Short abstract
Introduction
In contrast to orthotopic thyroid carcinoma, primary accessory thyroid carcinoma is very rare. We herein report a case involving primary accessory thyroid carcinoma in a patient with normal ultrasonography of the orthotopic thyroid and negative 99mTcO4− single-photon emission computed tomography (SPECT) scintigraphy.
Case presentation: A computed tomography (CT) scan showed soft tissue nodules at the left anterior edge of the thyroid cartilage. To determine whether the mass was accessory thyroid tissue, 99mTcO4− SPECT/CT was performed, and the findings were negative. However, pathological examination after resection showed that mass was a primary accessory thyroid papillary carcinoma. The 1-year follow-up ultrasound showed no lesion at the orthotropic thyroid and neck incision sites.
Conclusions
This case suggests that negative 99mTcO4− SPECT/CT imaging may not completely exclude the possibility of thyroid carcinoma. A punch biopsy or postoperative pathological examination is necessary for the diagnosis.
Keywords: Thyroid, cancer, scintigraphy, diagnosis, single-photon emission computed tomography, biopsy
Introduction
Accessory thyroid tissue is located between the tongue and the diaphragm. It originates from abnormal growth or descent of the original thyroid gland in the foetus as a result of abnormal migration or differentiation of the endoderm cells.1 Accessory thyroid carcinoma may occur in any part of the body but is more common in the neck areas such as the tongue, hyoid bone, trachea, larynx, oesophagus, and retrosternal region.2 Because primary cancer in accessory thyroid tissue is very rare, a cervical mass outside of the normal thyroid gland should be examined for carcinoma.3 In 2015, the American Thyroid Association published a guideline for the diagnosis and treatment of thyroid nodules and differentiated thyroid carcinoma, recommending ultrasonography as a preferred method for diagnosing thyroid nodules.4 For accessory thyroid tissue, however, the clinician must first determine whether the mass originates from the thyroid tissue and then whether it is benign or cancerous. Radionuclide imaging, including 131I imaging and 99mTcO4− imaging, is a well-adopted and noninvasive technique with which to diagnose accessory thyroid tissue or accessory thyroid carcinoma.5 Because of the short half-life and low γ-ray energy, 99mTcO4− single-photon emission computed tomography/computed tomography (SPECT/CT) is commonly used to identify accessory thyroid glands.5 This case suggests that negative 99mTcO4− SPECT/CT imaging may not completely exclude the possibility of parathyroid carcinoma and that a punch biopsy or postoperative pathological examination is necessary for an accurate diagnosis.
