Abstract
In this study we test the efficacy of Moment-by-Moment in Women’s Recovery (MMWR), a mindfulness-based intervention adapted to support women with substance use disorder (SUD) while in residential treatment. We use a parallel-group randomized controlled trial with a time-matched psychoeducation control to test MMWR effects on residential treatment retention. We used clinical staff-determined residential site discharge status and discharge date from the SUD treatment site record to determine retention. We tested for study group differences in retention defined as time to treatment non-completion without improvement (i.e., patient left treatment before completion of the treatment plan and made little or no progress toward achieving treatment goals based on clinical team determination), as well as differences in self-report of study intervention mechanisms of action (i.e., mindfulness, perceived stress, distress tolerance, emotion regulation, distress, affect, and drug and alcohol craving). The analytic timeframe for the survival analysis was from study intervention start date to 150 days later. The sample (N=200) was female, majority amphetamine/methamphetamine users (76%), Hispanic (58%), with a history of incarceration (62%). By the 150-day analytic endpoint, the sample had 74 (37%) treatment Completers, 42 (21%) still In-residence, 26 (13%) Non-completers with satisfactory progress, and 58 (29%) Non-completers without satisfactory progress. Survival analysis of the intent-to-treat sample showed the risk of non-completion without improvement was lower in MMWR as compared to the control group (adjusted hazard ratio=0.42, 95% CI: 0.16–1.08, p=.07). Both groups improved on select self-reported mechanism measure scores at immediate post-intervention, but only in the MMWR group did class attendance (dosage) have a large-size correlation with improved mindfulness (r=.61, p<.01), distress tolerance (r=.55, p<.01) and positive affect (r=.52, p<.01) scores. The hazard ratio for retention was of medium-to-large effect size, suggesting the clinical relevance of adding MMWR to an all-women’s, ethnoracially diverse, SUD residential treatment center. An extended curriculum may be helpful considering the protective benefits of class attendance on psychological health indicators.
Keywords: mindfulness, substance use disorder, residential, retention, dropout, women
Retention in substance use disorder (SUD) treatment is critical to improving long-term recovery outcomes, yet retention is a prevailing challenge in SUD treatment.1,2 As compared to SUD treatment completers, non-completers report more substance use relapses and SUD treatment readmissions.1 Further, non-completion is a significant predictor of negative outcomes including drug use and criminal activity.3,4 Intensive residential treatment, in contrast to outpatient treatment and individualized drug counseling, is a particularly important target for intervention development and testing because it largely serves vulnerable individuals who exhibit heightened levels of SUD severity and health related consequences.3,5
Women with SUD, in particular, represent a group that is vulnerable to non-completion as a result of complex social histories. For example, as compared to men receiving SUD treatment, women report significantly higher rates of trauma in the form of physical (70% vs. 32%) and sexual abuse (54% vs. 15%).6 Although gender alone is not consistently associated with treatment retention, women often enter SUD treatment with more complex medical comorbidities than men.7,8 Additionally, compared to women in mixed-gender programs, those in women-only residential programs are more likely to be homeless, on probation, and have longer histories of drug use.9,10 Based on national data, Black and Hispanic populations, in contrast to non-Hispanic White populations, are also less likely to complete SUD treatment, a disparity partly due to socioeconomic status inequities.11 These findings draw attention to the need for testing intervention approaches that could improve SUD treatment completion among women from diverse ethnoracial and socioeconomic backgrounds.
Mindfulness-Based Interventions (MBIs) defined here as the family of interventions that include mindfulness as their central therapeutic practice (e.g., Mindfulness-Based Stress Reduction, MBSR, and Mindfulness-Based Cognitive Therapy, MBCT),12 offer one approach to support women receiving SUD treatment. Mindfulness is a teachable state of being that, by definition, involves attending to one’s experiences on a moment-to-moment basis with openness and the intention to cultivate non-judgmental, non-reactive states of awareness.12 Conventional cognitive and behavioral therapies use shared dialogue focused on reducing or eliminating substance-using patterns (e.g., thought stopping or replacement, avoidance of challenging experiences) and replacing them with healthier alternative behaviors. Conversely, MBIs use meditation to cultivate an open, accepting, and non-reactive awareness of conscious experience that influences cognitive and emotional states and patterns. Programs such as Mindfulness-Based Relapse Prevention (MBRP)13 and Mindfulness Oriented Recovery Enhancement (MORE)14 are modeled after the first generation of mindfulness-based therapies like MBSR in terms of their structure and format, and are examples of how MBIs can be supportive of conventional approaches to SUD treatment.
The utility of MBIs as an add-on to SUD residential treatment is based on the theoretical rationale that cultivating mindfulness supports recovery by weakening the substance use cycle that leads to relapse, which is often spurred by cognitive and emotional states and patterns. MBIs emphasize intentional awareness and acceptance of experiences even when they are uncomfortable or unwanted, thus changing the relationship with stimuli and introducing personal control over cognitive and social triggers, craving sensations, and negative affect. This is an important distinction because suppression can lead to an increase in the activation of substance use craving.15 By encouraging a decentered relationship to distressing experiences and urges while cultivating relaxation, mindfulness is thought to interrupt a user’s cycle of craving and therefore prevents the escalation of these experiences to a habitual substance use response. Witkiewitz et al. have discussed these mechanisms in greater detail.16 As a coping skill, the user learns to experience the discomfort of aversive experiences without avoiding or reacting to them or employing imposed replacement thoughts or behaviors, thus possibly improving their self-regulation over substance use behavior. These skills are especially relevant for clients in residential treatment who experience challenging emotions as they adjust to a structured environment, endure withdrawal symptoms, and manage substance cravings.17
The mechanisms of action targeted by MBIs noted above have been mostly argued from a theoretical basis, and laboratory studies testing the reliability of these mechanisms with substance users remain early in development. One laboratory study by Brewer et al.18 with a SUD sample showed participants who received a MBI in comparison to Cognitive Behavioral Therapy (CBT) reported significantly attenuated anxiety after a stress provocation task. This stress mechanism was validated with corresponding differences observed for heart rate variability such that the MBI group showed decreased sympathetic/vagal ratios compared to the CBT group (effect size=0.42). Moreover, treatment completers in both MBI and CBT groups showed significantly increased mindfulness levels (Five Facet Mindfulness Questionnaire, FFMQ scores) over time with the MT group showing a tendency toward greater overall increases in mindfulness levels at postcourse. In Garland et al.,19 a comparison of a MBI (Mindfulness-Oriented Recovery Enhancement, MORE) against CBT for men diagnosed with co-occurring psychiatric disorders and SUD was made, and a significant indirect effect of the MBI on decreasing craving by increasing mindfulness level (FFMQ score) was observed. Taken together, these initial findings from experimental studies identify stress-reduction and mindfulness skills to be detectable MBIs mechanisms of therapeutic action for people with SUD.
Reviews of experimental research trials report that MBIs adapted for people with SUD, such as Mindfulness-Based Relapse Prevention (MBRP), show promise for treatment efficacy.20 MBRP is a MBI adapted for patients in SUD aftercare to prevent relapse.13 MBRP combines mindfulness strategies with relapse prevention to help people with SUDs encounter cravings with less automatic reactivity.21 A small yet growing body of literature has found that MBRP can reduce alcohol and illicit drug use and craving, while also increasing acceptance and awareness of thoughts and feelings in some populations.22,23 To date, only one MBI trial (i.e., MBRP) we are aware of has focused on women with SUD from ethnoracial minority groups.24 Despite the promise of MBIs for individuals with SUDs, empirical knowledge gaps persist. These gaps produce limitations associated with small sample sizes, quasi-experimental study designs, lack of representation of women from low-income and diverse ethnoracial groups, and restriction to aftercare treatment settings. Only one study to date has evaluated the use of a MBI during residential SUD treatment and used a historical control group. In that study, Marcus et al.25 conducted a survival analysis of time to treatment dropout and found no significant difference between a MBI and treatment as usual; however, greater engagement in the MBI was associated with decreased likelihood of treatment dropout. The study did not include random assignment to treatment conditions and lacked an attention control group. Current limitations in the field inform the need to evaluate the efficacy of MBIs on residential SUD treatment retention.
