Abstract
Purpose
Screening for prostate cancer (PCa) has seen several changes in practice that may affect prevalence and predictors of incidental PCa at surgery for benign prostatic hyperplasia (BPH). We looked at changes in the rate of incidental PCa after BPH surgery over the last decade.
Materials and methods
We identified 1,177 patients surgically treated for BPH (open prostatectomy, trans-urethral resection or holmium laser enucleation (HoLEP) of the prostate) in 2007–2016 at a single European academic center. Local polynomial regression was used to explore changes in the rate of incidental PCa detected after BPH surgery and of pre-operative biopsy performed over time. Logistic regression analyses tested the association of incidental PCa diagnosis with year of surgery and pre-operative biopsy.
Results
Incidental PCa was found in 6.4% (74) of cases, 67 (91%) with Grade group 1 disease. We observed an increased incidence of PCa diagnosis after BPH surgery over time (OR: 1.10; 95%CI: 1.01 – 1.21, p=0.02) along with a concomitant decrease in the rate of pre-operative prostate biopsies (OR: 0.83; 95%CI: 0.78 – 0.87, p<0.001). Patients undergoing a pre-operative biopsy showed a lower risk of being diagnosed with PCa after surgery (OR: 0.29; 95% CI: 0.12, 0.72 p=0.007). Patients treated with HoLEP had a higher chance of incidental PCa detection (OR: 2.28; 95%CI: 1.3 – 4; p=0.004), although this may be related to the significantly higher number of HoLEP performed over the last years.
Conclusions
The increased rate of low-risk PCa detected after BPH surgery in the last decade reflects the clinical practice changes in PCa screening and diagnosis leading to a reduced number of unnecessary biopsies and indolent cancer diagnosis.
Keywords: Prostate Cancer, Benign Prostatic Hyperplasia, Prostate biopsy
Introduction
The widespread use of prostate specific antigen (PSA) screening has led to an increased incidence of prostate cancer (PCa) over the last two decades 1. This trend has been mainly observed for low-risk diseases 2. Indeed, PSA test has shown inadequate specificity for detecting high-risk disease, leading to unnecessary biopsy and overdiagnosis of low risk tumors 2, 3. Patients candidate for surgical treatment of benign prostatic hyperplasia (BPH) are usually screened for PCa before treatment in order to rule out the presence of an incidental tumor that could eventually change the treatment management 4. Incidental PCa, defined as a non-palpable tumor detected after BPH surgery, has been reported as a low risk, indolent disease in the majority of cases 5, 6. Several studies have shown a decrease in the detection of incidental PCa after BPH surgery in the PSA era 6–9. Indeed, with the advent of PSA, it is likely that more BPH patients would have received a prostate biopsy and could have been submitted to treatments other than BPH surgery in the case of PCa diagnosis, thus reducing the risk of incidentally detected tumors after treatment for BPH.
In the last few years a more conservative attitude toward the indication for prostate biopsies has been observed in clinical practice10. Moreover, novel biomarkers and diagnostic tools have been recently introduced in order to reduce the risk of finding indolent tumors at biopsy: the PSA-based blood test 4kScore has shown higher accuracy for detecting clinically significant PCa on initial or repeat biopsy 11, leading to a reduction in the incidence of biopsies by almost 65% when introduced in routine US care 12. The Prostate Health Index (phi) test, is another PSA-based marker that aims to spare men at low risk of high-grade cancer from biopsy13. Moreover urinary markers, such as the PCA3, have been extensively validated for the detection of men deserving to repeat the biopsy after a previous negative assessment 14. Multi parametric Magnetic Resonance Imaging (mpMRI) has demonstrated high accuracy in the detection of significant PCa, showing a potential relative reduction of 31% in the over-diagnosis of clinically indolent cancers in a randomized trial 15. At the same time, biopsy itself has changed; indeed, the number of cores taken per biopsy has increased with the aim to reduce the risk of missing potentially significant cancer 16
Given the more conservative approach to biopsy we should expect an increase in the detection of incidental PCa after BPH surgery. On the other hand, amongst men who had previously undergone a prostate biopsy, we should see a decrease in the risk of incidental PCa, because contemporary biopsy is less likely to miss cancer. We looked at changes in the rate of incidental PCa diagnosis in the last decade in a cohort of patients undergoing surgery for BPH, as a mirror of clinical practice changes in terms of PCa screening and diagnosis.
