Abstract
Background
Patient experience is often measured quantitatively, but that approach has limitations for understanding the entire experience. Qualitative methods can help to understand more complex issues most important to patients and their families. The purpose of the present work was to use a qualitative analysis examining the patient experience of ambulatory cancer care in Ontario to generate a deeper understanding of the patient experience and to lead to solutions for improvement.
Methods
Data from the Ambulatory Oncology Patient Satisfaction Survey (aopss) for 2013–2015 were used to conduct a qualitative content analysis. The aopss is a retrospective paper-based survey, mailed to patients who are currently receiving cancer treatment or who have received cancer treatment within the preceding 6 months, that is designed to capture their experiences. Patients who were surveyed were asked, “Is there anything else you would like to tell us about your cancer care services?” The National Research Corporation Canada’s patient-centred care framework was used to guide the analysis.
Results
From the 5391 patients who responded, 7328 coded responses were generated, of which 3658 (49.9%) were related to the patient-centred care framework. New subthemes were identified: diagnosis sensitivity; emotional support resources; care delivery with care, compassion, and comfort; continuity of care between departments and in the community; access to cancer centre personnel; patient–health care provider communication; confidence in the health care provider; wait times; health care provider and treatment coordination; and parking.
Conclusions
The results identify facilitators and barriers to the patient experience in the ambulatory cancer treatment setting from the patient perspective and identify opportunities to improve the patient experience.
Keywords: Person-centred care, patient experiences, survey research, qualitative analyses
BACKGROUND
Patient experience plays an important role in defining and improving the quality of cancer care and services worldwide1–4. Defined as “the sum of all interactions, shaped by an organization’s culture that influences patient perceptions across the continuum of care”5, patient experience has 8 dimensions6:
■ Patient preferences
■ Emotional support
■ Physical comfort
■ Information and communication
■ Continuity and transition
■ Coordination of care
■ Involvement of family and friends
■ Access to care
In health care, patient experience data are traditionally collected through surveys or questionnaires3,7–9, capturing the patient’s view about their experience while receiving care10–12. The patient experience has been included as a core pillar of quality, having been identified as a means of improving patient safety and clinical effectiveness13. Literature suggests a positive association between the patient experience and health outcomes13,14, adherence to treatment and medications15–17, preventive care14,18, and health care resource use13. The patient experience has therefore often been used to drive improvements in care delivery and services through quality improvement and as a core measure of success1,11,19.
Evidence suggests that cancer patients encounter challenges related to the patient experience throughout their care20. Examples include reports by patients of delays in, and lack of coordination of, care21; errors in treatment and their consequences22; and gaps in emotional support23,24. Given an increasing focus on improving the patient experience in cancer care, there is a growing need to gain an in-depth understanding of the patient experience of cancer services to drive improvements in care delivery.
Measuring the patient experience through traditional methods poses challenges such as limiting a patient experience measure to a single dimension, which could discount the interactions that have a powerful effect on experience and outcomes25. Standard survey questions do not allow patients the opportunity to elaborate on their experience, often resulting in missed opportunities to understand issues most important to those patients25. Staff and clinicians therefore often find it difficult to interpret and act on survey results to effectively improve care or services, which has direct implications for the quality improvement realm25,26.
In Ontario, the focus on measuring the patient experience of ambulatory cancer services to improve its quality has been increasing. The Ambulatory Oncology Patient Satisfaction Survey (aopss) is used to collect data and to report on 8 dimensions of the patient experience in ambulatory cancer care settings27. The 105-question aopss is a retrospective paper-based mailed survey that allows patients receiving treatment (or those who have received cancer treatment in the preceding 6 months) to provide anonymous and personalized descriptions of their overall treatment experience27. Quantitative findings from the aopss are publicly reported annually on the Cancer System Quality Index27. The aopss also includes a qualitative open-ended question that patients can use to elaborate on their care experience.
Despite the availability of quantitative data from the aopss, its standard survey questions do not allow patients the opportunity to elaborate on their experience in a way that generates an in-depth understanding of the patient experience of cancer services and that leads to the identification of opportunities for quality improvement. To further understand the patient experience of ambulatory cancer services, an in-depth qualitative analysis was undertaken. The purpose of the study was to conduct a qualitative analysis of the aopss to examine the patient experience of ambulatory cancer care in Ontario, generating a deeper understanding of the patient experience in cancer care and leading to improvement solutions.
METHODS
Data Source
In the past, the aopss has been used in multiple Canadian provinces; however, that use is not part of a national initiative, because implementation of the survey is at the discretion of the province. In Ontario, Cancer Care Ontario is the legislative authority designated to collect aopss data, in partnership with the regional cancer centres and an approved survey vendor. Patients were eligible to complete the aopss if they were receiving or had received cancer treatment (that is, surgery, chemotherapy, radiation therapy) in the preceding 6 months at any of the 14 regional cancer centres in Ontario. Patients had to be 18 years of age or older to receive the aopss. The survey is available in English and French. On a monthly basis, each regional cancer centre submits a list of eligible patients to the approved survey vendor. The aopss is then disseminated by the survey vendor to a random sample of eligible patients. If the eligible patients complete and return the aopss, the survey vendor then transcribes the qualitative comments. Cancer Care Ontario subsequently receives the qualitative comments electronically—a resource to which we were granted access. In a very few cases, legibility is an issue.
The final question on the aopss is open-ended. It asks, “Is there anything else you would like to tell us about your cancer care services?” Anonymous qualitative data from that aopss question for fiscal years 2013/2014 and 2014/2015 were used.
Analysis
Using qualitative content analysis, the open-ended comments were coded in the NVivo software application (version 11: QSR International, Melbourne, Australia). Qualitative content analysis is an analytic approach whereby text data are interpreted in a systematic classification process of coding and identifying themes28. The process involves a close examination of the language used, both explicitly and through inference, to better understand a given phenomenon. Directed content analysis uses an existing conceptual or theoretical framework28. In our analysis, the NRC Health (Toronto, ON) patient-centred care framework was used (Table I).
TABLE I.
