Abstract
Objective
To report long term pregnancy rate in polycystic ovary syndrome (PCOS) treated by ovarian drilling. To evaluate predictive factors of pregnancy and possibility of a second drilling.
Design
Retrospective, observational, multicenter study.
Setting
Gynecologic departments of two teaching’s hospitals.
Patients
All infertile women with PCOS who were treated by ovarian drilling from 2004 to 2013. The Rotterdam criteria were applied to define PCOS.
Intervention(s)
Surgical ovarian drilling by laparoscopy and trans vaginal hydro laparoscopy.
Main Outcome Measure(s)
The primary endpoint was pregnancy rate after ovarian drilling. The secondary endpoints were the predictive factors of pregnancy and the possibility of a second ovarian drilling.
Results
289 women were included in the study. The mean follow-up period was 28.4 months (25.3–31.5). A pregnancy was obtained in at least 137 (47.4%) women after a drilling, and 71 (51.8%) of these pregnancies were spontaneous, 48 (16.6%) women achieved at least two pregnancies after drilling, and 27 (56.3%) of these were spontaneous. The predictive factors for effectiveness were a normal body mass index (BMI), an infertility period of less than three years, an AFC of less than 50, and an age of less than 35. Second drillings were performed on 33 women. Among them, 19 (57.6%) achieved at least one pregnancy, and 10 (52.6%) of these were spontaneous. It appeared that a second drilling was effective either when the first drilling had been successful (pregnancy achieved after drilling) or when it had failed in cases of high AFC (greater than 55).
Conclusion
Ovarian drilling permitted to obtain spontaneous pregnancy for women with PCOS. This surgery could have durably effect permitted to obtain more than one pregnancy.
Keywords: Fertility, Polycystic ovary syndrome (PCOS), Ovarian drilling, Transvaginal hydrolaparoscopy, Anti-müllerian hormone
Introduction
In 1935, Stein and Leventhal [1] described an association among polycystic ovaries, oligo-anovulation, and hirsutism, which was called polycystic ovary syndrome (PCOS). PCOS is defined using the Rotterdam criteria [2,3]. PCOS affects 5%–15% of women of reproductive age and is the first cause of infertility due to anovulation [[4], [5], [6]].
The first-line treatment for PCOS-related infertility is medical, using clomiphene citrate (CC) [[7], [8], [9]]. CC induces ovulation in 75%–80% of women [10]. Hyperandrogenism, obesity, high ovarian volume, and anovulation are predictive factors for the failure of CC [11]. In CC-resistant infertility, there is no gold standard for management. Aromatase inhibitor has been shown to be effective in restoring ovulation and pregnancy instead of the CC [12,13]. Nerveless it has not proved its efficiency for CC-resistant infertility compared with placebo (OR 3.17, 95% CI 0.12–83.17) or with ovarian drilling (OR 1.19, 95% CI 0.76–1.86) [14]. The two principal options available are a medical treatment by gonadotropin or a surgical management by ovarian drilling [[7], [8], [9]]. There is no significant difference in birth rate between these two options [15]. Ovarian drilling leads to a lower risk of multiple pregnancies (OR 0.21, CI 95% 0.08–0.58) [15] and avoids hyperstimulation syndrome [7]. Medical treatment requires biological and ultrasound follow-ups, which can be extended over a long period due to the low-dose protocol used. A laparoscopic or transvaginal hydrolaparoscopic drilling involves surgery and anesthesia. The duration during which the ovarian drilling allows to restore an ovulation and thus to obtain a spontaneous pregnancy in case of isolated PCOS is unknown. Published data on the efficacy of recurrent ovarian drillings are scarce [16,17]. Long-term efficacy, allowing more than one pregnancy through the recovery of spontaneous ovulation, may be a significant advantage over the medical treatment. The possibility of repeating this surgery after a couple of months or years should also be assessed.
The aim of this study was to evaluate, in a cohort of infertile women with PCOS who were treated by ovarian drilling, the long-term rate of pregnancy after this surgery. We also evaluated the predictive factors of pregnancy and the possibility of a second drilling.
Materials and methods
This was a retrospective, observational, multicenter study that took place in gynecology and obstetrics departments of two teaching hospitals.
The Rotterdam criteria [2] were applied to define PCOS. The study included all infertile women with PCOS who were treated by ovarian drilling in the participating departments between September 2004 and December 2013. There was no criterion of exclusion. Data were collected based on numeric and medical files. All medical and informatic files of the patients who had received drilling at these periods were consulted until April 2016. Loss to follow up was defined as no consultation after drilling. The patients having benefited from a first drilling carried out previously in another hospital, the drilling carried out in our hospital was considered as a second drilling.
The choice of treatment involved each couple and was made based on infertility assessments. In cases of surgery, the woman underwent an examination with the surgeon, surgery, and a postoperative examination at three months after surgery, during which anti-müllerian hormone (AMH) and antral follicular count (AFC) values were compared.
The surgeon chose between the laparoscopic and transvaginal hydrolaparoscopic surgical approaches. Transvaginal hydrolaparoscopy was preferred in these centers, which developed this technique [18]. The women were placed in the lithotomy position. Using a Veress needle, 300 ml of saline solution were instilled into the peritoneal cavity through the posterior vaginal fornix. A 4 mm introducer was inserted into the pouch of Douglas to allow exploration using a 2.9mm-diameter scope with a 30° lens. The ovaries were recognized via the adnexal pedicle. A bilateral ovarian drilling was performed, with about 10 perforations in each ovary and a depth of insertion of 10 mm. In laparoscopy, the ovarian drilling was performed using a monopolar hook or a bipolar probe. In transvaginal hydrolaparoscopy, the drilling was performed using a bipolar probe (5 fr probe type spring, Versapoint Ethicon SAS, 1 Rue Camille Desmoulins, 92,130 Issy-les-Moulineaux, France). Laparoscopy was proposed in cases of associated pathology requiring surgery or an inaccessible pouch of Douglas.
The ovarian drilling was performed under general anesthesia for laparoscopy and under general anesthesia, usually without curare, or spinal anesthesia for transvaginal hydrolaparoscopy. The surgery was performed during a short hospitalization (for outpatient or one-night surgery).
