Abstract
A patient with right iliac fossa pain underwent CT angiography which demonstrated isolated caecal necrosis with associated superior mesenteric artery (SMA) stenosis. This was supported by colonoscopic findings and histopathological analysis. Isolated caecal necrosis is a rare presentation of ischaemic colitis.. Clinical and imaging findings of ischaemic colitis may mimic other pathologies. To improve diagnostic accuracy both referrers and radiologists should be aware of risk factors associated with ischaemic colitis. Isolated bowel wall thickening and pneumatosis of a colonic segment on CT are suggestive of focal bowel ischaemia, in the right clinical context.
Clinical presentation
Ms P, a 78-year-old lady, presented to the acute surgical unit with a 4-day history of vomiting, abdominal pain and diarrhoea. There was no history of blood or mucus per rectum. Systems review was unremarkable. Her past medical history included an appendicectomy, hysterectomy and bilateral salpingo-oophorectomy (performed 44 years ago for menorrhagia), atrial fibrillation managed with warfarin, hypertension and chronic kidney disease Stage 3.
On examination, her vital signs were stable, with a heart rate of 65/min, blood pressure of 156/77 mmHg, temperature of 36.4°C, respiratory rate of 14/min and oxygen saturations of 96% on air. Abdominal examination revealed right iliac fossa tenderness without signs of peritonism. Systemic examination was otherwise unremarkable.
Initial blood tests showed a raised c-reactive protein of 109 mg l−1, normal white cell count of 10 × 109 cells per litre and haemoglobin of 134 g l−1. Coagulation screen was abnormal with an elevated INR of 5.45 and aPTT of 52.7 s. Renal and liver function tests were at the patient’s baseline. Urine dipstick was negative for nitrites and leucocytes.
Differential diagnosis and initial management
Based on Ms P’s presentation, a working diagnosis of right-sided colitis was established. Possible causes for the colitis included infection and ischaemia. Other causes e.g. inflammatory bowel disease or post-radiotherapy colitis were unlikely given the patient’s age and lack of previous history. Differential diagnoses included right-sided diverticulitis, stump appendicitis and bowel malignancy. A useful test would have been an arterial or venous blood gas, as this may have demonstrated a lactic acidosis secondary to ischaemia, but unfortunately this was not performed.
Hospital admission was arranged, and Ms P was commenced on i.v. fluids, i.v. antibiotics (co-amoxiclav) and analgesia. Warfarin was withheld. Abdominal and erect chest radiographs were requested.
Investigations/Imaging findings
The plain radiographs were unremarkable, with no signs of perforation. Following consultant post-take review, a CT scan of the abdomen and pelvis with contrast was requested. The clinical question provided on the request was “?appendicitis ?colitis”. The images were acquired in the portal venous phase and revealed a 67 × 37 mm gas and fluid-filled structure, with moderate surrounding fat stranding, which was reported as possible acute appendicitis with a contained perforation (Figure 1). The remainder of the GI tract and other systems were unremarkable.
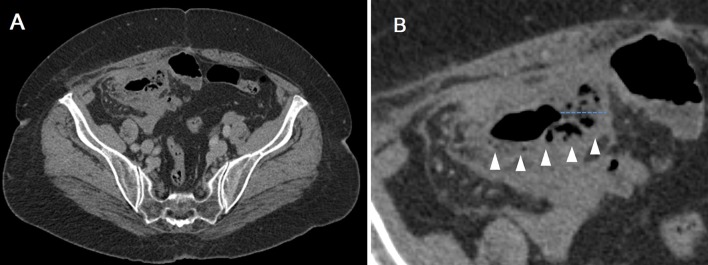
Figure 1.
(A) Axial CT image at the level of the caecum and (B) magnified view of the caecum, demonstrating intramural gas (white arrowheads) and thickened bowel wall (blue dotted line).
The clinical team clarified Ms P’s past medical history, and confirmed that she had had an appendicectomy aged 18. The images were then discussed in the departmental GI meeting, where upon review the imaging findings were thought to represent focal ischaemia involving the caecum with mural thickening, oedema and intramural gas, consistent with isolated caecal necrosis (Figure 1). No associated perforation or collection was noted. There also appeared to be significant narrowing of the superior mesenteric artery (SMA), which was thought to be a predisposing factor. Follow-up colonoscopy and CT angiography was recommended to exclude an underlying tumour, confirm the SMA stenosis and check for resolution.
