Abstract
Background:
Decisions made to undergo contralateral prophylactic mastectomy (CPM), in women at low risk for bilateral disease, are often attributed to a lack of knowledge. This study examines the role knowledge plays in determining surgical treatment for unilateral breast cancer made by laywomen and surgeons for themselves or loved ones.
Methods:
Our study cohort had three groups 1) laywomen in the general population 2) breast surgeons and 3) plastic surgeons. Laywomen were recruited using Amazon Mechanical Turk® Crowd Sourcing. Breast and plastic surgeons from 9 states were sent electronic surveys. Demographic and CPM specific information on decisions and knowledge were collected and analyzed.
Results:
Surveys from 1,333 laywomen, 198 plastic surgeons, and 142 breast surgeons were analyzed. A significantly greater proportion of laywomen in the general population favored CPM (67%) relative to plastic (50%) and breast surgeons (26%), p<0.0001. Breast surgeons who chose CPM were younger (p=0.044) and female (0.012). On assessment of knowledge, 78% of laywomen had a low-level breast cancer knowledge. Laywomen with higher levels of breast cancer knowledge had lower odds of choosing CPM (OR 0.37, 95% CI 0.28-0.49).
Conclusion:
Fewer women are likely to make decisions in favor of CPM with better breast cancer specific education. A knowledge gap likely explains the lower rates with which surgeons choose CPM for themselves or loved ones, however, some surgeons who were predominantly young and female, favor CPM. Improving patient education on surgical options for breast cancer treatment is critical, with well informed decisions as the goal.
Keywords: Contralateral prophylactic mastectomy, breast reconstruction, Amazon Mechanical Turk
INTRODUCTION
Newly diagnosed breast cancer patients, in addition to coping with a cancer diagnosis, also need to understand and navigate the complexities of the various surgical options available to them. Surgical treatment of early stage breast cancer includes lumpectomy and radiation, unilateral mastectomy and unilateral mastectomy with contralateral prophylactic mastectomy (CPM). Although CPM has been demonstrated to reduce the risk of cancer in the contralateral breast by approximately 95%, there have been no prospective randomized studies demonstrating a survival benefit (1–6).
CPM is generally accepted and even recommended in patients deemed to be at high risk for contralateral breast cancer. However, the impact of CPM on survival for average-risk women is less clear with some studies demonstrating a small survival benefit among women less than 49 years old and in those with ER-negative tumors (7–9). In contrast, a large Cochrane Review reviewing over 39 studies concluded that there was no survival benefit of CPM (10). Despite the proven efficacy and safety of breast conservation therapy with lumpectomy and radiation or unilateral mastectomy, the last few decades has seen the pendulum swing towards more aggressive surgical treatment for all stages of breast cancer (1–6, 11–13). This is evidenced by the increased rate of CPM among women with early stage breast cancer—estimated to be as high as 25% of newly diagnosed patients with breast cancer (1–6,10).
Lack of knowledge or misunderstanding of the breast cancer disease process, surgical options and survival benefits are commonly cited reasons for the increasing trend towards CPM among patients (1–6,11–13). This line of thinking suggests that women who are better educated on the facts regarding breast cancer and the risks and benefits of the various surgical options, would not choose CPM in the face of early stage breast cancer as CPM provides little to no survival benefit (1–6). To understand the impact that knowledge might have on decisions made for CPM, we have designed a study to evaluate the personal choices made by laywomen, breast surgeons and reconstructive surgeons, for themselves or a loved one when faced with a hypothetical diagnosis of early stage unilateral breast cancer.
METHODS
Study Population:
We conducted a cross-sectional survey using three questionnaires created specifically for each group—laywomen, breast surgeons and reconstructive surgeons. Laywomen, ages 25-65 were registered workers with Amazon Mechanical Turk®, which is a crowdsourcing platform providing quick, efficient and reliable workers who can select tasks to complete for specified fees (14–16). With this platform, investigators can quickly gain public insight on a specific topic of interest. The United States is the country of origin for the majority of Amazon Mechanical Turk® Workers (14–16). Breast Surgeons from the American Society of Breast Surgeons and Plastic Surgeons from the American Society of Plastic Surgeons practicing in NY, TX, CA, MI, PA, AZ, IL, WA, and FL were identified and sent an electronic survey for completion. The study was limited to these states as they represent the major regions of the US and were some of the largest states with a high number of practitioners.
Data Collection:
Crowdsourcing is a research method that leverages the opinion of a large group of workers in a short amount of time, allowing investigators to gain insight on a specific topic. One such crowdsourcing platform, Amazon Mechanical Turk®, allows researchers and businesses to request human assistance to complete certain tasks—in this case an electronic survey (14–16). Users have the opportunity to complete tasks that most meet their interests and convenience. For the current study, laywomen were compensated $0.50 per survey and payment was contingent on completion of the survey. Using a modified Dillman survey technique, surgeons were emailed an introductory letter with a link to complete the survey via Qualtrics® with a reminder sent to non-responders 1 month after the initial request (17). No compensation was provided to surgeons for completed surveys. Surgeons who replied and were retired or over the age limit were excluded. Surveys where respondents started the survey, but did not answer any questions were also excluded.