Infertility after drilling was characterized with no pregnancy after 6 months or more after drilling in case of isolated PCOS. A second drilling was sometimes performed in our hospital: in case of successful first drilling with secondary infertility or in case of failure of a first drilling with infertility despite an assistant reproductive therapy. Some patients had drilling surgery in another hospital before having a drilling in our hospital.
The primary objective was the rate of pregnancy; we check in the medical files the occurrence of a pregnancy for the patient until April 2016 in the two hospitals. The rate of pregnancy was calculating for all patients independently of the first or second drilling.
One of the secondary objectives was the predictive factor of success of drilling defined with a pregnancy or a spontaneous pregnancy. We have tested the following pre-operative predictive factors: BMI ≥ 25 kg/m², infertility > 3 years, age ≥ 35 years and the following post-operative predictive factors: decrease AMH ≥ 30%, decrease AFC ≥ 30%, restauration of ovulation.
In order to limit the selection bias, we look for the women who had a drilling with several cross-software (procedure coding software, operative programming software) with several key word (drilling, fertiloscopy, infertility). To avoid bias of lost to follow-up, all files were systematically consulted until April 2016.
The statistical analyses were performed with STATA/SE (version 14.0, Stata Press, College Station, TX, US). A p value of <0.05 was considered statistically significant. Means and odds ratios (OR) were described with a confidence interval (CI) of 95%. The study was approved by a gynecology ethics committee (CEROG) (IRB 2016-GYN-1006).
Results
Characteristics of women and surgery
This study included 289 women with PCOS. The population characteristics, infertility characteristics, treatments before drilling and ovarian drilling process are described in Table 1. Concerning body mass index (BMI), 22.9% of the participants were overweight (BMI ≥ 25 kg/m²), and 22.1% were obese (BMI ≥ 30 kg/m²). Ten women (3.5%) had already undergone surgery for uterine malformation, 11 (3.8%) infertility, 17 (5.9%) ovarian cystectomy, two (0.7%) bariatric surgery, and 68 (23.5%) another type of visceral surgery. Thirteen women had already undergone a previous ovarian drilling in another hospital.
Table 1.
Population, infertility characteristics and drilling procedure.
| Population characteristics (number) | Mean [CI 95%] or number (%) |
|---|---|
| Age (year) (289) | 30.8 [30.3-31.3] |
| BMI (kg/m²) (280) | 25.6 [24.9-26.3] |
| Tabaco use (283) | 44 (15.2) |
| Diabetic (279) | 7 (2.4) |
| Hypercholesterolemia (279) | 6 (2.1) |
| Hypertriglyceridemia (279) | 4 (1.4) |
| Prior surgery (280) | 118 (40.8) |
| Nulligravid (282) | 164 (56.7) |
| Nulliparous (282) | 241 (83.4) |
| Spontaneous pregnancy (282) | 50 (17.3) |
| Prior miscarriage (282) | 79 (27.3) |
| Repeated miscarriage (≥3) (282) | 12 (4.2) |
| Infertility characteristics and treatment before drilling (number) | |
| AMH (ng/ml) (220) | 13.3 [12.2-14.4] |
| Testosterone (ng/ml) (125) | 0.79 [0.66-0.92] |
| Delta 4 andrestenedione (ng/ml) (108) | 2.73 [2.37-3.08] |
| LH (UI/l) (234) | 8.73 [8.07-9.41] |
| FSH (UI/l) (233) | 6.06 [5.33-6.79] |
| LH/FSH (227) | 1.58 [1.46-1.71] |
| 17 OH progesterone (ng/ml) (84) | 1.39 [0.43-2.35] |
| Prolactin (ng/ml) (177) | 11.9 [10.8-13] |
| Estradiol (pg/ml) (213) | 47.2[43.2-51.1] |
| Primary infertility (282) | 164 (56.7) |
| Duration of infertility (years) (233) | 3.4 [3.1-3.3] |
| Normal spermogram (240) | 178 (61.6) |
| Medical infertility treatment (278) | 223 (77.2) |
| infertility treatment with CC (272) | 162 (56.1) |
| infertility treatment with IVF (289) | 80 (27.7) |
| Drilling surgery (number) | |
| Laparoscopy (282) | 80 (28.4) |
| Hydro-laparoscopy trans-vaginal (282) | 202 (71.6) |
| Number of right perforations (252) | 7.7 [7.4-8] |
| Number of left perforations (249) | 7.6 [7.3-7.9] |
| Tubal perviousness test (282) | 110 (38) |
| Per-operative complication (289) | 15 (5.2) |
| Post-operative complication (281) | 8 (2.8) |
Included women exhibited hirsutism in 37.4% of cases, amenorrhea in 20.8%, and oligomenorrhea in 69.5%. The population’s mean menstrual cycle duration was 57 days [[45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55]]. Ultrasound examinations found polycystic ovaries in 92.7% of cases, with a mean AFC of 50.5 (47.8–53.1).
Per-operative complications occurred in 15 women (5.2%): 11(3.9%) laparoscopic conversions due to failure of the transvaginal hydrolaparoscopy, 1(0.3%) conversion to open surgery due to failure of the laparoscopy, 2(0.7%) serous rectal wounds during the transvaginal hydrolaparoscopy, and 1(0.3%) case of ovarian bleeding without transfusion. Post-operative complications occurred in 8 women (2.8%): 6 (2.1%) had an emergency consultation for pain without hospitalization, 1(0.3%) had a severe ovary hemorrhage with a transfusion and 1(0.3%) had an abdominal dermal hematoma.
