Abstract
Critically ill patients often require life support measures such as mechanical ventilation or haemodialysis. Despite the essential role of nutrition in patients’ recovery, the inappropriate use of medical nutrition therapy can have deleterious effects, as is the case with the use of respiratory, circulatory, or renal support. To increase awareness and to monitor the effects of inappropriate medical nutrition therapy, we propose to introduce the concept of nutritrauma in clinical practice, defined as metabolic adverse events related to the inappropriate administration of medical nutrition therapy or inadequate nutritional monitoring.
Keywords: medical nutrition therapy, enteral nutrition, parenteral nutrition, nutritional support, critical care, iatrogenesis
1. Introduction
During the twentieth century, many medical interventions were introduced to treat clinical conditions that would previously have been fatal. The introduction of mechanical ventilation and haemodialysis increased the chance of survival among people with respiratory failure and renal failure. Far from being physiological, these life-support techniques can have adverse effects, which can produce activation of the inflammatory cascade, microscopic lesions at the cellular level, or precipitate organ failure [1,2].
The study of the clinical effects and outcomes following the administration of life support techniques has led to the development of safer and better-tolerated therapies [3,4]. In the case of mechanical ventilation, replacing the cycles of positive and negative pressure of spontaneous ventilation with positive pressure throughout the breath cycle produces a decrease in venous return, alterations in the immune response, and traumatic injuries due to hyperpressure (barotrauma), volutrauma, and atelectrauma (Table 1). Mechanical ventilation has provided life support for many patients who are in critical condition, but experience has taught us that it is insufficient to only program a suitable respiratory rate, tidal volume, and fraction of inspired oxygen (FiO2), but that it also requires choosing when to intubate, providing adequate sedation, the use of volume and pressure alarms, making postural changes, aspiration of secretions, and measures to prevent infections induced by the ventilation. The value of mechanical ventilation in intensive care units is not open to question. Without questioning its usefulness, we can continue to try to improve the ventilatory support for patients who cannot breathe, while minimising the adverse effects of its use [5].
Table 1.
Adverse events (AE) and iatrogenic injuries associated with life support techniques.
| Item | INVASIVE MECHANICAL VENTILATION | CONTINUOUS HAEMODIALYSIS | MEDICAL NUTRITION THERAPY |
|---|---|---|---|
| Indication | Alteration of ventilation Alteration of oxygenation Airway permeability |
Uraemia Dyselectrolytaemia Hypervolemia Removing toxins (endogenous and exogenous) Hypothermia |
Inadequate nutritional intake |
| Access | Tracheal tube Tracheostomy |
Central venous line | Central venous line Enteral tube |
| Adjuvant treatments | Sedation Neuromuscular block Artificial nutrition Physiotherapy |
Systemic anticoagulation Circuit heater or thermal blanket |
Insulin administration for glycaemic control Physiotherapy |
| AE related to access | Stenosis, Granulomas, Mucosal necrosis |
Hemorrhage Thrombosis |
Hemorrhage Thrombosis |
| AE related to infections | Ventilator-associated pneumonia | Catheter-related infections | Sinusitis Catheter-related infections |
| AE related to toxicity | Oxygen toxicity | Heparin-induced thrombocytopenia. Citrate-induced hypocalcemia |
Chemical phlebitis |
| AE related to the technique | Barotrauma: Lung injury due to positive pressure, overdistention and alveolar break Volutrauma: Lung injury due to local overdistention as a result of using excessive tidal volumes Atelectrauma: Alveolar damage as a result of transient and repeated closure and reopening of alveoli during the respiratory cycle. Biotrauma: Mechanical stress in response to using high tidal volume and inadequate positive end-expiratory pressure (PEEP) leading to a systemic inflammatory response |
Dialytrauma: Harmful effects of continuous renal replacement therapy Dyselectrolytaemia: hypokalaemia, hypophosphataemia, hyponatraemia, hypo/hypercalcaemia, alteration of lactate metabolism Loss of endogenous vital nutrients: water-soluble vitamins, antioxidants, carbohydrates, amino acids Incorrect adjustment of drugs Hypothermia Blood loss: secondary to circuit lifespan |
Nutritrauma: Over- and underfeeding, Hypervolaemia Uraemia Hypercapnia Hypertriglyceridaemia Refeeding syndrome Dyselectrolytaemia Hyperglycaemia Hepatobiliary disorders: Cholestasis, cholecystitis, cholelithiasis, hepatic steatosis, non-alcoholic fatty liver disease, hepatic fibrosis and cirrhosis Metabolic bone disease Malabsorptive diarrhea |
2. Medical Nutrition Therapy as a Form of Life Support
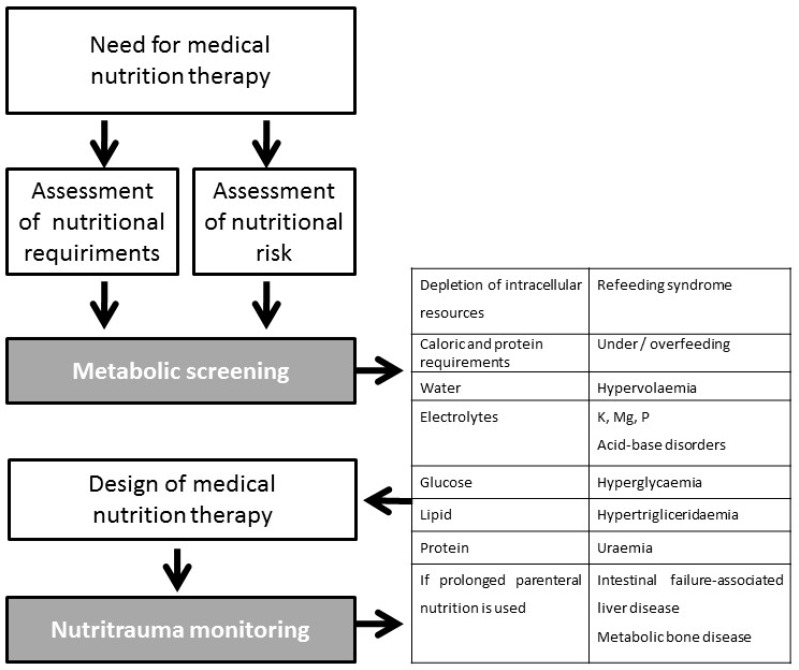
People need nutrients to stay alive. Maintaining the structure and function of the human body depends on the intake of energy and nutrient components. Therefore, in patients who cannot take nutrients due to anatomical or functional insufficiency, medical nutrition therapy (MNT) must be provided as a form of life support. However, as with other life support measures, in the design of MNT, the quantity and composition of nutrient intake is determined by the physician and not by the patient. Moreover, substrate utilisation in critically ill patients is affected by the inflammatory response associated with acute injury [6]. An inadequate assessment of when to initiate nutritional support, the patient’s capacity to manage the support, the route of administration, and the amount or composition or nutritional support, can have harmful consequences for the patient [7]. The iatrogenic effect of inappropriate nutritional support should be monitored [8] and included in health quality standards [9,10]. Use of the umbrella term “nutritrauma” to encompass the broad clinical spectrum of harms that can be caused by nutritional support could facilitate the spread of this concept, increase awareness of the iatrogenic effects of inappropriate nutritional support, and lead to training measures being introduced to minimise its occurrence (Figure 1).