Questionnaires:
In addition to gathering demographic data on variables such as age, race, employment and insurance status, we queried laywomen about breast cancer knowledge. Breast cancer knowledge questions were adapted from a previously published decision aide tool by Yao et al. which included questions on breast cancer knowledge, survival, treatment, and recurrence (18). Laywomen were asked about choice of CPM for themselves, a sister, or significant other receiving a hypothetical diagnosis of early stage breast cancer. Finally, we focused on factors that influence decisions made for or against CPM. Similar to the Yao et al study, the survey to laywomen was written in language that we expect individuals in the general population to understand.
Breast surgeon specific surveys included demographic questions as well as practice specific questions ranging from overall patient and procedure volume, to CPM volume, and provision of care through a tumor board. Reconstructive surgeons were asked similar questions, with the mastectomy questions substituted for reconstruction specific questions. Both groups of surgeons were asked about the choice for CPM for themselves, a sister, or spouse if diagnosed with early stage breast cancer as well as influencing factors on CPM choice and whether or not they would recommend reconstruction. Full versions of the surveys are available in the appendix. This study was reviewed and approved as IRB exempt by the University of Michigan Medical School Institutional Review Board (HUM00126731).
Statistical Analysis:
Sociodemographic, practice characteristics, CPM and reconstructive preferences as well as influencers were extracted from Qualtrics®, coded and tabulated. The choice of CPM for surgeon groups and laywomen were compared using a chi-square test. The association between sociodemographic characteristics and choice of CPM were compared within each surgeon group using Chi-squared or Fishers’ exact test. Statistical Analysis Software v9.4A was used for all analyses; the significance level was set at a two-sided alpha=0.05. A logistic regression analysis was performed to evaluate associations between laywomen sociodemographic and knowledge variables and the choice of CPM. Additionally, we performed a multivariable analysis of preference for CPM among laywomen, breast and reconstructive surgeons.
RESULTS
1,333 women completed the survey via Amazon Mechanical Turk®. Surveys were sent to 4,512 surgeons, with 362 responses received, for a response rate of 8% among surgeons. Duplicated surgeon surveys or those where the survey was started but none of the questions were answered were excluded (n=27), leaving 198 reconstructive surgeons and 142 breast surgeons responses that were included in the analysis (See Figure, Supplemental Digital Content 1, which shows the Study Flow Diagram, INSERT HYPER LINK).
The study cohort demographic data is presented in Table 1. Breast surgeons were predominantly female (68%), in contrast to reconstructive surgeons who were predominantly male (75%). Most of the surgeons were over 40 years of age whereas only 32% laywomen respondents were over 40 years of age. Women in all three groups were predominantly Caucasian. The majority of surgeons were married and largely in private practice. Among breast and plastic surgeon respondents within the last 12 months, 64% and 25% reported that >50% of their practice was spent caring for breast cancer patients, respectively. The laywomen respondents, majority had a college education and were insured.
Table 1.
Surgeon and Laywomen Demographics
| Breast Surgeons | Reconstructive Surgeons | Laywomen | ||||
|---|---|---|---|---|---|---|
| Totals | 142 | 198 | 1333 | |||
| Demographic Sex | n | % | n | % | n | % |
| Female | 96 | 67 | 49 | 24 | 1333 | 100 |
| Male | 46 | 32 | 149 | 75 | - | - |
| Race | ||||||
| Asian/Islander | 16 | 11 | 23 | 11 | 130 | 9 |
| Black | 5 | 3 | 4 | 2 | 134 | 10 |
| White | 119 | 84 | 159 | 80 | 1024 | 76 |
| Other | 2 | 1 | 12 | 6 | 44 | 3 |
| Missing | 1 | 1 | - | - | 1 | 0.1 |
| Marital Status | ||||||
| Married | 116 | 82 | 174 | 83 | 711 | 53 |
| Single | 17 | 12 | 9 | 5 | 440 | 33 |
| Other | 9 | 5 | 15 | 8 | 182 | 14 |
| Missing | 2 | 1 | - | - | 3 | 0.2 |
| Age | ||||||
| 18-30 | 0 | 0 | 0 | 0.0 | 453 | 34 |
| 30-40 | 26 | 18 | 55 | 28 | 467 | 35 |
| 40-50 | 36 | 25 | 64 | 32 | 227 | 17 |
| 50-60 | 78 | 55 | 76 | 38 | 183 | 14 |
| Missing | 2 | 1 | 3 | 2 | 3 | 0.2 |
| Type of Practice | ||||||
| Hybrid | 27 | 19 | 38 | 19.2 | - | - |
| Private | 77 | 54 | 119 | 60 | - | - |
| University | 34 | 24 | 41 | 20 | - | - |
| Missing | 4 | 3 | 0 | 0 | - | - |
| Breast Cancer Patient Volume | ||||||
| >50% of practice | - | 64 | - | 25 | - | - |
| >50 mastectomies or reconstructions* | - | 25 | - | 36 | - | - |
| Education | ||||||
| ≤High School | - | - | - | - | 125 | 9 |
| Some College | - | - | - | - | 427 | 32 |
| ≥College | - | - | - | - | 780 | 58 |
| Medical Insurance | ||||||
| No | - | - | - | - | 211 | 16 |
| Yes | - | - | - | - | 1121 | 84 |
| Missing | - | - | - | - | ||
Within the last 12 months
Sixty-eight percent of laywomen responded they would opt for CPM if faced with a diagnosis of early stage breast cancer in comparison to 26% of breast surgeons and 50% of reconstructive surgeons (Table 2). The majority of laywomen surveyed reported that they would opt for reconstruction (83%), with similar proportions choosing implant or autologous based reconstruction (44 and 39% respectively). Most breast (92%) and reconstructive (99%) surgeons reported that they would choose reconstruction for themselves or a loved one (Table 2). The surgeon cohorts were predominantly open to either implant or autologous reconstruction with 55% of breast surgeons and 42% of reconstructive surgeons responding as such.
