Abstract
We and others have reported that the anticancer activity of L-asparaginase (ASNase) against asparagine synthetase (ASNS)-positive cell types requires ASNase glutaminase activity, whereas anticancer activity against ASNS-negative cell types does not. Here we attempted to disentangle the relationship between asparagine metabolism, glutamine metabolism, and downstream pathways that modulate cell viability by testing the hypothesis that ASNase anticancer activity is based on asparagine depletion rather than glutamine depletion, per se. We tested ASNase wild-type (ASNaseWT) and its glutaminase deficient Q59L mutant (ASNaseQ59L) and found that ASNase glutaminase activity contributed to durable anticancer activity against xenografts of the ASNS-negative Sup-B15 leukemia cell line in NSG mice, whereas asparaginase activity alone yielded a mere growth delay. Our findings suggest that ASNase glutaminase activity is necessary for durable, single-agent anticancer activity in vivo, even against ASNS-negative cancer types.
Keywords: asparaginase, glutaminase, pharmacokinetics, pharmacodynamics, leukemia
INTRODUCTION
Escherichia coli L-asparaginase (ASNase) is a standard agent for treatment of acute lymphoblastic leukemia (ALL) and is being tested against other cancer types. As early as 1978, glutaminase activity was reported to contribute positively to the drug’s anticancer activity (1) but also to toxic side effects (2). Because side effects often prevent patients from completing the full treatment regimen necessary to achieve durable remission (3) the research community is actively pursuing development of glutaminase-deficient ASNase variants (4-6). We previously reported that one such mutational variant, ASNaseQ59L, retains anticancer activity against asparagine synthetase (ASNS)-negative leukemia cell types in vitro (4). However, we and others have also noted that glutaminase activity appears to be a major determinant of anticancer activity against ASNS-positive cell types (1,4,7,8) prompting the question: do glutaminase-deficient ASNase variants retain anticancer activity in vivo?
The expression of asparagine synthetase (ASNS) in most cells in the body poses a serious challenge to therapy with ASNase. Although asparagine levels were not found in one report to be increased in the bone marrow during asparaginase therapy (9) others have suggested that production of asparagine by the liver (10) and cells of the tumor microenvironment (e.g., mesenchymal stem cells (11,12) and adipocytes (13)) may contribute significantly to ASNase resistance in vivo. Here, we asked whether glutaminase-deficient ASNase can exert anticancer activity against an ASNS-negative human leukemia cell line, Sup-B15, in an ASNS-positive environment in NSG mice. Accordingly, we examined the in vivo anticancer activity associated with the asparaginase and glutaminase activities of ASNase by comparing wild-type enzyme (ASNaseWT) with a glutaminase-deficient mutant, ASNaseQ59L, which we designed through molecular dynamics calculations, generated by saturation mutagenesis, and characterized in kinetic and pharmacological assays (4).
MATERIALS AND METHODS
ASNase variants
E. coli L-asparaginase II (ASNase) recombinant proteins (wild type (WT) and mutant Q59L) were produced as described previously (4).
Determination of asparaginase and glutaminase enzymatic activity
Asparaginase and glutaminase activities of ASNase were measured as described previously (4). One unit (U) of asparaginase or glutaminase activity is defined as the amount of enzyme required to generate 1 μmol of aspartate or glutamate per minute from 100 μM asparagine or 2 mM glutamine, respectively, in 23-mM Tris buffer at pH 8.5 and 37°C. Specific activity is defined as units/mg of enzyme.
Mouse leukemia tumor model
Mouse studies were performed in a pathogen-free vivarium at The University of Texas MD Anderson Cancer Center under an approved Institutional Animal Care and Use Committee (IACUC) study protocol (ACUF #00001658-RN00). We injected 0.5 × 106 luciferase-engineered Sup-B15 cells in 100 μL PBS into each NSG mouse (NOD.Cg-PRKDC(scid) IL2RG(tm1Wjl); The Jackson Laboratory stock #005557) via the tail vein. After two weeks, leukemia burden was monitored using bioluminescence imaging (IVIS Imaging System, PerkinElmer), which was recently reported to be superior to peripheral blood monitoring of leukemia burden (14). We administered 100 μL 40 mg/mL D-potassium luciferin in PBS (Gold Biotechnolgy, St. Louis, MO) i.p. and measured leukemia burden 10 min later. After confirmation of engraftment (signal intensity ~1.0 × 105 p/s/cm2/sr), mice were randomized into three treatment groups (N=5/group): 1) ASNase wild-type (ASNaseWT), 2) ASNaseQ59L, and 3) phosphate-buffered saline (PBS) as a negative control. Treatments were administered intraperitoneally at 20,000 U/kg/day in 100 μL PBS for two weeks. Leukemia burden was assessed weekly using bioluminescent imaging (~9 weeks). Survival was monitored until termination of the study at Day 234.
