Abstract
A 16-year-old female patient showed up at the orthopaedics unit complaining of intolerable pain on her left hip. While being questioned and her clinical history written down, she shared that as part of her daily exercise routine, she ran 10 miles (16 km) daily at a speed of 9.5–10.5 mph (15–17 km/hour). MRI was consequently ordered, confirming the presence of a stress fracture. Therefore, immediate suspension of physical activity was indicated, followed by the prescription of crutches as well as restricted weight bearing. Gradually, she recovered complete functionality and approximately a month after she had entirely healed. While on a skiing trip, again she abruptly developed an acute pain on her right hip. Another MRI was ordered; its result confirmed a new stress fracture. Her previous treatment has proved so successful, a conservative approach was once again prescribed for her, showing optimum results 6 months later.
Keywords: orthopaedics, sports and exercise medicine
Background
A stress fracture may be most accurately defined as a complication derived from abnormal bone homeostasis due to the repetitive mechanical impact, which in turn leads to an increased osteoclastic-mediated bone resorption.1–8
Mostly uncommon, stress fractures amount to 10% of all sports-related injuries, femoral neck stress fractures being 3%–5% of the whole.2–7 It is mainly observed among military recruits and young female athletes due to constant exposure of the bone to repetitive loading in a specific area, which in turn predisposes for microfracture accumulation.1–4 9 Stress fractures most frequently appear in: the tibia (33%), tarsal bones (20%), metatarsals (20%), femur (11%), fibula (7%) and pelvis (7%).3 4
The main risk factors that are worth mentioning are as follows:
Female gender (especially those presenting the athlete triad that consists in the coexistence of amenorrhea, eating disorders and premature osteoporosis).1–4 6
Being a high-performance athlete.1–6 9
Prior stress fracture history.
Fracture predisposing comorbidity (such as hormonal, autoimmune, neoplastic and nutritional disorders).4 6
During the early stages, femoral neck stress fractures can present themselves only when the subject is actively exercising and it is characterised by the onset of deep pain in the hip or anterior groin regions, an inability to carry weight, presenting antalgic gait and a limited motion range.1–7
When unrecognised, untreated or mistreated, it may lead to the onset of acute pain in resting periods, which in turn denotes the possible presence of a displaced femoral fracture, a severe surgical emergency because of the high risk of avascular necrosis of the femoral head and late osteoarthritis of the hip joint, solved only by a total hip arthroplasty, it may also lead to delayed union or even non-union of fractures.1–9
Case presentation
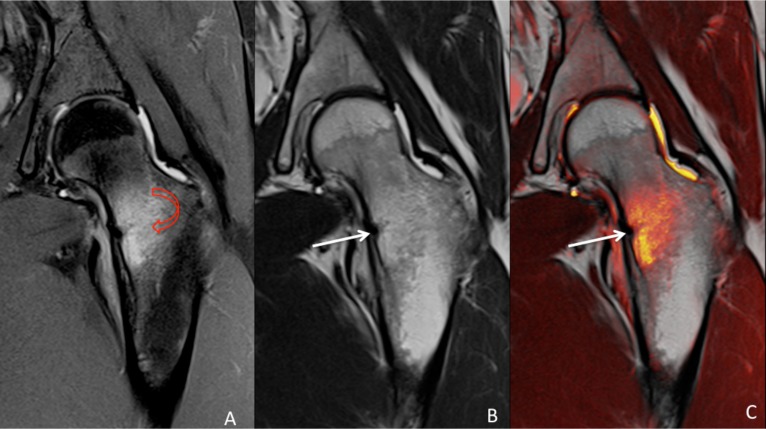
Previously healthy 16-year-old woman has a history of excessive physical activity for a year. She ran 10 miles (16 km) daily at a speed of approximately 9.5–10.5 mph. She began with spontaneous, intolerable left hip pain so an X-ray was obtained, showing no relevant information in order to establish a prompt diagnosis, which is why an MRI was indicated; its result confirmed a stress fracture diagnosis (figure 1). Besides being female and a high-performance athlete, patient presented no other risk factors, such as presence of hormonal, autoimmune, neoplastic, nutritional and eating disorders, as well as prior stress fracture history. Conservative treatment was opted; immediate exercise interruption was prescribed for a period of 9 months as well as the use of crutches and restricted weight bearing. She was gradually able to better support her weight on her limb.
Figure 1.
MRI of the left hip. Coronal view showing minimal cortical hypointensity in the medial aspect of the femoral neck, indicating compression side fracture (white arrow), with extensive surrounding oedema (red arrow). (A) proton density–weighted image, (B) T1-weighted image and (C) fusion image.
