Abstract
OBJECTIVE. Our objective was to identify perceived barriers and strategies to improve primary care encounters, as reported by adults with autism spectrum disorder (ASD), caregivers of adults with ASD, and primary care providers (PCPs) treating adults with ASD.
METHOD. As part of a larger mixed-methods design, adults with ASD, caregivers, and PCPs (N = 78) in Los Angeles and Philadelphia completed surveys examining barriers to care and strategies to improve care.
RESULTS. Multiple barriers to care were reported by adults with ASD and caregivers, including communication and sensory challenges. Adults with ASD and caregivers reported minimal use of strategies during primary care visits but indicated that those used were helpful during care. Expert PCPs reported using strategies more frequently than novice PCPs. All respondent groups endorsed that strategies had the potential to improve care in the future for adults with ASD.
CONCLUSION. Opportunities exist for occupational therapy collaboration in primary health care and primary care education to improve care for adults with ASD.
Primary care is envisioned as a patient-centered, medical-home model that provides first-contact care, continuity of care over time, and coordination with other integral parts of the health system (American Academy of Family Physicians, 2019). It exemplifies a patient-centered culture that values the patient’s needs above all else and considers the entire patient versus a single attribute of the patient’s health (Bodenheimer & Pham, 2010; Starfield et al., 2005). A strong primary care system is associated with improved population health outcomes, greater access to health care services, higher patient satisfaction, and reduced health care spending (Atun, 2004).
Disparities in health status exist, however, between people with and without disabilities. Adults with disability have reported fair or poor health significantly more than adults without disability (40% vs. 10%, respectively; Centers for Disease Control and Prevention, 2008). Consistent with current disability research, adults with autism spectrum disorder (ASD) have greater unmet physical and mental health care needs, higher use of the emergency department, and lower use of preventive services than adults without ASD (Nicolaidis et al., 2013).
Few studies have documented the challenges that adults with ASD encounter within primary care. Reported barriers include strained patient–provider communication, an overstimulating clinical physical environment, ASD-related stigma, incorrect assumptions about the patient’s level of functioning, and a lack of ASD-specific education for the provider (Bruder et al., 2012; Nicolaidis et al., 2013, 2015; Raymaker et al., 2017; Warfield & Gulley, 2006; Zerbo et al., 2015); access to care is another reported challenge (Murphy et al., 2016).
Given these challenges, it is not surprising that adults with ASD have reported diminished satisfaction with health care providers as well as more unmet physical and mental health care needs than peers without ASD (Nicolaidis et al., 2013); at the same time, adults with ASD experience elevated rates of both medical and psychiatric conditions relative to the general population (Croen et al., 2015). Because adults with ASD represent a growing segment of American society (Roux et al., 2015), the number who require primary care is expected to increase over the next decade. Consequently, a pressing need exists to improve the quality of primary health care experiences for adults with ASD with empirically validated, client-centered strategies and tools.
The purpose of this exploratory study was to identify perceived barriers and strategies to improve primary care health encounters, as reported by adults with ASD, caregivers of adults with ASD, and primary care providers (PCPs) treating adults with ASD. Specifically, the following research questions were addressed: 1. What are the barriers to the provision of primary care from the perspective of adults with ASD, caregivers of adults with ASD, and PCPs? 2. What strategies are perceived to support the provision of primary care from the perspective of adults with ASD, caregivers of adults with ASD, and PCPs?
These findings will provide potential areas of improvement for PCPs to address obstacles to the provision of successful primary health care services for adults with ASD.
Method
In this descriptive study, we gathered data through surveys completed by adults with ASD, caregivers of adults with ASD, and PCPs working with adults with ASD. This research was part of a larger mixed-methods study following a convergent parallel design. Quantitative and qualitative data were collected concurrently; results presented here are from the quantitative portion of the study. This study was approved by the institutional review board of the University of Southern California Health Sciences (HS-17-00477), and informed consent was obtained from all participants.
Participants
Adults With Autism Spectrum Disorder.
Participants who met inclusion criteria were age 18 yr or older; were able to communicate using verbal, written, or augmentative and alternative techniques in English or Spanish; and had undertaken at least one primary care medical visit. Participants self-reported a formal ASD diagnosis, confirmed for inclusion in this study by a score of ≥65, the stated ASD cutoff score, on the Ritvo Autism Asperger Diagnostic Scale–Revised (RAADS–R; Ritvo et al., 2011; Table 1).