Table 2.
CPM and Reconstruction Choices Among Surgeons and Laywomen
| Breast Surgeons | Reconstructive Surgeons | Laywomen | P-value | ||||
|---|---|---|---|---|---|---|---|
| Totals | 142 | 198 | 1,333 | ||||
| CPM Choice | n | % | n | % | n | % | |
| No | 90 | 74 | 69 | 50 | 426 | 32 | <0.0001 |
| Yes | 32 | 26 | 71 | 50 | 901 | 68 | |
| Missing | 20 | - | 58 | - | 6 | - | |
| Reconstruction | |||||||
| No | 10 | 8 | 1 | 0.6 | 226 | 17 | |
| Yes, autologous | 8 | 6 | 30 | 18 | 519 | 39 | <0.0001 |
| Yes, implant | 40 | 31 | 67 | 40 | 586 | 44 | |
| Either | 72 | 55 | 70 | 42 | - | ||
| Missing | 12 | - | 30 | - | - | ||
Table 3 presents demographics of respondents who were in favor of CPM. CPM was favored by a significantly greater proportion of younger (p=0.009) and white laywomen (p<0.0001). Among laywomen in favor of CPM there were no differences in level of education, marital status, and insurance status. A significantly greater proportion of female breast surgeons were in favor of CPM for themselves or a loved one as compared to their male counterparts 32% vs. 7% (p=0.012). A similar trend was observed among female reconstructive surgeons with 62% opting for CPM compared with 45% of male reconstructive surgeons, though this did not reach statistical significance (p=0.06). Breast surgeons who were 40 years of age and younger chose CPM more often than surgeons over the age of 40 (p=0.044). Among surgeons, race, marital status, and practice-type were not associated with a specific trend towards CPM.
Table 3.
Demographics of Laywomen and Surgeons In Favor of CPM *percentages equal percentage of that characteristic in favor of CPM
| Breast Surgeons | p-value | Reconstructive Surgeons | p-value | Laywomen | p-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Totals | 142 | 198 | 1333 | ||||||
| Demographic Sex | n | % | n | % | n | % | |||
| Female | 30 | 32 | 29 | 62 | |||||
| Male | 2 | 7 | 0.012 | 42 | 45 | 0.06 | |||
| Race | |||||||||
| Asian/Indian | 2 | 13 | 9 | 47 | 58 | 46 | |||
| Black | 1 | 25 | 2 | 50 | 85 | 64 | |||
| White | 29 | 29 | 55 | 50 | 736 | 72 | |||
| Other | 0 | 0 | 0.48 | 5 | 71 | 0.76 | 22 | 50 | <0.0001 |
| Marital Status | |||||||||
| Married | 24 | 25 | 61 | 50 | 0.26 | 468 | 66 | ||
| Single | 7 | 47 | 2 | 33 | 303 | 69 | |||
| Other | 1 | 11 | 0.13 | 8 | 73 | 130 | 72 | 0.26 | |
| Age | |||||||||
| 18-30 | - | - | - | - | 324 | 72 | |||
| 30-40 | 11 | 42 | 21 | 57 | 319 | 69 | |||
| 40-50 | 10 | 30 | 24 | 47 | 151 | 67 | |||
| 50-60 | 11 | 18 | 26 | 51 | 0.67 | 106 | 58 | ||
| Missing | 0.044 | 1 | 0.009 | ||||||
| Type of Practice | |||||||||
| Hybrid | 5 | 20 | 15 | 60.0 | - | - | |||
| Private | 15 | 23 | 44 | 52 | - | - | |||
| University | 11 | 38 | 0.23 | 12 | 39 | 0.25 | - | - | |
| Education | |||||||||
| ≤High School | - | - | - | - | - | - | 90 | 73 | |
| Some College | - | - | - | - | - | - | 297 | 70 | |
| ≥College | - | - | - | - | - | - | 514 | 66 | 0.18 |
| Medical Insurance | |||||||||
| No | - | - | - | - | - | - | 146 | 70 | |
| Yes | - | - | - | - | - | - | 754 | 68 | 0.71 |
Laywomen were asked standard breast cancer-related questions to assess their baseline knowledge. Seventy-four percent of women thought they knew breast cancer moderately to extremely well. The correct responses to individual questions in a 5-question breast cancer knowledge questionnaire ranged from 30-75%. Knowledge about the development of breast cancer in the contralateral breast following unilateral mastectomy had the lowest correct response rate at 30%. Twenty-two percent of laywomen had high-level (4-5 questions correct) breast cancer knowledge and 78% laywomen were categorized as low-level (0-3 correct) breast cancer knowledge (See Table, Supplemental Digital Content 2, which shows Breast Cancer Knowledge Among Laywomen, INSERT HYPER LINK). Laywomen with a “high-breast cancer knowledge” were significantly less in favor of CM than women with “low-breast cancer knowledge” (50% vs. 73%, p<0.0001).