Rate of pregnancy after drilling
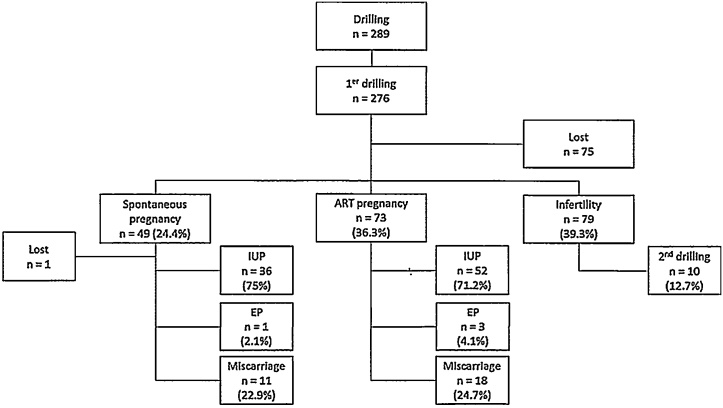
The mean follow-up period was 28.4 months (25.3–31.5). One hundred and thirty-seven women (61.4%) achieved at least one pregnancy after drilling (71 were spontaneous [51.8%]), and 48 women (16.6%) achieved at least two (27 were spontaneous [56.3%]). Concerning the live birth rate, 117 women (40.5%) obtained at least one live birth, and 22 women (7.6%) obtained at least two. The details of the first-pregnancy issues are presented in Fig. 1.
Fig. 1.
Fisrt-pregnancy issues.
The first spontaneous pregnancies occurred within a mean period of 4.5 months (CI 95% [3.6–5.4]). For assisted reproductive technology (ART) pregnancies, the mean time between drilling and pregnancy was 16.1 months (13.6–18.6).
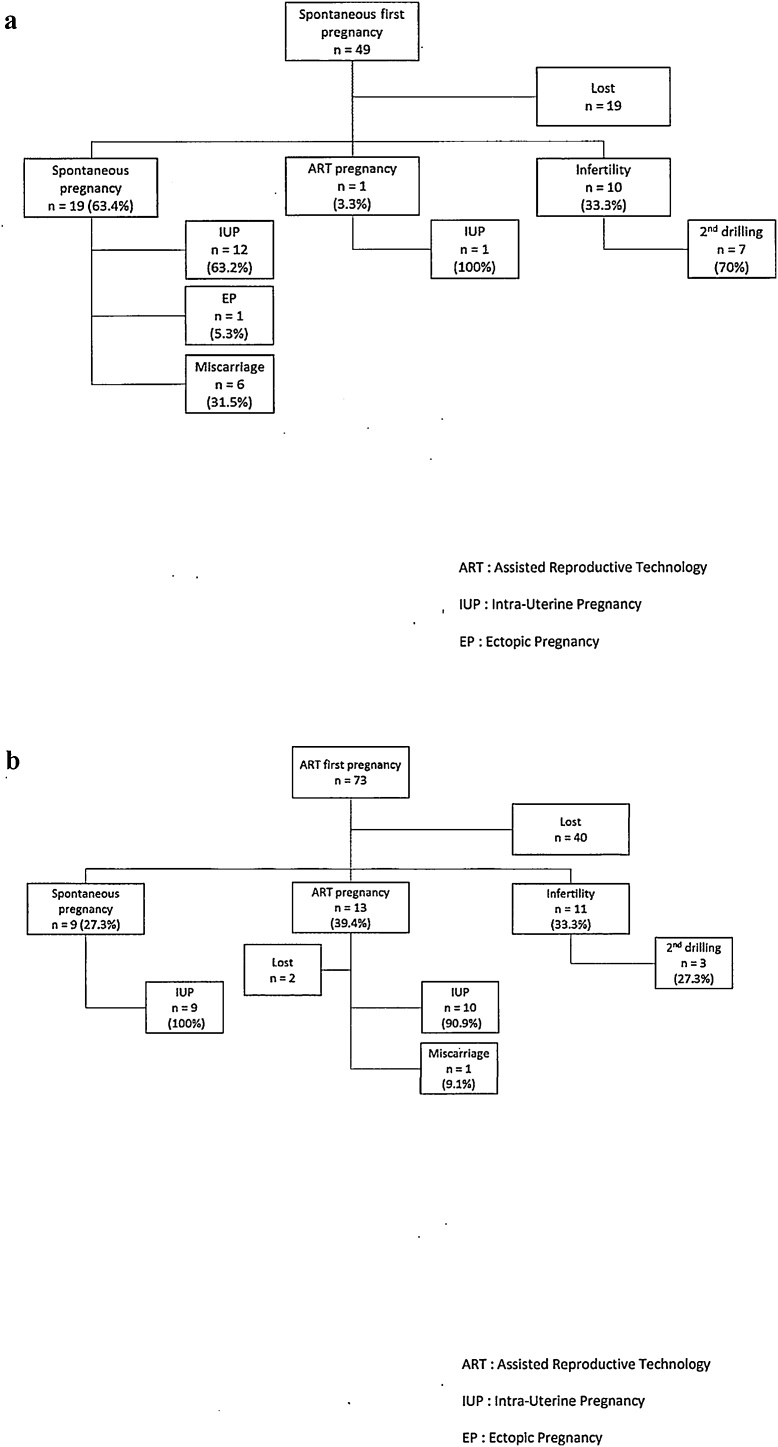
The details of the second-pregnancy issues are presented in Fig. 2a or b.
Fig. 2.
Second pregnancy issues. (a) After a spontaneous first pregnancy. (b) After an ART first pregnancy.
Predictive factors of pregnancy
The average post-operative AMH level, collected from 78 women, was 10.9 ng/ml (9.4–12.3). Twenty-five women (32.1%) presented a decrease of more than 30% in their AMH levels. The average post-operative AFC, collected from 80 women, was 44.3 (39.7–49). Twenty-one women (26.3%) presented a decrease of more than 30% in AFC. Ovulation recovery was noted after drilling for 109 women out of 164 (66.5%).
The predictive factors for successful drilling are presented in Table 2a, Table 2b.
Table 2a.
Predictive factors of success (univariate analysis).
| Rate of pregnancy | Rate of spontaneous pregnancy | |||
|---|---|---|---|---|
| OR [CI 95] | p | OR [CI 95] | p | |
| Pre-operative factors | ||||
| BMI ≥ 25 kg/m² | 0.55 [0.31-0.95] | 0.03 | 0.90 [0.51-1.59] | 0.71 |
| Infertility > 3 years | 0.43 [0.23-0.81] | 0.01 | 0.43 [0.23-0.82] | 0.01 |
| AFC > 50 | 0.70 [0.37-1.30] | 0.26 | 0.51 [0.26-1.00] | 0.05 |
| Age ≥ 35 years | 1.16 [0.55-2.42] | 0.69 | 0.35 [0.14-0.89] | 0.03 |
| Post-operative factors | ||||
| Decrease AMH ≥ 30% | 1.50 [0.57-3.93] | 0.41 | 0.76 [0.22-2.63] | 0.67 |
| Decrease AFC ≥ 30% | 1.17 [0.43-3.22] | 0.76 | 1.67 [0.42-6.65] | 0.46 |
| Ovulation | 2.34 [1.2-4.48] | 0.01 | 6.23 [2.59-15.02] | 0.0001 |
Table 2b.