Moment-by-Moment in Women’s Recovery (MMWR) is a MBI focused on SUD treatment retention and relapse prevention for vulnerable women from diverse ethnoracial backgrounds with complex social histories.26 The program was developed in 2009 by author H.A. in collaboration with a certified MBSR instructor Zayda Vallejo. MMWR is an adaptation of MBSR aimed at improving intervention acceptability and being suitable for women from low-income and racially and ethnically diverse groups in SUD treatment. As with other MBIs designed for people with SUD (e.g., MBRP), MMWR combines elements of stress reduction and relapse prevention27 skill development rooted in mindfulness and contemplative practice. It differs from other MBIs for people with SUD because it focuses on the specific needs of women in residential treatment (i.e., parenting roles, trauma exposure, interpersonal conflicts and frustrations with treatment staff and other clients, and situations that put them at risk for treatment dropout) as opposed to a mixed-gender program focused on SUD aftercare. The MMWR curriculum directly addresses specific aspects of residential treatment that may be stressful and lead to dropping out of treatment or relapsing. Residential treatment is especially challenging early on as clients adapt to residential site rules, the expectation of abstinence, the shared living situation, social conflicts, and the limited contact with significant others outside the facility.17 We expected that learning and using mindfulness skills and practices could be helpful in successfully managing these challenges, thereby enabling patients to stay in residential treatment and continue to expose themselves to the many services that support to recovery.
MMWR is intended to be integrated during residential treatment and addresses issues pertinent to SUD, relapse prevention, co-occurring mental health problems including trauma, and daily experiences of stress. Because of its intended population of women with low socioeconomic status and ethnoracial diversity, MMWR developers were sensitive to literacy level, using accessible language, and attentive to diverse cultural and socioeconomic backgrounds of women in SUD treatment. MMWR was developed to teach mindfulness skills that could assist clients in coping with factors (i.e., responses to internal and external stressors, emotion regulation, distress tolerance, craving) that can contribute both to treatment dropout and relapse. Using didactic, experiential self-observations, and exercises, the curriculum directly addresses specific aspects of residential treatment that may be stressful and lead to dropping out of treatment or relapsing (e.g., frustration with program rules and demands, conflictual relationships with other patients and/or staff, managing difficult emotions) and highlights how mindfulness practices can be used to respond rather than to react to challenging situations. Proposed target mechanisms of action for MMWR were related to skills developed during the classes and lessons related to precursors of relapse, and included mindfulness, perceived stress, distress tolerance, emotion regulation, distress, affect and drug and alcohol craving.
We previously tested the feasibility of MMWR using a within-subjects repeated-measures study that enrolled 318 low-income women attending SUD treatment from five sites (four residential and one outpatient) in Boston.28 Sample race and ethnicity was 45% Hispanic, 35% non-Hispanic Black, and 20% non-Hispanic White or other. Average length of stay in SUD treatment for the sample was 157 days. Participants reported high satisfaction with the MMWR program (rating of 3.4 out of 4, or excellent) as well as reduced perceived stress scores at 6- and 12-month follow assessments. Higher session dosage of the MMWR program significantly predicted reduced alcohol addiction severity and drug addiction severity at 12-month follow-up, after adjusting for baseline sociodemographic, criminal, and treatment exposure variables. This preliminary study did not randomly assign treatment exposures, lacked a control group, and did not examine discharge status.
The purpose of the current report is to test the efficacy of Moment-by-Moment in Women’s Recovery (MMWR) on residential SUD treatment retention. We use a parallel-group randomized controlled trial with a time-matched psychoeducation control to ascertain MMWR effects on residential treatment retention. The retention outcome was abstracted from the SUD treatment site record of clinical staff-determined discharge status and date of discharge. In our primary analysis, we tested for study group differences in time to non-completion event (i.e., patient left treatment before completion of the treatment plan and the clinical team determined that little or no progress was made toward achieving treatment goals). The analytic timeframe for the survival analysis was from study intervention start date to 150 days later, which was selected based on women’s average length of stay at the residential site. In our secondary analyses, we tested for group differences on self-reported measure scores of study intervention mechanisms of action (i.e., mindfulness, perceived stress, distress tolerance, emotion regulation, distress, affect, and drug and alcohol craving), which are not only targeted in MMWR but also associated with negative outcomes among people with SUD, including severity of dependence and early residential dropout.29–31
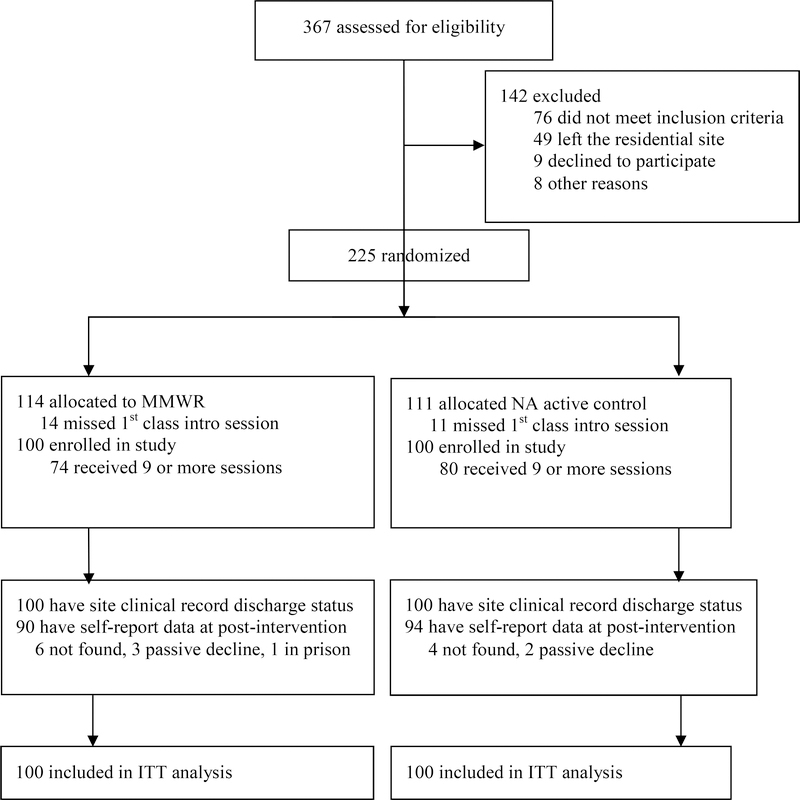
Methods
Study design
This parallel-group RCT () conducted from 2016 to 2018 was designed to compare retention days in residential treatment among participants randomly assigned to one of two study conditions as adjuncts to their residential SUD treatment: (1) MMWR and (2) Neurobiology of Addiction (NA), with the latter serving as the psychoeducational control condition (see Amaro and Black32 for detailed study protocol). Baseline interviews occurred prior to randomization and post-intervention interviews occurred up to 14 days after the last class session of the study intervention. All participants received SUD treatment services as normally provided by the treatment facility without affecting the level of usual care provided to patients. The study site offered no structured mindfulness-based activities or services during the study period. The University of Southern California Institutional Review Board approved this study (UP-14–00391).
Study Site Standard Care
The site for the study was a publicly-funded residential treatment facility for women diagnosed with SUD in Southern California. It had the capacity to provide on-site housing and comprehensive services for up to 110 women and their children. Childcare and children’s services were provided on-site along with an array of supportive services for pregnant and parenting women. The site coordinated services for women with multiple vulnerabilities, including those with mental health issues, trauma (physical and/or sexual abuse) in their past or present, and/or health problems such as HIV/AIDS. While women could remain in residential treatment for up to 12 months, the average length of stay was 5.5 months. The program included mental health and SUD diagnosis and treatment, bio-psychosocial assessment, chemical dependency education and counseling, individual and group therapy, relapse prevention, random drug testing, specialized women’s groups, trauma education and support, family education and counseling, vocational training, educational support, case management, nutritional education and support, health and wellness activities, and 12-step meetings. Referrals to the following services were made as needed: medical and dental, domestic violence, psychiatric care, GED classes, and Early Head Start. The residential treatment program was situated on a large 4-acre campus that includes residential quarters, space for group therapy and classes, a computer lab, a nursery, and a classroom for the pre-school program that is provided by the local school district.