Overview of the NRC Health patient-centred care framework6
| Care dimension | Definition |
|---|---|
| Respect for the values, preferences, and expressed needs of patients |
|
|
| |
| Coordination and integration of care |
|
|
| |
| Information and education |
|
|
| |
| Physical comfort |
|
|
| |
| Emotional support and alleviation of fear and anxiety |
|
|
| |
| Involvement of family and friends |
|
|
| |
| Continuity and transition |
|
|
| |
| Access to care |
|
Two authors (LGC, EB) independently coded the same sample of 500 responses (approximately 10% of the total responses) to ensure consistency in applying the NRC Health framework. Qualitative responses often included multiple sentences with separate ideas based on the NRC Health patient-centred care framework. Qualitative responses that contained more than 1 idea were therefore attributed to more than 1 dimension in the NRC Health patient-centred care framework. Upon completion, the two authors reviewed the codes together and established coding content and structure to refine inclusions and exclusions to the existing framework dimensions and to resolve discrepancies where necessary.
The remaining qualitative responses were divided equally between the two authors for open coding. The NRC Health patient-centred care framework was applied. Text that did not fit within the existing framework was categorized as “other comment.” Many responses included 2 or more discrete statements that were individually coded, generating more coded statements than total number of survey comments. Once the coding was completed, the two authors reviewed the application of the coding framework, refining inclusions and exclusions to each dimension and resolving any discrepant coding. Using the established coding structure, a constant comparison approach was used to refine the codes and content within each patient-centred care dimension29. The authors reread every response, establishing discrete subthemes within each dimension. One author (EB) iteratively read and coded all responses categorized within the patient-centred care framework dimensions; the second author (LGC) iteratively read all responses coded as “other comment.” A third review was then held to discuss the results.
In the final coding iteration, the two authors reviewed each other’s coding schemes. Each coded phrase was therefore reviewed twice to ensure data credibility29. The coded content of each patient-centred care dimension in the NRC Health framework and applicable subtheme was reread, compared against other codes within the subtheme, and then finalized. The authors then reorganized the subthemes within the NRC Health framework to align with the patient journey along the cancer continuum.
RESULTS
Of 24,822 patients who were mailed (postal mail) the aopss to complete during 2013/2014 and 2014/2015, 12,899 returned a completed questionnaire (response rate: 52.0%). Of the patients who returned aopss questionnaires, 5391 provided a qualitative response (overall response rate: 21.7%). Table II provides an overview of the sample’s demographics.
TABLE II.
Characteristics of the study patients
| Characteristic | Value |
|---|---|
| Patients (n) | 5391 |
|
| |
| Sex [n (%)] | |
| Women | 2641 (49) |
| Men | 1885 (35) |
| Missing | 865 (16) |
|
| |
| Age group [n (%)] | |
| ≤29 Years | 54 (1) |
| 30 49 Years | 466 (8.6) |
| 50 69 Years | 2730 (50.6) |
| ≥70 Years | 2141 (39.7) |
|
| |
| Education level [n (%)] | |
| Grade 9 or less | 350 (6.5) |
| Some high school but did not graduate | 468 (10.5) |
| High school graduate | 911 (16.9) |
| College, trade, or technical school | 1103 (20.5) |
| University undergraduate degree | 636 (11.8) |
| Post-university or graduate education | 492 (9.1) |
| Missing | 1431 (26.5) |
|
| |
| Cancer type [n (%)] | |
| Brain | 59 (1.1) |
| Breast | 1169 (21.7) |
| Cervix, uterine, or ovarian | 211 (3.9) |
| Colorectal or bowel | 360 (6.7) |
| Head and neck | 155 (2.9) |
| Hematologic | 162 (3.0) |
| Kidney or bladder | 61 (1.1) |
| Lung | 327 (6.1) |
| Lymphoma | 343 (6.4) |
| Melanoma | 114 (2.1) |
| Prostate or testicular | 446 (8.3) |
| Sarcoma | 51 (0.9) |
| Stomach | 45 (0.8) |
| Other | 352 (6.5) |
| Do not know | 19 (0.4) |
| Missing | 1517 (28.1) |
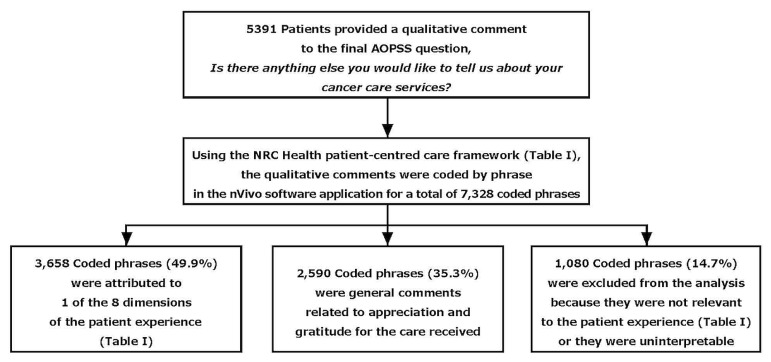
Figure 1 presents an overview of the content analysis. Using the NRC Health patient-centred care framework (Table I), 5391 qualitative responses were coded, resulting in 7328 coded phrases, of which 3658 (49.9%) were attributed to 1 of the 8 dimensions of patient-centred care. “Other comments” consisted of 2590 comments (35.3%) related to general appreciation and gratitude (for example, “Thank you so much for the care you provided”) and 1080 comments (14.7%) related to specific treatment courses or feedback on the survey format. The latter comments were excluded from the present analysis.
FIGURE 1.
Overview of the qualitative content analysis using NVivo (version 11: QSR International, Melbourne, Australia). AOPSS = Ambulatory Oncology Patient Satisfaction. Survey; NRC Health = National Research Corporation Health.
