Abstract
Background:
Clinical screening for basic social needs –such as food and housing insecurity – is becoming more common as health systems develop programs to address social determinants of health. Clinician attitudes toward such programs are largely unexplored.
Objective:
To describe the attitudes and experiences of social needs screening among a variety of clinicians and other health care professionals.
Research Design:
Multi-center electronic and paper-based survey.
Subjects:
Two hundred fifty-eight clinicians including primarily physicians, social workers, nurses, and pharmacists from a large integrated health system in Southern California.
Measures:
Level of agreement with prompts exploring attitudes toward and barriers to screening and addressing social needs in different clinical settings.
Results:
Overall, most health professionals supported social needs screening in clinical settings (84%). Only a minority (41%) of clinicians expressed confidence in their ability to address social needs, and less than a quarter (23%) routinely screen for social needs currently. Clinicians perceived lack of time to ask (60%) and resources (50%) to address social needs as their most significant barriers. We found differences by health profession in attitudes toward and barriers to screening for social needs, with physicians more likely to cite time constraints as a barrier.
Conclusions:
Clinicians largely support social needs programs, but they also recognize key barriers to their implementation. Health systems interested in implementing social needs programs should consider the clinician perspective around the time and resources required for such programs and address these perceived barriers.
INTRODUCTION:
Health care systems are increasingly interested in addressing patients’ “social needs”, 1,2,3,4,5 defined by basic resource needs such as safe housing, healthy food, or transportation. Social needs put patients at higher risk for poor health outcomes,6,7,8 and are a source of frustration and suffering for patients that complicate care delivery.9,10 Thus, social needs may serve as actionable indicators of adverse social determinants of health. Implementation of uniform social needs screening tools is increasing, especially as programs become better able to address social needs through referrals to social needs services.11,12,13,14 A growing list of health system leaders see social needs screening and resource referral as a standard of care to improve population health.15,16,17 However, it is unclear based on the little published evidence18,19,20 whether clinicians on the front lines of health care systems are supportive of such programs.
As health care systems implement tackling social needs, clinicians will likely be responsible for documenting and addressing them, among other roles not traditionally their responsibility. It is not known whether providers see themselves as the appropriate workforce for implementing social needs screening and interventions, or what utility they see in expanding the scope of medical care to include social factors. While evidence is emerging via small studies in one or two physician specialties,21,22 less is known about how provider attitudes toward addressing social determinants of health differ across care settings and professions.
We surveyed health professionals -- including physicians in various specialties, nurses, case managers, social workers, and pharmacists -- working across various care settings and clinical sites to better understand clinicians’ current practices regarding social needs screening, barriers to such screening, and attitudes toward adoption of programs that address social needs as a standard part of clinical care.
METHODS:
Participants and Setting
We surveyed physicians, nurses, case managers, pharmacists, and social workers from the fourteen medical centers within Kaiser Permanente Southern California (KPSC), a large integrated health system. All medical centers included share a common electronic health record. These clinicians care for a patient population that is racially/ethnically diverse, representative of the population of Southern California, and approximately 10% of whom have Medicaid insurance or are uninsured. The sample included clinicians with patient care responsibilities. Physicians surveyed represented the fields of internal medicine, pediatrics, family medicine, emergency medicine, and psychiatry and practiced in either the inpatient or outpatient setting.
Survey Administration
Clinicians were either approached in person during staff meetings to consent to complete a paper version of the survey or they were invited to participate via a standardized email invitation to an electronic version of the consent form and survey. Study investigators explained the goals of the survey and, if clinicians agreed, they consented to and completed the survey. No financial or other incentives were provided. Given that the survey collected no identifiable information and we relied on the surveys for demographic information on participants, no information on non-responders was obtainable for the study to compare them to responders. The Kaiser Permanente Southern California Institutional Review Board reviewed and approved the study as exempt due to minimal risk.
Measure Development
Surveys were designed to gather descriptive information and were developed by an iterative consensus process with input from clinicians, researchers, and experts in social needs screening. Survey items were revised with input from 47 clinicians (majority physicians) who took part in hour-long in-depth focus groups in which facilitators asked questions similar to those in the provider survey.23 A full copy of the survey is included in the online appendix.
Measures
Clinician characteristics including health profession, race/ethnicity, practice setting, and number of years in current practice were collected. Survey items asked clinicians the degree to which they agreed or disagreed with statements about their current practices screening for social needs, awareness of resources to address social needs, confidence in their own ability to help patients address their social needs, barriers experienced to screening for social needs, and attitudes toward the potential usefulness of social needs information and whether social needs were beyond appropriate scope of care or ought to be integrated as standard of care (measured as categorical variables with 5 possible values on a Likert Scale).