Table 1.
Descriptive Characteristics of Adults With ASD
| Variable | Adult With ASD (n = 34) | Caregiver Report (n = 31) |
| Age, M (SD) | 31.5 (12.0) | 24.3 (6.6) |
| RAADS–R score, M (SD) | 117.8 (50.6) | 124.4 (31.5) |
| Gender, n (%) | ||
| Male | 28 (82.4) | 27 (87.1) |
| Female | 6 (17.6) | 4 (12.9) |
| Race, n (%) | ||
| White | 23 (67.6) | 21 (67.7) |
| Not White | 10 (29.4) | 9 (29.0) |
| Not reported | 1 (2.9) | 1 (3.2) |
| Ethnicity, n (%) | ||
| Not Hispanic, not Latino | 28 (82.4) | 22 (71.0) |
| Hispanic or Latino | 6 (17.6) | 9 (29.0) |
| Primary language spoken in the home, n (%) | ||
| English | 31 (91.2) | 22 (71.0) |
| Spanish | 2 (5.9) | 5 (16.1) |
| Other | 1 (2.9) | 4 (12.9) |
| Highest level of education, n (%) | ||
| High school or GED | 13 (38.2) | 28 (90.3) |
| College | 18 (52.9) | 3 (9.7) |
| Graduate degree or greater | 3 (8.8) | 0 (0.0) |
| Communicates needs or wants by using,a n (%) | ||
| Sentences | N/A | 19 (61.3) |
| Single words or phrases | N/A | 10 (32.3) |
| Augmentative and alternative communication device | N/A | 2 (6.5) |
Note. ASD = autism spectrum disorder; GED = General Education Development; M = mean; N/A = not applicable; RAADS–R = Ritvo Autism Asperger Diagnostic Scale–Revised; SD = standard deviation.
Question only asked of caregivers; all adults with ASD interviewed were able to communicate verbally using sentences.
Caregivers of Adults With Autism Spectrum Disorder.
To meet inclusion criteria, caregivers had to be supporting an adult age 18 yr or older with a self-reported ASD diagnosis, confirmed by a score of ≥65 on the RAADS–R; speak English or Spanish; and have previously accompanied the adult with ASD to at least one primary care medical visit. In completing the RAADS–R, participants were asked to answer each question about the adult with ASD from their perspective as caregiver (see Table 1).
Primary Care Providers Working With Adults With Autism Spectrum Disorder.
To participate in the study, PCPs had to have provided care to at least one adult with ASD. PCPs were divided into novice, moderate experience, and expert providers on the basis of the number of adults with ASD they reported treating in the past 2 yr. A novice PCP had provided care to fewer than 10 adults with ASD, a provider with moderate experience had provided care to 10–99 patients, and an expert provider had provided care to 100 or more patients with ASD in the past 2 yr.
Recruitment
Participants were recruited with the support of multiple collaborative sites in the Southern California and Philadelphia areas as well as through social media outlets. Brochures and flyers were posted, and recruitment presentations took place at participating sites, including local support groups, therapy locations, primary care clinics, hospitals, and supported employment locations. Consecutive sampling of participants who indicated interest took place; snowball sampling was additionally used to identify and recruit PCPs.
Data Collection
Participants completed a survey designed to elicit information about current and previous primary health care experiences (a copy of the survey may be requested from the first author). Survey questions were developed on the basis of issues identified in the literature (e.g., physical and sensory environments, scheduling, desensitization, preparation). Questions were crafted by the authors, reviewed and edited by an expert in adult primary care, and then pilot tested by 5 adults with ASD and 1 PCP. Revisions were made secondary to all reviewers’ feedback.
Question topics included strategies previously used by the adult with ASD, caregiver, or PCP; the success of those strategies; and the potential of those strategies to improve care in the future. Additional questions included ones about participant demographics (age, gender, race, ethnicity, primary language) and general questions regarding primary care, overall health status, and experience treating adults with ASD (PCP group only). Adults with ASD and caregivers additionally answered the 17-item Barriers to Healthcare Checklist–Short Form (Raymaker et al., 2017), which was developed to identify health care barriers for adults with ASD. Surveys comprised a total of 50 items for adults with ASD, 74 items for caregivers, and 32 items for PCPs and included dichotomous yes–no and 5-point Likert-scale questions.
The survey was provided to respondents in person or online immediately before the qualitative component of the larger study. Trained research assistants were available to answer questions and to assist with survey completion as needed.
