Abstract
Objective:
To compare nurse preparedness and quality of patient handoff during interfacility transfers from a pre-transfer emergency department to a Pediatric Intensive Care Unit (PICU) when conducted over telemedicine versus telephone.
Design:
Cross-sectional nurse survey linked with patient electronic medical record data using multivariable, multilevel analysis.
Setting:
Tertiary PICU within an academic children’s hospital.
Participants:
PICU nurses who received a patient handoff between October 2017 and July 2018.
Interventions:
None.
Main Results and Measurements:
Among 239 eligible transfers, 106 surveys were completed by 55 nurses (44% survey response rate). Telemedicine was used for 30 (28%) handoffs and telephone was used for 76 (72%) handoffs. Patients were comparable with respect to age, gender, race, primary spoken language and insurance, but handoffs conducted over telemedicine involved patients with higher illness severity as measured by the Pediatric Risk of Mortality (PRISM III) score (4.4 versus 1.9, p=0.05). After adjusting for PRISM III score, survey recall time, and residual clustering by nurse, receiving nurses reported higher preparedness (measured on a 5-point adjectival scale) following telemedicine handoffs compared to telephone handoffs (3.4 versus 3.1, p=0.02). There were no statistically significant differences in both bivariable and multivariable analyses of handoff quality as measured by the Handoff Clinical Evaluation Exercise. Handoffs using telemedicine were associated with increased number of I-PASS components (3.3 versus 2.8, p=0.04), but this difference was not significant in the adjusted analysis (3.1 versus 2.9, p=0.55).
Conclusions:
Telemedicine is feasible for nurse-to-nurse handoffs of critically ill patients between pre-transfer and receiving facilities, and may be associated with increased perceived and objective nurse preparedness upon patient arrival. Additional research is needed to demonstrate that telemedicine during nurse handoffs improves communication, decreases preventable adverse events and impacts family and provider satisfaction.
Keywords: Nursing, Telemedicine, Patient Handoff, Pediatric Intensive Care Unit, Emergency Service, Interdisciplinary Communication
INTRODUCTION
Breakdowns and inefficiencies in communication during a patient handoff are strong contributors to preventable adverse events (1–3). In particular, communication breakdowns may be compounded during interfacility transfers, or transitions in care between different health care facilities, due to the complexity of the process, differences in education and training, differences in provider culture, and variability in approach to patient care (4, 5). Handoffs from pre-transfer (referring) emergency departments (EDs) to post-transfer (receiving) inpatient wards may have inaccuracies describing the patient (6) or may emphasize information that has less perceived utility to the receiving provider (7, 8). This may lead to mismatches in resource preparation and utilization upon admission and ultimately may impact patient outcomes. This is particularly relevant for the pediatric population since pediatric patients are transferred at higher rates than adults (9).
Using telemedicine, either in conjunction with or instead of a telephone call, has the potential to improve nurse handoffs and care coordination between pre-transfer EDs and post-transfer inpatient wards (10). Prior studies on interfacility physician communication—most commonly physician consultations to pre-transfer EDs—indicate that telemedicine is associated with improved clinical measures (11, 12), decreased transfer rates (13, 14), decreased medication errors (15), improved communication (16) and improved patient assessment accuracy (6). To the best of our knowledge, no study has evaluated the use of telemedicine for interfacility nurse handoffs (17); therefore, we implemented and evaluated an interfacility telemedicine nurse handoff program. The additional interactive visual information from telemedicine may improve the receiving nurse’s ability to assess the patient’s severity of illness prior to transfer and may improve the development of a shared mental model of the patient between the two nursing teams. Telemedicine may better replicate face-to-face communication, which is an important factor for improving handoffs (18, 19). In addition, telemedicine enables the receiving nurse to interact with the patient and the patient’s family to establish a provider-patient relationship before arrival.
The primary aim of this study was to evaluate the association between handoffs using telemedicine and nurse preparedness among interfacility transfers to a pediatric intensive care unit (PICU). The secondary aim of this study was to evaluate the association between nurse handoffs using telemedicine and handoff quality. We hypothesized that nurse handoffs using telemedicine would be associated with higher preparedness and higher handoff quality in comparison to handoffs using telephone, the current standard of care.
METHODS
We conducted a single-center, cross-sectional nurse survey linked with patient and hospital data. During this study, there were no standardized handoff protocols used for interfacility nurse handoffs. This study was approved by the University of California Davis Institutional Review Board.
Setting and Telemedicine Description:
The University of California Davis Health (UCDH) receives approximately 400 transfers to its 24-bed tertiary care PICU from approximately 50 general and community hospitals every year. Among these pre-transfer hospitals, 26 are part of a telemedicine network with the UCDH PICU. The telemedicine program is used to provide virtual bedside consultations to critically ill children presenting to the pre-transfer ED and uses pole-mounted turnkey, high definition videoconferencing units with remote pan-tilt-zoom capabilities in the EDs. In the UCDH PICU, providers are able to initiate consultations and handoff using standard videoconferencing software and webcams installed on several computers throughout the PICU. At each of these stations, laminated reference sheets summarize telemedicine set-up, camera functions and basic troubleshooting. Despite common use among physicians, nurses had not routinely used telemedicine for interfacility handoffs before this project.
