Abstract
Objective:
Several researchers have argued that racism-related stressors play an important role in adverse cardiovascular outcomes among African-American women. However, studies have primarily focused on experiences of racism; thus, the role of expectations of racism is insufficiently understood. The current proof-of-concept study was designed to examine associations among expectations of racism, self-reported experiences of racism, and carotid intima-media thickness (IMT), a marker of cardiovascular risk, in African-American women.
Methods:
Participants were 52 healthy African-American women, aged 30-50 (Mean=40.8, sd=4.3). Expectations of racism were assessed with a modified version of the Race-Based Rejection Sensitivity Questionnaire, experiences of racism were assessed with the Schedule of Racist Events, and carotid IMT was measured using B-mode ultrasound.
Results:
In linear regression analyses adjusted for age, expectations of racism were associated with higher levels of carotid IMT (b=.04, s.e.=.014, p=.013), after adjusting for experiences of racism. Findings remained significant after additional adjustments for cardiovascular risk factors (b=.03, s.e.=.014, p=.032). Associations were not confounded by additional stressors, hostility, or negative affect (depressive symptoms).
Conclusions:
Independent of actual reports of racism, “expectations” of racism may be associated with increased cardiovascular risk in African-American women. Additionally, although experiences of discrimination were associated with depressive symptoms, expectations of racism were not, suggesting that other negative emotions likely play a role. Future studies are needed to replicate these results in larger samples, and to explore the psychological and physiological pathways through which expectations of racism might affect CVD risk across a range of populations.
Keywords: Atherosclerosis, Cardiovascular Disease, Depression, Racism, Social Determinants of Health, Stress, Psychological, Vigilance
Introduction
Cardiovascular Disease (CVD) is the number one killer of adult women in the United States (1). Among women, African-American women are disproportionately burdened by CVD morbidity and mortality. Recent data suggest that African-American women aged 35–44 have rates of CVD that are higher than those of African-American men, White men and White women (2). Socioeconomic and traditional clinical risk factors do not completely explain this excess risk (2, 3); thus there is a pressing need to identify non-traditional risk factors that might affect early CVD in African-American women.
Racism-related stressors have been proposed as one potential pathway through which race heightens risk of CVD among African-American women. Reviews and meta-analytic findings have documented consistent associations between reports of racism (and other forms of discriminatory treatment) and markers of CVD risk across a range of populations (4–6). This research has been important in establishing empirical linkages between exposure to racism/discrimination and cardiovascular risk; however, it has largely focused on reports of interpersonal experiences of racism and discrimination, which, across cohorts, tend to be relatively low (7–12). Further, because reports of interpersonal experiences only capture a specific component of racism-related stress, focusing on these experiences alone may actually underestimate the impact of racism-related stressors on cardiovascular health.
In contrast to experiences of racism, expectations of racism exist even in the absence of an actual event. Researchers have argued that expectations of racism are largely fueled by an awareness of racism (13, 14). Prior studies suggest that African-Americans possess a more accurate knowledge of racism-related occurrences in United States history than Whites (15) and report an awareness of negative stereotypes about their group (14). Coupled with vicarious exposure to racism through family members, friends and media coverage (16), this knowledge about racism may increase expectations of racism among African-American women even when personal exposure is low. Consequently, the threat of potential racism is the psychological stressor in this instance, independent of the experience of racism itself.
In a qualitative study assessing racism-related exposures among African-American women, Nuru-Jeter and colleagues (17) observed that: “Many participants reported thinking about their race or racism at least daily…[in] the form of conscious efforts to prepare themselves—through heightened awareness and altered behaviors—for situations where they were likely to face racist attitudes or behaviors.” This is consistent with arguments presented by Williams in 1994 (18), and further emphasized by Myers and colleagues in 2003 (13), which posit that expectations of racism represent a form of chronic vigilance that may contribute to poor health among African-Americans. Tasks requiring vigilance, or “alert, watchful observation of the external environment” (p383) (19) have been associated with increased cardiovascular reactivity; and concerns about general interpersonal mistreatment have also been linked to cardiovascular reactivity (20) as well as hypertension (21) and self-reported sleep (22). To date, however, there has been limited empirical research on vigilance around racial/ethnic discrimination per se and health, and almost no data in African-Americans.
Thus, the current “proof of concept” study was designed to examine the association between “expectations” of racism and carotid intima media thickness (IMT) in a small sample of healthy adult African-American women. Carotid IMT is a biomarker of CVD risk that has been linked to incident myocardial infarction and stroke in both clinic and community samples (23–25). Prior studies have documented associations between increased carotid IMT and psychosocial stressors (26–28), including self-reported experiences of racism (29) and overall unfair treatment (30). Across studies, carotid IMT is typically higher among African-Americans as compared to Whites (31, 32), and may therefore be an important target for prevention efforts to reduce black-white disparities in CVD.
We hypothesized that higher levels of expected racism would be associated with greater carotid IMT, and that this association would be independent of reports of actual racism. We also examined whether any observed associations were independent of potential confounders such as: 1) additional chronic stressors not directly due to race, and 2) known correlates of CVD risk such as hostility and negative emotions in the form of depressive symptoms. Finally, we explored the synergistic (interactive) effects of expectations of racism and experiences of racism on IMT, in order to determine whether the effects of expectations of racism on carotid atherosclerosis were most pronounced in women who reported higher levels of experienced racism.
Methods
Participants
Participants were 52 pre-menopausal African-American women aged 35–50, from a mid-sized city in the Northeastern United States. Women were recruited through community advertisements and flyers/pamphlets posted in area beauty supply shops, hair salons, restaurants, churches and community organizations. Interested participants were pre-screened by telephone to determine eligibility. In order to participate in the study, women had to self-identify as non-Hispanic African-American and be free of self-reported cardiovascular disease and most CVD equivalents, such as diabetes and clinical CVD (including a history of myocardial infarction, symptoms of angina, intermittent claudication, cerebral ischemia or revascularization). Additional exclusion criteria included: chronic illnesses known to influence atherosclerotic disease (e.g. Human Immuno-deficiency Virus, certain autoimmune diseases, renal disease and liver disease); treatment for psychiatric disorders (depression, anxiety); having received a mastectomy and/or hysterectomy; and current illicit drug use or alcohol abuse. Women who were pregnant, breastfeeding, postmenopausal, or taking oral contraceptives were also ineligible for participation.
Procedure
Based on self-reported menstrual cycle information obtained during the pre-screening interview, participants were scheduled for study visits during the post-ovulation luteal phase of their menstrual cycle (days 15–27 in a 28 day cycle), following a 12-hour fast. Women were asked to discontinue any vasoactive medication(s), caffeine ingestion and smoking for 24 hours prior to their visit. During their visit, participants completed a standard protocol that included measured height and weight, clinical tests (e.g. blood pressure) and B-mode ultrasound imaging of the carotid artery. Detailed information on demographic, psychosocial and behavioral characteristics was also collected, via interviewer-administered questionnaires. Participants were compensated $150 for their time, effort and potential lost wages. Study procedures were approved by the Human Investigation Committee at Yale University. All participants provided written, informed consent. Assessments were conducted at the University’s Hospital Research Unit between April 2009-May 2010.
