Abstract
A doubling of Australian expenditure on mental health services over two decades, inflation-adjusted, has reduced prevalence of neither psychological distress nor mental disorders. Low rates of help-seeking, and inadequate and inequitable delivery of effective care may explain this partially, but not fully. Focusing on depressive disorders, drawing initially on ideas from the work of philosopher and socio-cultural critic Ivan Illich, we use evidence-based medicine statistics and simulation modelling approaches to develop testable hypotheses as to how iatrogenic influences on the course of depression may help explain this seeming paradox. Combined psychological treatment and antidepressant medication may be available, and beneficial, for depressed people in socioeconomically advantaged areas. But more Australians with depression live in disadvantaged areas where antidepressant medication provision without formal psychotherapy is more typical; there also are urban/non-urban disparities. Depressed people often engage in self-help strategies consistent with psychological treatments, probably often with some benefit to these people. We propose then, if people are encouraged to rely heavily on antidepressant medication only, and if they consequently reduce spontaneous self-help activity, that the benefits of the antidepressant medication may be more than offset by reductions in beneficial effects as a consequence of reduced self-help activity. While in advantaged areas, more comprehensive service delivery may result in observed prevalence lower than it would be without services, in less well-serviced areas, observed prevalence may be higher than it would otherwise be. Overall, then, we see no change. If the hypotheses receive support from the proposed research, then implications for service prioritisation and delivery could include a case for wider application of recovery-oriented practice. Critically, it would strengthen the case for action to correct inequities in the delivery of psychological treatments for depression in Australia so that combined psychological therapy and antidepressant medication, accessible and administered within an empowering framework, should be a nationally implemented standard.
Keywords: Mental health services, epidemiology, side effects (treatment), health behaviour, iatrogenesis
Introduction
The paradox: an outline
Australian mental health care expenditure per-person has increased in real terms through two decades by nearly 100%, and by 30% in the last decade (Meadows et al., 2018). The National Mental Health Strategy and the National Action Plan for Mental Health have guided large-scale mental health care investments, including the Better Access to Mental Health Care (‘Better Access’) programme, greatly increasing psychological services delivery (Jorm, 2018). But, Australian community health survey findings suggest no change from 2001 to 2014 in prevalence of the higher scores on the Kessler 10 instrument commonly associated with clinically significant mental health problems (Meadows et al., 2018). The two specific mental health surveys conducted in Australia in 1997 and 2007 also did not show decreasing prevalence (Jorm et al., 2017) while population health impact of ‘Better Access’ has yet to be detected (Jorm, 2018).
So, as others have highlighted in this journal, we have a seeming paradox to resolve (Mulder et al., 2017): why has more expenditure and more treatment not led to an identifiable decrease in prevalence? This is unlikely to have any one explanation. Contributory causes may include increasing inequality driving an underlying prevalence increase (Wilkinson and Pickett, 2018), possibly exacerbated by social, demographic, cultural and environmental changes in the cities (O’Hanlon, 2018), where most Australians live. These might have important implication for policy, widely framed. Considering healthcare more narrowly, perhaps the threshold for a population-level effect has not been reached yet (Meadows et al., 2018), but in which case, we might ask when might that threshold be crossed, and could anything be done to bring that time forward?
This paper will focus on healthcare planning, delivery and education, where there have been proposals for major services redesign and reorientation (Van Os et al., 2019) and the suggestion that ‘We need to, at the least, consider whether our current mental health systems might be causing unintentional harm in some areas. It is possible that in order to achieve better outcomes, we need to do less, not more’ (Mulder et al., 2017). We suggest a possible contributing mechanism that might indeed be causing unintentional harm, or iatrogenesis, and so contributing to this worrying situation. As a theoretical contribution in a scientific journal, the paper includes testable hypotheses. If supported from currently available or newly collected evidence, these might indicate in some cases doing less while suggesting that some of the doing might be better done differently or more comprehensively. Focusing on depressive disorders as a high-prevalence group of problems with a good treatment evidence base, and of indisputable importance for mental health policy, enables us to draw on diagnostic-specific sources of evidence. However, the findings may have broader implications diagnostically. Although the argument will be developed for Australia as a high-income country, there may be implications for other national contexts.