Predictive factors of success (multivariate analysis).
| Rate of pregnancy | Rate of spontaneous pregnancy | |||
|---|---|---|---|---|
| OR [CI 95] | p | OR [CI 95] | p | |
| Pre-operative factors | ||||
| BMI ≥ 25 kg/m² | 0.51 [0.27-0.95] | 0.04 | NS | NS |
| Infertility > 3 years | 0.43 [0.22-0.82] | 0.01 | 0.45 [0.22-0.91] | 0.03 |
| AFC > 50 | NS | NS | 0.47 [0.22-0.97] | 0.04 |
| Age ≥ 35 years | NS | NS | 0.21 [0.06-0.76] | 0.02 |
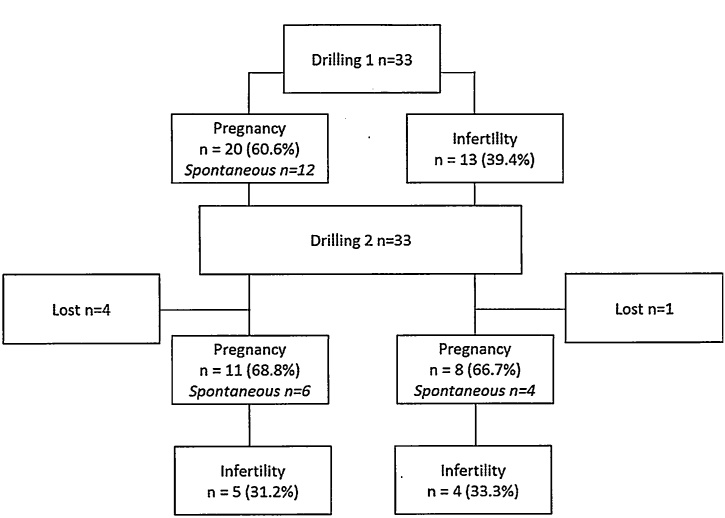
Second drilling
Two drillings were performed for 33 women, 13 after failure and 20 after success. The follow-up data are shown in Fig. 3. The average AMH and AFC values before the first drilling were respectively 13.6 ng/ml (11.9–14.3) and 55.9 (45.4–66.5). These figures present no significant difference between the women who had two drillings and the women who had only one (p = 0.82 and p = 0.21). The average time between the two surgeries was 36.1 months (28.6–43.5). Five women (15.1%) experienced ovary adhesions due to the first surgery. For 10 of the women who had two drillings, pre-operative AMH or AFC was not significantly different before the first or the second procedure, respectively 11.4 (6.9–15.9) and 8.9 (5.2–12.5) for AMH (p = 0.14) and 50.4 (49.5–61.3) and 50.9 (36.5–65.3) for AFC (p = 0.52). The number of perforations was similar during the two procedures: 14.5 (12.6–16.4) and 15.4 (13.1–17.7) (p = 0.52).
Fig. 3.
Issues after a second drilling.
The pregnancy rate after the second drilling was 57.6%, with 52.6% spontaneous pregnancies. There were no significant differences in the rates of pregnancy or of spontaneous pregnancy after the second ovarian drilling, depending on the issue of the first drilling (p = 0.30 and p = 0.25 respectively). Women who achieved pregnancy after the first ovarian drilling (n = 101) were compared with women who achieved pregnancy only after the second ovarian drilling (n = 8). Pre-operative AMH was 12.9 (11.2–14.7) versus 16.5 (8.4–24.6) respectively (p = 0.38). The pre-operative AFC was higher in the second group: 48.8 (44.6–53.0) versus 61 (36.2–85.8) respectively with p = 0.08 with an unilateral test. The number of perforations was similar in the two groups 15.1(14.3–15.9) and 16.3(13.2–19.4) respectively (p = 0.58).
Discussion
Among the study population, 47.4% obtained at least one pregnancy after drilling, and 56.3% of these were spontaneous. The predictive factors for effectiveness were a normal BMI, an infertility period of less than 3 years, an AFC of less than 50, and an age of less than 35. Among the women who had two drillings, 57.6% achieved pregnancies, of which 52.6% were spontaneous.
The external validity of our study is limited by the population mainly from a center of medically assisted procreation and the execution of drilling in an expert center. The evolution of practices and recommendations between 2004 and 2013 is also a bias limiting the external validity of the study. The large size of the sample with follow-up over 2 years is an undeniable advantage. The main biases of the study are related to lost to follow-up and the retrospective nature of the study.
Bayram et al. [19], in a study involving 186 infertile women with CC-resistant PCOS, found that the success of ovarian drilling was predicted by a mean infertility period of 2.8 (+/−2.1) years and a mean age of 28.6 (+/−3.9) years. In the present study, the participants were older, with longer infertility periods and a lower LH/FSH rate [16,19]. This difference is probably due to the assisted reproduction technology unit in one of the centers that referred the participants for surgery.
The approach options for ovarian drilling are regarded as equivalent for success [[20], [21], [22], [23]]. Transvaginal hydrolaparoscopy appears to reduce post-operative pain [21] and to be an easier surgical approach in case of excess weight or obesity [24]. Few complications were noticed [25]; the most frequent (5.4% of cases) was failure of the surgical approach leading to conversion to laparoscopy. Transvaginal hydrolaparoscopy requires a specific learning process with a short learning curve [18,26]. The rate of serous rectal injury was 1% [27]. The adherence rate was 15.1%, which is lower than the 20%–70% rate found in some previously published studies using laparoscopy [28,29]. Transvaginal hydrolaparoscopy may cause fewer adherences probably due to the use of bipolar energy in a liquid environment. Another study found a comparable rate of adherence 15% [30].
