Abstract
Background: Depression is commonly treated with anti-depressant medication and/or psychological interventions. Patients with depression are common users of complementary therapies, such as acupuncture, either as a replacement for, or adjunct to, their conventional treatments. This systematic review and meta-analysis examined the effectiveness of acupuncture in major depressive disorder. Methods: A search of English (Medline, PsychINFO, Google Scholar, and CINAL), Chinese (China National Knowledge Infrastructure Database (CNKI) and Wanfang Database), and Korean databases was undertaken from 1980 to November 2018 for clinical trials using manual, electro, or laser acupuncture. Results: Twenty-nine studies including 2268 participants were eligible and included in the meta-analysis. Twenty-two trials were undertaken in China and seven outside of China. Acupuncture showed clinically significant reductions in the severity of depression compared to usual care (Hedges (g) = 0.41, 95% confidence interval (CI) 0.18 to 0.63), sham acupuncture (g = 0.55, 95% CI 0.31 to 0.79), and as an adjunct to anti-depressant medication (g = 0.84, 95% CI 0.61 to 1.07). A significant correlation between an increase in the number of acupuncture treatments delivered and reduction in the severity of depression (p = 0.015) was found. Limitations: The majority of the included trials were at a high risk of bias for performance blinding. The applicability of findings in Chinese populations to other populations is unclear, due to the use of a higher treatment frequency and number of treatments in China. The majority of trials did not report any post-trial follow-up and safety reporting was poor. Conclusions: Acupuncture may be a suitable adjunct to usual care and standard anti-depressant medication.
Keywords: depression, acupuncture, dosage, frequency
1. Introduction
Clinical depression is characterized by behavioral, cognitive, and emotional features and is recognised as a major public health problem that has a substantial impact on individuals and on society. Depressive disorders are common in the general population. In the United States, the lifetime prevalence of a major depressive disorder (MDD) has been reported at 20.6% [1]. Most depressed patients are treated in primary care and do not require hospitalisation. In primary care, guidelines suggest depression is primarily managed with antidepressants [2]. A range of psychological interventions, including cognitive behavioural therapies, interpersonal therapy, psychotherapy, and counseling, are also recommended treatment options [3]. When patients fail to respond to a single modality, adjunctive or combined pharmacological and/or psychological treatments are recommended. However, around 30% may remain non responsive or partially responsive, even with augmentation [2].
Alternative approaches, such as complementary and alternative medicine (CAM), are frequently used in people with depression [4,5,6], either as an adjunct or replacement [4] for conventional therapies.
Contemporary acupuncture practice is commonly undertaken as part of the medical hospital system in modern China [7] and with provision either in hospital or in private practice in the United Kingdom [8]. Traditionally, acupuncture involves the insertion of fine needles into specific points, called acupuncture points, on the body to achieve a therapeutic effect. Following insertion, needles can be stimulated by hand (called ‘manual acupuncture’), or via the application of a small electrical current (called ‘electro-acupuncture’). A modern alternative is laser acupuncture, a non-penetrative form of acupuncture that uses low-power laser light to stimulate acupuncture points.
Current models of depression suggest that changes in the hypothalamic–pituitary–adrenal (HPA) axis, dysfunction among stress hormones, and disequilibrium in neurotransmitters, such as noradrenaline, serotonin, and dopamine, may be key factors in the onset and maintenance of major depressive disorder [9]. Results from animal experiments suggest a multitarget antidepressant effect of acupuncture, which may be related to amino acid metabolism and inflammatory pathways, especially the Toll-like receptor signaling pathway, tumor necrosis factor (TNF) signaling pathway, and nuclear factor kappa light chain enhancer of activated B cells (NF-kappa B) signaling pathway [10]. In addition, similar to antidepressant medications, acupuncture is capable of affecting the neurotransmitter levels of serotonin and noradrenaline, along with the adenylate cyclase cyclic adenosine monophosphate-protein kinase A (AC-cAMPPKA) cascade within the central nervous system [11].
A ‘dose’ of acupuncture is made up of multiple components. The exact components of a dose differ slightly between authors but consist of: (a) a neurophysiological dose, which includes the number of needles used, the retention time, and the type of stimulation used on the needles, and (b) a cumulative dose, made up of the frequency and total number of treatments [12,13,14]. Previous research has shown that changing the components of the acupuncture ‘dose’ appears to change the therapeutic outcomes in women undergoing in-vitro fertilization (IVF) [15] and period pain [12,16], with functional MRI (fMRI) studies showing that differing doses modulate brain activity differently [17]. Our recent Cochrane review on acupuncture for the treatment of depression [18] showed some evidence of benefits but did not explore the contribution of different dose components on the clinical outcomes for depression, for example, the number and frequency of acupuncture sessions provided.
The aim of this study was to examine the effectiveness of acupuncture compared to usual care (treatment as usual), compared to sham or placebo acupuncture, to a psychological intervention, and as an adjunct to selective serotonin reuptake inhibitors (SSRI) or serotonin and norepinephrine reuptake inhibitors (SNRI) medication. Based on a careful review of the existing literature, this study appears to be the first to explore the effect of variations in common dosage components on depression-related outcomes.
2. Methods
2.1. Search Strategy
The databases searched included:
English: Medline, PsychINFO, Google Scholar, and CINAL.
Chinese: China National Knowledge Infrastructure Database (CNKI) and Wanfang Database.
Korean: the Korean Studies Information Service System (KISS), DBPIA, Korea Institute of Science and Technology Information, Research Information Service System (RISS), Korea Med, Korean Medical Database (KM base), and Oriental Medicine Advanced Searching Integrated System (OASIS).
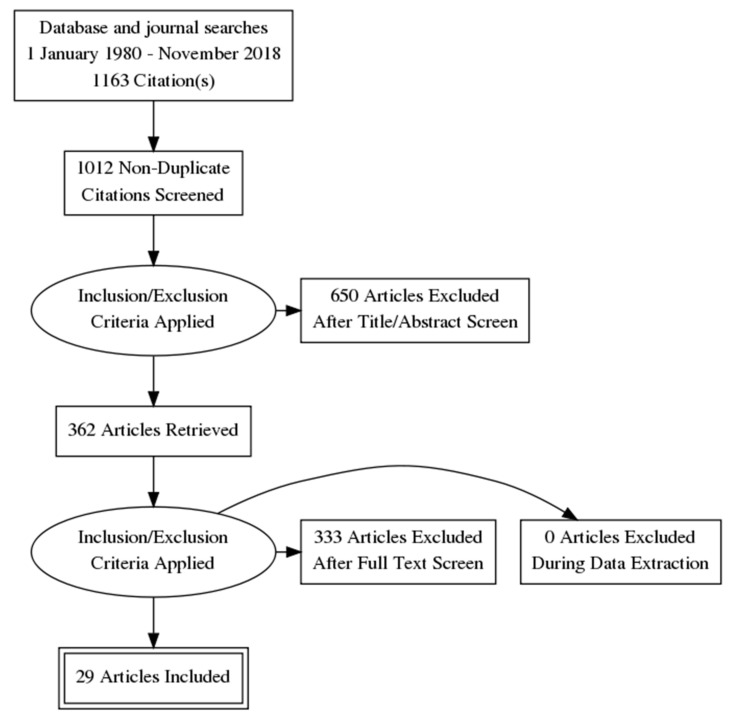
All databases were searched from 1 January 1980 to the end of November 2018, using the keywords (acupunct* or acupress* or acupoints* or electroacupunct* or electro-acupunct* or auriculotherap* or auriculoacupunct* or moxibust*) and (depress* or “affective disorder*” or “affective symptoms” or mood) using the Boolean ‘AND/OR’ operators. These keywords were the same as our recent Cochrane review of depression [18]. Both MESH and Non-MESH terms were included in this search. Papers that either had English full text, Korean full text, or Chinese full text available were eligible. Reference lists of full text papers were searched, and any relevant articles identified were screened. Figure 1 outlines the search process.
Figure 1.
PRISMA flow diagram.
2.2. Eligibility Criteria
We included participants with clinical depression. Depression needed to be the primary condition rather than a co-morbidity. We included studies of people of any gender and of any ethnicity, aged 16 years or above, with clinically diagnosed depression, where depression was diagnosed via one or more of the following of the following criteria: depression defined by the Diagnostic and Statistical Manual (DSM-III, DSM-IV or DSM 5) [19,20,21], the International Classification of Disease (ICD-10) [22], the Criteria for Classification and Diagnosis of Mental Diseases (CCMD-2 or CCMD-3) [23,24], the Clinical Interview Schedule—Revised [25], or using the Beck Depression Inventory [26].
