ABSTRACT
Chronic intestinal pseudo-obstruction is a rare syndrome with high morbidity and mortality. The pathophysiology is not well understood, although it is postulated that it involves some sort of neuropathic and/or myopathic dysfunction resulting in intestinal dysmotility. We present the first case of chronic intestinal pseudo-obstruction secondary to a paraneoplastic syndrome associated with a primary small cell prostate cancer.
INTRODUCTION
Ileus and intestinal pseudo-obstruction refer to dysmotility syndromes that have signs, symptoms, and radiographic appearance of obstruction in the absence of a mechanical cause.1 Abdominal surgery is the most common cause of ileus with consequent longer hospitalizations and costs. Chronic intestinal pseudo-obstruction (CIPO) is characterized by chronic intestinal dilatation associated with severe dysmotility and nutrient malabsorption. The etiology can be multifactorial, including neuropathic and myopathic disorders and dysfunction of the interstitial pacemaker or cells of Cajal. Paraneoplastic CIPO due to anti-Hu serum antibodies is an uncommon and rarely encountered etiology, most commonly associated with lung small cell malignancies.
CASE REPORT
A 75-year-old man admitted to the hospital after 2 days of worsening abdominal distention, constipation, voiding difficulty, and loss of appetite. He was on rescue treatment with pembrolizumab because of progressive small cell prostate cancer. He had no previous abdominal surgeries. On physical examination, he had absent bowel sounds, moderate distention, and diffuse tenderness on palpation. The rectal vault was empty. Laboratory tests revealed acute kidney injury and hyperkalemia. Abdominopelvic computed tomography (CT) showed an under-distended colon, severe small bowel dilatation (greatest diameter 4.7 cm), and overdistended stomach (Figure 1). Positron emission tomography CT demonstrated liver metastasis and widespread lymphadenopathy. Medical therapy was implemented with intravenous fluids and bowel rest.
Figure 1.
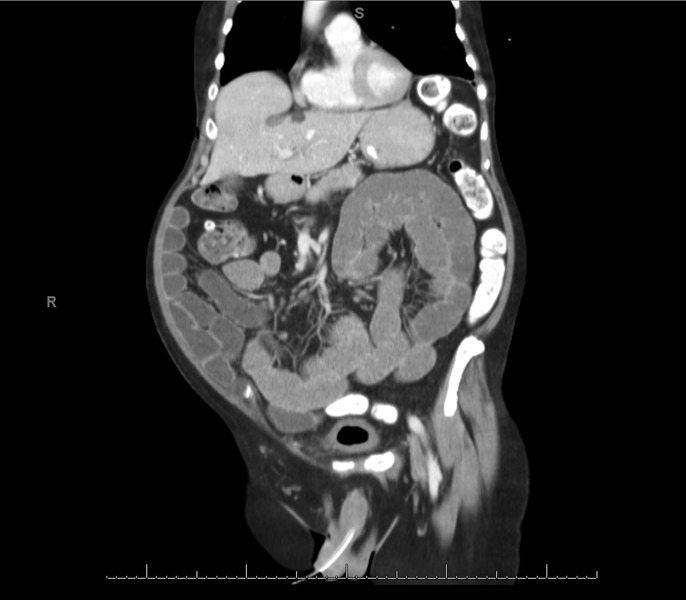
Severe small bowel dilatation and overdistended stomach.
Although the nasogastric tube was initially refused by the patient, he allowed its placement after 4 days of worsening symptoms, obtaining more than 5 L of fluid. The presumptive diagnosis was peritoneal carcinomatosis. The patient was transferred to the surgical intensive care unit because of tachycardia and new-onset leukocytosis. Repeated abdominopelvic CT excluded mechanical obstruction favoring pseudo-obstruction. A 24-hour erythromycin trial failed and had to be discontinued because of new-onset severe abdominal cramps. Total parenteral nutrition was initiated.
After 15 days without any significant improvement, a venting gastrostomy was placed as a comfort measure. A paraneoplastic syndrome was considered in view of the known advanced small cell cancer. Antineuronal antibodies (anti-Hu) were requested, which resulted markedly elevated (>1:640). The patient was subsequently transferred to the oncology ward to continue supportive medical treatment. Unfortunately, the patient died 6 weeks later.