Table 4 presents a multivariable logistic regression of those in favor for CPM. Breast surgeons had a lower odds of choosing CPM relative to laywomen and reconstructive surgeons and this was statistically significant (OR, 0.273; 95% CI 0.17-0.43), p<0.0001. Laywomen who were younger (50 years and younger) had significantly greater odds of choosing CPM (Age 18-30: OR, 2.62; 95% CI, 1.79-3.82; ages 31-40: OR, 2.10; 95% CI, 1.51-2.92; ages 41-50: OR 1.53; 95% CI,1.08-2.17) relative to patients over the age of 50. Women of other races including Blacks (OR, 0.66; 95% CI 0.45-0.96), Asian/Islander (OR, 0.31; 95% CI 0.22-0.45) and other races (OR, 0.43; 95% CI 0.24-0.76) had lower odds of choosing CPM relative to white women. Women with higher levels of breast cancer knowledge had lower odds of deciding for CPM than those with lower levels of knowledge (OR, 0.37; 95% CI 0.28-0.49).
Table 4:
Multivariable Analysis of Those in Favor of CPM
| Variable | Odds Ratio | 95% CI | p-value |
|---|---|---|---|
| Type of Surgeon (reference: laywomen) | |||
| Breast | 0.273 | 0.17-0.43 | <0.001 |
| Reconstructive | 1.16 | 0.65-2.07 | |
| Age (reference: 51-60 years) | |||
| 18-30 | 2.62 | 1.79-3.82 | <0.0001 |
| 31-40 | 2.10 | 1.51-2.92 | |
| 41-50 | 1.53 | 1.08-2.17 | |
| Race (reference: White) | |||
| Black | 0.66 | 0.45-0.96 | <0.0001 |
| Asian/Islander | 0.31 | 0.22-0.45 | |
| Other | 0.43 | 0.24-0.76 | |
| Marital Status (reference: single) | |||
| Married | 1.08 | 0.82-1.42 | 0.051 |
| Other | 1.63 | 1.08-2.46 | |
| Laywomen High Knowledge vs. Low | 0.37 | 0.28-0.49 | <0.0001 |
In evaluating factors that influence decisions made in favor of CPM among laywomen, the desire to lower the chance of getting breast cancer in the other breast, improve survival, prevent cancer spread, and enhance peace of mind, were of the greatest importance (Figure 1). Reconstructive surgeons responded “a lot” or “quite a bit” when considering, fear of recurrence, fear of occult breast cancer, symmetry, and freedom from surveillance (Figure 1). Breast surgeons in contrast did not have similar concerns and rated fear of recurrence, fear of occult breast cancer, symmetry, freedom from surveillance with scores indicating lower levels importance (Figure 1). Overall, with the exception of the influence of the need for chemotherapy/radiation, there was a statistically significant difference in the distribution of assigned importance placed by reconstructive and breast surgeons for all influencing factors assessed in relation to decisions made for CPM.