Materials and Methods
After institutional review board approval, we retrospectively analysed a cohort of 1,371 patients submitted to surgical treatment for BPH at a single European academic center, from January 2007 to September 2016. Pre-operative data including age at surgery, prostate volume (assessed with a trans-rectal ultrasound), total serum PSA and digital rectal examination were recorded for all patients. According to our protocol, all patients candidates for BPH surgery are routinely screened for PCa; BPH patients with a suspicion for PCa, on the base of clinical evaluation and available diagnostic tests, were submitted to prostate biopsies before surgery; those found with PCa at pre-operative biopsy were not submitted to BPH surgery and therefore are not included in the study cohort.
Patients were treated with either open prostatectomy (OP), monopolar trans-urethral resection of the prostate (TURP) or holmium laser enucleation of the prostate (HoLEP), according to both the prostate volume and the surgical expertise of the treating physician.
All surgical specimens were assessed by dedicated genito-urinary pathologists; in the case of incidental PCa diagnosis, patients were staged as T1a or T1b according to the 2017 TNM classification; moreover, all cancers were graded according to the Gleason score (GS).
Patients missing clinical or pathologic data [194(14.1%)] were excluded from the analysis.
Statistical analyses
The aim of the study was to assess the changes in the rate of incidental PCa detected at BPH surgery throughout the last decade. Local polynomial smoothing methods were used to visualize variations in the rate of incidental PCa, of preoperative biopsy and in the type of surgery over the study period. Logistic regression analyses tested the association between incidental PCa diagnosis with year of surgery and preoperative biopsy, after accounting for total PSA, prostate volume, age and type of surgery. Moreover, in order to confirm the correlation between preoperative biopsy and the changes in the detection of incidental PCa, the same analyses were performed in a subgroup of patients with a history of negative biopsies before surgery. Statistical analyses were conducted using Stata 13.0 (StataCorp, College Station, TX, USA), with a two-sided significance level set at p < 0.05.
Results
Clinical characteristics of the entire cohort (n=1,177) are reported in Table 1. Overall, patients were submitted to surgery for BPH at a median age of 66 years, with a median preoperative total PSA of 3.2 ng/mL. Of note, 330 (26%) patients received a preoperative prostate biopsy and resulted negative for cancer. Most patients were treated with HoLEP (45%). Incidental PCa was found after BPH surgery in 6.4% (74) of cases over the study period; most of them, were staged pT1a (86%) and had a GS of 6 (91%; Table 2).
Table 1 –
Clinical characteristics of the entire cohort of patients
| Age (years) | 66 (61, 72) |
