Abstract
Objectives:
Nonalcoholic fatty liver disease (NAFLD) is a very common liver disorder in Western countries. As of late, it has been found to be prevalent in Asia as well. It is a benign disease unless it develops into necroinflammation and fibrosis. This study was proposed to determine the prevalence and risk factors of sonography-detected NAFLD among Malaysian adults in Klang Valley, West Malaysia.
Study design:
An observational cross-sectional study.
Methods:
The participants were aged between 45 and 75 years who participated in a screening program at the Golden Horses Health Sanctuary in Klang Valley. Lipid profile and anthropometric measurements were collected from the subjects’ medical records. Ultrasound machine and a structured self-administered questionnaire were used as instruments for recruiting data from the subjects. The subjects who consumed alcohol (>140 g/wk for men and >70 g/wk for females), had hepatitis B or C viruses, liver insults, and surgery, and taken lipid-lowering medications were excluded from the study.
Results:
A total of 628 subjects were analyzed, and 235 (37.4%) subjects were diagnosed with definite NAFLD. They comprised 518 (82.5%) Chinese, 92 (14.6%) Malays, and 18 (2.9%) Indians. Peak prevalence of NAFLD was found in 53 to 60 years age group. The higher prevalence of NAFLD was among men (48.3%) than women (27.3%) and among Indians (61.1%) and Malays (51.1%) than among Chinese (34.2%). NAFLD has been found to be strongly correlated with male sex, high body mass index (≥23.0 kg/m2), hypertriglyceridemia, low high-density lipoprotein cholesterol, diabetes mellitus, and hypertension.
Conclusion:
NAFLD is quite common among adults in Malaysian urban population. The prevalence of NAFLD was inordinately high among the 53 to 60 years age group, male sex, Indians, and Malays (as compared with Chinese). Age >60 years, male sex, high body mass index (≥23.0 kg/m2), hypertriglyceridemia, and diabetes mellitus were proven to be risk predictors for NAFLD.
Keywords: Malaysia, nonalcoholic fatty liver disease, risk factors, sonography
Introduction
Nonalcoholic fatty liver disease (NAFLD) is known to be a very common cause of chronic liver disease worldwide and has been recognized as a main health problem.1–3 It has been identifies as the most prevalent liver disorder in Western countries and affects 20% to 40% of the general population.2,4,5 In Asia, it was initially thought to be uncommon but it has grown rapidly with prevalence of up to 30% of the general population.6,7 In Western countries, estimated prevalence of NAFLD about a decade ago in Italy and USA was 25% and 34%, respectively.8,9 In Malaysia, where prevalence of diabetes mellitus (DM), overweight and obesity has been reported to be on the increase, NAFLD would be a common disorder in this country as well.10 Simple hepatic steatosis is still considered a benign disease unless it evolves into inflammation and fibrosis.11 Kim et al12 indicated that NAFLD is not only a risk factor for chronic liver disease but is also considered an independent risk factor for developing cardiovascular disease (CVD). Histologically, NAFLD disease is evidenced by accumulation of fat in hepatocyte >5% of the wet liver weight without alcohol consumed.13,14 NAFLD changes are similar to those changes that are seen in alcoholic fatty liver disease but without a history of alcohol consumption.15 NAFLD is a spectrum of conditions ranging from a simple steatosis (without inflammation or fibrosis) to nonalcoholic steatohepatitis (NASH), which refers to steatosis with necroinflammatory that results to fibrosis, cirrhosis (liver cell scaring), and hepatocellular carcinoma.1,16–18
Ultrasound is widely used for detecting fatty liver changes as it is a noninvasive tool, available, safe, and relatively inexpensive in comparison with other imaging modalities such as computed tomography, magnetic resonance imaging, and proton magnetic resonance spectroscopy.19 However, liver biopsy still represents the criterion standard tool for the diagnosis of NAFLD and it can distinguish between NAFLD and its forms such as NASH and fibrosis.20 In the present study, we endeavored to identify prevalence and risk factors of sonography-diagnosed NAFLD among adults of urban Malaysian community.
Methods
Subjects
A cross-sectional observational study was carried out prospectively among subjects with age ranges between 45 and 75 years, who underwent a screening program for the period from August 15, 2015 to January 15, 2016 at the Golden Horses Health Sanctuary located in Seri Kembangan, Klang Valley, Malaysia. This center serves medical screening health programs and checkups for subjects who live in this area. The majority of the subjects who attend this center belong to the major races in Malaysia, which are Malays, Chinese, and Indians. Medical checkups carried out in this center include consultation with blood tests such as lipid profile, liver and renal function tests, physical examination, abdominal and breast ultrasonography, and computed tomography scanning. The ethical approval for this study was obtained from JKEUPM (Ethic Committee for Research Involving Human Subject).
In this study, respondents’ demographic data and alcoholic intake habits were recorded. However, lipid profile data were collected based on subjects’ medical records. The patients who had excessive fat infiltration in the liver and consumed alcohol <140 g/week for men and <70 g/week for women were classified as having NAFLD.21 Subjects with hepatitis B or C viruses, liver insults, and surgery, and those who had taken lipid-lowering medications were excluded from the study. Patients under diabetes and hypertensive medications were considered infected with diabetes and hypertension.
Biochemical and anthropometric measurements of metabolic risk factors
Lipid profile levels are defined based on the National Cholesterol Education Program, Adults Treatment Panel III (2002),22 as follows:
High-density lipoprotein cholesterol (HDL-C) <1.04 mmol/L for men and <1.30 mmol/L for women are considered reduced.
Triglyceride (TG) ≥1.70 mmol/L is considered elevated.
Total cholesterol (TC) ≥5.17 mmol/L is considered high.
Low-density lipoprotein cholesterol (LDL-C) ≥2.59 mmol/L is considered high.
