China | NA | NA | NA | NA | NA |
| Arantes et al. [46] | 2017 | miR-21 | 71 | Oropharynx 49.3% Larynx 39.4% Hypopharynx 11.3% | qRT-PCR | Brazil | Male (95.8%) | T2 + T3 (64.8%) T4 (35.2%) | NA | HPV (8.45%) Tobacco (80.3%) Alcohol (38.0%) | 40–76 |
| Xu et al. [47] | 2015 | miR-483-5p | 101 | Oral Cavity | qRT-PCR | China | Male (76.2%) | T1 + T2 (50.5%) T3 + T4 (49.5%) | NA | Smoking (72.3%) Alcohol (68.3%) | 53.2 ± 10.3 |
| Li et al. [48] | 2015 | miR-93 | 103 | Supraglottic 25.24% Glottic 55.33% Hypopharynx 9.7% Oral Cavity 9.7% | ISH, qRT-PCR | China | Male (96.1%) | T1 (15.5%) T2 (35%) T3 (40.8%) T4 (8.7%) | Metastases + ve (38.83%) | NA | <58 (46%) ≥58 (54%) |
| Hu et al. [49] | 2014 | miR-21 miR-375 | 46 | Glottic 71.7% Supraglottic 23.9% Subglottic 4.4% | qRT-PCR | China | Male (91.3%) | T0 + T1 + T2 (45.7%) T3 + T4 (54.3%) | NA | Smoking (72.1%) Alcohol (46.3%) | 59.2 ± 7.84 |
| Hedback et al. [50] | 2014 | miR-21 | 86 | Oral Cavity | ISH, Immunohistochemistry | Denmark | NA | NA | NA | NA | NA |
| Sun et al. [51] | 2015 | miR-320a | 450 | Salivary Gland | ISH, Immunohistochemistry | China | Male (47.56%) | T1 + T2 (65.33%) T3 + T4 (34.67%) | Metastases + ve (43.56%) | NA | <50 (49%) ≥50 (51%) |
| Saito et al. [52] | 2013 | miR-196a | 84 | Larynx | qRT-PCR | Japan | NA | NA | NA | NA | NA |
| Li et al. [53] | 2009 | miR-21 | 103 | Tongue | qRT-PCR | China | Male (54.36%) | T1 + T2 (58.25%) T3 + T4 (41.75%) | Metastases + ve (27.18%) | NA | <50 (46%) ≥50 (54%) |
| Liu et al. [54] | 2012 | miR-93 miR-142-3p miR-29c miR-26a miR-30e | 465 | Nasopharyngeal | qRT-PCR | China | Male (74.19%) | T1 (21.94%) T2 (27.31%) T3 (23.66%) T4 (27.10%) | Metastases + ve (19.78%)) | NA | 47.09 ± 11 |
| Summerer et al. [55] | 2013 | miR-425-5p miR-21-5p miR-106b-5p miR-93-5p | 18 | Larynx 27.77% Oropharynx 16.66% Mouth floor 11.11% Tongue 11.11% Esophagus 5.55% Hypopharynx 5.55% Maxilla 5.55% Nasopharyngeal 5.55% Sinuses 5.55% Soft palate 5.55% | qRT-PCR | Germany | Male (77.78%) | T1 (22.22%) T2 (11.11%) T3 (33.33%) T4 (33.33%) | Metastases + ve (11.11%) | NA | 45.1–80.6 |
| Suh et al. [56] | 2015 | miR-196a | 16 | Oral Cavity | qRT-PCR | UK | NA | NA | NA | NA | NA |
| Ogawa et al. [57] | 2012 | miR-34a | 24 | Sinonasal | miRNA-Microarray | Japan | Male (66.67%) | T2 (4%) T3 (41.67%) T4 (54.17%) | Metastases + ve (8.33%) | NA | >60 (59%) <60 (41%) |
| Avissar et al. [58] | 2009 | miR-375 miR-21 | 169 | Oral 64% Pharynx 21% Larynx 15% | qRT-PCR | USA | Male (68%) | T1 + T2 (28%) T3 + T4 (72%) | NA | HPV (17.4%) Alcohol (88.5%) Smoking (84.5%) | 61.5 ± 11.9 |
| Massimo Re et al. [59] | 2015 | miR-34c-5p | 90 | Supraglottic 21.1% Transglottic 73.3% Subglottic 5.6% | qRT-PCR | Italy | Male (96.6%) | T3 (66.7%) T4 (33.3%) | Metastases + ve (0%) | NA | 66.51 ± 8.02 |
| Sun et al. [60] | 2013 | miR-363 | 62 | Tongue 41.9% Gingival 21% Cheek 11.3% Floor of Mouth 17.7% Oropharynx 8.1% | qRT-PCR | China | Male (69.4%) | T1 + T2 (43.5%) T3 + T4 (36.5%) | Metastases + ve (54.83%) | Smoking (48.4%) Drinking (32.3%) | ≥60 (42%) <60 (58%) |
| Tian et al. [61] | 2014 | miR-203 | 56 | Glottic 53.57% Supraglottic 46.43% | qRT-PCR | China | Male (71.43%) | T1 + T2 (42.85%) T3 + T4 (57.14%) | Metastases + ve (50%) | NA | ≥59 (57%) <59 (43%) |
| Chang et al. [62] | 2013 | miR-17 miR-20a | 98 | Buccal Mucosa 43.88% Tongue 29.59% Gingiva 21.43% Floor of Mouth 5.10% | qRT-PCR | Taiwan | Male (84.7%) | T1 + T2 (44.9%) T3 + T4 (55.1%) | Metastases + ve (37.75%) | Smoking (82.65%) | >50 (35%) <50 (65%) |
| Gee et al. [63] | 2010 | miR-210 | 46 | Oral Cavity 21% Oropharynx 46% Hypopharynx 19% Larynx 11% Paranasal Sinus 2% | qRT-PCR | UK | Male (80.43%) | T1 (10.87%) T2 (30.43%) T3 (15.22%) T4 (43.48%) | NA | Smoking (86.96%) Alcohol (78.26%) | 43–92 |
| Lenarduzzi et al. [64] | 2013 | miR-193b | 51 | Head and Neck | qRT-PCR | Canada | NA | NA | NA | NA | NA |
| Childs et al. [65] | 2009 | miR-205 Let-7d miR-21 | 104 | Oral Cavity 30% Oropharynx 46% Hypopharynx 9% Larynx 31% | qRT-PCR | US | Male (68%) | T1 + T2 (23%) T3 + T4 (77%) | NA | Smoking (82%) HPV (36%) | <60 (40%) >60 (61%) |
| Shen et al. [66] | 2012 | miR-34a | 69 | Larynx | qRT-PCR | China | NA | T1 + T2 (60.87%) T3 + T4 (39.13%) | Metastases + ve (34.78%) | NA | <60 (48%) ≥60 (52%) |
| Luo et al. [67] | 2013 | miR-18a | 168 | Nasopharyngeal | qRT-PCR | China | Male (75.6%) | T1 + T2 (42.86%) T3 + T4 (57.14%) | Metastases + ve (64.88%) | NA | ≥50 (59%) <50 (41.%) |
| Jung et al. [68] | 2012 | miR-21 | 17 | Tongue 94.12% Oropharynx 5.88% | qRT-PCR | USA | NA | NA | NA | HPV (58.82%) | 41–69 |
| Sasahira et al. [69] | 2012 | miR-126a | 118 | Tongue 54.24% Other 45.76% | qRT-PCR | Japan | Male (57.63%) | T1 + T2 (76.27%) T3 + T4 (23.73%) | Metastases + ve (28.81%) | NA | ≤65 (39%) >65 (61%) |
| Liu et al. [70] | 2014 | miR-134a | 96 | Buccal Mucosa 35.41% Tongue 27.08% Oral pharynx 37.5% | qRT-PCR | Taiwan | Male (93.75%) | T1 + T2 + T3 (28.12%) T4 (71.88%) | Metastases + ve (6.25%) | NA | 53.5 (Average) |