| PSA (ng/mL) | 3.2 (1.9, 5.7) |
| Prostate volume (cc) | 76 (52, 105) |
| Year of surgery [N (%)] | |
| 2007 – 2009 | 273 (23%) |
| 2010 – 2011 | 206 (18%) |
| 2012 – 2013 | 327 (28%) |
| 2014 – 2016 | 371 (32%) |
| Preoperative negative biopsy | 330 (26%) |
| Type of surgery [N (%)] | |
| OP | 139 (12%) |
| TURP | 498 (42%) |
| HoLEP | 540 (46%) |
Keys: PSA= prostate specific antigen; OP= open prostatectomy; TURP= trans-urethral resection of the prostate; HoLEP= holmium laser enucleation of the prostate
Table 2 –
Pathological findings after BPH surgery
| iPCa | |
| No | 1103 (94%) |
| Yes | 74 (6.4%) |
| T stage [N(%)] | |
| T1a | 64 (86%) |
| T1b | 10 (14%) |
| Gleason score [N(%)] | |
| 6 | 67 (91%) |
| 7 | 5 (6.2%) |
| >7 | 2 (2.5%) |
Keys: BPH= benign prostatic hyperplasia; iPCa= incidental prostate cancer
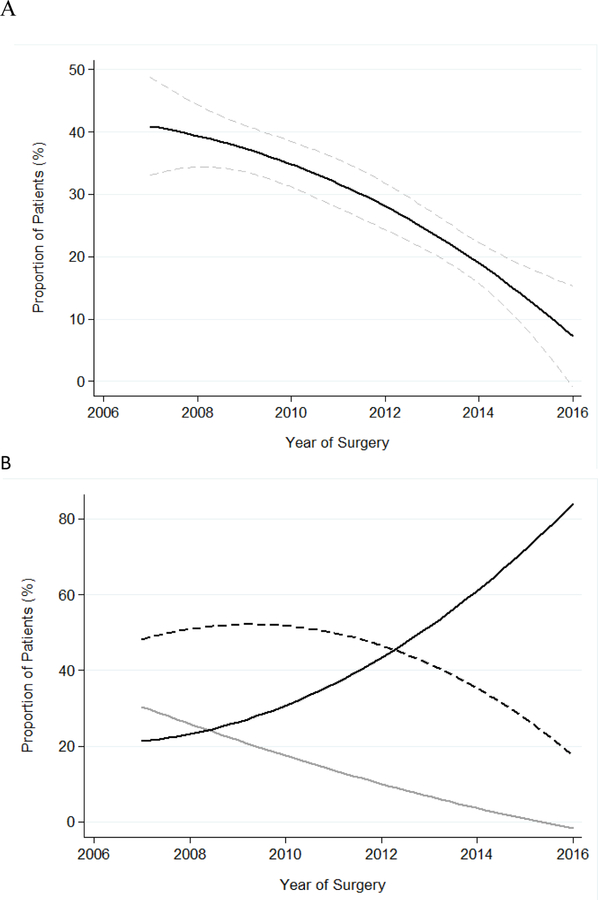
Figure 1a depicts the rate of incidental PCa by time. An increase in the proportion of patients diagnosed with incidental PCa after BPH surgery was observed from 2007 to 2016, with an odds ratio of 1.10 per year on univariate logistic regression analysis (95%CI: 1.01 – 1.21, p=0.02). The increase in incidental PCa over time has to be ascribed to an increase of GS 6-disease detected after surgery, while the rate of incidental PCa with a GS 7 or higher was found to be stable over the same period (Figure 1b). Similarly, we observed a significant decrease in the number of patients who received a preoperative biopsy found negative for PCa, throughout the same time frame (Figure 2a; OR: 0.83; 95%CI: 0.78 – 0.87, p<0.01). In the sub-analysis performed among patients biopsied before surgery, the association between the rate of incidental PCa diagnosis and the year of surgery was no longer significant (p=0.7).
Figure 1.
Changes in iPCa detection over the study period. (A) Overall iPCa incidence (B) Incidence of iPCa according to GS [thick black line represents GS 6 disease; thin black line represents GS 7 disease; gray line represents GS>7 disease].
The dashed lines indicate the 95% confidence interval
Figure 2.
(A) Changes in the rate of patients with negative preoperative biopsy over time (dashed lines indicate the 95% confidence interval) (B) Changes in the type of surgery over time (black line represents patients treated with HoLEP; dashed line represents patients treated with TURP; gray line represents patients treated with OP)
Rates of different types of surgeries changed across the investigated period, with an increase of HoLEP procedures performed over time (Figure 2b; OR:1.3; 95%CI: 1.2 – 1.4; p<0.001).
At multivariable logistic regression analysis (Table 3) preoperative biopsy was independently associated with the finding of incidental PCa (OR: 0.27; 95%CI: 0.1–0.6; p=0.007) as well as high PSA values and low prostate volume (all p<0.001). Likewise, patients treated with HoLEP were more likely to be diagnosed with incidental PCa after surgery (OR: 2.28; 95%CI: 0.98–0.99; p=0.004).