Figure 1:
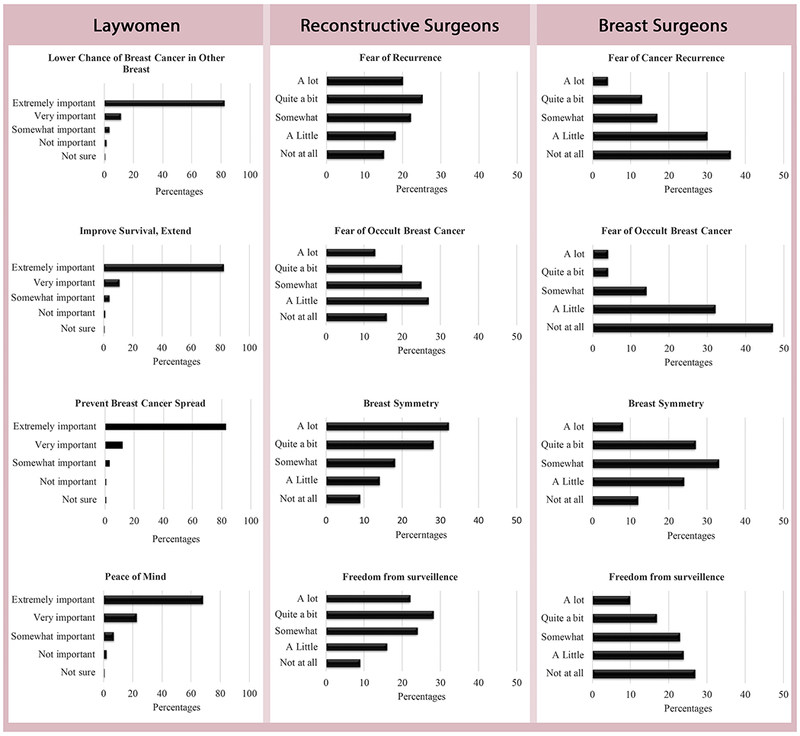
Most influential factors affecting CPM choice among Laywomen, Reconstructive and Breast Surgeons
DISCUSSION
CPM in women at low risk for future breast cancer has gained significant attention and raised some concern within the oncologic and surgical communities, leading to the recent creation of CPM consensus statements from multiple societies including American Society of Breast Surgeons (ASBS). The ASBS consensus statement outlines circumstances for which CPM should be considered including 1) documented BRCA1/2 carrier 2) strong family history of breast cancer and 3) history of mantle cell radiation before age 30 (1). In addition, the statement provides leeway for clinical judgment in situations where CPM “can” and “may” be considered including 1) to limit contralateral breast surveillance 2) improve breast reconstruction symmetry and 3) management of risk aversion or extreme anxiety (1). Given this current state, we sought to assess potential differences in decisions made for CPM among surgeons and laywomen when faced with a hypothetical early stage breast cancer diagnosis, with surgeons expected to have greater knowledge about breast cancer. We found that surgeon age and gender play a role with younger and female breast surgeons more in favor of CPM. This finding goes along with previous findings that demonstrated significantly higher CPM rate among patients of female oncology surgeons <50 years old (47%), as compared with male oncology surgeons (23%) even when controlling for male age (19). In addition to young age, white race amongst laywomen was associated with a choice for CPM, also consistent with other studies in the literature that have demonstrated higher rates of CPM in white women with early stage breast cancer (12,19–20).
On assessment of knowledge, laywomen with a high level of breast cancer knowledge had significantly lower odds of choosing CPM in comparison to women with lower levels of knowledge (OR 0.37, 95% CI 0.28-0.49). This goes along with findings from a recent study based on SEER data of women in Los Angeles and Georgia treated for early stage breast cancer (20). With a 17% CPM rate in the study population, only 38% of women who considered CPM knew that CPM does not improve survival for all women with breast cancer (20). It accordingly makes sense that specific level of breast cancer knowledge is likely influential in decisions made for CPM and as such decision aids could play a major role in delivery and processing of this information. In a comparison of breast cancer patient knowledge among women who received an in-visit decision aid versus usual care treatment discussion, Yao et al determined that the decision aid group had a higher percentage of women with high-level knowledge of breast cancer as determined by a post-visit questionnaire (18). Tucholka et al studied the most effective means of educating women on breast cancer treatment and survival comparing an electronic decision aid with providing url’s for select standard cancer websites, and determined that those receiving the electronic decision aid were more knowledgeable about survival, likelihood of death, and specific procedural risks, allowing them to make a more informed decision (21). In addition to content, how best to present treatment decision aids is challenging, particularly among the less educated and those of lower socioeconomic status. Currently, a multi-institutional randomized control trial comparing the effectiveness of written versus pictorial decision aides with typical office discussion, and its impact on breast cancer treatment decisions including CPM is underway and will provide clinician guidance on how best to improve the knowledge of patients facing this difficult decision (22).
Given their training, it is assumed that Breast and Reconstructive surgeons are overall more knowledgeable about breast cancer management and survival rates after unilateral mastectomy and CPM. Perhaps this knowledge gap explains the lower rates with which surgeons choose CPM for themselves or a loved one relative to laywomen in the general population. Yao et al examined breast surgeon knowledge among members of American Society of Breast Surgeons, and identified 232 of 592 surgeon respondents with a low (0-3 of 5) number of correct responses to knowledge questions about CPM and survival rates, contralateral breast cancer, and high-risk patients (23). We unfortunately did not assess surgeon knowledge in this study. Despite the presumed increased knowledge of surgeons, there are some who will opt for CPM when faced with a hypothetical early stage breast cancer diagnosis, demonstrating this to be a challenging personal decision for surgeons as well. This is significant, as surgeons have some influence over patient decisions and it has been shown that individual surgeons explain approximately 20% of the overall variation in CPM use in patients (24–26).