For nurse training, a train-the-trainer model was initially used, where selected nurse champions could teach other nurses how to use telemedicine and be a resource to other nurses. Three months before initiating data collection, two study researchers trained 10 volunteer nurse champions—5 from day-shift and 5 from night-shift—how to initiate and troubleshoot telemedicine. After identifying a decrease in the use of telemedicine after the first few months of the study, a larger, more comprehensive training approach was initiated to increase individual nurse familiarity setting up telemedicine independently from the nurse champions. The first author conducted in-service training over a week to provide a brief overview of telemedicine and technical support, including nurse champions and a 24/7 help-line. During this one-week period, 93 of the 119 nurses (78.8%) were trained, as well as all five of the hospital unit service coordinators.
Survey Implementation and Participants:
For a patient transfer to meet eligibility for the study, the PICU nurse must have both received handoff from the pre-transfer ED nurse and admitted the patient upon arrival during his/her same shift. The patient must have been less than 18 years old and must have been a direct admission to the PICU from the pre-transfer ED. Nurses were asked to complete the survey, described below, at the end of their shift after fully admitting the patient. Eligible transfers were identified through transfer logs in the electronic medical record (EMR). Nurses who did not complete a survey were emailed a reminder about the handoff survey within a week of the transfer. The survey was available in paper format in the PICU and in electronic format using Qualtrics online survey platform. Surveys completed more than 14 days after the transfer were excluded. Responding nurses were given a $5 Amazon gift card.
Outcomes:
The 36-item survey was developed iteratively by nurse champions and the research team. At the start of this study, there were no previously published instruments to measure the degree of nurse preparedness to admit a patient, the study’s primary outcome, thus, the research team developed the question “How prepared did you feel to admit this patient in comparison to previous patients you have admitted?” on a 5-point bipolar adjectival scale (Appendix 1). Nurses were also asked about their perceived change in patient illness severity between the time of handoff and upon patient arrival and the need for unanticipated medication changes, equipment changes, and changes in nursing staff to assist with the admission (Appendix 1). Using data abstracted from the EMR, the time elapsed from patient arrival until clinical nursing events was measured to serve as more objective measures of nurse preparedness: first recorded vitals, first recorded extended charting (which includes items such as vitals, Glasgow Coma Scale), and first text of the nursing admission chart note.
The secondary outcome was handoff quality as measured by the Handoff Clinical Evaluation Exam (Handoff CEX) (20) and by the total number of completed standardized handoff components in I-PASS (2). Used to evaluate both physician (20) and nurse handoffs (21), the Handoff CEX contains seven axes with 9-item scales, which results in a total score ranging from 7 to 54. The standardized handoff components of I-PASS include: illness severity, an action list, situation awareness/contingency planning and synthesis by receiver (2).
Other Variables:
The exposure variable of interest was the modality used for handoff: telemedicine versus telephone. If the handoffs were conducted using telephone, the survey asked for the reason for using telephone instead of telemedicine to gain insight into feasibility. Questions were also included from the technology acceptance model framework (22), with minor modifications, on perceived usefulness, perceived ease of use and intention to use telemedicine in the future. This was to assess nursing perceptions on technology as a possible confounder. The survey included additional questions on other possible nurse-level confounders, including prior telemedicine use before the handoff; prior PICU telemedicine training before the handoff; shift workload, measured indirectly by the number of patients in the nurse’s care at the time of transfer; usual work shift (‘days’, ‘nights’); and the years of experience as a PICU nurse. The time between handoff and patient arrival was calculated using the survey answer to “handoff time” and EMR timestamps, respectively. Other patient-level data such as age, gender, race, primary encounter diagnosis, illness severity as measured by the Pediatric Risk of Mortality (PRISM III) and encounter data such as transfer day of week and transport vehicle (ambulance, helicopter) were obtained from the internal Virtual PICU Systems database and linked by medical record number and admission date.
Study Size:
Prior to conducting the study, sample size calculations were conducted based on a 2-point difference effect size based on a 5-point adjectival scale with a standard deviation of 2.5 points. Assuming a power of 90% and alpha of 5%, at least 34 transfers would be needed in each group with equal allocation. With a more realistically anticipated ratio of one telemedicine to three telephone handoffs, and assuming a 15% rate of incomplete data, 28 telemedicine handoffs and 81 telephone handoffs would be needed for a total sample size of 109.