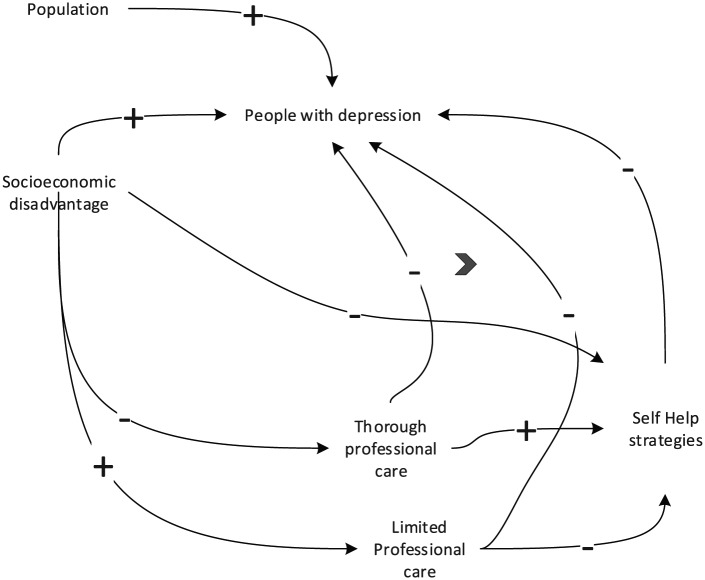
The active coping strategies of the population
People may employ various self-help strategies in response to depression, some of which might also be advised in psychological or psychosocial treatments, such as ‘Doing more things you enjoy’, ‘Exercise’, ‘Being with pets’ or ‘Meditation’. A cross-sectional community study found that with increasing depression severity, self-help strategies were reported less commonly (Jorm et al., 2004). The explanation suggested for this was ‘overlapping waves of action’ (Figure 1 – arrows have been added and are discussed later). That is, self-help strategies were employed as initial responses. If disorder severity increased, faith in self-help was reduced; these strategies might then be abandoned in favour of professional help-seeking. This then was seen as explaining why, among those with more severe disorders, self-help strategies were less frequently reported when rates of professional help were higher.
Figure 1.
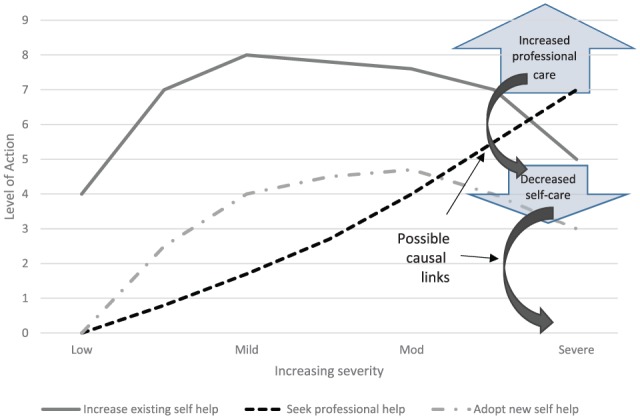
Overlapping waves of action in help-seeking for medical care.
Source: Adapted from Jorm et al. (2004) (Figure 2; p. 298).
Iatrogenesis considered
During the mid-1970s, the Austrian social theorist Ivan Illich (Hartch, 2015), influential then in social work, education and sociology, provided a critical perspective on directions being taken by modern medicine. Proposing that medicalisation of life problems had extended beyond the bounds of conditions where there was convincing evidence that medicine could help, and that in various ways the medical establishment was a source of disability as much or more than of therapeutic benefit, Illich (1976) expanded the concept of iatrogenesis or physician-caused illness beyond prior usage, suggesting a threefold nature for iatrogenesis: clinical, social and cultural – of which our summary follows.
Clinical iatrogenesis is a regularly used concept. Here, we may consider medication side effects, whether the nausea and sexual dysfunction commonly associated with serotonin-specific reuptake inhibitors or the weight gain and metabolic disturbance associated with antipsychotics which may also be used in treatment of depression.
Social iatrogenesis may occur where there is a clear expectation that people with some aspects of experience that become labelled as a mental disorder will seek help and primarily address those experiences through interactions with professional healthcare and the following of given advice. Specifically, this becomes iatrogenic if the following of this advice results in the reliance on an intervention that may on occasions be less effective than options for action otherwise in the repertoire of the individual or their community resources.
Cultural iatrogenesis can be identified if we see cultural norms shifting such that certain kinds of human experience that might be classed as normal aspects of the human condition lose that validated status. Here, we may consider the present-day functioning of social media with its encouragement to present a positive, buoyant picture of the self and where sharing normal human weaknesses and troubles may lead to ostracism and ridicule as forms of bullying.