Table 3 –
Multivariable logistic regression analysis predicting iPCa
| Variable | Odds Ratio | 95% Confidence Interval | p-value |
|---|---|---|---|
| Age | 1.02 | 0.1, 2.6 | 0.1 |
| Year of surgery | 1.04 | 0.93, 1.15 | 0.5 |
| Preoperative biopsy | 0.27 | 0.11, 0.66 | 0.004 |
| TURP vs OP | 0.58 | 0.12, 2.67 | 0.4 |
| TURP vs HoLEP | 2.28 | 1.30, 4.0 | 0.004 |
| prostate volume | 0.99 | 0.98, 0.99 | 0.0003 |
| PSA | 1.10 | 1.05, 1.16 | 0.0002 |
Keys: iPCA = incidental prostate cancer; PSA= prostate specific antigen; OP= open prostatectomy; TURP= trans-urethral resection of the prostate; HoLEP= holmium laser enucleation of the prostate
Discussion
We looked at changes in the rate of incidental PCa findings after BPH surgery throughout the last decade. Our data showed, a significant increase in terms of incidental PCa diagnosis over time. At the same time, we observed a significant decrease in the rate of patients who received a prostate biopsy prior to BPH surgery, with the odds of being biopsied decreasing by almost 20% per year. These findings are likely to reflect clinical practice changes in terms of PCa screening in the modern era; indeed, the lower number of biopsies performed in recent years among patients candidates for BPH surgery could be the consequence of the introduction of novel biomarkers and diagnostic tools allowing for a better discrimination of clinically significant cancers, and leading to a reduction of unnecessary biopsies and pre-operative diagnosis of indolent tumors. In line with this theory, our data showed that the increase in the rate of incidental PCa was mainly due to a higher number of low grade (GS 6) disease detected after surgery; of note, these features are associated with favorable oncological outcomes 5. We should also consider that an overall more conservative approach regarding the indication for prostate biopsy may have contributed to the lower number of biopsies performed over time. Data from a US population, for example, have shown a significant increase in the pre-biopsy PSA value over the last decade, suggesting that higher PSA thresholds have been recently used to prompt for biopsy in clinical practice 10. Considering our sample of men candidates for BPH surgery as a cohort of individuals systematically screened for PCa, we could speculate that our findings may hold true also for the overall population of patients usually subjected to PCa screening in the everyday clinical practice.
Previous studies have reported on time trends in the detection of incidental PCa after BPH surgical treatment. Tombal et al. 6, for instance, evaluated the incidence of T1a-T1b PCa in a series of 1,648 patients undergoing BPH surgery over a 13-year period, overlapping the introduction of PSA test. They found a decrease in the rate of incidental PCa from 23% to 7% over the study period. Similarly, Jones et al. 7 found a significant decrease in the incidence of both T1a and T1b diseases among men submitted to TURP in the pre-PSA era as compared with patients treated in the post-PSA era. Data coming from more recent series confirm those findings, showing an overall low rate of incidental PCa detected at BPH surgery after PSA test introduction, ranging from 4.8 to 1.8% 8, 9. Of note, in a systematic review of autopsy studies spanning over six decades, the authors did not find a visible trend in the estimated prevalence of undetected PCa found at the autopsy evaluation over time 17. However, all these studies included patients evaluated up to 2011, thus ruling out the possibility to observe a change in the detection of low-risk PCa as a consequence of the introduction of novel PSA-derived biomarkers and diagnostic tools such as the mpMRI. Conversely, we looked at patients treated from 2007 to 2016 thus overlapping the introduction of novel tools dedicated to the screening and detection of significant PCa; at the same time, our study was set in a period of a generally more conservative attitude toward the indication for prostate biopsy. Thereof, in contrast with previous findings, we observed a trend reversal in the rate of incidental PCa detection at BPH surgery with a constant increase in the incidence of cancer throughout the investigated time-period. Of note, the majority of patients were diagnosed with a pT1a GS 6 disease, thus suggesting that clinically significant cancers are likely to be properly detected at preoperative evaluation.
