ABSTRACT
Fibrovascular polyps (FVPs) are rare, benign tumors of the esophagus; they usually appear as an intraluminal mass within the esophagus, which can grow and reach enormous sizes if left untreated. They can cause a variety of symptoms, from mild dysphagia to life-threatening asphyxia. Diagnosis is challenging because FVPs can resemble any respiratory condition, which can lead to misdiagnosis and potentially dangerous therapies. We present a 47-year-old man who suffered from recurrent episodes of odynophagia. This time he suffered an incident of severe asphyxia and loss of consciousness. After complementary examinations, an FVP was detected and successfully treated.
INTRODUCTION
Fibrovascular polyps (FVPs) are rare, benign lesions of the esophagus and represent less than 2% of esophageal tumors. They have a tendency to develop in the upper third of the esophagus, and due to their wide spectrum of behavior, they can appear as an incidental finding, to a giant mass in a severely ill patient with life-threatening asphyxia.1–4 Diagnosis is challenging because the symptoms can resemble any respiratory disease. Complete resection is the treatment of choice.5
CASE REPORT
A 42-year-old man without any significant medical history presented to the emergency department after suffering severe asphyxia which led to a brief loss of consciousness while swallowing liquids. The episode lasted a few minutes, and afterward, he regained full consciousness without any neurologic damage. After further investigation, we discovered that he had a 4-month history of brief but recurrent episodes of dysphagia for which he was treated with antihistamines and antibiotics assuming that it was a respiratory disease. No weight loss or other symptoms were detected.
Clinical examination was unremarkable, and due to his history, he was assessed by an otorhinolaryngologist. Laryngoscopy revealed a mass that protruded from the esophagus toward the glottis and obstructed almost the entire airway (Video 1; watch the video at http://links.lww.com/ACGCR/A10). A neck and chest contrast-enhanced computed tomography (CT) exposed the 5 × 5 × 2-cm soft-tissue density (100 Hounsfield units) intraluminal polypoid esophageal mass. During the first stage of the CT, the mass extended from the upper third of the esophagus into the hypopharynx; however, when the contrast was administered, the mass remained in the esophagus, revealing the great mobility of the polyp. No other masses or lymph nodes were recognized (Figure 1). On endoscopy, the whitish submucosal polyp was seen obstructing almost 50% of the esophageal lumen; it was pedunculated, mobile, and covered by an ulcer in its distal end (Figure 2).
Figure 1.
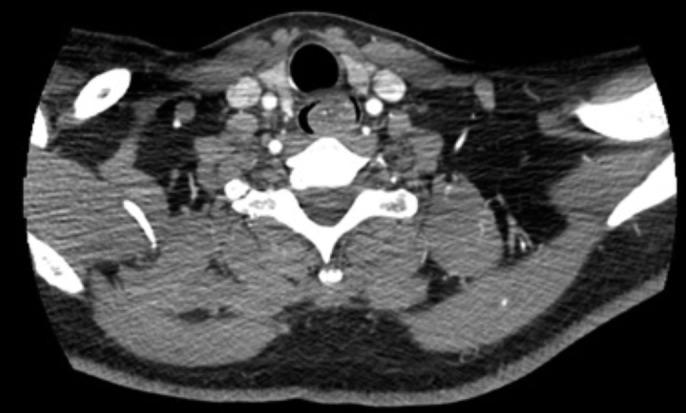
Contrast-enhanced computed tomography showing a mass with predominantly soft-tissue density in the upper third of the esophagus.
Figure 2.

Esophagogastroduodenoscopy showing a whitish, pedunculated, mobile submucosal mass covered with an apparent normal mucosa at the cricopharyngeal level.
Video 1.
Laryngoscopy showing a mass that protruded from the esophagus toward the glottis and obstructed almost the entire airway. Watch the video at http://links.lww.com/ACGCR/A10.
After a left cervicotomy, the esophagus was dissected and opened opposite to the base of the polyp; through this incision, the mass was completely resected with a 2 mm surgical margin, the esophagotomies were closed in a 2-layer fashion, a drain was left in place, and the remainder of the procedure was completed without any complications (Figure 3). Pathology reported an 8 × 2 × 1-cm pedunculated tumor lined by squamous epithelium with multiple ulcers and stroma composed mainly of adipocytes with areas of fibrovascular tissue. FVP of the esophagus was the final diagnosis (Figure 4).
Figure 3.
(A) Surgical picture showing complete resection of the fibrovascular polyp. (B) Surgical specimen after resection of an 8-cm pedunculated lesion and intraluminal mass.
Figure 4.