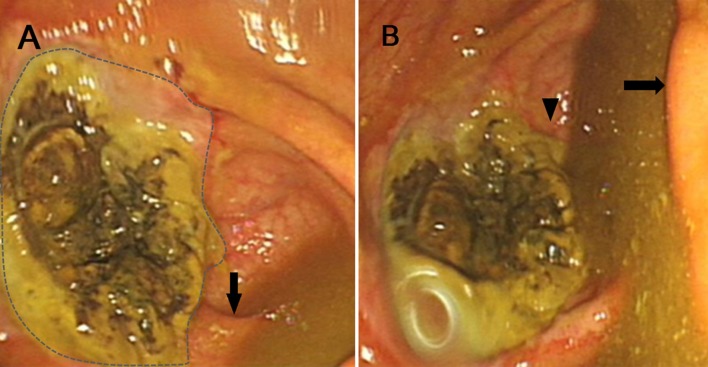
Colonoscopy was performed during the same admission and identified an ulcerated area in the caecal pole, adjacent to the appendiceal orifice (Figure 2a, and Supplementary Video 1, Colonoscopy video clip demonstrating ulcerated ischaemic mucosa (0 s), close up of unaffected appendiceal orifice (15 secs), and site of biopsy at the edge of the ulcerated area (25 secs).). The appearances were thought to be inflammatory rather than neoplastic. Biopsy samples were obtained, and showed focally ulcerated large bowel mucosa with adjacent mild architectural distortion showing regenerative crypts with mucin depletion, and extensive granulation tissue within the submucosa. The histopathology report supported the imaging findings, concluding that the microscopic features could represent a consequence of ischaemia, although the possibility of a submucosal lesion could not be excluded.
Figure 2.
(A) Endoscopic view of the caecum, showing the area of ulcerated ischaemic mucosa (dashed outline), adjacent to this is the unaffected appendix orifice (black arrow); (B) endoscopic view of the caecum showing the ileocaecal valve (black arrow) and appendix orifice (black arrowhead).
Following this, a repeat CT scan was performed pre- and post-arterial phase contrast administration. Imaging findings revealed a tight stenosis of the proximal SMA (Figure 3), with several pancreaticoduodenal collaterals suggesting chronicity (Figure 3 and Supplementary Video 2, 3D reconstruction video, rotating from AP to left lateral view, illustrating tight SMA stenosis and pancreatico-duodenal collateral vessels). There was partial resolution of the changes in the right iliac fossa, with reduction in the oedema and fat stranding around the caecum, which remained mildly thick-walled with some persistent intramural gas. The coeliac artery and inferior mesenteric artery were patent. In addition, a tight stenosis was noted at the origin of the right renal artery, and the right kidney was mildly atrophic. The remainder of the scan was unremarkable.
Figure 3.
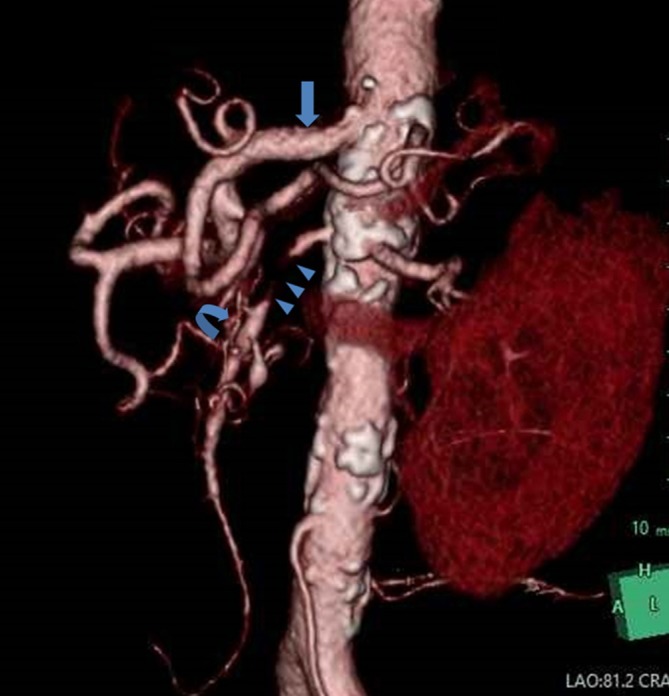
3D reconstruction of CT angiogram (left anterior oblique view), showing the coeliac axis (blue block arrow), tight SMA stenosis (blue arrowheads) and pancreatico-duodenal collaterals (curved arrow). SMA, superior mesenteric artery; 3D, three-dimensional.