For the purposes of this review, eligible interventions comprised of manual acupuncture, electro acupuncture, or laser acupuncture. Eligible comparator groups were:
Usual care: This varies depending on geographical location and patient preference and for many participants is likely to incorporate SSRI or SNRI classes of anti-depressant medication;
- Sham acupuncture or placebo acupuncture, which could consist of any of the following:
- Invasive acupuncture control: This includes the insertion of acupuncture needles into either ‘non-acupuncture points’, or acupuncture points that are assumed to be unrelated to the treatment of depression. Needles may be inserted superficially or to regular depths;
Acupuncture plus SSRI/SNRI medication: To reflect clinical practice in western countries, where clinical guidelines are unlikely to recommend acupuncture alone as an alternative to SSRI/SNRI medication or to recommend older tri-cyclic antidepressants (TCAs) [2,3], only trials comparing acupuncture as an adjunct to SSRI or SNRI medication were eligible. For clinical relevance, trials using medication that is no longer in use (such as Flupentixol/melitracen) were not eligible;
Psychological intervention, such as cognitive behavioural therapy (CBT), psychotherapy, or counseling.
For inclusion, outcome measures needed to include either a validated clinician rated measure of depression severity (such as the Hamilton Rating Scale for Depression (HAMD)) or a participant-reported measure, such as the Beck Depression Inventory (BDI) or Patient Health Questionnaire (PHQ-9). Cross over trials were excluded due to uncertainty regarding the period to allow for a washout for acupuncture treatment.
2.3. Data Extraction
Two authors extracted the data independently and a third author (MA or CS) resolved any disagreement. Where data was missing or unclear, the study authors were contacted via email by the authors to request the missing data be provided. Authors were contacted twice over a six-week period. If no response was received in that time, the data was marked as missing. One author (HM) was an author on an included study. HM had no part in the screening or data extraction of this study.
Data were extracted on all of the following outcomes (if reported):
-
-
Severity of depression at the end of the intervention;
-
-
Severity of depression at follow-up (short term, medium term, and long term);
-
-
Adverse events.
Where there were two or more ‘sham’ arms used in a single study, where one or more arms were ‘invasive’, such as using minimal needling of acupuncture points, then the non-invasive arm (e.g., using a park device) was chosen, as it was expected to have less activity compared to invasive needling [29].
When multiple data points were available post intervention (e.g., end of intervention or one month follow up), end of intervention data were used as the primary time point. If follow-up data were available, they were categorised into short term (less than or equal to three months), medium term (over three and up to six months), and long term (over six months). Where there were multiple eligible intervention groups, data were combined from active treatment arms into one group, as per the Cochrane guidelines [30]. When multiple scales were used for the severity of depression, if both clinician and participant reported scales were present, priority was given to clinician reported outcomes.
2.4. Risk of Bias
Included studies were also assessed using the Cochrane Collaboration’s risk-of-bias tool [30], as per our previous review [31]. Any disagreements were resolved by discussion.
2.5. Acupuncture Quality
The quality of the acupuncture delivered in the included trials was assessed using the National Institute for Complementary Medicine Acupuncture Network (NICMAN) scale. [32] This recently developed tool is reliable and is recommended to be used in conjunction with the Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) checklist [33]. The NICMAN consists of 11 items and is scored out of 23, with four main domains of appraisal:
-
(1)
Population Intervention Comparator Outcome measure (PICO) reporting, study design relevance, and paradigm based differential diagnosis (items 1–6);
-
(2)
Acupuncture point selections and locations, in reference to published literature (items 7 and 9);
-
(3)
Description of the needle dimensions, needling technique, and number of treatments (items 8 and 10);
-
(4)
Acupuncturist qualification and training (item 11).
Higher scores on the NICMAN scale are associated with an increase in the quality of the acupuncture intervention delivered. NICMAN scores were assessed by two authors independently, with any disagreement resolved by a third author (MA or CS).
2.6. Meta-Analysis
Random-effects meta-analyses were conducted using the Comprehensive Meta-Analysis software (Version 3). Intervention effect sizes were pre-post changes between intervention and control groups for the primary outcome measure (change in severity of depression) and were calculated using Hedges’ g statistic [34], along with 95% confidence intervals (CIs) around the estimated effect-size. For more details, please refer to our previous study [31].
2.7. Subgroup Analysis
The following sub-group analyses were decided on a priori:
-
-
Comparison between different acupuncture subtypes (manual, electro-acupuncture, and laser acupuncture)*;
-
-
Needle retention time* (<20 min versus >20 min);
-
-
Fixed versus individualised acupuncture.
Those sub-group analyses marked with a * indicate that these are components of acupuncture ‘dosage’. A postori, a decision was made to examine if cultural or geographical factors might influence the response to acupuncture treatment, so a sub-group analysis between studies conducted in China versus countries other than China was undertaken.
Variations in dose components (such as total number of treatments) between China compared to countries other than China will be explored via t-test for normally distributed data or a Mann–Whitney U test for non-normally distributed data.
If the frequency of treatment varied over the course of treatment (e.g., twice per week for the first week, then once per week for eight weeks), the frequency used in analysis was the average frequency calculated over the course of treatment. For studies that reported a treatment frequency of every second day, a treatment frequency of 3.5 treatments per week was used in the analysis. In studies where there was semi-standardised or individualised treatment, the number of acupuncture points was determined by either the minimum number that was required by the study protocol (excluding any optional points), or the average number of points used by practitioners, if this was reported in the manuscript. If both were reported, then preference was given to the average number of points used.
The relationship between continuous moderators and estimates of effect size were explored with a meta-regression analysis. These were performed for characteristics of acupuncture dosage that may have had an impact on the severity of depression—the frequency of treatment, the total number of treatments, the number of acupuncture points used—and for the quality of the acupuncture delivered, determined by the NICMAN scale score.
3. Results
A total of 29 studies including 2268 participants were included in this review. Table 1 outlines the characteristics of the included studies.
Table 1.
Summary of included studies.
| Study ID | Country | Sample Size | Diagnosis for Inclusion d | Intervention | Control | Number of Treatments | Frequency of Treatment | Variation in Acupuncture Points | Total Number of Acupuncture Points (for Fixed Points Only) | Outcome Measures | NICMAN Score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Allen 1998 [62] | USA | 17 a | DSM IV | Manual acupuncture | Invasive (Non-specific) | 12 | 2/week then 1/week | Fixed | NR c | HAMD | 21 |
| Allen 2006 [63] | USA | 74 a | DSM-IV | Manual acupuncture | Invasive (Non-specific) | 12 | 2/week then 1/week | Individualised | N/A | HAMD | 23 |
| Andreescu 2011 [52] | USA | 45 | DSM IV | Electro acupuncture | Sham | 12 | 2/week | Fixed | 2 | HAMD | 21 |
| Chung 2015 [53] | Hong Kong | 60 a | DSM IV | Electro acupuncture | Sham | 9 | 3/week | Fixed | 4 | HAMD | 19 |
| Duan 2008 [38] | China | 35 | CCMD | Electro acupuncture + Fluoxetine 20 mg | Fluoxetine 20 mg | 36 | 6/week | Semi-fixed | N/A | HAMD | 16 |
| Duan 2011 [39] | China | 60 | ICD | Electro acupuncture + Fluoxetine 20 mg | Fluoxetine 20 mg | 36 | 6/week | Semi-fixed | N/A | HAMD | 16 |
| Fan 2005 [54] | China | 39 a | CCMD-2 | Manual acupuncture | Sham | NR c | NR c | Fixed | 4 | HAMD | 7 |
| Fu 2008 [55] | China | 176 a | CCMD-2 | Manual acupuncture | Sham | 24 | 2/week | Fixed | 4 | HAMD | 14 |
| Huang 2013 [40] | China | 60 | CCMD | Manual acupuncture + Paroxetine 20–40 mg | Paroxetine 20–40 mg | 18 | 3–4/week | Fixed | 6 | HAMD | 10 |