Measures
Expectations of Racism were assessed with a modified version of the “expectations” subscale of the Race-Based-Rejection Sensitivity Questionnaire (14). The subscale inquires about expectations of racism across a variety of situations. As one example: “Imagine you have just finished shopping for new clothes, and you are leaving the store carrying several bags. It’s closing time, and several people are filing out of the store at once. Suddenly, the alarm begins to sound, and a security guard comes over to investigate.” Participants were then asked whether they “would expect that the guard might stop me because of my race/ethnicity”. Another item states: “Imagine that you and your friends are in a restaurant, trying to get the attention of your waitress. A lot of other people are trying to get her attention as well,” followed by a question asking participants if they: “…would expect that she might not attend to me right away because of my race/ethnicity”.
The subscale was originally designed to measure expectations of racism in African-American college students attending predominantly white universities (14) and consisted of 12 items, with good validity and test-retest reliability (14). Five items were dropped due to lack of applicability to a non-student population (e.g. items about grades and scholarships) or lack of current relevance (e.g. an item about using a payphone). Responses to the remaining 7 items were scored on a 6-point scale with higher scores indicative of greater expected racism. Responses were then averaged (total sum score divided by 7) to maintain the original distribution of the 1 to 6 point scale. The scale demonstrated good internal consistency in our sample (Cronbach’s alpha=.87).
The original Race-Based Rejection Sensitivity Questionnaire also included an “anxious/concerned” probe prior to asking about “expectations.” Thus, participants were asked how “anxious/concerned” they would be about experiencing racism in a specific instance (e.g. trying to get the attention of a waitress), followed immediately by a query of how much they would “expect” to experience racism in that setting. Our community-based sample of women found the two back-to-back probes with similar wording counterintuitive and confusing. Thus we dropped the anxious/concerned queries (these generated the most pushback), from the questionnaire in the initial stages of the study.
Experiences of Racism within the past 12 months were assessed by the 17-item Schedule of Racist Events (SRE) Recent (33). We used the “recent” scale in keeping with standard psychosocial stress paradigms, which capture negative life events that are fairly proximal to the outcome. Sample items include: “How many times have you been treated unfairly by people in service jobs (store clerks, waiters…) because you are Black?”), and “How many times have you been unfairly accused or suspected of doing something wrong (stealing, cheating) because you are Black?” Possible responses range from 1 to 5, with higher scores indicating greater exposure to racism. Scores were averaged (total sum score divided by 17) to retain the original 1 to 5 point scale. The SRE Recent demonstrated good internal consistency in the current sample (Cronbach’s alpha=.89).
Carotid Intima Media Thickness (IMT) was assessed non-invasively by a single ultrasonographer using a duplex ultrasound vascular imaging system connected to a 7 MHz linear array probe (Acuson Cypress™, Mountain View CA) with an imaging protocol adapted from guideline recommendations (34). Participants were studied in the supine position with the head laterally rotated 45 degrees to the left. B-mode ultrasound images of the far wall of the right common carotid artery were obtained 1 cm proximal to the carotid bulb for 3–5 cardiac cycles at anterior, posterior, and lateral angles and stored in Digital Imaging and Communication in Medicine (DICOM) format. IMT measurements (mm) were made at end-diastole with a previously validated computer-assisted edge detection image analysis system (Artery Measurement Systems, Gothenburg, Sweden) (35) by a single investigator blinded to clinical information. This software reports the mean value of 100 measurements along a 1 cm segment of the vessel. Using this software, the intraclass correlation coefficient for a single investigator is 0.97 with coefficient of variance of 3%. The average of the mean measurements across the different carotid artery imaging angles comprise the reported average IMT.
Demographics.
Age (in years), education (in years) and marital status were assessed for descriptive purposes via self-report.
Cardiovascular Risk Factors.
Blood Pressure measurements were obtained by a trained nurse and standardized for cuff size, position and rest period. Two blood pressure readings in the seated position were taken from the right arm of each participant and averaged for use in all analyses. Body Mass Index (BMI) was calculated as weight in kilograms divided by height in meters squared. BMI was categorized as normal, overweight and obese (36) for descriptive purposes, but was modeled continuously in all analyses.
Contextual Psychosocial Variables.
Measures of additional stressors, hostility, and depressive symptoms were also included as potential confounders (stressors, hostility) and/or mediators (depressive symptoms). Additional Stressors were assessed with the five-item chronic burden scale (37) designed to measure stressors that have a duration of six months or more such as: relationship difficulties; ongoing financial problems; or difficulties with a job/ability to work. Responses were scored as present/absent and summed across items, with higher scores indicating more chronic stressors. Hostility was assessed with the 27-item CHOST, derived from the Cook-Medley hostility scale (38). Items are asked in a True/False format, with one point assigned for each true response. Scores range from 0–27 with higher scores indicating greater hostility. Depressive Symptoms were assessed with the 21-item Beck Depression Inventory (BDI) (39). Scores range from 0–63, with higher total scores indicating more severe depression. All three scales have been widely used across community samples and have demonstrated good reliability and validity (29, 37).
Statistical Analyses
Descriptive statistics were used to characterize the study sample on demographics, racism variables, cardiovascular risk factors, IMT and additional psychological covariates. Five participants (9%) were missing data on the SRE (our measure of experiences of racism) due to a programming error. Although there are a number of highly sophisticated methods to account for missing data (40), because SRE scores were missing completely at random (MCAR), we ran all of our analyses without these women (which is considered appropriate under MCAR criteria but could result in too large of a standard error), and using mean substitution on the SRE (which could result in too small of a standard error) (41, 42). Our findings were almost identical using both methods; thus we chose the latter approach to allow for the inclusion of the most participants.
Correlation coefficients were used to examine associations between expectations of racism, experiences of racism, contextual psychosocial variables and IMT. Due to our relatively small sample size, in order to avoid over fitting our models we took a conservative approach to adding the contextual psychosocial variables; they were only considered to be potential confounders (i.e. third variables) or mediators and included in final models if they were associated with both the predictor and the outcome at p≤.05.
A series of multivariable linear regression models were conducted to examine the associations among expectations of racism, experiences of racism, and IMT. The initial, minimally adjusted model examined the main effect of expectations of racism on levels of IMT, after controlling for age and reports of racism. The second model added SBP and BMI as cardiovascular risk covariates, given their association with IMT in prior studies (43–45). A third model added any additional psychosocial covariates (potential confounders/mediators) meeting criteria for inclusion in the models. Following this first set of models, we then conducted a series of exploratory analyses in order to examine the expectations of racism by experiences of racism interaction, in both minimally and fully adjusted models.
Following this, we conducted a series of sensitivity analyses adjusting for education as a marker of socioeconomic status (SES). None of our primary models included this term, because several studies have found that African-Americans receive fairly limited health returns on education and other SES indicators (46, 47). Analyses with and without education produced similar results, thus this variable was not retained in final models. All analyses were conducted using SPSS.
Results
Participant Characteristics
Descriptive statistics for participant demographic, psychosocial and cardiovascular risk factor characteristics are presented in Table 1. Women ranged in age from 30–50, and were skewed toward the younger end of the distribution, with an average age of 41 (SD=4.31). Approximately 53 percent were married or living as married, 24.5 percent were never married and 20.8 percent were either separated or divorced. Participants were well educated, reporting a mean 15.7 years (SD=2.39) of education. On average, women had SBP and DBP levels in the normal range, although 15.1% (N=8) met criteria for hypertension based on the Seventh Joint National Committee (JNC7) guidelines (48). Participants were predominantly obese, with an average BMI of 30.64 (SD=5.98). Reports of expected racism were intermediate, with a mean score of 3.54 on a 6-point scale; however, reports of experiences of racism were skewed towards the lower end, with an average score of 1.68 on a 5-point scale (Table 1). Scores on the BDI were also skewed towards the low end of the distribution.