Furthermore, overweight, obese, and severe obese as well as high waist-to-hip ratio (WHR) are defined based on WHO guidelines23 for Asia-Pacific region as follows:
0–22.9 kg/m2 for normal
23.0–24.9 kg/m2 for overweight
25.0–29.9 kg/m2 for obese
≥30.0 kg/m2 for severe obese
WHR >0.90 for men is considered substantially increased.
WHR > 0.85 for women is considered substantially increased.
Ultrasound screening for fatty liver disease
Ultrasound machine (Philips medium range/HD 15) equipped with 3.5 MHz probe was used for screening subjects in this study. Ultrasound examination was achieved on each subject by radiologists with experience >10 years. NAFLD was detected on the basis of 2 of the following criteria: increasing liver echogenicity (bright liver) as compared with the right renal cortex and spleen, loss visualization of intrahepatic vascular walls, and impaired visualization of diaphragm and posterior portion of the right liver lobe.21
The demographic data, social history data (including alcohol consumption and pregnancy), medication history intake (including chemotherapy, radiotherapy, corticosteroids, anticholesterol medications) and herbal products, and liver diagnosis history were collected based on a structured self-administered questionnaire. The anthropometric measurements including body mass index (BMI) and WHR, lipid profile test including TC, TG, HDL-C, and LDL-C and medical history of diseases (including DM and hypertension) were collected from patients’ medical records and were set as secondary data. Subjects were asked to sign consent form before starting to fill up the questionnaire.
Statistical analysis
Data were analyzed with Statistical Package for the Social Sciences program version 22.0. Characteristics of the study population were obtained using descriptive statistics in which proportions and frequencies were carried out for categorical variables, whereas mean ± standard deviation was carried out for continuous variables. Association between categorical variables was conducted using Chi square test. P value <.05 was considered significant. The strength of association in the presence of particular factors was expressed as odds ratio (OR) with 95% confidence intervals (CIs). P value <.20 on univariate analysis was subjected to multiple logistic regression analysis.
Results
Subjects’ characteristics
The characteristics of the study participants are presented in Table 1. A total of 628 subjects were involved. The mean age of participants was 54.54 ± 6.69 years. When subanalysis for age was done, it revealed that mean age of men was 55.59 ± 6.91, whereas mean age of women was 53.57 ± 6.31 years. Our study population was predominantly woman (51.9%) and overwhelmingly Chinese (82.5%) in race. In light of this, the greatest proportion of BMI was for obese (36.5%) followed by normal (35.2%) and overweight (20.2%), whereas severe obese was the lowest (8.1%).
Table 1.
The characteristics of study population (n = 628)
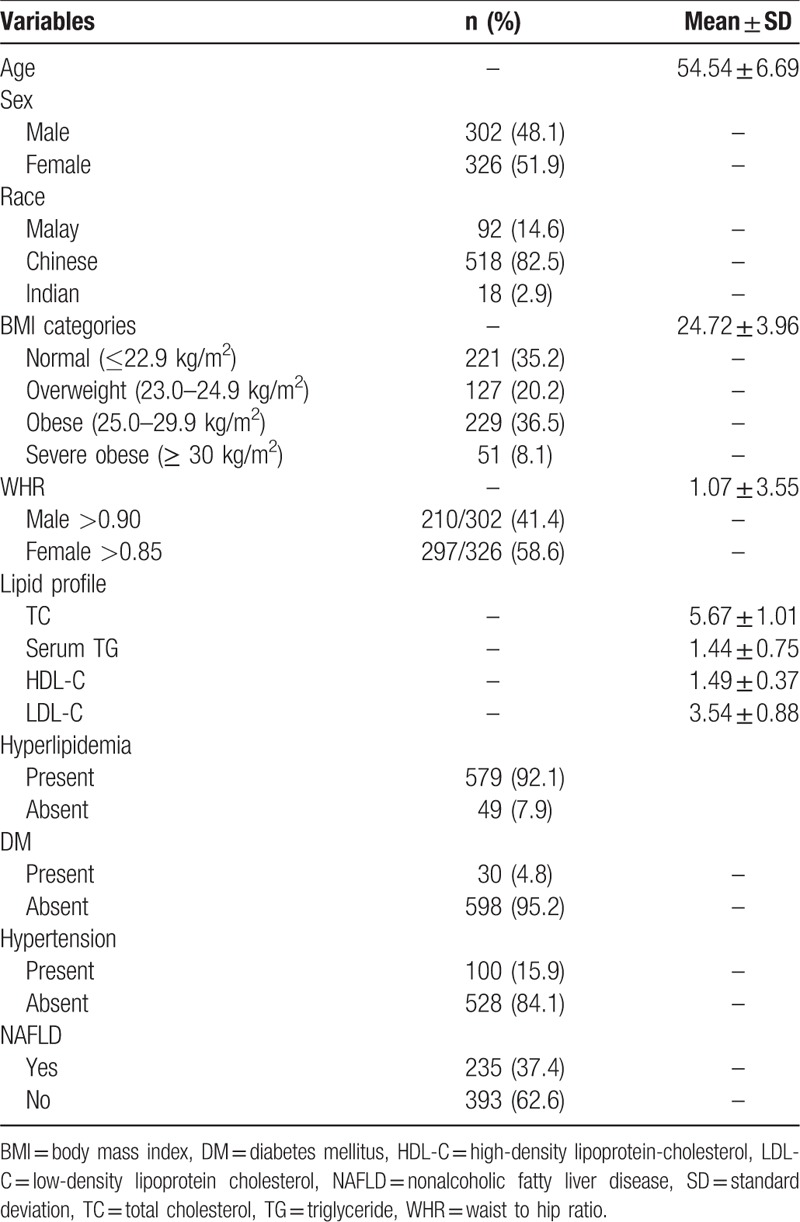
The lipid profile characteristics were as follows: 5.67 ± 1.01 mmol/L for TC, 1.44 ± 0.75 mmol/L for TG, 1.49 ± 0.37 mmol/L for HDL-C, and 3.54 ± 0.88 mmol/L for LDL-C. More specifically, 92.1% of study population was having hyperlipidemia. For the medical history of diseases, there were only 4.8% and 15.9% of subjects as having DM and hypertension, respectively.