| Huang 2018 [41] | China | 80 | ICD-10, CCMD-3 | Manual acupuncture + Paroxetine, Sertraline, Citalopram, Fluoxetine (dosage NR c) | Paroxetine, Sertraline, Citalopram, Fluoxetine (dosage NR c) | 20 | 5/week | Fixed | 6 | HAMD, SF-36, TESS | 19 |
| Li 2008 [56] | China | 52 | CCMD-2 | Manual acupuncture | Sham | 24 | 2/week | Fixed | 4 | HAMD | 12 |
| Lin 2012 [35] | China | 92 b | ICD | 1. Electro acupuncture 2. Manual acupuncture + Paroxetine (dosage NR c) |
Paroxetine (dosage NR c) | 18 | 3–4/week | 1. Fixed 2. Semi-fixed |
1. 2 2. N/A |
HAMD | 11 |
| Liu 2013 [44] | China | 90 | CCMD-3 | Manual Acupuncture + Fluoxetine or Paroxetine (dosage NR c) | Fluoxetine or Paroxetine (dosage NR c) | 14 | 3–4/week | Fixed | 5 | HAMD | 7 |
| Liu 2015 [43] | China | 90 | CCMD-3 | Manual acupuncture + Fluoxetine, paroxetine, citalopram 20–60 mg, sertraline 50–200 mg or fluvoxamine 50–300 mg | Fluoxetine, paroxetine, citalopram 20–60 mg, sertraline 50–200 mg or fluvoxamine 50–300 mg | 14 | 3–4/week | Semi-fixed | N/A | HAMD | 15 |
| Liu 2017 [42] | China | 91 | ICD-10 | Manual acupuncture + Venlafaxine 75–225 mg | Venlafaxine 75–225 mg | 40 | 5/week | Fixed | 8 | HAMD | 15 |
| MacPherson 2013 [36] | UK | 755 | BDI | Manual acupuncture + usual care | 1.Counseling + usual care 2. Usual care |
12 | 1/week | Individualised | N/A | PHQ-9 | 20 |
| Meng 2016 [45] | China | 60 | CCMD-3 | Manual acupuncture + Fluoxetine (2 tablets dosage NR c) | Fluoxetine (2 tablets dosage NR c) | 28 | 7/week | Semi-fixed | N/A | HAMD | 16 |
| Qu 2013 [37] | China | 160 b | ICD | 1. Electro acupuncture 2. Manual acupuncture + Paroxetine 10–40 mg |
Paroxetine 10–40 mg | 18 | 3/week | Fixed | 7 | BDI | 19 |
| Quah-Smith 2005 [58] | Australia | 26 | BDI | Laser acupuncture | Sham | 12 | 2/week then 1/week | Individualised | N/A | HAMD | 19 |
| Quah-Smith 2013 [57] | Australia | 37 | DSM IV | Laser acupuncture | Sham | 12 | 2/week then 1/week | Fixed | 5 | HAMD | 21 |
| Wang 2014 [46] | China | 71 | ICD | Manual acupuncture + Fluoxetine 20 mg, paroxetine 20 mg or duloxetine 40 mg | Fluoxetine 20 mg, paroxetine 20 mg or duloxetine 40 mg | 30 | 5/week | Semi-fixed | N/A | HAMD | 19 |
| Whiting 2008 [59] | UK | 17 | CISR | Manual acupuncture | Sham | 12 | NRc | Semi-fixed | N/A | HAMD | 19 |
| Xu 2011 [47] | China | 40 | CCMD | Manual + Electro acupuncture combined + Citalopram, paroxetine or fluoxetine 20 mg | Citalopram, paroxetine or fluoxetine 20 mg | 18 | 3/week | Fixed | 7 | HAMD | 9 |
| Yeung 2011 [60] | Hong Kong | 39 a | DSM-IV | Electro acupuncture | Sham | 9 | 3/week | Fixed | 8 | HAMD | 17 |
| Yin 2018 [61] | China | 64 | CCMD-3, DSM-IV | Manual acupuncture | Sham | 24 | 3/week | Fixed | 10 | HAMD | 18 |
| Zhang 2007 [48] | China | 42 | CCMD | Electro acupuncture + Paroxetine 10–40 mg | Paroxetine 10–40 mg | 36 | 7/week | Semi-fixed | N/A | HAMD | 14 |
| Zhu 2017 [49] | China | 61 | CCMD-3 | Manual acupuncture + Fluoxetine, paroxetine, fluvoxamine, sertraline, citalopram, estalcitalopram (dosage NR c) | Fluoxetine, paroxetine, fluvoxamine, sertraline, citalopram, estalcitalopram (dosage NR c) | 30 | 5/week | Semi-fixed | N/A | HAMD | 19 |
| Zhu 2018 [50] | China | 67 | CCMD-3 | Manual acupuncture + SSRI (Type and dosage NR c) | SSRI (Type and dosage NR c) | 30 | 5/week | Semi-fixed | N/A | HAMD | 20 |
| Zhu 2018 [51] | China | 70 | ICD-10 | Manual acupuncture + Sertraline (dosage NR c) | Sertraline (dosage NR c) | 40 | 5/week | Semi-fixed | N/A | HAMD | 21 |
a Three-armed trial, only eligible arms included in sample size. b Three-armed trial, both intervention arms eligible and included. c NR = Not reported. d DSM = Diagnostic and Statistical Manual (DSM-III, DSM-IV or DSM 5), ICD-10 = International Classification of Disease, CCMD, CCMD-2, CCMD-3 = Criteria for Classification and Diagnosis of Mental Diseases, CISR = Clinical Interview Schedule—Revised, BDI = Beck Depression Inventory.
3.1. Design
A parallel group design was used in all trials. Twenty-six trials had two eligible groups (acupuncture plus a control group). Three trials [35,36,37] had three eligible arms, where the unit of analysis was adjusted based on the description in the methods.
3.2. Control Groups
Control groups varied between studies dependent on the research question. Sixteen trials [35,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51] used SSRI or SNRI medication alone as the control. Twelve trials used an acupuncture control, with nine trials using sham acupuncture [52,53,54,55,56,57,58,59,60,61] and two trials [62,63] using an invasive control. One trial [36] of acupuncture plus usual care had two control groups, one of counseling plus usual care and one usual care alone.
3.3. Country
Twenty-two studies were undertaken in Chinese speaking countries (20 in mainland China and two in Hong Kong), and seven in English speaking countries (three in the United States of America, two in Australia, and two in the United Kingdom).
3.4. Sample Sizes
Sample sizes of trials included in this review ranged from 19 [59] to 755 [36], with an overall median of 60. Trials undertaken in Chinese speaking countries had a median sample size of 61, while those in English speaking countries had a median sample size of 37.
3.5. Participant Criteria
Trials recruited participants who met the diagnostic criteria for depression or who had a clinical presentation of depression, as defined by the trial authors. All trials recruited participants with major depressive disorder. Seven trials used the Diagnostic and Statistical Manual of Mental Disorders (DSM-II, III, IV or V), 11 trials used the Chinese Classification of Mental Disorders (CCMD-2 or 3), six trials used the Criteria for Diagnosis of Depression (ICD-10), two trials used the Beck Depression Inventory (BDI), and one trial used the Clinical Interview Schedule-Revised (CIS-R). One trial used both the CCMD-3 and ICD-10 [41], and one trial used both the CCMD-3 and DSM-IV [61].
3.6. Interventions
The acupuncture delivered in the trials varied in terms of point selection, frequency of treatments, and total number of treatments administered.
3.6.1. Type of Acupuncture
Eighteen trials used manual acupuncture, six trials used electro acupuncture, two trials used laser acupuncture, two trials included both manual and electro acupuncture arms, and one trial combined electro and manual acupuncture.
3.6.2. Frequency of Treatment
The frequency of acupuncture treatment ranged from daily to approximately once per week. Overall, 19 trials used acupuncture treatment three times a week or more, three trials used acupuncture treatment twice per week [52,55,56], five trials used acupuncture treatment once a week on average [36,57,58,62,63]. The frequency of acupuncture treatment was unclear in two trials [54,59]. In English speaking countries, the median frequency of treatments was once per week, while in Chinese speaking countries, the median frequency was treatment every second day (3.5 treatments per week). The median frequency of treatments delivered in China was significantly greater (U = 1, p < 0.00061).
3.6.3. Total Number of Treatments
The total number of acupuncture treatments ranged from nine treatments [53,60] to 40 treatments [42], with a median of 18 treatments, in the included studies. The total number of acupuncture treatments was unclear in one trial [54]. All trials in English speaking countries delivered 12 treatments, with trials undertaken in Chinese speaking countries delivering a median of 24 treatments. The median number of treatments delivered in China was significantly greater (U = 14, p = 0.0006).
3.6.4. Duration
The total duration of acupuncture treatments ranged from three weeks [53,60] to 12 weeks [36,55,56], with a median treatment duration of six weeks, in the included studies. The total duration of treatment was unclear in one trial [59].
3.6.5. Treatment Protocol
Fifteen trials used a standardised treatment protocol, with a fixed selection of points administered at each acupuncture session. The selection of points varied and included acupuncture points located on the arms, legs, abdomen, and head. Eleven trials used a semi-standardised treatment protocol consisting of semi-fixed points, including a pre-defined set of points used in combination with points selected on the basis of diagnosis and symptomatic patterns. Three trials used an individualised treatment protocol, with individual points selected on the basis of diagnosis and symptomatic patterns. Of the 15 trials using fixed points, the number of acupuncture points ranged from ten points [61] to two points [35,52], with a median number of six points. The number of acupuncture points was not reported in one of the trials using fixed points [62].
3.6.6. Needle Retention Times
The needle retention times ranged from 20 min [59,63] to 60 min [38,39]. Overall, 20 trials used a needle retention time of 30 min or less, and four trials used a needle retention time of more than 30 min. In five trials, the needle retention time was determined as unclear.
3.6.7. NICMAN Scores
NICMAN scores ranged from 7 [44,54] to 23 [63]. The median NICMAN score was 18.
