Abstract
Objective:
Effectively responding to suicide risk among veterans involves further developing understanding of reactions to combat experiences, including life-threatening events, traumatic losses, and morally injurious experiences. An important determinant of whether stressors lead to poor mental health outcomes is the perception of meaning. The current study aimed to determine whether global meaning (i.e., general beliefs, goals, and sense of purpose in life) moderates the relationship between morally injurious experiences and suicide ideation among combat veterans.
Method:
This analysis examined 564 participants in the National Health and Resilience in Veterans Study, which surveyed a nationally representative sample of U.S. military veterans, who reported a history of deployment to a combat zone. Multivariable logistic regressions examined interactions between morally injurious experiences and global meaning as predictors of the likelihood of current suicide ideation.
Results:
There were significant interactions between global meaning and two morally injurious experience subtypes—transgressions by others and betrayal experiences. Higher global meaning was associated with significantly lower likelihood of experiencing suicide ideation at higher levels of transgression by others and betrayal experiences.
Conclusions:
Veterans who report higher levels of morally injurious experiences involving transgressions by others and betrayal experiences in the presence of higher levels of global meaning are significantly less likely to experience suicide ideation. Continued research is needed to determine whether interventions aimed at cultivating global meaning may help mitigate suicide risk in combat veterans with high exposure to certain potentially morally injurious experiences.
Keywords: moral injury, meaning, suicide, veterans, military
INTRODUCTION
Suicide is currently the tenth leading causing of death in the United States, and veterans are 21% more likely to die by suicide compared to civilian adults after adjusting for age and gender (Department of Veterans Affairs, 2016). One avenue to effectively responding to suicide risk among veterans involves further developing our understanding of reactions to military-related stressors, including combat exposure, life-threatening events, traumatic losses, and moral injury (Litz, Lebowitz, Gray, & Nash, 2017; Stein et al., 2012; Wisco et al., 2017). Moral injury—the distressing psychological experience of having violated one’s personal moral code—is receiving increased attention as a potential psychological mechanism for increased suicide risk among veterans and military personnel. Reasons for the increased attention include that moral injury involves psychological features (e.g., shame, low self-worth) that are common among individuals who think about suicide; these features—as opposed to the presence of stressors—are amenable to behavioral intervention; and both moral injury and suicidal thinking involve the psychological process of meaning-making, suggesting the possibility of common intervention strategies.
Military service, because of the nature of war (i.e., adversarial, violent, and potentially morally ambiguous) and potential conflicts between the rules one is expected to follow as a civilian versus as a service member, increases risk for exposure to potentially morally injurious experiences (PMIEs), which are acts (or instances of inaction) that commonly violate individuals’ moral codes and beliefs about right and wrong Litz et al., 2009; Molendijk, 2018). Research suggests that there are three types of PMIEs that can be encountered by military personnel—transgressions by self (e.g., killing a child), transgressions by others (e.g., witnessing torture committed by others), and betrayal experiences (e.g., perceived failures by leadership or fellow service members; Currier et al., 2015; Held et al., 2018; Litz et al., 2009; Nash et al., 2013)Nash et al., 2013; Bryan et al., 2016). A previous study using the dataset analyzed in the current study found that 10.8 to 25.5% of a nationally representative sample of U.S. veterans deployed to combat zones during service were exposed to PMIEs (Wisco et al., 2017). These events are labelled as potentially morally injurious because, just as not all individuals who experience life-threatening traumas develop Post-Traumatic Stress Disorder (PTSD), not all individuals exposed to PMIEs will develop moral injuries. Given that individuals vary in how they define morality, experiences that cause moral injury in one soldier may not cause moral injury in another.
For those who do experience moral injury, many features of this experience—guilt, shame, anger, loss of meaning, loss of trust, social isolation, difficulty with forgiveness, anhedonia, substance abuse, and self-harm—are also associated with risk for suicide ideation and behavior (Bryan et al., 2018; Jinkerson, 2016; Litz et al., 2009). Thus it is not surprising that moral injury is associated with increased risk for adverse mental health outcomes including PTSD, depression, generalized anxiety disorder, substance use disorders, suicide ideation, and suicide attempts (Bryan, Bryan, Morrow, Etienne, & Ray-Sannerud, 2014; Bryan et al., 2018; Corona, Wisco, Gamble, Pietrzak, & Van Orden, 2018; Currier, Holland, & Malott, 2015; Held et al., 2018; Wisco et al., 2017). Higher levels of meaning and purpose in life are associated with decreased odds of making a suicide attempt in one’s life, less severe suicide ideation, and decreases in suicide ideation severity over time (Braden, Overholser, Fisher, & Ridley, 2015; Bryan et al., 2013; Heisel & Flett, 2016; Kleiman & Beaver, 2013). A previously published paper on the dataset used in the current manuscript found that greater scores on a measure of morally injurious experiences was associated with suicide ideation in the prior two weeks, but the only sub-type of PMIEs that was associated with suicide ideation independent of the other sub-types was transgressions by self (and not transgressions by others or betrayal experiences; Wisco et al., 2017).