Overall prevalence of NAFLD
Among the 628 subjects, 235 subjects were diagnosed with definite NAFLD, indicating that the prevalence of NAFLD was 37.4% among urban Malaysian adults in Klang Valley.
Demographic factors, anthropometric, lipid profile, and medical history of diseases correlates of NAFLD
Table 2 provides the demographic data and their correlation with the prevalence of NAFLD. The prevalence of NAFLD was the highest among patients with age ranging from 53 to 60 years (43.8%) as compared with other age groups. Also, it could be seen that prevalence of NAFLD was gradually increased with age advances from 45 to 60 years old (34.8%–43.8%) and then it declines over the age of 60 years (32.7%–16.7%). This indicated that prevalence of NAFLD had a significant association with age (x2 = 9.257, df = 3, P = .026).
Table 2.
Association of age groups, sex, and races with nonalcoholic fatty liver disease (n = 628)
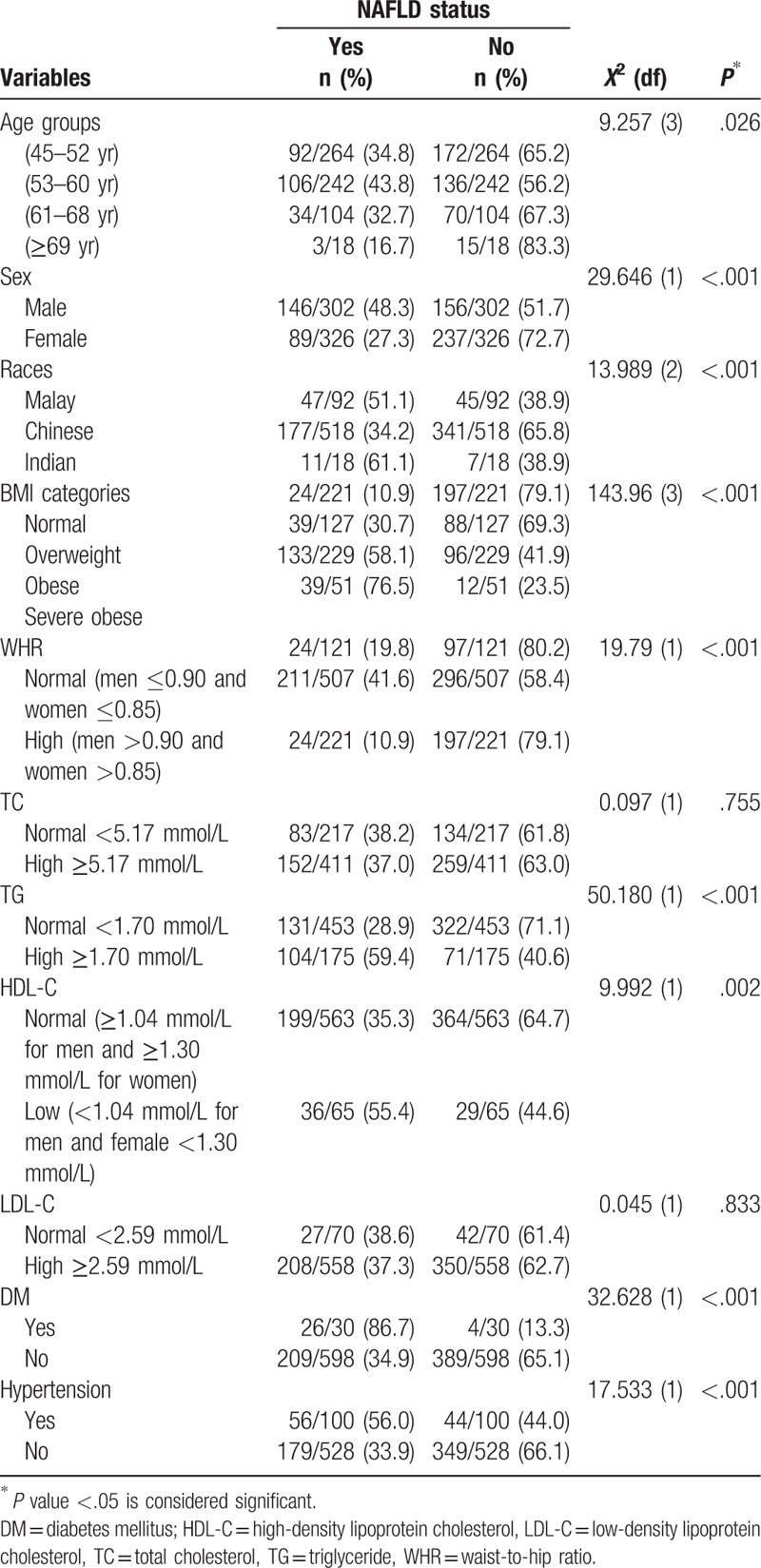
In the same manner, the prevalence of NAFLD was considerably higher in men (48.3%) than in women (27.3%) (x2 = 29.646, df = 1, P < .001). Likewise, the highest prevalence of NAFLD was among Indians (61.1%) followed by Malays (51.1%), whereas Chinese participants were the lowest (34.2%), indicating that there was significant association between prevalence of NAFLD and ethnic groups (x2 = 13.989, df = 2, P < .001). When further subanalysis of the race data was done, the differences between Malay versus Chinese and Chinese versus Indian were statistically significant (P = .002 and P = .019, respectively), wheras the differences between Indian versus Malay was not statistically significant (P = .436).