Statistical Analysis
We used Chi-square tests or Fisher’s exact tests, students t-tests, and tests of proportions to examine differences in clinician responses by participant characteristics including health profession, care setting, years in practice, demographics, and clinician perceptions of social need prevalence among their patients. All analyses were carried out using STATA 13 (StataCorp, College Station, TX).
RESULTS:
Of the clinicians invited to participate in the study, 258 (27%; 154 of 700 physicians invited and 104 of 263 non-physicians invited) agreed to participate and completed most or all of the survey. Among the participants, most did not identify as white, had been in practice for 10 years or more, and practiced in outpatient care settings (Table 1). Eighty-two percent (210) agreed or strongly agreed that social needs were an issue for most of their patients.
Table 1:
Participant Characteristics (N=258)
| Characteristic Data shown as percentage (Number) |
Overall Sample | Physician Sub- Sample |
Non-Physician Sub-Sample |
|---|---|---|---|
| Health Profession | |||
| Physician | 59.7% (154) | 100% (154) | - |
| Registered Nurse, Nurse Practitioner, or Nurse Case Manager | 12.8% (33) | - | 31.7% (33) |
| Pharmacist | 15.9% (41) | - | 39.4% (41) |
| Social Worker | 4.7% (12) | - | 11.5% (12) |
| Administrator or Other | 3.1% (8) | - | 7.7% (8) |
| Clinician Care Setting | |||
| Outpatient Only | 49.4% (124) | 48.1% (74) | 51.5% (50) |
| Number of Years in Current Practice | |||
| 10 years or fewer | 46.7 (122) | 44.4% (68) | 50.0% (51) |
| 11 to 20 years | 42.7% (109) | 44.4% (68) | 40.2% (41) |
| 21 or more years | 10.6% (27) | 11.1% (17) | 9.8% (10) |
| Race and Ethnicity | |||
| White | 29.2% (64) | 30.6% (41) | 27.1% (23) |
| Asian or Pacific Islander | 52.1% (114) | 51.5% (69) | 52.9% (45) |
| Other (African American, Latino, Multiple, Other) | 18.7% (41) | 17.1% (23) | 20% (17) |
Regarding attitudes toward social needs programs, 84% (215) of respondents, agreed or strongly agreed that screening for social needs should be a standard part of clinical care (Figure 1). Seventy-three percent (186) considered such screening within the scope of health care services. Large majorities of respondents either agreed or strongly agreed that information about social needs could be used to improve trust (93%, 239), communication with patients (96%, 247), and care overall (95%, 244).
Figure 1: Attitudes among clinician participants regarding screening for and addressing social needs.

Shaded bars display the proportion of the sample indicating degree of agreement with each questionnaire prompt on a scale from Strongly Disagree (1) to Strongly Agree (5).
Only about a fifth (23%, 59) of clinician respondents indicated that they always ask patients about their social needs, and similar proportions reported that they always review information on social needs available in the patient chart (22%, 55) or use information about patients’ social needs in medical management (35%, 87). Likewise, only 41% (106) of respondents agreed or strongly agreed that they were confident in their ability to help patients address their social needs, and 21% (53) expressed concern that patients will feel uncomfortable answering questions about their social needs.
Barriers to social needs screening most commonly identified were lack of time to ask and lack of resources to address any social needs identified, with 60% (152) and 50% (128). Lack of training and lack of comfort in asking patients about social needs were the least prevalent barriers (Figure 2).
Figure 2: Barriers experienced by clinician participants to screening for social needs in practice.
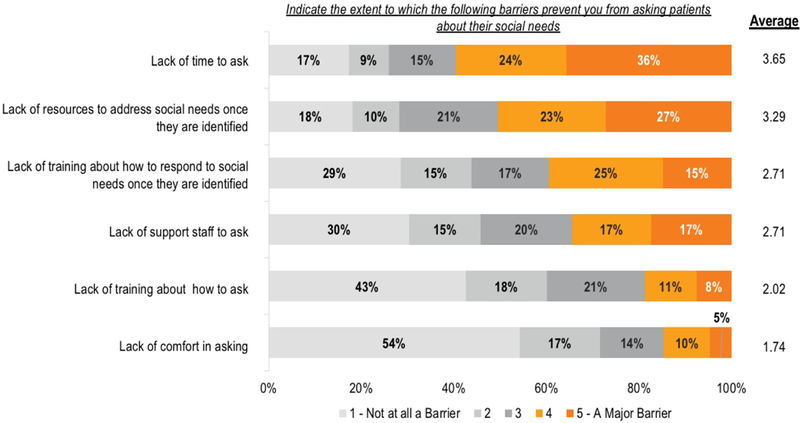
Legend: Shaded bars display the proportion of the sample indicating responses to each questionnaire prompt on a scale from Not at all a barrier (1) to A major barrier (5).