Participants and procedures
Participants were adult women clinically diagnosed with SUD and admitted to the residential SUD treatment program study site. Upon admission, all patients met one-on-one with the site’s intake clinician coordinator who conducted an assessment for substance use disorders, mental health disorders, and suicidality using the DSM-5.33 At that time, the same clinician also completed a psychosocial assessment using an in-house form to identify important aspects of patient history and patient needs to inform case management and treatment plan. The site psychiatrist and on-site clinician coordinator discussed diagnostic assessment, determined final diagnoses, and made record in the patient chart. The site intake counselor verified study eligibility, and for those women who were eligible, informed clients about our study. The names of clients who assented to be contacted by the study team were provided to the study interviewer. The study interviewer made appointments with prospective participants, conducted the informed consent and HIPAA process, and administered the baseline assessment interview. As part of the site’s normal post-admission protocol, patients began receiving services as usual including individual and group therapy, psychoeducation groups and other services. Psychoeducation and therapy groups were scheduled on a six-week cycle.
Inclusion criteria for the research trial were: client at the residential treatment study site, female, adult aged 18–65 years, diagnosed with SUD via clinical record, fluent in English, and agreed to participate in the study. Exclusion criteria were: inability to comprehend or sign informed consent, cognitive impairment, untreated psychotic disorder or severe chronic mental health condition based on clinical intake LR-DSM-IV or DSM-V diagnostic assessment, older than 65 years of age as this was unusual at the site, reported suicidality during the prior 30 days based on clinical intake assessment, current prisoner, more than 6 months pregnant, and not willing to sign a HIPAA form or be audio recorded during interviews and intervention sessions.
Trained research staff members, blinded to group assignment and study hypotheses, captured participant data during in-person interviews using the Research Electronic Data Capture (REDCap) computer-assisted interview process. To ensure data quality control for data not immediately entered into REDCap during the participant interview (i.e., alcohol and drug test results, services received, diagnosis, admission and discharge dates and status), we applied double data entry to a minimum of 10% of randomly selected data to ensure data correctness. Baseline interviews were conducted at the study site and subsequent interviews were conducted at the study site for participants who remained in treatment or at a convenient community location for those no longer in treatment at the study site. Participants (n=14) who were incarcerated in a county jail within 90 miles one-way from the project study office at the post-intervention assessment time point were interviewed at their respective incarceration location. The postintervention interview could be completed up to 14 days after the last study class session to accommodate participant’s schedules. Baseline assessment required approximately 1.5–2 hours and post-assessments took 45–60 minutes to complete. Participants received compensation for their time (baseline and post-intervention: $30 for the interview, $5 for a urine sample, $5 for a Breathalyzer test, and $20 for transportation/babysitting for women no longer receiving services at the study site at the post intervention assessment point. Enrollment in the study was rolling until a cohort was filled. Cohorts began the assigned intervention every 6 weeks, resulting in approximately 10 women per condition to maintain a reasonably small class size.
Study interventions were held separately two times per week during the same time slot. Study participants joined the first session of their assigned group, which started every six weeks per study site protocol. The average time between residential site admission and study intervention start was 37.9 (SD=15.0) days for our sample (75% of our sample started the study intervention within 50 days of residential entry). This time interval varied across study participants due to extenuating circumstances (i.e., patient was not available for baseline interview or for the initial class session, the intervention sessions quota was filled).
Randomization
To minimize bias across study groups related to participant characteristics and histories, we applied urn randomization as implemented by the Urn Randomization Program (version 1.01) after a group of 10–30 women were deemed eligible for randomization. Strata variables were current pregnancy (yes or no) and age (18–31 years or 32–65 years) to ensure these characteristics were equivalent across groups at baseline because they can affect SUD treatment outcomes. The urn approach is robust against experimental bias in clinical trials because it is a compromise between perfect balance in treatment assignments and complete randomization to eliminate experimental bias.34 Randomization proved successful in equalizing group characteristics (see Table 1).
Table 1.
Baseline characteristics for total sample and by study group
| Variable | NA (n=100) | MMWR (n=100) | Total (n=200) |
|---|---|---|---|
| Age in years, M(SD) | 32.6 (8.4) | 32.4 (9.8) | 32.5 (9.1) |
| Race/ethnicity | |||
| Hispanic or Latina | 56 | 60 | 116 (58.0) |
| Non-Hispanic Black | 21 | 18 | 39 (19.5) |
| Non-Hispanic White | 22 | 20 | 42 (21.0) |
| Other | 1 | 2 | 3 (1.5) |
| Marital status | |||
| Married or common law | 6 | 6 | 12 (6.0) |
| Never married | 75 | 76 | 151 (75.5) |
| Separated or divorced | 19 | 18 | 37 (18.5) |
| Currently pregnancy | 7 | 5 | 12 (6.0) |
| Has one or more children | 88 | 89 | 177 (88.5) |
| No. of children, M(SD) | 2.5 (2.0) | 2.4 (1.6) | 2.5 (1.8) |
| Education level | |||
| Less than high school | 46 | 47 | 93 (46.5) |
| Completed high school | 28 | 31 | 59 (29.5) |
| Some education after high school | 26 | 22 | 48 (24.0) |
| Unemployed prior to residential entry | 71 | 73 | 144 (72.0) |
| Homeless prior to residential entry | 23 | 24 | 47 (23.6) |
| Incarcerated any time 8 months prior to treatment entry | 65 | 59 | 124 (62.0) |
| In restricted environment in 8 months prior to residential entry | 100 | 99 | 199 (99.5) |
| Proportion of restricted days during 8 months prior to residential entry | 0.34 (0.28) | 0.30 (0.32) | 0.32 (0.3) |
| Mandated to residential | 82 | 83 | 165 (82.5) |
| Mandating agency | |||
| Criminal Justice System | 51 | 46 | 97 (48.5) |
| Department of Children and Family Services | 31 | 37 | 68 (34.0) |
| Not mandated | 18 | 17 | 35 (17.5) |
| Outpatient treatment received 30 days prior to residential entry | 20 | 18 | 38 (19.0) |
| Used substance during 8 months prior to residential entry | |||
| Amphetamines/methamphetamine | 79 | 73 | 152 (76.0) |
| Cannabis | 55 | 50 | 105 (52.5) |
| Alcohol to intoxication (5 or more drinks in one sitting) | 49 | 51 | 100 (50.0) |
| Cocaine and/or crack | 12 | 14 | 26 (13.0) |
| Other sedatives/hypnotics/tranquilizers | 10 | 7 | 17 (8.5) |
| Hallucinogens | 7 | 6 | 13 (6.5) |
| Heroin | 8 | 5 | 13 (6.5) |
| Opiates/analgesics | 6 | 7 | 13 (6.5) |
| Methadone, non-prescription | 1 | 2 | 3 (1.5) |
| SUD diagnosis at residential entry | |||
| AUD only | 10 | 9 | 19 (9.5) |
| DUD only | 71 | 74 | 145 (72.5) |
| Both AUD and DUD | 18 | 14 | 32 (16.0) |
| Current use of medically assistant treatment (MAT) for alcohol or opiates | 1 | 2 | 3 (1.5) |
| MHD diagnosis other than SUD+ | |||
| None | 30 | 37 | 67 (33.5) |
| One | 45 | 49 | 94 (47.0) |
| Two or more | 24 | 11 | 35 (17.5) |
| MHD diagnosisa | |||
| PTSD+ | 40 | 21 | 61 (30.5) |
| Depressive Disorder | 18 | 21 | 39 (19.5) |
| Trauma history, LSC-R | |||
| Childhood trauma | 84 | 86 | 170 (85.0) |
| Adulthood trauma+ | 83 | 74 | 157 (78.5) |
| Sexual trauma | 69 | 71 | 140 (70.0) |
| Physical trauma | 71 | 72 | 143 (71.5) |
| PTSD symptoms, PSS-SR total, M(SD)+ | 18.6 (13.1) | 16.2 (11.9) | 17.4 (12.5) |
| ASI severity during 30 days prior to study baseline, M(SD) | |||
| Alcohol problems | 0.10 (0.16) | 0.10 (0.17) | 0.10 (0.17) |
| Drug problems | 0.12 (0.10) | 0.11 (0.10) | 0.11 (0.10) |
| Family problems | 0.27 (0.25) | 0.24 (0.24) | 0.25 (0.24) |
| Legal problems | 0.23 (0.26) | 0.19 (0.24) | 0.21 (0.25) |
| Days in residential prior to study intervention start, M(SD) | 37.4 (14.1) | 38.4 (15.9) | 37.9 (15.0) |
Note. Data are presented as number (percent) unless otherwise noted as mean (standard deviation). NA = Neurobiological of Addiction active control condition; MMWR = Moment by Moment in Women’s Recovery; AUD = alcohol use disorder; DUD = drug use disorder; ASI = Addiction Severity Index; PSS-SR=PTSD Symptom Scale Self Report; LSC-R=Life Stressor Checklist Revised; MHD = Mental Health Disorder diagnosed by DSM-V.