Effectiveness of key interventions for depression
Recent meta-analysis work examined depression-remission associated with antidepressant medications (ADM) compared to placebos (Cipriani et al., 2018). The odds ratio (OR) reported for widely currently used ADMs was around 1.7. The implied number needed to treat (NNT), not provided in the article, can be estimated. Given the typical response rate in antidepressant studies through time of 30–40% (Furukawa et al., 2016), such an OR can be achieved with an NNT of 8; working: ADM response typically 47.7% vs 35.0% with placebo; OR = (47.7/52.3)/(35.0/65.0) = 1.7; absolute risk reduction (ARR) = 47.7–35.0% = 12.7%; and NNT = 1/ARR = 8. So typically, in a group of eight people given placebo or ADM for 8 weeks, in the placebo group, three will recover; while in the ADM group, four will recover. This difference might increase with more severe depression but decrease if diagnosis and treatment in primary mental health care were less well controlled than in analysed studies. NNT for typical psychological treatments of depression has been estimated as around 4 (Cuijpers et al., 2016).
Resolving the paradox: some contributions
Other ways of framing some of our proposals include drawing on concepts from health psychology, the social sciences or writings that might be termed antipsychiatry. In this paper, we concentrate on Illich’s formulation of social iatrogenesis while signposting possible influences of clinical and cultural iatrogenesis. We suggest this organising framework is one that lends itself to informing an epidemiological and clinical research programme.
We propose that when people with depression engage with healthcare delivered within a biomedical rather than either a biopsychosocial or recovery paradigm, they may transfer expectation of agency for recovery from themselves to the treating practitioner and prescribed treatments. They may then reduce their application of self-help strategies which may have considerable effectiveness for some people. So, the reduction in self-help disadvantages recovery. If the healthcare provided is of high potency for symptom reduction and functional restoration, this may not compromise clinical outcomes. But, if that care is of marginal or even no individual benefit, delivered in ways that discourage a sense of personal efficacy, or if benefit is outweighed by effects of clinical iatrogenesis – then, the overall intervention effect, in a variable number of cases, may be negative. In the case of ADM monotherapy, negative effects would follow if more benefit was lost from self-help actions suspended than the ADM effect (NNT ≃ 8, see above). Smaller NNTs imply greater effect, so self-help actions suspended would need to have an NNT less than 8. In the case of combined ADM (NNT ≃ 8) and psychotherapy (NNT ≃ 4), the benefit lost from suspended self-help actions would need to be considerably larger for negative effects to follow.
While accessible and respected Internet sources sometimes emphasise active personal and social coping strategies, there are prominent examples where a strong message is conveyed that professional help-seeking is central to recovery, for example, ‘The important thing is finding the right treatment and the right health professional for your needs’ (Beyondblue: the national depression initiative, 2018; italics added). Undoubtedly, there are people for whom early access to professional care will make a real difference to outcome, but, if that access is achieved at the cost of autonomy and empowerment with promotion of passivity in treatment, then results may be mixed. Stage-specific interventions may help determine who may benefit most from which kind of message, but without that, we suggest there is potential for harm.
To illustrate the proposition, we return to Figure 1 and the arrows added to this adaptation of the original figure. For some people who show the combination of professional care seeking, lower self-help and increased symptoms, it becomes possible that their symptom status may be directly or indirectly consequential on their seeking professional help, rather than this help-seeking being a consequence of the greater symptoms. The greater symptom severity can be a consequence of forms of iatrogenesis, rather than – or as well as – a determinant of greater intensity of service contact, and a positive feedback loop might operate here.
In many socioeconomically disadvantaged, regional or remote areas, depressed people are more likely to get general practitioner (GP) care than specialist, interdisciplinary or multidisciplinary care. Busy GPs in such areas, even if skilled and committed, may not themselves be able to add substantial psychological treatment to ADM prescription while psychology referral may not be available (Meadows et al., 2018). Pharmaceutical marketing to GPs and medicalised public information both will influence the patient–doctor interaction. So, combined modality treatment – featuring diagnostic caution then desirably nuanced endorsement of ADM effects, while respecting and encouraging self-help – may be less common in such areas. Instead, more simply medicalised, potentially iatrogenic, treatment may dominate.