Furthermore, there was statistically significant association between NAFLD and BMI (x2 = 143.96, df = 3, P = < .001). Obviously, prevalence of NAFLD was the highest among severe obese subjects followed by obese, overweight, and normal subjects (76.5%, 58.1%, 30.7%, and 10.9%, respectively). Similarly, the prevalence of NAFLD was significantly higher in high WHR (41.6%) than in normal (19.8%) (x2 = 19.79, df = 1, P = < .001).
Our results also revealed that prevalence of NAFLD among patients with high TC level was 37.0% versus normal TC of 38.2%. As such, the prevalence of NAFLD was 37.3% among patients with high LDL-C and 38.6% among those with normal LDL-C. This indicates that the association between NAFLD versus TC and NAFLD versus LDL-C was not statistically significant (x2 = 0.097, df = 1, P = .755 and x2 = 0.045, df = 1, P = .833, respectively). On the contrary, subjects with NAFLD were found to have significant hypertriglyceridemia (59.4%) compared to those with normal TG (28.9%) (x2 = 50.180, df = 1, P < .001). Similarly, there was significantly higher prevalence of NAFLD in patients with low HDL-C (55.4%) than in those with normal HDL-C (35.3%) (x2 = 9.992, df = 1, P = .002).
Of equal importance, the prevalence of NAFLD was noted to be greater in subjects with DM (86.7%) than in subjects without DM (34.9%). Similarly, there was higher prevalence of NAFLD among subjects with hypertension (56.0%) than those without hypertension (33.9%). Hence, it could be seen that DM and hypertension were significantly associated with NAFLD (x2 = 32.628, df = 1, P < .001, x2 = 17.533, df = 1, P < .001, respectively).
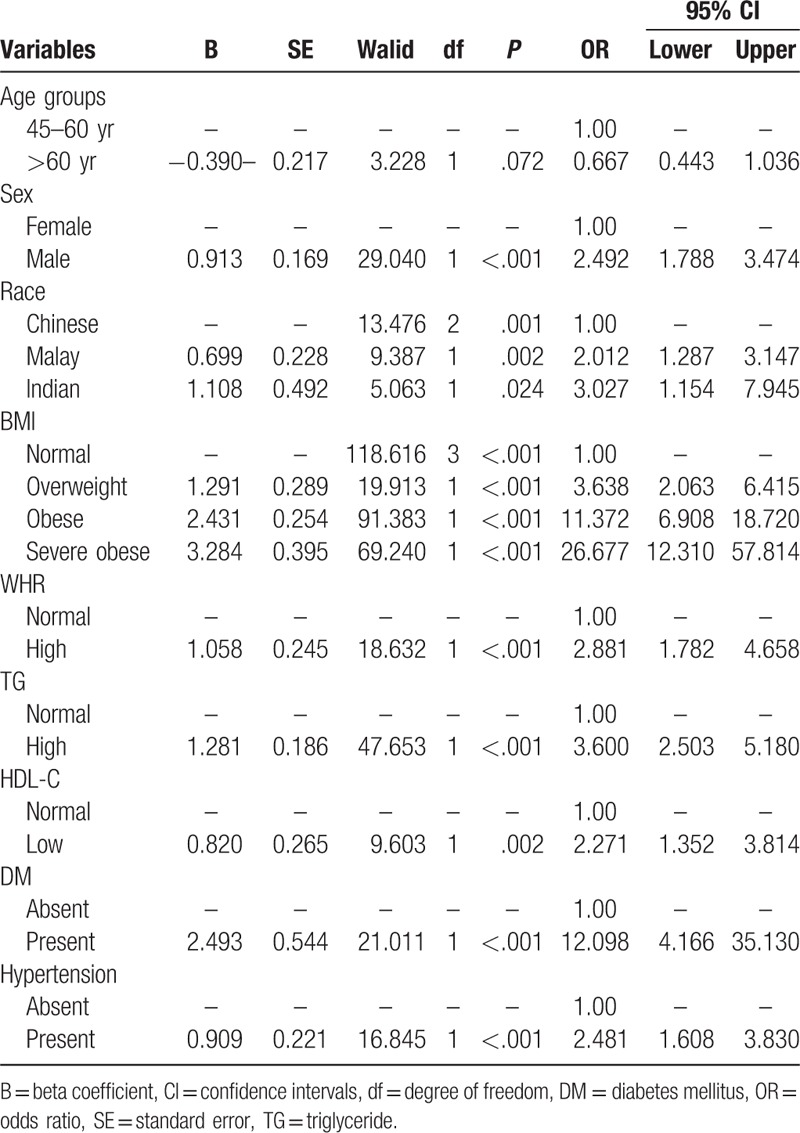
OR with 95% CI was adjusted for the following variables to determine the presence of NAFLD: those aged >60 years, Malays and Indians versus Chinese, male sex, overweight, obese, severely obese versus normal BMI, high WHR, high TG, low HDL-C, DM, and hypertension (Table 3). The findings of univariate analysis are presented in Table 3 with age >60 years, female sex, Malays and Indians (vs Chinese), overweight, obese and severely obese, high WHR, hypertriglyceridemia, low HDL-C, DM, and hypertension as having strongly significant association with NAFLD.
Table 3.