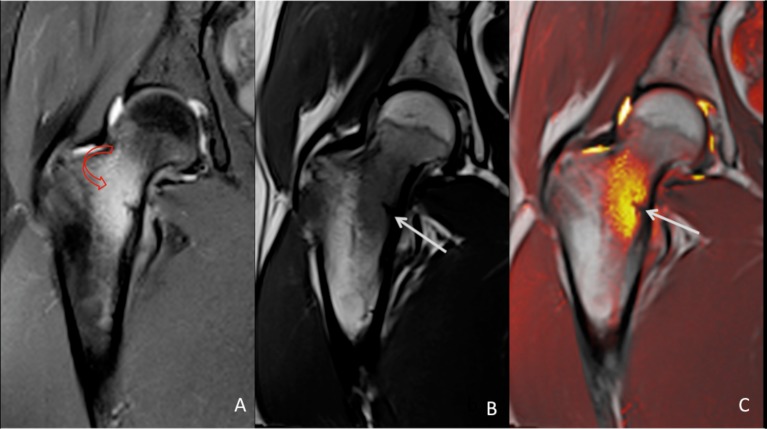
After finishing that period of time, the left hip had already healed and the patient was discharged. A month after she returned to her normal exercise routine and, while on a skiing trip, she developed spontaneous right hip pain that was evaluated at the orthopaedics unit where an MRI was asked for, confirming the presence of another stress fracture (figure 2). Because of the previous successful result, conservative treatment was again indicated.
Figure 2.
MRI of the right hip. Coronal view showing localised cortical hypointensity in the medial aspect of the femoral neck, indicating compression side fracture (white arrow), with extensive surrounding oedema (red arrow). (A) Proton density–weighted image, (B) T1-weighted image and (C) fusion image.
Outcome and follow-up
The patient showed a favourable outcome, she was able to return to her normal activities after 6 months of conservative treatment; she ended up with no sequelae.
Total follow-up of this patient lasted 24 months, an MRI was asked for after this period of time, which showed overt clinical improvement as well as manifest bone consolidation with preserved integrity. No visible bone oedema or fracture trace was found (figure 3). After this she was discharged from the orthopaedics unit.
Figure 3.
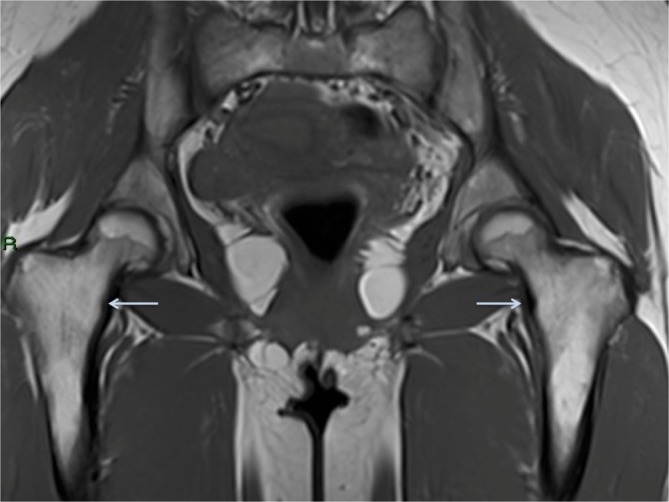
Pelvic MRI showing overt clinical improvement as well as manifest bone consolidation with preserved integrity. No visible bone edema or fracture line was found.
Discussion
Stress fractures of the femoral neck were first described by Blecher in 1905, followed by Asal in 1936 in the oldest scientific surgical journal, the Langenbeck’s Archiv für Chirugie.5 8
Two main types of stress fractures can be mentioned:
Fatigue fractures: those that occur when exposure to abnormal stress wears out the bone, frequently due to a sudden increase in intensity, duration or frequency in physical activity therefore becoming the most common type of stress fracture among young athletic individuals.2–5 8
Insufficiency fractures: those that occur when normal stress loading cannot be sustained by a deteriorated bone, mostly seen in geriatric patients.2–5 8
Any abrupt change in a patient’s routine is caused enough to suspect a possible development of a stress fracture.2 4 5 10 Once this is established, the immediate course of action is to take a simple X-ray, being the first-line diagnostic test, with a sensitivity ranging from 15% to 35%, and only showing radiological changes among those cases where 40% of the bone integrity has been compromised.1–9
MRI imaging should be reserved only for specific cases.4 7 9 It should be performed only with persisting symptoms and negative radiographs (radiographic changes can be present in only 20% of cases). Typical radiographic changes suggesting femoral neck stress fracture are: linear sclerosis (often perpendicular to primary trabeculae), periosteal or endosteal callous formation and a radiolucent fracture line through one cortex.4 7 9
MRI represents the gold-standard second-line diagnostic test (sensitivity 100%, specificity 85%).3 4 7 9 Lab tests such as a complete blood count, acute phase reactants and a hormone profile in female patients (particularly in those with prior history of amenorrhea) are also recommended.7
Treatment is generally conservative.1 4 5 7 9 It may include physiotherapy, ice applied locally, restricted weight bearing with the aid of crutches for up to 4–6 weeks and immediate restrain of any physical activity.7 9 Surgical intervention is needed in those cases where a tension-side fracture is present or, for compression-side fractures, either if the fracture line progresses on follow-up radiographs or if it is over 50% of the femoral neck width.