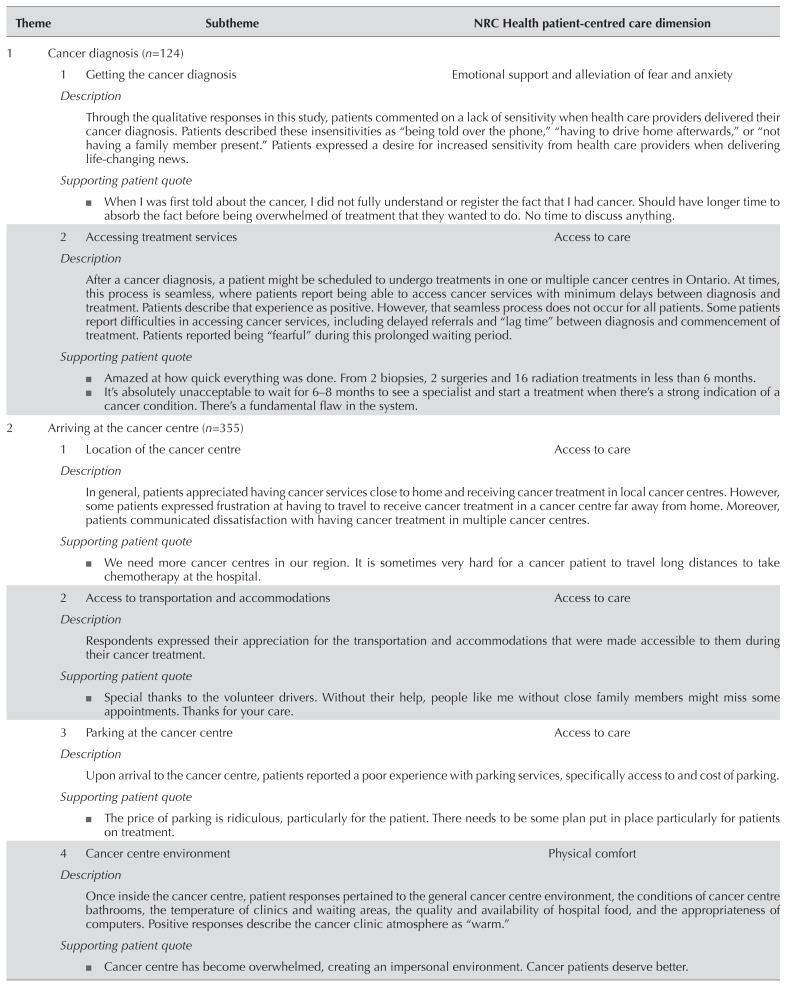
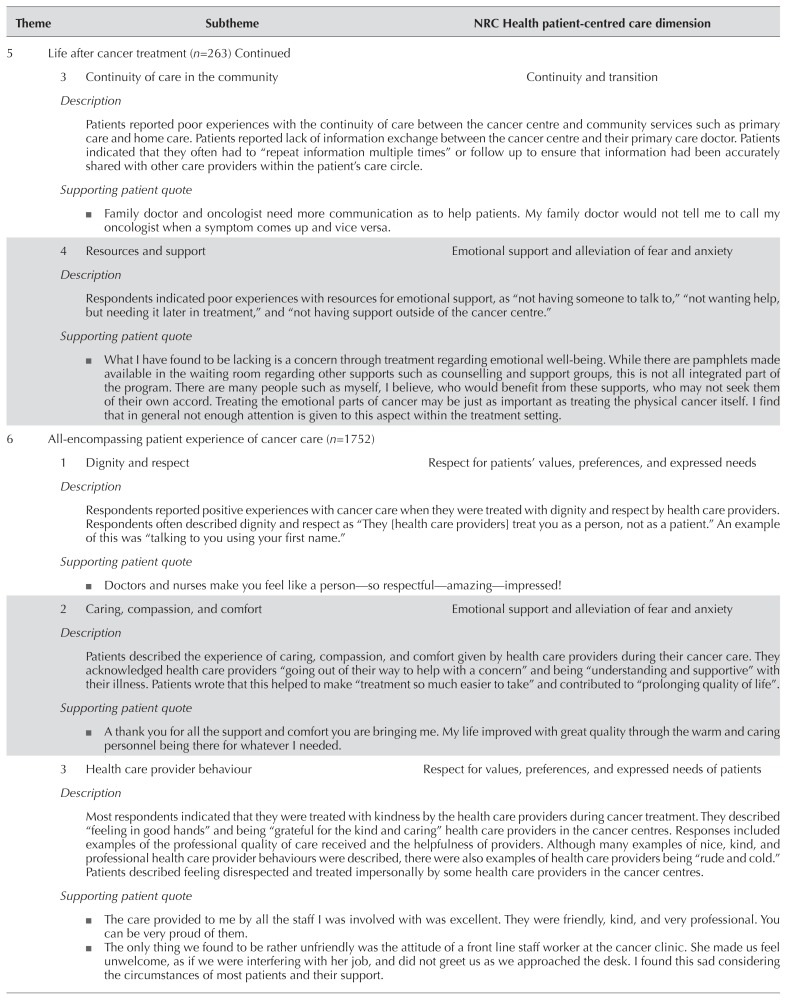
In the coded themes and subthemes, patients described positive and negative experiences as they progressed through the cancer continuum (Table III). That continuum begins with the experience of a cancer diagnosis, followed by the treatment experience and the experience with support after treatment. It ends with components of the overarching patient experience. Each part of the continuum is supported by a representative quote.
TABLE III.
Themes and subthemes, with associated patient quotes
| Theme | Subtheme | NRC Health patient-centred care dimension |
|---|---|---|
| 1 | Cancer diagnosis (n=124) | |
| 1 Getting the cancer diagnosis | Emotional support and alleviation of fear and anxiety | |
| Description | ||
| Through the qualitative responses in this study, patients commented on a lack of sensitivity when health care providers delivered their cancer diagnosis. Patients described these insensitivities as “being told over the phone,” “having to drive home afterwards,” or “not having a family member present.” Patients expressed a desire for increased sensitivity from health care providers when delivering life-changing news. | ||
| Supporting patient quote | ||
|
||
|
| ||
| 2 Accessing treatment services | Access to care | |
| Description | ||
| After a cancer diagnosis, a patient might be scheduled to undergo treatments in one or multiple cancer centres in Ontario. At times, this process is seamless, where patients report being able to access cancer services with minimum delays between diagnosis and treatment. Patients describe that experience as positive. However, that seamless process does not occur for all patients. Some patients report difficulties in accessing cancer services, including delayed referrals and “lag time” between diagnosis and commencement of treatment. Patients reported being “fearful” during this prolonged waiting period. | ||
| Supporting patient quote | ||
|
||
|
| ||
| 2 | Arriving at the cancer centre (n=355) | |
| 1 Location of the cancer centre | Access to care | |
| Description | ||
| In general, patients appreciated having cancer services close to home and receiving cancer treatment in local cancer centres. However, some patients expressed frustration at having to travel to receive cancer treatment in a cancer centre far away from home. Moreover, patients communicated dissatisfaction with having cancer treatment in multiple cancer centres. | ||
| Supporting patient quote | ||
| We need more cancer centres in our region. It is sometimes very hard for a cancer patient to travel long distances to take chemotherapy at the hospital. | ||
|
| ||
| 2 Access to transportation and accommodations | Access to care | |
| Description | ||
| Respondents expressed their appreciation for the transportation and accommodations that were made accessible to them during their cancer treatment. | ||
| Supporting patient quote | ||
|
||
|
| ||
| 3 Parking at the cancer centre | Access to care | |
| Description | ||
| Upon arrival to the cancer centre, patients reported a poor experience with parking services, specifically access to and cost of parking. | ||
| Supporting patient quote | ||
|
||
|
| ||
| 4 Cancer centre environment | Physical comfort | |
| Description | ||
| Once inside the cancer centre, patient responses pertained to the general cancer centre environment, the conditions of cancer centre bathrooms, the temperature of clinics and waiting areas, the quality and availability of hospital food, and the appropriateness of computers. Positive responses describe the cancer clinic atmosphere as “warm.” | ||
| Supporting patient quote | ||
|
||
|
| ||
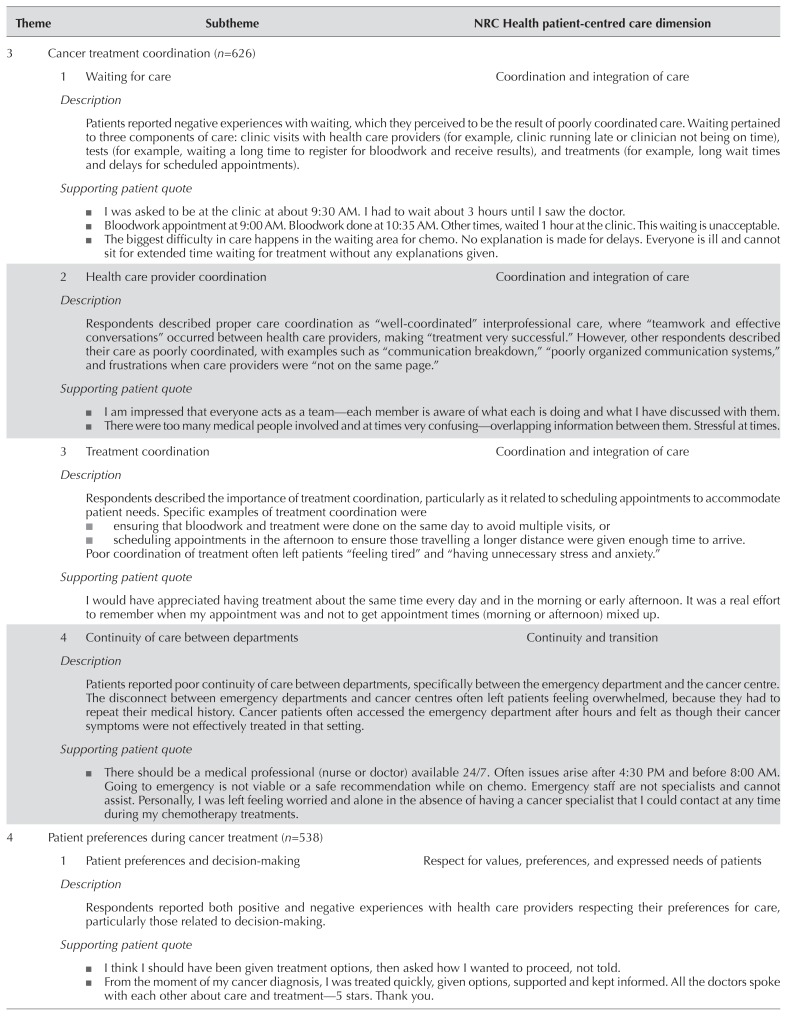
| 3 | Cancer treatment coordination (n=626) | |
| 1 Waiting for care | Coordination and integration of care | |
| Description | ||
| Patients reported negative experiences with waiting, which they perceived to be the result of poorly coordinated care. Waiting pertained to three components of care: clinic visits with health care providers (for example, clinic running late or clinician not being on time), tests (for example, waiting a long time to register for bloodwork and receive results), and treatments (for example, long wait times and delays for scheduled appointments). | ||
| Supporting patient quote | ||
|
||
|
| ||
| 2 Health care provider coordination | Coordination and integration of care | |
| Description | ||
| Respondents described proper care coordination as “well-coordinated” interprofessional care, where “teamwork and effective conversations” occurred between health care providers, making “treatment very successful.” However, other respondents described their care as poorly coordinated, with examples such as “communication breakdown,” “poorly organized communication systems,” and frustrations when care providers were “not on the same page.” | ||