3.7. Outcome Measures
Twenty-seven trials assessed the primary outcome of depression using the Hamilton Rating Scale for Depression (HAMD) [64], one trial [37] used the Beck Depression Inventory (BDI) [26], and one trial [36] used the PHQ-9 [65]. Only two trials [36,61] collected data for post-treatment follow-up, all others collected data to the end of the intervention. Seven studies reported adverse events. Four studies reported adverse event counts only [52,59,60,66], two used the Asberg Side Effect Rating Scale (SERS) scale and one used the Toxic Exposure Surveillance System (TESS) [38].
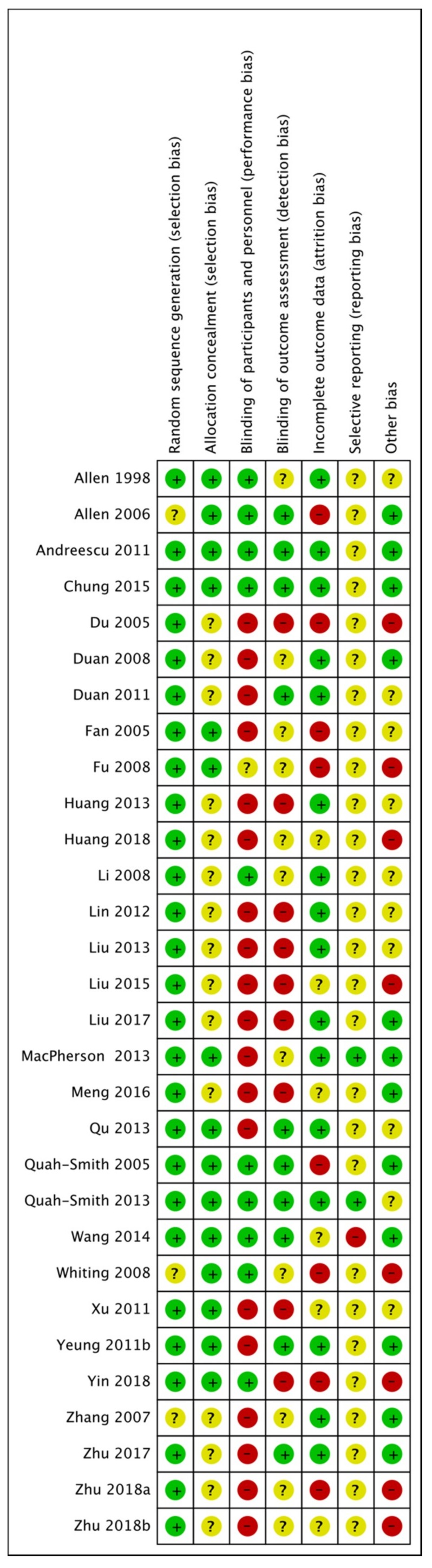
3.8. Risk of Bias in Included Studies
See Figure 2 for a graphical summary of risk of bias assessments performed by review authors for the 29 included studies, based on the seven risk-of-bias domains. No trials were assessed as having a low risk-of-bias across all domains. Three trials were at low risk-of-bias for six domains [52,53,57] and four trials were at low risk-of-bias for five domains [36,46,58,60]
Figure 2.
Risk-of-bias. Green, low risk of bias; yellow, unclear risk of bias; red, high risk of bias.
3.8.1. Randomization
Twenty-six trials were at a low risk of bias for randomization and three trials did not describe the method of randomization or were assessed as unclear [48,59,63].
3.8.2. Allocation
Fourteen trials were assessed as low risk of bias for allocation concealment. The remaining 15 trials did not report the method of allocation, so we assessed their risk as unclear.
3.8.3. Blinding
We assessed blinding as providing a low risk of performance bias in ten trials. For studies comparing acupuncture versus a sham or placebo acupuncture control, we sought evidence of verification of the blinding of participants, such as tests of blinding being reported. Most trials involved comparisons of acupuncture versus usual care or medication and participants could not be blinded; this contributed to an assessment of high risk. We assessed a total of 18 trials as having a high risk for performance bias and one trial as being unclear.
Most trials used clinician rated outcome measures. Ten trials were rated as having a low risk of detection bias, nine trials as high risk and the remaining ten did not report on blinding of the assessor/clinician, the analyst, or outcome measures, and were rated as unclear risk.
3.8.4. Incomplete Outcome Data
We assessed the majority of trials as having a low risk of bias for outcome reporting. Eight trials were at high risk, owing to dropout rates or incomplete data, and attrition bias was unclear in six trials. We rated trials as having high risk of bias if dropout rates were uneven between groups and the reason for dropout was related or suspected to be related to group allocation. We also rated trials as having a high risk for bias if investigators reported a dropout rate >20% and did not report how they dealt with this (e.g., intention to treat (ITT) analysis, last observation carried forward).
3.8.5. Selective Reporting
Twenty-six trials were rated as unclear risk, owing to no study protocol or trial registration records being available. Two trials [36,57] did report data on all included outcomes and were at low risk of bias. We rated one trial as having a high risk of bias [46].
3.8.6. Other Potential Sources of Bias
Risk of bias was unclear for nine trials. We rated risk from other sources of bias as low for 12 trials. We assessed an imbalance at randomisation in eight trials, and these were rated as high risk of bias [41,43,50,55,59,61,67].
3.9. Acupuncture versus Usual Care
One study [36] compared acupuncture plus usual care to usual care alone. There was evidence of a moderate benefit in the severity of depression in the acupuncture group compared to usual care g = 0.41 (N = 1, n = 301, 95% CI 0.18 to 0.63).
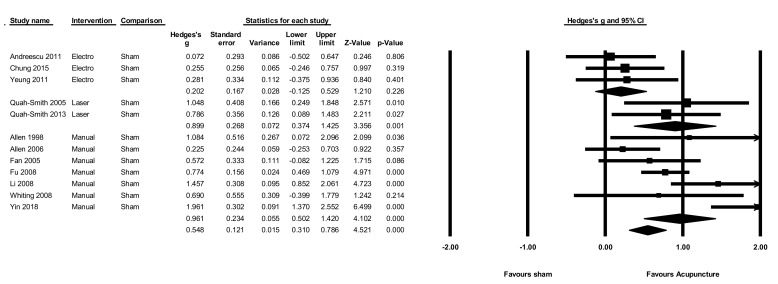
3.10. Acupuncture versus Sham
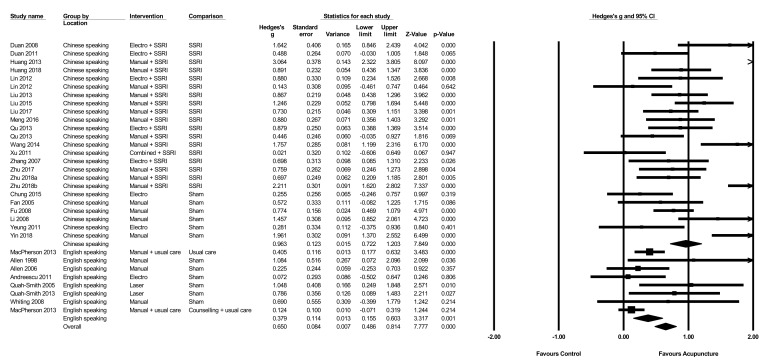
The pooled effect of acupuncture on the severity of depression compared to sham at the end of the intervention (Figure 3) was moderate g = 0.55 (N = 12, n = 646, 95% CI 0.31 to 0.79, Q = 38.15, p < 0.001, I2 = 71.2). When comparing different types of acupuncture, both manual (g = 0.96, N = 7, n = 439, 95% CI 0.50 to 1.4, Q = 25.1, p < 0.001, I2 = 76.1) and laser (g = 0.90, N = 2, n = 63, 95% CI 0.37 to 1.4, Q = 235, p = 0.62, I2 = 0) showed large effect sizes, while electro-acupuncture did not show a significant benefit compared to sham (g = 0.20, N = 3, n = 144, 95% CI −0.13 to 0.53, Q = 295, p = 0.863, I2 = 0). Only one study [61] contributed data for short term follow-up, so no meta-analysis was performed on follow-up data.
Figure 3.
Acupuncture versus sham control on the severity of depression.