Risk predictors associated with nonalcoholic fatty liver disease using univariate analysis with odds ratio and 95% confidence intervals
Risk predictors for NAFLD
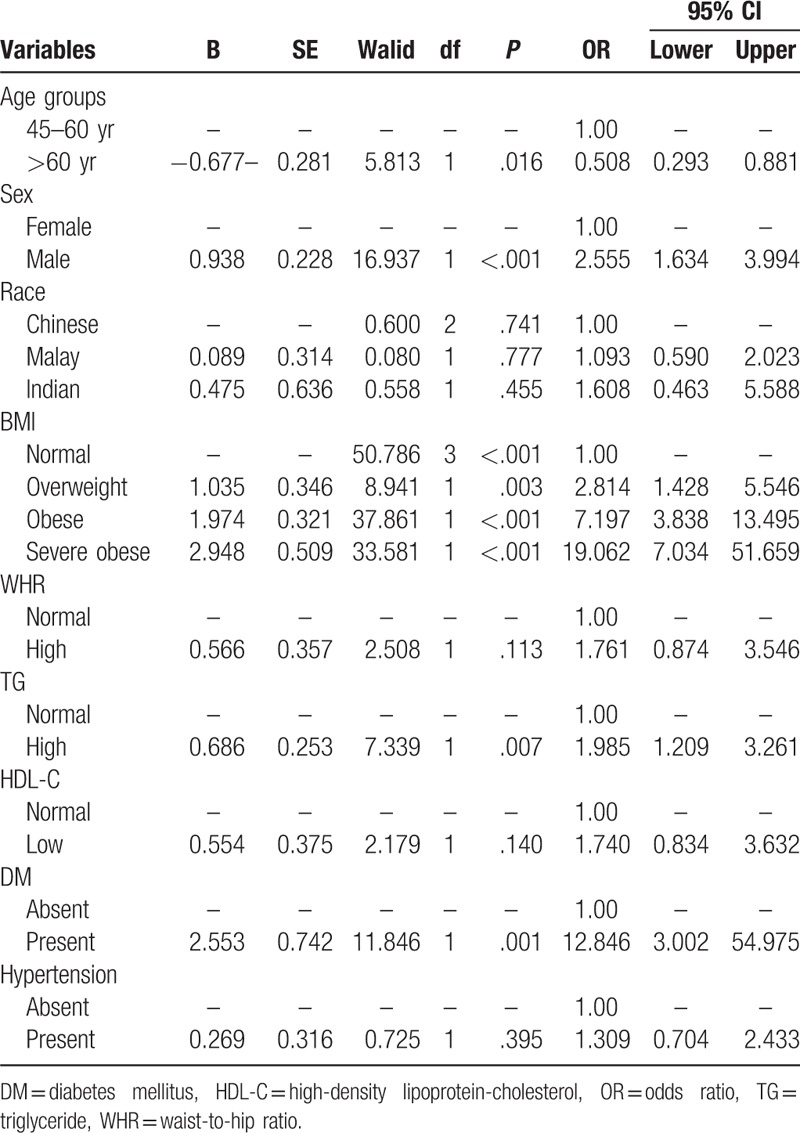
On multivariate analysis using multiple logistic regression analysis (Table 4), the results showed that subjects aged >60 years were significantly less likely to have NAFLD as compared with those in the age group from 45 to 60 years (P = .007, OR = 1.985, 95% CI = 1.209–3.261). As such, the following variables were found to be risk predictive factors for developing NAFLD: male sex (P ≤ .001, OR = 2.555, 95% CI = 1.634–3.994), overweight (P = .003, OR = 2.814, 95% CI = 1.428–5.546), obese (P ≤ .001, OR = 7.197, 95% CI = 3.838–13.495), severe obese (P ≤ .001, OR = 19.062, 95% CI = 7.034–51.659), hypertriglyceridemia (P = .007, OR = 1.985, 95% CI = 1.209–3.261), and DM (P = .001, OR = 12.846, 95% CI = 3.002–54.975). However, Malays and Indians, high WHR, low HDL-C, and hypertension were not revealed to be independent significant factors for NAFLD.
Table 4.
Multivariate analysis of risk predictors for nonalcoholic fatty liver disease using multiple logistic regression analysis
Discussion
NAFLD is very common cause of chronic liver disease in Western countries,24–26 with affecting ranges between 20% and 40% of general population.2,4 However, in Asia the prevalence of NAFLD has been reported to be from 12% to 37% among the general population.15,27–30 A histopathological picture of NAFLD shows a wide spectrum ranging from simple steatosis to NASH that leads to fibrosis, cirrhosis, and liver cancer.1,16–18 In the present study, we endeavored to investigate the prevalence and risk factors of NAFLD in the urban Malaysian population.
The prevalence of NAFLD among our study population has been estimated to be 37.4%, whereas 22.7% prevalence of NAFLD has been reported in a previous cross-sectional survey conducted in Petaling Jaya, also located in the Klang Valley, Malaysia.10 Our results revealed that prevalence of NAFLD had a significant correlation with age and it was also significantly higher in men than in women. In both sex, the prevalence of NAFLD was progressively increased with age advances even after reaching the highest peak between ages 52 and 60 years and then it declined over 60 years. This result is consistent with results obtained by Fan et al31 and Cheng et al32 which reported that prevalence of NAFLD was significantly increased with advancing age even after touching the highest point between ages 60 and 69 years, then it started to decline after 70 years of age. On the contrary, Almobarak et al16 confirmed that rates of NAFLD decreased with age increases and was higher in women than in men. Nevertheless, Ahmed et al25 documented an equal effect of prevalence of NAFLD between men and women.
We were particularly concerned about the need to determine whether there was association between prevalence of NAFLD and ethnicity in the urban multiracial Malaysian population. Overall, our study reported that prevalence of NAFLD had a significant association with Malaysian races in that; >60% of Indians had infected with NAFLD followed by 51.1% and 34.2% of Malays and Chinese, respectively. This indicates that the highest prevalence of NAFLD was among Indians, whereas the lowest was among Chinese. As with several recent studies conducted in Asia, we adopted the Asian definition to categorize BMI.23 In Malaysia, where prevalence of high BMI has been increased,33 it would be interesting to predict the possibility of NAFLD rates increasing in this country. We noted a preponderance of NAFLD among severely obese followed by obese, overweight, and normal. This indicates that prevalence of NAFLD has gradually increased with increase in BMI. This result is compatible with previous findings of the studies, which have shown that high BMI is closely correlated with NAFLD.34–36
As with recent studies, when risk factors for NAFLD are analyzed, it has been identified that overweight, obese, and severely obese were found to be risk factors of developing NAFLD.10,37 Consistent with a previous study by Shen et al30 we found that NAFLD was significantly correlated with WHR in that NAFLD was more prevalent in subjects with high WHR than in subjects with normal WHR. Because high WHR is related to increased visceral adiposity and abdominal fatty tissue, univariate regression analysis in the present study demonstrated a strong association between high WHR and NAFLD. Surprisingly, however, high WHR was not identified to be a risk predictive factor in the inducement of NAFLD on the multiple logistic regression analysis.