The significant increase in the number of minimally invasive ablative procedures for the treatment of BPH in the last two decades has been considered as a further factor influencing the rate of incidental PCa detection at surgery 18. Indeed, those procedures may not provide adequate prostate tissue for pathologic examination of surgical specimens. Although it was initially unplanned, we explored the changes in the use of different types of surgery over time and we found a significant increase in the proportion of patients treated with HoLEP along with a concomitant decrease in the number of performed OP and TURP procedures. Unexpectedly, patients treated with HoLEP were more likely to be diagnosed with incidental PCa at BPH surgery. We believe that these results should be interpreted with caution, given the strong correlation between the year of surgery and the number of HoLEP procedures performed. Indeed, in a previous study reporting data from our institute, the probability of PCa detection, as well as the quality of the tissue retrieved after surgery, was not significantly different between TURP and HoLEP 19; similar findings have been also confirmed in other series 20. Furthermore, our data showed that OP, which is based on the same surgical concept of prostatic adenoma enucleation as HoLEP, was not associated with a higher probability of detecting incidental PCa as compared to TURP, thus making harder to find a causal biological reason to explain the observed difference rate of incidental PCa detected between HoLEP and TURP procedures.
Our study has several limitations. First, as a retrospective study, we could not rule out the possibility that the baseline characteristics of candidates for BPH surgery and submitted to PCa screening may have changed over time due to a different attitude to BPH treatment itself, eventually influencing the risk of incidental PCa after surgery; however we performed sensitivity analysis showing no significant difference in terms of patients age, prostate volume and baseline PSA among patients treated in the earlier years as compared with those more recently treated. Second, we lack detailed data regarding the actual use of novel biomarkers and diagnostic tools for the preoperative assessment of patients included in the study; however, in a sub-analysis including only patients with a preoperative negative biopsy, we did not find evidence of a change in the rate of incidental PCa detected after surgery over time, thus confirming that the decision to perform a biopsy prior to treatment plays a major role in determining the chance of cancer diagnosis after BPH surgery. Third, we are aware that changes in the pathological evaluation of specimens may have occurred over time; however, within the investigated time frame these changes have affected mainly the grading of cancer rather then the detection of disease itself 21. Last, while these findings may be representative of this relatively large cohort of patients surgically treated at a single European academic institute, they deserve validation in larger population-based studies.
Conclusions
The significant increase in the detection of low grade incidental PCa after BPH surgery over the last decade is likely to reflect the occurred changes in clinical practice regarding PCa screening and detection. These findings confirm a general attitude toward a reduced number of unnecessary biopsies and consequent diagnosis of indolent tumors.
Supplementary Material
Acknowledgments:
This work was supported in part by a Cancer Center Support Grant from the National Cancer Institute made to Memorial Sloan Kettering Cancer Center (P30-CA008748).
Footnotes
Conflict of Interest: None.