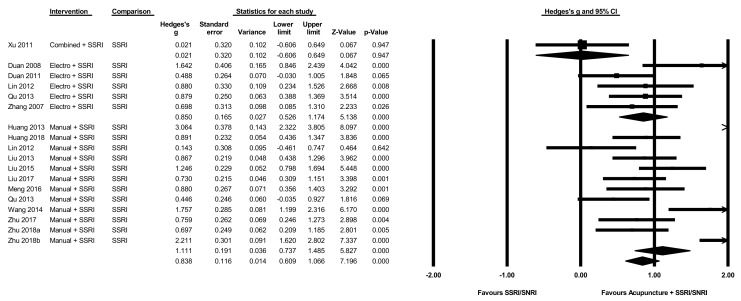
3.11. Acupuncture Plus SSRI/SNRI versus SSRI/SNRI Alone
The pooled effect of acupuncture plus SSRI/SNRI medication on the severity of depression at the end of intervention compared to SSRI/SNRI medication alone (Figure 4) was large g = 0.84 (N = 18, n = 1169, 95% CI 0.61 to 1.07, Q = 87, I2 = 80.5). When comparing different types of acupuncture in combination with SSRI/SNRI medication, both manual (g = 1.1, N = 12, n = 865, 95% CI 0.74 to 1.49, Q = 74, I2 = 85) and electro-acupuncture (g = 0.85, N = 5, n = 264, 95% CI 0.52 to 1.17, Q = 5.9, I2 = 32.4) showed large effect sizes, while the single study using combined manual and electro-acupuncture showed no evidence of significant benefits (g = 0.02, N = 1, n = 40, 95% CI −0.61 to 0.65).
Figure 4.
Acupuncture plus SSRI/SNRI versus SSRI/SNRI alone on the severity of depression.
3.12. Acupuncture versus Psychological Intervention
Only one study [36] compared acupuncture plus usual care to counseling plus usual care. There was no evidence of a significant difference in the severity of depression between groups (g = 0.12, N = 1, n = 453, 95% CI −0.07 to 0.32).
3.13. Adverse Events
When compared to sham, there was no increased rate of adverse events (RR1.66, N = 3, n = 146, 95% CI 0.56 to 4.9, Q = 2.6, I2 = 25). When compared to SSRI medication alone, there was no difference in adverse event scores (SMD 1.17, N = 3, n = 171, 95% CI −0.53 to 2.89, Q = 2, I2 = 95.8).
3.14. Subgroup Analysis
There was no difference in the reduction in severity of depression when comparing fixed, semi-standardised, and individualised acupuncture sub-groups (p = 0.468), or when comparing different needle retention times (p = 0.796). There were not enough studies using participant reported outcomes to allow meaningful comparison with clinician reported scales.
Trials in China had large effects in the reduction in severity of depression (g = 0.96, N = 24, n = 1599, 95% CI 0.72 to 1.2, Q = 114, I2 = 79.9), whereas trials undertaken outside of China had only small effects (g = 0.38, N = 7, n = 970, 95% CI 0.15 to 0.60, Q = 12, I2 = 45) (Figure 5). A test for between group differences showed that trials from China had significantly greater reductions in the severity of depression compared to those undertaken outside of China (Q = 12, p < 0.001).
Figure 5.
The effect of acupuncture on the severity of depression by study location.
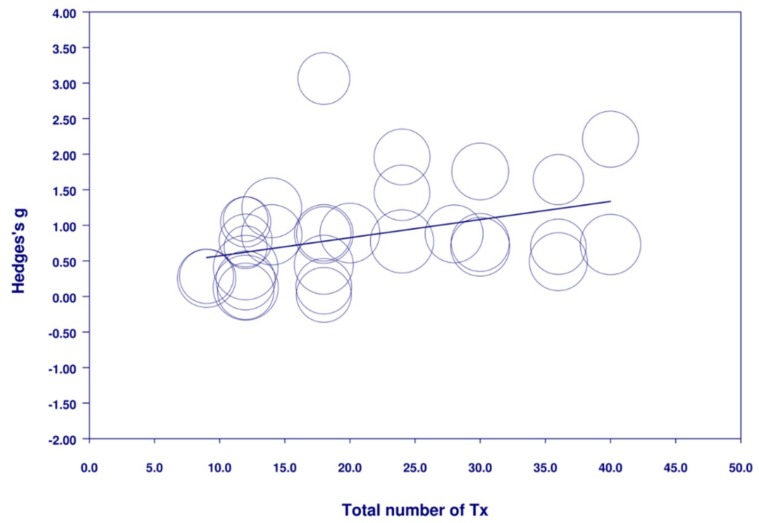
The meta-regression analysis (Figure 6) found that a greater total number of treatments was related to a greater reduction in the severity of depression (N = 29, n = 2268, B = 0.025, SE = 0.010, Z = 2.44, p = 0.015). Meta-regression showed a trend towards a greater reduction in the severity of depression with more frequent treatment (N = 29, n = 2268, B = 0.095, SE = 0.050, Z = 1.88, p = 0.061).
Figure 6.
Meta-regression of total number of treatments on the severity of depression.
A higher NICMAN score did not have a significant association with any difference between groups in the reduction in severity of depression (N = 29, n = 2268, B = −0.011, SE = 0.033, Z = −0.33, p = 0.73). The reporting on the number of acupuncture points used was only provided in 18 studies. There was no significant association between the number of acupuncture points and the reduction in the severity of depression (N = 29, n = 2268, B = 0.055, SE = 0.079, Z = 0.70, p = 0.48).
3.15. Publication Bias
There was no evidence of publication bias (p = 0.079) according to the Begg and Mazumdar test. Supplementary Figure S1 shows the funnel plot for publication bias. A Duval and Tweedie trim and fill analysis did not result in any studies to the left of the mean being trimmed.
4. Discussion
4.1. Principal Findings
In this review we identified 29 studies of acupuncture for depression, and these studies included 2268 participants. Acupuncture was found to be associated with clinically relevant effect sizes in reducing the severity of depression when compared to usual care alone, to sham acupuncture, and to SSRI/SNRI medication alone. With regard to the usual care comparison, the one relevant trial found moderate statistically significant benefits for those receiving acupuncture, with an effect size of 0.41. This was by far the largest trial, with 755 patients, and the only one to address the practical question of what impact acupuncture might have on patients with depression in primary care, who are routinely referred to acupuncturists. With regard to the sham acupuncture comparison, our meta-analysis of 12 trials showed acupuncture to significantly outperform varied forms of sham interventions, with a moderate effect size of 0.55, suggesting that acupuncture is more than a placebo. With regard to the comparison of acupuncture plus SSRI anti-depressants versus SSRI anti-depressants alone, our meta-analysis of 17 trials showed a moderate to large, and significant, effect size of 0.83, suggesting a potential role for acupuncture to be more routinely provided as an adjunct to SSRIs in cases where SSRIs are found to be ineffective or poorly tolerated.
Our review is the first to explore the correlation between the total number of treatments and the effect size, with the finding that when delivering acupuncture in a clinical setting, there appears to be benefits in longer courses of treatment. We found a trend between increased treatment frequency and a reduction in the severity of depression. The number of trials that delivered less than two treatments per week or more than five was small, and the addition of more studies with these treatment frequencies may change this result. Overall, it appears that the total number of treatments plays a greater role in reduction of depression than does the frequency of delivery of those treatments.
4.2. Strengths and Limitations
This review and meta-analysis had several strengths. The use of English, Chinese, and Korean databases allowed access to publications in the three most common languages for acupuncture research. The majority of included studies used clinician outcome measures to measure the severity of depression, and where multiple outcomes were given, clinician rated scales were given preference. Compared to the most recent Cochrane review of acupuncture for depression [18], within which databases were searched only up to June 2016, the present review differs in several important aspects. This review includes studies published until December 2018, increases clinical relevance by including only patients with depression as the primary presentation, includes a quality assessment measure for the acupuncture delivered in the form of the NICMAN scale, and explores the contribution of various dosage components on depression related clinical outcomes.
In terms of the limitations of this meta-analysis, the benefits we observed only relate to outcomes at the end of treatment. There was insufficient evidence to determine if the benefits were sustained due to the small number of trials (n = 2) that undertook any post trial follow-up. A key caveat with regard to the overall findings is the level of risk of bias across the seven risk of bias domains. No trials were assessed as having low risk of bias across all domains. Only four trials were identified as having a low risk of bias across at least five of these domains. Moreover, the transferability of the results may be compromised by the preponderance of trials from China. Only seven of the 29 trials were conducted in other countries, namely USA, UK, and Australia. The effect sizes were larger in China, which may be explained by the significantly more frequent treatment regimen and the significantly greater total number of sessions. The median number of total treatments delivered was twice that in China compared to other countries, and the median frequency of treatment much greater, with treatment being delivered with a median frequency of every second day in China, compared to once per week. A high risk of bias is associated with larger effect sizes [68], therefore an alternate view is that the high risk of bias of the trials in China may explain the larger effects seen. The percentage of trials assessed as having a low risk of bias in five or more domains conducted in China was 14% (3/22), while in other countries the rate was 57% (4/7).
The present review found moderate to large effect sizes when adding acupuncture to first line antidepressants, such as SSRIs. People who favour alternative treatments may elect to have acupuncture rather than other adjunctive approaches, such as a mood stabilizing agent like lithium. However, limitations of the research involving acupuncture and anti-depressants, particularly the high risk of bias from lack of blinding, tempers this conclusion. It should also be noted that all the trials involving acupuncture compared to SSRIs alone were conducted in China. Moreover, blinding for those participants in the acupuncture plus medication versus medication alone comparisons was not performed. This lack of blinding is likely to increase the non-specific/attention effects of those in the treatment group and may result in overestimating the effect size. Similarly, reporting on the blinding status of those clinicians who undertook the rating for depression was often unclear and this also may overestimate the effect size.