| Supporting patient quote | ||
|
||
|
| ||
| 3 Treatment coordination | Coordination and integration of care | |
| Description | ||
| Respondents described the importance of treatment coordination, particularly as it related to scheduling appointments to accommodate patient needs. Specific examples of treatment coordination were | ||
|
||
| Poor coordination of treatment often left patients “feeling tired” and “having unnecessary stress and anxiety.” | ||
| Supporting patient quote | ||
| I would have appreciated having treatment about the same time every day and in the morning or early afternoon. It was a real effort to remember when my appointment was and not to get appointment times (morning or afternoon) mixed up. | ||
|
| ||
| 4 Continuity of care between departments | Continuity and transition | |
| Description | ||
| Patients reported poor continuity of care between departments, specificallybetween the emergency department and the cancer centre. The disconnect between emergency departments and cancer centres often left patients feeling overwhelmed, because they had to repeat their medical history. Cancer patients often accessed the emergency department after hours and felt as though their cancer symptoms were not effectively treated in that setting. | ||
| Supporting patient quote | ||
|
||
|
| ||
| 4 | Patient preferences during cancer treatment (n=538) | |
| 1 Patient preferences and decision-making | Respect for values, preferences, and expressed needs of patients | |
| Description | ||
| Respondents reported both positive and negative experiences with health care providers respecting their preferences for care, particularly those related to decision-making. | ||
| Supporting patient quote | ||
|
||
|
| ||
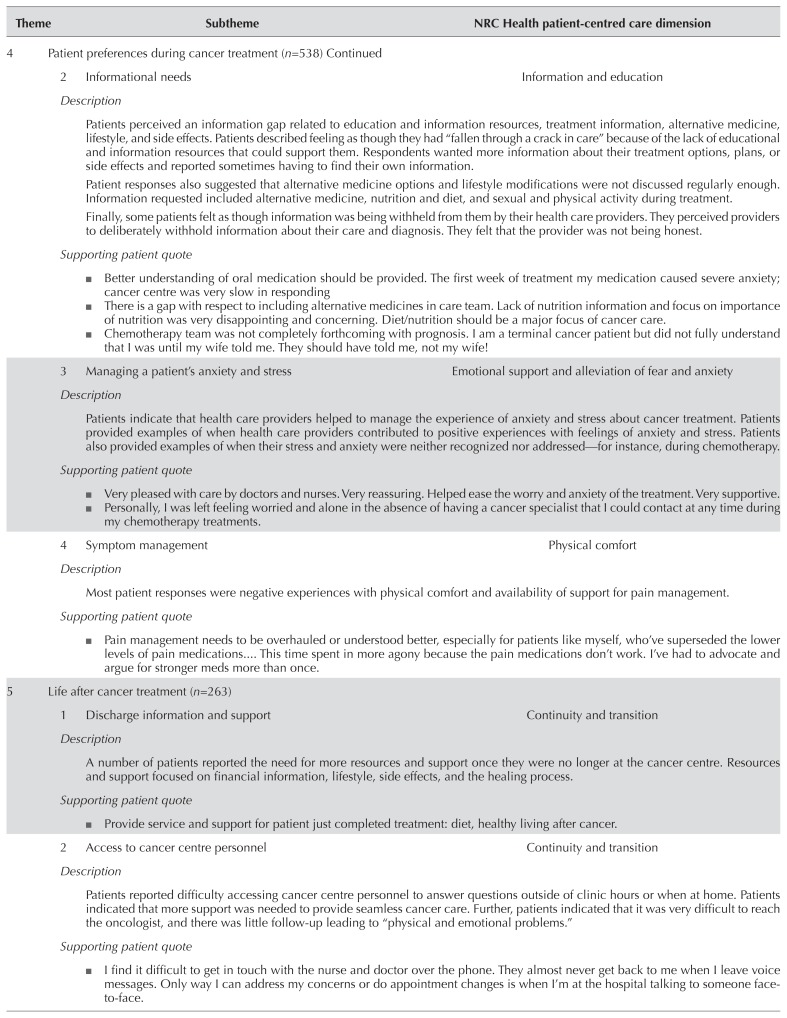
| 2 Informational needs | Information and education | |
| Description | ||
| Patients perceived an information gap related to education and information resources, treatment information, alternative medicine, lifestyle, and side effects. Patients described feeling as though they had “fallen through a crack in care” because of the lack of educational and information resources that could support them. Respondents wanted more information about their treatment options, plans, or side effects and reported sometimes having to find their own information. | ||
| Patient responses also suggested that alternative medicine options and lifestyle modifications were not discussed regularly enough. Information requested included alternative medicine, nutrition and diet, and sexual and physical activity during treatment. | ||
| Finally, some patients felt as though information was being withheld from them by their health care providers. They perceived providers to deliberately withhold information about their care and diagnosis. They felt that the provider was not being honest. | ||
| Supporting patient quote | ||
|
||
|
| ||
| 3 Managing a patient’s anxiety and stress | Emotional support and alleviation of fear and anxiety | |
| Description | ||
| Patients indicate that health care providers helped to manage the experience of anxiety and stress about cancer treatment. Patients provided examples of when health care providers contributed to positive experiences with feelings of anxiety and stress. Patients also provided examples of when their stress and anxiety were neither recognized nor addressed—for instance, during chemotherapy. | ||
| Supporting patient quote | ||
|
||
|
| ||
| 4 Symptom management | Physical comfort | |
| Description | ||
| Most patient responses were negative experiences with physical comfort and availability of support for pain management. | ||
| Supporting patient quote | ||
|
||
|
| ||
| 5 | Life after cancer treatment (n=263) | |
| 1 Discharge information and support | Continuity and transition | |
| Description | ||
| A number of patients reported the need for more resources and support once they were no longer at the cancer centre. Resources and support focused on financial information, lifestyle, side effects, and the healing process | ||
| Supporting patient quote | ||
|
||
|
| ||
| 2 Access to cancer centre personnel | Continuity and transition | |
| Description | ||
| Patients reported difficulty accessing cancer centre personnel to answer questions outside of clinic hours or when at home. Patients indicated that more support was needed to provide seamless cancer care. Further, patients indicated that it was very difficult to reach the oncologist, and there was little follow-up leading to “physical and emotional problems.” | ||