Statistical Methods:
All data linkages and statistics were completed in the R environment, version 3.4.4 (23). Adjectival-scale variables were encoded as numeric variables and treated as continuous variables. For bivariate comparisons, chi-square tests or Fisher exact test for categorical variables were used as necessary, and t-tests for continuous variables. Intraclass correlation was calculated in order to assess clustering by the bedside nurse, admitting physician and pre-transfer hospital. For both aims, covariates of interest were considered potential confounders if they were associated with handoff mode and associated with preparedness with a p-value less than a conservative threshold of 0.2. Potential confounders were included in the final model if they resulted in a 10% or greater change in the beta coefficient for variable handoff mode. Multilevel models were built using the package nlme (24) and distances between pre-transfer hospital and UCDH were calculated with geosphere using a ‘birds-eye’ Haversine formula between two sets of coordinates (25). The robust (sandwich) estimator in the package clubSandwich estimated corrected standard errors to protect against heteroscedasticity and model misspecification (26). Finally, sensitivity analyses were conducted by restricting the sample to transfers that originated from telemedicine-capable hospitals. This was done to account for the possibility that EDs with telemedicine capabilities would be inherently different than hospitals without telemedicine.
RESULTS
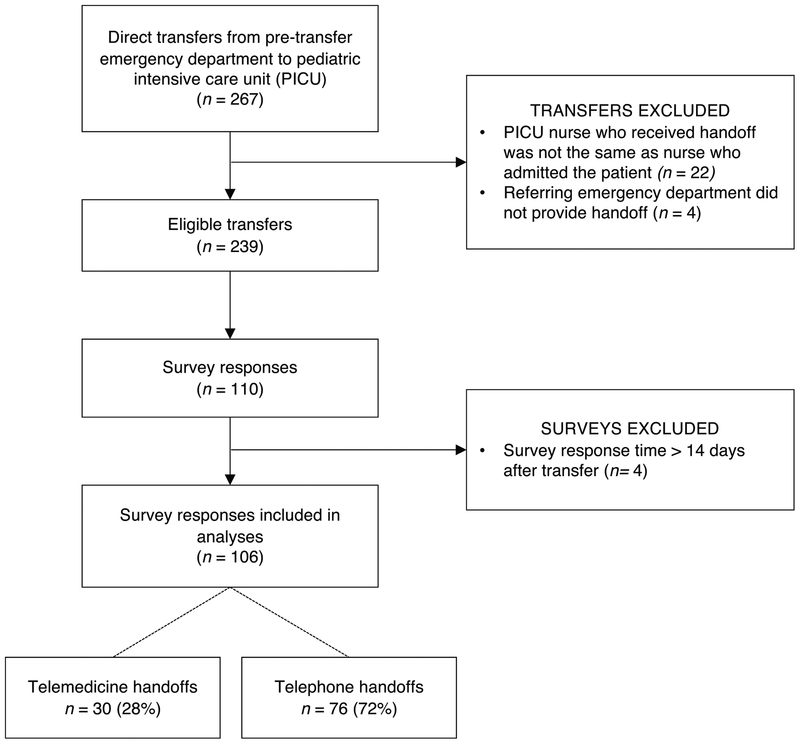
From October 1st, 2017 until July 1st, 2018, there were 239 eligible transfers from pre-transfer EDs that resulted in a direct PICU admission. Out of the 239 eligible transfers, 106 surveys were completed by 55 nurses in 14 days or less, for a survey response rate of 44% (Figure 1). There were two handoffs that were initiated over the telephone but switched to telemedicine and there was one handoff that was initiated over telemedicine, but due to connection issues, was conducted over the telephone. There were no statistically significant differences in the responding nurses’ years of experience as a PICU nurse or usual work shift (day versus night). Similarly, there were no differences among nurses’ technology acceptance scores between the telemedicine and telephone cohorts. Being a telemedicine nurse champion and receiving the telemedicine training prior to handoff did not result in differences in the frequencies of telephone or telemedicine handoffs conducted.
Figure 1.
Response rate flow chart.
Among the handoffs conducted by telemedicine and telephone, there were no statistically significant differences in patient age, gender, race, primary spoken language, insurance, and primary encounter diagnosis (Table 1). Handoffs conducted over telemedicine included patients with higher PRISM III Scores (4.4 versus 1.9, p=0.05). The transfers came from 24 (pre-transfer) hospitals across Northern California. The time between handoff and patient arrival was longer among handoffs conducted using telemedicine in comparison to handoffs over telephone (101 minutes versus 74 minutes, p=0.02). Despite this time difference, the average distances between pre-transfer hospital and UCDH were similar (74.6 kilometers versus 76.1 kilometers, p > 0.9).
Table 1.