ASNase pharmacokinetics/pharmacodynamics (PK/PD) mouse study
Asparagine, aspartic acid, glutamine, and glutamic acid in mouse whole blood were measured by liquid chromatography-tandem mass spectrometry (LC-MS/MS). After administering 20,000 U/kg of either ASNaseWT or ASNaseQ59L (or a matched volume of PBS lacking ASNase) to healthy NSG mice by i.p. injection, we serially sampled whole blood from individual mice to permit longitudinal analysis. Blood samples were collected immediately prior to treatment (t = 0) and at 1, 2, 4, 12, and 23 h after treatment. Whole blood was centrifuged at 3,000 g for 3 min to separate plasma and red blood cells, and a 2 μL aliquot of the plasma layer was immediately quenched with formic acid, combined with stable isotope-labeled internal standards, and analyzed by LC-MS/MS. ASNase enzymatic activity in mouse whole blood were determined by a colorimetric activity assay described previously (4). Paired t-test analysis was performed on all PK/PD data (Supplemental Table 1).
RESULTS
We performed a series of pilot experiments to optimize the dosage of ASNaseWT and ASNaseQ59L for PK/PD studies and in vivo anticancer activity against a preclinical model of ASNS-negative leukemia using the luciferase-engineered Sup-B15 cell line, which we previously showed to lack detectable ASNS protein expression before and after treatment with ASNase (5). We found that 14 daily treatments at 5,000 U/kg administered i.p., ASNaseWT and ASNaseQ59L failed to suppress leukemia progression (Supplemental Figures S1A and S1B). At the dosage of 10,000 U/kg, ASNaseWT was capable of inhibiting leukemia cell growth while ASNaseQ59L was still unable to stop leukemia progression (Supplemental Figures S1A and S1B). Mice tolerated the treatment well; we did not observe more than 10% weight loss (Supplemental Figure S1C), but one mouse in the ASNaseWT group died on Day 28 after the first treatment (Supplemental Figure S1A). The corresponding PD study indicated that daily administration of 20,000 U/kg of ASNaseQ59L was able to deplete plasma asparagine, whereas the dosage of 10,000 U/kg was not (Supplemental Figure S2). Those studies led to the selection of 20,000 U asparaginase activity per kg body weight (U/kg) as the dosage for further experiments.
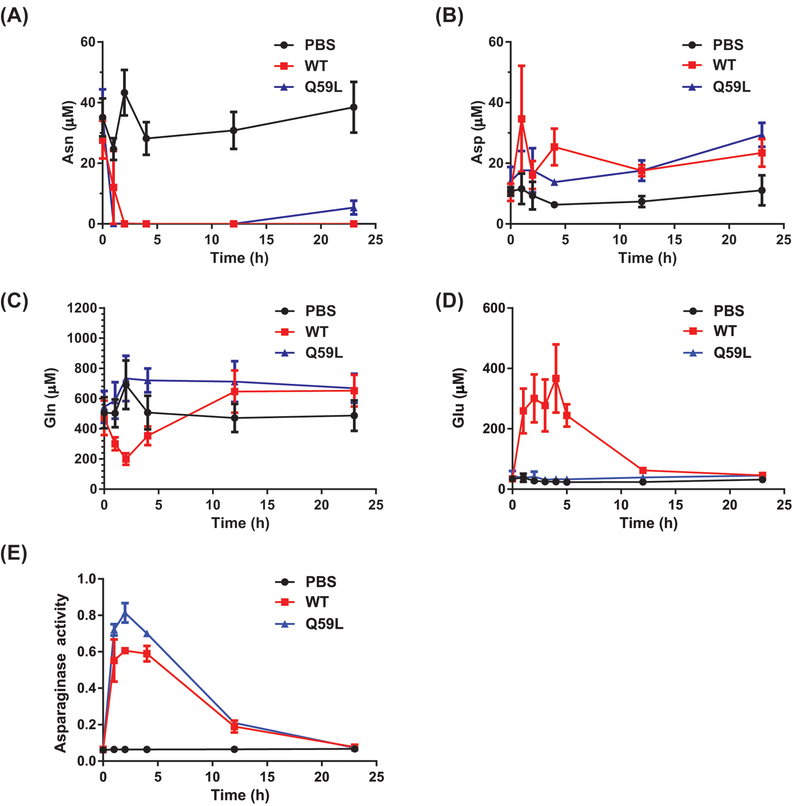
Pharmacodynamics and pharmacokinetics of ASNase variants in healthy NSG mice