Asked which health professions would be best suited to screen for and address social needs, responding clinicians most commonly chose social workers (94% said they should screen, 92% said they should address social needs), case managers (84% screen, 86% address), primary care providers (50% screen, 70% address), and registered nurses (44% screen, 55% address). Sixty-three percent of respondents (163) reported that their own health profession was best suited to screen for social needs. Seventy-three percent (188) of respondents indicated that medically complex, high utilizing patients were appropriate social needs screening populations. Roughly half (55%, 142) indicated that patients with one or more chronic medical condition should be screened. Forty-five percent (115) said that all patients should be screened for social needs.
Non-physician respondents were more likely than physicians to think that social needs were an issue for most of their patients (90.3% versus 76.4%, p = 0.02). Non-physician respondents were more likely to report that they were aware of resources to address social needs (64% versus 45%, p = 0.03) and were more likely to agree that they were confident in their ability to help patients address social needs (51% versus 34%, p = 0.03). Non-physician respondents were also more likely to endorse concerns that patients will feel uncomfortable answering questions about social needs (29% versus 15%, p < 0.01). The only noted barrier to screening for social needs that differed between physician and non-physicians was a lack of time to ask, which was endorsed as a substantial barrier by 70% of physicians versus 47% of non-physicians (p <0.001). Non-physician and physician respondents had similar rates of disagreement with a statement that collecting social needs information was beyond the scope of health care (Table 2).
Table 2.
Differences in Clinician Attitudes by Health Profession and Practice Setting
| Percentage in Agreement by Health Profession | Percentage in Agreement by Practice Setting | ||||||
|---|---|---|---|---|---|---|---|
| Statement | Physician (N=154) Percentage in Agreement |
All Non-Physician (N=104) Percentage in Agreement |
P-value | Only Outpatient Practice (N=111) |
Only Inpatient Practice (N=47) |
Neither Exclusively Outpatient nor Inpatient |
P-value |
| Social needs are an issue for most of my patients | 76.4% | 90.3% | 0.004 | 78.2% | 78.7% | 87.9% | 0.15 |
| I am confident in my ability to help patients address social needs | 34.4% | 51.4% | 0.007 | 31.5% | 29.8% | 57.6% | <0.001 |
| I am aware of resources available to address my patients’ social needs | 44.8% | 64.1 | 0.002 | 45.1% | 49.0% | 62.6% | 0.03 |
| I am concerned that patients will feel uncomfortable answering questions about their social needs | 15.6 | 28.5 | 0.01 | 19.1% | 12.8% | 26.3% | 0.15 |
| Collecting social needs information is beyond the scope of clinical care | 6.5 | 12.9 | 0.08 | 9.2% | 2% | 12.2% | 0.11 |
| Screening for social needs among patients should be a standard part of care | 81.2 | 88.2 | 0.13 | 87.4% | 80.9% | 81.6% | 0.43 |
Clinician respondents practicing exclusively in the outpatient setting more often agreed that lack of time to ask about social needs (79.3% versus 47.9% providing inpatient care, p<0.001), lack of training in how to respond to social needs and lack of resources to address social needs identified (59.5% versus 42.5%, p<0.01) were major barriers compared to clinicians in other settings. These outpatient clinicians were also less likely to agree that they were confident in their ability to help patients address their social needs (31.5% versus 48.6%, p<0.01).
DISCUSSION:
In this multi-site survey of clinician attitudes toward screening and addressing social needs, a majority of respondents support such programs as a standard part of clinical care and a majority reported that social needs were an issue for their patients. However, most clinicians in our study did not consistently screen for social needs despite nearly two thirds indicating their particular health profession was best suited to screen for social needs. The most cited barriers to screening included lack of time and resources, and a sizable proportion identified factors such as lack of training and staff support as significant barriers.
We found differences by health profession in attitudes, with physicians less likely to think that social needs were an issue for their patients and less confident in their ability to address their social needs. Clinicians who worked exclusively in the outpatient setting more often indicated time and resource constraints were barriers than respondents in other settings.