| Shi et al. [71] | 2014 | miR-155 | 30 | Oral Cavity | qRT-PCR, FISH | China | Male (63.33%) | T1 (10%) T2 (16.67%) T3 (33.33%) T4 (40%) | NA | Smoking (46.67%) Alcohol (53.33%) | 56.4 ± 8.6 (40-75) |
| Harris et al. [72] | 2012 | miR-375 | 123 | Oral Cavity 35% Oropharynx 30% Larynx 35% | qRT-PCR | US | Male (69.1%) | T1 + T2 (19.5%) T3 + T4 (80.5%) | NA | Smoking (60.9%) Alcohol (27.6%) HPV (25.2%) | ≤58 (37%) 59–66 (31%) ≥67 (33%) |
| Huang et al. [73] | 2014 | miR-491-p5 | 33 | Oral Cavity | qRT-PCR, FISH | Taiwan | Male (96.9%) | T1 (9.1%) T2 (51.5%) T3 (3.0%) T4 (36.4%) | NA | NA | ≤60 (21%) >60 (79%) |
| Shiiba et al. [74] | 2013 | miR-125b | 50 | Oral Cavity | qRT-PCR | Japan | NA | T1 (10%) T2 (12%) T3 (14%) T4 (64%) | NA | NA | NA |
| Zeng et al. [75] | 2012 | miR-20a | 160 | Nasopharyngeal | qRT-PCR | China | Male (61.25%) | T1 (1,25%) T2 (15.63%) T3 (34.38%) T4 (40%) | NA | NA | 46.41 ± 10.74 |
| Liu et al. [76] | 2013 | miR-451 | 280 | Nasopharyngeal | qRT-PCR | Taiwan | Male (73.57%) | T1 + T2 (50.71%) T3 + T4 (49.28%) | NA | NA | ≤45 (49%) >45 (51%) |
| Yang et al. [77] | 2011 | miR-181a | 39 | Oral Cavity | qRT-PCR | Taiwan | Male (44.87%) | T1 + T2 + T3 (33.33%) T4 (66.66%) | NA | NA | NA |
| Wu et al. [78] | 2014 | miR-19a | 83 | Laryngeal | qRT-PCR | China | Male (68.67%) | NA | Metastases + ve (34.93%) | NA | ≥56 (51%) <56 (49%) |
| Peng et al. [79] | 2014 | Let-7g miR-125b miR-218 | 29 | Oral Cavity | qRT-PCR | Taiwan | NA | NA | NA | NA | NA |
| Arriagada et al. [80] | 2018 | miR-215b | 32 | Head and Neck | qRT-PCR | Chile | Male (55.9%) | T1 + T2 (75.2%) T3 + T4 (47.7%) | NA | Smoking (62.5%) Drinking (50.5%) | <64 (86%) ≥64 years (44%) |
| Baroudi et al. [81] | 2017 | miR-377-3p | 199 | Larynx 31% Oral cavity 64% Oropharynx 5% | GSEA | NA | Male (28%) | T1 (9%) T2 (18%) T3 (27%) T4 (53%) | NA | Smoking (52%) Alcohol (66%) | ≤ 70 years (80%) > 70 years (20%) |
| Berania et al. [82] | 2017 | miR-18a miR-548b | 58 | Oral tongue squamous cell carcinoma | qRT-PCR | Canada | Male (71%) | NA | NA | Smoking (72%) Drinking (41%) HPV (22%) | ≤ 50 (28%) > 50 (72%) |
| He et al. [83] | 2017 | miR-300 | 133 | Laryngeal squamous cell carcinoma | qRT-PCR | China | Male (65%) | T1 + T2 (50%) T3 + T4 (50%) | Metastasis + ve (55%) | NA | <50 (35%) ≥50 (65%) |
| Hess et al. [84] | 2017 | miR-200b miR-155 miR-146a | 149 | Oropharynx 52% Hypopharynx 48% | qRT-PCR | Germany | NA | NA | NA | NA | NA |
| Jiang et al. [85] | 2017 | miR-212 | 73 | Nasopharyngeal | qRT-PCR | China | Male (59%) | T1 + T2 (34%) T3 + T4 (66%) | Metastasis + ve (56%) | NA | ≤45 (48%) >45 (52%) |
| Liu et al. [86] | 2017 | let-7a | 131 | Thyroid | qRT-PCR | China | Male (33%) | T1 + T2 (39%) T3 + T4 (61%) | Metastasis + ve (53%) | NA | < 45 (44%) ≥ 45 (56%) |
| Re et al. [87] | 2017 | miR-34c-5p | 43 | Supraglottic (18.60%) Transglottic (76.74%) Subglottic (4.65%) | qRT-PCR | Italy | Male (97.67%) | T3 (72%) T4 (28%) | Metastasis + ve (0%) | NA | 66.51 ± 8.02 |
| Romeo et al. [88] | 2018 | miR-375 | 36 | Medullary thyroid | qRT-PCR | Italy | Male (58.3%) | T1 + T2 (25%) T3 + T4 (63.8%) | Metastasis + ve (72.2%) | NA | Mean 55.5 |
| Wilkins et al. [89] | 2018 | miR-100 miR-125b Let-7a | 2083 | Oral cavity (31.7%) Pharynx (52.7%) Larynx (15.6%) | Axiom miRNA Target Site Genotyping Array | USA | Male (24.5%) | T1 + T2 (25.9%) T3 + T4 (74.1%) | NA | Smoking [current] (25.9%) Smoking [former] (42.9%) | ≤50 (24.8%) >50 to ≤60 (36.2%) >60 to ≤70 (25.9%) >70 (13.1%) |
| Yu et al. [90] | 2017 | miR-21 | 100 | Buccal mucosa (37%) Tongue (35%) Mouth floor (12%) Others (16%) | Immunohistochemistry | China | Male (92%) | T1 + T2 (23%) T3 + T4 (77%) | Metastasis + ve (28%) | NA | ≤55 (56%) >55 (44%) |
3.3. Meta-Analysis
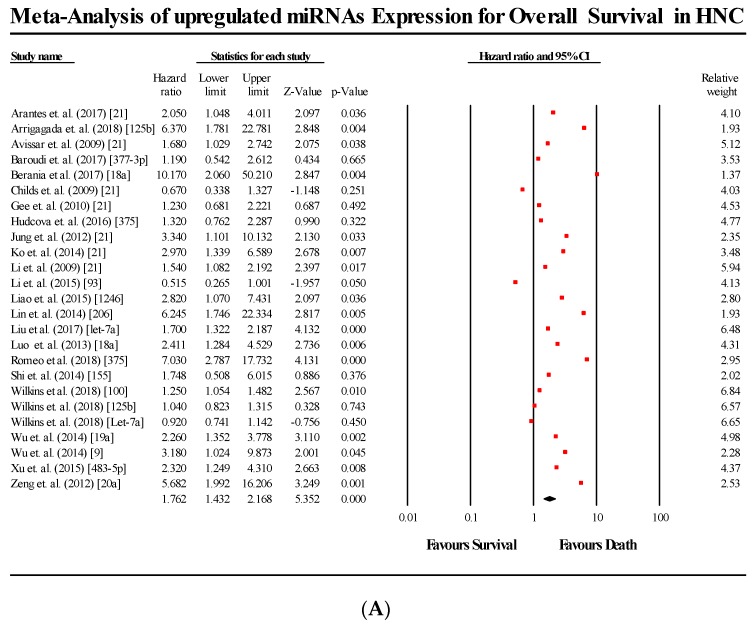
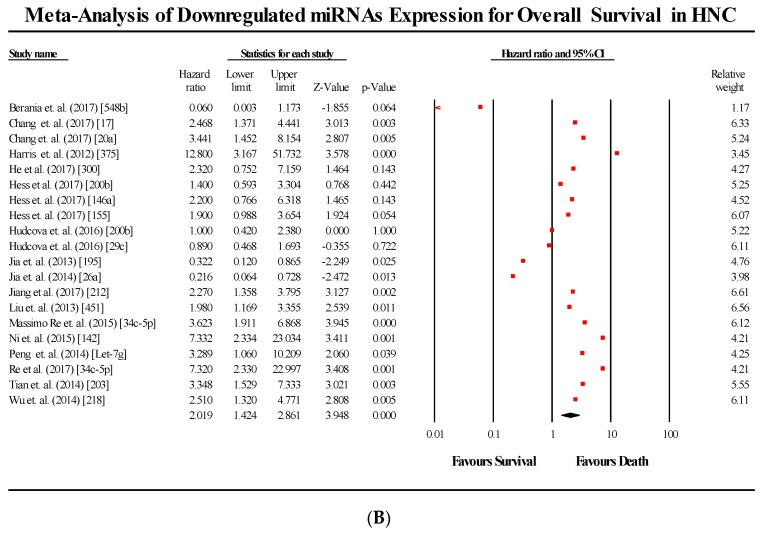
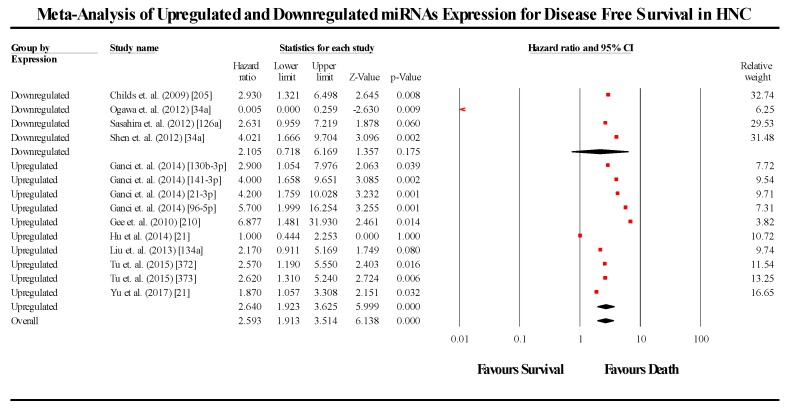
The primary meta-analysis studied the prognostic significance of 44 miRNA across 34 studies. The meta-analysis was conducted in 2 parts, based on the survival endpoint used by each study. The meta-analysis pooling the HR and 95% CIs of studies that used OS as their endpoint (n = 34), gave an overall effect size estimate (HR) of 1.825 (95% CI 1.527–2.181), while the pooled effect size estimate (HR) for studies using DFS as their survival endpoint was 2.596 (95% CI 1.917–3.514). The pooled effect estimate of OS studies (p < 0.05) as well as that of DFS studies (p < 0.05) were found to be statistically significant, thereby rejecting the null hypothesis. This indicates that any change in miRNA expression (either overexpressed or underexpressed) compared to controls, leads to a lower probability of survival in HNC patients. Additionally the between-study heterogeneity was found to be high, (I2 = 75.055; Tau2 = 0.228; Cochran’s Q= 176.38 for OS meta-analysis and I2 = 43.729; Tau2 = 0.155; Cochran’s Q = 23.103 for DFS). The forest plots of OS and DFS are presented in Figure 2 and Figure 3, respectively.