Figure 1.
Schema for incorporating the concept of nutritrauma into clinical practice.
3. Complications of Medical Nutrition Therapy that should be Included in the Definition of Nutritrauma
There are many complications of medical nutrition therapy that should be included in the definition of nutritrauma (Table 2). These include the following:
Table 2.
Complications of medical nutrition therapy included in the definition of nutritrauma.
| Component | Adverse Events | Therapeutic Approach |
|---|---|---|
| Inappropriate dosage | Overfeeding, underfeeding | Adjust calorie and protein administration to inflammatory status and clinical phase, Adjust non-nutritional calorie administration, Minimise interruptions and optimise enteral administration |
| Refeeding syndrome | Depletion of intracellular resources in previously malnourished or fasting patients | Assess nutritional risk and requirements, Restrict calorie intake during the first few days of transitioning back to a normal diet |
| Water | Fluid overload | Adjust prescription to liquid balances |
| Electrolytes | Electrolyte disturbances (K, Mg, P, acid-base disorders) | Periodic laboratory tests |
| Glucose | Hypoglycaemia, hyperglycaemia | Glycaemic control protocol |
| Calorie intake Lipid | Hypertriglyceridaemia, non-alcoholic fatty liver disease | Adjust lipid administration to calorie requirements, periodic laboratory test |
| Protein | Uraemia | Adjust protein prescription to requirements and stress |
| Prolonged use of Parenteral Nutrition | Intestinal failure-associated liver disease, metabolic bone disease | Test enteral tolerance if possible |
Miscalculation of calorie and protein requirements
Fluid overload
Metabolic complications of electrolyte and acid-base imbalance
Hypertriglyceridemia
Hepatobiliary disorders associated with parenteral nutrition (PN)
Metabolic bone disease
Hyperglycaemia
Food hypersensitivities
Refeeding syndrome
Each of these is discussed below.
3.1. Miscalculation of Calorie and Protein Requirements
Under-prescription and over-prescription of nutrients can cause metabolic complications and affect prognosis [11,12]. Overnutrition should be regarded as associated with not only PN but also the metabolic impact of providing direct intravenous infusion of nutrients. Stressed patients have a limited capacity to process water, energy and protein waste. Moreover, insulin resistance is related to inflammatory stress and leads to increased protein metabolism as the primary intracellular energy substrate in place of lipids or glucose. Ketosis is not frequent in patients with a negative protein balance [13]. Metabolic imbalances can be prevented by phasing the introduction of enteral nutrients, while the sudden introduction of parenteral nutrition without adjusting it to the patient’s nutritional requirements can result in metabolic disturbances [14]. Calories and protein should be evaluated and prescribed separately to avoid over- or under-feeding.
In the stressed critically ill patient, the amount of carbohydrate catabolized for metabolic fuel, and CO2 production is proportional to the amount administered [15]. CO2 production is also related to over-prescription of calories [16] and can produce hypercapnia in patients where the pulmonary reserve is limited, increasing days of mechanical ventilation [17]. Moreover, administration of >100% of the calories of resting energy expenditure, estimated by indirect calorimetry, has been shown to be associated with an increased mortality rate. In patients who received >70% of calories of resting energy expenditure, the number of days of mechanical ventilation that they required and the duration of their stay in the intensive care unit (ICU) were increased [12]. The Tight Calorie Control Study (TICACOS) showed similar results: Patients who received more calories did not have a higher survival rate, but they required more days of mechanical ventilation and stayed longer in the ICU [18]. Moreover, administering calories in excess of a patient’s energy requirements may lead to liver dysfunction and non-alcoholic fatty liver disease [19,20].
Multiple studies and meta-analyses have focused on undernutrition in recent years. These studies were heterogeneous, but none of them showed an increase in survival. In some of the studies in which a protein intake >1 g/kg/d was maintained, the incidence of nosocomial infections decreased, but this had no impact on mortality. Therefore, patients in critical condition require an adequate calorie intake (with indirect calorimetry is used as the gold standard for estimating energy expenditure), and a high protein intake (from 1.2 up to 2 g/kg/d, according to the latest guidelines) [21,22].