Patient, Nurse, Pre-Transfer Hospital and Handoff Characteristics by Handoff Mode
| Variable | Telemedicine N=30 |
Telephone N=76 |
p-value |
|---|---|---|---|
| Patient Characteristics | |||
| Patient age in years, mean (SD) | 6.2 (5.9) | 5.2 (5.3) | 0.40 |
| Female gendera, n (%) | 14 (48%) | 26 (38%) | 0.45 |
| Race, n (%) | |||
| White | 10 (33%) | 22 (29%) | 0.55 |
| Hispanic or Latino | 6 (20%) | 24 (32%) | |
| Black or African American | 2 (7%) | 4 (5%) | |
| Unspecified or Unknown | 3 (10%) | 12 (16%) | |
| Other/Mixed | 9 (30%) | 14 (18%) | |
| Primary spoken language, n (%) | |||
| English | 22 (79%) | 63 (83%) | 0.22 |
| Spanish | 2 (7%) | 7 (9%) | |
| Other language or unknown | 6 (20%) | 6 (8%) | |
| Public insurance, including Medicaid and militarya, n (%) | 21 (72%) | 51 (74%) | > 0.9 |
| Primary encounter diagnosisa, n (%) | |||
| Respiratory | 13 (45%) | 31 (51%) | 0.85 |
| Neurologic | 3 (10%) | 7 (10%) | |
| Infectious | 2 (7%) | 7 (10%) | |
| Other | 11 (37%) | 20 (26%) | |
| PRISM III Scorea,b, mean (SD) | 4.4 (6.5) | 1.9 (3.6) | 0.05 |
| Nurse Characteristics | |||
| PICU nursing experience in years, mean (SD) | 4.0 (5.1) | 3.7 (3.9) | 0.74 |
| Total technology acceptance model scorec, mean (SD) | 18.3 (2.7) | 17.2 (3.1) | 0.10 |
| Perceived usefulness, mean (SD) | 6.3 (1.0) | 6.0 (1.2) | 0.21 |
| Perceived ease of use, mean (SD) | 6.0 (1.0) | 5.5 (1.2) | 0.05 |
| Intention to use in future, mean (SD) | 6.1 (1.1) | 5.8 (1.2) | 0.25 |
| Usual work shift: nights (7PM – 7AM) | 15 (50%) | 39 (52%) | > 0.9 |
| Trained in telemedicine before encounter, n (%) | 17 (57%) | 36 (47%) | 0.52 |
| Telemedicine nurse champion, n (%) | 6 (20%) | 14 (18%) | > 0.9 |
| Number of patients in nurse care before patient arrival, n (%) | |||
| 0 | 5 (17%) | 11 (14%) | 0.75 |
| 1 | 23 (77%) | 62 (82%) | |
| 2 | 2 (7%) | 3 (4%) | |
| Pre-Transfer Hospital Characteristics | |||
| Telemedicine capable, n (%) | 30 (100%) | 64 (84%) | 0.02 |
| Distance from UCDH in kilometers, mean (SD) | 74.6 (81.9) | 76.1 (76.7) | > 0.9 |
| Handoff Characteristics | |||
| Time from handoff to patient arrival in minutesd, mean (SD) | 101 (52) | 74 (45) | 0.02 |
| Survey recall time in days, mean (SD) | 1.7 (3.0) | 3.4 (3.1) | 0.01 |
| Duration of handoff in minutese, mean (SD) | 8.9 (4.5) | 7.6 (3.8) | 0.16 |
| Weekend admission, n (%) | 7 (23%) | 23 (30%) | 0.64 |
| Transport vehiclef, n (%) | |||
| Ambulance | 17 (61%) | 53 (72%) | 0.53 |
| Helicopter | 11 (37%) | 19 (28%) |
Frequency missing: 2 (7%) in Telemedicine group, 7 (9%) in Telephone group.
Pediatric Risk of Mortality III Score, a pediatric physiology-based measure for severity of illness
The technology acceptance model items were worded specifically for use of telemedicine in nurse handoffs. The score is an average of two questions, both of which had a 7-item Likert scale. Frequency missing: 4 (13%) in Telemedicine group, 8 (11%) in Telephone group.
Frequency missing: 1 (3%) in Telemedicine group and 6 (8%) in Telephone group.
Handoff duration does not measure time for connection delays.
Frequency missing: 3 (10%) in Telemedicine, 8 (11%) in Telephone group.
On an adjectival scale from 1 to 5, nurses rated being more prepared than usual after conducting handoff using telemedicine compared to handoff using telephone (3.4 versus 3.0, p=0.01). There were similar changes in perception of illness severity in each group (3.1 versus 2.9, p=0.19). There were no statistically significant differences in unanticipated medication changes (18% versus 12%, p=0.51), equipment changes (25% versus 20%, p=0.81) or staffing changes (46% versus 39%, p=0.66) upon patient arrival to the PICU between the cohorts when telemedicine was used for handoff compared to when telephone was used. For the objective time measures, less time elapsed from patient arrival to the specified clinical events among transfers that used telemedicine for handoffs compared to those that used the telephone; however, these differences were not statistically significant (Table 2).
Table 2.