Individuals differ in how they interpret and make meaning around stressors and traumas. A key factor in determining whether potentially morally injurious experiences cause distress and impairment is how a given individual makes sense of his/her experiences and what perceived moral violations mean to the individual. Currier and colleagues (Currier et al., 2015) found that veterans exposed to PMIEs were at elevated risk for suicidal behavior when they reported difficulties making meaning regarding their experience with PMIEs, as assessed by the Integration of Stressful Life Events Scale (e.g., “I have difficulty integrating this event into my understanding of the world”). This finding underscores the central role of beliefs and meaning attributed to actions and events in the context of moral injury. This finding also raises the possibility that the ability to hold onto a sense of purpose and meaning in life more globally (i.e., outside the context of a specific stressor) could also provide protection against suicide risk for Veterans exposed to PMIEs.
In support of this hypothesis, previous studies have found that meaning and purpose in life protects against suicide risk among veterans and military personnel with PTSD (Kopacz, Currier, Drescher, & Pigeon, 2016; Pietrzak, et al., 2010). However, it is not known whether global purpose in life moderates the association between morally injurious experiences—rather than fear-based traumas—and suicide risk. This question is important to address for at least two reasons. First, fear-based traumas and morally-injurious experiences do not necessarily lead to the same type of problematic beliefs or interpretations and it is possible that beliefs about one’s self-worth or the worth of others that are commonly disrupted in moral injury are more pernicious regarding suicide risk and less amenable to modification by global meaning or purpose. If, however, the link between morally injurious experiences and suicide risk is influenced by global meaning, additional therapeutic strategies could be used to reduce suicide risk by fostering global purpose in life independent of making therapeutic progress on reducing distress related to moral injury.
To address this gap in the literature, we aimed to answer this question using a nationally representative sample of U.S. veterans deployed to a combat zone during their military service. We hypothesized that global meaning would moderate the association between morally injurious experiences and suicide risk. Furthermore, because different types of morally injurious experiences may affect individuals differently, an exploratory aim of the current study is to test this hypothesis using different subtypes of moral injury (i.e., based on transgressions by others, transgressions by self, and experiences of betrayal; Bryan et al., 2016; Nash et al., 2013).
METHOD
Participants
Participants were U.S. military veterans who participated in the National Health and Resilience in Veterans Study (NHRVS) and reported a history of deployment to a combat or war zone. This sample was recruited between September and October 2013 from a research panel that covered approximately 97% of U.S. households. The panel was developed by GfK Knowledge Networks, Inc. (Menlo Park, CA, USA) utilizing a sampling procedure that included households with or without internet access, listed and unlisted phone numbers, as well as households that were telephone, non-telephone, and cell-phone-only. A random sample of 2,273 U.S. military veterans enrolled in this panel was identified, and those included were sent a screening survey to confirm eligibility (i.e., their veteran status). Of these, 1,606 veterans (70.5%) completed the screening survey, and 1,484 eligible screening respondents (92.6%) subsequently completed a confidential online survey as participants in the NHRVS. Of the 1,484 participants, 564 (38.3%) reported deployment to a combat zone during service and were included in the current analyses. There was a wide range of time between most recent combat deployment and study participation, with an average of 34 years (range 0–72). Approval of study procedures was provided by the Human Subjects Subcommittee of the Veterans Affairs (VA) Connecticut Healthcare System and the VA Office of Research and Development. All study participants provided informed consent. Additional details about the sampling strategy and recruitment can be found elsewhere (Wisco et al., 2016).
Assessments
Participants completed a battery of self-report questionnaires assessing sociodemographic characteristics, military service characteristics, medical and psychiatric symptomatology, lifestyle, personality, quality of life, and resilience. The following measures from the larger battery were used in the analyses described in this manuscript.
The Combat Exposure Scale (CES; Keane et al., 1989) assessed frequency of various combat experiences during deployment. Number of lifetime traumatic experiences was assessed using the Trauma History Screen (THS; Carlson et al., 2011). The PTSD Checklist for DSM-5 (PCL-5; α=.96) was used to assess severity of PTSD symptoms as defined by DSM-5 within the past month (Blevins, Weathers, Davis, Witte, & Domino, 2015; Bovin et al., 2016). We selected a conservative cut-score of 38 on the PCL-5 as indicative of probable PTSD (Hoge, Riviere, Wilk, Herrell, & Weathers, 2014; Wisco et al., 2016). Depressive symptoms within the past two weeks were assessed using the Patient Health Questionnaire-2 (PHQ-2; α=.92; Kroenke, Spitzer, & Williams, 2003). A score of 3 or higher on the PHQ-2 indicates a likely depressive disorder (Löwe, Kroenke, & Gräfe, 2005). The Alcohol Use Disorders Identification Test (AUDIT; α=.80; Saunders, Aasland, Babor, de, & Grant, 1993) assessed alcohol use within the past year. An AUDIT score of 8 or higher indicates likely hazardous or harmful alcohol use (Saunders et al., 1993).