Table 1.
Sample Demographic, Psychosocial and Cardiovascular Risk Factor Characteristics
| Characteristic | All Participants (N=52) | ||
|---|---|---|---|
| Mean±SD or n,% | Range | Shapiro-Wilk Statistic |
|
| Age (years) | 40.9 ± 4.3 | 35-50 | .94* |
| Education (years) | 15.71 ± 2.34 | 12-21 | .94* |
| Expectations of Racism | 3.54 ± 1.29 | 1.43-6.00 | .95 |
| Experiences of Racism | 1.68 ± .57 | .29-3.65 | .92* |
| Systolic Blood Pressure, mm Hg | 124.95 ± 10.69 | 105-160 | .97 |
| Diastolic Blood Pressure, mm Hg | 81.27 ± 9.17 | 66-114 | .96 |
| Hypertension, n (%) | 8 (15.8) | ||
| Body Mass Index (kg/m2) | 30.64 ±5.99 | 19-51 | .95 |
| Normal weight, n (%) | 9 (17.0) | ||
| Overweight, n (%) | 12 (22.6) | ||
| Obese, n (%) | 31 (58.5) | ||
| Additional Chronic Stressors | 1.71 ±. 45 | 1.00-3.00 | .96 |
| Depressive Symptoms (BDI score) | 6.37 ± 5.79 | 0-34.00 | .78** |
| Hostility | 13.87 ± 3.81 | 4-21 | .97 |
Note: Values are mean ± SD or percentage.
p<.05
p<.001
Correlations Among Variables of Interest
As shown in Table 2, expectations of racism were significantly correlated with experiences of racism (r=.63, p<.001) and hostility (r=.43, p<.001), but were not significantly correlated with additional stressors (r=.23, p=.104) or depressive symptoms (r=.19, p=.178). Self-reported experiences of racism however, were significantly correlated with both additional stressors and depressive symptoms (both p-values<.001), as well as hostility. Other than expectations of racism, none of the psychological variables were significantly correlated with IMT (Table 2); thus none were considered to be potential confounders/mediators.
Table 2.
Correlations Among Study Variables
| Variable | Expectations of Racism |
Experiences of Racism |
Additional Stressors |
Hostility | Depressive Symptoms |
|---|---|---|---|---|---|
| Expectations of Racism | |||||
| Experiences of Racism | .61** | ||||
| Additional Stressors | .23 | .55** | |||
| Hostility | .43* | .31* | .28* | ||
| Depressive Symptoms | .19 | .44** | .53** | .36* | |
| IMT | .31* | .001 | −.12 | .13 | .02 |
Note:
p<.05,
p<.01
Associations Between Expectations of Racism and IMT
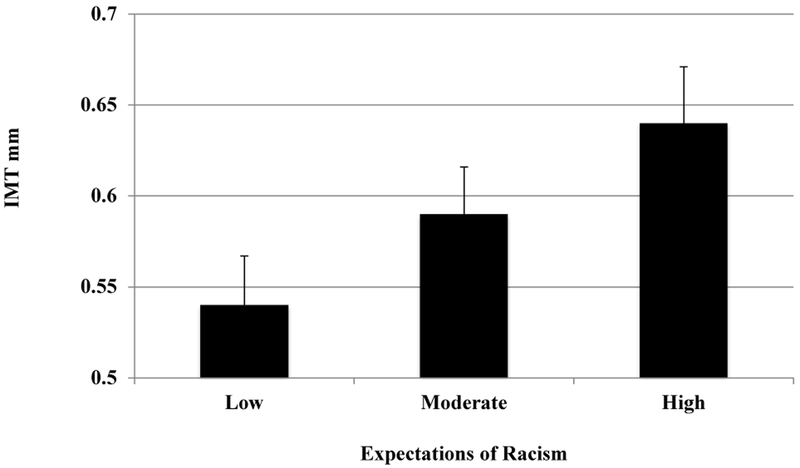
The crude association between expectations of racism and IMT is presented in a scatterplot in Figure 1. In linear regression analyses adjusting for age and self-reported racism, higher levels of expected racism were associated with a greater amount of carotid atherosclerosis (b=.04, s,e,=.014, p=.013). As shown in Figure 2 (with expectations of racism categorized for descriptive purposes), the relationship between expectations of racism and IMT was dose-response in nature, with each higher level of expected racism associated with a greater amount of carotid IMT, resulting in a 0.1mm difference between the lowest and highest tertiles. This association remained significant after further adjustment for BMI and SBP (b=.03, s,e,=.014, p=.032).
Figure 1.
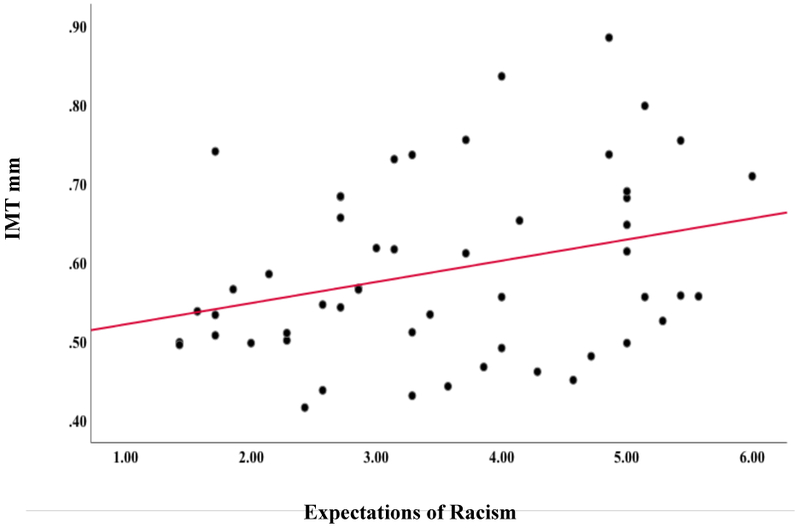
Scatterplot of the basic association between Expectations of Racism and IMT
Figure 2.
Expectations of Racism and Intima Media Thickening (IMT) in African-American Women
Note: Adjusted for age and self-reported experiences of racism. Expectations of racism were modeled continuously in analyses, but are categorized for graphical purposes.
Exploratory Analyses
We ran exploratory analyses to examine the synergistic effects of expectations of racism and experiences of racism on IMT. In linear regression analyses adjusted for age, experiences of racism and expectations of racism, the experiences of racism X expectations of racism interaction term was non-significant (p>.78), indicating that the effect of expectations of racism on IMT did not differ by level of reported racism.
Additionally, although hostility was not associated with IMT in bivariate analyses, due to its significant association with expectations of racism in our sample and linkages to CVD risk in prior studies (32, 49, 50), we also ran exploratory models adjusting for hostility. In linear regression models adjusting for age, experiences of racism and hostility, expectations of racism was significantly associated with carotid IMT (b=.04, p=.021). Fully adjusted models (data not shown), revealed similar results.