Data Analysis
Data were analyzed with IBM SPSS Statistics (Version 25; IBM Corp., Armonk, NY). For descriptive purposes, frequencies and percentages were calculated for each item. PCP data were stratified post hoc to identify differences in PCP perspectives on the basis of level of experience (novice, moderate experience, expert). This method provides a preliminary comparison to determine whether level of experience is an important consideration when interpreting data and designing future research and interventions.
Results
Survey Respondents
Participants included 34 adults with ASD and 31 caregivers of adults with ASD (Table 1). More than 60% of both respondent groups reported that the adult with ASD had very good or excellent overall health. Most adults with ASD reported having one specific PCP they see for care (79%). A smaller percentage (9%) reported that they were seen by any PCP available at their doctor’s office. Only 3 adults with ASD (9%) and 2 caregivers (6%) reported that they (or their adult child with ASD) did not have a PCP (see Table 1).
Participating caregivers were mothers (87%), fathers (10%), and 1 unrelated caregiver (3%). Caregivers self-identified as White (71%), Black (10%), Asian (7%), and more than one race (10%); 1 caregiver (3%) chose not to provide information on race. Ethnicity was reported as Hispanic or Latino for 32% of participants and not Hispanic or Latino for 65%. The primary language spoken at home was English (71%), Spanish (16%), or English and another language (13%; Spanish, Italian, Korean).
Thirteen PCPs participated in the study. In the previous 2 yr, novice providers (n = 5) reported treating an average of 3.4 (standard deviation [SD] = 2.4) adult patients with ASD, moderate-experience providers (n = 3) reported treating an average of 15 (SD = 5.0) patients, and expert providers (n = 5) reported treating an average of 200 (SD = 70.7) patients. No significant differences were found between demographic or history variables among novice, moderate-experience, and expert PCP groups. For the group as a whole, PCPs were medical doctors (77%) or doctors of osteopathic medicine (23%), with an average of 17.2 yr (SD = 9.2) working as a PCP. Most providers were female (62%), White, and not Hispanic or Latino (92%), and they had an average age of 48.1 yr (SD = 9.2). Most providers reported that they had received no autism-specific education (77%), 15% reported hands-on training, and 8% reported a combination of lecture and observation. Of the entire PCP group, 92% stated that their training did not prepare them to work with adults with ASD. Of the providers, 69% reported completing additional autism-specific continuing education or specialty courses.
Barriers to Health Care
Adults with ASD and caregivers endorsed approximately 30% of listed barriers: 5 (SD = 3.8) and 6 (SD = 3.9) of 17 total items, respectively. Both respondent groups reported that communication with health care providers and staff posed a challenge for the adult with ASD (adult with ASD report, 29%; caregiver report, 42%) and that health care providers and staff did not take the communications of the adult with ASD seriously (adult with ASD report: 21%; caregiver report: 42%). Sensory discomfort was reported to “get in the way” of the adult with ASD’s health care by approximately 35% of both groups; likewise, approximately 35% of adults with ASD were reported to experience challenges in the waiting room. Twenty-one percent of adults with ASD and 42% of caregivers reported that the behaviors of the adult with ASD were misinterpreted by health care providers and staff. Fewer than 20% of both groups reported that finding a provider to accommodate the needs of the adult with ASD was challenging (Table 2).
Table 2.