3.2. Fluid Overload
Fluid overload can be caused by failing to reduce the volume of fluids administered after the patient becomes stabilised. The volume of fluid required must be re-evaluated after prescribing nutritional support. The fluid requirement of adults with a normal hydration status is approximately 30 to 40 ml/kg/d [23], but it also depends on the patient’s underlying clinical condition and needs to be individualised. When calculating the total volume of PN, secondary sources of fluid inputs must be considered. Otherwise, PN can lead to fluid overload (hypervolaemia). A positive fluid balance is known to be associated with higher mortality and morbidity among ICU patients [24]. Patients with pre-existing fluid retention due to underlying cardiac and hepatic disease are more likely to deteriorate in condition while receiving PN [25]. On the other hand, during illness, there are multiple sources of fluid losses, such as nasogastric suctioning, vomiting, diarrhea and fistula drainage. Such losses must be replaced to prevent fluid deficits, and the PN solution must be adjusted accordingly. All patients receiving PN should have their fluid input and output monitored and recorded accurately.
3.3. Metabolic Complications of Electrolyte and Acid-Base Imbalance
Potassium is the most abundant intracellular cation. Potassium requirements range from 0.5 to 1.5 mmol/kg/d. Hypokalaemia is the most common electrolyte abnormality and is caused by the displacement of potassium from the extracellular space into the intracellular space as a result of metabolic alkalosis, refeeding syndrome, or the administration of insulin, catecholamines, and other drugs, such as diuretics and glucocorticoids [26]. Hypokalaemia can be treated by increasing intravenous potassium administration. Hypokalaemia is usually associated with hypomagnesaemia, and magnesium should be replenished before administering potassium because magnesium deficiency increases renal potassium losses and disrupts the equilibrium of the sodium–potassium ATPase pump [27]. Conversely, hyperkalaemia is less frequent and is usually related to impaired renal function, but it can also occur as a result of metabolic respiratory acidosis or administration of drugs, such as angiotensin-converting enzyme inhibitors, β-blockers, potassium-sparing diuretics, and nonsteroidal anti-inflammatory drugs [28].
Hypocalcemia is a common finding in critically ill patients. The aetiology of hypocalcemia is uncertain and potentially multifactorial, and the prevalence varies widely depending on the different underlying diseases and comorbidity [29,30]
Magnesium is an important cofactor in more than 3,000 enzyme reactions involving adenosine triphosphate (ATP) [31]. It also regulates the movement of calcium into smooth muscle cells to maintain cardiac contractile strength and peripheral vascular tone. Hypomagnesaemia is commonly observed in critically ill patients, and clinical manifestations include cardiac arrhythmias, muscle weakness, hyperreflexia, and hypokalaemia [26]. Magnesium intake for most patients ranges from 24 to 32 meq/day, whereas higher amounts can be required for patients with diarrhea [32]. Hypermagnesaemia is uncommon and typically only seen in patients with renal insufficiency and in patients who have received high doses of magnesium supplements.
Phosphorus is a major component in ATP production. Providing excessive intravenous dextrose calories, or a large increase in the amount of PN administered leads to increased insulin secretion and redistribution of phosphate from the extracellular fluid to the intracellular space [26]. Common signs of hypophosphataemia include ataxia, confusion, weakness, fatigue, muscle necrosis, and cardiac or respiratory failure. Most critically ill patients require about 0.32 mmol/d. An excess in phosphorus provision besides an impaired excretion due to renal insufficiency can lead to hyperphosphataemia. [25]
Excessive parenteral chloride administration can contribute to metabolic acidosis, while an excess of acetate salts can cause metabolic alkalosis. Although PN should not be used for correcting the acid–base balance, an increase in the intake of chlorine salts helps to correct metabolic alkalosis. Conversely, acetate is converted to the equivalent amount of bicarbonate, so higher levels of acetate salts can correct the bicarbonate deficit in patients with diarrhea and fluid loss through fistulae [33].
3.4. Hypertriglyceridaemia
Hypertriglyceridaemia is a well-known metabolic complication of medical nutrition therapy and is primarily associated with fat administration as part of PN. The prevalence of hypertriglyceridaemia ranges from 6% to 38%, depending upon the patient population studied and the definition of hypertriglyceridaemia used [34].
Hypertriglyceridaemia is caused not only by an excessive dose of lipids in PN but also by a drug-induced suppression of lipoprotein lipase or stimulation of lipogenesis induced by excessive carbohydrate ingestion. Therefore, hypertriglyceridaemia in patients in critical condition must be understood as an imbalance between fat administration and plasma fat clearance capacity. Several other factors are known to increase the risk of hypertriglyceridaemia during PN. These include the fat-overload syndrome (>3–4 g/Kg of lipids infused), renal failure, administration of high doses of corticosteroids (>0.5 mg/kg/d), sepsis, pancreatitis, hyperglycaemia (>180 mg/dL), whereas heparin infusion (>3 mg/kg/d) has shown protective effects that can be related to lipoprotein lipase stimulation [35]. In critically ill patients, blood triglyceride levels can be reduced by using the latest generation lipids [36]. Propofol is an anaesthetic substance commonly used in critically ill patients and is formulated as a lipid emulsion in 10% soybean oil. The use of propofol can lead to hypertriglyceridaemia, especially in patients with sepsis [37] Devlin et al. [38], reported on a case-series of 159 patients treated with propofol, of whom 18% had hypertriglyceridaemia, and 21% had triglyceride levels >1000 mg/dL.