Nurse Preparedness at Patient Arrival by Handoff Modea
| Variable | Telemedicine N=28 |
Telephone N=69 |
p-value |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| Nurse preparedness | 3.4 (0.7) | 3.0 (0.6) | 0.01 |
| Change in perceived patient illness severity at arrival versus handoff | 3.1 (0.8) | 2.9 (0.9) | 0.19 |
| Unanticipated changes at patient arrival | n (%) | n (%) | |
| Medication changes | 5 (18%) | 8 (12%) | 0.51 |
| Equipment changes | 7 (25%) | 14 (20%) | 0.81 |
| Nursing staff changes | 13 (46%) | 27 (39%) | 0.66 |
| Time in minutes from patient arrival until: | Mean (SD) | Mean (SD) | |
| First recorded vitals | 8.0 (10.0) | 9.8 (13.2) | 0.48 |
| First recorded extended chartingb | 9.0 (10.2) | 14.5 (18.5) | 0.08 |
| First chart notec | 131 (89) | 144 (142) | 0.61 |
These data exclude patients with missing PRISM III data: 2 (7%) in Telemedicine group, 7 (9%) in Telephone group.
Includes measurements beyond vitals such as Glasgow Coma Scale. Frequency missing: 3 (14%) in Telemedicine group and 3 (4%) in Telephone group.
Frequency missing: 3 (11%) in Telemedicine group and 8 (11%) in Telephone group.
Handoffs conducted using telemedicine tended to have higher handoff quality scores, but these differences were not statistically significant for the Handoff CEX (Table 3). Handoffs using telemedicine were associated with increased number of I-PASS components (3.3 versus 2.8, p=0.04). Among handoffs conducted using telemedicine, nurses were more likely to communicate with the patient’s family (63% versus 1%, p < 0.01) and the transport team (33% versus 12%, p=0.02) during the patient handoff.
Table 3.
Handoff Quality and Other Handoff Events by Handoff Mode
| Variable | Telemedicine N=30 |
Telephone N=76 |
p-value |
|---|---|---|---|
| Handoff Clinical Evaluation Exercise | Mean (SD) | Mean (SD) | |
| Total Handoff Clinical Evaluation Exercise Score | 40.9 (7.9) | 38.3 (9.1) | 0.16 |
| Setting | 6.6 (1.9) | 6.6 (1.7) | |
| Organization and Efficiency | 6.3 (1.4) | 6.1 (1.8) | |
| Communication Skills | 7.0 (1.4) | 6.6 (1.7) | |
| Content | 6.7 (1.4) | 6.1 (1.8) | |
| Clinical Judgment | 6.8 (1.3) | 6.2 (1.6) | |
| Professionalism | 7.4 (1.4) | 6.8 (1.9) | |
| Overall Quality | 6.9 (1.0) | 6.4 (1.7) | |
| I-PASS | |||
| Number of I-PASS Components | 3.3 (1.0) | 2.8 (1.1) | 0.04 |
| n (%) | n (%) | ||
| Illness Severity | 27 (90%) | 66 (87%) | |
| Patient Summary | 30 (100%) | 74 (97%) | |
| Action List | 16 (53%) | 24 (32%) | |
| Situational Awareness & Contingency Plans | 5 (17%) | 17 (22%) | |
| Synthesis by Receiving Nurse | 19 (63%) | 30 (39%) | |
| Other Handoff Components | n (%) | n (%) | |
| Reason for Transfer | 26 (87%) | 71 (93%) | 0.27 |
| Exam Findings/Lab Results | 25 (83%) | 59 (78%) | 0.70 |
| Opportunity for Receiving Nurse to Ask Outside Nurse Questions | 31 (100%) | 71 (93%) | 0.32 |
| Other Handoff Events | n (%) | n (%) | |
| Communication with the Patient’s Family | 19 (63%) | 1 (1%) | < 0.01 |
| Communication with the Transport Team | 10 (33%) | 9 (12%) | 0.02 |
Multivariable Models – Nurse Preparedness:
The following variables were statistically associated with both handoff mode and preparedness (threshold p < 0.2): survey recall time, illness severity (PRISM III Score) and total technology acceptance score. Time from handoff to patient arrival was not associated with preparedness. When evaluating for changes in beta, survey recall time and PRISM III resulted in beta-coefficient changes greater than 10% whereas the total technology acceptance score did not. The intra-class correlation was 29.4% for the receiving bedside nurse, smaller than 0.01% for the admitting physician and smaller than 0.01% for pre-transfer hospital. The final multivariable model adjusted for PRISM III score and survey recall time and included a random intercept for residual individual nurse effects. As shown in Table 4, handoffs conducted using telemedicine were significantly associated with higher nurse preparedness scores (3.4 versus 3.1 points, p=0.02) after multivariable adjustment.
Table 4.
Adjusted Model for Nurse Preparednessa
| Variable | Beta Coefficient (95% CI) | Standard Error | p-value |
|---|---|---|---|
| Handoff Mode; Telemedicine | 0.34 (0.07–0.61) | 0.13 | 0.02 |
| Survey Recall Time | −0.01 (−0.05–0.02) | 0.02 | 0.37 |
| PRISM III Score | 0.006 (−0.05–0.06) | 0.02 | 0.81 |
| Intercept | 3.07 (2.86–3.30) | 0.10 | <0.001 |
Linear multi-level model with nurse as a random intercept and nurse preparedness as the outcome. This model excludes patients with missing PRISM III scores and reflects the same patients in Table 2.