Affirmative Responses by Adults With ASD and Caregivers Regarding Perceived Barriers to Health Care
| Item | Affirmative Responses, n (%) | |
| Adults With ASD (n = 34) | Caregiver Report (n = 31) | |
| Fear, anxiety, embarrassment, or frustration keeps mea from getting primary care. | 7 (20.6) | 3 (9.7) |
| I have trouble following up on care (e.g., going to the pharmacy, taking prescribed drugs at the right time, or making a follow-up appointment). | 9 (26.5) | 15 (48.4) |
| I have difficulty understanding how to translate medical information into concrete steps that I can take to improve my health. | 10 (29.4) | 21 (67.7) |
| I don’t understand the health care system. | 12 (35.3) | 13 (41.9) |
| It is too difficult to make appointments for me. | 8 (23.5) | 19 (61.3) |
| I have problems filling out paperwork. | 12 (35.3) | 24 (77.4) |
| My behaviors are misinterpreted by my provider or the staff. | 7 (20.6) | 13 (41.9) |
| My providers or the staff do not take my communications seriously. | 7 (20.6) | 10 (32.3) |
| I cannot find a health care provider who will accommodate my needs. | 5 (14.7) | 6 (19.4) |
| My providers and staff do not include me in discussions about my health. | 6 (17.6) | 6 (19.4) |
| Communication with my health care provider or the staff is too difficult for me. | 10 (29.4) | 13 (41.9) |
| When I experience pain or other physical symptoms, I have difficulties identifying them and reporting them to my health care provider. | 14 (41.2) | 16 (51.6) |
| Sensory discomforts (lights, smells, or sounds) get in the way of my health care. | 12 (34.3) | 12 (38.7) |
| Concerns about cost or insurance coverage keeps me from getting primary care. | 13 (38.2) | 5 (16.1) |
| I do not have a way to get to my doctor’s office. | 1 (2.9) | 5 (16.1) |
| I have inadequate social, family, or caregiver support. | 11 (32.4) | 3 (9.7) |
| I find it hard to handle the waiting room. | 12 (35.3) | 10 (32.3) |
Note. ASD = autism spectrum disorder.
Surveys for adults with ASD read “I/me/my” in the question stem, whereas caregivers’ surveys read “my child/client with ASD.”
Strategies to Improve Care
Reports From Adults With Autism Spectrum Disorder and Caregivers.
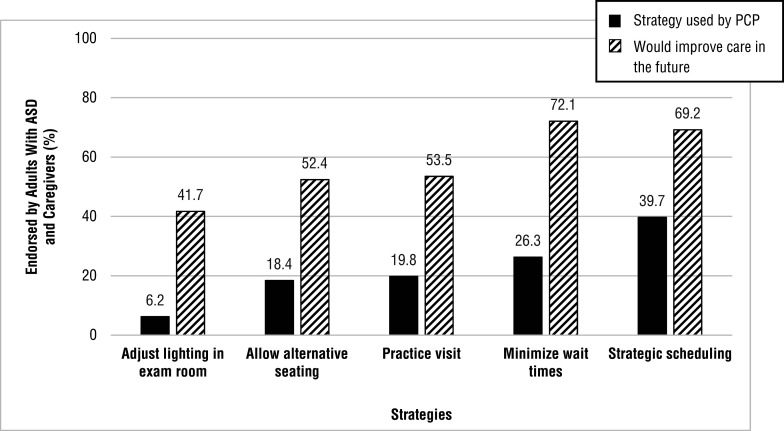
Adults with ASD and caregivers both reported minimal use of strategies by PCPs to improve care during visits. For example, only 6% of providers were reported to have adjusted lighting in the examination room, 18% allowed alternative seating (e.g., not on the exam table), 20% implemented a practice visit (e.g., tour, desensitization visit), 26% actively sought to minimize wait times in the waiting room and examination room, and 40% suggested strategic scheduling (e.g., first or last appointment of the day) for patients with ASD. Of the respondents whose PCPs used these strategies, 100% of caregivers reported that the strategy was helpful when used. All adults with ASD reported that adjusting lighting and minimizing wait times were helpful; the majority stated that strategic scheduling (94%), alternative seating (86%), and a practice visit (75%) were helpful. Respondents in both groups overwhelmingly stated that they believed implementing these strategies would improve care in the future (Figure 1).
Figure 1.
Strategies used by PCPs versus strategies perceived by adults with ASD and caregivers to improve care in future visits, as reported by adults with ASD and caregivers.
Note. ASD = autism spectrum disorder; PCPs = primary care providers.
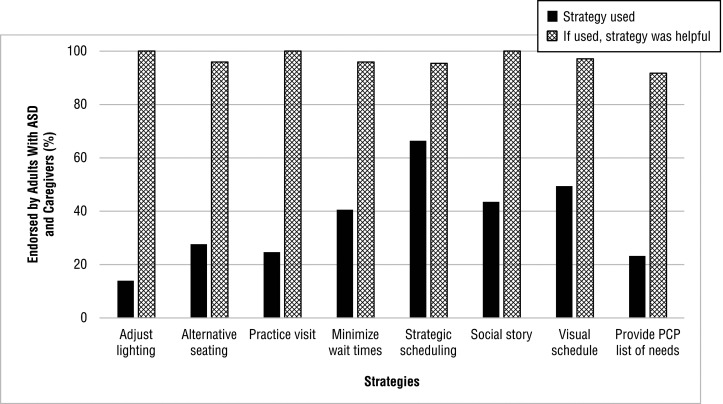
Adults with ASD and caregivers also reported that they only minimally used strategies during primary care visits. However, almost 100% of respondents who reported using strategies stated that using the strategy was helpful during the primary care visit. In addition, 50% or more of respondents stated that they felt using each of these strategies in the future would help to improve care. Of particular note, 60%–70% endorsed using a social story, using a visual schedule, or providing a provider with a list of needs before the appointment to improve future care; approximately 80% agreed that minimizing wait times and use of strategic scheduling would improve care in the future (Figure 2).
