ABSTRACT
Breast cancer is the most common malignancy affecting women and has a high mortality rate. It commonly metastasizes to the skeletal and pulmonary systems. Rare reports have described breast cancer spreading to the gastrointestinal tract. We present a female patient diagnosed with and treated for primary lobular-type breast cancer, who developed recurrent bowel obstruction due to metastasis.
INTRODUCTION
Breast cancer is the most prevalent malignancy with estimated 252,710 new cases of invasive breast cancer in women in the United States in 2017. It is also the second most common cause of malignancy-related death after lung cancer in females with an expected mortality rate of 16%.1 Breast cancer commonly metastasizes to the bones and lungs, however, very rarely to the gastrointestinal (GI) tract.2 We report a rare case of diffuse ileocecal valve thickening leading to recurrent bowel obstruction from the metastasis of remotely treated breast cancer.
CASE REPORT
A 72-year-old woman presented with a medical history significant for lobular-type, positive estrogen and progesterone receptor, negative HER-2 receptor breast cancer, diagnosed in 2006. She was initially treated with mastectomy, adjuvant systematic chemotherapy, and tamoxifen for a total of 5 years, with successful remission and last mammogram in 2015. In 2016, she presented with complaints of abdominal pain, nausea, and vomiting. The patient was hemodynamically stable at the time of presentation.
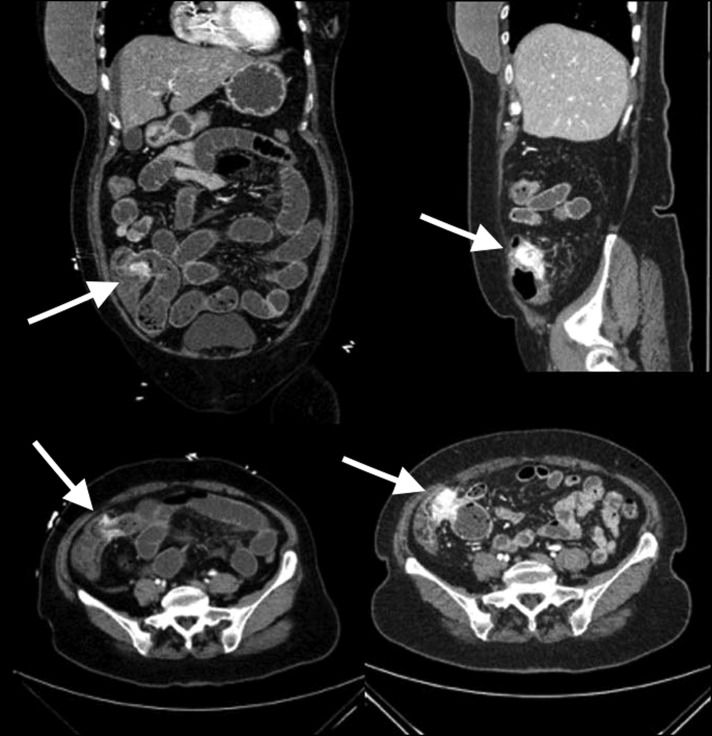
Computed tomography of the abdomen showed findings compatible with small bowel obstruction, and transition was seen at the ileocecal junction where there was focal mural thickening and avid contrast enhancement (Figure 1). The distal small bowel was fluid filled and showed intraluminal fecal debris. Colonoscopy was performed, which revealed thickened ileocecal valve and normal overlying mucosa. A biopsy obtained from the ileocecal valve showed lymphoid hyperplasia and was negative for malignancy (Figure 2). Conservative management improved her symptoms and the patient was discharged. However, 4 days later, the patient presented with recurrent symptoms of bowel obstruction. Computed tomography with enterography was obtained, which showed mass-like enhancement centered in the ileocecal valve causing stricture and small bowel obstruction (Figure 3). The patient underwent robotic-assisted right hemicolectomy and had an uncomplicated postoperative course.
Figure 1.

Initial abdominal computed tomography showing small bowel obstruction with transition at the ileocecal junction where there was focal mural thickening and avid contrast enhancement (arrow). The distal small bowel was fluid filled and showed intraluminal fecal debris.
Figure 2.