Multivariable Models – Handoff Quality:
For both Handoff CEX Score and total I-PASS components there was clustering at the receiving nurse level which corresponded to 53% and 41% of the variation, respectively. For Handoff CEX, admitting physician and pre-transfer hospital both corresponded to less than 0.01% of the variation. For total I-PASS components, intra-class correlation was 1.7% for the admitting physician and 3.7% for pre-transfer hospital. In the final Handoff CEX Score multivariable model, handoff modality (telemedicine versus telephone) was not significantly different after adjusting for survey recall time and including a random intercept for the nurse. For the I-PASS model development, two variables met the criteria for confounder consideration: survey recall time and handoff duration. In the final I-PASS multivariable model, handoff modality was not statistically significantly different (3.1 versus 2.9, p=0.55) after adjusting for survey recall time and handoff duration and including a random intercept for the nurse.
Additional analyses:
As a sensitivity analysis, the sample was restricted to transfers that originated from only telemedicine-capable hospitals and had VPS data. After removing the 11 telephone controls hospitals without telemedicine-capabilities, handoffs conducted using telemedicine were still significantly associated with higher scores of nurse preparedness after patient arrival (3.38 versus 3.04, p=0.02) while adjusting for PRISM III score, survey recall time and a random intercept for the receiving nurse.
Among the 64 telephone handoffs from telemedicine-capable hospitals where telemedicine was not used, more than half (n=35, 55%) of the receiving nurses reported later that they did not remember that telemedicine was an option for the handoff. Fifteen nurses (23%) tried to offer telemedicine, but the ED nurse from the pre-transfer hospital declined to use telemedicine on 7 occasions (9%) or the ED nurse called to give handoff after the patient had left on 8 occasions (14%). Some receiving nurses noted they were busy (“[M]y other patient had me busy so when the [Outside Hospital] called for report, it was easiest to take it that way, rather than move to a computer with telemedicine”) or that the timing was awkward (“Report was called right at change of shift, and the dayshift [nurse] was waiting for me to give report on my second patient,” “transport had arrived, patient being prepared for transport.”)
DISCUSSION
This study evaluated nurse handoffs using telemedicine from pre-transfer EDs to an academic PICU and compared them to handoffs conducted over telephone. Use of telemedicine seems to be associated with significantly higher nurse perceived preparedness upon patient arrival. Other objective measures of preparedness, such as time between patient arrival and the time to the first entered vitals, were shorter after having received handoff using telemedicine. However, there were no statistically significant differences in either handoff quality as measured by the handoff CEX or handoff quality as measured by I-PASS component scores. Finally, this study determined that telemedicine is feasible for nurse-to-nurse handoffs during interfacility transfers and is sometimes considered a preferred communication modality.
To the best of our knowledge, there have not been any studies describing or evaluating the use of telemedicine to facilitate nurse handoffs (17, 27). While other studies have examined healthcare provider preparedness as a clinical outcome, comparisons are difficult given the lack of validated objective or self-reported measures (28, 29). This study used both subjective and objective measures to quantify nurse preparedness during an interfacility patient handoff. Measures such as the time from patient arrival to definitive nursing documentation were extractable from the EMR and may be less biased than subjective measures (30). Additional work is needed to standardize the evaluation of preparedness after handoff and how these measures impact the reliability and validity of indirect, objective measures.
Compared to telephone handoffs, handoffs conducted using telemedicine may be more similar to face-to-face communication. This is important, because face-to-face bedside handoffs are associated with improved staff, patient and family satisfaction in several studies as well as a systematic review (19). The mean time between the time of handoff and patient arrival was longer among telemedicine handoffs, which is likely because telemedicine handoffs occurred earlier; telemedicine handoffs typically occurred while the patient was still present at the pre-transfer hospital whereas telephone handoffs often occur after the patient left the pre-transfer ED. While this study did not find statistically significant differences between the number of I-PASS components during handoffs, some components were more commonly discussed overall (illness severity, patient summary) and are similar to another study investigating physician-to-physician interfacility handoffs (31).
Our study has several limitations. The intervention was not blinded, and in combination with reporting biases inherent with survey responses, our results could have been biased favoring telemedicine handoffs. To address this, the research team took measures to ensure participant confidentiality and neutral language on the survey. However, there may still have been an unintended bias in favor of telemedicine due to the simultaneous implementation of the new service and its evaluation. This study also had a response rate of 44% which could have led to biased results, but this response rate is similar to the response rate of another study profiling interfacility transfer communication (31). An additional limitation was that survey data were not collected directly from the pre-transfer nurse nor the family. It is possible that the ED nurse workload and familiarity with telemedicine could have affected both the choice of handoff mode and the ability of the nurse to provide a quality handoff. Further, we report a statistically significant difference in nurse preparedness, but this statistical difference may not reflect a clinically relevant difference in care. Future studies, may investigate the role of telemedicine handoffs in changing nurse care. Recall bias may also affect this study. To address this, survey reminders were sent less than a week after handoff occurrence, surveys with a recall time longer than 14 days were excluded from analysis, and survey recall time was included in the multivariable analyses. Lastly, this study could have limited generalizability, as UCDH has been using telemedicine for physician communication and is a part of the PICU culture. This study also focused on direct transfers from pre-transfer hospital EDs to the PICU whereas other hospitals may prefer ED to ED interfacility transfer.