We then compared the pharmacodynamics of ASNaseWT and ASNaseQ59L in healthy NSG mice. At a dose of 20,000 U/kg, both ASNaseWT and ASNaseQ59L depleted asparagine very quickly and maintained that depletion (p < 0.05 compared to PBS treatment, Supplemental Table 1) after 2 h and for at least 12 h after treatment (Figure 1A and Supplemental Figure S3A). Even at 23 h after treatment, plasma asparagine concentration was below the limit of quantitation (< 1 μM) in mice treated with ASNaseWT and very low (~ 5 μM) in those treated with ASNaseQ59L. The greater extent of asparagine depletion by ASNaseWT was presumably due to the additional depletion of glutamine, which is a substrate needed for synthesis of asparagine by ASNS in cells throughout the body. As expected, ASNaseWT and ASNaseQ59L treatment led to elevation of plasma aspartate concentration (from ~10 μM to ~25 μM), presumably due to conversion of asparagine to aspartate (Figure 1B and Supplemental Figure S3B). We did not observe a significant difference between asparagine and aspartate profiles following ASNaseWT treatment and ASNaseQ59L treatment (p > 0.05, Supplemental Table 1).
Figure 1. Pharmacokinetics and pharmacodynamics of ASNaseWT and ASNaseQ59L in vivo.
The pharmacodynamics of ASNaseWT and ASNaseQ59L in the plasma of non-tumor bearing NSG mice were determined by LC-MS/MS-based analysis of the amino acids (A) asparagine, (B) aspartate, (C) glutamine, and (D) glutamate. NSG mice (3 per group) were treated with PBS (negative control), 20,000 U/kg ASNaseWT, or 20,000 U/kg ASNaseQ59L by intraperitoneal injection. Time 0 measurements were made on samples collected immediately before injection. (E) The pharmacokinetics of ASNaseWT and ASNaseQ59L in plasma were determined by colorimetric assay of asparaginase activity. Error bars represent standard error.
As also expected, ASNaseQ59L treatmentdid not decrease plasma glutamine concentration compared with PBS treatment (p > 0.2, Supplemental Table 1, Figure 1C, and Supplemental Figure S3C). ASNaseWT, in contrast, decreased glutamine concentration significantly from ~600 μM (pre-treatment) to ~200 μM at two hours after treatment (p < 0.05, Supplemental Table 1, Figure 3C, and Supplemental Figure S3C), but that effect was short-lived; glutamine rapidly returned to baseline (or perhaps slightly elevated) concentration. The slightly increased glutamine level following ASNaseQ59L treatment was not statistically significant (p > 0.05, Supplemental Table 1).
Glutamate accumulated (ASNaseWT vs PBS, p < 0.05, Supplemental Table 1) commensurately with the decrease of glutamine within the first four hours but regressed to baseline concentration within eight hours (Figure 1D and Supplemental Figure S3D). Notably, no glutamate accumulation was detected following ASNaseQ59L treatment (ASNaseQ59L vs PBS, p > 0.1, Supplemental Table 1), illustrating the absence of compensatory reaction and confirming its glutaminase deficiency.