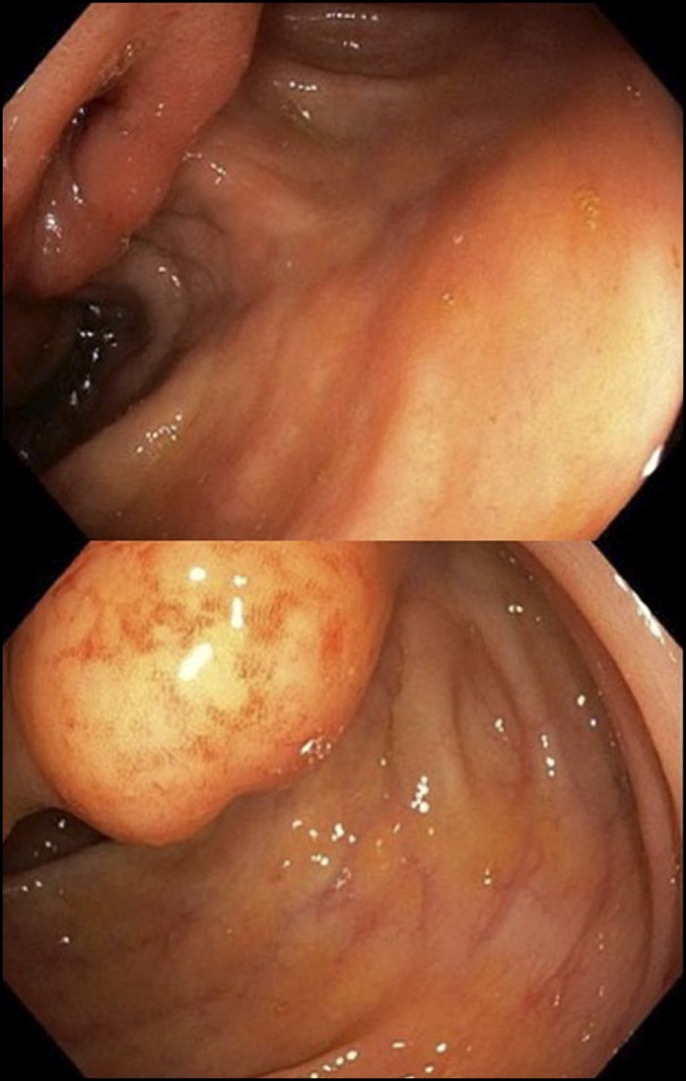
Colonoscopy showing a thickened ileocecal valve as seen in colonoscopy.
Figure 3.
Follow-up abdominal computed tomography with enterography showing a mass-like enhancement in the ileocecal area with obstruction (arrow).
Interestingly, surgical pathology results revealed signet ring cell adenocarcinoma involving ileocecal valve, terminal ileum, and right colon, positive for GATA-3 and negative for CDX2, consistent with metastasis from primary breast tumor of lobular type. Her metastasis was negative for hormonal receptor and HER-2. Unfortunately, the patient was lost to follow up after discharge from the hospital.
DISCUSSION
Breast cancer frequently metastasizes to skeletal and pulmonary systems, however, very rarely to the GI tract. Borst and Ingold reported a series of 2,600 cases of breast cancer with metastasis out of which 359 were lobular and 2,246 were ductal carcinoma. Among these cases, 4.5% in the lobular vs 0.2% in ductal carcinoma group developed GI tract metastasis. They concluded that there is no difference in the rate of metastasis between the ductal and lobular carcinoma to the lymph nodes, liver, and bones; however, lobular carcinoma tends to metastasize more to the GI tract in contrast to ductal carcinoma.3
McLemore et al reported 73 cases of breast cancer with GI or peritoneal metastasis after a retrospective review of all patients with breast cancer between 1985 and 2000. Out of these 73 patients, 23 had GI metastasis only, 32 had carcinomatosis only, and 18 were diagnosed with both. The GI metastasis rate was 8% to the esophagus, 28% to the stomach, 19% to the small intestine, and 45% to colon and rectum. The median interval between the diagnosis and metastasis presentation reported was 7 years, and the median survival was 28 months after the diagnosis. There was no survival benefit from palliative surgical intervention with some exception in special cases, and the only survival benefit was from the systemic chemotherapy or hormone therapy. Late presentation was associated with poor prognosis.4
Because of the late presentation and the similar signs and symptoms mimicking other GI disorders such as Crohn's disease and bowel obstruction from a hernia, diagnosis of tumor metastasis is very challenging. In most instances, accurate diagnosis will not be reached until surgical intervention takes place.5,6 Like in our patient who presented with upper GI tract obstruction symptoms with a transition point at the ileocecal valve, the colonoscopy failed to uncover the diagnosis. Even histologically, it is very challenging to come up with the final conclusion specifically with signet ring cells carcinoma type that can virtually arise from any tissue; however, most cases >90% arise from breast, stomach, and colon.7
GATA-3 is a transcription factor that is considered important for the differentiation of urothelial tissue, breast epithelia, and subsets of T lymphocytes.8 GATA-3 expression is found in up to 80%–90% of primary or metastatic breast cancers.8 Although CDX2 is known to be expressed by nuclei of cells of epithelial tissue throughout the intestine.9 Hence, negative CDX2 and positive GATA-3 favor the breast as origin over GI tract like in our case. In fact, to date, expression of CDX2 in breast cancer has been never reported.7,10
Santini et al presented a unique case of lobular breast cancer that metastasized to ileocecal valve after 5 years of diagnosis of the primary tumor. The diagnosis of the colonic metastasis was predicted by detecting an elevation of CA19-9, which is a marker of GI malignancy. Colonoscopy was then done, which showed an area of erythema that was biopsied. The biopsy result was consistent with epithelial mammary cancer. About 11 months later, the patient presented with bowel obstruction symptoms at the ileocecal valve. Interestingly, the metastasis was completely stable without peritoneal dissemination after 10 cycles of chemotherapy with capecitabine.11
There is still no consensus whether systemic hormonal vs chemotherapy along with surgery is more beneficial in terms of patient survival knowing the fact that patients usually have an extensive disease with multiple organs involved even though preoperative workup is negative.12 In cases of symptomatic obstruction, bleeding, or perforation, palliative surgical intervention is required even though no survival benefit may ensue. Only in a few instances such as patients with controlled primary tumor site surgical intervention might gain some survival benefits. Mourra et al reported that no individual with metastatic colon cancer regardless of the organ origin has survived beyond 5 years.13
In summary, metastasis to GI tract from breast cancer is a rare entity and not easy to diagnose. This diagnosis should be suspected when the patient has a history of breast cancer, especially of lobular type. Not surprisingly, in most cases, GI metastasis is part of widespread disease, and early diagnosis may help toward the improvement of the outcome. Involvement of surgeons early in such cases and earlier consideration of total or subtotal colectomy is a valuable learning point from our case.