Discussion
To our knowledge, the current proof-of-concept study is the first to document an association between “expectations” of racism and a biomarker of cardiovascular risk in African-Americans. We examined associations among expectations of racism, self-reported experiences of racism, and carotid atherosclerosis in a community sample of healthy, pre-menopausal African-American women. As anticipated, expectations of racism were more commonly reported than experiences of racism, and findings revealed a significant, dose-response association between expectations of racism and carotid IMT that was independent of self-reported experiences of racism, and three major risk factors for atherosclerotic disease –age, SBP and BMI. We explored whether the effect of expectations of racism on IMT differed by reports of experiences of racism, but did not observe a significant expectations by experiences interaction. Thus, findings indicate that regardless of whether (or how often) an actual racist event occurs, an awareness about or expectation of racism may increase cardiovascular risk in African-American women. Additionally, our observed difference in carotid IMT between African-American women in the highest versus lowest tertile of expected racism (detailed in Figure 2) is of potential clinical significance, as a meta-analysis of past population based studies indicate a 10% increased risk of myocardial infarction and 13% increased risk of stroke for every 0.1 mm difference in carotid IMT, when adjusting for age, sex, and other vascular risk factors (25).
Results from the current study are consistent with a laboratory study that found that expectations of racism also affect physiological pathways that might ultimately lead to increased IMT (51). Sawyer and colleagues (51) randomized 54 Latina college students to one of two conditions: 1) evaluation by a white female colleague who endorsed prejudiced beliefs or 2) evaluation by a white female colleague who endorsed non-prejudiced beliefs. Physiological parameters were assessed as the participants awaited their interactions. Findings revealed that Latinas anticipating an encounter with prejudiced evaluators had significantly higher SBP, DBP and heart rates than Latina participants anticipating an interaction with a non-prejudiced evaluator (51). Thus, in keeping with our findings, Sawyer et al observed that expectations of discrimination alone were associated with physiological arousal, even in the absence of actual exposure to discrimination.
Our findings are also in line with those from other studies examining expectations of mistreatment for reasons not directly attributed to race (or other protected classes (52)). Hicken et al (21, 22) and Clark and colleagues (20) have found significant associations between a measure entitled “racism-related vigilance” and indices of CVD, such as sleep (22), hypertension (21) and large arterial elasticity (20). Yet despite the title, the measure used in those studies does not actually inquire about expectations of mistreatment due to “race” (sample item: “how often do you…try to prepare for possible insults from other people before leaving home?”); thus it is not directly comparable to the measure used in our study. This is an important distinction, because measures that assess mistreatment overall typically include exposure to non-racial discriminatory experiences (e.g. ageism, sexism, classism, weight discrimination), as well as unfair treatment more broadly. Given the salience around race in the United States, and the prominence of racism compared to other forms of interpersonal mistreatment for African-American women (53, 54), examining expectations about racism specifically may be particularly important for this group. However, without a direct test, it is difficult to fully determine the uniqueness of racism-related expectations versus anticipated threat about discrimination due to other factors. Nonetheless, taken together, results from prior studies on vigilance more broadly combined with the current findings provide additional support for the notion that “expectations” may have a significant impact on cardiovascular health.
The mechanisms underlying the observed association between expectations of racism and IMT require further exploration. It is noteworthy that while depressive symptoms (and additional chronic stressors) were associated with self-reported experiences of racism, they were not associated with expectations of racism. This further supports the argument that “expectations” of racism may be a conceptually distinct form of racism-related stress. Consequently, the psychological pathways through which expectations exert their impact on cardiovascular health may also differ. For example, experiences of racism have been strongly linked to depression and depressive symptoms (4, 55, 56), which may be one pathway through which these experiences “get under the skin” to affect CVD risk. Expectations on the other hand, may be more strongly associated with anxiety, and a prolonged state of cognitive activation and threat-related attentional bias (57) that is unrelated to depressive symptoms (58); which would represent a slightly different pathway.
Thus, in contrast to the active cognitive appraisal process proposed by some that might link experiences of discrimination to depression and/or depressive symptoms (59), expectations of racism may operate either consciously, as proposed by Nuru-Jeter et al (17), or unconsciously, via a preattentive system that automatically screens the environment for cues about threat and safety (60, 61). In the latter instance, the absence of specific indicators of safety would co-occur with feelings of threat, leading to anxiety and heightened vigilance. This is consistent with Brosschot and colleagues’ generalized unsafety theory of stress, which posits that chronic stress responses in daily life are largely automatic (i.e. unconscious), resulting from feelings of unsafety that are independent of cognitive representations of, or actual exposure to, stressors (62, 63).
Threat and vigilance -- key components in the conceptualization of expectations of racism --are also defining characteristics of post-traumatic stress disorder (PTSD), which has also been linked to physiological arousal and IMT (64, 65). However, PTSD and other anxiety disorders are characterized as maladaptive fear responses (66); whereas expectations of racism may be an adaptive response to living in a society where racism-related events (e.g. police shootings (67), comments by political leaders (68), increasing hate crimes (69)) are highly publicized and salient in everyday life. But despite these differences, both PTSD and expectations of racism are characterized by sustained vigilance, threat, and feelings of unsafety–and these may be the critical underlying factors driving associations with poor cardiovascular health.
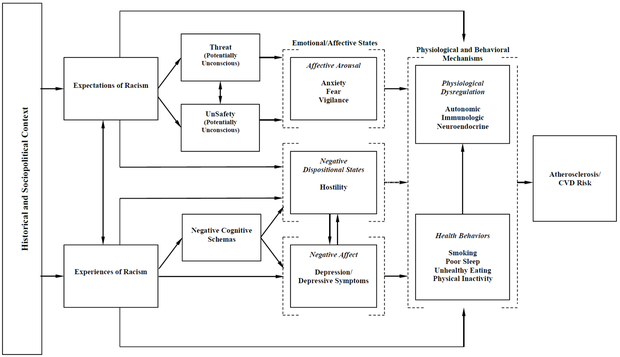
Our proposed conceptual framework linking expectations of racism to atherosclerosis and CVD risk is detailed in Figure 3. We begin with an acknowledgement of how both experiences and expectations of racism might vary based on the historical timeframe (e.g. pre- versus post the Civil Rights Act in the US; pre- versus post widespread use of social media (70)), and the sociopolitical climate (e.g. the election of Barack Obama in 2008 (71), the increase in hate crimes in 2017 (69)). The association between experiences and expectations of racism is highlighted, as well as the (potentially) different emotional and affective pathways linking the two separate constructs to atherosclerosis and CVD risk.
Figure 3.
Conceptual Framework linking Expectations of Racism to CVD Risk in African-American Women.
Experiences of racism are hypothesized to lead to depression/depressive symptoms and hostility; theoretically through negative relational schemas about others and the world (59), but also independent of those schemas, as individuals who have positive schemas about the world (e.g. believing that it is just) often report the lowest levels of well-being following discriminatory stressors (72, 73). Expectations, on the other hand, are hypothesized to result in affective states such as anxiety, fear, and vigilance—primarily via heightened feelings of threat and unsafety. Hostility might also play a role. Hostility was strongly correlated with expectations of racism in our sample, which was not surprising, given the strong correlation between hostility and sensitivity to interpersonal rejection found in other studies (74, 75). Still, hostility was not associated with IMT, and including hostility as a covariate in our analyses did not alter our results. However, this could conceivably be due to our small sample size, thus we have retained hostility in our conceptual model as an important variable to consider in future studies.
All of the emotional/affective states identified in our conceptual model could lead to similar physiological changes, such as increased autonomic dysregulation (76, 77), disruptions in the diurnal variation in cortisol via neuroendocrine pathways (78, 79), and/or increased inflammation (78, 80). These physiological changes could be independent of, or directly mediated through negative health behaviors known to be associated with negative affect: including smoking, poor sleep, unhealthy eating, and physical inactivity (81). Both sets of factors (physiological and behavioral mechanisms) could ultimately lead to greater atherosclerosis and increased CVD risk. It is also possible that expectations (and experiences) of racism exert an effect on physiological and behavioral processes independent of emotional and affective states. These pathways are all detailed in Figure 3.