Next, to analyze ASNase pharmacokinetics, we measured asparaginase activity in the same plasma samples as were collected for the analysis of ASNase pharmacodynamics. The pharmacokinetics of ASNaseWT and ASNaseQ59L were not statistically different (ASNaseWT vs ASNaseQ59L, p > 0.05, Supplemental Table 1), but the maximal enzymatic activity (Cmax) of ASNaseWT was slightly lower than that of ASNaseQ59L; the Cmax of ASNaseWT and ASNaseQ59L occurred at two hours after administration and remained at 25% of maximum at twelve hours (Figure 1E). Notably, the ASNaseWT pharmacokinetics profile (Figure 1E) matched the glutamate pharmacodynamic profile (Figure 1D) and inversely matched that of glutamine (Figure 1C); rapid clearance of ASNase enzyme activity was associated with a rapid return of plasma glutamine concentration to baseline level. In contrast, the ASNaseQ59L pharmacokinetics profile matched the asparagine depletion profile (Figure 1A). Overall, the pharmacokinetic and pharmacodynamic results suggested that administration of 20,000 U/kg i.p. daily should provide adequate conditions for the comparison of ASNaseWT and ASNaseQ59L anticancer activity in vivo.
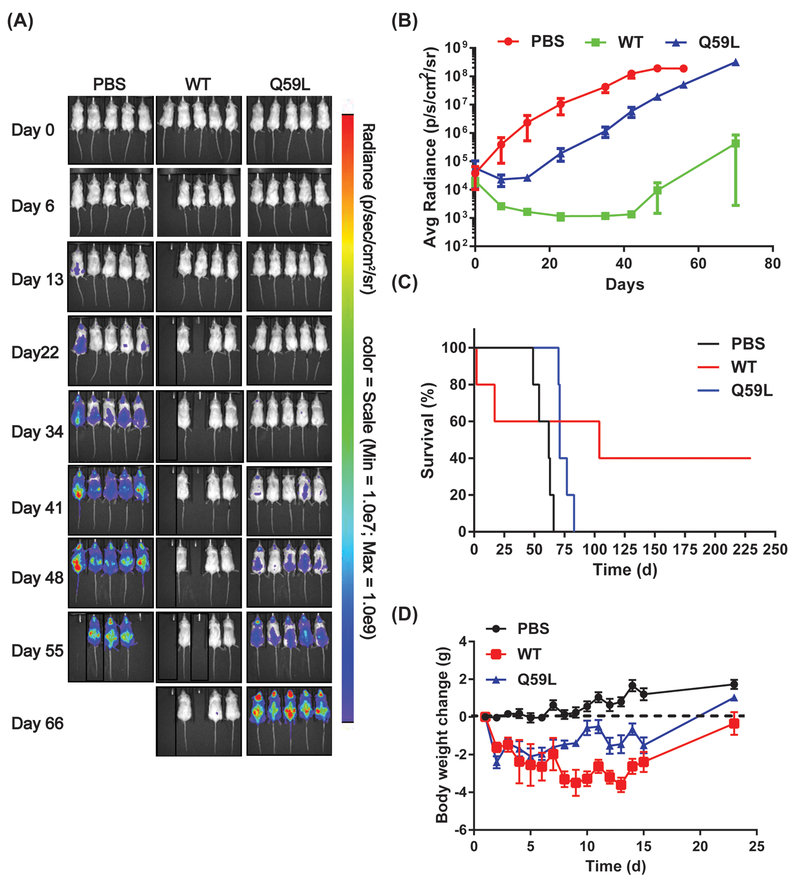
Asparaginase activity alone does not produce cytotoxic anticancer activity in vivo
We next tested the in vivo anticancer activity of ASNaseWT and ASNaseQ59L against the Sup-B15 leukemia model (4). Following 14 daily treatments at 20,000 U/kg administered i.p., ASNaseWT and ASNaseQ59L suppressed leukemia progression, whereas the PBS-treated group exhibited rapid progression (Figures 2A & 2B and Supplemental Figure S4). We continued to monitor leukemia burden and survival rate after cessation of treatment. ASNaseQ59L provided a growth delay of about 20 d (approximately 3 to 4 doubling times of the leukemia in mice) over the control group, whereas ASNaseWT yielded undetectable (background signal levels of) leukemia burden through the 66 days of imaging assessment (Figures 2A & 2B and Supplemental Figure S4). Strikingly, ASNaseWT extended survival to >100 d, with two of the mice showing no re-growth of this hard-to-cure leukemia through the time of sacrifice on Day 234. A third mouse responded well but showed a small region of bioluminescence in the late stages of imaging, suggesting recurrence of the leukemia, and it survived until Day 101 (Figure 2C). ASNaseWT and ASNaseQ59L were both toxic as reflected by the loss of body weight following drug treatment (Figure 2D and Supplemental Figure S5). That side effect was more severe in the ASNaseWT group (up to ~ 20% loss) than in the ASNaseQ59L group (up to ~10% loss). Overall, the data in Figure 2 indicate that ASNaseQ59L exhibited less toxic, but also less anticancer, activity than did ASNaseWT, which achieved results that approximate cure. It was unclear whether the early deaths of two mice from the ASNaseWT-treated group were caused by drug toxicity, but one of the two showed the largest early weight loss.
