Abstract
Billions of bacteria inhabit the gastrointestinal tract. Immune-microbial cross talk is responsible for immunological homeostasis, and symbiotic microbial species induce regulatory immunity, which helps to control the inflammation levels. In this study we aimed to identify species within the equine intestinal microbiota with the potential to induce regulatory immunity. These could be future targets for preventing or treating low-grade chronic inflammation occurring as a result of intestinal microbial changes and disruption of the homeostasis. 16S rRNA gene amplicon sequencing was performed on samples of intestinal microbial content from ileum, cecum, and colon of 24 healthy horses obtained from an abattoir. Expression of genes coding for IL-6, IL-10, IL-12, IL-17, 18 s, TNFα, TGFβ, and Foxp3 in the ileum and mesenteric lymph nodes was measured by qPCR. Intestinal microbiota composition was significantly different in the cecum and colon compared to the ileum, which contains large abundances of Proteobacteria. Especially members of the Clostridiales order correlated positively with the regulatory T-cell transcription factor Foxp3 and so did the phylum Verrucomicrobia. We conclude that Clostridiales and Verrucomicrobia have the potential to induce regulatory immunity and are possible targets for intestinal microbial interventions aiming at regulatory immunity improvement.
Subject terms: Mucosal immunology, Microbiome
Introduction
As in other mammals, the equine intestine is inhabited by billions of bacteria. Host-microbial interactions and pro- and anti-inflammatory responses elicited in response to intestinal bacteria are crucial in establishing and maintaining intestinal microbiota homeostasis1–4. In mammals, this homeostasis is mediated through interactions between microbial-associated molecular patterns (MAMPs), e.g., bacterial lipopolysaccharides (LPS) and lipoproteins, and pattern recognition receptors (PRRs) on the epithelial and immune cells in the gastrointestinal tract (GIT). Through these interactions differentiation of regulatory T-cells (Treg) mediate oral tolerance towards commensal microbes forming the intestinal microbiota5. Dietary changes and other environmental perturbations may cause shifts in the microbial balance, as shown in humans, mice, and horses6–8. Changes in microbial composition, such as the Firmicutes:Bacteroides ratio, termed dysbiosis, and disruption of the immunological homeostasis has been associated with inflammatory diseases both within the GIT and systemically in humans, animal models and livestock9–16. Dysbiosis has also been suggested as a predictor of post weaning diarrhea in pigs17. Consequently, shifting the microbiota towards a composition that stimulates a more immunosuppressive response dominated by Tregs and anti-inflammatory cytokines, such as interleukin 10 (IL-10), transforming growth factor beta (TGF-β) and transcription factor Forkhead box P3 (FoxP3) has been linked to prevention of disease development and amelioration of symptoms of inflammatory diseases in humans and animals18–21. The intestinal microbiota may, therefore, be regarded as a potential target to treat and prevent conditions governed by low-grade chronic inflammation in and outside of the GIT.
Microbiota disturbances leading to disease are also known in equine medicine. Starch overload of the cecum and colon with subsequent pH drop leading to the death of vast microbial populations, gastrointestinal tympani, diarrhea, and endotoxemia has been associated with intestinal microbiota dysbiosis22,23. Also, colitis and colonic obstruction have been linked to changes in the microbial composition24,25. Development of laminitis as a result of starch overload23,26, suggests that changes in intestinal microbiota may also influence diseases outside of the equine GIT. Many horses suffer from equine metabolic syndrome (EMS), which shares several similarities with the human disease of the same name, most importantly chronic low-grade inflammation27–29. A contributing factor to the chronic low-grade inflammation in human metabolic syndrome is microbiota dysbiosis, i.e., smaller changes in intestinal microbiota composition leading to altered immune-microbial homeostasis and increased inflammatory state9,10,14.
The availability of new sequencing technologies, which allow for the entire microbiome to be studied including the strict anaerobes, have increased the understanding of the equine intestinal microbiota importance. However, available studies seeking to establish a core microbiota in horses have unfortunately been inconsistent in profiling methods, sampling regions, and inclusion criteria30–39. Strong correlations between specific intestinal bacteria and key inflammatory parameters are well documented in other species, i.e., mice20,40,41, rats42, and humans43–45. An example of this is the induction of Treg differentiation and reduced inflammatory levels through up-regulation of intestinal bacteria with a well-known anti-inflammatory effect such as Lactobacillus spp., Bifidobacterium spp., and various Clostridiales spp. through the addition of oligosaccharides to the diet46–48. In the intestinal microbiota of overweight individuals, the ration of Firmicutes to Bacteroides is skewed with a reduction in Bacteroidetes and an increase in Firmicutes6,49. It is currently unknown whether similar effects of bacteria on systemic inflammatory status can be obtained in horses. In order to investigate this, basal information is needed on which members of the equine intestinal microbiota exert either a pro- or an anti-inflammatory impact on the immune system.
The objective of the present study was therefore to identify specific bacteria or clusters of bacteria in the equine GIT, which are related to a regulatory response and therefore may be potential targets for improvement of the regulatory immunity.
Method
Collection of samples
Samples were collected post mortem from healthy horses at an abbatoir (Knorrevängen Slakt in Glimåkra Sweden). Only horses that were considered healthy by the veterinarian were included in the study. In total samples were collected from 24 horses between June 30th and July 28th, 2014. The horses were of mixed breeds, 17 mare and 6 geldings and aged between 2 and 21 (mean +/−SD: 11.09 +/−5.03). Samples of intestinal content for microbial analysis were collected from the ileum (approximately 15 cm oral to the ileocecal valve), the cecum and the colon (left ventral colon just oral from the pelvic flexure). Samples were stored in a mobile freezing box at −20 °C until arrival at the laboratory approximately two hours later, where they were immediately frozen at −80 °C. Samples of the ileal mucosa were taken to investigate the local immune reaction in the ileum wall, which is very dense in immune tissue50. Also samples from the lymph nodes (MLN) at the root of the mesentery were taken to investigate the general immune reaction in the intestine. Samples were stored separately in RNAlater (ThermoFischer Scientific, Denmark) for gene expression analysis. Samples were stored at 5 °C for 24 hours, after which the excess RNAlater was removed, and the samples were stored at −80 °C.
Analysis of microbial composition
Extraction of DNA
Before extracting Deoxyribonucleic acid (DNA) from the intestinal content the samples were thawed, and 20 grams were suspended in 40 ml sterile milli-Q water in a stomacher bag with filter and processed in a stomacher (Seward 80 BA 7020 Stomacher Lab Blender, Seward, West Sussex, United Kingdom) in 2 min at maximum speed. A volume of 200 μl was then used for DNA-extraction using the MoBio Power Soil Kit (MoBio QIAGEN Nordic, Copenhagen) following the instructions of the manufacturer.