It is important to note that we did not observe a main effect of reports of racism on IMT in our sample. This is in direct contrast to a prior study of racial/ethnic discrimination and IMT by Troxel et al (29), and other studies in women that have observed linkages between self-reported experiences of discrimination and a range of cardiovascular indices including coronary artery calcification (8), visceral fat (82), and the metabolic syndrome (83). But all of these prior studies used the everyday discrimination scale (EDS) (84) to assess discriminatory experiences, and in the case of Troxel et al, only specific attributions to everyday racial/ethnic discrimination were associated with IMT. Because the construct of interest in the current analysis inquired about expected racism, we utilized the Schedule of Racist Events (SRE), as it assesses exposure to racism more explicitly than the EDS. However, the SRE is primarily event-based, capturing acute exposures to racism, while the EDS captures more chronic, day-to-day forms of mistreatment. Prior studies of acute exposures to racism and indices of cardiovascular health have also found null associations, particularly among African-Americans (85); and a 2014 meta-analysis found that studies using the EDS yielded larger racism and health effect sizes than studies that used other measures (5). Thus, it is possible that the absence of a main effect of racism on IMT in the current sample was primarily due to the measure of racism used. Consequently, Figure 3 outlines an association between experiences of racism and atherosclerosis and CVD risk, even though that association was not observed in the current analysis. Future studies in this area would benefit from the inclusion of measures that capture chronic, as well as acute, experiences of racial discrimination.
Because our conceptual model was primarily driven by a desire to explicate the potential mechanisms through which expectations of racism might affect CVD risk (independent of experiences of racism) it does not include additional chronic stressors or adverse life events. Studies have consistently found that associations between racism/discriminatory stressors and CVD risk persist even after adjustment for these factors (29, 86, 87). Although the extant research in this area has focused on experiences rather than expectations of racism, our findings on expectations of racism and IMT are in keeping with this broader trend. Thus, we are conceptualizing additional chronic stressors and adverse life events as important contextual confounding variables known to vary by race (29, 86, 87) that could be controlled for in future studies where appropriate. However, based on our observations and findings from prior studies, evidence suggests that these factors may not be the critical component(s) linking expectations of racism to CVD risk.
There are several limitations to this study that should be noted. To begin with, our findings are cross-sectional and thus directionality of the association between expectations of racism and carotid IMT cannot be fully determined. However, the “silent” nature of carotid atherosclerosis makes reverse causality (i.e. those with more disease reporting higher expectations of racism) highly unlikely. Another limitation is the relatively small sample size. This limited our ability to control for a range of psychological confounders, and may have affected the likelihood of detecting a main effect of experiences of racism, as well as a significant expectations by experiences of racism interaction. Also, the scale we used to measure expectations of racism, the Race-Based Rejection Sensitivity Questionnaire, is typically examined in conjunction with personal (i.e. non race-based) sensitivity to rejection, which was not assessed in the current study. Because personal sensitivity to rejection has not been strongly linked to racism-related exposures --including the Race-Based Rejection Sensitivity Questionnaire (14, 88–90)-- we included hostility, as a trait-level characteristic that has shown linkages with these factors. Nonetheless, future studies utilizing this scale should also consider adjusting for personal sensitivity to rejection. Additionally, in our modification of the Race-Based Rejection Sensitivity Questionnaire, we dropped the anxious/concerned subscale utilized in the original version. This decision was driven by feedback from our participants; but given the proposed linkages between expectations of racism and overall anxiety, it is unclear whether excluding this subscale might have affected our results. Further, our sample was primarily comprised of educated African-American women. Although this is an important group to focus on – primarily because they have more access to integrated environments and are more likely to report (and perhaps have concerns about) racism than their lower-SES counterparts (91, 92) —findings based on the experiences of educated African-Americans may not generalize to their less-educated counterparts. Similarly, findings based on African-American women may not generalize to men or women from other racial/ethnic groups. Finally, we only had data on smoking for a subset of women in the sample, thus were unable to control for it in multivariable models. Although the prevalence of smoking among African-American women is fairly low compared to White women, White men and African-American men (93) (particularly among educated African-American women, where the prevalence is less than 10% (94)); the lack of inclusion of smoking status in our analyses is a limitation of the current study.
These limitations are offset by several strengths. We utilized a well-validated social psychological measure of “expectations” of racism to test our hypotheses, and extended it for the first time to a community sample, with a pre-clinical biological endpoint. This allowed us to study a novel, culturally relevant stressor in a vulnerable sub-population at risk for CVD. We were also able to examine several key psychological factors that could potentially confound associations between expectations of racism and CVD risk, including chronic stress burden not directly due to race, depressive symptoms, and hostility. Further, although our study sample was small, the distribution of IMT measurements is concordant with published population norms for African American women (34).
In sum, current findings indicate that expectations of racism may be an important race-related stressor to consider in future research. We found evidence of a significant, independent association between expectations of racism and a marker of CVD risk; however prospective, longitudinal research is needed to determine whether expectations of racism are associated with changes in IMT and other markers of CVD risk over time. Additional observational and experimental studies are also needed to identify the psychological and physiological pathways through which expectations of racism might affect health. It may also be important to elucidate the circumstances that lead to heightened expectations of racism–such as vicarious exposure to racism and/or racial socialization – in order to determine whether these factors further contribute to elevated cardiovascular risk. Finally, additional research is needed to establish if stress-management interventions designed to improve coping with both the occurrence and expectation of racism might ultimately prove beneficial for African-American women’s cardiovascular health.
Acknowledgments
CONFLICTS OF INTEREST AND SOURCE OF FUNDING:
The authors have no relevant Conflicts of Interest.
TT Lewis received funding for this project from the National Center for Advancing Translational Sciences (NCATS) via a Clinical and Translational Science Award (CTSA) (Grant UL1 RR024139), the National Heart Lung and Blood Institute (Grant K01HL092591), and the American Heart Association (Grant 07–04-C). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the NHLBI, NCATS, or the National Institutes of Health (NIH).
Acronyms used in text:
- CVD
Cardiovascular Disease
- IMT
Intima Media Thickness
- BMI
Body Mass Index
- SBP
Systolic Blood Pressure
- BDI
Beck Depression Inventory
- DICOM
Digital Imaging and Communication in Medicine
Contributor Information
Tené T. Lewis, Department of Epidemiology, Rollins School of Public Health, Emory University, Atlanta, GA 30322, tene.t.lewis@emory.edu.
Rachel Lampert, Section of Cardiology, Yale University School of Medicine, New Haven, CT 06510, rachel.lampert@yale.edu.
Domonique Charles, Department of Pediatrics, Navicent Health, Mercer University School of Medicine.
Stuart Katz, Division of Cardiology, New York University School of Medicine, Stuart.Katz@nyumc.org.