Outcome/Follow up
Ms P made a gradual recovery, with an associated improvement in inflammatory markers. She was reviewed by the vascular team prior to discharge, warfarin was restarted, and aspirin and simvastatin were commenced. The case was discussed in the vascular MDT the following week, which concluded that the SMA stenosis may have been complicated by thromboembolic disease, leading to the acute presentation, as focal ischaemia is rare in isolated SMA stenosis. In view of the single vessel disease, in the presence of a well-developed collateral circulation, it was thought that the risks of vascular stenting would outweigh the potential benefits. Consequently, vascular stenting was not advised, and medical management in the form of an antiplatelet agent was recommended, in addition to Ms P's existing warfarin medication. Ms P would be re-imaged with a repeat CT scan in a year’s time.
Discussion
Ischaemic colitis is the most common form of intestinal ischaemia.1–3 It ranges from transient self-limiting ischaemia (in this case), to gangrenous pancolitis. The pathophysiology, as with other forms of ischaemia, is due to insufficient blood supply (in this setting a surrogate for oxygen delivery) to meet metabolic demands. The colon is particularly susceptible to ischaemia for various reasons, including its relatively low blood flow compared to the rest of the GI tract, and less developed microvasculature, embedded in a thicker wall.2
Specific factors affecting the right side of the colon include smaller and less developed vasa recta (end vessels supplying the colonic wall), which have sparse collaterals, and are particularly sensitive to vasospasm.2 The blood supply to the caecum is derived from the anterior and posterior caecal arteries, branches of the ileocolic, from the SMA. In an attempt to explain previous cases of isolated caecal necrosis, several authors have suggested that the caecum is a watershed area.4–6 The caecal arteries may arise from the ileal branch or colic branch of the ileocolic artery, or an ileocolic anastomotic arcade. Authors have postulated that those arising directly from either the ileal or colic branches without the presence of an anastomotic arcade are more susceptible to ischaemia. However, this has not been proven clinically as most patients, such as in Ms P’s case, do not undergo catheter angiography.
Many conditions may predispose to ischaemic colitis; essentially any factors that affect the haemodynamic stability of the colonic vascular bed may contribute, commonly atherosclerotic disease e.g. vascular stenosis, thromboembolic conditions e.g. atrial fibrillation and conditions predisposing to microvascular disease e.g. chronic kidney failure, all of which were present in Ms P’s case. Certain drugs, especially antihypertensive agents, are also a common risk factor. Ms P’s active drug history included four of these (Bendroflumethiazide, Irbesartan, Spironolactone and Diltiazem), although no episodes of hypotension were recorded on the observations charts. Other factors that are commonly associated include causes of shock, mechanical bowel obstruction, vasculitis and hypercoagulable states.2,3,7
Ischaemic colitis most commonly affects the left side of the colon. Watershed areas are most at risk, in particular Griffith’s point at the splenic flexure, and Sudeck’s point at the recto-sigmoid junction. Isolated right colon ischaemia is less common than left-sided pathology. In a series of 1000 patients, 8% of these affected the right colon,2 although in a more recent study involving 313 patients the right colon was involved in 25% of cases.8 In a recent multicentre Spanish study of 341 cases, 6.5% of these included caecal involvement.1 Isolated caecal necrosis is rare, with only a few case reports in the literature.4,5,9
Ischaemic colitis usually presents with a combination of acute abdominal pain, bloody diarrhoea and the urge to defaecate.1,2 Right-sided ischaemic colitis is less likely to present with blood per rectum, and may mimic other pathologies given in the differential diagnosis above. Laboratory test results are often similar in many diagnoses, showing raised inflammatory markers. A metabolic lactic acidosis may raise clinical suspicion, focusing the history to assess for risk factors of ischaemic colitis.
Imaging findings of bowel ischaemia can include circumferential bowel wall thickening, dilatation, abnormal or absent mural enhancement, mesenteric stranding, vascular engorgement, ascites, pneumatosis and portal venous gas.10,11 The most common radiological sign is bowel wall thickening, present in 94% of ischaemic colitis (Figure 1); however, this is also the least specific finding. The presence and degree of bowel wall thickening does not correlate with the severity of ischaemic colitis.10 Hypo-attenuation of the bowel wall (not apparent in Ms P’s case) has been reported in 61% of cases of ischaemic colitis, more commonly with venous occlusion. Pneumatosis (Figure 1) is less common, being present in 6–28% of cases, but the specificity of pneumatosis and portal venous gas for acute bowel ischaemia approaches 100% in the correct clinical setting.10
The appearance of isolated caecal necrosis may mimic other pathologies such as a caecal infection, Crohn’s disease, appendicitis with secondary inflammation of the caecum and malignancy of the caecum or appendix. Accurate clinical details may guide the radiologist to the correct diagnosis, and imaging findings of isolated caecal wall thickening and pneumatosis are suggestive.
Learning points
Accurate clinical information on imaging requests is vital to ensure ischaemia is considered in relevant cases and differentials such as appendicitis are excluded if there is a history of appendicectomy.