Conclusion:
The use of telemedicine for nurse-to-nurse interfacility handoffs seems to be associated with increased nurse preparedness upon patient arrival in the PICU. Telemedicine is feasible for nurse-to-nurse handoffs of critically ill children and gives the opportunity to the nurse to communicate with the patient’s family and transport team. Further research is needed to demonstrate that telemedicine during nurse handoffs improves communication, decreases preventable adverse events and impacts family and provider satisfaction.
Supplementary Material
ACKNOWLEDGEMENTS
We would like to thank the following: Patrick Romano, Laurel Beckett, and Kathy Kim for their insights on survey design; Daniel Tancredi and Heejung Bang for advice on statistical analysis; Gary Wold, Aron Farbstein and George Wu for providing telemedicine technical support for the nurses; Tracy Mincks, Ryan King, and Valerie Maestas for their invaluable assistance with workflow and implementation above their normal duties as hospital unit service coordinators; and all of the survey respondents.
Conflicts of Interest and Sources of Funding: Monica K. Lieng was supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health (NIH), through grant number UL1 TR001860 and linked award TL1 TR001861. Jennifer L. Rosenthal was supported by NCATS, NIH, through grant number UL1 TR001860 and linked award KL2 TR001859. The remaining authors have disclosed that they do not have any potential conflicts of interest. The telemedicine infrastructure for this study was developed with funds from grant number G01RH27872 from the Health Resources and Services Administration (HRSA), Federal Office of Rural Health Policy, Office for the Advancement of Telehealth (OAT) and from grant number H3AMC24073 from Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB), Emergency Medical Services for Children (EMSC) Program, State Partnership Regionalization of Care (SPROC).
Copyright form disclosure: Ms. Lieng’s institution received funding from National Center for Advancing Translational Sciences (NCATS), National Institutes of Health (NIH) - UL1 TR001860 and linked award TL1 TR001861 and KL2 TR001859. Ms. Lieng and Dr. Rosenthal received support for article research from the NIH. Dr. Rosenthal’s institution received funding from NCATS NIH - UL1 TR001860 and linked award KL2 TR001859. The remaining authors have disclosed that they do not have any potential conflicts of interest.
APPENDIX
Appendix 1.
Survey
Footnotes
Reprints: No reprints required.
Tweet: Telemedicine for interfacility handoffs is associated with improved nurse preparedness to admit critically ill pediatric patients.
REFERENCES
- 1.Ong M-S, Coiera E: A systematic review of failures in handoff communication during intrahospital transfers. Jt Comm J Qual Patient Saf 2011; 37:274–284 [DOI] [PubMed] [Google Scholar]
- 2.Starmer AJ, Sectish TC, Simon DW, et al. : Rates of medical errors and preventable adverse events among hospitalized children following implementation of a resident handoff bundle. JAMA 2013; 310:2262–2270 [DOI] [PubMed] [Google Scholar]
- 3.Arora V, Johnson J, Lovinger D, et al. : Communication failures in patient sign-out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care 2005; 14:401–407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosenthal JL, Hilton JF, Teufel RJ, et al. : Profiling Interfacility Transfers for Hospitalized Pediatric Patients. Hospital Pediatrics 2016; 6:345–353 [DOI] [PubMed] [Google Scholar]
- 5.Usher MG, Fanning C, Wu D, et al. : Information handoff and outcomes of critically ill patients transferred between hospitals. Journal of Critical Care 2016; 36:240–245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harvey JB, Yeager BE, Cramer C, et al. : The Impact of Telemedicine on Pediatric Critical Care Triage*. Pediatric Critical Care Medicine 2017; 18:e555–e560 [DOI] [PubMed] [Google Scholar]
- 7.Apker J, Mallak LA, Gibson SC: Communicating in the “gray zone”: perceptions about emergency physician hospitalist handoffs and patient safety. Academic Emergency Medicine 2007; 14:884–894 [DOI] [PubMed] [Google Scholar]
- 8.Gonzalez CE, Brito-Dellan N, Banala SR, et al. : Handoff Tool Enabling Standardized Transitions Between the Emergency Department and the Hospitalist Inpatient Service at a Major Cancer Center:. Am J Med Qual 2018; 14:106286061877609. [DOI] [PubMed] [Google Scholar]
- 9.Nacht J, Macht M, Ginde AA: Interhospital Transfers from U.S. Emergency Departments: Implications for Resource Utilization, Patient Safety, and Regionalization. Academic Emergency Medicine 2013; 20:888–893 [DOI] [PubMed] [Google Scholar]
- 10.Rosenthal JL, Okumura MJ, Hernandez L, et al. : Interfacility Transfers to General Pediatric Floors: A Qualitative Study Exploring the Role of Communication. Acad Pediatr 2016; 16:692–699 [DOI] [PubMed] [Google Scholar]