Case presentation
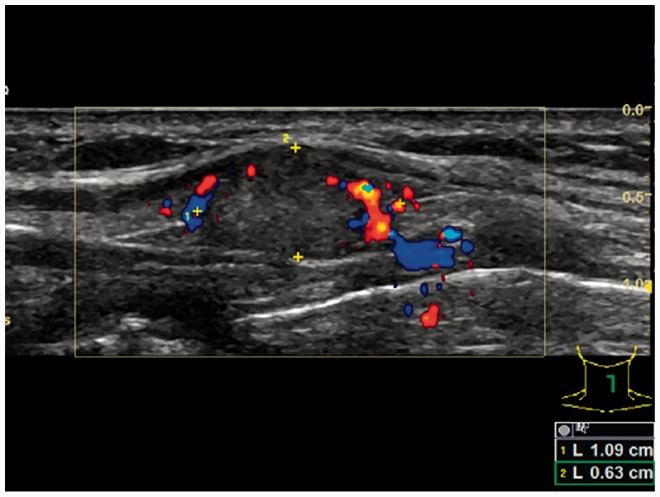
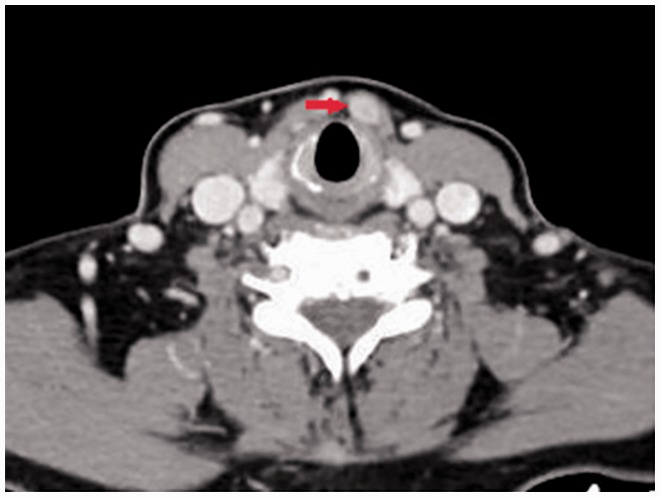
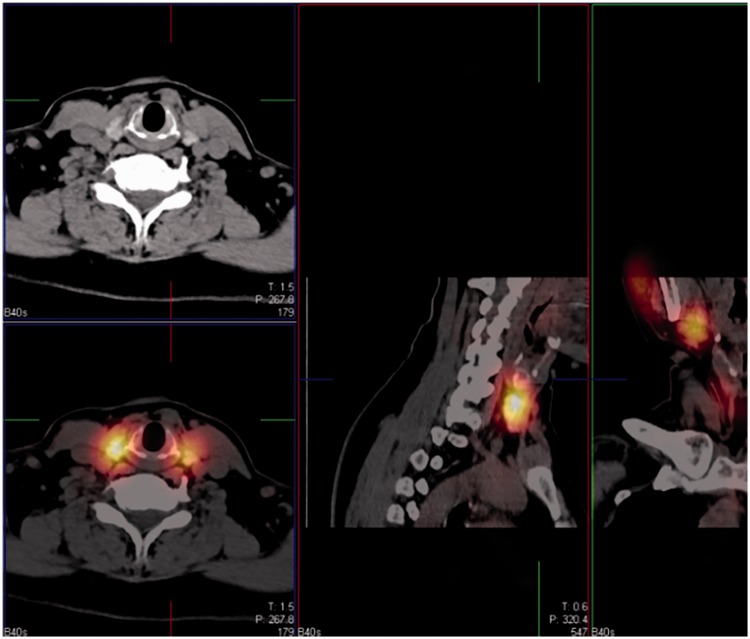
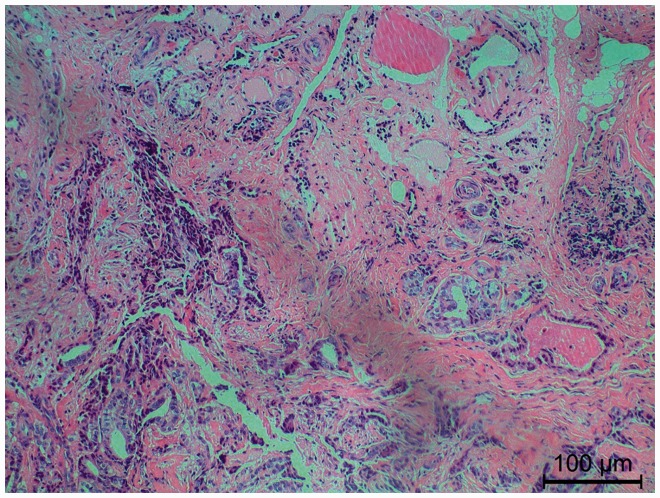
A 54-year-old woman presented with a 10-day history of a painless mass in the anterior neck. The mass moved up and down with swallowing, and the surface of the mass was smooth. She denied neck pain while eating and had no fever or history of malignancy, tuberculosis, or neck surgery. Ultrasonography revealed normal and homogeneous echogenicity in the thyroid gland with an intact capsule and no abnormal lymph nodes in the neck. A spherical, well-demarcated, 1.1- × 0.6-cm mass with low echogenicity was identified between the hyoid bone and the thyroid gland. The mass was not connected to the thyroid gland and was a solid hypoechoic nodule. Colour Doppler flow imaging showed blood flow signals in the surrounding area (Figure 1). Ultrasonography revealed a space-occupying lesion in the anterior neck. An enhanced CT examination of the neck showed homogeneous intensity of the thyroid gland without signs of a mass and a soft tissue nodule at the left anterior edge of the thyroid cartilage (Figure 2). To determine whether the nodule originated from the accessory thyroid, 99mTcO4− SPECT/CT was performed, and the results were negative (Figure 3). This excluded accessory thyroid tissue. The patient’s laboratory tests showed normal levels of free triiodothyronine, free thyroxine, and thyroid-stimulating hormone and negative carcinoembryonic antigen, cancer antigen 125, and carbohydrate antigen 19-9 levels. However, because both ultrasonography and CT examinations revealed a neck mass, the mass was resected under local anaesthesia. A solid mass was found and excised completely. Histological examination showed that the tumour cells formed glandular and papillary structures infiltrating into the fibrous stroma. The tumour cells were cubic or columnar with overlapping nuclei crowded to form a ground-glass appearance. The nuclear grooves were visible and surrounded by a few thyroid follicular cells (Figure 4). Immunohistochemical analyses showed cytoplasmic triacylglycerol staining and nuclear thyroid transcription factor 1 staining (Figure 4). The pathological findings suggested a papillary thyroid carcinoma. Taking the results of clinical and imaging studies together, the mass was considered an accessory thyroid papillary carcinoma. This study was approved by the ethical committee of Soochow University. Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Figure 1.