REFERENCES
- 1.Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, de Ferranti SD, Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jimenez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Lutsey PL, Mackey JS, Matchar DB, Matsushita K, Mussolino ME, Nasir K, O’Flaherty M, Palaniappan LP, Pandey A, Pandey DK, Reeves MJ, Ritchey MD, Rodriguez CJ, Roth GA, Rosamond WD, Sampson UKA, Satou GM, Shah SH, Spartano NL, Tirschwell DL, Tsao CW, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation. 2018;137:e67–e492. [DOI] [PubMed] [Google Scholar]
- 2.Jolly S, Vittinghoff E, Chattopadhyay A, Bibbins-Domingo K. Higher cardiovascular disease prevalence and mortality among younger blacks compared to whites. Am J Med. 2010;123:811–8. [DOI] [PubMed] [Google Scholar]
- 3.Jha AK, Varosy PD, Kanaya AM, Hunninghake DB, Hlatky MA, Waters DD, Furberg CD, Shlipak MG. Differences in Medical Care and Disease Outcomes Among Black and White Women With Heart Disease. Circulation. 2003;108:1089–94. [DOI] [PubMed] [Google Scholar]
- 4.Lewis TT, Cogburn CD, Williams DR. Self-Reported Experiences of Discrimination and Health: Scientific Advances, Ongoing Controversies, and Emerging Issues. Annual review of clinical psychology. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dolezsar CM, McGrath JJ, Herzig AJ, Miller SB. Perceived racial discrimination and hypertension: a comprehensive systematic review Health psychology : official journal of the Division of Health Psychology, American Psychological Association; 2014;33:20–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brondolo E, Love EE, Pencille M, Schoenthaler A, Ogedegbe G. Racism and hypertension: a review of the empirical evidence and implications for clinical practice. American journal of hypertension. 2011;24:518–29. [DOI] [PubMed] [Google Scholar]
- 7.Hunte HE, Williams DR. The association between perceived discrimination and obesity in a population-based multiracial and multiethnic adult sample. Am J Public Health. 2009;99:1285–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lewis TT, Everson-Rose SA, Powell LH, Matthews KA, Brown C, Karavolos K, Sutton-Tyrrell K, Jacobs E, Wesley D. Chronic exposure to everyday discrimination and coronary artery calcification in African-American women: the SWAN Heart Study. Psychosom Med. 2006;68:362–8. [DOI] [PubMed] [Google Scholar]
- 9.Lewis TT, Aiello AE, Leurgans S, Kelly J, Barnes LL. Self-reported experiences of everyday discrimination are associated with elevated C-reactive protein levels in older African-American adults. Brain, behavior, and immunity. 2010;24:438–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beydoun MA, Poggi-Burke A, Zonderman AB, Rostant OS, Evans MK, Crews DC. Perceived Discrimination and Longitudinal Change in Kidney Function Among Urban Adults. Psychosom Med. 2017;79:824–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Owens SL, Hunte HER, Sterkel A, Johnson DA, Johnson-Lawrence V. Association Between Discrimination and Objective and Subjective Sleep Measures in the Midlife in the United States Study Adult Sample. Psychosom Med. 2017;79:469–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ikram UZ, Snijder MB, Agyemang C, Schene AH, Peters RJG, Stronks K, Kunst AE. Perceived Ethnic Discrimination and the Metabolic Syndrome in Ethnic Minority Groups: The Healthy Life in an Urban Setting Study. Psychosomatic Medicine. 2017;79:101–11. [DOI] [PubMed] [Google Scholar]
- 13.Myers HF, Lewis TT, Parker-Dominguez T. Stress, coping and minority health. Handbook of racial and ethnic minority psychology. 2003:377–400. [Google Scholar]
- 14.Mendoza-Denton R, Downey G, Purdie VJ, Davis A, Pietrzak J. Sensitivity to status-based rejection: Implications for African American students’ college experience. Journal of personality and social psychology. 2002;83:896–918. [DOI] [PubMed] [Google Scholar]
- 15.Nelson JC, Adams G, Salter PS. The Marley Hypothesis: Denial of Racism Reflects Ignorance of History. Psychological Science. 2012. [DOI] [PubMed] [Google Scholar]
- 16.Dominguez TP, Dunkel-Schetter C, Glynn LM, Hobel C, Sandman CA. Racial differences in birth outcomes: The role of general, pregnancy, and racism stress. Health Psychology. 2008;27:194–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nuru-Jeter A, Dominguez T, Hammond W, Leu J, Skaff M, Egerter S, Jones C, Braveman P. “It’s The Skin You’re In”: African-American Women Talk About Their Experiences of Racism. An Exploratory Study to Develop Measures of Racism for Birth Outcome Studies. Maternal and Child Health Journal. 2009;13:29–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williams DR, Lavizzo-Mourey R, Warren RC. The concept of race and health status in America. Public Health Rep. 1994;109:26–41. [PMC free article] [PubMed] [Google Scholar]
- 19.Smith TW, Ruiz JM, Uchino BN. Vigilance, active coping, and cardiovascular reactivity during social interaction in young men Health psychology : official journal of the Division of Health Psychology, American Psychological Association; 2000;19:382–92. [DOI] [PubMed] [Google Scholar]
- 20.Clark R, Benkert RA, Flack JM. Large arterial elasticity varies as a function of gender and racism-related vigilance in black youth. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2006;39:562–9. [DOI] [PubMed] [Google Scholar]
- 21.Hicken MT, Lee H, Morenoff J, House JS, Williams DR. Racial/ethnic disparities in hypertension prevalence: reconsidering the role of chronic stress. Am J Public Health. 2014;104:117–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hicken MT, Lee H, Ailshire J, Burgard SA, Williams DR. “Every shut eye, ain’t sleep”: The role of racism-related vigilance in racial/ethnic disparities in sleep difficulty. Race Soc Probl. 2013;5:100–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE. Common Carotid Intima-Media Thickness and Risk of Stroke and Myocardial Infarction : The Rotterdam Study. Circulation. 1997;96:1432–7. [DOI] [PubMed] [Google Scholar]
- 24.Chambless LE, Heiss G, Folsom AR, Rosamond W, Szklo M, Sharrett AR, Clegg LX. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities (ARIC) Study, 1987–1993. American journal of epidemiology. 1997;146:483–94. [DOI] [PubMed] [Google Scholar]
- 25.Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of Clinical Cardiovascular Events With Carotid Intima-Media Thickness: A Systematic Review and Meta-Analysis. Circulation. 2007;115:459–67. [DOI] [PubMed] [Google Scholar]
- 26.Kamarck TW, Shiffman S, Sutton-Tyrrell K, Muldoon MF, Tepper P. Daily Psychological Demands Are Associated With 6-Year Progression of Carotid Artery Atherosclerosis: The Pittsburgh Healthy Heart Project. Psychosomatic Medicine. 2012;74:432–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.John-Henderson NA, Kamarck TW, Muldoon MF, Manuck SB. Early Life Family Conflict, Social Interactions, and Carotid Artery Intima-Media Thickness in Adulthood. Psychosomatic Medicine. 2016;78:319–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thurston RC, Chang Y, Barinas-Mitchell E, von Känel R, Jennings JR, Santoro N, Landsittel DP, Matthews KA. Child Abuse and Neglect and Subclinical Cardiovascular Disease Among Midlife Women. Psychosomatic Medicine. 2017;79:441–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Troxel WM, Matthews KA, Bromberger JT, Sutton-Tyrrell K. Chronic stress burden, discrimination, and subclinical carotid artery disease in African American and Caucasian women Health psychology : official journal of the Division of Health Psychology, American Psychological Association; 2003;22:300–9. [DOI] [PubMed] [Google Scholar]
- 30.Peterson LM, Matthews KA, Derby CA, Bromberger JT, Thurston RC. The relationship between cumulative unfair treatment and intima media thickness and adventitial diameter: The moderating role of race in the study of women’s health across the nation Health psychology : official journal of the Division of Health Psychology, American Psychological Association; 2016;35:313–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Breton CV, Wang X, Mack WJ, Berhane K, Lopez M, Islam TS, Feng M, Hodis HN, Kunzli N, Avol E. Carotid artery intima-media thickness in college students: race/ethnicity matters. Atherosclerosis. 2011;217:441–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Everson-Rose SA, Lewis TT, Karavolos KK, Matthews KA, Sutton-Tyrrell K, Powell LH. Cynical hostility and carotid atherosclerosis in African American and white women: The Study of Women’s Health Across the Nation (SWAN) Heart Study. American Heart Journal. 2006;152:982.e7-.e13. [DOI] [PubMed] [Google Scholar]