Table 1 presents area-specific disadvantage quintile rates for elevated psychological-distress and population sizes, estimating where people with very-high K10 scores live. Thirty percent of those with very-high K10 live in areas of greatest disadvantage by quintile, while 9% come from the least disadvantaged quintile. Possibly then, more people with depression receive limited, potentially iatrogenic care than more thorough, comprehensive care relatively lacking these risks. People in more socioeconomically deprived areas may have lower coping resources by virtue of educational, status or social capital variables, also greater income stress and other social determinants of depression. These may indicate more need for interdisciplinary or multidisciplinary care rather than less. These differential impacts in different geographical areas, while objectionable on social-justice grounds, might present quasi-experimental opportunities for collecting evidence bearing on these propositions.
Table 1.
Estimated population by socioeconomic disadvantage quintiles with very-high Kessler 10 scores.
| IRSDa quintiles: least (1) to greatest (5) disadvantage | Population (2016) Age: 16–64 yearsb |
Estimated population % of very-high K10c | Estimated number of people with very-high K10d | % of all Australians with very-high K10e |
|---|---|---|---|---|
| Capital cities | ||||
| 1 | 2,617,180 | 1.6 | 41,875 | 8 |
| 2 | 2,383,572 | 3.1 | 73,891 | 14 |
| 3 | 1,902,530 | 3.9 | 74,199 | 14 |
| 4 | 1,549,484 | 4.5 | 69,727 | 13 |
| 5 | 1,467,165 | 5.4 | 79,227 | 15 |
| Other areas | ||||
| 1 | 297,417 | 2.5 | 7435 | 1 |
| 2 | 607,052 | 2.9 | 17,605 | 3 |
| 3 | 1,007,006 | 3.5 | 35,245 | 7 |
| 4 | 1,323,931 | 3.6 | 47,662 | 9 |
| 5 | 1,302,272 | 6.1 | 79,439 | 15 |
| Total | 14,457,609 | 526,303 | 100 | |
Index of Relative Socioeconomic Disadvantage.
Australian Bureau of Statistics, 2016 Census of Population and Housing, TableBuilder data available at: www.abs.gov.au/websitedbs/censushome.nsf/home/tablebuilder.
Scores on the Kessler 10 questionnaire above 30, based on 2011 data (Isaacs et al., 2018).
Values calculated by multiplying column 2 with column 3.
Percentages calculated by dividing column 3 by total population provided at bottom of column 2.
This framework for considering pathogenic influences would lead us to seek practice-models that acknowledge risks of harm from therapeutic interventions; support attention to consumer-defined goals; avoid unhelpful biomedical labelling of normal life experiences; support social, educational and vocational participation; and encourage people to apply themselves energetically to self-help and other active strategies in their pathway through experiences of mental health problems. Our interventions should encourage, not replace or subvert, autonomy, independence and active coping. In primary care, this could be congruent with principles of patient-centred-care; taking here more of a specialist-care perspective, there is a connection with the constructs of personal recovery and recovery-oriented practice (ROP), for instance, as developed and implemented in Australian specialist mental health care (Meadows et al., 2019). ROP has emphasis on consumer-defined goals, on a coaching style of relationship between providers of care and recipients, and with domains of concern including fostering empowerment and a strong sense of identity.
Presenting a research programme
We have summarised elements of the thinking developed in this paper in a causal loop diagram, with some explaining notes for this format (Figure 2). While qualitative studies might usefully contribute to a research programme around these ideas, here, we concentrate on how we might formulate and test specific hypotheses for quantitative investigation.
Figure 2.
Simplified causal loop diagram of the hypothetical nexus.
+/− indicates positive or negative influence through the pathway.
 indicates that the left-hand pathway has greater influence than the right.
indicates that the left-hand pathway has greater influence than the right.
Self-help may share features with effective therapies and be experienced as helpful (Houle et al., 2013; Jorm et al., 2004; Morgan et al., 2012). This suggests benefit (and possible advantages to promoting helpful strategies), but future studies could seek strategy-specific effect estimates.
Simulation modelling approaches such as agent-based modelling (ABM) and system dynamics (SD) may be useful here. In Australia, we have little in the way of longitudinal data sets, but we have extensive and detailed national survey data with cross-sectional coverage. Simulation models could provide dynamic representations of the population, bringing together best available evidence and data with proposed causal models including operation of feedback loops. Systematic literature reviews and/or Delphi studies could be useful approaches to inform initial parameter setting. If simulation models generated values similar to the sequence of events that has unfolded in recent years, then this would provide, at low cost, some support to the hypotheses, while possibility also assisting in elaboration of detail of how the influences might operate separately and together. An example hypothesis might be that an ABM designed using available information on depression incidence and available models of care, also incorporating social iatrogenesis elements as described, would be found accurately to simulate existing socioeconomic disparities in prevalence.