Sequencing of the intestinal microbiota
The concentration and purity of extracted DNA in each sample was measured using Nanodrop 2000 (ThermoFischer Scientific, Denmark), and concentration was normalised to ~20 ng/μl. The V3-V4 region (~460 bp) of the 16S ribosomal ribonucleic acid (rRNA) gene was amplified using primers compatible with Nextera Index Kit (Illumina) (nxt341_F: 5′-TCGTCGGCAG CGTCAGATGT GTATAAGAGA CAGCCTAYGG GRBGCASCAG-3′and nxt806_R: 5′-GTCTCGTGGG CTCGGAGATG TGTATAAGAG ACAGGGACTA CNNGGGTATCTAAT-3′). Polymerase chain reaction (PCR) reactions containing 12 μl AccuPrimeTM SuperMix II (Life Technologies, CA, USA), 0.5 μl of each primer (10 μM), 5 μl of genomic DNA (~20 ng/μl), and nuclease-free water to a total volume of 20 µl were run on a SureCycler 8800 (Agilent, CA, USA). Cycling conditions applied were: Denaturation at 95 °C for 2 min; 33 cycles of 95 °C for 15 sec, 55 °C for 15 sec and 68 °C for 40 sec; followed by final elongation at 68 °C for 5 min. To incorporate primers with adapters and indexes PCR reactions contained 12 μl Phusion High-Fidelity PCR Master Mix (Thermo Fisher Scientific, USA, MA), 2 μl corresponding P5 and P7 primer (Nextera Index Kit), 2 μl PCR product and nuclease-free water for a total volume of 25 μl. Cycling conditions applied were: 98 °C for 1 min; 13 cycles of 98 °C for 10 sec, 55 °C for 20 sec and 72 °C for 20 sec; elongation at 72 °C for 5 min. The amplified fragments with adapters and tags were purified using AMPure XP beads (Beckman Coulter Genomic, CA, USA). Prior to library pooling clean constructs were quantified using a Qubit fluorometer (Invitrogen, Carlsbad, CA, USA) and mixed in approximately equal concentrations to ensure even representation of reads per sample followed by 250 bp pair-ended MiSeq (Illumina) sequencing performed according to the instructions of the manufacturer.
Sequencing data analysis
The raw dataset containing pair-ended reads with corresponding quality scores were joined, trimmed, filtered from chimeric reads and clustered to operational taxonomic units (OTUs) as previously described51. The Greengenes (13.8) rRNA gene collection was used as a reference database. Quantitative Insight Into Microbial Ecology (QIIME) open source software packages (1.7.0, 1.8.0, and 1.9.1(Various versions of QIIME dealt with different bugs making some of the tests more accurate in older versions of QIIME or more applicable for given format of the file.))52,53 were used for the analysis as previously described in details51 with the following adjustment: the subsampling was performed using 10,000 reads per sample.
Gene expression analysis
Ribonucleic acid (RNA) was extracted from both the MLNs and the ileal mucosa samples using the MagMAX™-96 Total RNA Isolation Kit (Thermo Fischer Scientific). Briefly tissue samples were thawed on ice and transferred to FastPrep® tubes containing 600–700 μl lysis buffer (MagMAX™-96 Total RNA Isolation Kit), 5 μl mercaptoethanol and 0.6 mg acid-washed glass beads (<106 μm, Sigma Life Science, Missouri, USA). The samples were homogenized using a Fast-Prep machine (Fast Prep®-24, MP Biomedicals, CA, USA) at speed 6.5 m/s for 45 sec for six runs. Subsequently, RNA was extracted from the supernatant on the MagMAX™ Express magnetic particle processor according to the manufacturer’s manual. After purification, the RNA concentration was determined by spectrophotometry at 260 nm using a NanoDrop 2000 (Thermo Fischer Scientific, Denmark) and RNA concentration was normalised to ~500 ng/μl. Complementary deoxyribonucleic acid (cDNA) synthesis was performed using the High-Capacity cDNA Reverse Transcriptase kit and GeneAmp PCR 9700 system (Applied Biosystems, Thermo Fischer Scientific, Denmark). Specialized equine probes were obtained from Applied Biosystems, Thermo Fischer Scientific for the genes Interleukin-6 (il6), Interleukin-10 (il10), Interleukin-12 (il12), Interleukin-17 (il17), Tranforming Growth Factor (tgfb), Tumor Necrosis Factor-alpha (tnfa), Forkhead Box P3 (foxp3) and 18 s (probe IDs: Ec03468680_m1, Ec03468647_m1, Ec03468747_m1, Ec03470096_m1, Ec03468030_m1, Ec03467871_m1, Ec04319948_m1, 4333760F). Quantitative PCR (qPCR) was performed on both tissues (MLN and mucosa) according to the manufacturer’s manuals using the TaqMan Gene expression Assay (Thermo Fischer Scientific, Denmark) and the 18S rRNA gene was used as reference. The amplification data was analysed using the StepOne v2.3 software (Applied Biosystems, Fischer Scientific Denmark) to obtain threshold cycle (CT) values. Quality check of the amplification data was performed and samples flagged NOSIGNAL (No detectable level of fluorescence), NOAMP (No amplification), BLFAIL (Baseline can not be fitted for the well) were excluded from the analysis.
Statistical analysis
The differences in taxa abundance between compartments were estimated with a statistic framework: analysis of composition of microbes (ANCOM)54. The rest of the statistical analysis was performed using SAS University Edition (SAS Institute Inc. NC, USA) and GraphPad (GraphPad Software, Inc. La Jolla, CA, USA).
A one-way analysis of variance (ANOVA) using normalized OTU-tables (10,000 reads per sample) was used to analyse the differences in abundance of all phyla comprising 0.1% or more of the total recovered sequences in at least one compartment between the three compartments. From the qPCR analysis, threshold cycle (Ct) values were obtained and normalized to the reference genes. The relative expression of the anti-inflammatory genes il10, tgfb, and foxp3, the pro-inflammatory genes il12, il17, tnfa, and il6, were correlated (Spearman Rank Correlation) with the bacterial abundances to assess a possible relationship between intestinal microbiota and T-cell polarization. An analysis was done both on Phylum and genus level. Abundances in ileum were correlated to gene expression in both the mucosa and MLN and abundances in cecum and colon were correlated to gene expression in the MLN. Only genera present in at least half of the samples and with abundances above 0.1% of total recovered sequences in the respective compartment (ileum, cecum, colon) were included in the analysis. For each cytokine, 46, 41, and 40 correlations were performed in the ileum, cecum, and colon, respectively, and FDR values were calculated.