Consistent with previously established findings, the desire to lower the chance of future contralateral breast cancer, prevent cancer spread, improve survival and enhance peace of mind were among the most prominent reasons cited in favor of CPM by laywomen responders (1–7,10,12,18–19). Rosenberg et al., in a study of women without bilateral breast cancer who underwent CPM, found that women tend to overestimate their risk for breast cancer recurrence (27). These errors in estimation of cancer risk and specific concerns of women related to CPM provide relevant areas that can be focused on in efforts made towards better patient education and shared decision making. Regarding a desire to enhance peace of mind, Katz et al demonstrated that among breast surgeons initially reluctant to perform CPM, ~20-40% are willing to do so in order to satisfy patients’ desire for peace of mind and avoid conflict (26). In contrast, they were not likely to perform CPM in order to improve quality of life, avoid losing patient, reduce recurrence or improve survival (26). Very interesting in the current study were the differences between reconstructive surgeons and breast surgeons when they responded to questions on factors of importance when considering CPM for themselves or a loved one. A high proportion of reconstructive surgeons responded, “a lot” and “quite a bit”, to questions on the influence of symmetry (60%), freedom from surveillance (50%) and fear of recurrence (45%). Consistent with previous studies, a high proportion of breast surgeons responded “not at all” and “a little” to the questions of symmetry (26%), freedom from surveillance (51%), and fear of recurrence (66%) (13). The fact that the responses from both groups of surgeons to all evaluated factors, with the exception of the influence of the need for chemotherapy and radiation, were significantly different suggests that the factors driving the decisions in this clinical problem are viewed differently by the surgeon groups. It also suggests that there might be differences in the level of knowledge about the disease process between the surgeon groups. These potential differences in specialty specific knowledge are minimized with care delivered through multidisciplinary tumor boards where continued learning can occur, ideas can be exchanged and different perspectives on care can come together to formulate the best care plans.
Interest in breast reconstruction amongst study participants was relatively high with 83% of laywomen, 92% of breast surgeons and 99% of reconstructive surgeons expressing an interest in undergoing breast reconstruction. The availability of breast reconstruction was thought to be very important or extremely important by 60% of laywomen. Investigating the relationship between CPM and breast reconstruction, Agarwal et al demonstrated that reconstruction was highly correlated with CPM; women who had undergone CPM were approximately three times more likely to undergo reconstruction compared to women who did not have CPM (28). In addition to higher reconstruction rates in patients who had undergone CPM, Anderson et al found that women who had undergone CPM had a higher overall satisfaction and positive psychologic outlook as compared to unilateral mastectomy patients 97% vs 89% respectively, this is in spite of a slightly increased complication rate (29). Ultimately a desire for symmetry with breast reconstruction has been shown to be a factor that influences women’s decisions to proceed with CPM. This desire for symmetry tends to be a secondary factor relative to oncologic concerns in the decision-making process (30–32).
This study has a number of limitations that have an impact on our findings. The hypothetical nature of the survey may not represent actual decisions that would be made in what is typically a stressful situation following a cancer diagnosis. The low surgeon survey response rate is another limitation that leads to a potential non-responder bias. While a 100% response rate is desirable, lower response rates can be equally informative. The response rate for plastic surgeons may be a reflection of the fact that surveys were sent to all plastic surgeons including aesthetic, hand, and craniofacial surgeons, who may not have been inclined to respond to a survey about breast cancer and reconstruction. Surgeons are notoriously difficult to get survey responses from and it has been shown that the time in which a survey is sent (i.e. holidays) affects response rate. Also, respondents maybe unwilling to respond if they have received multiple surveys within a short period of time (33). Questions on the specific subspecialty of breast surgeons were not asked and would have been of value. The generalizability of findings from laywomen responders using Amazon Mechanical Turk® may also be limited as workers from this platform were younger, predominantly Caucasian and more educated than the general population. Nevertheless, through this platform we were able to engage and incorporate the opinions of a large and diverse public group.
CONCLUSION
Knowledge about breast cancer seems to play a significant role in decisions made for CPM. In this study, women would make fewer decisions in favor of CPM with better education on the disease process and the actual benefit or lack thereof of CPM. It is also likely that with improved knowledge specific groups of women, including those who are younger and those who are white will still opt for CPM as was suggested by our surgeon cohort. The choice for CPM, in women with early stage unilateral breast cancer and low risk for contralateral breast cancer, is many times appropriate given the multifactorial and very personal concerns women have to consider; these decisions when well informed should be supported. Concerted efforts through the use of educational tools and decision aids, should however be made to ensure that women are making well informed decisions on surgical treatment of breast cancer.
Supplementary Material
Figure, Supplemental Digital Content 1: Study Flow Diagram, INSERT HYPER LINK.
Table, Supplemental Digital Content 2: Breast Cancer Knowledge Among Laywomen, INSERT HYPER LINK.
Acknowledgements:
Support for this study was provided by the Macnguyen Research Fund for Plastic Surgery Residents at the University of Michigan and the Midcareer Investigator Award in Patient-Oriented Research (K24-AR053120-06). A portion of this work was presented at the American Society for Reconstructive Microsurgery Meeting Phoenix, AZ 2018.