Lipid profile covers TC, TG, HDL-C, and LDL-C, which are obtained from lipid profile tests. Cholesterol is one type of blood lipids and it is an essential element to construct estrogen and other sex hormones and also synthesizes vitamin D so that it is considered a necessary item in body organisms. Red meats such as lamb and beef as well as dairy products are considered main sources for cholesterol. HDL-C and LDL-C are terms linked to good and bad cholesterol, respectively. HDL-C is linked to lower risk of CVD and metabolic syndrome by carrying cholesterol back to the liver and subsequently preventing cholesterol synthesis in the arteries so that it is known as good cholesterol, whereas LDL-C is linked to increased risk of CVD and metabolic syndrome by deposition in the arteries so that it is known as bad cholesterol. TG is another type of lipid that is employed to store energy from food.38 Thus, pathophysiology mechanism of NAFLD is summarized than hepatic steatosis due to deposition of serum TG into hepatocytes39 and then it induces the liver susceptibility to additional injury.40
Dyslipidemia among patients with NAFLD has been confirmed in several previous studies, and consistent with an earlier study by DeFilippis et al.41 The present study has shown that hypertriglyceridemia and low HDL-C are associated with NAFLD, whereas hypercholesterolemia and high LDL-C have not been found to be associated with NAFLD. On the contrary, Malik et al15 mentioned that high TC, high TG, low HDL-C, and high LDL-C have been associated with NAFLD. As of late, several studies have confirmed that hypercholesterolemia leads to NAFLD.42–45 These results prove that NAFLD resulting from overproduction of TC may be associated with atherosclerosis within arteries; causing the accumulation of fat in the liver and arteries.12
There is considerable controversial literature about lipid profile variables as predictors for NAFLD. For instance, we found only hypertriglyceridemia among lipid profile variables to be an independent predictive factor for NAFLD, whereas Goh et al,10 revealed that hypertriglyceridemia and low HDL-C were noted to be predictors of developing NAFLD. In addition to that, Malik et al15 found that TC, TG, HDL-C, and LDL-C were not revealed to be predictors for NAFLD.
Moreover, DM and hypertension are manifestations of the metabolic abnormalities which are associated with the inducement of NAFLD.6,46 Our findings are in conformity with previous published results by Gariani et al18 and Stefan and Haring,47 which indicated that prevalence of NAFLD was higher among patients with DM than among their counterparts without diabetes. In Malaysia, recent studies demonstrated an increase in the prevalence of DM in the local population, especially among Malays and Indians.48 Both univariate and multivariate regression analyses showed a strong correlation between DM and NAFLD. As with other studies, the presence of DM was noted to be an important risk factor for NAFLD on multiple logistic regression,10,30 whereas Almobarak et al34 affirmed no significant correlation between DM and NAFLD. When glucose level is raised in the context of pre-DM or overt DM, it supplies further substrate for TG synthesis. Furthermore, impaired very low-density lipoprotein excretion, which mostly happens with insulin resistance, additionally contributes to fat deposition in hepatocytes.49
Our study is in line with other studies carried out by Donati et al50 and Lopez-Suarez et al,51 which revealed that NAFLD was more prevalent among hypertensive subjects. As with more published researches, again, univariate analysis showed a close correlation between hypertension and NAFLD.10,30 This result is inconsistent with several recent studies,6,16,34 which confirmed that there was no association between hypertension and NAFLD. Statistically, we observed that hypertension was not predictor for developing NAFLD.
There are, however, limitations to the study, which linked to the sampling method for subject in this study. Although subjects were randomly selected, our study population has not included all ages because the majority of subjects who come there are adults and elderly. Therefore, the studied respondents are not reflected of the entire population in Klang valley. As such, the respondents attended voluntarily and the demography has been affected by the health-seeking behavior of these respondents, females, elderly, and Chinese. The health check-up center serves a typical urban, affluent area of the country. Otherwise, ultrasound is widely used so far for detecting moderate and severe fatty liver changes in epidemiological studies and clinical practice but it lacks in diagnosing mild fatty liver. Therefore, the prevalence of NAFLD might have been underestimated because mild fatty liver patients might have been lost on ultrasound scanning.
In summary, NAFLD is common among Malaysian adults in the urban study area. It is highly correlated with male sex, Malays and Indians, high BMI (≥23.0 kg/m2), high WHR, hypertriglyceridemia, low HDL-C, DM, and hypertension. The following variables were demonstrated to be significant risk predictive factors for NAFLD: age >60 years, male sex, high BMI (≥23.0 kg/m2), hypertriglyceridemia, and DM.
Acknowledgments
The authors would like to acknowledge the help from Dr. Norafida Bahari/radiologist from the Department of Imaging, Faculty of Medicine and Health Sciences, UPM. The authors are thankful and grateful to all of administrators and medical personnel who have willingly helped us out with their abilities in Golden Horses Health Sancturay, Klang Valley as well.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
The authors have no competing interests.