There is no consensus regarding the classification of levels of hypertriglyceridaemia or methods to manage hypertriglyceridaemia in patients receiving PN. Currently, the recommended lipid intake for patients receiving PN varies from 0.7 to 1.5 g/kg/d in critically ill patients [39]. It has been proposed that the lipid level in PN be reduced if patients have low or moderate plasma triglyceride levels [40] and that lipids be withdrawn in patients with plasma triglyceride levels in the 400 mg/dL [41] to 1000 mg/dL range [42]. When cyclic nutrition is applied, the optimal time to measure triglycerides is the 6 to 8 hours trough, and not while lipids are being infused.
Intestinal failure-associated liver disease (IFALD) is a hepatic dysfunction secondary to intestinal failure in the presence of PN, and it has a range of manifestations. The prevalence of IFALD in adults receiving PN ranges from 15% to 85%, and its occurrence and severity increase with longer duration of PN [43,44].
3.5. Hepatobiliary Disorders Associated with Parenteral Nutrition
PN-associated cholestasis (PNAC) is a serious complication which may progress to cirrhosis and to liver failure. Patients with PNAC have an elevated conjugated bilirubin (>2 mg/dL) and increased serum gamma-glutamyltransferase and alkaline phosphatase. Gallbladder stasis is generally related to a lack of enteral stimulation rather than the PN infusion [45]. The aetiology of the hepatic complications in patients receiving PN is unclear, but there are some risk factors that contribute to IFALD. Providing excess nutrients, particularly carbohydrates and lipids results in fat deposition in the liver and contributes to essential fatty acid deficiency, leading to the development of steatosis [46]. Continuous infusion of nutrients can also increase the risk of hepatic complications by causing hyperinsulinaemia [26]. Dosing, source and the phytosterol content of the fat emulsions should all be considered to prevent the development of steatosis and cholestasis [26]. The new generation of fat emulsions containing a combination of soya bean oil, olive oil, fish oil, and medium-chain triglycerides have anti-inflammatory properties, higher antioxidant content, and are less likely to cause cholestasis [46]. In patients receiving PN, other risk factors for liver injury include essential fatty acid deficiency, taurine deficiency and hypermagnesaemia [47].
Prevention of IFALD may include different strategies, such as decreasing the macronutrient content of PN, especially the dextrose content, providing cyclic PN and, most importantly, switching to enteral nutrition as soon as possible [26].
3.6. Metabolic Bone Disease
PN is associated with loss of bone calcium and low bone density, with reported prevalence as high as 84% in patients receiving PN for an extended period [48]. The aetiology of metabolic bone disease (MBD) is poorly understood and may be related to various components of PN and patients’ underlying risk factors.
An excess of amino acid in PN, administered during repletion, can cause hypercalciuria and negative total calcium balance. Low calcium and phosphate intake can also lead to the development of MBD. There is a limitation on PN calcium dosing due to physical compatibility of calcium and phosphorus. PN formulations should contain ≥15 mEq/d of calcium and 20 to 40 mmol/d of phosphate to prevent excessive calcium excretion [47,49]
3.7. Hyperglycaemia
Hyperglycaemia is the most common metabolic complication of artificial nutrition. PN formulations are usually initiated at 2 g/kg/d of glucose to prevent the gluconeogenesis derived from amino acid precursors provided by skeletal muscle proteolysis. Administration of >4 mg/kg/min often leads to hyperglycaemia [47]. The prevalence of hyperglycaemia in patients receiving PN is high and has exceeded 40% in some studies [50,51]. In patients receiving PN, hyperglycaemia is associated with increased mortality, infections, organ dysfunction, and longer hospitalisation [52,53].
During the first 24 hours after starting PN, blood glucose should be measured at least 4-hourly in critically ill patients, and the frequency of blood glucose monitoring should only be decreased once the patient has stabilised, usually after about 48 hours [26]. There is a lack of consensus regarding the optimal blood glucose range, especially as tight control is associated with an increased risk of hypoglycaemia and an increased risk of death [54]. The American Society for Parenteral and Enteral Nutrition (ASPEN) recommends that blood glucose be maintained in the 140–180 mg/dL range [22] for adult patients who are critically ill, but the European Society for Clinical Nutrition and Metabolism (ESPEN) does not give any specific recommendation [21].
3.8. Hypersensitivity
Hypersensitivity to the components of PN is a rare but an important complication which can cause problems ranging from minor symptoms, such as pruritus, [55] to life-threatening conditions, such as anaphylaxis [56]. In a recent systematic review, the components of PN most frequently identified as allergens were fat emulsions multivitamin solutions [57].
3.9. Refeeding Syndrome
Refeeding syndrome is a complex metabolic phenomenon related to the depletion of intracellular resources, minerals (phosphate, potassium, and magnesium), vitamins (thiamine), and trace elements caused by the reactivation of metabolism in previously underfed patients [58]. Patients with a low BMI, unintentional weight loss in the previous few months, little nutritional intake for >10 days, or with abnormal plasma potassium, phosphate, or magnesium levels are at risk of refeeding syndrome after receiving nutritional support. Clinical symptoms of refeeding syndrome vary widely. Phosphate is present in energy transfer reactions, nervous and cardiac conduction systems, and other membrane-mediated cellular functions in the renal, haematological, muscular, and immunological systems. During the transition from PN to regular feeding, intracellular phosphate depletion can be prevented by gradually increasing calorie intake following calorie restriction, thiamine and electrolyte supplementation, and electrolyte monitoring [59].
4. Monitoring Requirements
Appropriate design of MNT requires an evaluation of nutritional risk, nutritional access, and quantitative and qualitative composition of the supplemental nutrition components, including water, electrolytes, calories (lipid and non-lipid calories) and protein [6,21,60,61].