The type of energy used and the delivered dose were not recorded. Some studies have demonstrated more efficient drilling when the energy dose was adjusted to the ovarian volume [31]. In the present study, no complication such as premature ovarian failure were noticed [32,33].
The pregnancy rate, spontaneous pregnancy rate, and live birth rate (respectively 61.4%, 24.6%, and 40.5%) were in between the results found by Farquhar et al. [15], with a unknown follow-up period (live birth rate of 34.1%), and the results found by Lund et al. [34] (respectively 88%, 60.5%, and 78%) with a longer follow-up period (15–25 years). These results are comparable to those of Pouly et al. [35], the follow-up period for this study was not specified. In another study, the follow-up period was 1–9 years after ovarian drilling in 116 women [16], the live birth rate was 56%, and the spontaneous pregnancy rate was 61%. However, the diagnosis of PCOS was not based on the Rotterdam criteria, and no flow chart is available. Nahuis et al. reported a live birth rate of 86% with 33% spontaneous pregnancies in 83 women over a follow-up period of 134 months [17]. A second pregnancy was obtained for 61% of the participants (35% spontaneously), and a third was obtained in 13%. This study by Nahuis et al. concluded that drilling reduced the use of ART and increased the chance of a second pregnancy. The present study sustained these hypotheses, as numerous participants achieved several pregnancies, particularly spontaneously, after drilling.
The medical costs of drilling are lower than those of ART [[36], [37], [38]]. Ovarian drilling can prevent complementary ART and can improve fertility [39]. Ovarian drilling is well accepted by women [40], and they mainly choose this procedure over others with equal efficacy [41].
In cases of isolated CC-resistant PCOS, drilling can be proposed before a medical ovulation induction treatment. In cases of associated infertility factors it is more difficult to pinpoint the best time for ovarian drilling [[42], [43], [44]].
Abu Hashim et al. [48] found two factors predicting failures in ovarian drilling: an infertility period of more than 3 years and a BMI ≥ 25 kg/m². A normal weight can increase the chance of pregnancy with a relative risk (RR) of 1.73 (1.39–2.17). Some retrospective studies have found a high level of LH to be a prognostic factor for success. AMH levels were not found to be prognostic factors in ovarian drilling [52,53], but the studies included small populations. High ovarian volume could be a predictive factor for success [54]. There is no valid model to estimateing the chance of pregnancy after ovarian drilling [55]. Elmashad et al (59) found a significant difference in AMH levels between the group with and without spontaneous ovulation after drilling. In the present study, the recovery of ovulation was the only post-operative prognostic factor for pregnancy.
Amer et al. [56], in a retrospective study of 20 women who had undergone a previous ovarian drilling, repeated this surgery after CC failure. The population was separated into two groups, women with a previous successful ovarian drilling and women with a previous failed ovarian drilling. After the second drilling, ovulation and pregnancy rates were significantly higher in the first group. In the present study, 33 women underwent a second drilling, and there was no significant difference between those with a previous success and those with a previous failure (p = 0.30). The rates of pregnancy and spontaneous pregnancy, respectively 57.6% and 52.6%, were higher in both groups after the second drilling. AFC values appeared higher in the group that only achieved success with the second ovarian drilling (mean AFC 61.0[36.2–85.8]) than it did in the group that achieved success with the first drilling (mean AFC 48.8[44.6–53.0]) (p = 0.08). Some women with high ovarian volumes perhaps required a higher dose of energy obtained by two drillings.
Conclusion
Ovarian drilling by laparoscopy or transvaginal hydrolaparoscopy allowed to obtain a correct rate of pregnancy. The main advantage of this procedure is its extended period of efficacy that lead to more than one pregnancy in some cases. The predictive factors for effectiveness were a normal body mass index (BMI), an infertility period of less than three years, an AFC of less than 50, and an age of less than 35 years. A second ovarian drilling may be an option in cases of transitory success after the first drilling or in cases of failure due to high ovarian volume.
Further studies would be required to substantiate the efficacy and long term effects of procedure. In cases of CC-resistant women with isolated polycystic ovary syndrome, ovarian drilling could become the first-line treatment.
Declaration of Competing Interest
The authors declare that they have no competing interest.
References
- 1.Stein I., Leventhal M. Amenorrhea associated with bilateral polycystic ovaries. Am J Obstet Gynecol. 1935;29:181–191. [Google Scholar]
- 2.Rotterdam ESHRE/ASRM-Sponsored PCOS consensus workshop group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS) Hum Reprod Oxf Engl. 2004;19(1):41–47. doi: 10.1093/humrep/deh098. [DOI] [PubMed] [Google Scholar]