References
- 1.Siegel RL, Miller KD, Jemal A: Cancer Statistics, 2017. CA Cancer J Clin, 67: 7, 2017 [DOI] [PubMed] [Google Scholar]
- 2.Cooperberg MR, Lubeck DP, Meng MV et al. : The changing face of low-risk prostate cancer: trends in clinical presentation and primary management. J Clin Oncol, 22: 2141, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ilic D, Neuberger MM, Djulbegovic M et al. : Screening for prostate cancer. Cochrane Database Syst Rev: CD004720, 2013 [DOI] [PMC free article] [PubMed]
- 4.Gratzke C, Bachmann A, Descazeaud A et al. : EAU Guidelines on the Assessment of Non-neurogenic Male Lower Urinary Tract Symptoms including Benign Prostatic Obstruction. Eur Urol, 67: 1099, 2015 [DOI] [PubMed] [Google Scholar]
- 5.Capitanio U, Scattoni V, Freschi M et al. : Radical prostatectomy for incidental (stage T1a-T1b) prostate cancer: analysis of predictors for residual disease and biochemical recurrence. Eur Urol, 54: 118, 2008 [DOI] [PubMed] [Google Scholar]
- 6.Tombal B, De Visccher L, Cosyns JP et al. : Assessing the risk of unsuspected prostate cancer in patients with benign prostatic hypertrophy: a 13-year retrospective study of the incidence and natural history of T1a-T1b prostate cancers. BJU Int, 84: 1015, 1999 [DOI] [PubMed] [Google Scholar]
- 7.Jones JS, Follis HW, Johnson JR: Probability of finding T1a and T1b (incidental) prostate cancer during TURP has decreased in the PSA era. Prostate Cancer Prostatic Dis, 12: 57, 2009 [DOI] [PubMed] [Google Scholar]
- 8.Yoo C, Oh CY, Kim SJ et al. : Preoperative clinical factors for diagnosis of incidental prostate cancer in the era of tissue-ablative surgery for benign prostatic hyperplasia: a korean multi-center review. Korean J Urol, 53: 391, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Otto B, Barbieri C, Lee R et al. : Incidental prostate cancer in transurethral resection of the prostate specimens in the modern era. Adv Urol, 2014: 627290, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Banerji JS, Wolff EM, Massman JD 3rd et al. : Prostate Needle Biopsy Outcomes in the Era of the U.S. Preventive Services Task Force Recommendation against Prostate Specific Antigen Based Screening. J Urol, 195: 66, 2016 [DOI] [PubMed] [Google Scholar]
- 11.Vickers AJ, Cronin AM, Roobol MJ et al. : A four-kallikrein panel predicts prostate cancer in men with recent screening: data from the European Randomized Study of Screening for Prostate Cancer, Rotterdam. Clin Cancer Res, 16: 3232, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Konety B, Zappala SM, Parekh DJ et al. : The 4Kscore(R) Test Reduces Prostate Biopsy Rates in Community and Academic Urology Practices. Rev Urol, 17: 231, 2015 [PMC free article] [PubMed] [Google Scholar]
- 13.Lazzeri M, Haese A, de la Taille A et al. : Serum isoform [−2]proPSA derivatives significantly improve prediction of prostate cancer at initial biopsy in a total PSA range of 2–10 ng/ml: a multicentric European study. Eur Urol, 63: 986, 2013 [DOI] [PubMed] [Google Scholar]
- 14.Haese A, de la Taille A, van Poppel H et al. : Clinical utility of the PCA3 urine assay in European men scheduled for repeat biopsy. Eur Urol, 54: 1081, 2008 [DOI] [PubMed] [Google Scholar]
- 15.Ahmed HU, El-Shater Bosaily A., Brown LC et al. : Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet, 389: 815, 2017 [DOI] [PubMed] [Google Scholar]
- 16.Mottet N, Bellmunt J, Bolla M et al. : EAU-ESTRO-SIOG Guidelines on Prostate Cancer. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. Eur Urol, 71: 618, 2017 [DOI] [PubMed] [Google Scholar]
- 17.Bell KJ, Del Mar C, Wright G et al. : Prevalence of incidental prostate cancer: A systematic review of autopsy studies. Int J Cancer, 137: 1749, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yu X, Elliott SP, Wilt TJ et al. : Practice patterns in benign prostatic hyperplasia surgical therapy: the dramatic increase in minimally invasive technologies. J Urol, 180: 241, 2008 [DOI] [PubMed] [Google Scholar]
- 19.Naspro R, Freschi M, Salonia A et al. : Holmium laser enucleation versus transurethral resection of the prostate. Are histological findings comparable? J Urol, 171: 1203, 2004 [DOI] [PubMed] [Google Scholar]
- 20.Herlemann A, Wegner K, Roosen A et al. : “Finding the needle in a haystack”: oncologic evaluation of patients treated for LUTS with holmium laser enucleation of the prostate (HoLEP) versus transurethral resection of the prostate (TURP). World J Urol, 2017 [DOI] [PubMed]
- 21.Epstein JI, Egevad L, Amin MB et al. : The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma: Definition of Grading Patterns and Proposal for a New Grading System. Am J Surg Pathol, 40: 244, 2016 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.