Footnotes
Disclosure: None of the authors have a financial interest to declare in relation to the content of this article
References:
- 1.Boughey JC, Attai DJ, Chen SL, Cody HS, Dietz JR, Feldman SM, Greenberg GC, Kass RB, Landercasper J, Lemaine V, MacNeill F, Song DH, Staely AC, Wike LG, Willey SC, Yao KA, Margenthaler JA. Contralateral Prophylactic Mastectomy (CPM) Consensus Statement from the American Society of Breast Surgeons: Data of CPM Outcomes and Risks. Annals Surgical Oncology 2016; 23:3100–3105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Angelos P, Bedrosian I, Euthus DM, Herrmann VM, Katz SJ and Pusic A. Prophylactic Mastectomy: Challenging Considerations for the Surgeon. Annals Surgical Oncology 2015; 22:3208–3212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mutter RW, Frost MH, Hoskin TL, Johnson JL, Hartman LC, and Boughey JC. Breast Cancer after Prophylactic Mastectomy (bilateral or contralateral prophylactic mastectomy), a clinical entity: presentation, management, and outcomes. Breast Cancer Treatment. 2015; 153: 183–190. [DOI] [PubMed] [Google Scholar]
- 4.Wong SM, Freedman RA, Sagara Y, Ayogan F, Barry WT, and Golshan M. Growing Use of Contralateral Prophylactic Mastectomy Despite no Improvement in Long-term Survival for Invasive Breast Cancer. Annals Surgery 2017; 265:581–589. [DOI] [PubMed] [Google Scholar]
- 5.Zendejas B, Moriarty JP, O’Bryne J, Degnim AC, Farley DR, and Boughey JC. Cost-Effectiveness of Contralateral Prophylactic Mastectomy Versus Routine Surveillance in Patients with Unilateral Breast Cancer. Journal Clinical Oncology 2011; 29: 2393–3000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roberts A, Habibi M, Frick KD. Cost Effectiveness of Contralateral Prophylactic Mastectomy for Prevention of Contralateral Breast Cancer. Annals Surgical Oncology 2014; 21:2209–2217. [DOI] [PubMed] [Google Scholar]
- 7.Bedrosian I, Hu CY, and Chang GJ. Population-Based Study of Contralateral Prophylactic Mastectomy and Survival Outcomes of Breast Cancer Patients. J Natl Cancer Inst 2010; 102: 401–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Herrinton LJ, Barlow WE, Geiger AM, Elmore JG, Barton MB, Harris EL, Rolnick S, Pardee R, Husson G, Macedo A, Fletcher SW. Efficacy of prophylactic mastectomy in women with unilateral breast cancer a cancer research network project. J Clin Oncol 2005; 23:4275–86. [DOI] [PubMed] [Google Scholar]
- 9.Boughey JC, Hoskin TL, Degim AC, Sellers TA, Johnson JL, Kasner MJ, Hartmann LC, Frost MH. Contralateral Prophylactic Mastectomy is Associated with a Survival Advantage in high-risk Women with a Personal History of Breast Cancer. Ann Surg Oncol 2010; 17: 2702–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lostumbo L, Carbine NE, Wallace J. Prophylactic Mastectomy for the prevention of Cancer. Cochrane Database Syst Rev. 2010; 11: CD002748.. [DOI] [PubMed] [Google Scholar]
- 11.Pinell-White XA, Kolegraff K, Carlson GW. Predictors of Contralateral Prophylactic Mastectomy and the Impact on Breast Reconstruction. Ann Plas Surg 2014; 72; S153–S157. [DOI] [PubMed] [Google Scholar]
- 12.Jagsi R, Hawley ST, Griffith KA, Janz NK, Kurian AW, Ward KC, Hamilton AS, Morrow M, Katz SJ. Contralateral Prophylactic Mastectomy Decisions in a Population-Based Sample of Patients With Early Breast Cancer. JAMA Surg 2017;152: 272–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pesce C, Liederbach E, Wang C, Lapin B, Winchester DJ, and Yao K. Contralateral Prophylactic Mastectomy Provides No Survival Benefit In Young Women With Estrogen Receptor-Negative Breast Cancer. Annals Surgical Oncology. 2014. 21:3231–3239. [DOI] [PubMed] [Google Scholar]
- 14.Ipeirotis P “The New Demographics of Mechanical Turk| A Computer Scientist in Business School.” March 9, 2010, Behind-enemy-lines.com.