Figure 2.
Strategies used by adults with ASD and caregivers and their perceived helpfulness during care, as reported by adults with ASD and caregivers.
Note. ASD = autism spectrum disorder; PCP = primary care provider.
Reports From Primary Care Providers.
Almost 85% of PCPs reported that they collaborated with other health care professionals on strategies regarding how to treat adults with ASD. These collaborators included ASD researchers, developmental pediatricians, psychiatrists, psychologists, and occupational therapy practitioners. All PCPs stated that making accommodations for patients with ASD did not deter them from treating these patients. However, PCPs with more experience believed that making accommodations for patients with ASD did deter other PCPs from treating them (novice, 20%; moderate experience, 67%; expert, 100%).
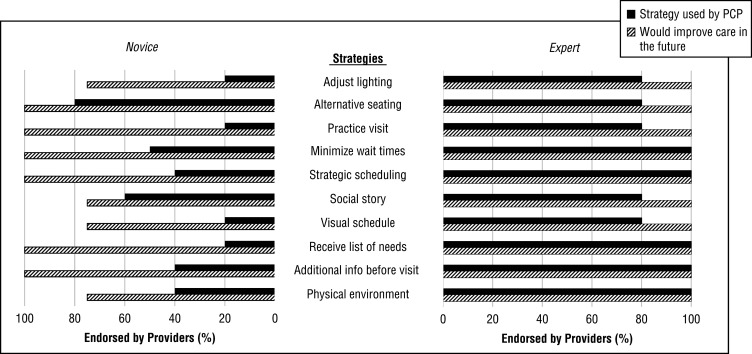
Providers were asked (1) to rank how important they believed each stated strategy was in providing a positive health care experience for adults with ASD, (2) whether they currently used that strategy in their practice, and (3) whether they felt each strategy might be helpful to improve care in the future. Of the providers, 100% responded that they believed strategic scheduling and minimizing wait times in the waiting room and exam room were moderately to extremely important. More than 75% of PCPs in all experience groups reported that using a social story, receiving a list of requested needs and strategies, and having additional information about the patient before the visit (e.g., communication preferences, sensory sensitivities) were moderately to extremely important in providing a positive health care experience for adults with ASD.
All novice and expert providers reported that the physical environment of the waiting room and clinic were moderately to extremely important. Most novice (75%) and all moderate-experience (100%) PCPs reported that a practice visit and adjusting the lighting were moderately to extremely important, whereas expert providers only endorsed these items at 60% and 40%, respectively. Conversely, only 25% of novice providers and 50% of moderate-experience providers ranked a visual schedule as moderately to extremely important compared with 80% of expert providers. Most expert providers reported currently using multiple strategies to treat adults with ASD; all providers, regardless of expertise level, endorsed that the use of these strategies had the potential to improve care in the future for adults with ASD (Figure 3).
Figure 3.
Strategies used by PCPs and their perceived benefit to improve care in future visits, as reported by novice and expert PCPs.
Note. ASD = autism spectrum disorder; PCP = primary care provider.
Discussion
Results of the current study align with past research, suggesting that many adults with ASD and caregivers of adults with ASD experience challenges with primary health care encounters (Bruder et al., 2012; Nicolaidis et al., 2013, 2015; Raymaker et al., 2017; Warfield & Gulley, 2006; Zerbo et al., 2015). Of the most commonly endorsed barriers reported by adults with ASD and caregivers in this study, two—sensory discomforts and concerns about cost—overlap with the top five barriers to care reported by Raymaker et al. (2017). In addition, difficulty communicating with providers was similarly endorsed by adults with ASD in both studies (29%). Occupational therapy practitioners have the ability to collaborate with health care providers to adapt the sensory environment to decrease discomfort and stress both while waiting for and during health care encounters. For example, practitioners have developed a sensory-adapted dental environment to decrease physiological and behavioral stress in children with ASD receiving dental care (Cermak et al., 2015); they have also explored their unique value in creating sensory-friendly waiting rooms (Hong et al., 2018).