| Supporting patient quote | ||
|
||
|
| ||
| 3 Continuity of care in the community | Continuity and transition | |
| Description | ||
| Patients reported poor experiences with the continuity of care between the cancer centre and community services such as primary care and home care. Patients reported lack of information exchange between the cancer centre and their primary care doctor. Patients indicated that they often had to “repeat information multiple times” or follow up to ensure that information had been accurately shared with other care providers within the patient’s care circle. | ||
| Supporting patient quote | ||
|
||
|
| ||
| 4 Resources and support | Emotional support and alleviation of fear and anxiety | |
| Description | ||
| Respondents indicated poor experiences with resources for emotional support, as “not having someone to talk to,” “not wanting help, but needing it later in treatment,” and “not having support outside of the cancer centre.” | ||
| Supporting patient quote | ||
|
||
|
| ||
| 6 | All-encompassing patient experience of cancer care (n=1752) | |
| 1 Dignity and respect | Respect for patients’ values, preferences, and expressed needs | |
| Description | ||
| Respondents reported positive experiences with cancer care when they were treated with dignity and respect by health care providers. Respondents often described dignity and respect as “They [health care providers] treat you as a person, not as a patient.” An example of this was “talking to you using your first name.” | ||
| Supporting patient quote | ||
|
||
|
| ||
| 2 Caring, compassion, and comfort | Emotional support and alleviation of fear and anxiety | |
| Description | ||
| Patients described the experience of caring, compassion, and comfort given by health care providers during their cancer care. They acknowledged health care providers “going out of their way to help with a concern” and being “understanding and supportive” with their illness. Patients wrote that this helped to make “treatment so much easier to take” and contributed to “prolonging quality of life”. | ||
| Supporting patient quote | ||
|
||
|
| ||
| 3 Health care provider behaviour | Respect for values, preferences, and expressed needs of patients | |
| Description | ||
| Most respondents indicated that they were treated with kindness by the health care providers during cancer treatment. They described “feeling in good hands” and being “grateful for the kind and caring” health care providers in the cancer centres. Responses included examples of the professional quality of care received and the helpfulness of providers. Although many examples of nice, kind, and professional health care provider behaviours were described, there were also examples of health care providers being “rude and cold.” Patients described feeling disrespected and treated impersonally by some health care providers in the cancer centres. | ||
| Supporting patient quote | ||
|
||
|
| ||
| 4 Patient–health care provider communication | Information and education | |
| Description | ||
| In general, patients perceived the quality of communication with health care providers to be acceptable, describing health care providers as “skilled communicators” who were able to close the communication loop by “spending time” and “answering all questions.” However, some patients felt that patient–provider communication needed improvement. Patients expressed disappointment with the lack of time for discussion information or concerns. | ||
| Supporting patient quote | ||
|
||
|
| ||
| 5 Health care provider knowledge and skills | Information and education | |
| Description | ||
| Patients commented on the lack of health care provider knowledge and skills as important to the patient experience. Patients described a lack of knowledge with regard to patient questions, as well as perceptions of health care provider’s lack of expertise. | ||
| Supporting patient quote | ||
|
||
|
| ||
| 6 Inclusion of family and friends | Involvement of family and friends | |
| Description | ||
| Patient respondents describe both positive and negative experiences of family member, caregiver, and friend involvement in care. | ||
| Supporting patient quote | ||
|
||
The findings of our study showcase positive and negative experiences of patient care in the Ontario ambulatory oncology setting. Most patients reported receiving compassionate and comforting care from health care providers who were nice, kind, and professional. Those findings are consistent with previous patient experience research that highlights caring, compassionate, and comforting care as a core value of the patient experience30,31.