Our findings have implications for health systems considering implementing or standardizing programs to identify and address social needs. The results demonstrate that most clinicians support addressing social needs in principle and see potential benefits to their patients. However, they also recognize barriers that would need to be addressed to make implementation of such programs practicable. These barriers also have implications for the patient populations that can practicably be screened (i.e. all patients versus just those with complex needs, tailoring based on neighborhood or sociodemographic risk factors, etc.). There are also mixed perceptions about which health professions and care settings are best suited for screening, making social needs everyone’s problems to solve without clarity on how to do so efficiently as a coordinated health care team. In addition to seeking clinician buy-in, these findings suggest that health systems interested in implementing social needs programs should take steps to account for the time, resources, professional scope, and other structural factors that currently prevent clinicians from addressing social needs.
The study’s limitations include its response rate, especially among physicians relative to non-physicians. Though the proportion of respondents was consistent with previously reported online surveys of clinicians,24,25 it still raises the possibility of nonresponse bias. Reassuringly, our sample had a similar average length of employment to the overall KPSC workforce and similar race/ethnicity breakdown and rates of exclusively outpatient practice to previously published studies involving KPSC provider samples. The results may not generalize to other health systems or settings with different financial incentives, care processes, or institutional cultures. Likewise, at the time of the study, none of the sites involved had standardized social needs screening and referral programs in place. Though measurement items were vetted by content experts, our survey tool had not been previously validated because no published surveys to date had reported evidence on attitudes and common barriers to social needs screening and intervention programs. Future studies should examine differences in attitudes and barriers toward social needs across different health systems to examine structural predictors of clinician perceptions.
Conclusion
Clinicians across health professions and care settings reported that 1) social needs were prevalent among their patients, 2) they experienced logistical barriers to addressing those social needs including time and resource constraints, and 3) they support expansion of clinical programs to address social needs for patients. As social needs screening and referral programs become more common in health care, future studies should continue to examine attitudes and experiences regarding social needs in various health professions to determine whether they are changing with time and familiarity with such programs.
Supplementary Material
ACKNOWLEDGEMENTS:
Contributors: We thank Dr. Michael Kanter for assistance with distribution of the survey and Dr. Nirav Shah for comments on the manuscript.
Footnotes
Conflict of Interest: The authors have no conflicts of interest to disclose.
Contributor Information
Adam Schickedanz, University of California Los Angeles, Department of Pediatrics, 10960 Wilshire Blvd, Los Angeles, CA 90024.
Courtnee Hamity, Care Management Institute, Kaiser Permanente, 1 Kaiser Plaza, Oakland, CA 94612.
Artair Rogers, Health Leads, 24 School Street, Boston, MA 02108.
Adam L. Sharp, Kaiser Permanente Southern California, Research and Evaluation Department. Kaiser Permanente Los Angeles Medical Center, Department of Emergency Medicine, 100 South Los Robles Ave, Pasadena, CA 91101.
Ana Jackson, Care Management Institute, Kaiser Permanente, 1 Kaiser Plaza, Oakland, CA 94612.
References
- 1.LaForge K, Gold R, Cottrell E, Bunce AE, Proser M, Hollombe C, Dambrun K, Cohen DJ, Clark KD. How 6 Organizations Developed Tools and Processes for Social Determinants of Health Screening in Primary Care: An Overview. The Journal of ambulatory care management. 2018. January;41(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smith L, Sion P, Stevenson A, Kasen P, Harstad N. Primed: Addressing Social Factors in the Health Care Safety Net. California Healthcare Foundation; November 2017. [Google Scholar]
- 3.Billioux A, Conway PH, Alley DE. Addressing population health: Integrators in the Accountable Health Communities model. JAMA. 2017;318(19):1865–1866. PMID: . [DOI] [PubMed] [Google Scholar]
- 4.Byhoff E, Freund KM, Garg A. Accelerating the implementation of social determinants of health interventions in internal medicine. J Gen Intern Med. 2017; Epub ahead of print. PMID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gottlieb L, Ackerman S, Wing H, Adler N. Evaluation activities and influences at the intersection of medical and social services. J Health Care Poor Underserved. 2017;28(3):931–951. [DOI] [PubMed] [Google Scholar]