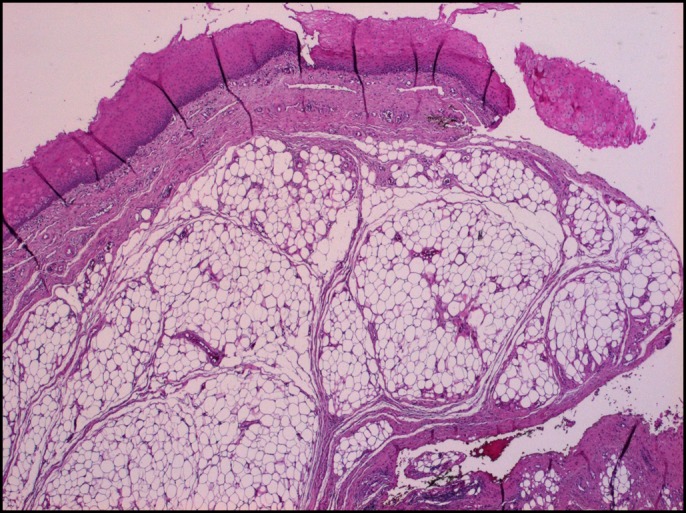
Hematoxylin and eosin stain (4×) of the fibrovascular polyp showing diffuse adipose tissue and extensive areas of a fibrovascular structure lined by squamous epithelium.
His postoperative course was uneventful; on his seventh postoperative day, an esophagogram ruled out an esophageal leak. Sips of liquids were initiated, and the drain was removed. After a full diet was established, the patient was discharged. On follow-up controls, the patient was completely asymptomatic, and he no longer had episodes of dysphagia.
DISCUSSION
Benign tumors of the esophagus are rare lesions that appear in 0.5% of the adult population.1 From both clinical and pathology viewpoints, benign tumors may be divided into 2 large groups: the intramural group and the intraluminal group. The intramural group consists of solid tumors or cysts, whereas the intraluminal group is formed by tumors that usually originate in the submucosa and develop in the lumen of the esophagus. They are usually covered with normal epithelium and are constituted of fibrous tissue with a rich vascular supply. Some are quite loose (myxoma, myxofibroma), others are more collagenous (fibroma), and some contain adipose tissue (fibrolipoma). These diverse group of tumors are frequently named as FVPs.6 FVPs tend to grow in the upper third of the esophagus.2,7
Up to 95% of FVPs are located behind the cricoid cartilage3,4; this zone is considered a weak region due to the fact that it does not have a posterior muscular structure; this combined with the excessive mucous folds in the area and the constant traction from the peristaltic activity of the esophagus aid in the formation of the polyps.3–5,8 FVPs can range from small lesions to bulky enormous masses that completely fill the esophageal lumen and compresses the trachea.1,9 Clinical presentation may be nonspecific and varied because the tumor grows very slowly; nonetheless, dysphagia, regurgitation, and weight loss are among the most common symptoms.10 Upper gastrointestinal bleeding, chest or abdominal pain, fever, and anemia, although rarer, have also been described in several case reports.11–14 In our case, the patient experienced episodes of respiratory symptoms, dysphagia, and finally an episode of severe asphyxia. Complementary tests aid in the diagnosis and are valuable in deciding the surgical approach.5,15 Magnetic resonance imaging is the best test to fully delineate this tumor as it gives better information on its location, volume, and anatomy. Nonetheless, CT, esophagogram, ultrasound, laryngoscopy, and esophagoscopy can also help in preoperative planning.4,8
In our patient, laryngoscopy was done, which revealed the mechanism by which FVP caused suffocation. In addition, a CT determined its location and size. Surgery is the treatment of choice, and complete excision must be achieved to avoid recurrence.16 Several approaches are available, and no matter which one is used, adequate visualization of the polyp, and its stalk, is vital as hemorrhage of the blood vessels in the pedicle must be avoided.1,14 Endoscopy is usually performed in small polyps with an identifiable stalk and excised with either a snare, stapler, ligature, laser, or ultrasonic technology.11,17,18 Larger lesions greater than 10 cm may be difficult to treat endoscopically and are better treated with an open approach.11,19,20 In our patient, open surgery was performed and complete resection was achieved. FVPs of the esophagus are rare, and due to broad clinical behavior, they can easily be misdiagnosed. In-depth knowledge of the esophageal pathology is required for all surgeons; this along with an appropriate history, an accurate physical examination, and complementary tests are vital to identify the underlying process and define its treatment.