Poor patient experiences were most notably reported with respect to informational needs—waiting for care, and patient–health care provider communication. As in previously published studies, patients reported a gap with respect to the availability and accessibility of quality, patient-tailored information related to diagnosis and treatment, alternative medicine, lifestyle changes, and side effects32–34. A focus on improving the availability and accessibility of quality information for cancer patients can empower those patients, thus providing opportunities to engage in decision-making, leading to improved person-centred health care35.
Patients reported negative experiences with waiting in the ambulatory setting (waiting for a scheduled appointment with a health care provider or for tests or treatment), which they attributed to poor coordination of care. Coordination and continuity of care is not a new concept in health care: both aspects have been highlighted as important areas for improvement to ensure timely care for patients36,37.
Finally, patients indicated that patient–health care provider communication could be enhanced to improve the patient experience of care. Enhanced patient–health care provider communication in health care and its influence on health outcomes has increasingly been studied in recent years38. Effective patient–health care provider communication has been shown to have a positive effect on adherence to treatment recommendations and self-management of chronic disease24,38–40.
DISCUSSION
The purpose of the present study was to conduct a qualitative analysis of the aopss to examine the patient experience of ambulatory cancer care in Ontario, with the aim of gaining an in-depth understanding of the patient experience of cancer services. Using a well-established existing patient-centred care framework6, open-ended comments on the aopss from patients who were currently receiving treatment or who had received cancer treatment in the preceding 6 months underwent a qualitative content analysis.
The NRC Health patient-centred care framework provides a solid foundation for understanding the patient experience of ambulatory cancer care across the continuum of care. Nearly half the comments (49.9%) were attributed to 1 of the 8 dimensions of patient-centred care outlined in the framework (Table III). Although the results of the present study help to build on the NRC Health patient-centred care framework, they also offer a different perspective of the experience of cancer patients in the identification of new subthemes outside the scope of the NRC Health framework.
For instance, Coronado and colleagues41 examined the experience of patients with cancer during the diagnosis and treatment planning phases, and indicated that 92% of respondents felt that their care provider told them of their cancer diagnosis in a sensitive manner. Contrary to those findings, respondents in the present study indicated that health care providers lacked sensitivity in delivering the cancer diagnosis. Patients reported “being told over the phone,” or “having [to] drive home afterwards,” or “not having a family member present.” The latter findings are similar to those from the Wales Cancer Patient Experience Survey, the U.K. National Cancer Patient Experience Survey, and the Scottish Cancer Patient Experience Survey42–44. Not surprisingly, patients in the present study and others42–44 often report that caring, compassion, and comfort provided by health care providers during their cancer was of utmost importance to them, praising those providers for “going out of their way to help with a concern” and “being understanding and supportive.” Those findings support patient concerns about the lack of emotional support resources available and the need for improvements in patient–health care provider communication during clinical encounters. Making such improvements might build additional rapport and trust between patients and health care providers, not only instilling patient confidence in their health care provider’s knowledge and skills, but also in the system.
Although the “continuity and transition” dimension outlines responsibilities of the health care provider to ensure continuity and transition for the patient, it fails to include inter- or intra-organization continuity and communication. For instance, patients in the present study reported poor intra-organization continuity between departments—specifically, between the emergency department and the cancer centre, with patients often being left feeling “disconnected” and “overwhelmed.” The inter-organizational continuity and communication showed similar characteristics, with a reported lack of communication between the cancer centres and community services such as primary and home care, with the patient having to “repeat information multiple times.” For that reason, it is not surprising that patients reported attempting to contact the cancer centre. However, such efforts were met with difficulty in accessing cancer centre personnel who could respond to the questions and inquiries. That finding is similar to results from the Wales Cancer Patient Experience Survey, the U.K. National Cancer Patient Experience Survey, and the Scottish Cancer Patient Experience Survey42–44.
When examining new subthemes related to “coordination and integration” of care, patients reported a negative experience waiting for cancer care services within the outpatient clinics. Although complaints concerning wait times for cancer care and even health care in general are not new21,42–44, the NRC Health framework does not include waits as a subdimension. In the present study, patients reported 3 main wait time components relating to the clinic environment (as opposed to the full continuum of care):
■ Waiting for health care providers
■ Waiting for tests
■ Waiting for treatment
Improvements within those areas should be considered in future research. Furthermore, patients expressed certain preferences for health care provider coordination in terms of “always seeing the same health care professional” and “ensuring that tests and treatment [are] scheduled on the same day” (or on a day and at a time of their choosing) as being important to their experience. Considering patient preferences in terms of coordination and integration of cancer care is therefore important.
Finally, patients reported extremely poor experiences related to parking. Although parking complaints are not uncommon in the health care literature and are often cited as a barrier to a positive patient experience42–44, the NRC Health framework does not include access to parking within the “access to care” dimension. Access to parking might sometimes seem irrelevant in comparison with larger issues such as emotional health and support for patients, but respondents in the present study reported stress and anxiety related not only to accessing a parking spot, but also to the cost and their inability to pay. Those sentiments are consistent with the prior literature42–44. Drawing attention to that finding (in terms of ensuring the provision of equitable cancer services) is important, and seeking solutions to improve this equity gap is encouraged.