To increase awareness regarding inappropriate MNT and to improve monitoring, we propose introducing the word “nutritrauma” as a new term in clinical nutrition [9], defined as metabolic adverse events related to an inadequate nutritional assessment and inappropriate prescription of MNT (in terms of timing, route of administration, and quantitative and qualitative composition). We recommend that non-metabolic complications of supplemental nutrition, such as infections (e.g., catheter-related bacteraemia and nasogastric tube-associated sinusitis), mechanical and vascular complications (e.g., non-occlusive intestinal ischemia), not be included in the definition because these complications require other forms of management and different resources.
Defining nutritrauma monitoring as a key safety indicator would enable nutritional support to be included in quality and safety improvement programmes. Independently of nutritrauma incidence, adding nutritrauma monitoring to such programmes may help to draw attention to the relevance of nutritional support and the need to develop a standardised approach to providing nutritional support, reducing variability and non-evidence-based management. This approach could also enable more professionals to become involved with nutritional management as a life support technique. In Table 3, we propose a definition for “monitoring nutritrauma” as a safety indicator.
Table 3.
Establishing nutritrauma monitoring as a key safety indicator.
| Indicator Name | Nutritrauma Monitoring |
|---|---|
| Area | Safety |
| Justification | Inappropriate dosage of medical nutrition therapy is associated with greater morbidity and mortality in the critically ill patient. Monitoring the components of nutritional support can assist in recovery and improve prognosis |
| Formula | (No. of patients monitored) × 100 ÷ (No. of patients with medical nutritional support) |
| Explanation of terms | Monitoring of nutritrauma includes: An initial assessment of the nutritional status Assessment of calorie and protein requirements Monitoring of the administration of supplemental nutrition Monitoring water balance Monitoring of hypoglycaemia and hyperglycaemia Monitoring the incidence of uraemia not attributable to renal failure Monitoring the incidence of hypolipidaemia and hyperlipidaemia Monitoring the incidence of dyselectrolytaemia Monitoring the incidence of hepatopathy |
| Population | All critically ill patients who receive medical nutritional support |
| Type | Process |
| Data source | Medical records and clinical information systems |
| Standard | 100% |
5. Conclusions
Is well established that inappropriate MNT is associated with metabolic complications that affect the prognosis of critically ill patients. Introducing the concept of nutritrauma, defined as iatrogenic metabolic effects of MNT, in clinical practice could be a useful means of increasing awareness of the need for thorough nutritional assessment and appropriate prescription of MNT, and could facilitate monitoring strategies, thus reducing adverse events related to nutritional support. Moreover, monitoring the occurrence of nutritrauma should be considered to be a safety indicator. Monitoring and reporting of nutritrauma in critically ill patients should be implemented without delay.
Author Contributions
J.C.Y., L.C. and I.M.d.L. developed the initial concept of Nutritrauma. The concept was discussed by the Working Group on Nutrition and Metabolism of the Spanish Society of Critical Care. All the authors contributed to the design of the paper, revised it critically and gave final approval to the submitted version.
Funding
This research received no external funding.
Conflicts of Interest
The authors have no conflict of interest to declare.
References
- 1.Gordo Vidal F., Delgado Arnaiz C., Calvo Herranz E. Mechanical ventilation induced lung injury. Med. Intensiva. 2007;31:18–26. doi: 10.1016/S0210-5691(07)74765-4. [DOI] [PubMed] [Google Scholar]
- 2.Akhoundi A., Singh B., Vela M., Chaudhary S., Monaghan M., Wilson G.A., Dillon J.J., Cartin-Ceba R., Lieske J.C., Gajic O., et al. Incidence of Adverse Events during Continuous Renal Replacement Therapy. Blood Purif. 2015;39:333–339. doi: 10.1159/000380903. [DOI] [PubMed] [Google Scholar]
- 3.International Consensus Conferences in Intensive Care Medicine Ventilator-associated lung injury in ARDS. American Thoracic Society, European Society of Intensive Care Medicine, Societé de Réanimation Langue Française. Intensive Care Med. 1999;25:1444–1452. doi: 10.1164/ajrccm.160.6.ats16060. [DOI] [PubMed] [Google Scholar]
- 4.Maynar Moliner J., Honore P.M., Sánchez-Izquierdo Riera J.A., Herrera Gutiérrez M., Spapen H.D. Handling continuous renal replacement therapy-related adverse effects in intensive care unit patients: The dialytrauma concept. Blood Purif. 2012;34:177–185. doi: 10.1159/000342064. [DOI] [PubMed] [Google Scholar]