DISCLOSURES
Author contributions: SA Endara wrote the manuscript and is the article guarantor. FB Corral, GA Molina, and WJ Cisneros wrote the manuscript. GA Davalos, RJ Yepez, and DF Luna collected the data and designed the report.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
REFERENCES
- 1.Bayram AS, Erol MM, Saraydaroglu O. Giant fibrovascular polyp of the esophagus—Case report. Indian J Thorac Cardiovasc Surg. 2004;20(2):104–5. [Google Scholar]
- 2.Choong C, Meyers BF. Benign esophageal tumors: introduction, incidence, classification, and clinical features. Semin Thorac Cardiovasc Surg. 2003;15(1):1–8. [DOI] [PubMed] [Google Scholar]
- 3.Zhang H, Nie RH. A rare case of giant fibrovascular polyp of the esophagus. Saudi Med J. 2015;36(11):1348–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Borges A, Bikhazi H, Wensel JP. Giant fibrovascular polyp of the oropharynx. Am J Neuroradiol. 1999;4:1979–82. [PMC free article] [PubMed] [Google Scholar]
- 5.Yannopoulos P, Manes K. Giant fibrovascular polyp of the esophagus—Imaging techniques can localize, preoperatively, the origin of the stalk and designate the way of surgical approach: A case report. Cases J. 2009;2(1):6854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vantrappen G, Pringot J. Benign tumors and cysts of the esophagus. In: Diseases of the Esophagus. Handbuch der inneren Medizin (Verdauungsorgane), vol 3 Springer: Berlin, Germany, 1974. [Google Scholar]
- 7.Ozcelik C, Onat S, Dursun M, Arslan A. Fibrovascular polyp of the esophagus: Diagnostic dilemma. Interact Cardiovasc Thorac Surg. 2004;3(2):260–2. [DOI] [PubMed] [Google Scholar]
- 8.Levine MS, Buck JL, Pantongrag-Brown L, Buetow PC, Hallman JR, Sobin LH. Fibrovascular polyps of the esophagus: Clinical, radiographic, and pathologic findings in 16 patients. AJR Am J Roentgenol. 1996;166:781–7. [DOI] [PubMed] [Google Scholar]
- 9.Rees CJ, Belafsky PC. Giant fibrovascular polyp of the esophagus. Ear Nose Throat J. 2007;86(10):606. [PubMed] [Google Scholar]
- 10.Cuk V, Knezevic-Usaj S, Ignjatovic M, et al. Giant esophageal fibrovascular polyp with clinical behaviour of inflammatory pseudotumor: A case report and the literature review. Vojnosanitetski Pregled. 2014;71(8):784–91. [DOI] [PubMed] [Google Scholar]
- 11.Valdivielso Cortázar E, Redondo Martínez J, Alonso Aguirre P. Giant fibrovascular polyp of the esophagus: A case report and diagnostic-therapeutic issues. Revista Española de Enfermedades Digestivas. 2018;111:251–2. [DOI] [PubMed] [Google Scholar]
- 12.Park J-S, Bang BW, Shin J, et al. A case of esophageal fibrovascular polyp that induced asphyxia during sleep. Clin Endosc. 2014;47(1):101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cockbain AJ, England R, Dexter SPL, Sarela AI. Surveillance is important after surgical excision of giant fibrovascular polyps of the esophagus. Ann Thorac Surg. 2017;104(4):e341–3. [DOI] [PubMed] [Google Scholar]
- 14.Pinto A, Abastado B, Cattan P. An esophageal tumor unlike others: The fibrovascular polyp. J Visc Surg. 2018. Published online December 20, 2018 (10.1016/j.jviscsurg.2018.11.009). [DOI] [PubMed] [Google Scholar]
- 15.Chourmouzi D, Drevelegas A. Giant fibrovascular polyp of the oesophagus: A case report and review of the literature. J Med Case Rep. 2008;2(1):337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lolley D, Razzuk MA, Urschel HC. Giant fibrovascular polyp of the esophagus. Ann Thorac Surg. 1976;22(4):383–5. [DOI] [PubMed] [Google Scholar]
- 17.Fries MR, Galindo RL, Flint PW, Abraham SC. Giant fibrovascular polyp of the esophagus. Arch Pathol Lab Med. 2003;127:485–7. [DOI] [PubMed] [Google Scholar]
- 18.Temes R, Quinn P, Davis M, et al. Endoscopic resection of esophageal liposarcoma. J Thorac Cardiovasc Surg. 1998;116(2):365–7. [DOI] [PubMed] [Google Scholar]
- 19.Ongkasuwan J, Anzalone C, Salazar E, Donovan D. Presentation and management of giant fibrovascular polyps of the hypopharynx and esophagus. Ann Otol Rhinol Laryngol. 2016;126(1):29–35. [DOI] [PubMed] [Google Scholar]
- 20.Sestini S, Gisabella M, Pastorino U, Billé A. Presenting symptoms of giant fibrovascular polyp of the oesophagus: Case report and literature review. Ann R Coll Surgeons Engl. 2016;98(5):e71–3. [DOI] [PMC free article] [PubMed] [Google Scholar]