4.3. Implications for Research and Practice
In terms of the implications for research, the stand-out requirement is for more higher-quality randomised control trials to evaluate the effectiveness of acupuncture for treatment for depression. Such trials need to be designed with a low risk of bias, with large enough sample sizes to be sufficiently powered, with long enough follow-ups beyond the end of treatment, ideally for 12 months after randomisation, and with sufficient numbers of treatment sessions provided. More research into the dosage of acupuncture would be helpful, with the intention of clarifying what comprises a sufficient number of acupuncture sessions for the average patient. In terms of trial designs, this review has highlighted the need for more practical trials, in which the treatment as usual, or usual care, is the primary comparator, as only one trial [36] included a usual care comparison. More trials of this type are needed to model real-world settings, and in different countries. The results of these trials will provide important evidence for patients when considering the option of acupuncture, for clinicians when considering the referral of their patients to an acupuncturist, for decision-makers when considering providing resources to fund mental health treatments, and for policy-makers when considering questions of health policy related to depression. Moreover, such pragmatic designs provide an ideal framework for a parallel cost-effectiveness analysis, thereby supporting economic-related decision-making.
In terms of implications for clinical practice, the findings of this review provide some limited support for acupuncture as a treatment for depression. Most patients with depression will be offered SSRI or SNRI anti-depressants as a first line treatment, and our evidence shows a moderate effect size is associated with acupuncture provided for this patient group. A smaller effect size in a single trial was found when acupuncture plus usual care was compared to usual care alone. The difference may in part be explained by the former trials all being conducted in China, where significantly more treatment sessions were delivered, and the latter trial recruiting from primary care in the UK, with only those patients who had moderate to severe depression, and who mostly received only one treatment a week. There remain many unanswered questions regarding what might be considered optimal acupuncture, including the number of sessions, frequency of sessions, diagnostic frameworks, flexibility of point prescriptions, role of theoretically informed life-style advice, and the engagement and self-efficacy of the patient. Manual acupuncture showed larger effect sizes than electro-acupuncture when compared to both sham and SSRI/SNRI medication alone. This is an unexpected finding because compared to manual acupuncture, electro-acupuncture has been thought to deliver a greater ’dose’ of acupuncture, as a result of the duration and intensity of stimulation [69]. Similar to our findings in this regard, evidence for additional benefits of adding electro-stimulation to acupuncture is unclear when outcomes are not related to pain [69,70].
There remain further unanswered questions regarding which patients might find acupuncture most beneficial, in terms of severity of depression, whether on anti-depressants or not, and the implications of comorbidity. We know that when a patient is depressed, they often are experiencing a range of other symptoms, commonly chronic pain, insomnia, digestive disorders, and low energy. Typically, a traditional acupuncturist will take into account this range of symptoms when constructing a treatment plan [71]. In cases where multi-morbidity from the perspective of biomedicine is perceived as problematic, research is needed to confirm, or otherwise, whether a multi-faceted acupuncture treatment provides a useful single modality solution.
5. Conclusions
Acupuncture showed clinically-relevant benefits in reducing the severity of depression at the end of treatment compared to sham acupuncture, usual care, and as an adjunct treatment to anti-depressant medication. The high risk of bias for participant blinding in the majority of studies means these results must be interpreted cautiously. Both the total number of treatments and the frequency of treatment may play a role in depression-related outcomes. The clinical relevance of these findings to a non-Chinese population requires further interpretation, due to the majority of studies being undertaken in China, where treatment frequencies and the total number of treatments were significantly greater than those undertaken in English speaking countries, but where trials were also rated as having a higher risk of bias. Future studies need to include both short, medium-, and long-term follow-up to determine if any benefits on the severity of depression are maintained.
Acknowledgments
Thanks to the staff of the Cochrane Common Mental Disorders (CCMD) group for their support in our original Cochrane review.
Supplementary Materials
The following are available online at https://www.mdpi.com/2077-0383/8/8/1140/s1, Figure S1: Funnel plot of standard error by Hedges’s g.
Author Contributions
M.A. conceptualised the study, performed the English searches, search screening, data extraction and risk of bias on English language papers, data entry, performed the meta-analysis, NICMAN scoring, and drafted the manuscript. C.A.S. conceptualised the study, data extraction and risk of bias on English language papers, NICMAN scoring, and provided input into the manuscript. L.-Q.W. and G.-Y.Y. both performed the Chinese searches, data extraction on Chinese language papers and NICMAN scoring, and provided feedback on the manuscript. D.N. performed data extraction and risk of bias on English language papers, and data entry. H.M. helped conceptualise the study, assisted with data extraction and risk of bias on English language papers, and provided input into the manuscript. M.S.L. performed the Korean searches and screened the Korean papers and provided feedback on the manuscript. P.H. helped conceptualise the study, assisted with screening, data extraction and risk of bias on English language papers, and provided input into the manuscript.
Funding
M.S.L. was supported by Korea Institute of Oriental Medicine (KSN1522120). The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Conflicts of Interest
M.A., C.A.S., D.N. and G.-Y.Y. As a medical research institute, NICM Health Research Institute receives research grants and donations from foundations, universities, government agencies and industry. Sponsors and donors provide untied and tied funding for work to advance the vision and mission of the Institute. This study was not specifically supported by donor or sponsor funding to NICM. L.-Q.W.: none P.H.: Hay receives/has received sessional fees and lecture fees from the Australian Medical Council, Therapeutic Guidelines publication, and New South Wales Institute of Psychiatry and royalties/honoraria from Hogrefe and Huber, McGraw Hill Education, and Blackwell Scientific Publications, Biomed Central and PlosMedicine and she has received research grants from the NHMRC and ARC. She is Chair of the National Eating Disorders Collaboration Steering Committee in Australia (2019-) and Member of the ICD-11 Working Group for Eating Disorders (2012-) and was Chair Clinical Practice Guidelines Project Working Group (Eating Disorders) of RANZCP (2012–2015). She has prepared a report under contract and conducted education for Psychiatrists funded by Shire Pharmaceuticals (2017–2018). All views in this paper are her own. H.M.: MacPherson is an Emeritus Professor of Acupuncture Research, Department of Health Sciences, University of York, UK, Chair of Trustees of the Northern College of Acupuncture, York, UK, and Clinical Director of the York Clinic for Integrated Healthcare, York, UIK. M.S.L.: Korea Instutute of Oriental Medicine is a Korean government funded institute for researching Korean Medicine (KIOM).