Results
Expression of specific regulatory genes in the ileum and MLN correlates with abundances of Verrucomicrobia and specific Clostridiales spp
With few exceptions, gene-expression of all genes was measured in all animals (Supplementary Fig. S1). The initial correlation analysis between intestinal microbiota composition summarised to phylum level and cytokine levels revealed two significant correlations in the ileum. Levels of Firmicutes correlated negatively, and levels of Proteobacteria correlated positively with the expression of il6 encoding IIL-6 measured in the mucosa (Table 1). The abundance of Verrucomicrobia correlated positively with expression of the gene foxp3 coding for Foxp3 measured in the MLNs (Table 1). At the genus level, a majority of statistically significant correlations (19 out of 26) were found to be between specific taxa and the expression of genes related to anti-inflammatory or regulatory immunity (Table 1). Microbial composition in the ileum was correlated to gene expression in both the ileal mucosa and MLNs and resulted in 10 significant correlations between bacterial abundances and MLN gene expression. No correlation to gene expression in the ileal mucosa was found at the genus level. Cecal and colonic microbial compositions were correlated to gene expression in the MLN, and 14 significant correlations were observed for the cecal microbiota, while only two for the colonic. All correlations can be found in Table 1. Increasing abundances in both ileum and cecum of several Colstridiales spp. correlated positively with increased expression in MLN of the regulatory T-cell transcription factor foxp3 gene or the il10 gene encoding anti-inflammatory IL-10. An unclassified Ruminococcaceae correlated negatively with the expression of il17, a pro-inflammatory gene produced by T-helper cell type 17 (Th17). Positive correlations were found between increasing abundances of CF213 (Bacteroidetes) and the anti-inflammatory gene tgfb. Finally, increased levels of an unclassified member of the Desulfovibrionaceae family (Proteobacteria) correlated positively with the expression of il10, foxp3, and tgfb in the MLN.
Table 1.
The table shows significant correlations (p > 0.05), in a Speerman Rank Correation, at the Phylum and genus level.
| Level | Compartment | Effect | Taxa | Cytokine | Tissue | Corellation coeff | p value | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Phylum | Order | Family | Genus | |||||||
| ileum | Anti-inflammatory | Firmicutes | il6 | mucosa | −0.47218 | 0.0503 | ||||
| Verrucomicrobia | foxp3 | mln | 0.43337 | 0.0497 | ||||||
| Pro-inflammatory | Proteobacteria | il6 | mucosa | 0.30376 | 0.0381 | |||||
| ileum | Anti-inflammatory | Spirochaetes | Spirochaetales | Spirochaetaceae | Treponema | foxp3 | mln | 0.45015 | 0.0406 | |
| Unclassified | foxp3 | mln | 0.51818 | 0.0161 | ||||||
| [Mogibacteriaceae] | Unclassified | foxp3 | mln | 0.44699 | 0.0422 | |||||
| Peptostreptococcaceae | Other | foxp3 | mln | 0.55038 | 0.0097 | |||||
| Ulclassified | foxp3 | mln | 0.55325 | 0.0093 | ||||||
| Firmicutes | Clostridiales | Lachnospiraceae | Ruminococcus | foxp3 | mln | 0.49593 | 0.0222 | |||
| Roseburia | foxp3 | mln | 0.51891 | 0.0159 | ||||||
| Dorea | foxp3 | mln | 0.56303 | 0.0079 | ||||||
| Ruminococcaceae | Unclassified | foxp3 | mln | 0.46004 | 0.0359 | |||||
| Oscillospira | foxp3 | mln | 0.49887 | 0.0213 | ||||||
| cecum | Anti-inflammatory | Dorea | il10 | mln | 0.42192 | 0.0400 | ||||
| Lachnospiraceae | Coprococcus | il10 | mln | 0.45749 | 0.0246 | |||||
| Firmicutes | Clostridiales | Blautia | il10 | mln | 0.43183 | 0.0351 | ||||
| Ruminococcaceae | Unclassified | il17 | mln | −0.52647 | 0.0362 | |||||
| Oscillospira | foxp3 | mln | 0.53014 | 0.0077 | ||||||
| Bacteroidetes | Bacteroidales | [Paraprevotellaceae] | CF231 | tgfb | mln | 0.53652 | 0.0069 | |||
| il10 | mln | 0.60945 | 0.0016 | |||||||
| Proteobacteria | Desulfovibrionale | Desulfovibrionaceae | Unclassified | tgfb | mln | 0.56850 | 0.0037 | |||
| foxp3 | mln | 0.45568 | 0.0252 | |||||||
| Pro-inflammatory | Firmicutes | Clostridiales | Lachnospiraceae | Coprococcus | il6 | mln | 0.46227 | 0.0229 | ||
| Veillonellaceae | Phascolatobacterium | il6 | mln | 0.44100 | 0.0314 | |||||
| Bacteroidetes | Bacteroidales | [Paraprevotellaceae] | CF231 | il6 | mln | 0.44000 | 0.0314 | |||
| il12 | mln | 0.53652 | 0.0069 | |||||||
| Proteobacteria | Desulfovibrionale | Desulfovibrionaceae | Unclassified | il12 | mln | 0.56850 | 0.0037 | |||
| colon | Pro-inflammatory | Firmicutes | Clostridiales | Lachnospiraceae | Coprococcus | il6 | mln | 0.45532 | 0.0254 | |
| Bacteroidetes | Bacteroidales | [Paraprevotellaceae] | [Prevotella] | foxp3 | mln | −0.62647 | 0.0011 | |||
At the phylum level, significant correlations were found between the expression of genes encoding the pro-inflammatory cytokine IL-6 and regulatory T-cell transcription factor Foxp3 in the ileal mucosa and MLN and phylum abundances. At the genus level, taxa present in more than 50% of all samples and with an abundance above 0.1% in the gastrointestinal tract of horses were used for the analysis. Significant correlations were found between bacterial abundances in ileum, cecum, and colon, and the expression of genes encoding the two anti-inflammatory cytokines IL-10 and TGF-β, the four pro-inflammatory cytokines IL-6, IL-12, IL-17 and TNF-α, and regulatory T-cell transcription factor Foxp3.