= diagnoses present in <10% of total sample not reported
used as covariates in adjusted models due to a priori standard set for baseline group difference at p<.20.
Interventions
Moment-by-Moment in Women’s Recovery (MMWR)
This intervention was delivered twice weekly for 80 minutes each for a total of 12 group sessions (6 weeks) during residential treatment. MMWR was guided by an instructional manual with standardized lesson plans. An experienced teacher trained in both MBSR and MMWR facilitated all sessions along with an on-site masters-level clinician with experience in SUDs who co-facilitated the intervention. Each class session had a central theme divided into five segments in the following general order: (1) welcome, review of group culture, brief homework practice check-in, objectives, and brief mindfulness meditation or practice; (2) didactic psychoeducational presentation and discussion of lesson content; 3) experiential meditation and mindfulness practices related to the session’s theme; (4) practice of sitting or walking meditation, body scan, and/or standing stretching; and (5) selected reading related to session topic, assignments for the next class, and closing meditation. Trainees were expected to learn skills to approach experiences and stressors using mindfulness principles. Students learned about the role of automatic reactivity to stressors and its relation to addiction and relapse; the connections between stress, triggers, and relapse; and how to use mindfulness practices to respond best to related thoughts, emotions, body sensations (including those related to stress in a residential treatment setting that could lead to treatment dropout), and triggers while still avoiding relapse. As with MBSR, trainees learned and practiced self-regulation strategies using four foundational mindfulness practices. Teachers instructed on the use of formal (audio-guided sitting meditation, sitting meditation without audio, loving kindness meditation, walking meditation, body scan, and mindful stretching) and informal practices (stop light technique, triangle of awareness, mindfulness of breath, mindfulness of emotions, mindfulness of thoughts, mindfulness of body sensations, and mindfulness of cravings). Throughout the course, students were encouraged to bring mindful awareness into their daily activities by using informal practices and to engage in practice formal meditation practices as homework in accordance with practice assignments and guided meditation audio recordings. Participants received a MMWR Participant Workbook at the beginning of the course organized by session, containing key concepts and practices introduced in each session, and homework and practice assignments for each session. Participants were asked to bring their Workbook to each session so that they could report on the previous week’s assignment and the current session’s homework and practice assignments could be explained by the facilitator and reviewed as women followed along. Some assignments asked participants for specific reflections and written responses. Participants received a MP3 player with meditation audios for each session to guide participants through practices introduced in each session.
Neurobiology of Addiction (NA) psychoeducation attention control
This intervention was delivered twice weekly for 80 minutes each for a total of 12 group sessions (6 weeks) during residential treatment. NA was guided by an instructional manual with standardized lesson plans (Amaro 2016, unpublished facilitator’s manual). The curriculum was previously developed by H.A. over 3 years with input and review from focus groups of women and providers in SUD treatment, and subsequently reviewed by three experts in NA. A masters-level educator with a background and training in the NA facilitated all sessions and an on-site masters-level clinician with experience in SUDs and training in NA co-facilitated the intervention. Participants received didactic education on the structure and function of the brain and the neurobiology of addiction. Although educational and centered on knowledge acquisition, the program has no proven efficacy in altering substance use behavior. It included didactic psychoeducational presentation using PowerPoint, video recordings, exercises, games, and group discussions to reinforce the session content and respond to questions. Sessions did not address behavior change strategies, stress reduction, mindfulness, or relapse-related content. Films, videos, exercises, activities, and discussions were used to explain content and promote participant engagement. Topics included: (1) definition of addiction and why it is a brain disease; (2) brain structures and functions and those related to addiction; (3) effects of various types of substances on the brain; (4) rewarding effects of substances and how these effects lead to addiction; (5) definitions and brain functions related to craving and withdrawal; and (6) the roles of treatment in recovery. Participants were expected to gain knowledge pertaining to basic brain structure and function and the effects of drugs on both. The intervention was equivalent to MMWR in time, teacher attention, expectancy of benefit, and group support. Participants received a NA Participant Workbook organized by session that included session specific information covered in each session such as selected PowerPoint slides and were asked to bring these to class to help them identify questions they had from the previous session. Participants received MP3 players with audio clips of key sections of videos introduced in class.
Teacher training and certification
Teachers for each intervention had at least two years of experience in their respective topics. MMWR lead teachers hired for this project were experienced mindfulness facilitators; one was in the process of acquiring MBSR instructor certification at the start of the project. The first MMWR facilitator received five days of intensive training by H.A. The second teacher, hired later in the project, received training in mindfulness intervention delivery and was trained on MMWR by the first teacher, the MMWR certified senior teacher, and the co-developers of MMWR. Both facilitators received training and ongoing supervision from a MBSR-certified senior teacher and co-developer of MMWR to ensure that the MMWR teachers in the study remained adherent to the foundational principles of mindfulness practice and the MMWR curriculum. The group was led by one masters-level teacher hired by the research project and co-led by an on-site counselor. Both received an intensive 5-day training by H.A. After initial training, lead teachers conducted an audiotaped 12-session cohort of their respective intervention with a pilot group of participants at the study site. Audio recordings of the pilot groups were rated for fidelity by independent raters to ensure high fidelity prior to onset of study cohorts. We established interrater reliability on fidelity ratings at study onset using one pilot cohort and continued to review rater agreement every two months. Ongoing supervision and support were provided to MMWR teachers by H.A. and a certified MBSR consultant who co-developed MMWR with H.A and to NA teachers by H.A. and a SUD clinician consultant who co-developed NA with H.A.
After the pilot sessions, all study intervention group sessions were recorded, and 6 out of 12 (50%) randomly selected sessions for each cohort were assessed for fidelity by two raters trained and supervised by H.A. A detailed description of treatment fidelity methods for this trial has been previously published.35 Trained research staff members used a published MBI fidelity measure called the Mindfulness-Based Relapse Prevention Adherence and Competence Scale36 that was slightly modified to fit the intervention content in order to independently rate the selected sessions for each cohort. In the current study, scores on adherence to respective curriculum (MMWR M=1.99/2; NA M=1.94/2) and teacher competence in delivering their respective intervention were high (Mean = 4.9/5 in both groups).