- 5.Gattinoni L., Marini J.J., Collino F., Maiolo G., Rapetti F., Tonetti T., Vasques F., Quintel M. The future of mechanical ventilation: Lessons from the present and the past. Crit. Care. 2017;21:183. doi: 10.1186/s13054-017-1750-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wischmeyer P.E. Tailoring nutrition therapy to illness and recovery. Crit. Care. 2017;21(Suppl. S3):316. doi: 10.1186/s13054-017-1906-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arabi Y.M., Casaer M.P., Chapman M., Heyland D.K., Ichai C., Marik P.E., Martindale R.G., McClave S.A., Preiser J.-C., Reignier J., et al. The intensive care medicine research agenda in nutrition and metabolism. Intensive Care Med. 2017;43:1239–1256. doi: 10.1007/s00134-017-4711-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schindler K., Pichard C., Sulz I., Volkert D., Streicher M., Singer P., Ljungqvistf O., Van Gossumg A., Bauerc P., Hiesmayrh H. NutritionDay: 10 years of growth. Clin. Nutr. 2017;36:1207–1214. doi: 10.1016/j.clnu.2016.11.004. [DOI] [PubMed] [Google Scholar]
- 9.Cederholm T., Barazzoni R., Austin P., Ballmer P., Biolo G., Bischoff S.C., Compher C., Correia I., Higashiguchi T., Holst M., et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin. Nutr. 2017;36:49–64. doi: 10.1016/j.clnu.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 10.Fuentes Padilla P., Martínez G., Vernooij R.W.M., Cosp X.B., Alonso-Coello P. Nutrition in critically ill adults: A systematic quality assessment of clinical practice guidelines. Clin. Nutr. 2016;35:1219–1225. doi: 10.1016/j.clnu.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 11.Weijs P.J., Stapel S.N., de Groot S.D., Driessen R.H., de Jong E., Girbes A.R., Rob J.M., van Schijndel S., Beishuizen A. Optimal protein and energy nutrition decreases mortality in mechanically ventilated, critically ill patients: A prospective observational cohort study. J. Parenter. Enter. Nutr. 2012;36:60–68. doi: 10.1177/0148607111415109. [DOI] [PubMed] [Google Scholar]
- 12.Zusman O., Theilla M., Cohen J., Kagan I., Bendavid I., Singer P. Resting energy expenditure, calorie and protein consumption in critically ill patients: A retrospective cohort study. Crit. Care. 2016;20:367. doi: 10.1186/s13054-016-1538-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shaw J.H., Wolfe R.R. An integrated analysis of glucose, fat, and protein metabolism in severely traumatized patients. Studies in the basal state and the response to total parenteral nutrition. Ann. Surg. 1989;209:63–72. doi: 10.1097/00000658-198901000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reintam Blaser A., Berger M.M. Early or Late Feeding after ICU Admission? Nutrients. 2017;9:1278. doi: 10.3390/nu9121278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jebb S.A., Prentice A.M., Goldberg G.R., Murgatroyd P.R., Black A.E., Coward W.A. Changes in macronutrient balance during over- and underfeeding assessed by 12-d continuous whole-body calorimetry. Am. J. Clin. Nutr. 1996;64:259–266. doi: 10.1093/ajcn/64.3.259. [DOI] [PubMed] [Google Scholar]
- 16.Talpers S.S., Romberger D.J., Bunce S.B., Pingleton S.K. Nutritionally associated increased carbon dioxide production. Excess total calories vs high proportion of carbohydrate calories. Chest. 1992;102:551–555. doi: 10.1378/chest.102.2.551. [DOI] [PubMed] [Google Scholar]
- 17.Bordeje M.L. Nuestros grandes olvidados, los enfermos respiratorios crónicos. Nutr. Hosp. 2017;34(Suppl. S1):38–45. doi: 10.20960/nh.1238. [DOI] [PubMed] [Google Scholar]
- 18.Singer P., Anbar R., Cohen J., Shapiro H., Shalita-Chesner M., Shaul L., Grozovski E., Theilla M., Frishman S., Madar Z. The Tight Calorie Control Study (TICACOS): A prospective, randomized, controlled pilot study of nutritional support in critically ill patients. Intensive Care Med. 2011;37:601–609. doi: 10.1007/s00134-011-2146-z. [DOI] [PubMed] [Google Scholar]
- 19.Grau T., Bonet A. Caloric intake and liver dysfunction in critically ill patients. Curr. Opin. Clin. Nutr. Metab. Care. 2009;12:175–179. doi: 10.1097/MCO.0b013e3283252f9e. [DOI] [PubMed] [Google Scholar]
- 20.Grau T., Bonet A., Rubio M., Mateo D., Farré M., Acosta J.A., Blesa A., Montejo J.C., de Lorenzo A.G., Mesejo A., et al. Liver dysfunction associated with artificial nutrition in critically ill patients. Crit. Care. 2007;11:R10. doi: 10.1186/cc5670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singer P., Blaser A.R., Berger M.M., Alhazzani W., Calder P.C., Casaer M.P., Hiesmayr M., Mayer K., Montejo J.C., Pichard C., et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin. Nutr. 2019;38:48–79. doi: 10.1016/j.clnu.2018.08.037. [DOI] [PubMed] [Google Scholar]
- 22.McClave S.A., Taylor B.E., Martindale R.G., Warren M.M., Johnson D.R., Braunschweig C., McCarthy M.S., Davanos E., Rice T.W., Cresci G.A., et al. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) JPEN J. Parenter. Enter. Nutr. 2016;40:159–211. doi: 10.1177/0148607115621863. Erratum in: JPEN J. Parenter Enteral Nutr.2016, 40, 1200. [DOI] [PubMed] [Google Scholar]
- 23.Biesalski H.K., Bischoff S.C., Boehles H.J., Muehlhoefer A., Working group for developing the guidelines for parenteral nutrition of The German Association for Nutritional Medicine Water, electrolytes, vitamins and trace elements—Guidelines on Parenteral Nutrition, Chapter 7. Ger. Med. Sci. 2009;7:Doc21. doi: 10.3205/000080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boyd J.H., Forbes J., Nakada T.A., Walley K.R., Russell J.A. Fluid resuscitation in septic shock: A positive fluid balance and elevated central venous pressure are associated with increased mortality. Crit. Care Med. 2011;39:259–265. doi: 10.1097/CCM.0b013e3181feeb15. [DOI] [PubMed] [Google Scholar]