DISCUSSION
Other than skin malignancy, prostate cancer is the most common cancer in American men.2 The American Urological Association states that over 95% of prostate cancers are adenocarcinomas, whereas small cell tumors account for less than 1%. Neuroendocrine cells are scattered throughout all the prostatic anatomical zones but comprise less than 1% of the glandular epithelium justifying the infrequent occurrence of this neoplasm.3 Because these tumors do not affect prostate-specific antigen levels, cancer screening strategies are less sensitive, and they are often discovered because of symptoms of advanced disease.4 Overall, the prognosis is poor with a disease‐specific mortality rate approaching 90% and a median disease-specific survival of 13.1 months.5
Paraneoplastic neurological syndromes are rare clinical manifestations caused by either altered immune response to a systemic malignancy or onconeuronal antibodies produced by tumors. These are more commonly associated with small cell lung cancer in up to 3%–5%.6 This is the first case, to our knowledge, of a primary prostate cancer producing a paraneoplastic syndrome targeting the gastrointestinal tract.
CIPO is an uncommon condition characterized by a marked derangement of gut propulsive motility mimicking mechanical obstruction in the absence of a lumen-occluding lesion.7 The estimated incidence ranges from 0.2 to 0.24 per 100,000 adults/yr.8 CIPO can progress to chronic intestinal failure because affected individuals are usually unable to meet daily nutritional requirements. Abnormalities in the neuromuscular apparatus involved in the complex coordination of effective gastrointestinal motility are believed to be the main pathophysiologic mechanism. Infections such as Chagas disease, radiotherapy to the abdomen, genetic disorders, and immune-mediated diseases have been associated.
The most common symptoms resemble bowel mechanical obstruction. Diagnosis is challenging for which a stepwise approach aimed at ruling out mechanical causes, identifying underlying diseases, and understanding that the pathophysiological features should be undertaken. In current clinical practice, CT is the preferred modality because it is more accurate at demonstrating air-fluid levels while ruling out mechanical causes.9 Screening tests for diabetes mellitus, neurotropic viruses (cytomegalovirus and Epstein-Barr), celiac disease, connective tissue and skeletal muscle disorders (antinuclear antibody, anti–double-stranded DNA, anti-topoisomerase I-70, creatine phosphokinase, and aldolase), and thyroid function should be performed.10 In very selected cases, CIPO has been associated with an underlying inflammatory neuropathy established by tissue analysis or by the identification of circulating anti-Hu antibodies usually seen in paraneoplastic syndromes. The antibody is postulated to be directed toward an epitope that is shared between the neuronal elements within the enteric nervous system and the underlying malignancy.11 A recent study described that anti-Hu antibodies act via excitatory effects with direct nerve activation through nicotinic receptors and activates mechanosensitive visceral afferents, which may explain the gut dysfunction.12
Current therapeutic approaches are not very effective, and this generates frustration in patients and physicians. Management of patients with CIPO is aimed at avoiding unnecessary surgery, restoring fluid and electrolyte balance, maintaining an adequate caloric intake, and symptom relief.10 Diarrhea secondary to small intestinal bacterial overgrowth has also been described, and treatment is warranted. Prokinetics, which seem to be the rational remedy, unfortunately fail to achieve an effective noninvasive decompression. Surgical options such as excision procedures and decompressive interventions such as gastrostomy placement usually provide a temporary relief and often result in a high rate of stoma prolapse along with a considerable risk of dehydration due to enteric fluid loss.13 In a recent study involving 7 patients with CIPO, placement of a gastrojejunostomy tube via percutaneous endoscopic gastrostomy demonstrated a significant improvement in abdominal symptoms, wasting, and malnutrition.14 Few reports include mild success with rituximab and B-cell–targeted chemotherapies after failed conventional treatment.15 The early treatment of the underlying malignancy offers the most favorable chance for improvement before irreversible neuronal damage ensues in cases of paraneoplastic CIPO.16