In our results, participants reported using a variety of strategies to try to improve primary care visits. The most common strategies used by all three groups included strategic scheduling, use of a social story, and minimizing wait times; adults with ASD and caregivers also commonly reported the use of visual schedules. Use of these specific strategies were overwhelmingly reported to be successful in improving the visit. These techniques are commonly discussed and used by occupational therapy researchers and practitioners in their work with people with ASD in health care and other (e.g., school and therapy) environments and are well within their repertoire of skills (Case-Smith & Arbesman, 2008; Pfeiffer & Stein Duker, 2016; Stein Duker, 2019; Stein Duker et al., 2019).
In our study, approximately one-quarter of adults with ASD and caregivers reported that they could not find a provider who would accommodate their needs, and all expert PCPs reported that they believed making accommodations deterred other PCPs from treating patients with ASD. As reported by adults with ASD, caregivers, and novice PCPs, PCPs minimally used strategies or accommodations to improve care for adults with ASD. Also, most PCP participants reported inadequate training to prepare them to work with adults with ASD, similar to previous studies (Bruder et al., 2012; Warfield & Gulley, 2006; Zerbo et al., 2015).
Many approaches are needed to develop and implement programs to ameliorate the challenges centered around identifying and implementing accommodations, for example, the development of autism-specific medical education curricula, continuing education, workshops, and ASD-specific guidelines to care (such as in the UpToDate database, which currently only includes surveillance and screening in primary care for this population; Bridgemohan, 2018). Another approach to improve care, as described by Van Cleave et al. (2018), may be to develop individualized care plans to ensure that standardized accommodations are applied at visits for adults with ASD. In addition, the use of a guided list of questions for the PCP (Pfeiffer & Stein Duker, 2016) or providing PCPs with a personalized list of accommodations requested, such as the Autism Healthcare Accommodations Tool (Nicolaidis et al., 2016), may help to bridge this gap, providing PCPs with the necessary knowledge that they need to provide tailored and individualized care for adults with ASD.
Occupational therapy practitioners possess the multifaceted skill set needed for the development and application of techniques to provide individualized care for adults with ASD. As identified in the Occupational Therapy Practice Framework: Domain and Process (3rd ed.; American Occupational Therapy Association, 2014), occupational therapy practitioners address both the person and the environmental factors when identifying and developing feasible, effective interventions for best practice that incorporate a full portfolio of practical strategies for enhanced care. Consistent with the International Classification of Functioning, Disability and Health (World Health Organization, 2001), contextual factors linked to health provision and outcomes include both the person and the environment. This unique approach of targeting strategies to improve the person–environment fit (Law et al., 1996) supports the use of tailored interventions necessary with a heterogeneous population, such as people with ASD, while also integrating both consumer and provider needs. Occupational therapy practitioners also have the research skills required to investigate the discrepancies between the current use of strategies and the belief that strategies have the potential to improve care; it is essential to understand why easily implemented strategies are not being used, even when providers believe they would help improve health care experiences. Last, of the providers in our study who collaborated with other health care professionals for strategies regarding how to treat adults with ASD, only 1 referenced an occupational therapy practitioner. It is integral that occupational therapy practitioners articulate their unique value as a part of an interprofessional team working to address the challenges that adults with ASD face in primary care health encounters.
Limitations
This exploratory study adds to the understanding of the barriers to primary health care that adults with ASD and their caregivers face as well as potential strategies to improve that care. However, certain limitations should be noted. First, our study design infers a nonrandom sample, suggesting that our results might not be representative of all adults with ASD, caregivers of adults with ASD, and PCPs treating adults with ASD. Second, the researchers experienced great challenges identifying and recruiting PCPs working with adults with ASD, regardless of the snowball sampling techniques, resulting in a small sample size. All providers who were approached agreed to participate in this study; the challenge was identifying PCPs who self-identified as working with this population.
Implications for Occupational Therapy Practice
The findings of this study have the following implications for occupational therapy practice:
Occupational therapy practitioners have nuanced knowledge of the relationship between the person and the environment and understand the impact that the health care environment may have on the health care experience of people with ASD. As such, practitioners need to advocate for the distinct value of having occupational therapy practitioners as part of the interdisciplinary team during primary care health encounters, specifically as it relates to supporting adults with ASD.