DISCLOSURES
Author contributions: M. Sharbatji, S. Khalid, M. Wazir and AG Jain wrote the manuscript. U. Majeed reviewed the manuscript. AG Jain is article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
REFERENCES
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017;67(1):7–30. [DOI] [PubMed] [Google Scholar]
- 2.Colzani E, Johansson AL, Liljegren A, et al. Time-dependent risk of developing distant metastasis in breast cancer patients according to treatment, age and tumour characteristics. Br J Cancer. 2014;110(5):1378–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Borst MJ, Ingold JA. Metastatic patterns of invasive lobular versus invasive ductal carcinoma of the breast. Surgery. 1993;114(4):637–42 [PubMed] [Google Scholar]
- 4.McLemore EC, Pockaj BA, Reynolds C, et al. Breast cancer: Presentation and intervention in women with gastrointestinal metastasis and carcinomatosis. Ann Surg Oncol. 2005;12(11):886–94. [DOI] [PubMed] [Google Scholar]
- 5.Oyasiji T, Shoemake P, Bakhos C, Mansourian V. Small bowel obstruction from metastatic breast cancer masquerading as an obstructed incisional hernia. Conn Med. 2009;73(7):403–6. [PubMed] [Google Scholar]
- 6.Sato T, Muto I, Hasegawa M, et al. Breast signet-ring cell lobular carcinoma presenting with duodenal obstruction and acute pancreatitis. Asian J Surg. 2007;30(3):220–3. [DOI] [PubMed] [Google Scholar]
- 7.Chen YY. Immunostain Update: Diagnosis of Metastatic Breast Carcinoma, Emphasizing the Distinction from Gynecologic Cancers. UCSF Pathology Department, 2010. [Google Scholar]
- 8.Miettinen M, McCue PA, Sarlomo-Rikala M, et al. GATA3: A multispecific but potentially useful marker in surgical pathology: A systematic analysis of 2500 epithelial and nonepithelial tumors. Am J Surg Pathol. 2014;38(1):13–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Werling RW, Yaziji H, Bacchi CE, Gown AM. CDX2, a highly sensitive and specific marker of adenocarcinomas of intestinal origin: An immunohistochemical survey of 476 primary and metastatic carcinomas. Am J Surg Pathol. 2003;27(3):303–10. [DOI] [PubMed] [Google Scholar]
- 10.O'Connell FP, Wang HH, Odze RD. Utility of immunohistochemistry in distinguishing primary adenocarcinomas from metastatic breast carcinomas in the gastrointestinal tract. Arch Pathol Lab Med. 2005;129(3):338–47. [DOI] [PubMed] [Google Scholar]
- 11.Santini D, Altomare A, Vincenzi B, et al. An increase of CA 19.9 as the first clinical sign of ileocecal valve metastasis from breast cancer. In Vivo 2006;20(1):165–8. [PubMed] [Google Scholar]
- 12.López Deogracias M, Flores Jaime L, Arias-Camisón I, et al. Rectal metastasis from lobular breast carcinoma 15 years after primary diagnosis. Clin Transl Oncol. 2010;12(2):150–3. [DOI] [PubMed] [Google Scholar]
- 13.Mourra N, Jouret-Mourin A, Lazure T, et al. Metastatic tumors to the colon and rectum: A multi-institutional study. Arch Pathol Lab Med. 2012;136(11):1397–401. [DOI] [PubMed] [Google Scholar]