- 3.Legro R.S., Arslanian S.A., Ehrmann D.A., Hoeger K.M., Murad M.H., Pasquali R. Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2013;98(12):4565–4592. doi: 10.1210/jc.2013-2350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Azziz R., Woods K.S., Reyna R., Key T.J., Knochenhauer E.S., Yildiz B.O. The prevalence and features of the polycystic ovary syndrome in an unselected population. J Clin Endocrinol Metab. 2004;89(6):2745–2749. doi: 10.1210/jc.2003-032046. [DOI] [PubMed] [Google Scholar]
- 5.Knochenhauer E.S., Key T.J., Kahsar-Miller M., Waggoner W., Boots L.R., Azziz R. Prevalence of the polycystic ovary syndrome in unselected black and white women of the southeastern United States: a prospective study. J Clin Endocrinol Metab. 1998;83(9):3078–3082. doi: 10.1210/jcem.83.9.5090. [DOI] [PubMed] [Google Scholar]
- 6.Joham A.E., Boyle J.A., Ranasinha S., Zoungas S., Teede H.J. Contraception use and pregnancy outcomes in women with polycystic ovary syndrome: data from the Australian Longitudinal Study on Women’s Health. Hum Reprod Oxf Engl. 2014;29(4):802–808. doi: 10.1093/humrep/deu020. [DOI] [PubMed] [Google Scholar]
- 7.Balen A.H., Morley L.C., Misso M., Franks S., Legro R.S., Wijeyaratne C.N. The management of anovulatory infertility in women with polycystic ovary syndrome: an analysis of the evidence to support the development of global WHO guidance. Hum Reprod Update. 2016 doi: 10.1093/humupd/dmw025. [DOI] [PubMed] [Google Scholar]
- 8.Thessaloniki ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Consensus on infertility treatment related to polycystic ovary syndrome. Hum Reprod Oxf Engl. 2008;23(3):462–477. doi: 10.1093/humrep/dem426. [DOI] [PubMed] [Google Scholar]
- 9.Royal College of Obstetricians & Gynaecologists; London: 2013. National collaborating centre for women’s and children’s health (UK). fertility: assessment and treatment for people with fertility problems [Internet]http://www.ncbi.nlm.nih.gov/books/NBK247932/ [cited 2016 Sep 26]. Available from: [PubMed] [Google Scholar]
- 10.Homburg R. Clomiphene citrate--end of an era? A mini-review. Hum Reprod Oxf Engl. 2005;20(8):2043–2051. doi: 10.1093/humrep/dei042. [DOI] [PubMed] [Google Scholar]
- 11.Imani B., Eijkemans M.J.C., te Velde E.R., Habbema J.D.F., Fauser B.C.J.M. A nomogram to predict the probability of live birth after clomiphene citrate induction of ovulation in normogonadotropic oligoamenorrheic infertility. Fertil Steril. 2002;77(1):91–97. doi: 10.1016/s0015-0282(01)02929-6. [DOI] [PubMed] [Google Scholar]
- 12.Mitwally M.F., Casper R.F. Use of an aromatase inhibitor for induction of ovulation in patients with an inadequate response to clomiphene citrate. Fertil Steril. 2001;75(2):305–309. doi: 10.1016/s0015-0282(00)01705-2. [DOI] [PubMed] [Google Scholar]
- 13.Elnashar A., Fouad H., Eldosoky M., Saeid N. Letrozole induction of ovulation in women with clomiphene citrate-resistant polycystic ovary syndrome may not depend on the period of infertility, the body mass index, or the luteinizing hormone/follicle-stimulating hormone ratio. Fertil Steril. 2006;85(2):511–513. doi: 10.1016/j.fertnstert.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 14.Franik S., Kremer J.A.M., Nelen W.L.D.M., Farquhar C. Aromatase inhibitors for subfertile women with polycystic ovary syndrome. Cochrane Database Syst Rev. 2014;(2) doi: 10.1002/14651858.CD010287.pub2. [DOI] [PubMed] [Google Scholar]
- 15.Farquhar C., Brown J., Marjoribanks J. Laparoscopic drilling by diathermy or laser for ovulation induction in anovulatory polycystic ovary syndrome. Cochrane Database Syst Rev. 2012;6 doi: 10.1002/14651858.CD001122.pub4. [DOI] [PubMed] [Google Scholar]
- 16.Amer Sa.K., Gopalan V., Li T.C., Ledger W.L., Cooke I.D. Long term follow-up of patients with polycystic ovarian syndrome after laparoscopic ovarian drilling: clinical outcome. Hum Reprod Oxf Engl. 2002;17(8):2035–2042. doi: 10.1093/humrep/17.8.2035. [DOI] [PubMed] [Google Scholar]
- 17.Nahuis M.J., Kose N., Bayram N., van Dessel H.J.H.M., Braat D.D.M., CJCM Hamilton. Long-term outcomes in women with polycystic ovary syndrome initially randomized to receive laparoscopic electrocautery of the ovaries or ovulation induction with gonadotrophins. Hum Reprod Oxf Engl. 2011;26(7):1899–1904. doi: 10.1093/humrep/der141. [DOI] [PubMed] [Google Scholar]
- 18.Fernandez H., Alby J.D., Gervaise A., de Tayrac R., Frydman R. Operative transvaginal hydrolaparoscopy for treatment of polycystic ovary syndrome: a new minimally invasive surgery. Fertil Steril. 2001;75(3):607–611. doi: 10.1016/s0015-0282(00)01746-5. [DOI] [PubMed] [Google Scholar]
- 19.Bayram N., van Wely M., Kaaijk E.M., Bossuyt P.M.M., van der Veen F. Using an electrocautery strategy or recombinant follicle stimulating hormone to induce ovulation in polycystic ovary syndrome: randomised controlled trial. BMJ. 2004;328(7433):192. doi: 10.1136/bmj.328.7433.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Darai E., Dessolle L., Lecuru F., Soriano D. Transvaginal hydrolaparoscopy compared with laparoscopy for the evaluation of infertile women: a prospective comparative blind study. Hum Reprod Oxf Engl. 2000;15(11):2379–2382. doi: 10.1093/humrep/15.11.2379. [DOI] [PubMed] [Google Scholar]
- 21.Giampaolino P., Morra I., Della Corte L., Sparice S., Di Carlo C., Nappi C. Serum anti-Mullerian hormone levels after ovarian drilling for the second-line treatment of polycystic ovary syndrome: a pilot-randomized study comparing laparoscopy and transvaginal hydrolaparoscopy. Gynecol Endocrinol Off J Int Soc Gynecol Endocrinol. 2016:1–4. doi: 10.1080/09513590.2016.1188280. [DOI] [PubMed] [Google Scholar]