With their ASD-related knowledge and expertise in examining person–environment fit, occupational therapy practitioners should be involved in collaborating to develop autism-specific medical education curricula, continuing education, and workshops for medical students and PCPs.
It is essential that an interdisciplinary team, including occupational therapy practitioners and researchers, develops and tests the efficacy of environmentally focused interventions to improve primary health care encounters for adults with ASD. High-quality evidence is crucial to expand the role of practitioners in primary care as it relates to people with ASD.
Conclusion
Adults with ASD, their caregivers, and their PCPs all report multiple challenges with primary care health encounters. Opportunities exist for occupational therapy to collaborate with primary health care and primary care education to improve care for adults with ASD.
Acknowledgments
This work was supported by an American Occupational Therapy Foundation Intervention Research Grant (AOTFIRG16DUKER). Leah I. Stein Duker was also supported by National Center for Medical Rehabilitation Research Grant K12 HD055929.
References
- American Academy of Family Physicians. (2019). The medical home. Retrieved from https://www.aafp.org/practice-management/transformation/pcmh.html
- American Occupational Therapy Association. (2014). Occupational therapy practice framework: Domain and process (3rd ed.). American Journal of Occupational Therapy, 68(Suppl. 1), S1–S48. 10.5014/ajot.2014.682006 [DOI] [PubMed] [Google Scholar]
- Atun, R. (2004). What are the advantages and disadvantages of restructuring a health care system to be more focused on primary care services? Copenhagen: World Health Organization Regional Office for Europe’s Health Evidence Network. Retrieved from http://www.euro.who.int/document/e82997.pdf [Google Scholar]
- Bodenheimer, T., & Pham, H. H. (2010). Primary care: Current problems and proposed solutions. Health Affairs, 29, 799–805. 10.1377/hlthaff.2010.0026 [DOI] [PubMed] [Google Scholar]
- Bridgemohan, C. (2018). Autism spectrum disorder: Surveillance and screening in primary care. In Augustyn M. (Ed.), UpToDate. Retrieved from https://www.uptodate.com/contents/autism-spectrum-disorder-surveillance-and-screening-in-primary-care
- Bruder, M. B., Kerins, G., Mazzarella, C., Sims, J., & Stein, N. (2012). Brief report: The medical care of adults with autism spectrum disorders: Identifying the needs. Journal of Autism and Developmental Disorders, 42, 2498–2504. 10.1007/s10803-012-1496-x [DOI] [PubMed] [Google Scholar]
- Case-Smith, J., & Arbesman, M. (2008). Evidence-based review of interventions for autism used in or of relevance to occupational therapy. American Journal of Occupational Therapy, 62, 416–429. 10.5014/ajot.62.4.416 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2008). Racial/ethnic disparities in self-rated health status among adults with and without disabilities—United States, 2004–2006. Morbidity and Mortality Weekly Report, 57, 1069–1073. [PubMed] [Google Scholar]
- Cermak, S. A., Stein Duker, L. I., Williams, M. E., Dawson, M. E., Lane, C. J., & Polido, J. C. (2015). Sensory adapted dental environments to enhance oral care for children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 45, 2876–2888. 10.1007/s10803-015-2450-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croen, L. A., Zerbo, O., Qian, Y., Massolo, M. L., Rich, S., Sidney, S., & Kripke, C. (2015). The health status of adults on the autism spectrum. Autism, 19, 814–823. 10.1177/1362361315577517 [DOI] [PubMed] [Google Scholar]
- Hong, E. Y., Cermak, S. A., & Stein Duker, L. I. (2018). Occupational therapists’ distinct value in creating a sensory-friendly waiting room. SIS Quarterly Practice Connections, 3(3), 11–13. [Google Scholar]
- Law, M., Cooper, B., Strong, S., Steward, D., Rigby, P., & Letts, L. (1996). The Person–Environment–Occupation Model: A transactive approach to occupational performance. Canadian Journal of Occupational Therapy, 63, 9–23. 10.1177/000841749606300103 [DOI] [PubMed] [Google Scholar]