Limitations
The main limitation of the present study is its use of aopss to collect qualitative data. The aopss shares several limitations common to surveys, including its retrospective nature, the potential for recall bias, and the length of the survey (105 items). Further, coverage error can also be a problem, given that patients are required to respond in writing (in either English or French). Patients who do not speak either language or who cannot not express their experience in written form are therefore unable to respond. Table II provides an overview of the demographic characteristics of the respondents. Because of missing data, some categories could be overrepresented or underrepresented. Generalization of the findings from the present study to all recipients of cancer care can therefore not be inferred. The findings could be strengthened by understanding more about the demographics of patients who completed the open-ended questions. Future research should be conducted with that metric in mind, in an attempt to address that gap.
The deductive data analysis approach using the NRC Health patient-centred care framework was advantageous in that it allowed us to examine pre-established patient experience concepts with cancer patients undergoing treatment in the ambulatory setting. However, a major limitation to using a deductive approach to data analysis is that the themes and subthemes are not developed inductively based on the data, and therefore only the content that fits the context of the framework can be chosen from the data, which is a limitation of the present study.
CONCLUSIONS
Our research holds implications for both the individual and the system levels of ambulatory cancer care. The present study is unique in that it used a large qualitative dataset from a provincial survey of patients and their families to describe the components of care that are most important to them. Using that approach, we were able to examine the experience of cancer care from a patient perspective across the continuum of care, with patients outlining their needs, wants, and preferences. Our examination of those dimensions will help to ensure that improvements are driven by a patient-first approach.
At the system level, the results of the study provide an in-depth understanding of the patient experience of ambulatory cancer care and treatment in Ontario. That feedback will in turn help to tailor quality improvement initiatives. Specifically, the results of the present study identify facilitators and barriers to the patient experience from the patient perspective and identify actionable opportunities to improve the patient experience of ambulatory cancer treatment in Ontario. For example:
■ Improving patient–health care provider communication, especially during diagnosis
■ Ensuring timely and coordinated care in the cancer centres, through a better understanding of wait times
■ Improving continuity and transition intra- and inter-organizationally
■ Examining parking from an equity lens
Consultations and working groups with patient and family advisors are ongoing to help develop quality improvement initiatives related to those actionable opportunities.
Finally, in terms of defining the patient experience, the NRC Health patient-centred care framework provides a foundation for understanding the general patient experience of care. However, evidence from the present study and others42–44 suggests that cancer patients often encounter unique challenges related to the patient experience20. Those observations contribute to this research area. We therefore encourage researchers and health care administrators to look beyond general patient-centred care frameworks and to examine specific issues of importance to their patient populations.
ACKNOWLEDGMENTS
This research was conducted with the support of Cancer Care Ontario (cco) through funding provided by the Ontario Ministry of Health and Long-Term Care. The opinions, results, views, and conclusions reported in this publication are those of the authors and do not necessarily reflect those of cco. No endorsement by cco is intended or should be inferred.
Footnotes
CONFLICT OF INTEREST DISCLOSURES
We have read and understood Current Oncology’s policy on disclosing conflicts of interest, and we declare that we have none.
REFERENCES
- 1.de Silva D. Measuring Patient Experience. London, U.K: The Health Foundation; 2013. [Google Scholar]
- 2.Klazinga N, Fischer C, ten Asbroek A. Health services research related to performance indicators and benchmarking in Europe. J Health Serv Res Policy. 2011;12(suppl 2):38–47. doi: 10.1258/jhsrp.2011.011042. [DOI] [PubMed] [Google Scholar]
- 3.Canadian Institute for Health Information (cihi) Patient Experience [Web resource] Ottawa, ON: cihi; n.d.. [Available at: https://www.cihi.ca/en/patient-experience; cited 8 May 2018] [Google Scholar]
- 4.Balik B. What makes a positive patient experience? Patient Saf Monit J. 2011;12:1–5. [Google Scholar]
- 5.Zimlichman E, Rozenblum R, Millenson ML. The road to patient experience of care measurement: lessons from the United States. Isr J Policy Health Res. 2013;2:35. doi: 10.1186/2045-4015-2-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.NCR Health. Eight Dimensions of Patient Centred Care. Boston, MA: NRC Health; 2008. [Google Scholar]
- 7.The Beryl Institute. Nashville, TN: The Beryl Institute; n.d.. Defining Patient Experience [Web page] [Available at: http://www.theberylinstitute.org/?page=definingpatientexp; cited 8 May 2018] [Google Scholar]
- 8.Agency for Healthcare Research and Quality (ahrq) CAHPS Hospital Survey [Web page] Rockville, MD: ahrq; 2018. [Avai lable at: https://www.ahrq.gov/cahps/surveysguidance/hospital/index.html; cited 8 May 2018. [Google Scholar]
- 9.Health Quality Ontario. Primary Care Patient Experience Survey: Support Guide. Toronto, ON: Health Quality Ontario; 2015. [Available online at: http://www.hqontario.ca/Portals/0/documents/qi/primary-care/primary-care-patientexperience-survey-support-guide-en.pdf; cited 8 May 2018] [Google Scholar]
- 10.Foot C, Fitzsimons B. The policy and practice of measuring patient experience. Nurs Manag (Harrow) 2011;18:18–19. doi: 10.7748/nm2011.06.18.3.18.c8535. [DOI] [PubMed] [Google Scholar]
- 11.Delnoij DM. Measuring patient experiences in Europe: what can we learn from the experiences in the USA and England. Eur J Pub Health. 2009;19:354–6. doi: 10.1093/eurpub/ckp105. [DOI] [PubMed] [Google Scholar]
- 12.Pettersen KI, Veenstra M, Guldvog B, Kolstad A. The Patient Experience Questionnaire: development, validity and reliability. Int J for Qual Health Care. 2004;16:453–63. doi: 10.1093/intqhc/mzh074. [DOI] [PubMed] [Google Scholar]