Figure 2. Anticancer activity of ASNaseWT and ASNaseQ59L in vivo.
(A) NSG mice (5 per group) xenografted with the luciferase-engineered leukemia cell line Sup-B15 were treated daily with the PBS negative control, 20,000 U/kg ASNaseWT, or 20,000 U/kg ASNaseQ59L for two weeks by intraperitoneal injection. Leukemia burden was monitored using bioluminescence imaging at the indicated time points. Day 0 is defined as one day before the first treatment. (B) Average bioluminescent signal in each treatment group as described for panel A. (C) Kaplan-Meier survival analysis of the mice in panel A. (D) The average of daily body weight loss of each group in panel A. Mice had unrestricted access to food and water. *Two mice died early, but it was not clear whether they died from ASNaseWT-related toxicity. Mean and SEM are shown.
DISCUSSION
We previously found that asparaginase activity played a role in the anticancer activity of ASNase in vitro, but glutaminase activity was dominant, especially in the case of ASNS-positive cell types (4). In the present study, we asked similar questions in vivo, intentionally biasing the case in favor of asparaginase activity by using xenografts of the ASNS-negative Sup-B15 line in NSG mice. In that model system, ASNaseQ59L did exert anticancer activity, but comparison with ASNaseWT showed that glutaminase activity was again dominant; ASNaseWT elicited a durable response (consistent with a cytotoxic mode of action) whereas ASNaseQ59L achieved only a fraction of the effect produced by ASNaseWT.
We previously found that ASNS expression (pre- and post-treatment) was a key mediator of resistance to ASNaseQ59L in vitro (4). It was, therefore, unexpected in this study to find that ASNaseQ59L lacked significant anticancer activity in vivo. That is, depletion of asparagine alone in vivo elicited growth inhibition but not a durable response. One hypothesis to explain the discrepancy between in vitro and in vivo results is that the leukemia cell microenvironment consists of ASNS-positive cell types capable of synthesizing and transporting asparagine to the extracellular environment for consumption by leukemia cells (15,16), thereby fueling resistance to ASNaseQ59L. In contrast, the in vitro cell culture models lack such additional sources of asparagine. Our results suggest that better in vitro models and/or a focus on in vivo data are critical for assessing the ability of glutaminase-deficient ASNase variants to overpower the supportive microenvironment.
Although our data support the conclusion that glutaminase activity is necessary for ASNase’s in vivo anticancer activity, significant side effects including pancreatitis, thrombosis, immunosuppression and impaired functions of liver, kidney or central nervous system, have been attributed to its glutaminase activity. Indeed, we observed greater weight loss in the ASNaseWT-treated group compared to the ASNaseQ59L-treated group during the two-week treatment. In addition, two out of five mice in the ASNaseWT-treated group died, but none died in the ASNaseQ59L-treated group during the first three-weeks. Aside from weight loss, we did not observe any obvious differences in the physical appearance or behavior of mice between two treatment groups, prompting a need for further studies to identify the causes of early death in the ASNaseWT-treated group. Additionally, there is a need to probe the metabolic pathways that are modulated downstream of the short-term glutamine decrease achieved by ASNaseWT in vivo. To overcome toxicities associated with ASNase glutaminase activity, combinations of ASNaseWT and glutaminase-deficient mutants such as ASNaseQ59L may be customized to achieve durable anticancer activity with minimal toxicity. In addition, monitoring glutamine concentration may be as important as monitoring asparagine concentration in patients during the course of ASNase therapy.