Ultrasound image showing a mass with slightly low echogenicity surrounded by blood flow signals.
Figure 2.
Enhanced computed tomography image showing a significantly enhanced mass with contrast (red arrow).
Figure 3.
99mTcO4− single-photon emission computed tomography/computed tomography images showing absence of 99mTcO4− uptake in the mass.
Figure 4.
Immunohistochemical staining of the tumour cells showing glandular and papillary structures that infiltrate into the fibrous stroma (×100).
Discussion and conclusions
Accessory thyroid gland or primary accessory thyroid carcinomas are often initially misdiagnosed, and pathological examination is needed to confirm the diagnosis. The most common thyroid carcinoma is papillary carcinoma (well to moderately differentiated), and other types are rare.6 Malignant tumours in the accessory thyroid tissue are extremely rare, and only 43 cases have been reported in the literature, including 10 cases of papillary thyroid carcinoma.7 Papillary thyroid carcinoma is the most common subtype of carcinoma in accessory thyroid tissue.8 Several techniques are available to distinguish a cervical mass from accessory thyroid gland tissue or primary accessory thyroid carcinoma. Colour Doppler ultrasound is able to show whether a normal thyroid gland is present in the neck and to reveal the echogenicity and blood supply of the mass. Radionuclide imaging can be used to diagnose accessory thyroid tissue because 99mTcO4− is specifically concentrated in the thyroid tissue. Enhanced CT and magnetic resonance imaging can locate the lesion and display the intensity and size of the mass. Puncture biopsy can be used to determine the mass type. When diagnosing accessory thyroid carcinoma, care should be taken to distinguish it from a round or oval thyroglossal cyst located in the upper and lower regions of the thyroid hyoid and from a tuberculous abscess in the lymph node, which is more common in young women and presents as multiple unilateral, multi-zone enlarged lymph nodes in which liquefaction and necrosis may occur. The former shows an enhanced cyst wall without enhanced nodules and occasionally with a capsular septum, while the latter often gives rise to flower-lace-like enhancement on enhanced CT with a blurred and coarse fat layer and spot- or patch-like calcification within the lesion.
In the present case, the mass showed no 99mTcO4− uptake, resulting in a misdiagnosis of a non-thyroid tissue lesion. However, the pathological examination confirmed that it was a primary accessory thyroid papillary carcinoma. One reason for the negative 99mTcO4− uptake might be attributed to the sodium–iodine transporter on the membrane of follicular cells in normal thyroid tissue; this transporter takes up and concentrates iodine. Technetium is a member of the iodine family. Therefore, 99mTcO4− might be absorbed and concentrated by the thyroid tissue. However, the absorbed 99mTcO4− is unable to be organified by the thyroid tissue to synthesise thyroid hormone in the thyroid cells. Thus, it can only reflect the uptake function, not the organification function, of iodine in the thyroid cells.9 Because of the poor differentiation of cancerous tissues, the expression level of the sodium–iodine transporter in primary accessory thyroid tissue is lower than that in normal thyroid tissue. Therefore, in routine thyroid static imaging, cancerous tissues may generate “cool nodules” or “cold nodules” because of reduced uptake of 99mTcO4−.10 Our patient had a primary accessory thyroid papillary carcinoma; thus, the ability of the accessory thyroid carcinoma tissues to take up 99mTcO4− was probably lower because of the presence of a normal orthotopic thyroid. The 99mTcO4− imaging characteristics of accessory thyroid carcinoma have not been reported to date. A few case reports have described the uptake of 99mTcO4− by thyroid carcinoma,11,12 showing that the uptake is closely related to the differentiation of the thyroid carcinoma. Highly differentiated thyroid carcinoma has functions similar to those of normal thyroid tissue. Therefore, highly differentiated thyroid carcinoma and its metastatic lesions may be able to uptake 99mTcO4−.