Figure 2.
Forest plots for the miRNAs associated with OS. (A) Upregulated miRNA; (B) Downregulated miRNA.
Figure 3.
Forest plot for the miRNAs associated with DFS.
3.4. Subgroup Analysis
3.4.1. Upregulation and Downregulation Subgroups
Subgroups were formed based on whether the miRNAs assessed in each study was found to be upregulated or downregulated compared to controls. The subgroups for upregulated and downregulated miRNA were assessed separately for OS and DFS.
For OS, the upregulated miRNA cohorts (n = 25) showed a pooled effect estimate (HR) of 1.762 (95% CI 1.432–2.168; p < 0.05), while the downregulated miRNA (n = 20) cohorts showed a pooled effect estimate (HR) of 2.018 (95% CI 1.431–2.168; p < 0.05). The results were also found to be statistically significant for both upregulation and downregulation.
For DFS, the upregulated miRNA cohort (n = 10) showed a pooled effect estimate (HR) of 2.641 (95% CI 1.925–3.623; p < 0.05), while the downregulated miRNA cohorts (n = 4) showed a pooled effect estimate (HR) of 2.135 (0.730–6.179; p > 0.05). Although the pooled effect estimate of studies assessing upregulated miRNA was statistically significant, the same was not observed in the downregulated miRNA studies. For the meta-analysis analysing the effect of downregulated miRNA on DFS, three out of the four cohorts indicated a lower probability of survival and were consistent, while a single study by Ogawa et al [57] was observed to be contradictory to the three studies above, and served to severely skew the overall pooled results. As three of the four studies were consistent with a reduced probability of survival, it is likely that the single study is the outlier, disregarding which, the pooled effect estimate of the three cohorts alone was found to be statistically significant (p < 0.05).
3.4.2. miRNA Subgroups
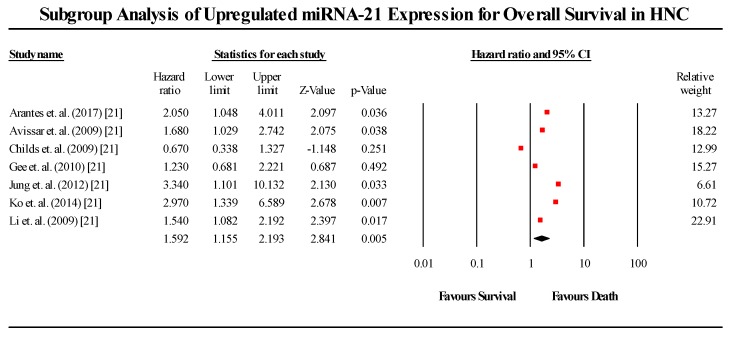
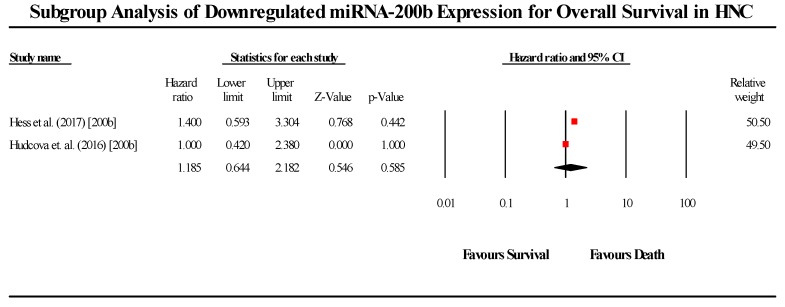
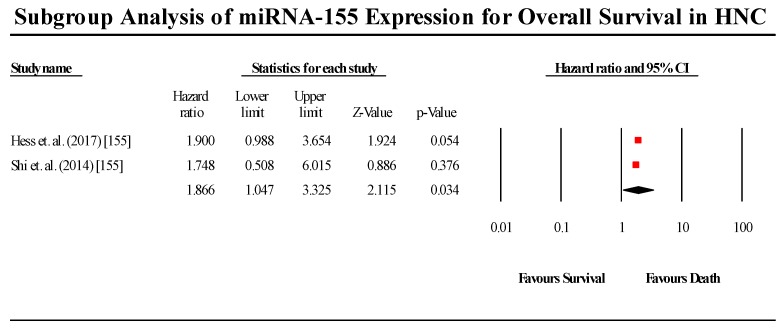
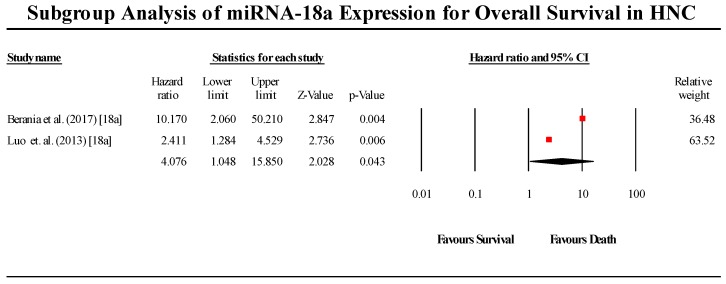
miRNA subgroups were selected based on the miRNA that was frequently represented in multiple cohorts across all studies included in the meta-analysis. miRNA subgroups were also assessed separately based on the survival endpoints (OS and DFS). The miRNA subgroups assessed are miR-21, 155, 200b, 18a, 34c-5p, 125b, 20a, and 375 for the OS group (Supplementary Figure S1A–H) and miR-21, and 34a for the DFS group (Supplementary Figure S2A,B).
3.5. Overall Survival Group
3.5.1. miR-21
A total of 7 studies assessed miR-21 expression in HNC patients in this group (Figure 4). All seven studies showed that miR-21 is upregulated in HNC patients. The pooled effect size estimate (HR) was found to be 1.591 (1.154–2.194; p < 0.05). The pooled effect estimate was statistically significant. Of the seven studies, six showed that upregulated miR-21 expression leads to a lower probability of survival, while a single study presented an outlier result, indicating the opposite. (I2 = 48.122; Tau2 = 0.085; Cochran’s Q = 11.566).
Figure 4.
Forest plot for miR-21 association with OS.
3.5.2. miR-200b
A total of 2 studies assessed miR-200b expression in HNC patients in this group (Figure 5). Both studies showed that miRNA-200b is downregulated in HNC patients. The pooled effect size estimate (HR) was found to be 1.185 (95% CI 0.644–2.182). Both studies individually did not present statistically significant results, and the pooled effect size estimate (HR) was similarly found to be non-significant. (I2 = 0.00; Tau2 = 0.00; Cochran’s Q = 0.292).
Figure 5.
Forest plot for miR-200b association with OS.
3.5.3. miR-155
A total of two studies assessed miR-155 expression in HNC patients (Figure 6). The two studies showed contradicting results regarding miR-155 expression in HNC, with the Hess et al. (2017) study indicating that miR-155 is downregulated in HNC, while the Shi et al. (2015) study claimed that miR-155 is upregulated in HNC. The pooled effect estimate (HR) was found to be statistically significant, with a value of 1.866 (95% CI 1.047–3.326; p < 0.05). However, contradicting results of the individual studies limits the applicability of these results to all HNC cases (I2 = 0.00; Tau2 = 0.00; Cochran’s Q = 0.014).
Figure 6.
Forest plot for miR-155 association with OS.
3.5.4. miR-18a
A total of 2 studies assessed miR-18a expression in HNC patients (Figure 7). Both studies indicated that miR-18a is upregulated in HNC. The pooled effect estimate (HR) was found to be statistically significant, with a value of 1.866 (95 % CI 1.047–3.326; p < 0.05). (I2 = 62.964; Tau2 = 0.652; Cochran’s Q = 2.7).
Figure 7.
Forest plot for miR-18a association with OS.
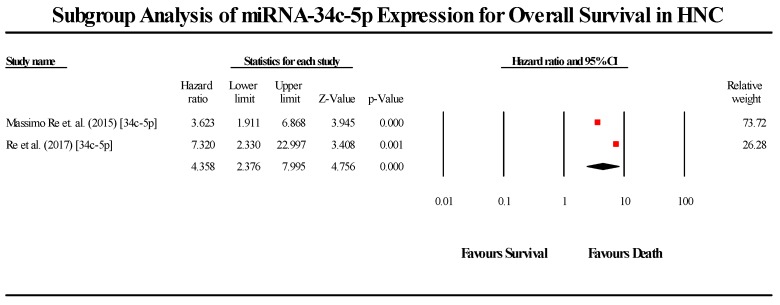
3.5.5. miR-34c-5p
A total of 2 studies assessed miR-34c-5p expression in HNC patients (Figure 8). Both studies indicated that miR-34c-5p is downregulated in HNC patients. The pooled effect estimate (HR) was found to be statistically significant, with a value of 4.358 (95% CI 2.376–7.995; p < 0.05). (I2 = 9.506; Tau2 = 0.024; Cochran’s Q = 1.105).