- 33.Landrine H, Klonoff EA. The Schedule of Racist Events: A Measure of Racial Discrimination and a Study of Its Negative Physical and Mental Health Consequences. Journal of Black Psychology. 1996;22:144–68. [Google Scholar]
- 34.Stein JH, Korcarz CE, Hurst RT, Lonn E, Kendall CB, Mohler ER, Najjar SS, Rembold CM, Post WS. Use of Carotid Ultrasound to Identify Subclinical Vascular Disease and Evaluate Cardiovascular Disease Risk: A Consensus Statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force Endorsed by the Society for Vascular Medicine. Journal of the American Society of Echocardiography. 2008;21:93–111. [DOI] [PubMed] [Google Scholar]
- 35.Wendelhag I, Liang Q, Gustavsson T, Wikstrand J. A new automated computerized analyzing system simplifies readings and reduces the variability in ultrasound measurement of intima-media thickness. Stroke; a journal of cerebral circulation. 1997;28:2195–200. [DOI] [PubMed] [Google Scholar]
- 36.Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. National Institutes of Health. Obes Res. 1998;6 Suppl 2:51S–209S. [PubMed] [Google Scholar]
- 37.Bromberger JT, Matthews KA. A longitudinal study of the effects of pessimism, trait anxiety, and life stress on depressive symptoms in middle-aged women. Psychology and aging. 1996;11:207–13. [DOI] [PubMed] [Google Scholar]
- 38.Barefoot JC, Dodge KA, Peterson BL, Dahlstrom WG, Williams RB Jr. The Cook-Medley hostility scale: item content and ability to predict survival. Psychosom Med. 1989;51:46–57. [DOI] [PubMed] [Google Scholar]
- 39.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of general psychiatry. 1961;4:561–71. [DOI] [PubMed] [Google Scholar]
- 40.Enders CK. A Primer on the Use of Modern Missing-Data Methods in Psychosomatic Medicine Research. Psychosomatic Medicine. 2006;68:427–36. [DOI] [PubMed] [Google Scholar]
- 41.Sterne JA, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, Wood AM, Carpenter JR. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ (Clinical research ed). 2009;338:b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dibal NP, Okafor R, Dallah H. Challenges and Implications of Missing Data on the Validity of Inferences and Options for Choosing the Right Strategy in Handling Them. International Journal of Statistical Distributions and Applications. 2017;3:87. [Google Scholar]
- 43.Li S, Chen W, Srinivasan SR, Tang R, Bond MG, Berenson GS. Race (black-white) and gender divergences in the relationship of childhood cardiovascular risk factors to carotid artery intima-media thickness in adulthood: the Bogalusa Heart Study. Atherosclerosis. 2007;194:421–5. [DOI] [PubMed] [Google Scholar]
- 44.Ferreira JP, Girerd N, Bozec E, Machu JL, Boivin JM, London GM, Zannad F, Rossignol P. Intima-Media Thickness Is Linearly and Continuously Associated With Systolic Blood Pressure in a Population-Based Cohort (STANISLAS Cohort Study). Journal of the American Heart Association. 2016;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bauer M, Delaney JA, Mohlenkamp S, Jockel KH, Kronmal RA, Lehmann N, Mukamal KJ, Moebus S, Polak JF, Dragano N, Budoff MJ, Erbel R, McClelland RL. Comparison of factors associated with carotid intima-media thickness in the Multi-ethnic Study of Atherosclerosis (MESA) and the Heinz Nixdorf Recall Study (HNR). Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2013;26:667–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fuller-Rowell TE, Curtis DS, Doan SN, Coe CL. Racial disparities in the health benefits of educational attainment: a study of inflammatory trajectories among African American and white adults. Psychosom Med. 2015;77:33–40. [DOI] [PubMed] [Google Scholar]
- 47.Lewis TT, Everson-Rose SA, Sternfeld B, Karavolos K, Wesley D, Powell LH. Race, education, and weight change in a biracial sample of women at midlife. Archives of internal medicine. 2005;165:545–51. [DOI] [PubMed] [Google Scholar]
- 48.Lenfant C, Chobanian AV, Jones DW, Roccella EJ. Seventh report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) resetting the hypertension sails. Circulation. 2003;107:2993–4. [DOI] [PubMed] [Google Scholar]
- 49.Chida Y, Steptoe A. The Association of Anger and Hostility With Future Coronary Heart Disease: A Meta-Analytic Review of Prospective Evidence. Journal of the American College of Cardiology. 2009;53:936–46. [DOI] [PubMed] [Google Scholar]
- 50.Everson-Rose SA, Lewis TT. Psychosocial factors and cardiovascular diseases. Annu Rev Public Health. 2005;26:469–500. [DOI] [PubMed] [Google Scholar]
- 51.Sawyer PJ, Major B, Casad BJ, Townsend SSÄ, Mendes WB. Discrimination and the Stress Response: Psychological and Physiological Consequences of Anticipating Prejudice in Interethnic Interactions. American Journal of Public Health. 2012;102:1020–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Civil Rights Act of 1964, (1964). [Google Scholar]
- 53.Levin S, Sinclair S, Veniegas RC, Taylor PL. Perceived discrimination in the context of multiple group memberships. Psychological Science. 2002;13:557–60. [DOI] [PubMed] [Google Scholar]
- 54.Brown C, Matthews KA, Bromberger JT, Chang Y. The Relation between Perceived Unfair Treatment and Blood Pressure in a Racially/Ethnically Diverse Sample of Women. Am J Epidemiol. 2006;164:257–62. [DOI] [PubMed] [Google Scholar]
- 55.McLaughlin KA, Hatzenbuehler ML, Keyes KM. Responses to discrimination and psychiatric disorders among Black, Hispanic, female, and lesbian, gay, and bisexual individuals. Am J Public Health. 2010;100:1477–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Paradies Y A systematic review of empirical research on self-reported racism and health. International journal of epidemiology. [Review]. 2006;35:888–901. [DOI] [PubMed] [Google Scholar]
- 57.Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg MJ, Van Ijzendoorn MH. Threat-related attentional bias in anxious and nonanxious individuals: a meta-analytic study. Psychological bulletin. 2007;133:1. [DOI] [PubMed] [Google Scholar]
- 58.Mogg K, Bradley BP. Attentional bias in generalized anxiety disorder versus depressive disorder. Cognitive therapy and research. 2005;29:29–45. [Google Scholar]
- 59.Brondolo E, Blair IV, Kaur A. Biopsychosocial Mechanisms Linking Discrimination to Health: A Focus on Social Cognition In: Major B, Dovidio JF, Link BG, editors. The Oxford Handbook of Stigma, Discrimination, and Health: Oxford University Press; 2017. [Google Scholar]
- 60.Teachman BA, Joormann J, Steinman SA, Gotlib IH. Automaticity in anxiety disorders and major depressive disorder. Clinical psychology review. 2012;32:575–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Larsen R Emotion and cognition: The case of automatic vigilance. Psychological Science Agenda (APA Online). 2004;18. [Google Scholar]
- 62.Brosschot JF, Verkuil B, Thayer JF. Exposed to events that never happen: Generalized unsafety, the default stress response, and prolonged autonomic activity. Neuroscience and biobehavioral reviews. 2017;74:287–96. [DOI] [PubMed] [Google Scholar]
- 63.Brosschot JF. Ever at the ready for events that never happen. European journal of psychotraumatology. 2017;8:1309934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Shah AJ, Lampert R, Goldberg J, Veledar E, Bremner JD, Vaccarino V. Posttraumatic stress disorder and impaired autonomic modulation in male twins. Biological psychiatry. 2013;73:1103–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Goetz M, Shah A, Goldberg J, Cheema F, Shallenberger L, Murrah NV, Bremner JD, Vaccarino V. Posttraumatic Stress Disorder, Combat Exposure, and Carotid Intima-Media Thickness in Male Twins. American journal of epidemiology. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®): American Psychiatric Pub; 2013. [Google Scholar]
- 67.U.S. Department of Justice Civil Rights Division. Investigation of Chicago Police Department. 2017. [Google Scholar]
- 68.Louis E Trump’s Insults of Black Americans are Disgusting and Dangerous. cnn.com: cnn.com; 2018. [updated November 10, 2018; cited 2018 November 10]; Available from: https://http://www.cnn.com/2018/11/10/opinions/trumps-insults-of-black-americans-louis/index.html.