- 22.Watrelot A., Nisolle M., Chelli H., Hocke C., Rongières C., Racinet C. Is laparoscopy still the gold standard in infertility assessment? A comparison of fertiloscopy versus laparoscopy in infertility. Results of an international multicentre prospective trial: the “FLY” (Fertiloscopy-LaparoscopY) study. Hum Reprod Oxf Engl. 2003;18(4):834–839. doi: 10.1093/humrep/deg180. [DOI] [PubMed] [Google Scholar]
- 23.Fernandez H., Gervaise A., Alby J.D., Kadoch J. [Ovarian drilling for surgical approach of polycystic ovary syndrome] Gynã©cologie Obs Fertil Sã©nologieâ. 2003;31(3):207–213. doi: 10.1016/s1297-9589(03)00041-9. [DOI] [PubMed] [Google Scholar]
- 24.Fernandez H., Morin-Surruca M., Torre A., Faivre E., Deffieux X., Gervaise A. Ovarian drilling for surgical treatment of polycystic ovarian syndrome: a comprehensive review. Reprod Biomed Online. 2011;22(6):556–568. doi: 10.1016/j.rbmo.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 25.Watrelot A., Nisolle M., Chelli H., Hocke C., Rongières C., Racinet C. Is laparoscopy still the gold standard in infertility assessment? A comparison of fertiloscopy versus laparoscopy in infertility. Results of an international multicentre prospective trial: the “FLY” (Fertiloscopy-LaparoscopY) study. Hum Reprod Oxf Engl. 2003;18(4):834–839. doi: 10.1093/humrep/deg180. [DOI] [PubMed] [Google Scholar]
- 26.Franz M., Ott J., Watrelot A., Küssel L., Husslein H. Prospective evaluation of the learning curve of fertiloscopy with and without ovarian drilling. Reprod Biomed Online. 2015;30(4):408–414. doi: 10.1016/j.rbmo.2014.12.015. [DOI] [PubMed] [Google Scholar]
- 27.Shibahara H., Shimada K., Kikuchi K., Hirano Y., Suzuki T., Takamizawa S. Major complications and outcome of diagnostic and operative transvaginal hydrolaparoscopy. J Obstet Gynaecol Res. 2007;33(5):705–709. doi: 10.1111/j.1447-0756.2007.00636.x. [DOI] [PubMed] [Google Scholar]
- 28.Mercorio F., Mercorio A., Di Spiezio Sardo A., Barba G.V., Pellicano M., Nappi C. Evaluation of ovarian adhesion formation after laparoscopic ovarian drilling by second-look minilaparoscopy. Fertil Steril. 2008;89(5):1229–1233. doi: 10.1016/j.fertnstert.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 29.Felemban A., Tan S.L., Tulandi T. Laparoscopic treatment of polycystic ovaries with insulated needle cautery: a reappraisal. Fertil Steril. 2000;73(2):266–269. doi: 10.1016/s0015-0282(99)00534-8. [DOI] [PubMed] [Google Scholar]
- 30.Giampaolino P., Morra I., Tommaselli G.A., Di Carlo C., Nappi C., Bifulco G. Post-operative ovarian adhesion formation after ovarian drilling: a randomized study comparing conventional laparoscopy and transvaginal hydrolaparoscopy. Arch Gynecol Obstet. 2016;294(4):791–796. doi: 10.1007/s00404-016-4146-2. [DOI] [PubMed] [Google Scholar]
- 31.Zakherah M.S., Kamal M.M., Hamed H.O. Laparoscopic ovarian drilling in polycystic ovary syndrome: efficacy of adjusted thermal dose based on ovarian volume. Fertil Steril. 2011;95(3):1115–1118. doi: 10.1016/j.fertnstert.2010.10.037. [DOI] [PubMed] [Google Scholar]
- 32.Api M. Is ovarian reserve diminished after laparoscopic ovarian drilling? Gynecol Endocrinol Off J Int Soc Gynecol Endocrinol. 2009;25(3):159–165. doi: 10.1080/09513590802585605. [DOI] [PubMed] [Google Scholar]
- 33.Weerakiet S., Lertvikool S., Tingthanatikul Y., Wansumrith S., Leelaphiwat S., Jultanmas R. Ovarian reserve in women with polycystic ovary syndrome who underwent laparoscopic ovarian drilling. Gynecol Endocrinol Off J Int Soc Gynecol Endocrinol. 2007;23(8):455–460. doi: 10.1080/09513590701485212. [DOI] [PubMed] [Google Scholar]
- 34.Lunde O., Djøseland O., Grøttum P. Polycystic ovarian syndrome: a follow-up study on fertility and menstrual pattern in 149 patients 15-25 years after ovarian wedge resection. Hum Reprod Oxf Engl. 2001;16(7):1479–1485. doi: 10.1093/humrep/16.7.1479. [DOI] [PubMed] [Google Scholar]
- 35.Pouly J.-L., Krief M., Rabischong B., Brugnon F., Gremeau A.-S., Dejou L. [Ovarian drilling by fertiloscopy: feasibility, results and predictive values] Gynã©cologie Obs Fertil Sã©nologieâ. 2013;41(4):235–241. doi: 10.1016/j.gyobfe.2013.02.010. [DOI] [PubMed] [Google Scholar]
- 36.van Wely M., Bayram N., van der Veen F., Bossuyt P.M.M. An economic comparison of a laparoscopic electrocautery strategy and ovulation induction with recombinant FSH in women with clomiphene citrate-resistant polycystic ovary syndrome. Hum Reprod Oxf Engl. 2004;19(8):1741–1745. doi: 10.1093/humrep/deh319. [DOI] [PubMed] [Google Scholar]
- 37.Nahuis M.J., Oude Lohuis E., Kose N., Bayram N., Hompes P., Oosterhuis G.J.E. Long-term follow-up of laparoscopic electrocautery of the ovaries versus ovulation induction with recombinant FSH in clomiphene citrate-resistant women with polycystic ovary syndrome: an economic evaluation. Hum Reprod Oxf Engl. 2012;27(12):3577–3582. doi: 10.1093/humrep/des336. [DOI] [PubMed] [Google Scholar]
- 38.Farquhar C.M. An economic evaluation of laparoscopic ovarian diathermy versus gonadotrophin therapy for women with clomiphene citrate-resistant polycystic ovarian syndrome. Curr Opin Obstet Gynecol. 2005;17(4):347–353. doi: 10.1097/01.gco.0000175351.18308.3a. [DOI] [PubMed] [Google Scholar]