Figure 8.
Forest plot for miR-34c-5p association with OS.
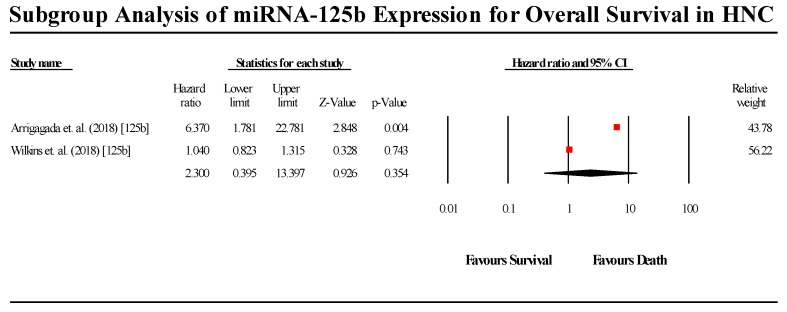
3.5.6. miR-125b
A total of 2 studies assessed miR-125b expression in HNC patients (Figure 9). Both studies indicated that miR-125b is upregulated in HNC patients. The pooled effect estimate (HR) was found to be 2.3 (95% CI 0.395–13.397; p > 0.05). The results were not statistically significant, although, of the two studies, the Arrigagada et al. (2018) study was found to be statistically significant, indicating miR-125b upregulation leads to a lower probability of patient survival, while the Wilkins et al. (2018) study did not reject the null hypothesis. (I2 = 86.696; Tau2 = 1.424; Cochran’s Q = 7.516).
Figure 9.
Forest plot for miR-125b for association with OS.
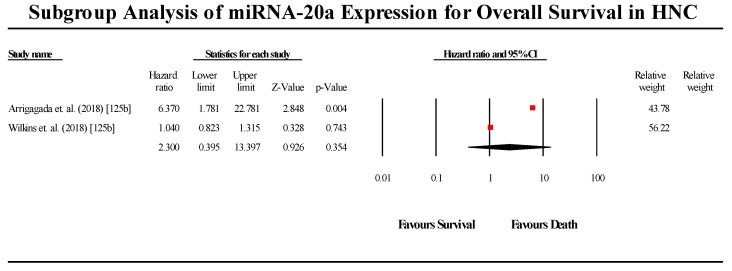
3.5.7. miR-20a
A total of two studies assessed miR-20a expression in HNC patients (Figure 10). The two studies showed contradicting results regarding miR-20a expression in HNC, with the Chang et al. (2017) study indicating that miR-20a is downregulated in HNC, while the Zeng et al. (2012) study claimed that miR-20a is upregulated in HNC. The pooled effect estimate (HR) was found to be statistically significant, with a value of 4.214 (95% CI 2.165–8.203; p < 0.05). However, contradicting results of the individual studies limits the applicability of these results to all HNC cases. (I2 = 0.00; Tau2 = 0.00; Cochran’s Q = 0.524).
Figure 10.
Forest plot for miR-20a association with OS.
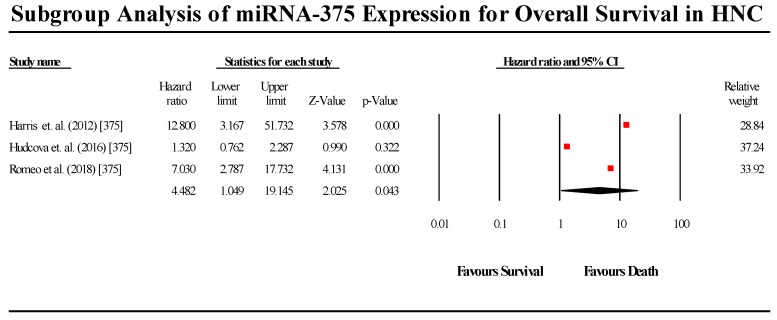
3.5.8. miR-375
A total of 3 studies assessed miR-375 expression in HNC patients (Figure 11). Of the three studies, two indicated that miR-375 is upregulated in HNC, while 1 study by Harris et al. (2012) claimed that miR-375 is downregulated in HNC patients. The overall pooled effect estimate (HR) was statistically significant, with a value of 4.482 (95% CI 1.049–19.145). Individually, only the Harris et al. (2012) study results did not reject the null hypothesis, while the remaining two studies individually showed a high degree of statistical significance. Therefore, we may consider the Harris et al. (2012) study as the outlier in this group of studies. (I2 = 86.872; Tau2 = 1.395; Cochran’s Q = 15.235).
Figure 11.
Forest plot for miR-375 association with OS.
3.6. Disease-Free Survival Group
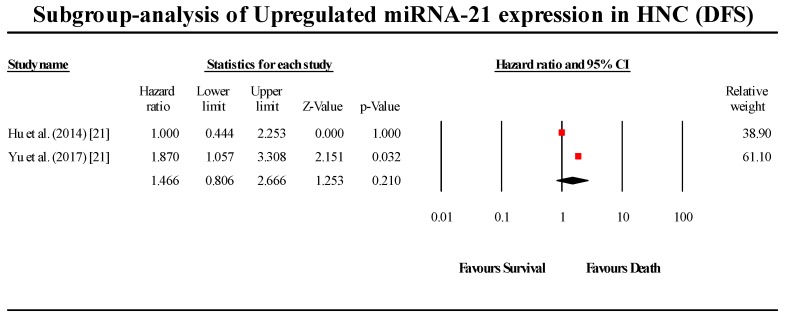
3.6.1. miR-21
A total of two studies assessed miR-21 expression in HNC patients in this group (Figure 12). Both studies indicated that miR-21 is upregulated in HNC. The pooled effect size estimate (HR) was found to be 1.466 (95% CI 0.806–2.666; p > 0.05). The pooled results were not statistically significant. (I2 = 34.5; Tau2 = 0.068; Cochran’s Q = 1.527).
Figure 12.
Forest plot for miR-21 association with DFS.
3.6.2. miR-34a
A total of two studies assessed miR-34a expression in HNC patients in this group (Figure 13). Both studies indicated that miR-34a is downregulated in HNC. The pooled effect size estimate (HR) was found to be 0.190 (95% CI 0.001–130.514; p > 0.05). The results were not found to be statistically significant. (I2 = 90.317; Tau2 = 20.210; Cochran’s Q = 10.327).
Figure 13.
Forest plot for miR-34a association with DFS.
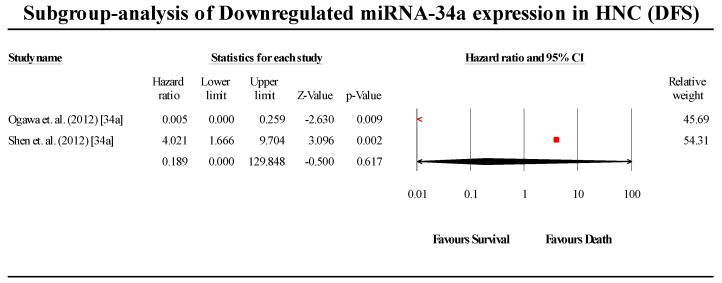
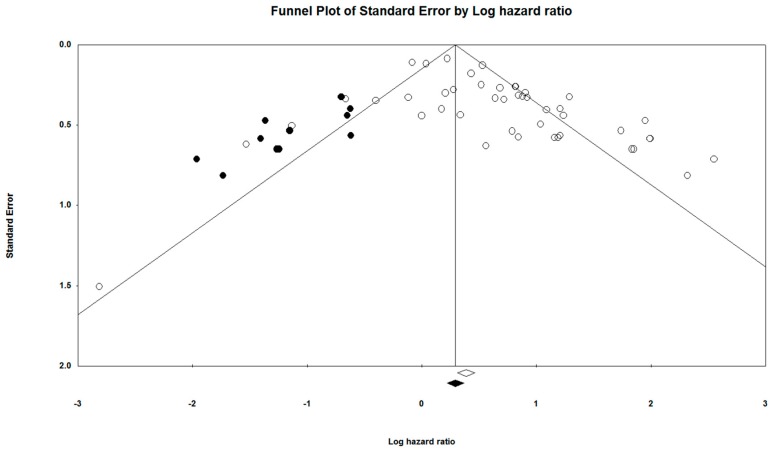
3.7. Publication Bias
The Egger’s graphical test was used to assess for publication bias. The funnel plot was constructed alongside the meta-analysis using the CMA software (Ver 3.3.070, USA). The funnel plots provided in Figure 14 and Figure 15 visually represent the likelihood of publication bias in the OS and DFS groups, respectively, of this systematic review and meta-analysis study. The funnel plot for OS was observed to be slightly asymmetric with a more significant number of studies falling on the right of the line of mean effect. Trim and fill was used to impute for possible missing studies, which led to the imputation of 12 missing studies, adjusting the point estimate and its 95% CI from 1.90043 (1.58306–2.28143) to 1.21935 (1.17451–1.71522), after imputation. Orwin’s Fail-safe N test did not apply to this assessment of publication bias, since the HR of observed studies did not fall between the HRs of the missing studies. Begg and Mazumdar’s rank correlation test presented a Kendall’s Tau value of 0.21919, with continuity correction. For the DFS group, the funnel plot was relatively symmetrical, with the trim and fill required to adjust for two missing studies. Overall, publication bias was not found to have any significant impact on the results of this meta-analysis.