References
- [1].Duan X, Qiao L, Fan J. Clinical features of nonalcoholic fatty liver disease-associated hepatocellular carcinoma. Hepatobiliary Pancreat Dis Int. 2012;11:18–27. [DOI] [PubMed] [Google Scholar]
- [2].Li N, Zhang G, Zhang J, et al. Non-alcoholic fatty liver disease is associated with progression of arterial stiffness. Nutr Metab Cardiovasc Dis. 2015;25:218–223. [DOI] [PubMed] [Google Scholar]
- [3].Nseir W, Hellou E, Assy N. Role of diet and lifestyle changes in nonalcoholic fatty liver disease. World J Gastroenterol. 2014;20:9338–9344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Chitturi S, Farrell GC, Hashimoto E, et al. Non-alcoholic fatty liver disease in the Asia–Pacific region: definitions and overview of proposed guidelines. J Gastroenterol Hepatol. 2007;22:778–787. [DOI] [PubMed] [Google Scholar]
- [5].Park SH, Jeon WK, Kim SH, et al. Prevalence and risk factors of non-alcoholic fatty liver disease among Korean adults. J Gastroenterol Hepatol. 2006;21:138–143. [DOI] [PubMed] [Google Scholar]
- [6].Chan W, Tan AT, Vethakkan SR, et al. Non-alcoholic fatty liver disease in diabetics–prevalence and predictive factors in a multiracial hospital clinic population in Malaysia. J Gastroenterol Hepatol. 2013;28:1375–1383. [DOI] [PubMed] [Google Scholar]
- [7].Wah-Kheong C, Khean-Lee G. Epidemiology of a fast emerging disease in the Asia-Pacific region: non-alcoholic fatty liver disease. Hepatol Int. 2013;7:65–71. [DOI] [PubMed] [Google Scholar]
- [8].Adams LA, Harmsen S, Sauver JLS, et al. Nonalcoholic fatty liver disease increases risk of death among patients with diabetes: a community-based cohort study. Am J Gastroenterol. 2010;105:1567–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Kim HJ, Kim HJ, Lee KE, et al. Metabolic significance of nonalcoholic fatty liver disease in nonobese, nondiabetic adults. Arch Intern Med. 2004;164:2169–2175. [DOI] [PubMed] [Google Scholar]
- [10].Goh S, Ho EL, Goh K. Prevalence and risk factors of non-alcoholic fatty liver disease in a multiracial suburban Asian population in Malaysia. Hepatol Int. 2013;7:548–554. [DOI] [PubMed] [Google Scholar]
- [11].Mehta SR, Thomas EL, Bell JD, et al. Non-invasive means of measuring hepatic fat content. World J Gastroenterol. 2008;14:3476–3483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Kim EJ, Kim B, Seo HS, et al. Cholesterol-induced non-alcoholic fatty liver disease and atherosclerosis aggravated by systemic inflammation. PLoS One. 2014;9:e97841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Chen C, Huang M, Yang J, et al. Prevalence and risk factors of nonalcoholic fatty liver disease in an adult population of Taiwan: metabolic significance of nonalcoholic fatty liver disease in nonobese adults. J Clin Gastroenterol. 2006;40:745–752. [DOI] [PubMed] [Google Scholar]
- [14].Dai H, Chu L, Song S, et al. Prevalence of and risk factors for fatty liver disease in a professional population of Wuhan, China. Public Health. 2009;123:545–548. [DOI] [PubMed] [Google Scholar]
- [15].Malik A, Cheah P, Hilmi IN, et al. Non-alcoholic fatty liver disease in Malaysia: a demographic, anthropometric, metabolic and histological study. J Dig Dis. 2007;8:58–64. [DOI] [PubMed] [Google Scholar]
- [16].Almobarak AO, Barakat S, Suliman EA, et al. Prevalence of and predictive factors for nonalcoholic fatty liver disease in Sudanese individuals with type 2 diabetes: is metabolic syndrome the culprit? Arab J Gastroenterol. 2015;16:58–58. [DOI] [PubMed] [Google Scholar]
- [17].Fruci B, Giuliano S, Mazza A, et al. Nonalcoholic fatty liver: a possible new target for type 2 diabetes prevention and treatment. Int J Mol Sci. 2013;14:22933–22966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Gariani K, Philippe J, Jornayvaz FR. Non-alcoholic fatty liver disease and insulin resistance: from bench to bedside. Diabetes Metab. 2013;39:16–26. [DOI] [PubMed] [Google Scholar]
- [19].Lindbäck SM, Gabbert C, Johnson BL, et al. Pediatric nonalcoholic fatty liver disease: a comprehensive review. Adv Pediatr. 2010;57:85–40. [DOI] [PubMed] [Google Scholar]
- [20].Nobili V, Alisi A, Raponi M. Pediatric non-alcoholic fatty liver disease: preventive and therapeutic value of lifestyle intervention. World J Gastroenterol. 2009;15:6017–6022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Farrell GC, Chitturi S, Lau GK, et al. Guidelines for the assessment and management of non-alcoholic fatty liver disease in the Asia–Pacific region: executive summary. J Gastroenterol Hepatol. 2007;22:775–777. [DOI] [PubMed] [Google Scholar]
- [22].National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adults Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adults Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- [23].World Health Organization. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment. Health Communications Australia, Melbourne, Australia: 2002. [Google Scholar]
- [24].Adams LA, Lymp JF, Sauver JS, et al. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129:113–121. [DOI] [PubMed] [Google Scholar]
- [25].Ahmed MH, Barakat S, Almobarak AO. Nonalcoholic fatty liver disease and cardiovascular disease: has the time come for cardiologists to be hepatologists? J Obes. 2012;2012:483135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Muhidin SO, Magan AA, Osman KA, et al. The relationship between nonalcoholic fatty liver disease and colorectal cancer: the future challenges and outcomes of the metabolic syndrome. J Obes. 2012;2012:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Amarapurkar D, Kamani P, Patel N, et al. Prevalence of non-alcoholic fatty liver disease: population based study. Ann Hepatol. 2007;6:161–163. [PubMed] [Google Scholar]