References
- 1.Hasin D.S., Sarvet A.L., Meyers J.L., Saha T.D., Ruan W.J., Stohl M., Grant B.F. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry. 2018;75:336–346. doi: 10.1001/jamapsychiatry.2017.4602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Malhi G.S., Bassett D., Boyce P., Bryant R., Fitzgerald P.B., Fritz K., Hopwood M., Lyndon B., Mulder R., Murray G., et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders. Aust. N. Z. J. Psychiatry. 2015;49:1087–1206. doi: 10.1177/0004867415617657. [DOI] [PubMed] [Google Scholar]
- 3.National Institute for Health and Care Excellence . Depression in Adults: Recognition and Management (NICE Clinical Guideline 30) NICE; London, UK: 2009. [PubMed] [Google Scholar]
- 4.Kessler R.C., Soukup J., Davis R.B., Foster D.F., Wilkey S.A., Van Rompay M.I., Eisenberg D.M. The use of complementary and alternative therapies to treat anxiety and depression in the United States. Am. J. Psychiatry. 2001;158:289–294. doi: 10.1176/appi.ajp.158.2.289. [DOI] [PubMed] [Google Scholar]
- 5.Hansen A.H., Kristoffersen A.E. The use of CAM providers and psychiatric outpatient services in people with anxiety/depression: A cross-sectional survey. BMC Complement. Altern. Med. 2016;16:461. doi: 10.1186/s12906-016-1446-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Druss B.G., Rosenheck R.A. Use of practitioner-based complementary therapies by persons reporting mental conditions in the United States. Arch. Gen. Psychiatry. 2000;57:708–714. doi: 10.1001/archpsyc.57.7.708. [DOI] [PubMed] [Google Scholar]
- 7.Robinson N., Lorenc A., Ding W., Jia J., Bovey M., Wang X.M. Exploring practice characteristics and research priorities of practitioners of traditional acupuncture in China and the EU-A survey. J. Ethnopharmacol. 2012;140:604–613. doi: 10.1016/j.jep.2012.01.052. [DOI] [PubMed] [Google Scholar]
- 8.Hopton A.K., Curnoe S., Kanaan M., MacPherson H. Acupuncture in practice: Mapping the providers, the patients and the settings in a national cross-sectional survey. BMJ Open. 2012;2:e000456. doi: 10.1136/bmjopen-2011-000456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hou Z., Jiang W., Yin Y., Zhang Z., Yuan Y. The Current Situation on Major Depressive Disorder in China: Research on Mechanisms and Clinical Practice. Neurosci. Bull. 2016;32:389–397. doi: 10.1007/s12264-016-0037-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang Y., Jiang H., Meng H., Li J., Yang X., Zhao B., Sun Y., Bao T. Antidepressant Mechanism Research of Acupuncture: Insights from a Genome-Wide Transcriptome Analysis of Frontal Cortex in Rats with Chronic Restraint Stress. Evid.-Based Complementary Altern. Med. 2017;2017:1676808. doi: 10.1155/2017/1676808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leung M.C., Yip K.K., Ho Y.S., Siu F.K., Li W.C., Garner B. Mechanisms underlying the effect of acupuncture on cognitive improvement: A systematic review of animal studies. J. Neuroimmune Pharmacol. 2014;9:492–507. doi: 10.1007/s11481-014-9550-4. [DOI] [PubMed] [Google Scholar]
- 12.Armour M., Smith C.A. Treating primary dysmenorrhoea with acupuncture: A narrative review of the relationship between acupuncture ‘dose’ and menstrual pain outcomes. Acupunct. Med. 2016;34:416–424. doi: 10.1136/acupmed-2016-011110. [DOI] [PubMed] [Google Scholar]
- 13.White A., Cummings M., Barlas P., Cardini F., Filshie J., Foster N.E., Lundeberg T., Stener-Victorin E., Witt C. Defining an adequate dose of acupuncture using a neurophysiological approach—A narrative review of the literature. Acupunct. Med. 2008;26:111–120. doi: 10.1136/aim.26.2.111. [DOI] [PubMed] [Google Scholar]
- 14.Smith C.A., Zaslawski C.J., Zheng Z., Cobbin D., Cochrane S., Lenon G.B., Loyeung B., Meier P.C., Walsh S., Xue C.C., et al. Development of an Instrument to Assess the Quality of Acupuncture: Results from a Delphi Process. J. Altern. Complementary Med. 2011;17:441–452. doi: 10.1089/acm.2010.0457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith C.A., Armour M., Shewamene Z., Tan H.Y., Norman R.J., Johnson N.P. Acupuncture performed around the time of embryo transfer: A systematic review and meta-analysis. Reprod. BioMed. Online. 2019;38:364–379. doi: 10.1016/j.rbmo.2018.12.038. [DOI] [PubMed] [Google Scholar]
- 16.Armour M., Dahlen H.G., Zhu X., Farquhar C., Smith C.A. The role of treatment timing and mode of stimulation in the treatment of primary dysmenorrhea with acupuncture: An exploratory randomised controlled trial. PLoS ONE. 2017;12:e0180177. doi: 10.1371/journal.pone.0180177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lin Y.-J., Kung Y.-Y., Kuo W.-J., Niddam D.M., Chou C.-C., Cheng C.-M., Yeh T.-C., Hsieh J.-C., Chiu J.-H. Effect of acupuncture ‘dose’ on modulation of the default mode network of the brain. Acupunct. Med. 2016;34:425–432. doi: 10.1136/acupmed-2016-011071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith C.A., Armour M., Lee M.S., Wang L.Q., Hay P.J. Acupuncture for depression. Cochrane Database Syst. Rev. 2018;3 doi: 10.1002/14651858.CD004046.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders: DSM-III-R. American Psychiatric Association; Washington, DC, USA: 1987. [Google Scholar]
- 20.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. American Psychiatric Association; Washington, DC, USA: 1994. [Google Scholar]
- 21.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders: DSM-5. American Psychiatric Association; Arlington, VA, USA: 2013. [Google Scholar]
- 22.World Health Organization . ICD-10: International Statistical Classification of Diseases and Related Health Problems. World Health Organization; Geneva, Switzerland: 2004. [Google Scholar]
- 23.Chinese Society of Psychiatry . The Chinese Classification of Mental Disorders (CCMD-3) 3rd ed. Shandong Science and Technology Press; Shandong, China: 2001. [Google Scholar]
- 24.Chinese Society of Psychiatry . Classification and Diagnostic Criteria of Mental Disorders in China (CCMD-2) Hunan Medical University; Changsha, China: 1989. [Google Scholar]
- 25.Brugha T.S., Bebbington P.E., Jenkins R., Meltzer H., Taub N.A., Janas M., Vernon J. Cross validation of a general population survey diagnostic interview: A comparison of CIS-R with SCAN ICD-10 diagnostic categories. Psychol. Med. 1999;29:1029–1042. doi: 10.1017/S0033291799008892. [DOI] [PubMed] [Google Scholar]
- 26.Beck A.T., Steer R.A., Ball R., Ranieri W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J. Personal. Assess. 1996;67:588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- 27.Park J., White A., Stevinson C., Ernst E., James M. Validating a new non-penetrating sham acupuncture device: Two randomised controlled trials. Acupunct. Med. 2002;20:168–174. doi: 10.1136/aim.20.4.168. [DOI] [PubMed] [Google Scholar]
- 28.Streitberger K., Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet. 1998;352:364–365. doi: 10.1016/S0140-6736(97)10471-8. [DOI] [PubMed] [Google Scholar]
- 29.Cai R.L., Shen G.M., Wang H., Guan Y.Y. Brain functional connectivity network studies of acupuncture: A systematic review on resting-state fMRI. J. Integr. Med. 2018;16:26–33. doi: 10.1016/j.joim.2017.12.002. [DOI] [PubMed] [Google Scholar]
- 30.Higgins J.P., Altman D.G., Gotzsche P.C., Juni P., Moher D., Oxman A.D., Savovic J., Schulz K.F., Weeks L., Sterne J.A., et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343 doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Armour M., Smith C.A., Steel K.A., Macmillan F. The effectiveness of self-care and lifestyle interventions in primary dysmenorrhea: A systematic review and meta-analysis. BMC Complement. Altern. Med. 2019;19:22. doi: 10.1186/s12906-019-2433-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Smith C.A., Zaslawski C.J., Cochrane S., Zhu X., Zheng Z., Loyeung B., Meier P.C., Walsh S., Xue C.C., Zhang A.L., et al. Reliability of the NICMAN Scale: An Instrument to Assess the Quality of Acupuncture Administered in Clinical Trials. Evid. Based Complement. Alternat. Med. 2017;2017:5694083. doi: 10.1155/2017/5694083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.MacPherson H., Altman D.G., Hammerschlag R., Li Y., Wu T., White A., Moher D., Group S.R. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): Extending the CONSORT statement. Acupunct. Med. 2010;28:83–93. doi: 10.1136/aim.2009.001370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hedges L., Olkin I. Statistical Methods for Meta-Analysis. Academic Press; San Diego, CA, USA: 1985. [Google Scholar]
- 35.Lin W.R., Huang Y., Chen J.Q., Wang S.X. Global improvement in agitated depression treated with the alliance therapy of acupuncture and seroxat and the observation of the quality of life. Zhongguo Zhen Jiu. 2012;32:1063–1069. [PubMed] [Google Scholar]