Item 9 of the Patient Health Questionnaire-9 (PHQ-9; Kroenke & Spitzer, 2002) was used to assess current suicide ideation (i.e., within the past two weeks). In the NHRVS, this question was divided into two questions: one asking about passive suicide ideation (i.e., “thoughts that you might be better off dead”), and the other asking about active suicide ideation (i.e., “thoughts of hurting yourself in some way”; Thompson, Henkel, & Coyne, 2004). Responses of “several days,” “more than half the days,” and “nearly every day” to either question were considered positive for suicide ideation; responses of “not at all” on both questions were considered negative.
The Moral Injury Events Scale (MIES; α=.88; Nash et al., 2013) is a 9-item measure that assesses exposure and reaction to events during military service that violated one’s moral code. The MIES includes three subscales (i.e., transgressions by others, transgressions by self, and betrayal experiences; αs=.87, .93, and .74, respectively; Bryan et al., 2016). Examples of items include, “I am troubled by having witnessed others’ immoral acts” (transgression by others subscale), “I am troubled by having acted in ways that violated my own morals or values” (transgressions by self subscale), and “I feel betrayed by leaders who I once trusted” (betrayal experiences subscale). Respondents rate their agreement with each statement on a Likert scale ranging from 1 (“strongly disagree”) to 6 (“strongly agree”), and items are summed to give subscale and total MIES scores.
The Purpose in Life Test-Short Form (PIL-SF; α=.87; Schulenberg, Schnetzer, & Buchanan, 2011) is a 4-item global meaning measure that asks respondents to rate the presence of life goals, their sense of life being meaningful, the extent to which they believe their life goals have been achieved, and their sense of purpose in life. Scores on the PIL-SF range from 4 to 28, with higher scores indicating higher levels of global meaning.
Data Analysis
Four multivariable binary logistic regressions were conducted using the logit command in Stata version 15. The models included interactions between continuous, mean-centered scores of moral injury and global meaning as predictors of the likelihood of current suicide ideation. One regression was conducted using the interaction between MIES total score and global meaning, and included the main effects of both variables. The remaining three each used one of the three MIES subscales in an interaction with global meaning, and included the main effects of global meaning as well as all three MIES subscales. Given that including interactions affects interpretation of coefficients for the model’s main effects, we focus our interpretation on coefficients for the interactions only.
All models were also adjusted for relevant covariates including demographics (i.e., age, gender, race/ethnicity, education, employment status, income), combat exposure, PTSD symptoms, depressive symptoms, alcohol use, and number of lifetime traumas. To enhance the generalizability of findings, analyses were weighted utilizing poststratification weights, computed by GfK statisticians, which were based on sociodemographic characteristics of U.S. veterans at the time the NHRVS survey was fielded; these characteristics included age, gender, education, race/ethnicity, and geography (i.e., Census region and metropolitan area).
Significant interactions were further examined by plotting the association between moral injury and the likelihood of current suicide ideation at different levels of global meaning (i.e., simple slopes). Follow-up tests were then conducted to determine the magnitude and direction of these slopes, and whether they were significantly different from zero.
RESULTS
Participant characteristics are displayed in Table 1. Raw (i.e., unweighted) descriptive statistics are reported. The mean age of the sample was 62 years. Current suicide ideation (i.e., passive or active suicide ideation within the last two weeks) was endorsed by 11.9% of the sample (n=54). All inferential statistics are weighted using the poststratification weights described above.