Firmicutes is the dominant phylum in the horse gastrointestinal tract although the microbiota significantly differs between the ileum, cecum, and colon
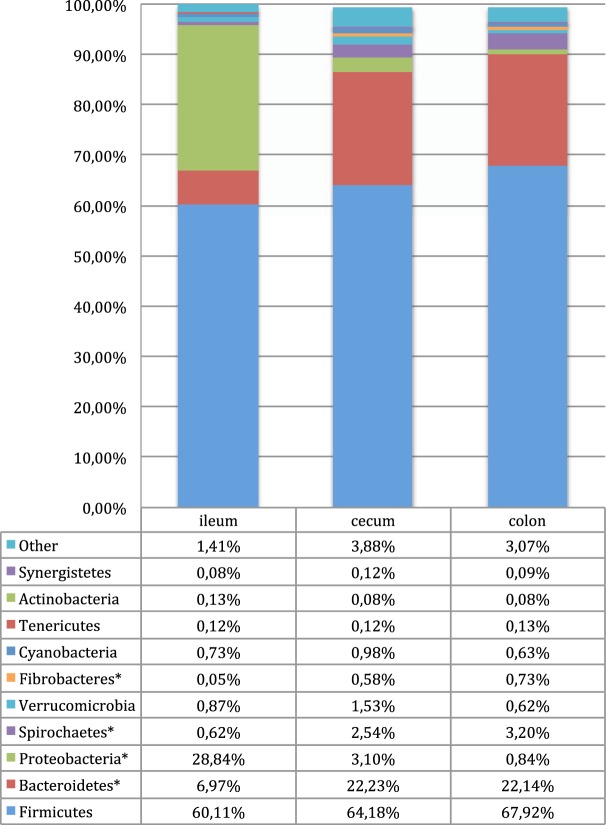
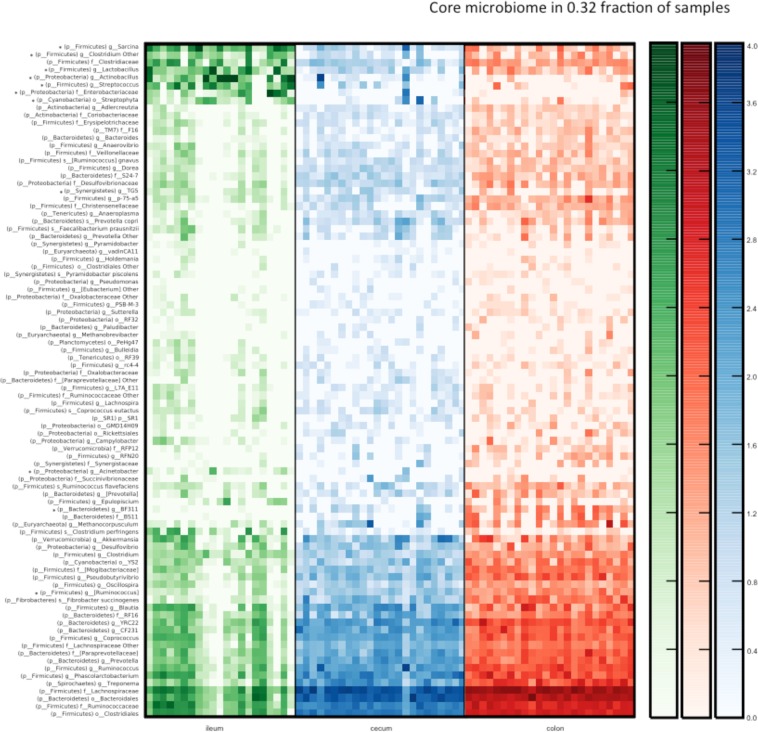
Ten phyla were consistently detected across all sample sites (ileum, cecum, and colon) with a mean abundance above 0.1% (Fig. 1). These were Firmicutes, Bacteroidetes, Proteobacteria, Spirochaetes, Verrucomicrobia, Fibrobacteres (mean abundance ileum 0.05%), Cyanobacteria, Tenericutes, bacteria (mean abundance cecum and colon 0.08%) and Synergisteres (mean abundance ileum 0.08% and colon 0.09%). Additionally, Planctomycetes and candidate phyla SR1, TM7 and WSR-2 were detected in all compartments although at abundances below 0.1%. Firmicutes was the most abundant phylum in all three intestinal compartments followed by Proteobacteria in ileum and Bacteroidetes in the cecum and colon (Fig. 1). Proteobacteria were significantly (p = 0.0001) more abundant in the ileum compared to the cecum and colon, and Bacteroidetes were significantly more abundant in the cecum and colon compared to the ileum (p = 0.0001). Compared to the ileum, Fibrobacteres and Spirochaetes were significantly (p = 0.02 for Fibrobacteres, p = 0.01 for Spirochaetes) more abundant in the colon, and in both cecum and colon respectively (Fig. 1). A core equine microbiota was defined on the genus level. A core microbiota member was defined as a taxa present in at least 32% of the samples. This definition was decided upon before the data analysis. 32% was chosen to both ensure a general high abundance in the samples and at the same time ensure that taxa present in high abundance in only one of the three compartments would still be included in the core microbiota (Fig. 2). Significant differences in abundances of the core bacteria were present between the compartments, primarily between the ileum and cecum/colon. Within Firmicutes, ANCOM analysis (Fig. 2) demonstrated significantly (p < 0.05) higher abundances of Lactobacillus, Streptococcus, unclassified Clostridium and Sarcina in the ileum, and a significantly (p < 0.05) higher abundance of members of Ruminococcus in both cecum and colon, compared to the ileum. The higher abundance of Proteobacteria in the ileum was caused by significantly higher abundances (p < 0.05) of Actinobacillus, Acinetobacter and Enterobacteriaceae compared to the cecum and colon (Supplementary Fig. S2). In the cecum and colon, Bacteroidetes was the second most prominent phylum with the candidate genera BF311 being significantly (p < 0.05) more abundant than in the ileum. Streptophyta belonging to Cyanobacteria and TG5 belonging to Synergisteres differed significantly between the colon and ileum, but not between the ileum and cecum (Supplementary Fig. S2).
Figure 1.
Phyla identified by amplicon sequencing of the V3-V4 region of the 16S rRNA gene and percentage abundance based on normalized OTU numbers in the ileum, cecum and colon of 24 horses. Phyla with abundance above 0.1% in at least one compartment are shown separately. The group “Other” includes the phyla Elusimicrobia, Fusobacteria, Planctomycetes, SR1, TM7, and WPS-2 all with abundances below 0.1%. Samples from 21 horses were used to analysis of the microbial composition in the Ileum and from 24 horses for the Cecum and Colon. Significant differences were found between ileum and the hind gut (cecum/colon), but not between the cecum and colon in an ANOVA analysis. Phyla that differed significantly are marked with *(p < 0.05).
Figure 2.
Heatmap illustrating a core microbiome (taxa represented in at least 32% of all samples) characterized with amplicon sequencing of 16S rRNA gene (V3-V4 region) within three sections of horse gastrointestinal tract. *Indicates taxa with significantly shifted abundance between the three sections (ANCOM, FDR p < 0.05). No major differences in the taxa abundance were detected between the colon and cecum microbiota composition. Scale on the right indicate log abundance.
Discussion
The aim of this study was to investigate the influence of the horse’s intestinal microbiota on the expression of genes signifying regulatory immunity. Our results show a significant correlation between certain bacterial species and the regulatory gene expression profile in the horse GIT, indicating that these species may induce regulatory immunity. We found a potential regulatory effect of Verrucomicrobia in the ileum on the up-regulation of foxp3. Verrucomicrobia and particularly the species Akkermansia muciniphila (A. muciniphila) have been shown to induce regulatory immunity in mice and to have a positive impact on diseases modulated by low-grade chronic inflammation18,55,56. A. muciniphila inhabits the mucous layer of the GIT and modulates pathways involved in immune regulation toward oral tolerance to commensal bacteria57. In the present study we found A. muciniphila in the ileum and a trend towards a positive correlation with foxp3 in the MLN (p = 0.0561) this may indicate that other members of the Verrucomicrobia phylum also contribute to the positive correlation with foxp3. Foxp3 is involved in differentiation of regulatory T-cells mediating tolerance toward commensals, and A. muciniphila has been shown to induce differentiation of Foxp3 positive regulatory T-cells18. The present study suggests that A. muciniphila also have beneficial immune properties in horses. However, further studies should be conducted to confirm the mucin degrading and immune modulating properties of A. muciniphila in horses on the molecular level. Overall we found Firmicutes to correlate with decreasing levels of the gene il6 encoding the pro-inflammatory cytokine IL-6. A closer look at members of the Firmicutes phylum showed that Clostridiales spp. might play a prominent role in inducing regulatory immunity. Increasing abundance of eleven Clostridiales spp. (an unclassified member of Clostridiales, Rumminococcaceae, Lachnospiraceae, Mogibacteriaceae, and Peptostreptococcaceae, and Ruminococcus, Roseburia, Dorea, Oscillospira, Coprococcus, and Blautia) correlated positively with expression of the gene encoding regulatory T-cells transcription factor foxp3 or the gene encoding the anti-inflammatory cytokine IL-10 or both (Table 1). In addition, increasing levels of unclassified Ruminococcaceae (also of the Clostridiales order) correlated negatively with expression of the pro-inflammatory cytokine il17 gene (Table 1) supporting our theory that members of this order may indeed have regulatory properties.