Figure 14.
Funnel plot for the studies prognostic of OS.
Figure 15.
Funnel plot for the studies prognostic of DFS.
3.8. Quality Assessment
The NHLBI Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies was used to assess the quality of included studies. A majority of the studies had good quality scores (38/50), with all the rest having satisfactory scores. However, the core requirement for inclusion into the meta-analysis was based on the availability of good quality statistical data (HR and 95% CI).
4. Discussion
This systematic review and meta-analysis were conducted to investigate the prognostic potential of miRNA as biomarkers in HNC, via exploring the association between miRNA expression and survival in HNC patients. The use of miRNAs as prognostic markers in HNC has been the subject of much research, with previous studies reporting that miRNAs have both tumour-suppressing and oncogenic roles and may be either upregulated or downregulated in HNC patients. Therefore, in lieu of miRNAs impact upon cancer progression, they have also been proposed as potential biomarkers predicting patient prognosis. Previous studies have pursued this thread of logic, and have attempted to identify miRNAs that may have the capacity of being utilised as prognostic markers. However, despite this, no new miRNAs have been proposed as prognostic markers in HNC. Furthermore, no previous study has attempted to explore the prognostic potential of multiple miRNAs, as well as explore the impact on HNC based on the magnitude and direction of the deregulation of miRNA expression. This study is the first systematic review and meta-analysis on this topic to have assessed such a wide variety of miRNA and assessed their capacity to act as prognostic markers.
A previous study has also conducted a similar systematic review and meta-analysis [6]. However, the study only focused on miR-21 as a potential prognostic marker in HNC and did not explore the impact or differences of upregulation or downregulation of miRNA on the prognosis of HNC patients. Another previous meta-analysis study was conducted, regarding HNC and miRNA, but focused on the molecular network aspects of miRNA and cancer rather than the clinical utility of miRNA.
This systematic review and meta-analysis of 50 studies involving 6843 patients, investigating the prognostic value of 43 different miRNA summarises the results via pooled HR values as the effect size estimate of the study. While all miRNA were assessed in a combined meta-analysis to observe their prognostic potential of miRNA as a whole, a few select miRNAs were individually assessed to identify and highlight the specific miRNA which may have potential clinical utility. These miRNA were miR-21, 200b, 155, 18a, 34c-5p, 125b, 20a, 375 and 34a.
While multiple studies were pooled for miR-21 and miR-375, only two cohorts each were pooled for the rest of the miRNAs. miR-21 has been reported as an oncogenic factor and a potential prognostic marker indicating a poor prognosis in multiple types of cancers. Therefore, even though miR-21 is well known for its prognostic potential in cancers, it is not specific to detecting HNC, and is therefore not an ideal miRNA for HNC prognosis in particular. miR-375 is similarly found to be expressed in several cancer types, thereby indicating its lack of specificity. Nevertheless, miR-21 and 375 are dominant miRNA markers for cancer in general and could be considered as prognostic markers for HNC in conjunction with other cancers.
miR-155 and 20a have significant HR values; however, the conflicting reports of the individual studies regarding whether they are upregulated or downregulated hampers their potential for use in the clinical scenario. This uncertainty requires further investigation in longitudinal cohort studies, where the effect of miR-155 and 20a in HNC is further verified, and consistent results are observed.
miR-200b and 125b have effect sizes that are non-significant and do not reject the null hypothesis. This implies that both these miRNAs have a low power of detection, and may not be suitable for use as prognostic markers. However, future studies with larger patient cohorts presenting significant results concerning miR-200b and 125b may serve to highlight the prognostic potential of these miRNA.
miR-18a and 34c-5p are miRNAs offer great potential for prognostic markers in HNC. The effect size values of the pooled results for both miRNAs are significant, as well as high in magnitude, indicating a high power of prognosis. However, as the meta-analysis for these two miRNA was conducted based on the pooling of only two studies each, further verification in future studies is necessary.
This study does have a few limitations [34,91,92,93]. Ideally, meta-analysis should be conducted on all miRNA included in the study. However, this is limited by the quantity of high-quality literature and data that is published in this field. Additionally, this same limitation also makes accounting for other subgroups such as ethnicity, gender and age impossible, as forming these subgroups would fragment the data even further, such that no analysis can be conducted. This meta-analysis was also conducted using HR and 95% CI values extracted from KM curves, which requires approximations to be made during the extraction process, thus introducing some degree of error into the study.
Overall, this systematic review and meta-analysis highlight the miRNA that may have the potential for use as prognostic biomarkers in HNC patients. As the pool of available literature regarding this topic continues to expand, recognizing the influence of miRNAs as a whole and select miRNA specifically may facilitate the transfer of the prognostic value of miRNA from the hypothetical to the clinical sphere of HNC treatment and prognosis.
5. Conclusions
The study highlights miR-21, 375, 155, 18a, 34c-5p, 125b, 20a and 375 as miRNA markers that may have the potential for clinical use as prognostic markers in HNC. However, further validation is imperative before we can confirm their utility. Although a few of the miRNA have shown significant results concerning impacting patient survival, the small number of studies that have been pooled to generate the results reduces their applicability in the clinical sphere. Therefore, further large scale and longitudinal patient studies focusing on these miRNA are required.
Acknowledgments
We would like to acknowledge the meta-analysis concepts and applications workshop manual by Michael Borenstein for his guidelines on reporting meta-analysis, subgroup analysis and publication bias, (www.meta-analysis-workshops.com).
Supplementary Materials
The following are available online at https://www.mdpi.com/2073-4409/8/8/772/s1. Table S1. Prisma checklist, Table S2. Hypothesis testing table for OS (Overall Survival) and DFS (Disease Free Survival), Table S3. Hypothesis testing table for individual miRNA under the endpoints of OS and DFS.
Author Contributions
R.J. and C.K. contributed to the conceptualisation, study design, search strategy, protocol development, and review by revising different versions. R.J., C.K., M.R.M., S.S., S.B., A.G., S.K. and K.M.G. provided input into the study design, supervision, ensured the absence of errors and arbitrated in case of disagreement. C.K., M.R.M., S.S. and R.J. engaged in initial searches to determine the feasibility, data collection, analysis and drafting the manuscript. All authors read and approved the final version of the manuscript.
Funding
This work was not supported by any funding source.
Conflicts of Interest
The authors declare no competing interests.