Table:
Participant characteristics
| n1 | %2 | ||
|---|---|---|---|
| Male | 527 | 93.00 | |
| Female | 37 | 7.00 | |
| White | 461 | 76.19 | |
| Non-White | 103 | 23.81 | |
| Some College + | 483 | 70.17 | |
| No College | 81 | 29.83 | |
| Retired | 282 | 46.46 | |
| Working | 207 | 37.69 | |
| Unemployed | 75 | 15.84 | |
| $60k + | 302 | 48.08 | |
| < $60k | 262 | 51.92 | |
| No | 510 | 88.15 | |
| Yes | 54 | 11.85 | |
| M1 | SD1 | Range1 | |
| Age | 61.71 | 15.60 | 20–92 |
| Lifetime Traumas (#) | 4.01 | 3.02 | 0–15 |
| Combat Exposure Scale (CES) Score | 10.81 | 10.84 | 0–41 |
| PCL-5 Score | 9.68 | 14.38 | 0–80 |
| PHQ-2 Score | 0.67 | 1.39 | 0–6 |
| AUDIT Score | 3.43 | 4.24 | 0–32 |
| Purpose in Life Test (PIL-SF) Score | 21.52 | 4.98 | 4–28 |
| Moral Injury Events Scale (MIES) Score (9 items) | 18.39 | 9.51 | 9–54 |
| MIES Transgressions-Other (2 items) | 5.11 | 3.15 | 2–12 |
| MIES Transgressions-Self (4 items) | 6.72 | 4.41 | 4–24 |
| MIES Betrayal Experiences (3 items) | 6.56 | 3.93 | 3–18 |
Raw (i.e., unweighted)
Weighted using the poststratification weights described in the manuscript
There were significant interactions between global meaning and transgressions by others (b=−0.04; z= −2.72; p= .006) as well as global meaning and betrayal experiences (b=− 0.03; z= −2.30; p= .021). However, the interaction between global meaning and MIES total score was not significant (b = −0.01; z = −1.86; p= .063), nor was the interaction between global meaning and transgressions by self (b = −0.003; z= −0.31; p= .755). This suggests that global meaning moderates the association between suicide risk and scores of transgressions by others and betrayal experiences, but does not moderate the association between suicide risk and scores of transgressions by self.
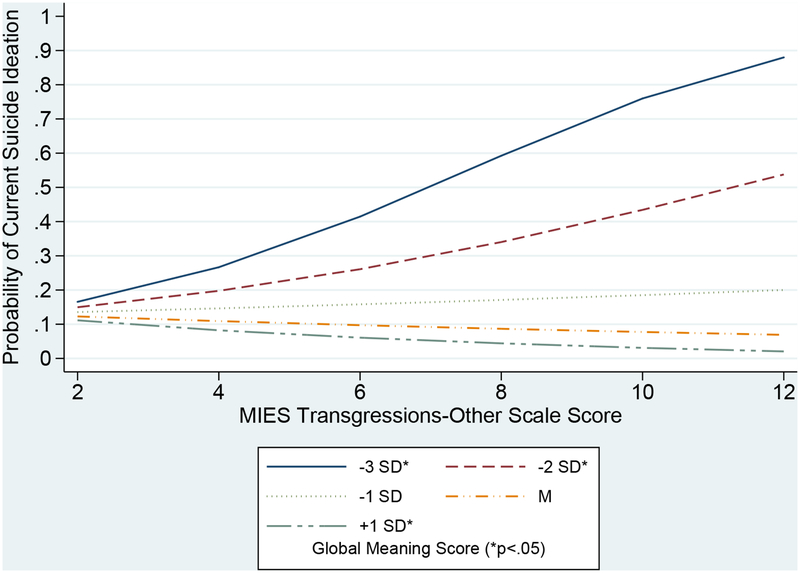
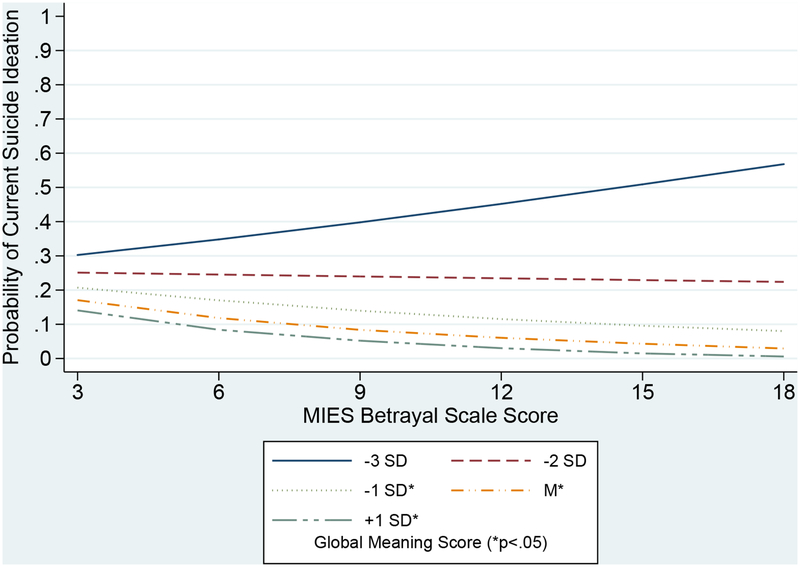
As shown in Figure 1, tests of simple slopes revealed that the relationship between transgressions by others and suicide ideation was statistically significant at both low (i.e., two and three standard deviations below the mean) and high (i.e., one standard deviation above the mean) levels of global meaning. Furthermore, these slopes decreased as global meaning increased from −3SD to −2SD to +1SD (i.e., 0.48, 0.28, and −0.33, respectively). Similarly, Figure 2 illustrates that the relationship between betrayal experiences and suicide ideation was statistically significant at higher levels of global meaning (i.e., −1SD, M, +1SD). Again, these slopes decreased as global meaning increased from −1SD to M to +1SD (i.e., −0.15, −0.28, and −0.41, respectively). These results indicate that higher global meaning is associated with significantly lower likelihood of experiencing suicide ideation at higher levels of transgression by others and betrayal experiences. Furthermore, lower global meaning is associated with significantly higher likelihood of experiencing suicide ideation at higher levels of transgression by others.