- 39.Farhi J., Soule S., Jacobs H.S. Effect of laparoscopic ovarian electrocautery on ovarian response and outcome of treatment with gonadotropins in clomiphene citrate-resistant patients with polycystic ovary syndrome. Fertil Steril. 1995;64(5):930–935. doi: 10.1016/s0015-0282(16)57904-7. [DOI] [PubMed] [Google Scholar]
- 40.van Wely M., Bayram N., Bossuyt P.M.M., van der Veen F. Laparoscopic electrocautery of the ovaries versus recombinant FSH in clomiphene citrate-resistant polycystic ovary syndrome. Impact on women’s health-related quality of life. Hum Reprod Oxf Engl. 2004;19(10):2244–2250. doi: 10.1093/humrep/deh406. [DOI] [PubMed] [Google Scholar]
- 41.Bayram N., van Wely M., van der Veen F., Bossuyt P.M.M., Nieuwkerk P. Treatment preferences and trade-offs for ovulation induction in clomiphene citrate-resistant patients with polycystic ovary syndrome. Fertil Steril. 2005;84(2):420–425. doi: 10.1016/j.fertnstert.2005.02.026. [DOI] [PubMed] [Google Scholar]
- 42.Rimington M.R., Walker S.M., Shaw R.W. The use of laparoscopic ovarian electrocautery in preventing cancellation of in-vitro fertilization treatment cycles due to risk of ovarian hyperstimulation syndrome in women with polycystic ovaries. Hum Reprod Oxf Engl. 1997;12(7):1443–1447. doi: 10.1093/humrep/12.7.1443. [DOI] [PubMed] [Google Scholar]
- 43.Eftekhar M., Deghani Firoozabadi R., Khani P., Ziaei Bideh E., Forghani H. Effect of laparoscopic ovarian drilling on outcomes of in vitro fertilization in clomiphene-resistant women with polycystic ovary syndrome. Int J Fertil Steril. 2016;10(1):42–47. doi: 10.22074/ijfs.2016.4767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cai J., Liu L., Sun L., Sha A., Jiang X., Ren J. Effects of previous ovarian drilling on cumulative ongoing pregnancy rates among patients with polycystic ovarian syndrome undergoing in vitro fertilization. Int J Gynaecol Obstet Off Organ Int Fed Gynaecol Obstet. 2016;134(3):272–277. doi: 10.1016/j.ijgo.2016.03.008. [DOI] [PubMed] [Google Scholar]
- 45.Qin J.Z., Pang L.H., Li M.J., Fan X.J., Huang R.D., Chen H.Y. Obstetric complications in women with polycystic ovary syndrome: a systematic review and meta-analysis. Reprod Biol Endocrinol RBE. 2013;11:56. doi: 10.1186/1477-7827-11-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kjerulff L.E., Sanchez-Ramos L., Duffy D. Pregnancy outcomes in women with polycystic ovary syndrome: a metaanalysis. Am J Obstet Gynecol. 2011;204(6):558. doi: 10.1016/j.ajog.2011.03.021. e1-6. [DOI] [PubMed] [Google Scholar]
- 47.Palomba S., de Wilde M.A., Falbo A., Koster M.P.H., La Sala G.B., Fauser B.C.J.M. Pregnancy complications in women with polycystic ovary syndrome. Hum Reprod Update. 2015;21(5):575–592. doi: 10.1093/humupd/dmv029. [DOI] [PubMed] [Google Scholar]
- 48.Abu Hashim H. Predictors of success of laparoscopic ovarian drilling in women with polycystic ovary syndrome: an evidence-based approach. Arch Gynecol Obstet. 2015;291(1):11–18. doi: 10.1007/s00404-014-3447-6. [DOI] [PubMed] [Google Scholar]
- 49.Baghdadi L.R., Abu Hashim H., Amer S.A.K., Palomba S., Falbo A., Al-Ojaimi E. Impact of obesity on reproductive outcomes after ovarian ablative therapy in PCOS: a collaborative meta-analysis. Reprod Biomed Online. 2012;25(3):227–241. doi: 10.1016/j.rbmo.2012.05.010. [DOI] [PubMed] [Google Scholar]
- 50.Ott J., Wirth S., Nouri K., Kurz C., Mayerhofer K., Huber J.C. Luteinizing hormone and androstendione are independent predictors of ovulation after laparoscopic ovarian drilling: a retrospective cohort study. Reprod Biol Endocrinol RBE. 2009;7:153. doi: 10.1186/1477-7827-7-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li T.C., Saravelos H., Chow M.S., Chisabingo R., Cooke I.D. Factors affecting the outcome of laparoscopic ovarian drilling for polycystic ovarian syndrome in women with anovulatory infertility. Br J Obstet Gynaecol. 1998;105(3):338–344. doi: 10.1111/j.1471-0528.1998.tb10097.x. [DOI] [PubMed] [Google Scholar]
- 52.Amer Sa.K., Li T.C., Ledger W.L. Ovulation induction using laparoscopic ovarian drilling in women with polycystic ovarian syndrome: predictors of success. Hum Reprod Oxf Engl. 2004;19(8):1719–1724. doi: 10.1093/humrep/deh343. [DOI] [PubMed] [Google Scholar]
- 53.Elmashad A.I. Impact of laparoscopic ovarian drilling on anti-Müllerian hormone levels and ovarian stromal blood flow using three-dimensional power Doppler in women with anovulatory polycystic ovary syndrome. Fertil Steril. 2011;95(7):2342–2346. doi: 10.1016/j.fertnstert.2011.03.093. 2346.e1. [DOI] [PubMed] [Google Scholar]
- 54.Sunj M., Canic T., Baldani D.P., Tandara M., Jeroncic A., Palada I. Does unilateral laparoscopic diathermy adjusted to ovarian volume increase the chances of ovulation in women with polycystic ovary syndrome? Hum Reprod Oxf Engl. 2013;28(9):2417–2424. doi: 10.1093/humrep/det273. [DOI] [PubMed] [Google Scholar]
- 55.van Wely M., Bayram N., van der Veen F., Bossuyt P.M.M. Predictors for treatment failure after laparoscopic electrocautery of the ovaries in women with clomiphene citrate resistant polycystic ovary syndrome. Hum Reprod Oxf Engl. 2005;20(4):900–905. doi: 10.1093/humrep/deh712. [DOI] [PubMed] [Google Scholar]
- 56.SAKS Amer, Li T.C., Cooke I.D. Repeated laparoscopic ovarian diathermy is effective in women with anovulatory infertility due to polycystic ovary syndrome. Fertil Steril. 2003;79(5):1211–1215. doi: 10.1016/s0015-0282(02)04960-9. [DOI] [PubMed] [Google Scholar]