- 25.Rhoda K.M., Porter M.J., Quintini C. Fluid and electrolyte management: Putting aplan in motion. JPEN J. Parenter. Enter. Nutr. 2011;35:675–685. doi: 10.1177/0148607111421913. [DOI] [PubMed] [Google Scholar]
- 26.Davila J., Konrad D. Metabolic Complications of Home Parenteral Nutrition. Nutr. Clin. Pract. 2017;32:753–768. doi: 10.1177/0884533617735089. [DOI] [PubMed] [Google Scholar]
- 27.Whang R., Whang D.D., Ryan M.P. Refractory potassium repletion: A consequence of magnesium deficiency. Arch. Intern. Med. 1992;152:40–45. doi: 10.1001/archinte.1992.00400130066006. [DOI] [PubMed] [Google Scholar]
- 28.Brown R.O., Hamrick K.D., Dickerson R.N., Lee N., Parnell D.H., Jr., Kudsk K.A. Hyperkalemia secondary to concurrent pharmacotherapy in a patient receiving home parenteral nutrition. J. Parenter. Enter. Nutr. 1996;20:429–432. doi: 10.1177/0148607196020006429. [DOI] [PubMed] [Google Scholar]
- 29.Steele T., Kolamunnage-Dona R., Downey C., Toh C.H., Welters I. Assessment and clinical course of hypocalcemia in critical illness. Crit. Care. 2013;3:R106. doi: 10.1186/cc12756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kelly A., Levine M.A. Hypocalcemia in the critically ill patient. J. Intensive Care Med. 2013;28:166–177. doi: 10.1177/0885066611411543. [DOI] [PubMed] [Google Scholar]
- 31.Mirtallo J.M. Introduction to parenteral nutrition. In: Gottschlich M.M., Fuhrman M.P., Hammond K.A., Holcombe B.J., Seidner D.L., editors. The Science and Practice of Nutrition Support. A Case-Based Core Curriculum. Part III: The Clinical Foundations of Nutrition Support. Kendall Hunt Publishing; Dubuque, IA, USA: 2001. pp. 211–222. [Google Scholar]
- 32.Mirtallo J., Canada T., Johnson D., Kumpf V., Petersen C., Sacks G., Seres D., Guenter P. Task Force for the Revision of Safe Practices for Parenteral Nutrition. Safe practices for parenteral nutrition. J. Parenter. Enter. Nutr. 2004;26:S39. doi: 10.1177/0148607104028006S39. [DOI] [PubMed] [Google Scholar]
- 33.Btaiche J.F., Khalidi N. Metabolic complications of parenteral nutrition in adults, Part 1. Am. J. Health Syst. Pharm. 2004;61:1938–1949. doi: 10.1093/ajhp/61.18.1938. [DOI] [PubMed] [Google Scholar]
- 34.Mirtallo J.M., Dasta J.F., Kleinschmidt K.C., Varon J. State of the art review: Intravenous fat emulsions: Current applications, safety profile, and clinical implications. Ann. Pharmacother. 2010;44:688–700. doi: 10.1345/aph.1M626. [DOI] [PubMed] [Google Scholar]
- 35.Llop J., Sabin P., Garau M., Burgos R., Pérez M., Massó J., Cardona D., Sánchez Segura J.M., Garriga R., Redondo S., et al. The importance of clinical factors in parenteral nutrition-associated hypertriglyceridemia. Clin. Nutr. 2003;22:577–583. doi: 10.1016/S0261-5614(03)00082-7. [DOI] [PubMed] [Google Scholar]
- 36.Mateu-de Antonio J., Grau S., Luque S., Marin-Casino M., Albert I., Ribes E. Comparative effects of olive oil-based and soyabean oil-based emulsions on infection rate and leucocyte count in critically ill patients receiving parenteral nutrition. Br. J. Nutr. 2008;99:846–854. doi: 10.1017/S0007114507837433. [DOI] [PubMed] [Google Scholar]
- 37.Devaud J.C., Berger M.M., Pannatier A., Marques-Vidal P., Tappy L., Rodondi N., Voirol C.P. Hypertriglyceridemia: A potential side effect of propofol sedation in critical illness. Intensive Care Med. 2012;38:1990–1998. doi: 10.1007/s00134-012-2688-8. [DOI] [PubMed] [Google Scholar]
- 38.Devlin J.W., Lau A.K., Tanios M.A. Propofol-associated hypertriglyceridemia and pancreatitis in the intensive care unit: An analysis of frequency and risk factors. Pharmacotherapy. 2005;25:1348–1352. doi: 10.1592/phco.2005.25.10.1348. [DOI] [PubMed] [Google Scholar]
- 39.Berger M.M., Reintam-Blaser A., Calder P.C., Casaer M., Hiesmayr M.J., Mayer K., Montejoj J.C., Pichardk C., Preiserl J.-C., van Zantenm A.R.H., et al. Monitoring nutrition in the, I.C.U. Clin. Nutr. 2019;38:584–593. doi: 10.1016/j.clnu.2018.07.009. [DOI] [PubMed] [Google Scholar]
- 40.Braga M., Ljungqvist O., Soeters P., Fearon K., Weimann A., Bozzetti F. ESPEN guidelines on parenteral nutrition: Surgery. Clin. Nutr. 2009;28:378–386. doi: 10.1016/j.clnu.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 41.Visschers R.G., Olde Damink S.W., Gehlen J.M., Winkens B., Soeters P.B., van Gemert W.G. Treatment of hypertriglyceridemia in patients receiving parenteral nutrition. J. Parenter. Enter. Nutr. 2011;35:610–615. doi: 10.1177/0148607110389616. [DOI] [PubMed] [Google Scholar]
- 42.Adolph M., Heller A.R., Koch T., Koletzko B., Kreymann K.G., Krohn K., Pscheidl E., Senkal M., Working group for developing the guidelines for parenteral nutrition of The German Association for Nutritional Medicine Lipid emulsions—Guidelines on parenteral nutrition, Chapter 6. Ger. Med. Sci. 2009;7:Doc22. doi: 10.3205/000081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kumpf V.J., Gervasio J. Complications of parenteral nutrition. In: Mueller C.M., Kovacevich D.S., McClave S.A., Stephen A.M., Schwartrz D.B., Miller S.J., editors. The ASPEN Nutrition Support Core Curriculum. 2nd ed. ASPEN; Silver Spring, MD, USA: 2012. pp. 284–298. [Google Scholar]