Figure 1:
Suicide ideation as a function of transgressions by others and global meaning
Figure 2:
Suicide ideation as a function of betrayal and global meaning
DISCUSSION
In the current study, we examined whether global meaning (i.e., the presence of life goals, one’s sense of life being meaningful, the extent to which one believes their life goals have been realized, and one’s sense of purpose in life) moderated the relationship between morally injurious experiences and suicide ideation in a nationally representative sample of U.S. combat veterans. Our hypothesis that global meaning would moderate the relationship between moral injurious experiences and suicide ideation was partially supported. When analyzing the total score on the moral injury measure used in the current study, global meaning did not significantly moderate the relationship between morally injurious experiences and the likelihood of current suicide ideation. Global meaning also did not significantly moderate the relationship between the likelihood of current suicide ideation and one moral injury subtype—transgressions by self. However, higher global meaning was associated with significantly lower likelihood of current suicide ideation at higher levels of transgressions by others and betrayal experiences. Furthermore, lower global meaning was associated with significantly higher likelihood of current suicide ideation at higher levels of transgressions by others.
These results align with previous research indicating that higher global meaning is associated with less severe suicide ideation among military personnel (Bryan et al., 2013), and build upon previous work examining the role of meaning in the relationship between moral injury and suicide risk among veterans (Currier et al., 2015). Past work has examined the extent to which adaptively making meaning out of specific events (i.e., situational meaning) determines whether exposure to potentially morally injurious experiences is associated with increased suicide risk. The current findings indicate that global meaning (i.e., general meaning in life that is not necessarily related to interpreting specific events) may also serve a protective function for veterans reporting certain types of moral injury regarding suicide ideation. This suggests a potential role for global purpose and meaning as intervention targets to reduce suicide risk for veterans who experienced morally injurious experiences of betrayal and transgressions by others: in addition to addressing the experience of moral injury directly, interventions could reduce suicide risk by increasing a protective factor – global meaning and purpose – offering an additional path to managing suicide risk.
An important caveat of the current findings is that global meaning did not moderate the association between transgressions by self and suicide ideation. This finding suggests that transgressions by self may represent an especially pernicious type of moral injury that is unaffected by global meaning. This is consistent with findings indicating that transgressions by self are associated with significantly more severe suicide ideation than either transgressions by others or betrayal experiences (Bryan et al., 2014). Further, a previous study using a sample of military personnel found that transgressions by self was the only MIES subscale significantly associated with increased hopelessness, which is a robust risk factor for suicide ideation (Bryan et al., 2016; Qiu, Klonsky, & Klein, 2017).
Important limitations of the current study are the cross-sectional nature of the data and the exclusion of suicide attempt as an outcome due to low statistical power. Future studies using longitudinal data would enable the examination of how the relationship among moral injury, global meaning, and suicide risk changes over time. Furthermore, because suicide attempt history is a robust predictor of death by suicide (Bostwick, Pabbati, Geske, & McKean, 2016), the inclusion of this outcome would strengthen future studies of the effect of global meaning on suicide risk among veterans reporting moral injury. An additional limitation points to an avenue for future study: our study did not examine whether the moderation effect we described is unique (or specific to) suicide ideation or whether purpose in life might function similarly with regards to the association between moral injurious experiences and other indicators of psychological distress and suicide risk. Similarly, future research seeking to further define the boundaries of the construct of moral injury could compare our findings regarding PMIEs to other types of stressors commonly experienced in military service. An additional direction for future research is continuing to refine understanding of different types or forms of morally injurious experiences. We examined three sub-types of PMIEs in this study, consistent with prior analyses of this dataset; however, given that measurement of moral injury continues to evolve and that different types of moral injury may have different associations with health outcomes, it will be important to refine measurement of these experiences and evaluate whether different psychological mechanisms are involved in the association with health outcomes, as this could have clinical implications. Finally, the average age of our sample was 62 years and was not a treatment-seeking sample; thus findings may not generalize to younger veterans and those seeking treatment for military stressors.