References
- 1.Jemal A., Bray F., Center M.M., Ferlay J., Ward E., Forman D. Global cancer statistics. Ca A Cancer J. Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Dhull A.K., Atri R., Dhankhar R., Chauhan A.K., Kaushal V. Major Risk Factors in Head and Neck Cancer: A Retrospective Analysis of 12-Year Experiences. World J. Oncol. 2018;9:80–84. doi: 10.14740/wjon1104w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mehanna H., West C.M.L., Nutting C., Paleri V. Head and neck cancer—Part 2: Treatment and prognostic factors. Bmj. 2010;341:c4690. doi: 10.1136/bmj.c4690. [DOI] [PubMed] [Google Scholar]
- 4.Denaro N., Merlano M.C., Russi E.G. Follow-up in head and neck cancer: Do more does it mean do better? A systematic review and our proposal based on our experience. Clin. Exp. Otorhinolaryngol. 2016;9:287. doi: 10.21053/ceo.2015.00976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mehanna H., Kong A., Ahmed S.K. Recurrent head and neck cancer: United Kingdom National Multidisciplinary Guidelines. J. Laryngol. Otol. 2016;130:S181–S190. doi: 10.1017/S002221511600061X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jamali Z., Asl Aminabadi N., Attaran R., Pournagiazar F., Ghertasi Oskouei S., Ahmadpour F. MicroRNAs as prognostic molecular signatures in human head and neck squamous cell carcinoma: A systematic review and meta-analysis. Oral Oncol. 2015;51:321–331. doi: 10.1016/j.oraloncology.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 7.Macfarlane L.-A., Murphy P.R. MicroRNA: Biogenesis, Function and Role in Cancer. Curr. Genom. 2010;11:537–561. doi: 10.2174/138920210793175895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xie Y., Ma X., Chen L., Li H., Gu L., Gao Y., Zhang Y., Li X., Fan Y., Chen J. MicroRNAs with prognostic significance in bladder cancer: A systematic review and meta-analysis. Sci. Rep. 2017;7:5619. doi: 10.1038/s41598-017-05801-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gu W., Xu Y., Xie X., Wang T., Ko J.H., Zhou T. The role of RNA structure at 5’ untranslated region in microRNA-mediated gene regulation. RNA. 2014;20:1369–1375. doi: 10.1261/rna.044792.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Felekkis K., Touvana E., Stefanou C., Deltas C. microRNAs: A newly described class of encoded molecules that play a role in health and disease. Hippokratia. 2010;14:236–240. [PMC free article] [PubMed] [Google Scholar]
- 11.Wahid F., Shehzad A., Khan T., Kim Y.Y. MicroRNAs: Synthesis, mechanism, function, and recent clinical trials. Biochim. Biophys. Acta (Bba)-Mol. Cell Res. 2010;1803:1231–1243. doi: 10.1016/j.bbamcr.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 12.Schoof C.R.G., Botelho E.L.d.S., Izzotti A., Vasques L.D.R. MicroRNAs in cancer treatment and prognosis. Am. J. Cancer Res. 2012;2:414–433. [PMC free article] [PubMed] [Google Scholar]
- 13.Khawar M.B., Fatima N., Abbasi M.H., Mehmood R., Suqaina S.K., Sheikh N. Diagnosis and Management of Head and Neck Cancer. IntechOpen; Rijeka, Croatia: 2017. Head and neck cancer: Epidemiology and role of microRNAs. [Google Scholar]
- 14.Moher D., Liberati A., Tetzlaff J., Altman D.G., Group P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Heart L.a.B.I. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. [(accessed on 12 February 2018)]; Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
- 16.Borenstein M., Rothstein H. Comprehensive Meta-Analysis. Biostat; Englewood, NJ, USA: 1999. [Google Scholar]
- 17.Hedges L.V., Vevea J.L. Fixed-and random-effects models in meta-analysis. Psychol. Methods. 1998;3:486. doi: 10.1037/1082-989X.3.4.486. [DOI] [Google Scholar]
- 18.Higgins J.P.T., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cochran W.G. The comparison of percentages in matched samples. Biometrika. 1950;37:256–266. doi: 10.1093/biomet/37.3-4.256. [DOI] [PubMed] [Google Scholar]
- 20.Deeks J.J., Higgins J.P.T., Altman D.G. Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Collaboration; London, UK: 2008. Analysing data and undertaking meta-analyses; pp. 243–296. (Cochrane Book Series). [Google Scholar]
- 21.Von Hippel P.T. The heterogeneity statistic I(2) can be biased in small meta-analyses. BMC Med. Res. Methodol. 2015;15:35. doi: 10.1186/s12874-015-0024-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jayaraj R., Kumarasamy C., Madhav M.R., Pandey V., Sabarimurugan S., Ramesh N., Gothandam K.M., Baxi S. Comment on “Systematic Review and Meta-Analysis of Diagnostic Accuracy of miRNAs in Patients with Pancreatic Cancer”. Dis. Mark. 2018;2018:6904569. doi: 10.1155/2018/6904569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jayaraj R., Kumarasamy C. Comment on ‘Prognostic biomarkers for oral tongue squamous cell carcinoma: A systematic review and meta-analysis’. Br. J. Cancer. 2018;118:e11. doi: 10.1038/bjc.2017.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jayaraj R., Kumarasamy C., Sabarimurugan S., Baxi S. Letter to the Editor in response to the article. “The epidemiology of oral human papillomavirus infection in healthy populations: A systematic review and meta-analysis”. Oral Oncol. 2018;84:121–122. doi: 10.1016/j.oraloncology.2018.07.018. [DOI] [PubMed] [Google Scholar]
- 25.Jayaraj R., Kumarasamy C., Sabarimurugan S., Baxi S. Commentary: Blood-Derived microRNAs for Pancreatic Cancer Diagnosis: A Narrative Review and Meta-Analysis. Front. Physiol. 2018;9:1896. doi: 10.3389/fphys.2018.01896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jayaraj R., Kumarasamy C. Conceptual interpretation of analysing and reporting of results on systematic review and meta-analysis of optimal extent of lateral neck dissection for well-differentiated thyroid carcinoma with metastatic lateral neck lymph nodes. Oral Oncol. 2019;89:153. doi: 10.1016/j.oraloncology.2018.12.031. [DOI] [PubMed] [Google Scholar]
- 27.Jayaraj R., Kumarasamy C.J.A.R. Conceptual, statistical and clinical interpretation of results from a systematic review and meta-analysis of prevalence of cervical HPV infection in women with SLE. Autoimmun. Rev. 2019;18:433–434. doi: 10.1016/j.autrev.2018.12.003. [DOI] [PubMed] [Google Scholar]
- 28.Jayaraj R., Kumarasamy C., Gothandam K.M. Letter to the editor “Prognostic value of microRNAs in colorectal cancer: A meta-analysis”. Cancer Manag. Res. 2018;10:3501–3503. doi: 10.2147/CMAR.S177875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jayaraj R., Kumarasamy C. Letter to the Editor about the Article: “Performance of different imaging techniques in the diagnosis of head and neck cancer mandibular invasion: A systematic review and meta-analysis”. J. Oral Oncol. 2018;89:159–160. doi: 10.1016/j.oraloncology.2018.12.024. [DOI] [PubMed] [Google Scholar]
- 30.Kumarasamy C., Devi A., Jayaraj R. Prognostic value of microRNAs in head and neck cancers: A systematic review and meta-analysis protocol. Syst. Rev. 2018;7:150. doi: 10.1186/s13643-018-0812-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jayaraj R., Kumarasamy C. Comment on, “Survival for HPV-positive oropharyngeal squamous cell carcinoma with surgical versus non-surgical treatment approach: A systematic review and meta-analysis”. J. Oral Oncol. 2018;90:137–138. doi: 10.1016/j.oraloncology.2018.12.019. [DOI] [PubMed] [Google Scholar]
- 32.Jayaraj R., Kumarasamy C. Systematic review and meta-analysis of cancer studies evaluating diagnostic test accuracy and prognostic values: Approaches to improve clinical interpretation of results. Cancer Manag. Res. 2018;10:4669–4670. doi: 10.2147/CMAR.S183181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jayaraj R., Kumarasamy C., Ramalingam S., Devi A. Systematic review and meta-analysis of risk-reductive dental strategies for medication related osteonecrosis of the jaw among cancer patients: Approaches and strategies. Oral Oncol. 2018;86:312–313. doi: 10.1016/j.oraloncology.2018.09.017. [DOI] [PubMed] [Google Scholar]
- 34.Sabarimurugan S., Kumarasamy C., Baxi S., Devi A., Jayaraj R. Systematic review and meta-analysis of prognostic microRNA biomarkers for survival outcome in nasopharyngeal carcinoma. PLoS ONE. 2019;14:e0209760. doi: 10.1371/journal.pone.0209760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sabarimurugan S., Madurantakam Royam M., Das A., Das S., Gothandam K.M., Jayaraj R. Systematic Review and Meta-analysis of the Prognostic Significance of miRNAs in Melanoma Patients. Mol. Diagn. 2018;22:653–669. doi: 10.1007/s40291-018-0357-5. [DOI] [PubMed] [Google Scholar]