In humans, a low abundance of Clostridiales spp. has been linked to pathological conditions, such as irritable bowel syndrome58. Especially the Clostridiales member Faecalibacterium prausnitzii has been found to be less abundant in human patients with Chrohn’s disease59 or obesity60. Concurrently reduced abundance of both Lachnospiraceae and Ruminococcus (both Clostridiales) have been found in horses with Equine Metabolic Syndrome (EMS)61. As in humans, EMS is a multifactorial disease characterized by a low-grade chronic inflammatory state, obesity, and insulin resistance62,63. An increase in the relative abundances of bacterial taxa associated with regulatory responses such as bifidobacteria has preventive and curative effects on the low-grade inflammation in human metabolic syndrome19. The decrease of Clostridiales members in the GIT of horses suffering from EMS, and the positive correlations between abundances of Clostridiales and markers of regulatory immunity, imply that members of this order have similar beneficial effects in horses as Bifidobacterium have in humans. Not all members of the Clostridiales order may be equally good at inducing regulatory immunity. Coprococcus abundances correlated with both anti-inflammatory il10 and il6 encoding interleukin IL-6 which can induce Th17 differentiation and is involved in upholding the Treg/Th17 balance64. In addition increasing abundances of CF231 correlated with expression of tgfb known inducer of Treg, but also with the pro-inflammatory genes il6 and il12 in the MLN. This underlines the multifaceted relationship between intestinal microbiota and the immune system and the sensitivity of the immunological homeostasis to the surrounding cytokine, chemokine, and microbial stimuli.
As in previous studies attempting at establishing a common microbiome of other mammalian species we found Firmicutes to be the most abundant phylum in all three compartments30–35, but with a significant difference between the ileum and the hindgut (cecum, colon) (Fig. 1). The majority of the differences were found as significant differences in abundances of the phyla Firmicutes, Bacteroidetes, and Proteobacteria. This apparent difference between the ileum and the hindgut seems logical as there are important physiological and digestive differences between the two parts of the intestinal tract, with the hindgut being the main place of bacterial fermentation. In the ileum Proteobacteria was the second most abundant phylum representing 28.8% of the taxa. High abundances of Proteobacteria have been associated with intestinal inflammatory diseases in mice, humans, and cattle15,65,66. However high abundances of Proteobacteria in the upper part of the gastrointestinal tract of clinically healthy horses as observed in this study, have also been observed by others30,37. On the phylum level we saw a positive correlation between Proteobacteria levels and il6 expression, but on the genus level no correlations were found between Proteobacteria in the ileum and the expression of the cytokine-encoding genes. In the cecum and colon Proteobacteria were much less abundant, and one member of the phylum and unclassified Desulfovibrionaceae positively correlated with increased expression of both pro-inflammatory (il6) and anti-inflammatory (il10, tgfb, foxp3) cytokines. The presence of Proteobacteria thus seems to have some immunological effects, but the high abundance found in the ileum in healthy horses in this study, and others lead us to believe that they are part of the normal microbiota. Bacteroidetes was the second largest phylum in the hindgut and significantly more abundant in the hindgut compared to the ileum. At the genus level the Bacteroidetes spp. BF311 was significantly increased in the colon compared to the ileum. Two previous studies have found significant increases in BF311 abundance when horses were turned to a more fibre-rich diet8,67. This suggests that members of the Bacteroidetes phylum are important for the digestion of fibres and for maintaining a healthy intestinal microbiota in the hindgut. While BF311 correlated positively with anti-inflammatory tgfb, it also correlated positively to pro-inflammatory cytokines il6 and il12, and therefore this was not considered an ideal candidate for increasing regulatory immunity.
The above findings suggest that Verrucomicrobia and Clostridiales spp. are potential targets for inducing regulatory immunity. The only described Verrucimicrobia member having the GIT as its ecological niche is A. muciniphila, which also have been shown to be promoted by oligosaccharide feeding68. Clostridiales play an important role in the digestion of poly- and oligosaccharides69, and Ruminococcus (belonging to the Clostridiales) has previously been identified as major fibre fermenters in the equine GIT32,70,71. Oligosaccharides may therefore, be a possible stimulator of Verrucomicrobia spp. and Clostridiales spp. growth in the equine GIT and subsequently have a positive impact on the immune-microbial homeostasis.
As the aim was to describe a core microbiome and to study immune-microbial interaction in the general equine population, the varied nature of the horses and uncontrolled diet, age, and sex, may very well be a good representation of a typical equine population. However the study has several limitations and additional studies should be conducted to confirm the results and to address the limitations mentioned below. It would have been beneficial if the information on certain factors such as diet had been available because the diet has been shown to affect the microbiota25,67, as has age, as the not fully established microbiota in younger horses differ from that of older horses72. Studies suggest that the equine gut microbiota stabilises within the first year of life72–74. The youngest horse in this study was two years of age and we therefore expect all horses to have an adult-like microbiota. Additionally age and gender may have an effect on the microbiota composition, and further studies should be conducted to clarify this. To our knowledge this is the first study investigating the immune microbial interactions in the equine gut. Further studies should be conducted to investigate the regulatory and anti-inflammatory potential of the identified bacteria, preferably by using a broader spectrum of immune markers. Based on the knowledge from this study in vitro fermentation experiments and studies investigating the immune cell distribution locally and systemically would help to further elucidate the immunological impact of the microbiota.
Conclusion
In conclusion, we showed that members of the intestinal microbiota, especially Verrucomicrobia spp. and Clostridiales spp., are associated with increased expression levels of the regulatory cytokines il10 and tgfb and the Treg transcription factor foxp3 in the horse. These bacteria may therefore, be possible candidates for induction of regulatory immunity in the host. We identified a core microbiota in the equine GIT with significant differences in composition between the ileum and the hindgut. These results suggest that the species of the intestinal microbiota identified above have the potential to be useful targets for increasing of the regulatory immunity in the GIT.
Supplementary information
Acknowledgements
The study was supported by the Innovation Fund Denmark (Grant No. 4019-00032B). The authors would like to thank Marianne Petersen for assistance with qPCR procedures.
Author Contributions
F.L., J.F., H.F., G.v.G., D.S.N. and A.K.H. planned the experiment, F.L. collected the samples, F.L. performed the DNA extraction, F.L., L.K. and W.K. performed the sequencing. F.L., L.K. and D.S.N. performed the data analysis of the sequencing data. F.L. performed the RNA extraction and qPCR and F.L. and H.F. performed the data analysis. F.L., L.K. and A.K.H. performed the statistics. All authors took part in drafting and approving the manuscript.