Measures
Discharge Status
Following routine site protocol, the SUD site treatment team (i.e., certified SUD counselor, masters-level clinician therapist, and team supervisor masters-level therapist; the latter two registered with the Board of Behavioral Sciences) decided on a case-by-case basis if a client developed the necessary skills to complete residential treatment. One of three clinical progress designations was documented in a patient’s chart at discharge based on their progress. Completer: patient completed course of treatment, met treatment goals and were sufficiently stable (i.e., developed sufficient coping skills, attended groups, adhered to requirements on days away from the facility such as calling in, returning on time and negative drug screen) to transition to stepped-down care. Non-completer with satisfactory progress: patient left treatment before completion of the treatment plan and before achieving all treatment goals, but deemed by the clinical team as having made important progress toward treatment goals and improved stability. Non-completer without satisfactory progress: patient left treatment before completion of the treatment plan and the clinical team determined that little or no progress was made toward achieving treatment goals (i.e., left early in treatment without being able to receive many services, administratively discharged due to multiple occasions of relapse as assessed by drug screens without changes in behavior, repeatedly violated residential treatment rules such as bringing drugs on site). In-residence: patient remained in treatment at the residential treatment facility at the end of the analytic period (i.e., day 150). It was not possible to blind the discharge team to group assignment; however, the study was presented to the discharge team as a test of two alternative intervention approaches in an effort to prevent any unbalanced expectation of treatment benefit.
Days until discharge
We used site discharge records to calculate the number of days in residential treatment beginning from the study intervention start date (day 0) and ending at day 150. We selected an analytic time period to approximate the average length of stay at the SUD treatment site (5.5 months).
Self-report measures
Measures were assessed at baseline and post-intervention by participant self-report on validated psychometric scales of mindfulness disposition (Five Facet Mindfulness Questionnaire, FFMQ-SF),37 perceived stress (Perceived Stress Scale, PSS-10),38 distress tolerance (Distress Tolerance Scale, DTS),39 emotion regulation (Difficulties in Emotional Regulation Scale, DERS),40 psychological distress (Depression, Anxiety and Stress Scale, DASS-21),41 affect (Positive and Negative Affect Scale, PANAS),42 and drug and alcohol craving (Penn Alcohol Craving Scale, inclusive of multiple substances, PACS).43 Intervention satisfaction was assessed via self-report at the 2nd and 11th class sessions using a form comprised of 17 items (response options of 1–5 with higher score indicating more satisfaction with the intervention) developed by the research team that assessed the learning experience, usefulness, enjoyment, and the facilitator. We computed an overall mean score for the two assessments with greater score indicating higher satisfaction with the course. Class attendance was obtained by sign-in sheet.
Data analysis
Power analysis yielded an estimated sample size of 200 to 225 needed to detect a medium-sized effect (hazard ratio=0.52 to 0.54) for residential treatment retention using a log-rank test with a two-sided 5% significance level and 80% power, given the probability of remaining in the treatment program in the control group is 50%. We conducted standard statistical diagnosis and performed descriptive analyses of background variables, assessed variable distributional properties, plotted means of the continuous outcome variables at each time point, and assessed internal consistency and test–retest reliability of study scales. We verified the adequacy of randomization on demographic and clinical covariates, and identified variables found to differ between groups at p<.20 (Table 1) to include them as model covariates. Based on this criteria, the covariates included in all adjusted models were number of mental health diagnoses (i.e., SUD only, 1 comorbid mental health dx, 2+ comorbid mental health dx), adulthood trauma exposure (LSC-R), PTSD diagnosis by DSM-5, and PTSD symptom score (PSS-SR), as well as a study design feature (i.e., days in residential treatment prior to study intervention start date obtained from clinic records) to account for exposure to residential treatment prior to the start of our study intervention.
To examine the differential risk of the outcome event (i.e., patient left treatment before completion of the treatment plan and made little or no progress toward achieving treatment goals based on clinical team determination), we applied Kaplan-Meier survival analysis using an intent-to-treat (ITT) approach with time starting on the first day of the study intervention and ending 150 days later. Participants with the discharge status of completer, non-completer with significant progress, and in-residence were coded as 1 for “retention”. Participants with the discharge status of non-completers without significant progress were coded as 0 for “non-retention.” Our examination of the survival curves revealed that group curves crossed at 50 days from the start of the intervention, which indicated the need for a piecewise model. Thus, a multivariable, 2-piece model (i.e., Piece 1 predicting outcome events during day 0–50 and Piece 2 predicting outcome events for days 51–150) was calculated. The first piece of the model coincided with the study intervention period and the second piece to the post-intervention period. Adjusted Cox proportional hazards regression (PROC PHREG), with days as the time scale, provide estimates of hazard ratios (HR) and the 95% confidence intervals (CI) for the non-retention outcome event. HR effect size estimates are categorized as small (0.77), medium (0.53), and large (0.36).44 We conducted logistic regression (PROC LOGISTIC) to test for group differences in satisfactory progress among the subgroup of non-completers. We used general linear mixed models (PROC MIXED) to examine differential changes in the self-reported mechanism of action variables from pre-intervention to post-intervention by group, adjusting for covariates. We used Pearson r to test for correlation between class attendance (as a dosage variable) and change in mechanisms of action measure scores. Pearson r effect sizes are small (.10), moderate (.30), or large (.50). All analyses were conducted in SAS version 9.4 (SAS Institute). All models used a maximum likelihood estimated approach to account for missingness.
Results
Of 367 potential participants who were screened for the study at the residential site, 225 were eligible and randomized to study conditions (see Figure 1 for CONSORT diagram). Those who missed the first study class session (class overview and introduction) were excluded from the study by design leaving N=200 enrolled in the trial, 100 per condition. Average class attendance was 9.5 (SD=3.2) sessions in the MMWR group and 9.9 (SD=2.9) sessions in the control group (p=.33). The number of women completing 9 or more of the 12 class sessions (i.e., classified as intervention completion) did not differ by group (MMWR n=74; NA n=80, p=.60). For the total sample, the length of stay in residential treatment from study intervention start date to analytic endpoint (days 150) was 94.4 days (SD=59.3, range=190), which did not differ by group. Overall loss to follow-up at post-interview assessment was low at 8% and did not differ by group (MMWR=10%, NA=6%, p=.30).
Figure 1. Trial CONSORT diagram.
Note. NA = Neurobiology of Addiction active control condition; MMWR = Moment by Moment in Women’s Recovery; ITT = intent to treat. By design, women missing the first class introduction session were not enrolled in the study, as they were likely to have already left the treatment facility.
Table 1 provides descriptive characteristics for the total sample and by group. The mean age of the sample was 32.5, 58% of the women self-identified as Hispanic or Latina, 46.5% had less than a high school education, 62% had been incarcerated in the 8 months prior to residential treatment entry, and 76% were amphetamine/methamphetamine users. There were no significant (p<.05) differences at baseline measure scores by group; however, p<.20 (determined a priori) trends were observed for four clinically meaningful variables including comorbid mental health diagnosis, adulthood trauma history, PTSD diagnosis, and PTSD symptom score. Scores for participant self-reported satisfaction with the study interventions were high and did not differ by group (MMWR: M=4.13 (SD=0.61) out of 5; control: M=4.13 (SD=0.67) out of 5, p=.93).