Notwithstanding these limitations, notable strengths of this study include the use of robust models that incorporate continuous measures and relevant covariates, significant effects despite the low rate of endorsement of the outcome variable (i.e., current suicide ideation), and the examination of an emerging topic related to suicide risk in a nationally representative sample of U.S. combat veterans. Collectively, our results indicate that U.S. combat veterans who report higher levels of morally injurious experiences of transgressions by others and betrayal experiences are significantly less likely to experience suicide ideation in the presence of higher levels of global meaning, and that veterans who report higher levels of transgressions by others are significantly more likely to experience suicide ideation in the presence of lower levels of global meaning. Continued research using longitudinal designs and additional suicide-related outcomes (e.g., attempts) is needed to definitively determine the effect of global meaning on the relationship between moral injury and suicide risk among veterans, and whether the study of interventions aimed at cultivating goals, purpose, and meaning in life (e.g., logotherapy, volunteering; Held et al., 2018; Smith, 2012; Southwick et al., 2006) may help mitigate suicide risk in combat veterans with exposure to morally injurious experiences.
Clinical Impact Statement.
The current study provides evidence that having a greater sense of global meaning in life (i.e., general beliefs, goals, and sense of purpose in life) is associated with lower likelihood of reporting suicide ideation among U.S. combat veterans with exposure to morally injurious experiences involving witnessing transgressions by others and betrayal. This information may be of use to those who seek to further understand experiences that place combat veterans at increased risk for suicide, and to develop interventions aimed at reducing suicide risk in this population.
Acknowledgments
The National Health and Resilience in Veterans Study is supported by the U.S. Department of Veterans Affairs National Center for Posttraumatic Stress Disorder. Preparation of this manuscript was supported by the Department of Veterans Affairs Office of Academic Affiliations Advanced Fellowship Program in Mental Illness Research and Treatment, and by the VISN 2 Center of Excellence for Suicide Prevention at the Canandaigua Veterans Affairs Medical Center. The views expressed in this article are those of the authors, and do not reflect the official policy of the Department of Veterans Affairs or the United States Government.
References
- Blevins CA, Weathers FW, Davis MT, Witte TK, & Domino JL (2015). The posttraumatic stress disorder checklist for DSM 5 (PCL 5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. doi: 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- Bostwick JM, Pabbati C, Geske JR, & McKean AJ (2016). Suicide attempt as a risk factor for completed suicide: Even more lethal than we knew. American Journal of Psychiatry, 173(11), 1094–1100. doi: 10.1176/appi.ajp.2016.15070854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders–fifth edition (PCL-5) in veterans. Psychological Assessment, 28(11), 1379–1391. doi: 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Braden A, Overholser J, Fisher L, & Ridley J (2015). Life meaning is associated with suicidal ideation among depressed veterans. Death Studies, 39(1), 24–29. doi: 10.1080/07481187.2013.871604 [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Elder WB, McNaughton-Cassill M, Osman A, Hernandez AM, & Allison S (2013). Meaning in life, emotional distress, suicidal ideation, and life functioning in an active duty military sample. The Journal of Positive Psychology, 8(5), 444–452. doi: 10.1080/17439760.2013.823557 [DOI] [Google Scholar]
- Bryan AO, Bryan CJ, Morrow CE, Etienne N, & Ray-Sannerud B (2014). Moral injury, suicidal ideation, and suicide attempts in a military sample. Traumatology, 20(3), 154–160. doi: 10.1037/h0099852 [DOI] [Google Scholar]
- Bryan CJ, Bryan AO, Anestis MD, Anestis JC, Green BA, Etienne N,…Ray-Sannerud B (2016). Measuring moral injury: Psychometric properties of the moral injury events scale in two military samples. Assessment, 23(5), 557–570. doi: 10.1177/1073191115590855 [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Bryan AO, Roberge E, Leifker FR, & Rozek DC (2018). Moral injury, posttraumatic stress disorder, and suicidal behavior among national guard personnel. Psychological Trauma, 10(1), 33–45. doi: 10.1037/tra0000290 [DOI] [PubMed] [Google Scholar]