- 69.Potok M The Year in Hate and Extremism. 2017. [Google Scholar]
- 70.Social Media Fact Sheet. Washington, D.C.: Pew Research Center; 2018; Available from: http://www.pewinternet.org/fact-sheet/social-media/. [Google Scholar]
- 71.Franco M, Smith-Bynum M. The Relationship between Racial Identity and Perceived Significance of the Election of President Barack Obama among African American Mothers. Identity (Mahwah, NJ). 2016;16:182–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kim E, Park H, editors. Perceived gender discrimination, belief in a just world, self-esteem, and depression in Korean working women: A moderated mediation model Women’s Studies International Forum; 2018: Elsevier. [Google Scholar]
- 73.Major B, Kaiser CR, O’brien LT, McCoy SK. Perceived discrimination as worldview threat or worldview confirmation: Implications for self-esteem. Journal of personality and social psychology. 2007;92:1068. [DOI] [PubMed] [Google Scholar]
- 74.Ayduk O, Downey G, Testa A, Yen Y, Shoda Y. Does rejection elicit hostility in rejection sensitive women? Social Cognition. 1999;17:245–71. [Google Scholar]
- 75.Leary MR, Twenge JM, Quinlivan E. Interpersonal rejection as a determinant of anger and aggression. Personality and Social Psychology Review. 2006;10:111–32. [DOI] [PubMed] [Google Scholar]
- 76.Vaccarino V, Lampert R, Bremner JD, Lee F, Su S, Maisano C, Murrah NV, Jones L, Jawed F, Afzal N. Depressive symptoms and heart rate variability: evidence for a shared genetic substrate in a study of twins. Psychosomatic medicine. 2008;70:628–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bleil ME, Gianaros PJ, Jennings JR, Flory JD, Manuck SB. Trait Negative Affect: Toward an Integrated Model of Understanding Psychological Risk for Impairment in Cardiac Autonomic Function. Psychosomatic Medicine. 2008;70:328–37 10.1097/PSY.0b013e31816baefa. [DOI] [PubMed] [Google Scholar]
- 78.O’Donovan A, Hughes BM, Slavich GM, Lynch L, Cronin M-T, O’Farrelly C, Malone KM. Clinical anxiety, cortisol and interleukin-6: Evidence for specificity in emotion–biology relationships. Brain, behavior, and immunity. 2010;24:1074–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Dienes KA, Hazel NA, Hammen CL. Cortisol secretion in depressed, and at-risk adults. Psychoneuroendocrinology. 2013;38:927–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Vaccarino V, Johnson BD, Sheps DS, Reis SE, Kelsey SF, Bittner V, Rutledge T, Shaw LJ, Sopko G, Bairey Merz CN. Depression, inflammation, and incident cardiovascular disease in women with suspected coronary ischemia: the National Heart, Lung, and Blood Institute-sponsored WISE study. Journal of the American College of Cardiology. 2007;50:2044–50. [DOI] [PubMed] [Google Scholar]
- 81.Cohen BE, Edmondson D, Kronish IM. State of the Art Review: Depression, Stress, Anxiety, and Cardiovascular Disease. American journal of hypertension. 2015;28:1295–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lewis TT, Kravitz HM, Janssen I, Powell LH. Self-reported Experiences of Discrimination and Visceral Fat in Middle-aged African-American and Caucasian Women. American journal of epidemiology. 2011;173:1223–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Beatty Moody DL, Chang Y, Brown C, Bromberger JT, Matthews KA. Everyday Discrimination and Metabolic Syndrome Incidence in a Racially/Ethnically Diverse Sample: Study of Women’s Health Across the Nation. Psychosomatic Medicine. 2018;80:114–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Williams DR, Yu Y, Jackson JS. Discrimination, race, and health. Ann Arbor. 1997;1001:48106. [Google Scholar]
- 85.Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, Gupta A, Kelaher M, Gee G. Racism as a Determinant of Health: A Systematic Review and Meta-Analysis. PLoS One. 2015;10:e0138511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lewis TT, Kravitz HM, Powell LH. Three of the Authors Respond to Discrimination and Cardiovascular Disease. American journal of epidemiology. 2011;173:1244–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Slopen N, Williams DR. Discrimination, other psychosocial stressors, and self-reported sleep duration and difficulties. Sleep. 2014;37:147–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mendoza-Denton R, Goldman-Flythe M, Pietrzak J, Downey G, Aceves MJ. Group-value ambiguity: Understanding the effects of academic feedback on minority students’ self-esteem. Social Psychological and Personality Science. 2010;1:127–35. [Google Scholar]
- 89.Mendoza-Denton R, Pietrzak J, Downey G. Distinguishing institutional identification from academic goal pursuit: Interactive effects of ethnic identification and race-based rejection sensitivity. Journal of personality and social psychology. 2008;95:338–51. [DOI] [PubMed] [Google Scholar]
- 90.Page-Gould E, Mendoza-Denton R, Mendes WB. Stress and coping in interracial contexts: The influence of race-based rejection sensitivity and cross-group friendship in daily experiences of health. The Journal of social issues. 2014;70:256–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hunt MO, Wise LA, Jipguep MC, Cozier YC, Rosenberg L. Neighborhood racial composition and perceptions of racial discrimination: Evidence from the black women’s health study. Social Psychology Quarterly. 2007;70:272. [Google Scholar]
- 92.Krieger N, Waterman PD, Kosheleva A, Chen JT, Carney DR, Smith KW, Bennett GG, Williams DR, Freeman E, Russell B, Thornhill G, Mikolowsky K, Rifkin R, Samuel L. Exposing racial discrimination: implicit & explicit measures--the My Body, My Story study of 1005 US-born black & white community health center members. PLoS One. 2011;6:e27636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Centers for Disease Control and Prevention. Vital Signs: Current Cigarette Smoking Among Adults Aged ≥18 Years--United States, 2005–2010. MMWR. 2011. p. 1207–12. [PubMed] [Google Scholar]
- 94.American Lung Association. Smoking Rates Among African-Americans. 2010. [cited 2014 August 6, 2014]; Available from: http://www.lung.org/stop-smoking/about-smoking/facts-figures/african-americans-and-tobacco.html-8.