Multidisciplinary imaging meetings can be very useful for troubleshooting unusual cases.
Isolated right colon ischaemia should be included in the differential for right-sided abdominal pain.
Numerous risk factors in the history may make colonic ischaemia more likely, e.g. vascular risk factors, atrial fibrillation, antihypertensive agents, shock, mechanical bowel obstruction, vasculitis and hypercoagulable states.
Localised colonic wall thickening and pneumatosis on CT in the setting of acute abdominal pain is suggestive of ischaemic colitis.
Footnotes
Acknowledgment: I would like to thank the patient for her gracious support and patience, Dr Hameed Rafiee for his valuable time and tireless effort, and Dr Ian Beales for providing the excellent endoscopy images and video.
Consent: Written informed consent was obtained from the patient for publication of this case report, including accompanying figures.
Contributor Information
Nathan Howard Ho Leung Chan, Email: nchan@hotmail.co.uk.
Hameed Rafiee, Email: hameed.rafiee@nnuh.nhs.uk.
Ian L P Beales, Email: ian.beales@nnuh.nhs.uk.
Ravindran Karthigan, Email: rkarthigan@gmail.com.
Annabel Ciorra, Email: annabel.ciorra@nnuh.nhs.uk.
Taeyang Kim, Email: taeyang.kim@nnuh.nhs.uk.
REFERENCES
- 1. Montoro MA , Brandt LJ , Santolaria S , Gomollon F , Sánchez Puértolas B , Vera J , et al. . Clinical patterns and outcomes of ischaemic colitis: results of the Working Group for the Study of Ischaemic Colitis in Spain (CIE study) . Scand J Gastroenterol 2011. ; 46 : 236 – 46 . doi: 10.3109/00365521.2010.525794 [DOI] [PubMed] [Google Scholar]
- 2. Green BT , Tendler DA . Ischemic colitis: a clinical review . South Med J 2005. ; 98 : 217 – 22 . doi: 10.1097/01.SMJ.0000145399.35851.10 [DOI] [PubMed] [Google Scholar]
- 3. Theodoropoulou A , Koutroubakis IE . Ischemic colitis: clinical practice in diagnosis and treatment . World J Gastroenterol 2008. ; 14 : 7302 – 8 . doi: 10.3748/wjg.14.7302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Simon AM , Birnbaum BA , Jacobs JE . Isolated infarction of the cecum: CT findings in two patients . Radiology 2000. ; 214 : 513 – 6 . doi: 10.1148/radiology.214.2.r00fe15513 [DOI] [PubMed] [Google Scholar]
- 5. Yamazaki T , Shirai Y , Tada T , Sasaki M , Sakai Y , Hatakeyama K . Ischemic colitis arising in watershed areas of the colonic blood supply: a report of two cases . Surg Today 1997. ; 27 : 460 – 2 . doi: 10.1007/BF02385714 [DOI] [PubMed] [Google Scholar]
- 6. Rist CB , Watts JC , Lucas RJ . Isolated ischemic necrosis of the cecum in patients with chronic heart disease . Dis Colon Rectum 1984. ; 27 : 548 – 51 . doi: 10.1007/BF02555524 [DOI] [PubMed] [Google Scholar]
- 7. Gandhi SK , Hanson MM , Vernava AM , Kaminski DL , Longo WE . Ischemic colitis . Dis Colon Rectum 1996. ; 39 : 88 – 100 . doi: 10.1007/BF02048275 [DOI] [PubMed] [Google Scholar]
- 8. Brandt LJ , Feuerstadt P , Blaszka MC . Anatomic patterns, patient characteristics, and clinical outcomes in ischemic colitis: a study of 313 cases supported by histology . Am J Gastroenterol 2010. ; 105 : 2245 – 52 . doi: 10.1038/ajg.2010.217 [DOI] [PubMed] [Google Scholar]
- 9. Schuler JG , Hudlin MM . Cecal necrosis: infrequent variant of ischemic colitis. Report of five cases . Dis Colon Rectum 2000. ; 43 : 708 – 12 . [DOI] [PubMed] [Google Scholar]
- 10. Wiesner W , Khurana B , Ji H , Ros PR . CT of acute bowel ischemia . Radiology 2003. ; 226 : 635 – 50 . doi: 10.1148/radiol.2263011540 [DOI] [PubMed] [Google Scholar]
- 11. Balthazar EJ , Yen BC , Gordon RB . Ischemic colitis: CT evaluation of 54 cases . Radiology 1999. ; 211 : 381 – 8 . doi: 10.1148/radiology.211.2.r99ma28381 [DOI] [PubMed] [Google Scholar]