- Carlson EB, Smith SR, Palmieri PA, Dalenberg C, Ruzek JI, Kimerling R,…Spain DA (2011). Development and validation of a brief self-report measure of trauma exposure: The trauma history screen. Psychological Assessment, 23(2), 463–477. doi: 10.1037/a0022294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corona CD, Wisco B, Gamble S, Pietrzak R, & Van Orden K (2018, April). Moral injury, substance abuse, and suicide ideation among veterans. Poster session presented at the 51st Annual Conference of the American Association of Suicidology, Washington, DC. [Google Scholar]
- Currier JM, Holland JM, & Malott J (2015). Moral injury, meaning making, and mental health in returning veterans. Journal of Clinical Psychology, 71(3), 229–240. doi: 10.1002/jclp.22134 [DOI] [PubMed] [Google Scholar]
- Department of Veterans Affairs. (2015). Post-deployment surveillance report (Vol. 1, No. 1). Washington, DC: Epidemiology Program. [Google Scholar]
- Department of Veterans Affairs. (2016). Suicide among veterans and other Americans, 2001–2014. Washington, DC: Office of Suicide Prevention. [Google Scholar]
- Drescher KD, Foy DW, Kelly C, Leshner A, Schutz K, & Litz B (2011). An exploration of the viability and usefulness of the construct of moral injury in war veterans. Traumatology, 17(1), 8–13. doi: 10.1177/1534765610395615 [DOI] [Google Scholar]
- Fontana A, & Rosenheck R (2005). The role of loss of meaning in the pursuit of treatment for posttraumatic stress disorder. Journal of Traumatic Stress, 18(2), 133–136. doi: 10.1002/jts.20014 [DOI] [PubMed] [Google Scholar]
- Heisel MJ, & Flett GL (2016). Does recognition of meaning in life confer resiliency to suicide ideation among community-residing older adults? A longitudinal investigation. The American Journal of Geriatric Psychiatry, 24(6), 455–466. doi: 10.1016/j.jagp.2015.08.007 [DOI] [PubMed] [Google Scholar]
- Held P, Klassen BJ, Hall JM, Friese TR, Bertsch-Gout MM, Zalta AK, & Pollack MH (2018). “I knew it was wrong the moment I got the order”: A narrative thematic analysis of moral injury in combat veterans. Psychological Trauma. doi: 10.1037/tra0000364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge CW, Riviere LA, Wilk JE, Herrell RK, & Weathers FW (2014). The prevalence of post-traumatic stress disorder (PTSD) in US combat soldiers: A head-to-head comparison of DSM-5 versus DSM-IV-TR symptom criteria with the PTSD checklist. The Lancet Psychiatry, 1(4), 269–277. doi: 10.1016/S2215-0366(14)70235-4 [DOI] [PubMed] [Google Scholar]
- Jinkerson JD (2016). Defining and assessing moral injury: A syndrome perspective. Traumatology, 22(2), 122. doi: 10.1037/trm0000069 [DOI] [Google Scholar]
- Keane TM, Fairbank JA, Caddell JM, Zimering RT, Taylor KL, & Mora CA (1989). Clinical evaluation of a measure to assess combat exposure. Psychological Assessment, 1(1), 53–55. doi: 10.1037/1040-3590.1.1.53 [DOI] [Google Scholar]
- Kleiman EM, & Beaver JK (2013). A meaningful life is worth living: Meaning in life as a suicide resiliency factor. Psychiatry Research, 210(3), 934–939. doi: 10.1016/j.psychres.2013.08.002 [DOI] [PubMed] [Google Scholar]
- Kopacz MS, Currier JM, Drescher KD, & Pigeon WR (2016). Suicidal behavior and spiritual functioning in a sample of Veterans diagnosed with PTSD. J Inj Violence Res, 8(1), 6–14. doi: 10.5249/jivr.v8i1.728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, & Spitzer RL (2002). The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals, 32(9), 509–515. doi: 10.3928/0048-5713-20020901-06 [DOI] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JBW (2003). The patient health questionnaire-2: Validity of a two-item depression screener. Medical Care, 41(11), 1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C [DOI] [PubMed] [Google Scholar]
- Larner B, & Blow A (2011). A model of meaning-making coping and growth in combat veterans. Review of General Psychology, 15(3), 187–197. doi: 10.1037/a0024810 [DOI] [Google Scholar]
- Litz BT, Lebowitz L, Gray MJ, & Nash WP (2017). Adaptive disclosure: A new treatment for military trauma, loss, and moral injury. New York, NY: Guilford Press. [Google Scholar]
- Litz BT, Stein N, Delaney E, Lebowitz L, Nash WP, Silva C, & Maguen S (2009). Moral injury and moral repair in war veterans: A preliminary model and intervention strategy. Clinical Psychology Review, 29(8), 695–706. doi: 10.1016/j.cpr.2009.07.003 [DOI] [PubMed] [Google Scholar]