- 6.Szymkowiak D, Montgomery AE, Johnson EE, Manning T, O’Toole TP. Persistent super-utilization of acute care services among subgroups of veterans experiencing homelessness. Med Care. 2017;55(10):893–900. PMID: . [DOI] [PubMed] [Google Scholar]
- 7.Ash AS, Mick EO, Ellis RP, Kiefe CI, Allison JJ, Clark MA. Social determinants of health in managed care payment formulas. JAMA Intern Med. Epub ahead of print. PMID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morales ME, Epstein MH, Marable DE, Oo SA, Berkowitz SA. Food insecurity and cardiovascular health in pregnant women: Results from the Food for Families Program, Chelsea, Massachusetts, 2013–2015. Prev Chronic Dis. 2016;13:E152 PMID: DOI: 10.5888/pcd13.160212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Basu S, Berkowitz SA, Seligman H. The monthly cycle of hypoglycemia: An observational claims-based study of emergency room visits, hospital admissions, and costs in a commercially insured population. Med Care. 2017; EPUB ahead of print. PMID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lawson NR, Klein MD, Ollberding NJ, Wurster Ovalle V, Beck AF. The impact of infant well-child care compliance and social risks on emergency department utilization. Clin Pediatr (Phila). 2017; Epub ahead of print. PMID: DOI: 10.1177/0009922817706145. [DOI] [PubMed] [Google Scholar]
- 11.Lundeen EA, Siegel KR, Calhoun H, et al. Clinical-community partnerships to identify patients with food insecurity and address food needs. Prev Chronic Dis. 2017;14:E113 PMID: DOI: 10.5888/pcd14.170343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pinto AD, Bloch G. Framework for building primary care capacity to address the social determinants of health. Can Fam Physician. 2017;63(11):e476–e482. [PMC free article] [PubMed] [Google Scholar]
- 13.Cutts D, Cook J. Screening for food insecurity: short-term alleviation and long-term prevention. Am J Public Health. 2017;107(11):1699–1700. PMID: DOI: 10.2105/AJPH.2017.304082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gottlieb LM, Wing H, Adler NE. A systematic review of interventions on patients’ social and economic needs. Am J Prev Med. 2017; Epub ahead of print. PMID: DOI: 10.1016/j.amepre.2017.05.011. [DOI] [PubMed] [Google Scholar]
- 15.Thomas-Henkel C, Schulman M. Screening for Social Determinants of Health in Populations with Complex Needs: Implementation Considerations. Center for Health Care Strategies; October 2017. Available online. [Google Scholar]
- 16.Makelarski JA, Abramsohn E, Benjamin JH, Du S, Lindau ST. Diagnostic accuracy of two food insecurity screeners recommended for use in health care settings. Am J Public Health. 2017;107(11):1812–1817. PMID: DOI: 10.2105/AJPH.2017.304033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gottlieb LM, Garcia K, Wing H, Manchanda R. Clinical interventions addressing nonmedical health determinants in Medicaid managed care. Am J Manag Care. 2016;22(5):370–376. PMID: . [PubMed] [Google Scholar]
- 18.Palakshappa D, Vasan A, Khan S, Seifu L, Feudtner C, Fiks AG. Clinicians’ perceptions of screening for food insecurity in suburban pediatric practice. Pediatrics. 2017; Epub ahead of print. PMID: DOI: 10.1542/peds.2017-0319. [DOI] [PubMed] [Google Scholar]
- 19.Garner AS, Storfer-Isser A, Szilagyi M, et al. Promoting early brain and child development: Perceived barriers and the utilization of resources to address them. Academic Pediatrics (2016). 11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fleming MD, Shim JK, Yen IH, et al. Patient engagement at the margins: Health care providers’ assessments of engagement and the structural determinants of health in the safety-net. Soc Sci Med. 2017;183:11–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Minier Mark. Staff and parent support in implementation of universal screening for toxic stress during well child visits: The Addressing Social Key Questions for Health Study. Poster presentation. Pediatric Academic Societies Annual Meeting San Francisco, May, 2017. [Google Scholar]
- 22.Tong ST, Liaw WR, Kashiri PL, Pecsok J, Rozman J, Bazemore AW, & Krist AH Clinician experiences with screening for social needs in primary care. The Journal of the American Board of Family Medicine. 2018. 31(3), 351–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hamity C, Jackson A, Peralta L, Bellows J. Perceptions and experience of patients, staff, and clinicians with social needs assessment. Perm J. 2018;22:18–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cunningham CT, Quan H, Hemmelgarn B, Noseworthy T, Beck CA, Dixon E, ... & Jetté N Exploring physician specialist response rates to web-based surveys. BMC medical research methodology. 2015: 15(1), 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cook DA, Wittich CM, Daniels WL, West CP, Harris AM, & Beebe TJ Incentive and reminder strategies to improve response rate for internet-based physician surveys: a randomized experiment. Journal of medical Internet research. 2016. 18(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