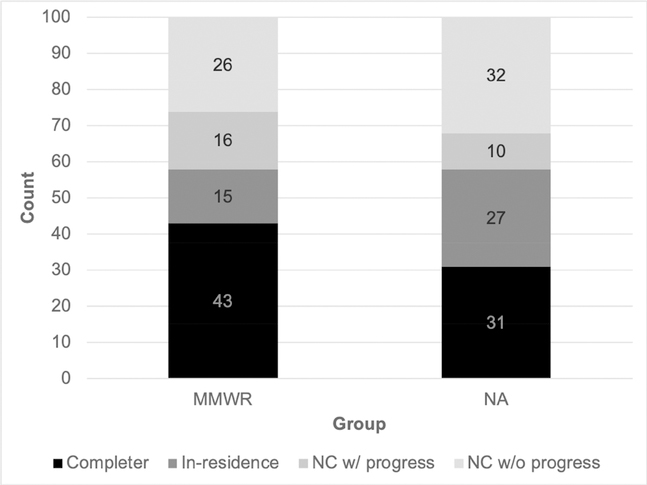
Discharge status and time to non-retention event by study group
Figure 2 shows the discharge status of participants by group from intervention start date to day 150. The count of women defined as treatment Completers was 43/100 in the MMWR group versus 31/100 in the control group (adjusted OR=1.63, CI: 0.88–3.01, p=.12). The count of women In-residence was 15/100 in the MMWR group and 27/100 in the control group (adjusted OR=0.51, CI: 0.25–1.07, p=.08). Among the 84 treatment Non-completers, satisfactory progress was made by 16/42 women in the MMWR group and 10/42 women in the control group (adjusted OR=2.75, CI: 0.91–8.30, p=.07). For the ITT sample (N=200), the adjusted piecewise Cox proportional hazards model results are presented in Table 2. Survival analysis showed that risk of non-completion without improvement was lower in MMWR as compared to the control group after the study intervention (Piece 1: adjusted HR=1.20, 95% CI: 0.59–2.24, p=.68; Piece 2: adjusted HR=0.42, 95% CI: 0.16–1.08, p=.07). This HR effect of 0.42 is characterized as medium-to-large size.
Figure 2. Residential treatment discharge status by group across 150 day period, N=200.
Note. NC=Non-completer with (w) or without (w/o) satisfactory progress. Completer: patient completed the course of SUD residential treatment; In-residence: patient still at the residential treatment site at analytic endpoint (i.e., day 150); NC w/ progress: patient left treatment site before completion of the treatment plan and before achieving all treatment goals but are deemed by the clinical team as having made important progress toward their treatment goals and person demonstrated improved stability but require additional intensive treatment; NC w/o progress: patient did not complete treatment and the clinical team determines that they made little to no progress toward achieving treatment goals.
Table 2.
Piecewise Cox proportional-hazards model predicting days until residential leave without satisfactory progress
| Variable | B (SE) | Hazard Ratio (95% CI) | p |
|---|---|---|---|
| Piece 1: Study intervention period | |||
| Group (reference: control) | 0.14 (0.34) | 1.12 (0.59–2.24) | .68 |
| Piece 2: Post-intervention period | |||
| Group (reference: NA control) | −0.8 (0.49) | 0.42 (0.16–1.08) | .07 |
| Covariates | |||
| Days in residential prior to study intervention | −0.02 (0.01) | 0.98 (0.96–0.99) | .03 |
| Number of mental health diagnoses | −0.18 (0.24) | 0.83 (0.52–1.27) | .45 |
| Adulthood trauma (LSC-R) | −0.36 (0.31) | 0.70 (0.38–1.27) | .24 |
| PTSD diagnosis | 0.02 (0.37) | 1.03 (0.49–2.13) | .95 |
| PTSD symptoms (PSS-SR) | −0.01 (0.01) | 0.99 (0.97–1.01) | .50 |
Note. Piece 1 defined as overlapping with the study intervention period (day 0 to 50); Piece 2 defined as post-intervention period (day 51 to 150); PSS-SR=PTSD Symptom Scale Self Report; LSC-R=Life Stressor Checklist Revised.
Change in self-reported intervention mechanisms of action by group and by class attendance
The results of the general linear mixed models are presented in Table 3. Baseline mean scores for the eight proposed self-report measures did not differ by groups (p range=.15-.86). At post-intervention, the eight measures were in the direction of improvement for both groups, and a significant time effect was observed in both groups for FFMQ, DTS, DERS and PACS scores at post-intervention. The group by time effect did not reach statistical significance for any of the eight measures. A large-size correlation was found between study intervention class attendance (i.e., an intervention dosage measure) and increased FFMQ scores in the MMWR group (r=.61, p<.01) but not the control group (r=.15, p=.14). In the MMWR group, dosage had a large-size correlation with increased DTS scores (r=.55, p<.01) and increased PANAS-P (r=.52, p<.01) and small-size correlation with increased PSS scores (r=.21, p=.03). In the control group, dosage had a small-size correlation with increased PSS scores (r=.20, p=.04), increased DERS scores (r=.20, p=.04), and increased DASS scores (r=.21, p=.04). No other mechanisms measure scores met the significance threshold for either group in relation to class attendance.
Table 3.
Self-report measure scores by group and time
| Pre-intervention | Post-intervention | Group x time p | Cohen’s d | |||
|---|---|---|---|---|---|---|
| Measure | NA | MMWR | NA | MMWR | ||
| FFMQ-SF | 78.1 (1.2) | 77.9 (1.2) | 85.0 (1.2)** | 83.4 (1.3)** | .50 | 0.10 |
| PSS-10 | 20.8 (0.6) | 19.7 (0.6) | 17.6 (0.6)* | 18.1 (0.7) | .21 | 0.24 |
| DTS | 2.9 (0.1) | 3.1 (0.08) | 3.2 (0.1)* | 3.3 (0.1)* | .36 | 0.15 |
| DERS | 85.7 (2.3) | 82.7 (2.3) | 74.4 (2.4)** | 73.9 (2.4)** | .52 | 0.11 |
| DASS-21 | 10.72 (0.61) | 10.16 (0.61) | 9.13 (0.63) | 9.54 (0.64) | .40 | 0.16 |
| PANAS-N | 26.2 (0.8) | 24.5 (0.8) | 23.7 (0.8)* | 23.2 (0.8) | .47 | 0.13 |
| PANAS-P | 36.4 (0.9) | 36.9 (0.9) | 37.3 (0.9) | 38.4 (0.9) | .60 | 0.08 |
| PACS | 2.2 (0.2) | 2.1 (0.2) | 1.4 (0.2)** | 1.6 (0.2)** | .26 | 0.28 |
Note. Data are mean (standard deviation) unless otherwise noted. FFMQ-SF=Five Facet Mindfulness Questionnaire-short form; PSS-10=Perceived Stress Scale; DTS=Distress Tolerance Scale; DERS=Difficulties in Emotion Regulation Scale; DASS-21= Depression Anxiety and Stress Scale; PANAS=Positive and Negative Affect Scale – Negative (N) or Positive (P); PACS=Penn Alcohol Craving Scale. All models adjusted for days in residential prior to study intervention, number of mental health diagnoses, LSC-R, and PSS-SS. Measure scores do not differ by study group at baseline (all p’s>.10).
p<.01 and
p<.05 for within-subjects time effect.
Discussion
In this experimental trial, we tested MMWR against a psychoeducational attention control group to determine its efficacy in improving SUD treatment retention when applied as an adjunctive intervention to residential treatment. Survival analysis showed that MMWR participants compared to controls were less likely to leave residential treatment without satisfactory progress following the intervention period. The effect size was medium-to-large, thus suggesting clinical importance for effects on residential SUD retention, a factor previously predictive of relapse and readmission to SUD treatment.45 We interpret the trial results to show that the skills achieved in MMWR were responsible for clinically meaningful changes that guided site clinical team determination of treatment completion and/or satisfactory progress made at discharge. This treatment effect was medium-to-large, and exceeded that of an attention control condition, while both conditions were being delivered during residential treatment for SUD wherein several intensive psychotherapies and social services were simultaneously provided to clients at the site. We interpret this finding to show that MMWR helped women better manage the challenges posed by intensive residential treatment and thus supported SUD treatment retention and satisfactory progress made while at the site.