Data Availability
Data and associated protocols are stored on the University of Copenhagen’s backup servers, the sequencing data is available in the European Nucleotide Archive (EAN) with the study number PRJEB33830 and the Q-PCR data at Figshare, 10.6084/m9.figshare.9311813.
Competing Interests
The authors declare no conflicts of interest, apart from the fact that F.L. is employed by Brogaarden Diets Aps.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1038/s41598-019-49081-5.
References
- 1.Macpherson AJ, Harris NL. Interactions between commensal intestinal bacteria and the immune system. Nature reviews.Immunology. 2004;4:478–485. doi: 10.1038/nri1373. [DOI] [PubMed] [Google Scholar]
- 2.Tlaskalová-Hogenová Helena, Štěpánková Renata, Kozáková Hana, Hudcovic Tomáš, Vannucci Luca, Tučková Ludmila, Rossmann Pavel, Hrnčíř Tomáš, Kverka Miloslav, Zákostelská Zuzana, Klimešová Klára, Přibylová Jaroslava, Bártová Jiřina, Sanchez Daniel, Fundová Petra, Borovská Dana, Šrůtková Dagmar, Zídek Zdeněk, Schwarzer Martin, Drastich Pavel, Funda David P. The role of gut microbiota (commensal bacteria) and the mucosal barrier in the pathogenesis of inflammatory and autoimmune diseases and cancer: contribution of germ-free and gnotobiotic animal models of human diseases. Cellular & Molecular Immunology. 2011;8(2):110–120. doi: 10.1038/cmi.2010.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tlaskalova-Hogenova H, et al. Interaction of mucosal microbiota with the innate immune system. Scandinavian Journal of Immunology. 2005;62(Suppl 1):106–113. doi: 10.1111/j.1365-3083.2005.01618.x. [DOI] [PubMed] [Google Scholar]
- 4.Umesaki Y, Setoyama H. Structure of the intestinal flora responsible for development of the gut immune system in a rodent model. Microbes and infection/Institut Pasteur. 2000;2:1343–1351. doi: 10.1016/S1286-4579(00)01288-0. [DOI] [PubMed] [Google Scholar]
- 5.O’Mahony C, et al. Commensal-induced regulatory T cells mediate protection against pathogen-stimulated NF-kappaB activation. PLoS pathogens. 2008;4:e1000112. doi: 10.1371/journal.ppat.1000112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Backhed F, et al. The gut microbiota as an environmental factor that regulates fat storage. Proceedings of the National Academy of Sciences of the United States of America. 2004;101:15718–15723. doi: 10.1073/pnas.0407076101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang J, et al. Dietary history contributes to enterotype-like clustering and functional metagenomic content in the intestinal microbiome of wild mice. Proc Natl Acad Sci USA. 2014;111:E2703–2710. doi: 10.1073/pnas.1402342111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Willing B, et al. Changes in faecal bacteria associated with concentrate and forage-only diets fed to horses in training. Equine veterinary journal. 2009;41:908–914. doi: 10.2746/042516409X447806. [DOI] [PubMed] [Google Scholar]
- 9.Cani PD, et al. Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes. 2008;57:1470–1481. doi: 10.2337/db07-1403. [DOI] [PubMed] [Google Scholar]
- 10.Delzenne NM, Cani PD. Gut microbiota and the pathogenesis of insulin resistance. Current diabetes reports. 2011;11:154–159. doi: 10.1007/s11892-011-0191-1. [DOI] [PubMed] [Google Scholar]
- 11.Turnbaugh PJ, et al. A core gut microbiome in obese and lean twins. Nature. 2009;457:480–484. doi: 10.1038/nature07540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Belkaid Y, Hand TW. Role of the microbiota in immunity and inflammation. Cell. 2014;157:121–141. doi: 10.1016/j.cell.2014.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cani, P. D., Osto, M., Geurts, L. & Everard, A. Involvement of gut microbiota in the development of low-grade inflammation and type 2 diabetes associated with obesity. Gut microbes3 (2012). [DOI] [PMC free article] [PubMed]
- 14.Cani PD, et al. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes. 2007;56:1761–1772. doi: 10.2337/db06-1491. [DOI] [PubMed] [Google Scholar]
- 15.Fecteau Marie-Eve, Pitta Dipti W., Vecchiarelli Bonnie, Indugu Nagaraju, Kumar Sanjay, Gallagher Susan C., Fyock Terry L., Sweeney Raymond W. Dysbiosis of the Fecal Microbiota in Cattle Infected with Mycobacterium avium subsp. paratuberculosis. PLOS ONE. 2016;11(8):e0160353. doi: 10.1371/journal.pone.0160353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ley RE, et al. Obesity alters gut microbial ecology. Proceedings of the National Academy of Sciences of the United States of America. 2005;102:11070–11075. doi: 10.1073/pnas.0504978102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dou Samir, Gadonna-Widehem Pascale, Rome Véronique, Hamoudi Dounia, Rhazi Larbi, Lakhal Lyes, Larcher Thibaut, Bahi-Jaber Narges, Pinon-Quintana Arturo, Guyonvarch Alain, Huërou-Luron Isabelle L. E., Abdennebi-Najar Latifa. Characterisation of Early-Life Fecal Microbiota in Susceptible and Healthy Pigs to Post-Weaning Diarrhoea. PLOS ONE. 2017;12(1):e0169851. doi: 10.1371/journal.pone.0169851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shin NR, et al. An increase in the Akkermansia spp. population induced by metformin treatment improves glucose homeostasis in diet-induced obese mice. Gut. 2014;63:727–735. doi: 10.1136/gutjnl-2012-303839. [DOI] [PubMed] [Google Scholar]
- 19.Cani PD, et al. Selective increases of bifidobacteria in gut microflora improve high-fat-diet-induced diabetes in mice through a mechanism associated with endotoxaemia. Diabetologia. 2007;50:2374–2383. doi: 10.1007/s00125-007-0791-0. [DOI] [PubMed] [Google Scholar]
- 20.Ellekilde M, et al. Characterization of the gut microbiota in leptin deficient obese mice - Correlation to inflammatory and diabetic parameters. Res Vet Sci. 2014;96:241–250. doi: 10.1016/j.rvsc.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 21.Ricardo, N. A. T. et al. Molecules produced by probiotics prevent enteric colibacillosis in pigs. BMC Veterinary Research13, 10.1186/s12917-017-1246-6 (2017). [DOI] [PMC free article] [PubMed]
- 22.Milinovich GJ, et al. Microbial ecology of the equine hindgut during oligofructose-induced laminitis. The ISME journal. 2008;2:1089–1100. doi: 10.1038/ismej.2008.67. [DOI] [PubMed] [Google Scholar]