- Löwe B, Kroenke K, & Gräfe K (2005). Detecting and monitoring depression with a two-item questionnaire (PHQ-2). Journal of Psychosomatic Research, 58(2), 163–171. doi: 10.1016/j.jpsychores.2004.09.006 [DOI] [PubMed] [Google Scholar]
- Molendijk T (2018). Toward an interdisciplinary conceptualization of moral injury: From unequivocal guilt and anger to moral conflict and disorientation. New Ideas in Psychology, 51, 1–8. doi: 10.1016/j.newideapsych.2018.04.006 [DOI] [Google Scholar]
- Nash WP, Marino Carper TL, Mills MA, Au T, Goldsmith A, & Litz BT (2013). Psychometric evaluation of the moral injury events scale. Military Medicine, 178(6), 646–652. doi: 10.7205/MILMED-D-13-00017 [DOI] [PubMed] [Google Scholar]
- Owens GP, Steger MF, Whitesell AA, & Herrera CJ (2009). Posttraumatic stress disorder, guilt, depression, and meaning in life among military veterans. Journal of Traumatic Stress, 22(6), 654–657. doi: 10.1002/jts.20460 [DOI] [PubMed] [Google Scholar]
- Panagioti M, Gooding P, & Tarrier N (2009). Post-traumatic stress disorder and suicidal behavior: A narrative review. Clinical Psychology Review, 29(6), 471–482. doi: 10.1016/j.cpr.2009.05.001 [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein MB, Malley JC, Rivers AJ, Johnson DC, & Southwick SM (2010). risk and protective factors associated with suicidal ideation in veterans of Operations Enduring Freedom and Iraqi Freedom. Journal of Affective Disorders, 123, 102–107. doi: 10.1016/j.jad.2009.08.001 [DOI] [PubMed] [Google Scholar]
- Pompili M, Sher L, Serafini G, Forte A, Innamorati M, Dominici G,…Girardi P (2013). Posttraumatic stress disorder and suicide risk among veterans: A literature review. The Journal of Nervous and Mental Disease, 201(9), 802–812. doi: 10.1097/NMD.0b013e3182a21458 [DOI] [PubMed] [Google Scholar]
- Qiu T, Klonsky ED, & Klein DN (2017). Hopelessness predicts suicide ideation but not attempts: A 10-year longitudinal study. Suicide and Life-Threatening Behavior, 47(6), 718–722. doi: 10.1111/sltb.12328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de l. F., & Grant M (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction, 88(6), 791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x [DOI] [PubMed] [Google Scholar]
- Schulenberg SE, Schnetzer LW, & Buchanan EM (2011). The purpose in life test-short form: Development and psychometric support. Journal of Happiness Studies, 12(5), 861–876. doi: 10.1007/s10902-010-9231-9 [DOI] [Google Scholar]
- Smith A (2012, March). New and innovative applications of logotherapy for the treatment of posttraumatic stress disorder. Paper session presented at the 6th Annual Conference of the American Counseling Association, San Francisco, CA. [Google Scholar]
- Southwick SM, Gilmartin R, McDonough P, & Morrissey P (2006). Logotherapy as an adjunctive treatment for chronic combat-related PTSD: A meaning-based intervention. American Journal of Psychotherapy, 60(2), 161–174. doi: 10.1176/appi.psychotherapy.2006.60.2.161 [DOI] [PubMed] [Google Scholar]
- Steenkamp MM, Litz BT, Hoge CW, & Marmar CR (2015). Psychotherapy for military-related PTSD: A review of randomized clinical trials. Journal of the American Medical Association, 314(5), 489–500. doi: 10.1001/jama.2015.8370 [DOI] [PubMed] [Google Scholar]
- Stein NR, Mills MA, Arditte K, Mendoza C, Borah AM, Resick PA,…Strong Star Consortium. (2012). A scheme for categorizing traumatic military events. Behavior Modification, 36(6), 787–807. doi: 10.1177/0145445512446945 [DOI] [PubMed] [Google Scholar]
- Terhakopian A, Sinaii N, Engel CC, Schnurr PP, & Hoge CW (2008). Estimating population prevalence of posttraumatic stress disorder: An example using the PTSD checklist. Journal of Traumatic Stress, 21(3), 290–300. doi: 10.1002/jts.20341 [DOI] [PubMed] [Google Scholar]
- Thompson R, Henkel V, & Coyne JC (2004). Suicidal ideation in primary care: Ask a vague question, get a confusing answer. Psychosomatic Medicine, 66(3), 455–456. [DOI] [PubMed] [Google Scholar]
- Wisco BE, Marx BP, Miller MW, Wolf EJ, Mota NP, Krystal JH,…Pietrzak RH (2016). Probable posttraumatic stress disorder in the US veteran population according to DSM-5: Results from the national health and resilience in veterans study. The Journal of Clinical Psychiatry, 77(11), 1503–1510. doi: 10.4088/JCP.15m10188 [DOI] [PubMed] [Google Scholar]
- Wisco BE, Marx BP, May CL, Martini B, Krystal JH, Southwick SM, & Pietrzak RH (2017). Moral injury in U.S. combat veterans: Results from the national health and resilience in veterans study. Depression and Anxiety, 34(4), 340–347. doi: 10.1002/da.22614 [DOI] [PubMed] [Google Scholar]