This work builds on our previous study that tested the acceptability and promise of MMWR using a within-subjects repeated-measures design among women attending outpatient or residential SUD treatment.28 Our earlier study did not randomly assign treatment exposures, lacked a control group, and did not assess SUD residential treatment retention. Only one other study we are aware of has evaluated the use of a MBI (i.e., Mindfulness Based Therapeutic Community, MBTC) during residential SUD treatment, but the study included a mixed-gender, majority White sample and used an inactive historical control group. We delivered MMWR twice per week across 12 sessions, while Marcus et al25 delivered MBTC in 6 sessions across 4 weeks, and conducted a survival analysis of time to treatment dropout, founding no significant difference between a MBI and treatment as usual. However, their index of greater participation (i.e., the product of the number of class hours attended multiplied by the average level of teacher-reported engagement score for all classes attended) was associated with decreased likelihood of treatment dropout in the MBI group. Beyond days until dropout as used in Marcus et al., our study extends these findings by examining the level of satisfactory progress premature dropouts make up to their discharge date, which is an important clinical outcome as it suggests a client is making therapeutic progress toward recovery.
We assessed change in a comprehensive set of self-reported measures that we considered as potential mechanisms of action that aligned with previous theoretical arguments16 as well as results garnered from laboratory and clinical studies.18,19 As expected, women reported measure scores in the direction of improvement for all outcomes at post-intervention. However, these improvements were not found to differ by study group likely due to the commensurate improvements in the control group and the overall sample receiving extensive SUD treatment services at the residential site. More informative about the MMWR therapeutic process is our observed associations between study intervention class attendance as a dosage measure and the proposed mechanisms measures. Both study intervention groups showed a small-sized correlation between dosage and perceived stress levels, a finding to support our premise that exposure to any course as part of residential treatment can moderately increase stress levels due to the many challenges of engaging with the SUD treatment process and therapeutic change. However, we observed that MMWR dosage had a large-size correlation with increased mindfulness and positive affect levels and reduced distress levels. Thus, stress can be common as part of residential living and recovery, yet people may use mindfulness skills to better navigate stress as a means to bolster positive affect and stymie distress. The control group, which focused on psychoeducation about alcohol and drug use and related health effects, did not show a protective effect of dosage and any of the mechanisms measures. In fact, control group dosage was associated with increased emotion dysregulation and distress. This could suggest that psychoeducation alone without therapeutic content such as mindfulness might slightly increase stress levels during residential treatment and lack the adaptive benefits in affect and distress tolerance found for MMWR. It is also possible that other intervention mechanisms were at work outside of those we measured in this study such as reduction in personal conflicts at the residential site, motivation to stay in treatment, and self-efficacy to make satisfactory clinical progress. These intervention mechanisms should be considered in future studies of people in residential treatment for SUD.
Most experimental trials testing MBIs among adults with SUD have focused on the outpatient, aftercare period with mixed-sex samples.13,22 As a result, there are few comparisons to make for our findings on MMWR intervention mechanisms of action. However, one RCT conducted at a residential site tested a MBI against TAU in a mixed-sex sample.46 After their four-week intervention, MBI participants reported improvements on mindfulness disposition, psychological flexibility, and substance craving measure scores. As with our findings, these changes did not differ by group at post-intervention. This replicated finding may be attributable to the daily, intensive psychotherapy and milieu of interventions received during residential treatment that overlapped with the study intervention period. It is also possible that the observable benefits of MBIs on psychological outcomes among populations with complex mental health diagnoses require longer than six weeks to develop, and thus may be seen upon longer term follow-up assessment, especially if the practice of mindfulness is continued with some consistency.
In terms of study limitations, we do not administer a MBI sham control group, which is a promising protocol to support the internal validity of experimental trials. Our decision to exclude a sham was intended to avoid possible negative effects of inaccurate meditation training on this vulnerable population that exhibits active mental health disorders. As a strength, our psychoeducational attention control condition matched MMWR in terms of time, attention, intervention satisfaction, teacher, social support, and other nonspecific effects. Given the effect size for retention and the lack of change in mechanisms measures by group, it is also possible that our control curriculum was equally beneficial to some self-reported measures of therapeutic change, which was evident for significantly improved scores in both groups for the FFMQ, DTS, DERS and PACS. NA included pertinent information about the impact of drugs on brain activity and pathology, which could be motivating for women fearful of further damaging their brain to remain in treatment and hence improving measure scores. It is also possible that MMWR has a true null effect on the mechanisms of action measured and the treatment retention outcome; however, the significant study intervention dosage findings are at least somewhat contradictory to this argument. Given the lack of group blinding, participants figure out the treatment type once the treatment begins and so there is the associated possibility of reporting bias. However, we masked assignment information from participants until the first day of the study intervention to guard against this threat, and there were no group differences on study intervention satisfaction scores. We also masked individuals who conducted the outcome interviews from group assignment. Cross-contamination is possible because both classes were delivered at the same residential site, so we used separate class locations at the facility and fidelity ratings by teacher report in each group indicated negligible threat. We did not collect self-report data coinciding with the 150 day analytic end-point, negating our ability to test for delayed treatment effects on these measures. Lastly, we delivered MMWR across 6 weeks to better fit the residential site clinical services structure, which is an interval that differs from the traditional 8–12 weeks common to MBIs and our previous study that employed MMWR delivery over 12 weeks, and so it may take longer for therapeutic changes to occur. Future studies could consider investigating the optimal length of MMWR delivery in a residential setting.
Highlights.
MMWR participants compared to attention controls were less likely to leave residential treatment without satisfactory progress following the intervention period.
The effect size was medium-to-large, thus suggesting clinical importance for effects on residential SUD retention, a factor previously predictive of relapse and readmission to SUD treatment.
The effect size for retention as compared to a psychoeducational control group is impressive considering the sample was simultaneously exposed to daily, intensive, SUD residential services.
We interpret this finding to show that MMWR helped women better manage the challenges posed by intensive residential treatment and thus supported SUD treatment retention and satisfactory progress made while at the site.
Acknowledgements
Funding support provided by a grant from the National Institute on Drug Abuse and the National Institute on Alcohol Abuse and Alcoholism (R01DA038648 to D.B. and H.A.). The ideas and opinions expressed herein are those of the authors. Endorsement of those opinions by funders is neither intended nor inferred. We are grateful to Jimi Huh and Lei Duan for the statistical analyses, to Guillermo Prado for comments on an earlier draft of this manuscript, and to our project staff: Luz Rodriguez, Connie Valencia, Sydney Reece, Joslyn Hitter, study interviewers, research assistants, and treatment site staff: April Wilson, Garett Scaley, Danielle Buckland, Kellie Wittet, Katie Williams, Jaclyn Padilla, and Denise Valdivia.