- 23.Milinovich GJ, Klieve AV, Pollitt CC, Trott D. J. Microbial events in the hindgut during carbohydrate-induced equine laminitis. The Veterinary clinics of North America.Equine practice. 2010;26:79–94. doi: 10.1016/j.cveq.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 24.Costa MC, et al. Comparison of the fecal microbiota of healthy horses and horses with colitis by high throughput sequencing of the V3-V5 region of the 16S rRNA gene. PloS one. 2012;7:e41484. doi: 10.1371/journal.pone.0041484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Daly K, et al. Alterations in microbiota and fermentation products in equine large intestine in response to dietary variation and intestinal disease. The British journal of nutrition. 2012;107:989–995. doi: 10.1017/S0007114511003825. [DOI] [PubMed] [Google Scholar]
- 26.Toth F, Frank N, Chameroy KA, Bostont RC. Effects of endotoxaemia and carbohydrate overload on glucose and insulin dynamics and the development of laminitis in horses. Equine veterinary journal. 2009;41:852–858. doi: 10.2746/042516409X479027. [DOI] [PubMed] [Google Scholar]
- 27.Hoffman RM, Boston RC, Stefanovski D, Kronfeld DS, Harris PA. Obesity and diet affect glucose dynamics and insulin sensitivity in Thoroughbred geldings. Journal of animal science. 2003;81:2333–2342. doi: 10.2527/2003.8192333x. [DOI] [PubMed] [Google Scholar]
- 28.Johnson PJ, Wiedmeyer CE, LaCarrubba A, Ganjam VK, Messer NTT. Diabetes, insulin resistance, and metabolic syndrome in horses. Journal of diabetes science and technology. 2012;6:534–540. doi: 10.1177/193229681200600307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ertelt A, Barton AK, Schmitz RR, Gehlen H. Metabolic syndrome: is equine disease comparable to what we know in humans? Endocrine connections. 2014;3:R81–93. doi: 10.1530/ec-14-0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dougal K, et al. Identification of a core bacterial community within the large intestine of the horse. PloS one. 2013;8:e77660. doi: 10.1371/journal.pone.0077660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Costa MC, Weese JS. The equine intestinal microbiome. Animal health research reviews/Conference of Research Workers in Animal Diseases. 2012;13:121–128. doi: 10.1017/S1466252312000035. [DOI] [PubMed] [Google Scholar]
- 32.Daly K, Stewart CS, Flint HJ, Shirazi-Beechey SP. Bacterial diversity within the equine large intestine as revealed by molecular analysis of cloned 16S rRNA genes. FEMS microbiology ecology. 2001;38:141–151. doi: 10.1016/S0168-6496(01)00178-7. [DOI] [Google Scholar]
- 33.Dougal K, et al. A comparison of the microbiome and the metabolome of different regions of the equine hindgut. FEMS microbiology ecology. 2012;82:642–652. doi: 10.1111/j.1574-6941.2012.01441.x. [DOI] [PubMed] [Google Scholar]
- 34.Shepherd ML, Swecker WS, Jr., Jensen RV, Ponder MA. Characterization of the fecal bacteria communities of forage-fed horses by pyrosequencing of 16S rRNA V4 gene amplicons. FEMS microbiology letters. 2012;326:62–68. doi: 10.1111/j.1574-6968.2011.02434.x. [DOI] [PubMed] [Google Scholar]
- 35.Steelman SM, Chowdhary BP, Dowd S, Suchodolski J, Janecka JE. Pyrosequencing of 16S rRNA genes in fecal samples reveals high diversity of hindgut microflora in horses and potential links to chronic laminitis. BMC veterinary research. 2012;8:231-6148–6148-6231. doi: 10.1186/1746-6148-8-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhao Y, et al. Comparison of Fecal Microbiota of Mongolian and Thoroughbred Horses by High-throughput Sequencing of the V4 Region of the 16S rRNA Gene. Asian-Australas J Anim Sci. 2016;29:1345–1352. doi: 10.5713/ajas.15.0587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ericsson AC, Johnson PJ, Lopes MA, Perry SC, Lanter HR. A Microbiological Map of the Healthy Equine Gastrointestinal Tract. PLOS ONE. 2016;11:e0166523. doi: 10.1371/journal.pone.0166523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schoster A, Arroyo LG, Staempfli HR, Weese JS. Comparison of microbial populations in the small intestine, large intestine and feces of healthy horses using terminal restriction fragment length polymorphism. BMC research notes. 2013;6:91-0500–0506-0591. doi: 10.1186/1756-0500-6-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Costa MC, et al. Characterization and comparison of the bacterial microbiota in different gastrointestinal tract compartments in horses. Vet J. 2015;205:74–80. doi: 10.1016/j.tvjl.2015.03.018. [DOI] [PubMed] [Google Scholar]
- 40.Lundberg R, et al. Gastrointestinal microbiota and local inflammation during oxazolone-induced dermatitis in BALB/cA mice. Comp Med. 2012;62:371–380. [PMC free article] [PubMed] [Google Scholar]
- 41.Bangsgaard BKM, et al. Gut microbiota composition is correlated to grid floor induced stress and behavior in the BALB/c mouse. PloS one. 2012;7:e46231. doi: 10.1371/journal.pone.0046231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Golubeva AV, et al. Prenatal stress-induced alterations in major physiological systems correlate with gut microbiota composition in adulthood. Psychoneuroendocrinology. 2015;60:58–74. doi: 10.1016/j.psyneuen.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 43.Claesson MJ, et al. Gut microbiota composition correlates with diet and health in the elderly. Nature. 2012;488:178–+. doi: 10.1038/nature11319. [DOI] [PubMed] [Google Scholar]
- 44.Remely M, et al. Gut microbiota composition correlates with changes in body fat content due to weight loss. Benef. Mirbobes. 2015;6:431–439. doi: 10.3920/bm2014.0104. [DOI] [PubMed] [Google Scholar]
- 45.Sundin J, et al. Gut Microbiota Correlate With Psychological Distress and Intestinal Lymphocyte Composition in Post-Infectious Irritable Bowel Syndrome Patients. Gastroenterology. 2015;148:S584–S584. [Google Scholar]
- 46.Hansen CH, et al. Dietary xylooligosaccharide downregulates IFN-gamma and the low-grade inflammatory cytokine IL-1beta systemically in mice. The Journal of nutrition. 2013;143:533–540. doi: 10.3945/jn.112.172361. [DOI] [PubMed] [Google Scholar]
- 47.Gobinath D, Madhu AN, Prashant G, Srinivasan K, Prapulla SG. Beneficial effect of xylo-oligosaccharides and fructo-oligosaccharides in streptozotocin-induced diabetic rats. Br J Nutr. 2010;104:40–47. doi: 10.1017/s0007114510000243. [DOI] [PubMed] [Google Scholar]
- 48.Qiu X, Zhang M, Yang X, Hong N, Yu C. Faecalibacterium prausnitzii upregulates regulatory T cells and anti-inflammatory cytokines in treating TNBS-induced colitis. Journal of Crohn’s & colitis. 2013;7:e558–568. doi: 10.1016/j.crohns.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 49.Ley RE, Turnbaugh PJ, Klein S, Gordon JI. Microbial ecology: human gut microbes associated with obesity. Nature. 2006;444:1022–1023. doi: 10.1038/4441022a. [DOI] [PubMed] [Google Scholar]
- 50.Lowden S, Heath T. Lymphoid tissues of the ileum in young horses: distribution, structure, and epithelium. Anatomy and Embryology. 1995;192:171–179. doi: 10.1007/BF00186005. [DOI] [PubMed] [Google Scholar]