The new results presented here have potentially significant implications. First, attempts to achieve better clinical responses by increasing ASNase treatment intensity (and, therefore, glutaminase activity) are often overruled by evidence of increased toxicity (2,17) but the new results here are consistent with arguments in favor of increasing the glutaminase dosage for both ASNS-negative and ASNS-positive leukemia cell types. The single-agent ASNaseWT treatment regimen used in the current study thus achieved results similar to those reported with optimized Vincristine, deXamethasone, L-asparaginase (VXL) combination therapy in a patient-derived xenograft (PDX) model of acute lymphoblastic leukemia, whereby weekly administration of vincristine (0.15 mg/kg) together with weekday treatment with dexamethasone (5 mg/kg) and L-asparaginase (1,000 U/kg) for 4 weeks yielded 34-week survival of one of five mice engrafted with the chemosensitive T-ALL xenograft ALL-16 (18). On that note, given the single-agent activity observed here for ASNaseQ59L, further in vivo studies to assess Q59L’s potential in the VXL regimen are warranted.
Another recently published report indicated that a low-glutaminase mutant of Erwinia chrysanthemi ASNase (a different backbone than the Escherichia coli ASNase used in the present studies), retained anticancer activity in vivo (6). Specifically, with 14-day and 29-day study designs, a low-glutaminase ASNase mutant yielded anticancer activity in the short-term. The new results presented here using a glutaminase-deficient variant of ASNase with even lower relative glutaminase activity (< 0.2% of WT) provide critical additional information. In our extended survival analysis, glutaminase-deficient ASNaseQ59L was insufficiently active to prevent recurrence of the leukemia. In contrast, ASNaseWT at the same dose in terms of asparaginase activity, yielded a durable response, with two of the mice surviving until sacrifice at day 234. Overall, the results presented here indicate that ASNase glutaminase activity is a key component, although not the only component, of the mechanism of action of ASNase.
Supplementary Material
ACKNOWLEDGEMENTS
This work was supported in part by U.S. National Cancer Institute (NCI) grant numbers CA143883 (J.N. Weinstein), CA083639 (J.N. Weinstein), CA235510 (J.N. Weinstein), and CA016672 (J.N. Weinstein and P.L. Lorenzi); Cancer Prevention and Research Institute of Texas grant number RP130397 (J.N. Weinstein and P.L. Lorenzi); NIH high-end instrument grant 1S10OD012304–01 (P.L. Lorenzi), the Chapman Foundation, and the Michael and Susan Dell Foundation (honoring Lorraine Dell). SNL is a multi-mission laboratory managed and operated by NTESS for the US DOE, NNSA under contract DE-NA-0003525 (S.B. Rempe). Sup-B15-luc cells were a kind gift from Michael Jensen (Seattle Children’s Research Hospital).
Financial Support: SBR: US DOE NNSA contract DE-NA-0003525; MK: ; JNW: NIH/NCI grant numbers CA143883, CA083639, and CA016672, CPRIT grant number RP130397, the Chapman Foundation, and the Michael and Susan Dell Foundation (honoring Lorraine Dell); PLL: NIH/NCI grant numbers CA016672, 1S10OD012304–01, and CPRIT grant number RP130397.
Footnotes
Conflict of Interest Disclosure Statement: PLL and JNW have patents and receive royalties related to ASNS as a predictive biomarker of response to L-asparaginase. PLL serves as a consultant to Erytech Pharma regarding L-asparaginase pharmacology.