- 13.Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2012-001570. pii:e001570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaplan SH, Greenfield S, Ware JE., Jr Assessing the effects of physician–patient interactions on the outcomes of chronic disease. Med Care. 1989;27(suppl):S110–27. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- 15.Kahn KL, Schneider EC, Malin JL, Adams JL, Epstein AM. Patient centered experiences in breast cancer: predicting longterm adherence to tamoxifen use. Med Care. 2007;45:431–9. doi: 10.1097/01.mlr.0000257193.10760.7f. [DOI] [PubMed] [Google Scholar]
- 16.Schoenthaler A, Chaplin WF, Allegrante JP, et al. Provider communication effects medication adherence in hypertensive African Americans. Patient Ed Couns. 2009;75:185–91. doi: 10.1016/j.pec.2008.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008:CD000011. doi: 10.1002/14651858.CD000011.pub3. [DOI] [PubMed] [Google Scholar]
- 18.Carcaise-Edinboro P, Bradley CJ. Inf luence of patient–provider communication on colorectal cancer screening. Med Care. 2008;46:738–45. doi: 10.1097/MLR.0b013e318178935a. [DOI] [PubMed] [Google Scholar]
- 19.Weldring T, Smith S. Patient-reported outcomes (pros) and patient-reported outcome measures (proms) Health Serv Insight. 2013;6:61–8. doi: 10.4137/HSI.S11093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pelzang R. Time to learn: understanding patient-centred care. Br J Nurs. 2010;19:912–17. doi: 10.12968/bjon.2010.19.14.49050. [DOI] [PubMed] [Google Scholar]
- 21.Black G, Sheringham J, Spencer-Hughes V, et al. Patients’ experiences of cancer diagnosis as a result of an emergency presentation: a qualitative study. Plos One. 2015;10:e0135027. doi: 10.1371/journal.pone.0135027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lipczak H, Dorflinger LH, Enevoldsen C, Vinter MM, Knudsen JL. Cancer patients’ experiences of error and consequences during diagnosis and treatment. PXJ. 2015;2:102–10. [Google Scholar]
- 23.Beach MC, Inui T on behalf of the Relationship-Centered Care Research Network. Relationship-centered care. A constructive reframing. J Gen Intern Med. 2006;21(suppl 1):S3–8. doi: 10.1111/j.1525-1497.2006.00302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stewart MA. Effective physician–patient communication and health outcomes: a review. CMAJ. 1995;152:1423–33. [PMC free article] [PubMed] [Google Scholar]
- 25.LaVela SL, Gallan AS. Evaluation and measurement of patient experience. PJX. 2014;1:28–36. [Google Scholar]
- 26.Edwards A, Evans R, White P, Elwyn G. Experiencing patient-experience surveys: a qualitative study of the accounts of gps. Br J Gen Pract. 2011;61:157–66. doi: 10.3399/bjgp11X567072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cancer Quality Council of Ontario. Person-centred care and patient experience with outpatient cancer care [Web page] Toronto, ON: Cancer Care Ontario; 2018. [Available at: https://www.csqi.on.ca/indicators/person-centred-care-patientexperience-outpatient-cancer-care; cited 8 May 2018] [Google Scholar]
- 28.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–88. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 29.Ezzy D. Qualitative Analysis: Practices and Innovation. London, U.K: Routledge; 2002. [Google Scholar]
- 30.MacKean GL, Thurston WE, Scott CM. Bridging the divide between families and health professionals’ perspectives on family-centred care. Health Expect. 2005;8:74–85. doi: 10.1111/j.1369-7625.2005.00319.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Drach-Zahavy A. Patient-centred care and nurses’ health: the role of nurses’ caring orientation. J Adv Nurs. 2009;65:1463–74. doi: 10.1111/j.1365-2648.2009.05016.x. [DOI] [PubMed] [Google Scholar]
- 32.Rutten LJ, Arora NK, Bakos AD, Aziz N, Rowland J. Information needs and sources of information among cancer patients: a systematic review of research (1980–2003) Patient Educ Couns. 2005;57:250–61. doi: 10.1016/j.pec.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 33.Boltong A, Byrnes M, McKiernan S, Quin N, Chapman K. Exploring the preferences, perceptions and satisfaction of people seeking cancer information and support: implications for the Cancer Council Helpline. Australian Journal of Cancer Nursing. 2015;16:20–2. 24–8. [Google Scholar]
- 34.Matsuyama RK, Kuhn LA, Molisani A, Wilson-Genderson MC. Cancer patients’ information needs the first nine months after diagnosis. Patient Educ Couns. 2013;90:96–102. doi: 10.1016/j.pec.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 35.Cancer Care Ontario (cco) Person-Centred Care Guideline. Toronto, ON: cco; 2015. [Downloadable from: https://www.cancercareontario.ca/en/guidelines-advice/types-of-cancer/38631; cited 8 May 2018] [Google Scholar]
- 36.Matthews M, Ryan D, Bulman D. What does satisfaction with wait times mean to cancer patients? BMC Cancer. 2015;15:1017. doi: 10.1186/s12885-015-2041-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Matthews M, Ryan D, Bullman D. Patient-expressed perceptions of wait-time causes and wait-related satisfaction. Curr Oncol. 2015;22:105–12. doi: 10.3747/co.22.2243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Street RL, Makoul G, Arora NK, Epstein RM. How does communication heal? Pathways linking clinician–patient communication to health outcomes. Patient Educ Couns. 2009;74:295–301. doi: 10.1016/j.pec.2008.11.015. [DOI] [PubMed] [Google Scholar]
- 39.McCabe C. Nurse–patient communication: an exploration of patients’ experiences. J Clin Nurs. 2004;13:41–9. doi: 10.1111/j.1365-2702.2004.00817.x. [DOI] [PubMed] [Google Scholar]
- 40.Levinson W, Lesser CS, Epstein RM. Developing physician communication skills for patient-centered care. Health Aff (Millwood) 2010;29:1310–18. doi: 10.1377/hlthaff.2009.0450. [DOI] [PubMed] [Google Scholar]
- 41.Coronado AC, Tran K, Chadder J, et al. on behalf of the System Performance Steering Committee and the Technical Working Group. The experience of patients with cancer during diagnosis and treatment planning: a descriptive study of Canadian survey results. Curr Oncol. 2017;24:332–7. doi: 10.3747/co.24.3782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cunningham M, Wells M. Qualitative analysis of 6961 free-text comments from the first National Cancer Patient Experience Survey in Scotland. BMJ Open. 2017;7:e015726. doi: 10.1136/bmjopen-2016-015726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bracher M, Corner DJ, Wagland R. Exploring experiences of cancer care in Wales: a thematic analysis of free-text responses to the 2013 Wales Cancer Patient Experience Survey (wcpes) BMJ Open. 2016;6:e011830. doi: 10.1136/bmjopen-2016-011830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wiseman T, Lucas G, Sangha A, et al. Insights into the experiences of patients with cancer in London: framework analysis of free-text data from the National Cancer Patient Experience Survey 2012/2013 from the two London Integrated Cancer Systems. BMJ Open. 2015;5:e007792. doi: 10.1136/bmjopen-2015-007792. [DOI] [PMC free article] [PubMed] [Google Scholar]