- 51.Zachariassen LF, et al. Sensitivity to oxazolone induced dermatitis is transferable with gut microbiota in mice. Scientific reports. 2017;7:44385. doi: 10.1038/srep44385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Caporaso JG, et al. QIIME allows analysis of high-throughput community sequencing data. Nature methods. 2010;7:335–336. doi: 10.1038/nmeth.f.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.McDonald D, et al. An improved Greengenes taxonomy with explicit ranks for ecological and evolutionary analyses of bacteria and archaea. ISME J. 2012;6:610–618. doi: 10.1038/ismej.2011.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mandal S, et al. Analysis of composition of microbiomes: a novel method for studying microbial composition. Microbial ecology in health and disease. 2015;26:27663. doi: 10.3402/mehd.v26.27663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hansen CH, et al. Early life treatment with vancomycin propagates Akkermansia muciniphila and reduces diabetes incidence in the NOD mouse. Diabetologia. 2012;55:2285–2294. doi: 10.1007/s00125-012-2564-7. [DOI] [PubMed] [Google Scholar]
- 56.Everard A, et al. Cross-talk between Akkermansia muciniphila and intestinal epithelium controls diet-induced obesity. Proc Natl Acad Sci USA. 2013;110:9066–9071. doi: 10.1073/pnas.1219451110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Derrien M, et al. Modulation of Mucosal Immune Response, Tolerance, and Proliferation in Mice Colonized by the Mucin-Degrader Akkermansia muciniphila. Front Microbiol. 2011;2:166. doi: 10.3389/fmicb.2011.00166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rangel I, et al. The relationship between faecal-associated and mucosal-associated microbiota in irritable bowel syndrome patients and healthy subjects. Alimentary Pharmacology & Therapeutics. 2015;42:1211–1221. doi: 10.1111/apt.13399. [DOI] [PubMed] [Google Scholar]
- 59.Sokol H, et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc Natl Acad Sci USA. 2008;105:16731–16736. doi: 10.1073/pnas.0804812105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Andoh A, et al. Comparison of the gut microbial community between obese and lean peoples using 16S gene sequencing in a Japanese population. Journal of clinical biochemistry and nutrition. 2016;59:65–70. doi: 10.3164/jcbn.15-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Elzinga SE, Weese JS, Adams AA. Comparison of the Fecal Microbiota in Horses With Equine Metabolic Syndrome and Metabolically Normal Controls Fed a Similar All-Forage Diet. Journal of Equine Veterinary Science. 2016;44:9–16. doi: 10.1016/j.jevs.2016.05.010. [DOI] [Google Scholar]
- 62.Frank N, et al. Equine metabolic syndrome. Journal of veterinary internal medicine/American College of Veterinary Internal Medicine. 2010;24:467–475. doi: 10.1111/j.1939-1676.2010.0503.x. [DOI] [PubMed] [Google Scholar]
- 63.Vick MM, et al. Effects of systemic inflammation on insulin sensitivity in horses and inflammatory cytokine expression in adipose tissue. Am J Vet Res. 2008;69:130–139. doi: 10.2460/ajvr.69.1.130. [DOI] [PubMed] [Google Scholar]
- 64.Kimura A, Kishimoto T. IL-6: regulator of Treg/Th17 balance. Eur J Immunol. 2010;40:1830–1835. doi: 10.1002/eji.201040391. [DOI] [PubMed] [Google Scholar]
- 65.Carvalho Frederic A., Koren Omry, Goodrich Julia K., Johansson Malin E.V., Nalbantoglu Ilke, Aitken Jesse D., Su Yueju, Chassaing Benoit, Walters William A., González Antonio, Clemente Jose C., Cullender Tyler C., Barnich Nicolas, Darfeuille-Michaud Arlette, Vijay-Kumar Matam, Knight Rob, Ley Ruth E., Gewirtz Andrew T. Transient Inability to Manage Proteobacteria Promotes Chronic Gut Inflammation in TLR5-Deficient Mice. Cell Host & Microbe. 2012;12(2):139–152. doi: 10.1016/j.chom.2012.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Walujkar SA, et al. Characterization of bacterial community shift in human Ulcerative Colitis patients revealed by Illumina based 16S rRNA gene amplicon sequencing. Gut Pathogens. 2014;6:1–11. doi: 10.1186/1757-4749-6-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fernandes KA, et al. Faecal microbiota of forage-fed horses in New Zealand and the population dynamics of microbial communities following dietary change. PloS one. 2014;9:e112846. doi: 10.1371/journal.pone.0112846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Everard A, et al. Responses of gut microbiota and glucose and lipid metabolism to prebiotics in genetic obese and diet-induced leptin-resistant mice. Diabetes. 2011;60:2775–2786. doi: 10.2337/db11-0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Krause L, et al. Taxonomic composition and gene content of a methane-producing microbial community isolated from a biogas reactor. Journal of biotechnology. 2008;136:91–101. doi: 10.1016/j.jbiotec.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 70.Hastie PM, Mitchell K, Murray JA. Semi-quantitative analysis of Ruminococcus flavefaciens, Fibrobacter succinogenes and Streptococcus bovis in the equine large intestine using real-time polymerase chain reaction. Br J Nutr. 2008;100:561–568. doi: 10.1017/s0007114508968227. [DOI] [PubMed] [Google Scholar]
- 71.Julliand V, de Vaux A, Millet L, Fonty G. Identification of Ruminococcus flavefaciens as the predominant cellulolytic bacterial species of the equine cecum. Appl Environ Microbiol. 1999;65:3738–3741. doi: 10.1128/aem.65.8.3738-3741.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.E. Earing Jennifer, C. Durig Andrew, L. Gellin Gloria, M. Lawrence Laurie, D. Flythe Michael. Bacterial Colonization of the Equine Gut; Comparison of Mare and Foal Pairs by PCR-DGGE. Advances in Microbiology. 2012;02(02):79–86. doi: 10.4236/aim.2012.22010. [DOI] [Google Scholar]
- 73.Faubladier C, Sadet-Bourgeteau S, Philippeau C, Jacotot E, Julliand V. Molecular monitoring of the bacterial community structure in foal feces pre- and post-weaning. Anaerobe. 2014;25:61–66. doi: 10.1016/j.anaerobe.2013.11.010. [DOI] [PubMed] [Google Scholar]
- 74.Costa MC, Stampfli HR, Allen-Vercoe E, Weese JS. Development of the faecal microbiota in foals. Equine Vet J. 2016;48:681–688. doi: 10.1111/evj.12532. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data and associated protocols are stored on the University of Copenhagen’s backup servers, the sequencing data is available in the European Nucleotide Archive (EAN) with the study number PRJEB33830 and the Q-PCR data at Figshare, 10.6084/m9.figshare.9311813.