- 36.MacPherson H., Richmond S., Bland M., Brealey S., Gabe R., Hopton A., Keding A., Lansdown H., Perren S., Sculpher M., et al. Acupuncture and counselling for depression in primary care: A randomised controlled trial. PLoS Med. 2013;10:e1001518. doi: 10.1371/journal.pmed.1001518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Qu S.S., Huang Y., Zhang Z.J., Chen J.Q., Lin R.Y., Wang C.Q., Li G.L., Wong H.K., Zhao C.H., Pan J.Y., et al. A 6 week randomised controlled trial with 4 week follow up of acupuncture combined with paroxetine in patients with major depressive disorder. J. Psychiatr. Res. 2013;47:726–732. doi: 10.1016/j.jpsychires.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 38.Duan D.M., Tu Y., Chen L.P. Assessment of effectiveness of electroacupuncture and fluoxetine for treatment of depression with physical symptoms. Zhongguo Zhen Jiu. 2008;28:167–170. [PubMed] [Google Scholar]
- 39.Duan D.M., Tu Y., Liao S., Qin W. The relevance between symptoms and magnetic resonance imaging analysis of the hippocampus of depressed patients given electro-acupuncture combined with Fluoxetine intervention: A randomized controlled trial. Chin. J. Integr. Med. 2011;17:190–199. doi: 10.1007/s11655-011-0666-6. [DOI] [PubMed] [Google Scholar]
- 40.Huang Y., Wang X.J., Wang L.L., Lu S.F., Zhu B.M., Xu L. Effect of acupuncture on selective serotonin reuptake inhibitors. Chin. J. Integr. Med. 2013;33:1341–1344. [PubMed] [Google Scholar]
- 41.Huang Z.Y., Chen J.D., Xie B., Xia Y.P., Wang W.Q., Su Z.B., Xie Y.Y., Tang F., Gu W.J., Yang F.L. Clinical curative effect of Shugan Jianpi acupuncture manipulation combined with magnetic stimulation in Yintang acupoint in the treatment of depression with liver-qi stagnation and spleen deficiency type. Chin. J. Behav. Med. Brain Sci. 2018;27:333–337. doi: 10.3760/cma.j.issn.1674-6554.2018.04.009. [DOI] [Google Scholar]
- 42.Liu Y., Feng H., Liu W.J., Mao H.J., Zhang Y.H., Hu L.L., Yin Y., Xu L.L. Effect of acupuncture of soothing-liver and nourishing-heart method combined with venlafaxine on residual symptoms and serum monoamine neurotransmitter of depressive disorder patients. Chin. J. Gen. Pract. 2017;15:1378–1381. doi: 10.16766/j.cnki.issn.1674-4152.2017.08.031. [DOI] [Google Scholar]
- 43.Liu Y., Feng H., Mao H., Mo Y., Yin Y., Liu W., Song M., Wang S. Impact on serum 5-HT and TH1/TH2 in patients of depressive disorder at acute stage treated with acupuncture and western medication. Chin. Acupunct. Moxibustion. 2015;35:539–543. [PubMed] [Google Scholar]
- 44.Liu Y., Zhang Y.H., Jin M., Liu W.J. Study on clinical effect enhancement of acupuncture for depression with chronic pain treated with SSRI antidepressants. Chin. Acupunct. Moxibustion. 2013;13:689–691. [PubMed] [Google Scholar]
- 45.Meng X., Zheng Z., Wu D., Miao Y. Observation on the clinical effect of cluster needling method on scalp acupoints of depression. Biotech. World. 2016;2:86. [Google Scholar]
- 46.Wang T., Wang L., Tao W., Chen L. Acupuncture combined with an antidepressant for patients with depression in hospital: A pragmatic randomised controlled trial. Acupunct. Med. 2014;32:308–312. doi: 10.1136/acupmed-2013-010469. [DOI] [PubMed] [Google Scholar]
- 47.Xu L., Wang L.L. Clinical observation on depression treated by eletroacupuncture combined with western medicine. Chin. Acupunct. Moxibustion. 2011;31:779–782. [PubMed] [Google Scholar]
- 48.Zhang G.J., Shi Z.Y., Liu S., Gong S.H., Liu J.Q. Clinical observation of treatment of depression by electro-acupuncture combined with paroxetine Clinical observations. Chin. J. Integr. Med. 2007;13:228–230. doi: 10.1007/s11655-007-0228-0. [DOI] [PubMed] [Google Scholar]
- 49.Zhu W.X., Wang J., Wang Q.S., Ji X.D., Yuan G.Z. Antidepressant effect of acupuncture and its influence on peripheral inflammatory cytokines. Med. J. Chin. People’s Armed Police Forces. 2017;28:816–819. doi: 10.14010/j.cnki.wjyx.2017.08.019. [DOI] [Google Scholar]
- 50.Zhu W.X., Wang J., Wang Q.S., Ji X.D., Yuan G.Z. Effect of acupuncture on the autonomic nervous system in patients with major depressive disorder. Lishizhen Med. Mater. Med. Res. 2018;29:381–383. doi: 10.3969/j.issn.1008-0805.2018.02.044. [DOI] [Google Scholar]
- 51.Zhu Z.M., Xu Y., Zeng Y.B., Lu L.S., Xu C.W. Effect of acupuncture combined with sertraline for depression. J. Pract. Tradit. Chin. Med. 2018;34:175–176. [Google Scholar]
- 52.Andreescu C., Glick R.M., Emeremni C.A., Houck P.R., Mulsant B.H. Acupuncture for the treatment of major depressive disorder: A randomised controlled trial. J. Clin. Psychiatry. 2011;72:1129–1135. doi: 10.4088/JCP.10m06105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chung K.F., Yeung W.F., Yu Y.M., Yung K.P., Zhang S.P., Zhang Z.J., Wong M.-T., Lee W.K., Chan L.W. Acupuncture for residual insomnia associated with major depressive disorder: A placebo and sham controlled subject and assessor blind randomised trial. J. Clin. Psychiatry. 2015;76:752–760. doi: 10.4088/JCP.14m09124. [DOI] [PubMed] [Google Scholar]
- 54.Fan L., Fu W.B., Meng C.R., Zhu X.P., Mi J.P., Li W.X., Wen X. Effect of acupuncture at routine acupoint and no-acupoint on depressive neurosis evaluated by Hamilton depression scale. Chin. J. Clin. Rehabil. 2005;9:14–16. [Google Scholar]
- 55.Fu W.B., Fan L., Zhu X.P., He Q., Wang L., Zhuang L.X., Liu Y.S., Tang C.Z., Li Y.W., Meng C.R., et al. Acupuncture for treatment of depressive neurosis: A multi-centred randomized controlled trial. Chin. Acupunct. Moxibustion. 2008;28:3–6. [PubMed] [Google Scholar]
- 56.Li Y.W., Fu W.B., Zhu X.P. Clinical observation on acupuncture for depressive of 27 cases. J. Tradit. Chin. Med. 2008;49:431–433. [Google Scholar]
- 57.Quah-Smith I., Smith C., Crawford J.D., Russell J. Laser acupuncture for depression: A randomised double blind controlled trial using low intensity laser intervention. J. Affect. Disord. 2013;148:179–187. doi: 10.1016/j.jad.2012.11.058. [DOI] [PubMed] [Google Scholar]
- 58.Quah-Smith J.I., Tang W.M., Russell J. Laser acupuncture for mild to moderate depression in a primary care setting—A randomised controlled trial. Acupunct. Med. 2005;23:103–111. doi: 10.1136/aim.23.3.103. [DOI] [PubMed] [Google Scholar]
- 59.Whiting M., Leavey G., Scammell A., Au S., King M. Using acupuncture to treat depression: A feasibility study. Complementary Ther. Med. 2008;16:87–91. doi: 10.1016/j.ctim.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 60.Yeung M.F., Chung K.F., Tso K.C., Zhang S.P., Zhang Z.J., Ho L.M. Electroacupuncture for residual insomnia associated with major depressive disorder: A randomised controlled trial. SLEEP. 2011;34:807–815. doi: 10.5665/SLEEP.1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yin P., Ma J., Wu H.G., Xu S.F. Clinical observation of Jie Yu Tong Fu needling for depression coupled with constipation. Shanghai J. Acupunct. Moxibustion. 2018;37:159–164. doi: 10.13460/j.issn.1005-0957.2018.02.0159. [DOI] [Google Scholar]
- 62.Allen J.B., Schyner R.N., Hitt S.K. The efficacy of acupuncture in the treatment of major depression in women. Psychol. Sci. 1998;9:397–401. doi: 10.1111/1467-9280.00074. [DOI] [Google Scholar]
- 63.Allen J.J., Schyner R.N., Chambers A.S., Hitt S.K. Acupuncture for depression: A randomised controlled trial. J. Clin. Psychiatry. 2006;67:1665–1673. doi: 10.4088/JCP.v67n1101. [DOI] [PubMed] [Google Scholar]
- 64.Hamilton M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cheng Y., Tang Q.S. Abdominal acupuncture in treating liver-qi stagnation and spleen deficiency in the elderly with post-stroke depression: A randomized and controlled observation. Chin. J. Clin. Rehabil. Tissue Eng. Res. 2007;11:7791–7794. [Google Scholar]
- 67.Du Y.H., Li G.P., Yan H., Zhang X.J., Huang L.F. Clinical study on needling method for regulating mental activities and soothing liver for treatment of melancholia. Zhongguo Zhen Jiu. 2005;25:151–154. [PubMed] [Google Scholar]
- 68.Schulz K.F., Altman D.G., Moher D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomized trials. Ann. Intern. Med. 2010;152:726–732. doi: 10.7326/0003-4819-152-11-201006010-00232. [DOI] [PubMed] [Google Scholar]
- 69.Mayor D. An exploratory review of the electroacupuncture literature: Clinical applications and endorphin mechanisms. Acupunct. Med. 2013;31:409–415. doi: 10.1136/acupmed-2013-010324. [DOI] [PubMed] [Google Scholar]
- 70.Langevin H.M., Schnyer R., MacPherson H., Davis R., Harris R.E., Napadow V., Wayne P.M., Milley R.J., Lao L., Stener-Victorin E., et al. Manual and electrical needle stimulation in acupuncture research: Pitfalls and challenges of heterogeneity. J. Altern. Complement. Med. 2015;21:113–128. doi: 10.1089/acm.2014.0186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hopton A., Eldred J., MacPherson H. Patients’ experiences of acupuncture and counselling for depression and comorbid pain: A qualitative study nested within a randomised controlled trial. BMJ Open. 2014;4:e005144. doi: 10.1136/bmjopen-2014-005144. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.