Footnotes
Conflict of interest statement: All authors declare that there are no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Brorson HH, Ajo Arnevik E, Rand-Hendriksen K, Duckert F. Drop-out from addiction treatment: a systematic review of risk factors. Clin Psychol Rev. 2013;33(8):1010–1024. [DOI] [PubMed] [Google Scholar]
- 2.McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA : the journal of the American Medical Association. 2000;284(13):1689–1695. [DOI] [PubMed] [Google Scholar]
- 3.Hser YI, Evans E, Huang D, Anglin DM. Relationship between drug treatment services, retention, and outcomes. Psychiatr Serv. 2004;55(7):767–774. [DOI] [PubMed] [Google Scholar]
- 4.Simpson DD, Joe GW, Brown BS. Treatment retention and follow-up outcomes in the Drug Abuse Treatment Outcome Study (DATOS). Psychology of Addictive behaviors. 1997;11(4):294. [Google Scholar]
- 5.Condelli WS, Koch MA, Fletcher B. Treatment refusal/attrition among adults randomly assigned to programs at a drug treatment campus: The New Jersey Substance Abuse Treatment Campus, Seacaucus, NJ. J Subst Abuse Treat. 2000;18(4):395–407. [DOI] [PubMed] [Google Scholar]
- 6.Du J, Huang D, Zhao M, Hser YI. Drug-abusing offenders with co-morbid mental disorders: gender differences in problem severity, treatment participation, and recidivism. Biomed Environ Sci. 2013;26(1):32–39. [DOI] [PubMed] [Google Scholar]
- 7.Hser YI, Huang D, Teruya C, Douglas Anglin M. Gender comparisons of drug abuse treatment outcomes and predictors. Drug Alcohol Depend. 2003;72(3):255–264. [DOI] [PubMed] [Google Scholar]
- 8.Grella CE, Joshi V. Gender differences in drug treatment careers among clients in the national Drug Abuse Treatment Outcome Study. Am J Drug Alcohol Abuse. 1999;25(3):385–406. [DOI] [PubMed] [Google Scholar]
- 9.Grella CE. Women in residential drug treatment: differences by program type and pregnancy. J Health Care Poor Underserved. 1999;10(2):216–229. [DOI] [PubMed] [Google Scholar]
- 10.Niv N, Hser YI. Women-only and mixed-gender drug abuse treatment programs: service needs, utilization and outcomes. Drug Alcohol Depend. 2007;87(2–3):194–201. [DOI] [PubMed] [Google Scholar]
- 11.Saloner B, Le Cook B. Blacks and Hispanics are less likely than whites to complete addiction treatment, largely due to socioeconomic factors. Health Aff (Millwood). 2013;32(1):135–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kabat-Zinn J Mindfulness-Based Interventions in Context: Past, Present, and Future. Clinical Psychology: Science and Practice. 2003;10(2):144–156. [Google Scholar]
- 13.Bowen S, Witkiewitz K, Clifasefi SL, et al. Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: a randomized clinical trial. JAMA Psychiatry. 2014;71(5):547–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garland EL, Manusov EG, Froeliger B, Kelly A, Williams JM, Howard MO. Mindfulness-oriented recovery enhancement for chronic pain and prescription opioid misuse: results from an early-stage randomized controlled trial. J Consult Clin Psychol. 2014;82(3):448–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garland EL, Roberts-Lewis A. Differential roles of thought suppression and dispositional mindfulness in posttraumatic stress symptoms and craving. Addict Behav. 2013;38(2):1555–1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Witkiewitz K, Lustyk MKB, Bowen S. Retraining the addicted brain: a review of hypothesized neurobiological mechanisms of mindfulness-based relapse prevention. Psychol Addict Behav. 2013;27(2):351–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ali B, Green KM, Daughters SB, Lejuez CW. Distress tolerance interacts with circumstances, motivation, and readiness to predict substance abuse treatment retention. Addict Behav. 2017;73:99–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brewer JA, Sinha R, Chen JA, et al. Mindfulness training and stress reactivity in substance abuse: results from a randomized, controlled stage I pilot study. Substance Abuse. 2009;30(4):306–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garland EL, Roberts-Lewis A, Tronnier CD, Graves R, Kelley K. Mindfulness-Oriented Recovery Enhancement versus CBT for co-occurring substance dependence, traumatic stress, and psychiatric disorders: Proximal outcomes from a pragmatic randomized trial. Behav Res Ther. 2016;77:7–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chiesa A, Serretti A. Are mindfulness-based interventions effective for substance use disorders? A systematic review of the evidence. Subst Use Misuse. 2014;49(5):492–512. [DOI] [PubMed] [Google Scholar]
- 21.Witkiewitz K, Bowen S, Douglas H, Hsu SH. Mindfulness-based relapse prevention for substance craving. Addict Behav. 2013;38(2):1563–1571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bowen S, Chawla N, Collins SE, et al. Mindfulness-based relapse prevention for substance use disorders: a pilot efficacy trial. Subst Abus. 2009;30(4):295–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Witkiewitz K, Warner K, Sully B, et al. Randomized Trial Comparing Mindfulness-Based Relapse Prevention with Relapse Prevention for Women Offenders at a Residential Addiction Treatment Center. Substance use & misuse. 2014;49(5):536–546. [DOI] [PubMed] [Google Scholar]
- 24.Witkiewitz K, Greenfield BL, Bowen S. Mindfulness-based relapse prevention with racial and ethnic minority women. Addict Behav. 2013;38(12):2821–2824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marcus MT, Schmitz J, Moeller G, et al. Mindfulness-based stress reduction in therapeutic community treatment: a stage 1 trial. Am J Drug Alcohol Abuse. 2009;35(2):103–108. [DOI] [PubMed] [Google Scholar]
- 26.Vallejo Z, Amaro H. Adaptation of mindfulness-based stress reduction program for addiction relapse prevention. The Humanistic Psychologist. 2009;37(2):192–206. [Google Scholar]
- 27.Marlatt GA, George WH. Relapse prevention: introduction and overview of the model. Br J Addict. 1984;79(3):261–273. [DOI] [PubMed] [Google Scholar]
- 28.Amaro H, Spear S, Vallejo Z, Conron K, Black DS. Feasibility, acceptability, and preliminary outcomes of a mindfulness-based relapse prevention intervention for culturally-diverse, low-income women in substance use disorder treatment. Subst Use Misuse. 2014;49(5):547–559. [DOI] [PubMed] [Google Scholar]
- 29.Bowen S, Enkema MC. Relationship between dispositional mindfulness and substance use: findings from a clinical sample. Addict Behav. 2014;39(3):532–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hopwood CJ, Schade N, Matusiewicz A, Daughters SB, Lejuez CW. Emotion regulation promotes persistence in a residential substance abuse treatment. Subst Use Misuse. 2015;50(2):251–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Andersson HW, Steinsbekk A, Walderhaug E, Otterholt E, Nordfjaern T. Predictors of Dropout From Inpatient Substance Use Treatment: A Prospective Cohort Study. Subst Abuse. 2018;12:1178221818760551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Amaro H, Black DS. Moment-by-Moment in Women’s Recovery: Randomized controlled trial protocol to test the efficacy of a mindfulness-based intervention on treatment retention and relapse prevention among women in residential treatment for substance use disorder. Contemp Clin Trials. 2017;62:146–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Association AP. Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: Author; 2013. [Google Scholar]
- 34.Wei LJ, Lachin JM. Properties of the urn randomization in clinical trials. Control Clin Trials. 1988;9(4):345–364. [DOI] [PubMed] [Google Scholar]
- 35.Kechter A, Amaro H, Black DS. Reporting of Treatment Fidelity in Mindfulness-Based Intervention Trials: A Review and New Tool using NIH Behavior Change Consortium Guidelines. Mindfulness (N Y). 2019;10(2):215–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chawla N, Collin S, Bowen S, et al. The mindfulness-based relapse prevention adherence and competence scale: development, interrater reliability, and validity. Psychother Res. 2010;20(4):388–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. [DOI] [PubMed] [Google Scholar]
- 38.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 39.Simons JS, Gaher RM. The Distress Tolerance Scale: Development and validation of a self-report measure. Motivation and Emotion. 2005;29(2):83–102. [Google Scholar]
- 40.Gratz KL, Roemer L. Multidimensional Assessment of Emotion Regulation and Dysregulation: Development, Factor Structure, and Initial Validation of the Difficulties in Emotion Regulation Scale. J Psychopathol Behav. 2004;26(1):41–54. [Google Scholar]
- 41.Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour research and therapy. 1995;33(3):335–343. [DOI] [PubMed] [Google Scholar]
- 42.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54(6):1063–1070. [DOI] [PubMed] [Google Scholar]
- 43.Flannery BA, Volpicelli JR, Pettinati HM. Psychometric properties of the Penn Alcohol Craving Scale. Alcohol Clin Exp Res. 1999;23(8):1289–1295. [PubMed] [Google Scholar]
- 44.Azuero A A note on the magnitude of hazard ratios. Cancer. 2016;122(8):1298–1299. [DOI] [PubMed] [Google Scholar]
- 45.Greenfield SF, Brooks AJ, Gordon SM, et al. Substance abuse treatment entry, retention, and outcome in women: a review of the literature. Drug Alcohol Depend. 2007;86(1):1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shorey RC, Elmquist J, Gawrysiak MJ, et al. A Randomized Controlled Trial of a Mindfulness and Acceptance Group Therapy for Residential Substance Use Patients. Subst Use Misuse. 2017;52(11):1400–1410. [DOI] [PMC free article] [PubMed] [Google Scholar]