The original cross-sectional data set on self-help (Jorm et al., 2004) could be re-examined, for instance, to investigate a hypothesis that data from individuals living in areas with greater socioeconomic disadvantage show a pattern of more severe disorder associated with lower active self-help and more limited service use compared with findings from more advantaged areas. But, the mechanisms proposed here rely on causal connections that may better show themselves with longitudinal data. A self-help survey (Jorm et al., 2004) could be repeated and its content extended within a longitudinal design. Examination of associations with disparities in psychological treatment delivery might allow testing of the hypothesis that combined psychological and ADM treatment is typically associated with less reduction in self-help than is ADM treatment alone. It may also, perhaps, confirm expectations from efficacy studies of better outcomes from combined treatment. Useful data collection might also be integrated into national health surveillance surveys or into any further National Survey of Mental Health and Wellbeing. Again, inclusion of a longitudinal design would represent a great advantage for examining the influences suggested here while dynamic simulation models can both inform and be informed by such data.
The hypothesis that among people with depression those who are more activated and empowered consumers have better outcomes could be investigated in clinical observational studies although there would be considerable design challenges in terms of bias and confounding. Arguably, most powerful would be intervention studies that introduced ROP or associated interventions and delivered combined treatment in an ROP framework in areas that have historically been deprived of it with exploration of effects on outcome. Here, hypotheses might include that ROP in primary care for people with depression will yield some increase where ADM only was provided, but have greater benefits in conjunction with combined ADM and psychotherapeutic treatment.
Implications
Accumulation of evidence for iatrogenic influences suggested here would indicate the need for greater cross-government action on equitable services delivery. Inequitable service delivery may not only mean some areas benefit less but also that imbalanced service delivery in poorer-serviced areas might there do population mental health more harm than good. More people with depression live in disadvantaged areas than advantaged ones, many also in regional and remote areas, so we may see no overall change from increased investment. Increasing funding to existing models of care may be doomed to failure as a population health strategy if health gains in areas where care is more often comprehensive are more than offset by losses in other areas where it is not. Increased funding certainly is needed, but it should encourage the best service models and reach areas of greater need. Correcting service inequities that are under governmental control can be very challenging (Meadows et al., 2018); for instance, for the Australian Government, directing where national insurance funded health-services are delivered faces regulatory, procedural and arguably constitutional points of resistance (through Article 51:xxiiiA and its prohibition of medical ‘civil conscription’). A powerful argument such as this may be needed to prompt such politically difficult action.
ROP is well established in specialist mental health care and Australian evidence supports effectiveness of ROP promotion through training interventions (Meadows et al., 2019). The arguments set out in the paper suggest that there is importance to the task of advancing its implementation in primary mental health care (Enticott et al., 2016). We note here though that providing depressed people in socioeconomically advantaged areas with combined ADM and psychotherapy while providing ADM monotherapy in an ROP framework to those in regional, remote or disadvantaged areas would be perpetuating an unjust situation. Rather, we should work towards ensuring that accessible delivery of combined psychosocial interventions and ADM, administered within an empowering framework and adapted as necessary to community needs, is a nationally implemented standard rather than a notional entitlement accessed only by a relatively privileged and better located minority of people with depression. Both pharmacological and psychosocial interventions are also recommended in low- and middle-income countries, but resource and workforce constraints often limit activity in the latter; drugs are simpler and quicker to deliver (Patel et al., 2018). Mechanisms proposed here might suggest that the sequencing of these two interventions, and the expectations conveyed about ADMs, could be important in maximising health gain from limited investment. Where data are available, simulations could begin the exploration of iatrogenicity in this context with field studies to follow.
Conclusion
Proposing some ideas that might go towards explaining the seeming paradox of why increased expenditure and treatment activity have not identifiably decreased prevalence, we have suggested research strategies around some described hypotheses. If these propositions gain support, indicated actions, although variable between areas, would include some targeted changes to existing service distribution and delivery models. Increased funding might then be invested with greater confidence of improving population mental health.
Acknowledgments
Professor Anthony Jorm and Associate Professor Morton Rawlin each provided helpful comments on the concepts presented in this paper and on earlier manuscript drafts.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
ORCID iD: Graham N Meadows  https://orcid.org/0000-0002-3227-815X
https://orcid.org/0000-0002-3227-815X
References
- Beyondblue: the national depression initiative (2018) Treatments for depression. Available at: https://www.beyondblue.org.au/the-facts/depression/treatments-for-depression (accessed 7 June 2019).