- 36.Jayaraj R., Kumarasamy C., Piedrafita D. Systematic review and meta-analysis protocol for Fasciola DNA vaccines. Online J. Vet. Res. 2018;22:517. [Google Scholar]
- 37.Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Orwin R.G. A fail-safe N for effect size in meta-analysis. J. Educ. Stat. 1983;8:157–159. doi: 10.2307/1164923. [DOI] [Google Scholar]
- 39.Duval S., Tweedie R. Trim and fill: A simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341X.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 40.Begg C.B., Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- 41.De Carvalho A.C., Scapulatempo-Neto C., Maia D.C.C., Evangelista A.F., Morini M.A., Carvalho A.L., Vettore A.L. Accuracy of microRNAs as markers for the detection of neck lymph node metastases in patients with head and neck squamous cell carcinoma. BMC Med. 2015;13:108. doi: 10.1186/s12916-015-0350-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hou B., Ishinaga H., Midorikawa K., Shah S.A., Nakamura S., Hiraku Y., Oikawa S., Murata M., Takeuchi K. Circulating microRNAs as novel prognosis biomarkers for head and neck squamous cell carcinoma. Cancer Biol. Ther. 2015;16:1042–1046. doi: 10.1080/15384047.2015.1045692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Maia D., de Carvalho A.C., Horst M.A., Carvalho A.L., Scapulatempo-Neto C., Vettore A.L. Expression of miR-296-5p as predictive marker for radiotherapy resistance in early-stage laryngeal carcinoma. J. Transl. Med. 2015;13:262. doi: 10.1186/s12967-015-0621-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hudcova K., Raudenska M., Gumulec J., Binkova H., Horakova Z., Kostrica R., Babula P., Adam V., Masarik M. Expression profiles of miR-29c, miR-200b and miR-375 in tumour and tumour-adjacent tissues of head and neck cancers. Tumor Biol. 2016;37:12627–12633. doi: 10.1007/s13277-016-5147-2. [DOI] [PubMed] [Google Scholar]
- 45.Wang H., Zhang G., Wu Z., Lu B., Yuan D., Li X., Lu Z. MicoRNA-451 is a novel tumor suppressor via targeting c-myc in head and neck squamous cell carcinomas. J. Cancer Res. Ther. 2015;11:216. doi: 10.4103/0973-1482.168189. [DOI] [PubMed] [Google Scholar]
- 46.Arantes L.M.R.B., Laus A.C., Melendez M.E., de Carvalho A.C., Sorroche B.P., De Marchi P.R.M., Evangelista A.F., Scapulatempo-Neto C., de Souza Viana L., Carvalho A.L. MiR-21 as prognostic biomarker in head and neck squamous cell carcinoma patients undergoing an organ preservation protocol. Oncotarget. 2017;8:9911. doi: 10.18632/oncotarget.14253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Xu H., Yang Y., Zhao H., Yang X., Luo Y., Ren Y., Liu W., Li N. Serum miR-483-5p: A novel diagnostic and prognostic biomarker for patients with oral squamous cell carcinoma. Tumor Biol. 2016;37:447–453. doi: 10.1007/s13277-015-3514-z. [DOI] [PubMed] [Google Scholar]
- 48.Li G., Ren S., Su Z., Liu C., Deng T., Huang D., Tian Y., Qiu Y., Liu Y. Increased expression of miR-93 is associated with poor prognosis in head and neck squamous cell carcinoma. Tumor Biol. 2015;36:3949–3956. doi: 10.1007/s13277-015-3038-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hu A., Huang J.-J., Xu W.-H., Jin X.-J., Li J.-P., Tang Y.-J., Huang X.-F., Cui H.-J., Sun G.-B. miR-21 and miR-375 microRNAs as candidate diagnostic biomarkers in squamous cell carcinoma of the larynx: Association with patient survival. Am. J. Transl. Res. 2014;6:604. [PMC free article] [PubMed] [Google Scholar]
- 50.Hedbäck N., Jensen D.H., Specht L., Fiehn A.-M.K., Therkildsen M.H., Friis-Hansen L., Dabelsteen E., von Buchwald C. MiR-21 expression in the tumor stroma of oral squamous cell carcinoma: An independent biomarker of disease free survival. PLoS ONE. 2014;9:e95193. doi: 10.1371/journal.pone.0095193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sun L., Liu B., Lin Z., Yao Y., Chen Y., Li Y., Chen J., Yu D., Tang Z., Wang B. MiR-320a acts as a prognostic factor and Inhibits metastasis of salivary adenoid cystic carcinoma by targeting ITGB3. Mol. Cancer. 2015;14:96. doi: 10.1186/s12943-015-0344-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Saito K., Inagaki K., Kamimoto T., Ito Y., Sugita T., Nakajo S., Hirasawa A., Iwamaru A., Ishikura T., Hanaoka H. MicroRNA-196a is a putative diagnostic biomarker and therapeutic target for laryngeal cancer. PLoS ONE. 2013;8:e71480. doi: 10.1371/journal.pone.0071480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li J., Huang H., Sun L., Yang M., Pan C., Chen W., Wu D., Lin Z., Zeng C., Yao Y. MiR-21 indicates poor prognosis in tongue squamous cell carcinomas as an apoptosis inhibitor. Clin. Cancer Res. 2009;15:3998–4008. doi: 10.1158/1078-0432.CCR-08-3053. [DOI] [PubMed] [Google Scholar]
- 54.Liu N., Chen N.-Y., Cui R.-X., Li W.-F., Li Y., Wei R.-R., Zhang M.-Y., Sun Y., Huang B.-J., Chen M. Prognostic value of a microRNA signature in nasopharyngeal carcinoma: A microRNA expression analysis. Lancet Oncol. 2012;13:633–641. doi: 10.1016/S1470-2045(12)70102-X. [DOI] [PubMed] [Google Scholar]
- 55.Summerer I., Niyazi M., Unger K., Pitea A., Zangen V., Hess J., Atkinson M.J., Belka C., Moertl S., Zitzelsberger H. Changes in circulating microRNAs after radiochemotherapy in head and neck cancer patients. Radiat. Oncol. 2013;8:296. doi: 10.1186/1748-717X-8-296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Suh Y.E., Raulf N., Gäken J., Lawler K., Urbano T.G., Bullenkamp J., Gobeil S., Huot J., Odell E., Tavassoli M. MicroRNA-196a promotes an oncogenic effect in head and neck cancer cells by suppressing annexin A1 and enhancing radioresistance. Int. J. Cancer. 2015;137:1021–1034. doi: 10.1002/ijc.29397. [DOI] [PubMed] [Google Scholar]
- 57.Ogawa T., Saiki Y., Shiga K., Chen N., Fukushige S., Sunamura M., Nagase H., Hashimoto S., Matsuura K., Saijo S. mi R-34a is downregulated in cis-diamminedichloroplatinum treated sinonasal squamous cell carcinoma patients with poor prognosis. Cancer Sci. 2012;103:1737–1743. doi: 10.1111/j.1349-7006.2012.02338.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Avissar M., McClean M.D., Kelsey K.T., Marsit C.J. MicroRNA expression in head and neck cancer associates with alcohol consumption and survival. Carcinogenesis. 2009;30:2059–2063. doi: 10.1093/carcin/bgp277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Re M., Çeka A., Rubini C., Ferrante L., Zizzi A., Gioacchini F.M., Tulli M., Spazzafumo L., Sellari-Franceschini S., Procopio A.D. Micro RNA-34c-5p is related to recurrence in laryngeal squamous cell carcinoma. Laryngoscope. 2015;125:E306–E312. doi: 10.1002/lary.25475. [DOI] [PubMed] [Google Scholar]
- 60.Sun Q., Zhang J., Cao W., Wang X., Xu Q., Yan M., Wu X., Chen W. Dysregulated miR-363 affects head and neck cancer invasion and metastasis by targeting podoplanin. Int. J. Biochem. Cell Biol. 2013;45:513–520. doi: 10.1016/j.biocel.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 61.Tian L., Li M., Ge J., Guo Y., Sun Y., Liu M., Xiao H. MiR-203 is downregulated in laryngeal squamous cell carcinoma and can suppress proliferation and induce apoptosis of tumours. Tumour Biol. J. Int. Soc. Oncodev. Biol. Med. 2014;35:5953–5963. doi: 10.1007/s13277-014-1790-7. [DOI] [PubMed] [Google Scholar]
- 62.Chang C.-C., Yang Y.-J., Li Y.-J., Chen S.-T., Lin B.-R., Wu T.-S., Lin S.-K., Kuo M.Y.-P., Tan C.-T. MicroRNA-17/20a functions to inhibit cell migration and can be used a prognostic marker in oral squamous cell carcinoma. Oral Oncol. 2013;49:923–931. doi: 10.1016/j.oraloncology.2013.03.430. [DOI] [PubMed] [Google Scholar]
- 63.Gee H.E., Camps C., Buffa F.M., Patiar S., Winter S.C., Betts G., Homer J., Corbridge R., Cox G., West C.M., et al. hsa-mir-210 is a marker of tumor hypoxia and a prognostic factor in head and neck cancer. Cancer. 2010;116:2148–2158. doi: 10.1002/cncr.25009. [DOI] [PubMed] [Google Scholar]
- 64.Lenarduzzi M., Hui A.B., Alajez N.M., Shi W., Williams J., Yue S., O’Sullivan B., Liu F.F. MicroRNA-193b enhances tumor progression via down regulation of neurofibromin 1. PLoS ONE. 2013;8:e53765. doi: 10.1371/journal.pone.0053765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Childs G., Fazzari M., Kung G., Kawachi N., Brandwein-Gensler M., McLemore M., Chen Q., Burk R.D., Smith R.V., Prystowsky M.B., et al. Low-level expression of microRNAs let-7d and miR-205 are prognostic markers of head and neck squamous cell carcinoma. Am. J. Pathol. 2009;174:736–745. doi: 10.2353/ajpath.2009.080731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Shen Z., Zhan G., Ye D., Ren Y., Cheng L., Wu Z., Guo J. MicroRNA-34a affects the occurrence of laryngeal squamous cell carcinoma by targeting the antiapoptotic gene survivin. Med. Oncol. 2012;29:2473–2480. doi: 10.1007/s12032-011-0156-x. [DOI] [PubMed] [Google Scholar]