Urgent reduction and fracture fixation using percutaneous screw fixation or a dynamic hip screw should prevent further fracture displacement and damage to the femoral head blood supply.3–5 7–10
Periodic follow-up with X-rays must be made in order to ensure fracture resolution, and the return to sporting activities relies on the certainty of clinical and radiological welfare.3 7 9
Patient’s perspective.
I am 16 years old, and jog daily at a speed of approximately 10 mph (16 km/hour). One day, while I was running, I had a sudden, extremely strong pain on my left side. I was taken to the Orthopaedics Unit at the nearest hospital, where the doctor ordered an MRI. The study showed a stress fracture in my left hip. I had to interrupt my daily exercise, and had to use crutches for a period of time. I had a full recovery, and 1 month after I had finished treatment, left on a skiing trip. There, one day I felt an acute pain, but this time, on my right side. A second MRI was taken, and the result confirmed a new stress fracture on my right hip. Once again I had to suspend all physical activities and walk with the aid of crutches, and 6 months later I was fine.
Learning points.
Mostly seen among military recruits and young female athletes, stress fractures occur when the microfracture accumulation in the bone exceeds its normal homeostasis capacity
Look for a femoral neck stress fracture in any given case of an abrupt change in the physical routine and most specifically when it is accompanied by severe hip or groin pain
As soon as a stress fracture is confirmed, physical activity must be immediately restrained and weight bearing ought to be restricted
Calcium and vitamin D levels may be worth evaluated in this type of patients
Footnotes
Contributors: SJ-R worked up and diagnosed the patient. AlJ-B, ArJ-B and SJ-R wrote the script. YF-D-L-B performed imaging. SJ-R is overall guarantor of the paper. All people named as authors meet all four ICMJE Recommendations criteria. All authors approved the manuscript for publication.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Polacek M, Småbrekke A. Displaced stress fracture of the femoral neck in young active adults. BMJ Case Rep 2010;2010:bcr0220102749 10.1136/bcr.02.2010.2749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fonte H, Rodrigues-Pinto R. Femoral neck stress fracture in a young female recruit: case report. Sicot J 2018;4:16 10.1051/sicotj/2018011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kovacevic D, Mariscalco M, Goodwin RC. Injuries about the hip in the adolescent athlete. Sports Med Arthrosc Rev 2011;19:64–74. 10.1097/JSA.0b013e31820d5534 [DOI] [PubMed] [Google Scholar]
- 4. Matcuk GR, Mahanty SR, Skalski MR, et al. Stress fractures: pathophysiology, clinical presentation, imaging features, and treatment options. Emerg Radiol 2016;23:365–75. 10.1007/s10140-016-1390-5 [DOI] [PubMed] [Google Scholar]
- 5. Moo IH, Lee YH, Lim KK, et al. Bilateral femoral neck stress fractures in military recruits with unilateral hip pain. J R Army Med Corps 2016;162:387–90. 10.1136/jramc-2014-000401 [DOI] [PubMed] [Google Scholar]
- 6. Frank JS, Gambacorta PL, Eisner EA. Hip pathology in the adolescent athlete. J Am Acad Orthop Surg 2013;21:665–74. 10.5435/JAAOS-21-11-665 [DOI] [PubMed] [Google Scholar]
- 7. Robertson GA, Wood AM. Femoral neck stress fractures in sport: a current concepts review. Sports Med Int Open 2017;1:E58–68. 10.1055/s-0043-103946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Livingston JI, Deprey SM, Hensley CP. Differential diagnostic process and clinical decision making in a young adult female with lateral hip pain: a case report. Int J Sports Phys Ther 2015;10:712–22. [PMC free article] [PubMed] [Google Scholar]
- 9. Neubauer T, Brand J, Lidder S, et al. Stress fractures of the femoral neck in runners: a review. Res Sports Med 2016;24:283–97. 10.1080/15438627.2016.1191489 [DOI] [PubMed] [Google Scholar]
- 10. Robertson GA, Wood AM. Lower limb stress fractures in sport: optimising their management and outcome. World J Orthop 2017;8:242–55. 10.5312/wjo.v8.i3.242 [DOI] [PMC free article] [PubMed] [Google Scholar]