- Cipriani A, Furukawa TA, Salanti G, et al. (2018) Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: A systematic review and network meta-analysis. The Lancet 391: 1357–1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, Cristea IA, Karyotaki E, et al. (2016) How effective are cognitive behavior therapies for major depression and anxiety disorders? A meta-analytic update of the evidence. World Psychiatry: Official Journal of the World Psychiatric Association (WPA) 15: 245–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enticott JC, Shawyer F, Brophy L, et al. (2016) The PULSAR primary care protocol: A stepped-wedge cluster randomized controlled trial to test a training intervention for general practitioners in recovery-oriented practice to optimize personal recovery in adult patients. BMC Psychiatry 16: 451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furukawa TA, Cipriani A, Atkinson LZ, et al. (2016) Placebo response rates in antidepressant trials: A systematic review of published and unpublished double-blind randomised controlled studies. The Lancet Psychiatry 3: 1059–1066. [DOI] [PubMed] [Google Scholar]
- Hartch T. (2015) The Prophet of Cuernavaca: Ivan Illich and the Crisis of the West. New York: Oxford University Press. [Google Scholar]
- Houle J, Gascon-Depatie M, Belanger-Dumontier G, et al. (2013) Depression self-management support: A systematic review. Patient Education and Counselling 91: 271–279. [DOI] [PubMed] [Google Scholar]
- Illich I. (1976) Limits to Medicine: Medical Nemesis: The Expropriation of Health. London: Marion Boyars. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isaacs A, Enticott J, Meadows G, et al. (2018) Lower income levels in Australia are strongly associated with elevated psychological distress: Implications for healthcare and other policy areas. Frontiers in Psychiatry 9: 536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorm AF. (2018) Australia’s ‘Better Access’ scheme: Has it had an impact on population mental health? Australian & New Zealand Journal of Psychiatry 52: 1057–1062. [DOI] [PubMed] [Google Scholar]
- Jorm AF, Griffiths KM, Christensen H, et al. (2004) Actions taken to cope with depression at different levels of severity: A community survey. Psychological Medicine 34: 293–299. [DOI] [PubMed] [Google Scholar]
- Jorm AF, Patten SB, Brugha TS, et al. (2017) Has increased provision of treatment reduced the prevalence of common mental disorders? Review of the evidence from four countries. World Psychiatry 16: 90–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meadows G, Brophy L, Shawyer F, et al. (2019) Refocus-Pulsar recovery-oriented practice training in specialist mental health care: A stepped-wedge cluster randomised controlled trial. The Lancet Psychiatry 6: 103–114. [DOI] [PubMed] [Google Scholar]
- Meadows G, Enticott J, Rosenberg S. (2018) Three charts on: Why rates of mental illness aren’t going down despite higher spending. Available at: https://theconversation.com/three-charts-on-why-rates-of-mental-illness-arent-going-down-despite-higher-spending-97534 (accessed 7 June 2019).
- Morgan AJ, Jorm AF, Mackinnon AJ. (2012) Usage and reported helpfulness of self-help strategies by adults with sub-threshold depression. Journal of Affective Disorders 136: 393–397. [DOI] [PubMed] [Google Scholar]
- Mulder R, Rucklidge J, Wilkinson S. (2017) Why has increased provision of psychiatric treatment not reduced the prevalence of mental disorder? Australian and New Zealand Journal of Psychiatry 51: 1176–1177. [DOI] [PubMed] [Google Scholar]
- O’Hanlon S. (2018) City Life; the New Urban Australia. Sydney, NSW, Australia: NewSouth Publishing. [Google Scholar]
- Patel V, Saxena S, Lund C, et al. (2018) The Lancet Commission on global mental health and sustainable development. The Lancet 392: 1553–1598. [DOI] [PubMed] [Google Scholar]
- Van Os J, Guloksuz S, Vijn TW, et al. (2019) The evidence-based group-level symptom-reduction model as the organizing principle for mental health care: Time for change? World Psychiatry 18: 88–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson R, Pickett K. (2018) The Inner Level: How More Equal Societies Reduce Stress, Restore Sanity and Improve Everyone’s Well-being. London: Penguin Press. [DOI] [PMC free article] [PubMed] [Google Scholar]