REFERENCES
- 1.Wu MC, Arimura GK, Yunis AA. Mechanism of sensitivity of cultured pancreatic carcinoma to asparaginase. Int J Cancer 1978;22(6):728–33. [DOI] [PubMed] [Google Scholar]
- 2.Kafkewitz D, Bendich A. Enzyme-induced asparagine and glutamine depletion and immune system function. Am J Clin Nutr 1983;37(6):1025–30. [DOI] [PubMed] [Google Scholar]
- 3.Silverman LB, Gelber RD, Dalton VK, Asselin BL, Barr RD, Clavell LA, et al. Improved outcome for children with acute lymphoblastic leukemia: results of Dana-Farber Consortium Protocol 91–01. Blood 2001;97(5):1211–8. [DOI] [PubMed] [Google Scholar]
- 4.Chan WK, Lorenzi PL, Anishkin A, Purwaha P, Rogers DM, Sukharev S, et al. The glutaminase activity of l-asparaginase is not required for anticancer activity against ASNS-negative cells. Blood 2014;123(23):3596–606 doi 10.1182/blood-2013-10-535112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anishkin A, Vanegas JM, Rogers DM, Lorenzi PL, Chan WK, Purwaha P, et al. Catalytic Role of the Substrate Defines Specificity of Therapeutic l-Asparaginase. J Mol Biol 2015;427(17):2867–85 doi 10.1016/j.jmb.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 6.Nguyen HA, Su Y, Zhang JY, Antanasijevic A, Caffrey M, Schalk AM, et al. A Novel l-Asparaginase with low l-Glutaminase Coactivity Is Highly Efficacious against Both T- and B-cell Acute Lymphoblastic Leukemias In Vivo. Cancer Res 2018;78(6):1549–60 doi 10.1158/0008-5472.CAN-17-2106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Offman MN, Krol M, Patel N, Krishnan S, Liu J, Saha V, et al. Rational engineering of L-asparaginase reveals importance of dual activity for cancer cell toxicity. Blood 2011;117(5):1614–21 doi 10.1182/blood-2010-07-298422. [DOI] [PubMed] [Google Scholar]
- 8.Parmentier JH, Maggi M, Tarasco E, Scotti C, Avramis VI, Mittelman SD. Glutaminase activity determines cytotoxicity of L-asparaginases on most leukemia cell lines. Leukemia research 2015;39(7):757–62 doi 10.1016/j.leukres.2015.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tong WH, Pieters R, Hop WC, Lanvers-Kaminsky C, Boos J, van der Sluis IM. No evidence of increased asparagine levels in the bone marrow of patients with acute lymphoblastic leukemia during asparaginase therapy. Pediatr Blood Cancer 2013;60(2):258–61 doi 10.1002/pbc.24292. [DOI] [PubMed] [Google Scholar]
- 10.Avramis VI, Panosyan EH. Pharmacokinetic/pharmacodynamic relationships of asparaginase formulations: the past, the present and recommendations for the future. Clin Pharmacokinet 2005;44(4):367–93 doi 10.2165/00003088-200544040-00003. [DOI] [PubMed] [Google Scholar]
- 11.Ding Y, Li Z, Broome JD. Epigenetic changes in the repression and induction of asparagine synthetase in human leukemic cell lines. Leukemia 2005;19(3):420–6 doi 10.1038/sj.leu.2403639. [DOI] [PubMed] [Google Scholar]
- 12.Iwamoto S, Mihara K, Downing JR, Pui CH, Campana D. Mesenchymal cells regulate the response of acute lymphoblastic leukemia cells to asparaginase. J Clin Invest 2007;117(4):1049–57 doi 10.1172/JCI30235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ehsanipour EA, Sheng X, Behan JW, Wang X, Butturini A, Avramis VI, et al. Adipocytes cause leukemia cell resistance to L-asparaginase via release of glutamine. Cancer Res 2013;73(10):2998–3006 doi 10.1158/0008-5472.CAN-12-4402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jones L, Richmond J, Evans K, Carol H, Jing D, Kurmasheva RT, et al. Bioluminescence Imaging Enhances Analysis of Drug Responses in a Patient-Derived Xenograft Model of Pediatric ALL. Clin Cancer Res 2017;23(14):3744–55 doi 10.1158/1078-0432.CCR-16-2392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Avramis VI. Asparaginases: biochemical pharmacology and modes of drug resistance. Anticancer Res 2012;32(7):2423–37. [PubMed] [Google Scholar]
- 16.Ehsanipour EA, Sheng X, Behan JW, Wang X, Butturini A, Avramis VI, et al. Adipocytes Cause Leukemia Cell Resistance to L-Asparaginase via Release of Glutamine. Cancer Res 2013. doi 10.1158/0008-5472.CAN-12-4402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lebovic R, Pearce N, Lacey L, Xenakis J, Faircloth CB, Thompson P. Adverse effects of pegaspargase in pediatric patients receiving doses greater than 3,750 IU. Pediatr Blood Cancer 2017;64(10) doi 10.1002/pbc.26555. [DOI] [PubMed] [Google Scholar]
- 18.Szymanska B, Wilczynska-Kalak U, Kang MH, Liem NL, Carol H, Boehm I, et al. Pharmacokinetic modeling of an induction regimen for in vivo combined testing of novel drugs against pediatric acute lymphoblastic leukemia xenografts. PLoS One 2012;7(3):e33894 doi 10.1371/journal.pone.0033894. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.