- 11.Dayal P, Hojman NM, Kissee JL, et al. : Impact of Telemedicine on Severity of Illness and Outcomes Among Children Transferred From Referring Emergency Departments to a Children’s Hospital PICU. Pediatric Critical Care Medicine 2016; 17:516–521 [DOI] [PubMed] [Google Scholar]
- 12.Marcin JP, Nesbitt TS, Kallas HJ, et al. : Use of telemedicine to provide pediatric critical care inpatient consultations to underserved rural Northern California. J Pediatr 2004; 144:375–380 [DOI] [PubMed] [Google Scholar]
- 13.Labarbera JM, Ellenby MS, Bouressa P, et al. : The impact of telemedicine intensivist support and a pediatric hospitalist program on a community hospital. Telemed J E Health 2013; 19:760–766 [DOI] [PubMed] [Google Scholar]
- 14.Desai S, Williams ML, Smith AC: Teleconsultation from a secondary hospital for paediatric emergencies occurring at rural hospitals in Queensland. J Telemed Telecare 2013; 19:405–410 [DOI] [PubMed] [Google Scholar]
- 15.Dharmar M, Kuppermann N, Romano PS, et al. : Telemedicine consultations and medication errors in rural emergency departments. Pediatrics 2013; 132:1090–1097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heath B, Salerno R, Hopkins A, et al. : Pediatric critical care telemedicine in rural underserved emergency departments. Pediatric Critical Care Medicine 2009; 10:588–591 [DOI] [PubMed] [Google Scholar]
- 17.Flodgren G, Rachas A, Farmer AJ, et al. : Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2015; 15:CD002098–583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Solet DJ, Norvell JM, Rutan GH, et al. : Lost in translation: challenges and opportunities in physician-to-physician communication during patient handoffs. Acad Med 2005; 80:1094–1099 [DOI] [PubMed] [Google Scholar]
- 19.Mardis T, Mardis M, Davis J, et al. : Bedside Shift-to-Shift Handoffs: A Systematic Review of the Literature. J Nurs Care Qual 2016; 31:54–60 [DOI] [PubMed] [Google Scholar]
- 20.Horwitz LI, Rand D, Staisiunas P, et al. : Development of a handoff evaluation tool for shift-to-shift physician handoffs: the Handoff CEX. J Hosp Med 2013; 8:191–200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smeulers M, Lucas C, Vermeulen H: Effectiveness of different nursing handover styles for ensuring continuity of information in hospitalised patients. Cochrane Database Syst Rev 2014; 43:CD009979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hu PJ, Chau PYK, Sheng ORL, et al. : Examining the Technology Acceptance Model Using Physician Acceptance of Telemedicine Technology. Journal of Management Information Systems 2015; 16:91–112 [Google Scholar]
- 23.R Development Core Team: R: A language and environment for statistical computing [Internet]. Available from: http://www.R-project.org/
- 24.Pinheiro J, Bates D, DebRoy S, et al. : Linear and Nonlinear Mixed Effects Models [R package nlme version 3.1–137] [Internet]. 2018; Available from: https://CRAN.R-project.org/package=nlme
- 25.Hijmans RJ, Williams E, Vennes C: Spherical Trigonometry [R package geosphere version 1.5–7] [Internet]. [cited 2018 Oct 19] Available from: https://CRAN.R-project.org/package=geosphere
- 26.Pustejovsky JE, Tipton E: Small-Sample Methods for Cluster-Robust Variance Estimation and Hypothesis Testing in Fixed Effects Models [R Package 0.3.2] [Internet]. Journal of Business & Economic Statistics 2017; 36:672–683 Available from: https://cran.r-project.org/web/packages/clubSandwich/index.html [Google Scholar]
- 27.Nadar M, Jouvet P, Tucci M, et al. : Impact of Synchronous Telemedicine Models on Clinical Outcomes in Pediatric Acute Care Settings: A Systematic Review. Pediatric Critical Care Medicine 2018; 1 [DOI] [PubMed] [Google Scholar]
- 28.Parent B, LaGrone LN, Albirair MT, et al. : Effect of Standardized Handoff Curriculum on Improved Clinician Preparedness in the Intensive Care Unit: A Stepped-Wedge Cluster Randomized Clinical Trial. JAMA Surg 2018; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Feng X, Colvin J, French J, et al. : Utilization of Quality Improvement Methodology to Standardize Communication of Outside Hospital Transfers in a General Surgery Program. Journal of Surgical Education 2018; [DOI] [PubMed] [Google Scholar]
- 30.Hribar MR, Read-Brown S, Goldstein IH, et al. : Secondary use of electronic health record data for clinical workflow analysis. J Am Med Inform Assoc 2018; 25:40–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rosenthal JL, Romano PS, Kokroko J, et al. : Receiving Providers’ Perceptions on Information Transmission During Interfacility Transfers to General Pediatric Floors. Hospital Pediatrics 2017; hpeds.2016–0152 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.