- 44.Cavicchi M., Beau P., Crenn P., Degott C., Messing B. Prevalence of liver disease and contributing factors in patients receiving home parenteral nutrition for permanent intestinal failure. Ann. Intern. Med. 2000;132:525–532. doi: 10.7326/0003-4819-132-7-200004040-00003. [DOI] [PubMed] [Google Scholar]
- 45.Kumpf V. Parenteral nutrition-associated liver disease in adult and pediatric patients. Nutr. Clin. Pract. 2006;21:279–290. doi: 10.1177/0115426506021003279. [DOI] [PubMed] [Google Scholar]
- 46.Anez-Bustillos L., Dao D.T. Intravenous fat emulsion formulations for the adult and pediatric patient: Understanding the differences. Nutr. Clin. Pract. 2016;31:596–609. doi: 10.1177/0884533616662996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lappas B.M., Patel D., Kumpf V., Adams D.W., Seidner D.L. Parenteral Nutrition: Indications, Access, and Complications. Gastroenterol. Clin. N. Am. 2018;47:39–59. doi: 10.1016/j.gtc.2017.10.001. [DOI] [PubMed] [Google Scholar]
- 48.Pironi L., Labate A.M., Pertkiewicz M., Przedlacki J., Tjellesen L., Staun M., De Francesco A., Gallenca P., Guglielmi F.W., Van Gossum A.N.D.R.É, et al. Prevalence of bone disease in patients on home parenteral nutrition. Clin. Nutr. 2002;21:289–296. doi: 10.1054/clnu.2002.0548. [DOI] [PubMed] [Google Scholar]
- 49.Verhage A.H., Cheong W.K., Allard J.P., Jeejeebhoy K.N., Harry M. Vars Research Award. Increase in lumbar spine bone mineral content in patients on long-term parenteral nutrition without vitamin D supplementation. J. Parenter. Enter. Nutr. 1995;19:431–436. doi: 10.1177/0148607195019006431. [DOI] [PubMed] [Google Scholar]
- 50.Pleva M., Mirtallo J.M., Steinberg S.M. Hyperglycemic events in non-intensive care unit patients receiving parenteral nutrition. Nutr. Clin. Pract. 2009;24:626–634. doi: 10.1177/0884533609339069. [DOI] [PubMed] [Google Scholar]
- 51.Gosmanov A.R., Umpierrez G.E. Management of hyperglycemia during enteral and parenteral nutrition therapy. Curr. Diabetes Rep. 2013;13:155–162. doi: 10.1007/s11892-012-0335-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ziegler T.R. Parenteral nutrition in the critically ill patient. N. Engl. J. Med. 2009;361:1088–1097. doi: 10.1056/NEJMct0806956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kumar P.R., Crotty P., Raman M. Hyperglycemia in hospitalized patients receiving parental nutrition is associated with increased morbidity and mortality: A review. Gastroenterol. Res. Pract. 2011;10:1155. doi: 10.1155/2011/760720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Finfer S., Chittock D.R., Su S.Y., Blair D., Foster D., Dhingra V., Bellomo R., Cook D., Dodek P., Henderson W.R., et al. Intensive versus conventional glucose control in critically ill patients. New Engl. J. Med. 2009;360:1283–1297. doi: 10.1056/NEJMoa0810625. [DOI] [PubMed] [Google Scholar]
- 55.Buchman A.L., Ament M.E. Comparative hypersensitivity in intravenous lipid emulsions. J. Parenter. Enter. Nutr. 1991;15:345–346. doi: 10.1177/0148607191015003345. [DOI] [PubMed] [Google Scholar]
- 56.Market A.D., Lew D.B., Schropp K.P., Hak E.B. Parenteral nutrition-associated anaphylaxis in a 4-year-old child. J. Pediatr. Gastroenterol. Nutr. 1998;26:229–231. doi: 10.1097/00005176-199802000-00022. [DOI] [PubMed] [Google Scholar]
- 57.Christian V.J., Tallar M., Walia C.L.S., Sieracki R., Goday P.S. Systematic Review of Hypersensitivity to Parenteral Nutrition. J. Parenter. Enter. Nutr. 2018;42:1222–1229. doi: 10.1002/jpen.1169. [DOI] [PubMed] [Google Scholar]
- 58.Mehanna H.M., Moledina J., Travis J. Refeeding syndrome: What it is, and how to prevent and treat it. BMJ. 2008;336:1495–1498. doi: 10.1136/bmj.a301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Boot R., Koekkoek K.W.A.C., van Zanten A.R.H. Refeeding syndrome: Relevance for the critically ill patient. Curr. Opin. Crit. Care. 2018;24:235–240. doi: 10.1097/MCC.0000000000000514. [DOI] [PubMed] [Google Scholar]
- 60.Bonet Saris A., Márquez Vácaro J.A., Serón Arbeloa C., Metabolism and Nutrition Working Group of the Spanish Society of Intensive Care Medicine and Coronary units Guidelines for specialized nutritional and metabolic support in the critically ill patient: Update. Consensus SEMICYUC-SENPE: Macronutrient and micronutrient requirements. Nutr. Hosp. 2011;26(Suppl. S2):16–20. doi: 10.1016/s0210-5691(11)70004-3. [DOI] [PubMed] [Google Scholar]
- 61.Fernández-Ortega J.F., Herrero Meseguer J.I., Martínez García P., Metabolism and Nutrition Working Group of the Spanish Society of Intensive Care Medicine and Coronary units Guidelines for specialized nutritional and metabolic support in the critically ill patient: Update. Consensus SEMICYUC-SENPE: Indications, timing and routes of nutrient delivery. Nutr. Hosp. 2011;26(Suppl. S2):7–11. doi: 10.1590/S0212-16112011000800002. [DOI] [PubMed] [Google Scholar]