- 15.Truitt AR, Monsell SE, Avins AL, Nerenz DR, Lawrence SO, Bauer Z, Comstock BA, Edwards TC, Patrick DL, Jarwik JG, Lavellee DC. Prioritizing research topics: a comparison of crowdsourcing and patient registry. Qual Life Res. Doi: 10.1007/s11136-017-1566-9, 2017 [DOI] [PubMed] [Google Scholar]
- 16.Kim HS, Hodgins DC. Reliability and validity of data obtained from alcohol, cannabis, and gambling populations on Amazon’s Mechanical Turk. Psychol Addict Behav February;31 (1): 85–94, 2017 [DOI] [PubMed] [Google Scholar]
- 17.Hoddinott SN and Bass MJ. The Dillman Total Design Survey Method: A Sure-Fire Way to Get High Survey Return Rates. Can Fam Physician 1986. 32: 2366–2368. [PMC free article] [PubMed] [Google Scholar]
- 18.Yao K, Belkora J, Bedrosian I, Rosenberg S, Sisco M, Barrera E, Kyrillios A, Tilburt J, Wang C, Rabbitt S, Pesce C, Simovic S, Winchester DJ, Sepucha K. Impact of an In-visit Decision Aid on Patient Knowledge About Contralateral Prophylactic Mastectomy: A Pilot Study. Annals of Surgical Oncology 2017; 1:91–99. [DOI] [PubMed] [Google Scholar]
- 19.Arrington AK, Jarosek SL, Virnig BA. Patient and Surgeon Characteristics associated with Increased Use of Contralateral Prophylactic Mastectomy in Patients with Breast Cancer. Annals of Surgical Oncology 2009; 16:2697–2704. [DOI] [PubMed] [Google Scholar]
- 20.Kim Y, McCarthy AM, Bristol M, and Armstrong K. Disparities in contralateral prophylactic mastectomy use among women with early-stage breast cancer. Npj Breast Cancer. 2017. 3:2 doi: 10.1038/s41523-017-004-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tuckolka JL, Yang DY, Bruce JG, Steffens NM, Schumacher JR, Greenberg CC, Wilke LG, Steiman J, Neuman HB. A Randomized Controlled Trial Evaluating the Impact of Web-Based Information on Breast Cancer Patients’ Knowledge of Surgical Treatment Options. J Am Coll Surg 2018;226: 126–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Durand MA, Yen RW, O’Malley J, Politi MC, Dhage S, Rosenkranz K, Weihman K, Margenthaler J, Tosteson ANA, Crayton E, Jackson S, Bradlet A, Volk RJ, Sepucha K, Ozanne E, Perac-Lima S, Song J, Acosta J. What Matters Most: Protocol for a Randomized Controlled Trial of Breast Cancer Surgery Encounter Decision Aids Across Socioeconomic Strata. BMC Public Health 2018; 18: 241–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yao K, Belkora J, Sisco M, Rosenberg S, Bedrosian I, Liederbach E, Wang C. Survey of the Deficits of Surgeon Knowledge of Contralateral Prophylactic Mastectomy. JAMA Surgery. 2016. 151: 391–393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hershman DL, Buono D, Jacobson JS, McBride RB, Tsai WY, Joseph KA, Neugut AI. Surgeon Characteristics and Use of Breast Conservation Surgery in Women with Early Stage Breast Cancer. Ann Surg 2009; 249: 828–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bellavance E, Peppercorn J, Kronsberg S, Greenup R, Keune J, Lynch J, Collyar D, Magder L,Tilburt J, Hubocky F, Yao, K. Surgeons’ Perspective of Contralateral Prophylactic Mastectomy. Annals of Surgical Oncology 2016; 23:2779–278. [DOI] [PubMed] [Google Scholar]
- 26.Katz SJ, Hawley ST, Hamilton AS, Ward KC, Morrow M, Jagsi R, Hofer TP. Surgeon Influence on Variation in Receipt of Contralateral Prophylactic Mastectomy for Women with Breast Cancer. JAMA Surgery. 2018; 153:29–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosenberg SM, Tracey MS, Meyer ME, Sepucha K, Gelber S, Hirsfield-Barek J, Troyan S, Morrow M, Schapira L, Come SE, Wilner EP, Partridge AN. Perceptions, knowledge, and satisfaction with contralateral prophylactic mastectomy among young women with breast cancer: a cross-sectional survey. Annals Internal Medicine 2013; 159: 373–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Agarwal S, Kidwell KM, Kraft CT, Kozlow JH, Sabel MS, Chung KC, and Momoh AO. Defining the Relationship between Patient Decisions to Undergo Breast Reconstruction and Contralateral Prophylactic Mastectomy. Plastic and Reconstructive Surgery. 2015;135:661–670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Anderson C, Islam JY, Hodgson E, Sabatino SA, Rodriguez JL, Lee CN, Sandler DP, Nichols HB. Long-term Satisfaction and Body Image After Contralateral Prophylactic Mastectomy. Annals of Surgical Oncology 2017;24:1499–1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Momoh AO, Cohen WA, Kidwell KM, Hamill JB, Qi J, Pusic AL, Wilkins EG, Matros E. Tradeoffs Associated With Contralateral Prophylactic Mastectomy in Women Choosing Breast Reconstruction. Annals of Surgery. 2017. 266:158–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Awis Ashfaq, McGhan LJ Pockaj BA, Gray RJ Bageria SP, McLaughlin SA Casey WJ, Rebecca AM, Kreymerman P, Wasif N. Impact of Breast Reconstruction on the Decision to Undergo Contralateral Prophylactic Mastectomy. Annals of Surgical Oncology 2014;21:2934–2940. [DOI] [PubMed] [Google Scholar]
- 32.Buchanan PJ, Abdulghani M, Waljee JF, Kozlow JH, Sabel MS, Newman LA, Chung KC, Momoh AO. An Analysis of the Decisions Made for Contralateral Prophylactic Mastectomy and Breast Reconstruction. 2016138: 29–40. [DOI] [PubMed] [Google Scholar]
- 33. Lau FH, Chung KC Survey Research: A Primer for Hand Surgery. J Hand Surg Am. 2005;30 (5): 893.E1–11. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure, Supplemental Digital Content 1: Study Flow Diagram, INSERT HYPER LINK.
Table, Supplemental Digital Content 2: Breast Cancer Knowledge Among Laywomen, INSERT HYPER LINK.