- [28].Fan J, Saibara T, Chitturi S, et al. What are the risk factors and settings for non-alcoholic fatty liver disease in Asia–Pacific? J Gastroenterol Hepatol. 2007;22:794–800. [DOI] [PubMed] [Google Scholar]
- [29].Omagari K, Kadokawa Y, Masuda J, et al. Fatty liver in non-alcoholic non-overweight Japanese adults: incidence and clinical characteristics. J Gastroenterol Hepatol. 2002;17:1098–1105. [DOI] [PubMed] [Google Scholar]
- [30].Shen L, Fan J, Shao Y, et al. Prevalence of nonalcoholic fatty liver among administrative officers in shanghai: an epidemiological survey. World J Gastroenterol. 2003;9:1106–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Fan J-G, Zhu J, Li X-J, et al. Prevalence of and risk factors for fatty liver in a general population of Shanghai, China. J Hepatol. 2005;43:508–514. [DOI] [PubMed] [Google Scholar]
- [32].Cheng H-Y, Wang H-Y, Chang W-H, et al. Nonalcoholic fatty liver disease: prevalence, influence on age and sex, and relationship with metabolic syndrome and insulin resistance. Int J Gerontol. 2013;7:194–198. [Google Scholar]
- [33].Rampal L, Rampal S, Khor GL, et al. A national study on the prevalence of obesity among 16,127 Malaysians. Asia Pac J Clin Nutr. 2007;16:561–566. [PubMed] [Google Scholar]
- [34].Almobarak AO, Barakat S, Khalifa MH, et al. Non alcoholic fatty liver disease (NAFLD) in a sudanese population: What is the prevalence and risk factors? Arab J Gastroenterol. 2014;15:12–15. [DOI] [PubMed] [Google Scholar]
- [35].De Alwis NM, Day CP. Non-alcoholic fatty liver disease: the mist gradually clears. J Hepatol. 2008;48:S104–S112. [DOI] [PubMed] [Google Scholar]
- [36].Kirovski G, Schacherer D, Wobser H, et al. Prevalence of ultrasound-diagnosed non-alcoholic fatty liver disease in a hospital cohort and its association with anthropometric, biochemical and sonographic characteristics. Int J Clin Exp Med. 2010;3:202–210. [PMC free article] [PubMed] [Google Scholar]
- [37].Machado MV, Cortez-Pinto H. Non-alcoholic fatty liver disease: what the clinician needs to know. World J Gastroenterol. 2014;20:12956–12980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Durstine JL. Action Plan for High Cholesterol Human Kinetics. D. Mark Robertson, American College of Sports Medicine, United States of America: 2006. [Google Scholar]
- [39].Marchesini G, Brizi M, Morselli-Labate AM, et al. Association of nonalcoholic fatty liver disease with insulin resistance. Am J Med. 1999;107:450–455. [DOI] [PubMed] [Google Scholar]
- [40].Sanyal AJ, Campbell–Sargent C, Mirshahi F, et al. Nonalcoholic steatohepatitis: association of insulin resistance and mitochondrial abnormalities. Gastroenterology. 2001;120:1183–1192. [DOI] [PubMed] [Google Scholar]
- [41].DeFilippis AP, Blaha MJ, Martin SS, et al. Nonalcoholic fatty liver disease and serum lipoproteins: the multi-ethnic study of atherosclerosis. Atherosclerosis. 2013;227:429–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Kleemann R, Verschuren L, Van Erk MJ, et al. Atherosclerosis and liver inflammation induced by increased dietary cholesterol intake: a combined transcriptomics and metabolomics analysis. Genome Biol. 2007;8:R200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Lee L, Alloosh M, Saxena R, et al. Nutritional model of steatohepatitis and metabolic syndrome in the Ossabaw miniature swine. Hepatology. 2009;50:56–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Ma KL, Ruan XZ, Powis SH, et al. Inflammatory stress exacerbates lipid accumulation in hepatic cells and fatty livers of apolipoprotein E knockout mice. Hepatology. 2008;48:770–771. [DOI] [PubMed] [Google Scholar]
- [45].Tous M, Ferré N, Camps J, et al. Feeding apolipoprotein E-knockout mice with cholesterol and fat enriched diets may be a model of non-alcoholic steatohepatitis. Mol Cell Biochem. 2005;268:53–58. [DOI] [PubMed] [Google Scholar]
- [46].Fan J, Li F, Cai X, et al. The importance of metabolic factors for the increasing prevalence of fatty liver in shanghai factory workers. J Gastroenterol Hepatol. 2007;22:663–668. [DOI] [PubMed] [Google Scholar]
- [47].Stefan N, Haring HU. The metabolically benign and malignant fatty liver. Diabetes. 2011;60:2011–2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Rampal S, Rampal L, Rahmat R, et al. Variation in the prevalence, awareness, and control of diabetes in a multiethnic population: a nationwide population study in Malaysia. Asia Pac J Public Health. 2010;22:194–202. [DOI] [PubMed] [Google Scholar]
- [49].Bhatt HB, Smith RJ. Fatty liver disease in diabetes mellitus. Hepatobil Surg Nutr. 2015;4:101–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Donati G, Stagni B, Piscaglia F, et al. Increased prevalence of fatty liver in arterial hypertensive patients with normal liver enzymes: role of insulin resistance. Gut. 2004;53:1020–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Lopez-Suarez A, Guerrero JM, Elvira-Gonzalez J, et al. Nonalcoholic fatty liver disease is associated with blood pressure in hypertensive and nonhypertensive individuals from the general population with normal levels of alanine aminotransferase. Eur J Gastroenterol Hepatol. 2011;23:1011–1017. [DOI] [PubMed] [Google Scholar]