Although 99mTcO4− SPECT/CT has been used as the gold standard noninvasive imaging technique with which to diagnose a simple ectopic thyroid gland, it may generate a misdiagnosis when accessory thyroid tissue is cancerous. To avoid this, when 99mTcO4− SPECT/CT images are negative, 131I SPECT/CT should be performed, although biopsy or postoperative pathological examination is still ultimately needed to confirm the diagnosis. Additionally, the concentration of 99mTcO4− in the thyroid tissue is not as specific as the concentration of iodine, and the result may be different from that of scintigraphy with radioiodine. Finally, we did not perform cytological examination with a fine needle to confirm our diagnosis.
Abbreviations
SPECT: single-photon emission computed tomography; CT: computed tomography
Authors’ contributions
YM and FQ designed the study. FQ, JW, YL, and SL conducted the diagnosis and treatments. FQ and JW drafted the manuscript. All authors read and approved the final manuscript.
Availability of data and material
The datasets used during the current study are available from the corresponding author on reasonable request.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Ghanem N, Bley T, Altehoefer C, et al. Ectopic thyroid gland in the porta hepatis and lingua. Thyroid 2003; 13: 503–507. DOI: 10.1089/105072503322021188 [DOI] [PubMed] [Google Scholar]
- 2.Gierek T, Klimczak-Gołab L, Jura-Szołtys E. Ectopic thyroid glad–a case report. Otolaryngol Pol 2003; 57: 421. [PubMed] [Google Scholar]
- 3.Basaria S, Westra WH, Cooper DS. Ectopic lingual thyroid masquerading as thyroid cancer metastases. J Clin Endocrinol Metab 2001; 86: 392–395. DOI: 10.1210/jcem.86.1.7130 [DOI] [PubMed] [Google Scholar]
- 4.Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 2016; 26: 1–133. DOI: 10.1089/thy.2015.0020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Verelst J, Chanoine JP, Delange F. Radionuclide imaging in primary permanent congenital hypothyroidism. Clin Nucl Med 1991; 16: 652–655. [DOI] [PubMed] [Google Scholar]
- 6.Kondo T, Katoh R, Omata K, et al. Incidentally detected liver metastasis of well-differentiated follicular carcinoma of the thyroid, mimicking ectopic thyroid. Pathol Int 2000; 50: 509–513. [DOI] [PubMed] [Google Scholar]
- 7.Choi JY, Kim JH. A case of an ectopic thyroid gland at the lateral neck masquerading as a metastatic papillary thyroid carcinoma. J Korean Med Sci 2008; 23: 548–550. DOI: 10.3346/jkms.2008.23.3.548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kushwaha JK, Sonkar AA, Goel MM, et al. Papillary carcinoma of thyroid arising from ectopic thyroid tissue inside branchial cleft cyst: a rare case. BMJ Case Rep 2012; 2012: pii: bcr0220125783. DOI: 10.1136/bcr.02.2012.5783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu G, Li N, Li X, et al. Thyroid remnant estimation by diagnostic dose (131)I scintigraphy or (99m)TcO4(-) scintigraphy after thyroidectomy: a comparison with therapeutic dose (131)I imaging. Biomed Res Int 2016; 2016: 4763824. DOI: 10.1155/2016/4763824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fujiyoshi T, Mogi G. Ectopic malignant cervical thymoma in association with occult papillary adenocarcinoma in thyroid. Nihon Kikan Shokudoka Gakkai Kaiho 2010. 36: 37–44. [Google Scholar]
- 11.Scott GC, Meier DA, Dickinson CZ. Cervical lymph node metastasis of thyroid papillary carcinoma imaged with fluorine-18-FDG, technetium-99m-pertechnetate and iodine-131-sodium iodide. J Nucl Med 1995; 36: 1843–1845. [PubMed] [Google Scholar]
- 12.Verma N, Singh-Wadhwa S, Arvela OM. Metastatic thyroid cancer visualized on technetium pertechnetate and iodine-131 scintigraphy. Clin Nucl Med 2002; 27: 610. DOI: 10.1097/01.RLU.0000020744.19209.35 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used during the current study are available from the corresponding author on reasonable request.