DISCLOSURES
Author contributions: C. Fernandez-Cruz, R. Estremera-Marcial, H. Pagan-Torres, and J. Martinez-Souss co-wrote the case report. DH Toro edited the manuscript and is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
REFERENCES
- 1.Foxx-Orenstein AE. Sleisenger and Fordtran's Gastrointestinal and Liver Disease, Chapter 124, Elsevier: New York, NY, 2171–95.e6. [Google Scholar]
- 2.American Cancer Society. Cancer Facts & Figures 2018. American Cancer Society, Atlanta, GA, 2018. [Google Scholar]
- 3.Parimi V, Goyal R, Poropatich K, Yang X. Neuroendocrine differentiation of prostate cancer: A review. Am J Clin Exp Urol. 2014;2(4):273–85. [PMC free article] [PubMed] [Google Scholar]
- 4.Deorah S, Rao MB, Raman R, Gaitonde K, Donovan JF. Survival of patients with small cell carcinoma of the prostate during 1973—2003: A population-based study. BJU Int. 2011;109:824–30. [DOI] [PubMed] [Google Scholar]
- 5.Spiess PE, Pettaway CA, Vakar-Lopez F, et al. Treatment outcomes of small cell carcinoma of the prostate: A single-center study. Cancer. 2007;110:1729–37. [DOI] [PubMed] [Google Scholar]
- 6.Dalmau J, Rosenfield MR. Paraneoplastic syndromes of the CNS. Lancet Neurol. 2008;7:327–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stanghellini V, Cogliandro RF, de Giorgio R, Barbara G, Salviolo B, Corinaldesi R. Chronic intestinal pseudo-obstruction: Manifestations, natural history and management. Neurogastroenterol Motil. 2007;19:440–52. [DOI] [PubMed] [Google Scholar]
- 8.Iida H, Ohkubo H, Inamori M, Nakajima A, Sato H. Epidemiology and clinical experience of chronic intestinal pseudo-obstruction in Japan: A Nationwide Epidemiologic Survey. J Epidemiol. 2013;23(4):288–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Merlin A, Soyer P, Boudiaf M, Hamzi L, Rymer R. Chronic intestinal pseudo-obstruction in adult patients: Multidetector row helical CT features. Eur Radiol. 2008;18:1587–95. [DOI] [PubMed] [Google Scholar]
- 10.Di Nardo G, Karunaratne TB, Frediani S, De Giorgio R. Chronic intestinal pseudo-obstruction: Progress in management? Neurogastroenterol Motil. 2017;29:e13231. [DOI] [PubMed] [Google Scholar]
- 11.Lennon VA, Sas DF, Busk MF, et al. Enteric neuronal autoantibodies in pseudoobstruction with small-cell lung carcinoma. Gastroenterology. 1991;100:137. [DOI] [PubMed] [Google Scholar]
- 12.Li Q, Michel K, Annahazi A, et al. Anti-Hu antibodies activate enteric and sensory neurons. Sci Rep. 2016;6:38216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sabbagh C, Amiot A, Maggiori L, Corcos O, Joly F, Panis Y. Non-transplantation surgical approach for chronic intestinal pseudo-obstruction; analysis of 63 adult consecutive cases. Neurogastroenterol Motil. 2013;25:680–6. [DOI] [PubMed] [Google Scholar]
- 14.Ohkubo H, Fuyuki A, Arimoto J, et al. Efficacy of percutaneous endoscopic gastro-jejunostomy (PEG-J) decompression therapy for patients with chronic intestinal pseudo-obstruction (CIPO). Neurogastroenterol Motil. 2017;29:E13127. [DOI] [PubMed] [Google Scholar]
- 15.Badari A, Farolino D, Nasser E, et al. A novel approach to paraneoplastic intestinal pseudo-obstruction. Support Care Cancer. 2012;20:425–8. [DOI] [PubMed] [Google Scholar]
- 16.Vedeler CA, Antoine JC, Giometto B, et al. Management of paraneoplastic neurological syndromes: Report of an EFNS Task Force. Eur J Neurol. 2006;13:682–90. [DOI] [PubMed] [Google Scholar]