- 67.Luo Z., Dai Y., Zhang L., Jiang C., Li Z., Yang J., McCarthy J.B., She X., Zhang W., Ma J., et al. miR-18a promotes malignant progression by impairing microRNA biogenesis in nasopharyngeal carcinoma. Carcinogenesis. 2013;34:415–425. doi: 10.1093/carcin/bgs329. [DOI] [PubMed] [Google Scholar]
- 68.Jung H.M., Phillips B.L., Patel R.S., Cohen D.M., Jakymiw A., Kong W.W., Cheng J.Q., Chan E.K. Keratinization-associated miR-7 and miR-21 regulate tumor suppressor reversion-inducing cysteine-rich protein with kazal motifs (RECK) in oral cancer. J. Biol. Chem. 2012;287:29261–29272. doi: 10.1074/jbc.M112.366518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sasahira T., Kurihara M., Bhawal U.K., Ueda N., Shimomoto T., Yamamoto K., Kirita T., Kuniyasu H. Downregulation of miR-126 induces angiogenesis and lymphangiogenesis by activation of VEGF-A in oral cancer. Br. J. Cancer. 2012;107:700–706. doi: 10.1038/bjc.2012.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Liu C.J., Shen W.G., Peng S.Y., Cheng H.W., Kao S.Y., Lin S.C., Chang K.W. miR-134 induces oncogenicity and metastasis in head and neck carcinoma through targeting WWOX gene. Int. J. Cancer. 2014;134:811–821. doi: 10.1002/ijc.28358. [DOI] [PubMed] [Google Scholar]
- 71.Shi L.J., Zhang C.Y., Zhou Z.T., Ma J.Y., Liu Y., Bao Z.X., Jiang W.W. MicroRNA-155 in oral squamous cell carcinoma: Overexpression, localization, and prognostic potential. Head Neck. 2015;37:970–976. doi: 10.1002/hed.23700. [DOI] [PubMed] [Google Scholar]
- 72.Harris T., Jimenez L., Kawachi N., Fan J.-B., Chen J., Belbin T., Ramnauth A., Loudig O., Keller C.E., Smith R., et al. Low-level expression of miR-375 correlates with poor outcome and metastasis while altering the invasive properties of head and neck squamous cell carcinomas. Am. J. Pathol. 2012;180:917–928. doi: 10.1016/j.ajpath.2011.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Huang W.C., Chan S.H., Jang T.H., Chang J.W., Ko Y.C., Yen T.C., Chiang S.L., Chiang W.F., Shieh T.Y., Liao C.T., et al. miRNA-491-5p and GIT1 serve as modulators and biomarkers for oral squamous cell carcinoma invasion and metastasis. Cancer Res. 2014;74:751–764. doi: 10.1158/0008-5472.CAN-13-1297. [DOI] [PubMed] [Google Scholar]
- 74.Shiiba M., Shinozuka K., Saito K., Fushimi K., Kasamatsu A., Ogawara K., Uzawa K., Ito H., Takiguchi Y., Tanzawa H. MicroRNA-125b regulates proliferation and radioresistance of oral squamous cell carcinoma. Br. J. Cancer. 2013;108:1817–1821. doi: 10.1038/bjc.2013.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zeng X., Xiang J., Wu M., Xiong W., Tang H., Deng M., Li X., Liao Q., Su B., Luo Z., et al. Circulating miR-17, miR-20a, miR-29c, and miR-223 combined as non-invasive biomarkers in nasopharyngeal carcinoma. PLoS ONE. 2012;7:e46367. doi: 10.1371/journal.pone.0046367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Liu N., Jiang N., Guo R., Jiang W., He Q.M., Xu Y.F., Li Y.Q., Tang L.L., Mao Y.P., Sun Y., et al. MiR-451 inhibits cell growth and invasion by targeting MIF and is associated with survival in nasopharyngeal carcinoma. Mol. Cancer. 2013;12:123. doi: 10.1186/1476-4598-12-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yang C.C., Hung P.S., Wang P.W., Liu C.J., Chu T.H., Cheng H.W., Lin S.C. miR-181 as a putative biomarker for lymph-node metastasis of oral squamous cell carcinoma. J. Oral Pathol. Med. 2011;40:397–404. doi: 10.1111/j.1600-0714.2010.01003.x. [DOI] [PubMed] [Google Scholar]
- 78.Wu T.-Y., Zhang T.-H., Qu L.-M., Feng J.-P., Tian L.-L., Zhang B.-H., Li D.-D., Sun Y.-N., Liu M. MiR-19a is correlated with prognosis and apoptosis of laryngeal squamous cell carcinoma by regulating TIMP-2 expression. Int. J. Clin. Exp. Pathol. 2013;7:56–63. [PMC free article] [PubMed] [Google Scholar]
- 79.Peng S.C., Liao C.T., Peng C.H., Cheng A.J., Chen S.J., Huang C.G., Hsieh W.P., Yen T.C. MicroRNAs MiR-218, MiR-125b, and Let-7g predict prognosis in patients with oral cavity squamous cell carcinoma. PLoS ONE. 2014;9:e102403. doi: 10.1371/journal.pone.0102403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Gonzalez-Arriagada W.A., Olivero P., Rodriguez B., Lozano-Burgos C., de Oliveira C.E., Coletta R.D. Clinicopathological significance of miR-26, miR-107, miR-125b, and miR-203 in head and neck carcinomas. Oral Dis. 2018;24:930–939. doi: 10.1111/odi.12872. [DOI] [PubMed] [Google Scholar]
- 81.El Baroudi M., Machiels J.P., Schmitz S. Expression of SESN1, UHRF1BP1, and miR-377-3p as prognostic markers in mutated TP53 squamous cell carcinoma of the head and neck. Cancer Biol. 2017;18:775–782. doi: 10.1080/15384047.2017.1373212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Berania I., Cardin G.B., Clement I., Guertin L., Ayad T., Bissada E., Nguyen-Tan P.F., Filion E., Guilmette J., Gologan O., et al. Four PTEN-targeting co-expressed miRNAs and ACTN4-targeting miR-548b are independent prognostic biomarkers in human squamous cell carcinoma of the oral tongue. Int. J. Cancer. 2017;141:2318–2328. doi: 10.1002/ijc.30915. [DOI] [PubMed] [Google Scholar]
- 83.He F.Y., Liu H.J., Guo Q., Sheng J.L. Reduced miR-300 expression predicts poor prognosis in patients with laryngeal squamous cell carcinoma. Eur. Rev. Med. Pharmacol. Sci. 2017;21:760–764. [PubMed] [Google Scholar]
- 84.Hess A.K., Muer A., Mairinger F.D., Weichert W., Stenzinger A., Hummel M., Budach V., Tinhofer I. MiR-200b and miR-155 as predictive biomarkers for the efficacy of chemoradiation in locally advanced head and neck squamous cell carcinoma. Eur. J. Cancer. 2017;77:3–12. doi: 10.1016/j.ejca.2017.02.018. [DOI] [PubMed] [Google Scholar]
- 85.Jiang C., Wang H., Zhou L., Jiang T., Xu Y., Xia L. MicroRNA-212 inhibits the metastasis of nasopharyngeal carcinoma by targeting SOX4. Oncol. Rep. 2017;38:82–88. doi: 10.3892/or.2017.5641. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 86.Liu N., Zhou Q., Qi Y.H., Wang H., Yang L., Fan Q.Y. Effects of long non-coding RNA H19 and microRNA let7a expression on thyroid cancer prognosis. Exp. Mol. Pathol. 2017;103:71–77. doi: 10.1016/j.yexmp.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 87.Re M., Magliulo G., Gioacchini F.M., Bajraktari A., Bertini A., Ceka A., Rubini C., Ferrante L., Procopio A.D., Olivieri F. Expression Levels and Clinical Significance of miR-21-5p, miR-let-7a, and miR-34c-5p in Laryngeal Squamous Cell Carcinoma. Biomed Res. Int. 2017;2017:3921258. doi: 10.1155/2017/3921258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Romeo P., Colombo C., Granata R., Calareso G., Gualeni A.V., Dugo M., De Cecco L., Rizzetti M.G., Zanframundo A., Aiello A., et al. Circulating miR-375 as a novel prognostic marker for metastatic medullary thyroid cancer patients. Endocr. Relat. Cancer. 2018;25:217–231. doi: 10.1530/ERC-17-0389. [DOI] [PubMed] [Google Scholar]
- 89.Wilkins O.M., Titus A.J., Salas L.A., Gui J., Eliot M., Butler R.A., Sturgis E.M., Li G., Kelsey K.T., Christensen B.C. MicroRNA-Related Genetic Variants Associated with Survival of Head and Neck Squamous Cell Carcinoma. Cancer Epidemiol. Biomark. Prev. 2019;28:127–136. doi: 10.1158/1055-9965.EPI-18-0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Yu E.H., Tu H.F., Wu C.H., Yang C.C., Chang K.W. MicroRNA-21 promotes perineural invasion and impacts survival in patients with oral carcinoma. J. Chin. Med. Assoc. JCMA. 2017;80:383–388. doi: 10.1016/j.jcma.2017.01.003. [DOI] [PubMed] [Google Scholar]
- 91.Madurantakam R.M., Kumarasamy C., Baxi S., Gupta A., Ramesh N., Kodiveri M.G., Jayaraj R. Current Evidence on miRNAs as Potential Theranostic Markers for Detecting Chemoresistance in Colorectal Cancer: A Systematic Review and Meta-Analysis of Preclinical and Clinical Studies. Mol. Diagn. Ther. 2019;23:65–82. doi: 10.1007/s40291-019-00381-6. [DOI] [PubMed] [Google Scholar]
- 92.Madhav M.R., Nayagam S.G., Biyani K., Pandey V., Kamal D.G., Sabarimurugan S., Ramesh N., Gothandam K.M., Jayaraj R. Epidemiologic analysis of breast cancer incidence, prevalence, and mortality in India: Protocol for a systematic review and meta-analyses. Medicine. 2018;97:e13680. doi: 10.1097/MD.0000000000013680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Poddar A., Aranha R.R., Muthukaliannan G.K., Nachimuthu R., Jayaraj R. Head and neck cancer risk factors in India: Protocol for systematic review and meta-analysis. BMJ Open. 2018;8:e020014. doi: 10.1136/bmjopen-2017-020014. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.