- Murphy, C. M., Wilson, C. E., Robertson, D. M., Ecker, C., Daly, E. M., Hammond, N., . . . McAlonan, G. M. (2016). Autism spectrum disorder in adults: Diagnosis, management, and health services development. Neuropsychiatric Disease and Treatment, 12, 1669–1686. 10.2147/NDT.S65455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicolaidis, C., Raymaker, D. M., Ashkenazy, E., McDonald, K. E., Dern, S., Baggs, A. E., . . . Boisclair, W. C. (2015). “Respect the way I need to communicate with you”: Healthcare experiences of adults on the autism spectrum. Autism, 19, 824–831. 10.1177/1362361315576221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicolaidis, C., Raymaker, D., McDonald, K., Dern, S., Boisclair, W. C., Ashkenazy, E., & Baggs, A. (2013). Comparison of healthcare experiences in autistic and non-autistic adults: A cross-sectional online survey facilitated by an academic–community partnership. Journal of General Internal Medicine, 28, 761–769. 10.1007/s11606-012-2262-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicolaidis, C., Raymaker, D., McDonald, K., Kapp, S., Weiner, M., Ashkenazy, E., . . . Baggs, A. (2016). The development and evaluation of an online healthcare toolkit for autistic adults and their primary care providers. Journal of General Internal Medicine, 31, 1180–1189. 10.1007/s11606-016-3763-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeiffer, B., & Stein Duker, L. I. (2016). The impact of the sensory environment on patient care for individuals with autism spectrum disorders. In Giarelli E. & Fisher K. (Eds.), Integrated health care for people with autism spectrum disorder: Interdisciplinary planning and delivery of care (pp. 69–92). Springfield, IL: Charles C Thomas. [Google Scholar]
- Raymaker, D. M., McDonald, K. E., Ashkenazy, E., Gerrity, M., Baggs, A. M., Kripke, C., . . . Nicolaidis, C. (2017). Barriers to healthcare: Instrument development and comparison between autistic adults and adults with and without other disabilities. Autism, 21, 972–984. 10.1177/1362361316661261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritvo, R. A., Ritvo, E. R., Guthrie, D., Ritvo, M. J., Hufnagel, D. H., McMahon, W., . . . Eloff, J. (2011). The Ritvo Autism Asperger Diagnostic Scale–Revised (RAADS–R): A scale to assist the diagnosis of autism spectrum disorder in adults: An international validation study. Journal of Autism and Developmental Disorders, 41, 1076–1089. 10.1007/s10803-010-1133-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roux, A. M., Shattuck, P. T., Rast, J. E., Rava, J. A., & Anderson, K. A. (2015). National Autism Indicators Report: Transition into young adulthood. Philadelphia: Life Course Outcomes Research Program, A. J. Drexel Autism Institute, Drexel University. [Google Scholar]
- Starfield, B., Shi, L., & Macinko, J. (2005). Contribution of primary care to health systems and health. Milbank Quarterly, 83, 457–502. 10.1111/j.1468-0009.2005.00409.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein Duker, L. I. (2019). Adapting oral care protocols to support children with sensory sensitivities: Occupational therapy and dentistry. In Nelson T. & De Bord J. R. (Eds.), Dental care for children with special needs: A clinical guide (pp. 77–98). New York: Springer. [Google Scholar]
- Stein Duker, L. I., Floríndez, L. I., Como, D. H., Tran, C. F., Henwood, B. F., Polido, J. C., & Cermak, S. A. (2019). Strategies for success: A qualitative study of caregiver and dentist approaches to improving oral care for children with autism. Pediatric Dentistry, 41, 4E–12E. [PMC free article] [PubMed] [Google Scholar]
- Van Cleave, J., Holifield, C., Neumeyer, A. M., Perrin, J. M., Powers, E., Van, L., & Kuhlthau, K. A. (2018). Expanding the capacity of primary care to treat co-morbidities in children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 48, 4222–4230. 10.1007/s10803-018-3630-x [DOI] [PubMed] [Google Scholar]
- Warfield, M. E., & Gulley, S. (2006). Unmet need and problems accessing specialty medical and related services among children with special health care needs. Maternal and Child Health Journal, 10, 201–216. 10.1007/s10995-005-0041-3 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2001). International classification of functioning, disability and health. Geneva: Author. [Google Scholar]
- Zerbo, O., Massolo, M. L., Qian, Y., & Croen, L. A. (2015). A study of physician knowledge and experience with autism in adults in a large integrated healthcare system. Journal of Autism and Developmental Disorders, 45, 4002–4014. 10.1007/s10803-015-2579-2 [DOI] [PubMed] [Google Scholar]